- 1Kings College London, London, United Kingdom
- 2Guys and St Thomas’ NHS Foundation Trust, London, United Kingdom
- 3Moorfields Eye Hospital NHS Foundation Trust, London, United Kingdom
- 4Institute of Neurology, University College London, London, United Kingdom
- 5South London and Maudsley NHS Foundation Trust, London, United Kingdom
Visual snow syndrome (VSS) is a neurological disorder characterized by intrusive visual symptoms and associated with dysregulation in brain networks, including the Salience Network, Default Mode Network, and thalamocortical circuits. This perspective paper examines the application of mindfulness-based cognitive therapy modified for visual symptoms (MBCT-vision) as an intervention for VSS. Drawing on clinical experience, our recent open-label study, and ongoing randomized controlled trial, we propose that VSS symptoms may perpetuate through attentional mechanisms, including heightened vigilance and threat attribution. We outline how mindfulness practices in MBCT-vision address these processes by enhancing attentional flexibility, increasing metacognitive awareness, and fostering a non-reactive stance toward symptoms. The group-based format of MBCT-vision provides additional therapeutic benefits through shared understanding and validation. We discuss potential neuroplastic mechanisms underlying observed improvements, particularly involving the Default Mode Network. This paper advances the understanding of mindfulness mechanisms in VSS and provides a foundation for developing comprehensive, evidence-based approaches that integrate neurobiological insights with person-centered therapeutic strategies for this challenging condition.
Introduction
Visual snow syndrome (VSS) is a disorder involving brain network dysregulation, in the presence of normal ophthalmological and neurological examinations (1–3). VSS causes intrusive and disruptive visual symptoms, including “visual snow”: so-called because of the resemblance to “TV show” (analog TV static due to background electromagnetic radiation). Also reported to be intrusive are: after-images, trailing of moving images and entoptic phenomena (arising within the eye itself) such as flashes and floaters, and the blue field entoptic phenomenon (caused by the movement of white blood cells through retinal vessels). Beyond visual disruption, individuals often experience significant non-visual symptoms, including depersonalization and tinnitus (4).
Our recent open-label study using a mindfulness-based intervention, mindfulness-based cognitive therapy modified for visual symptoms (MBCT-vision), improved self-reported VSS symptoms with associated changes on functional magnetic resonance imaging (fMRI) (5).
Building on these findings, we share our perspective on how mindfulness can benefit people with VSS. Our perspective is informed by clinical experience treating individuals with VSS, including observations from our open-label study (5) and ongoing randomized controlled trial (ClinicalTrials.gov: NCT06018103).
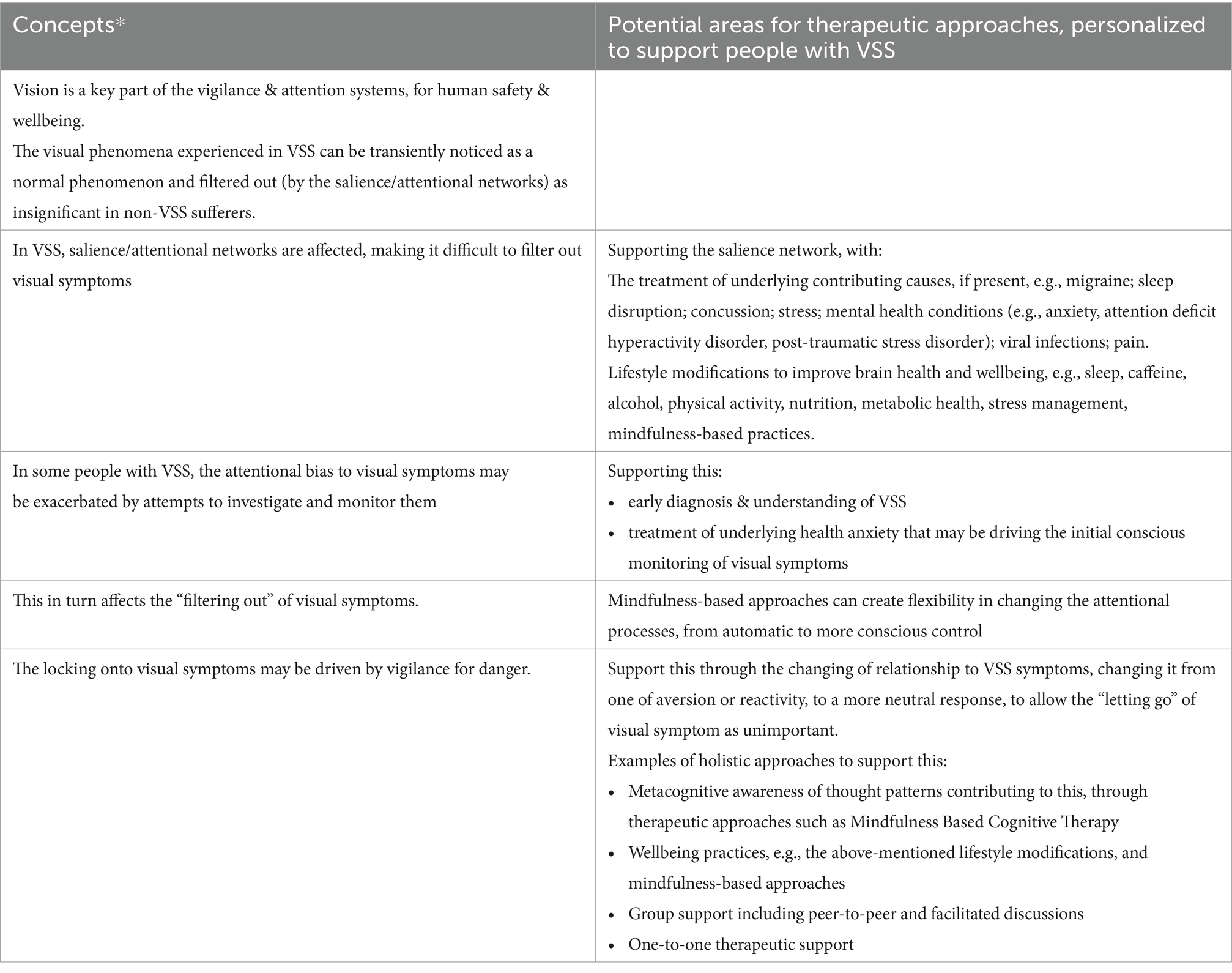
This paper aims to advance the understanding of mindfulness mechanisms in VSS and provide a foundation for developing comprehensive, evidence-based treatment approaches. By examining the intersection of salience and attentional networks, mindfulness practices, and VSS symptomatology, we offer insights into a holistic, person-centered therapeutic strategy for this challenging condition (summarized in Box 1 and Figure 1).
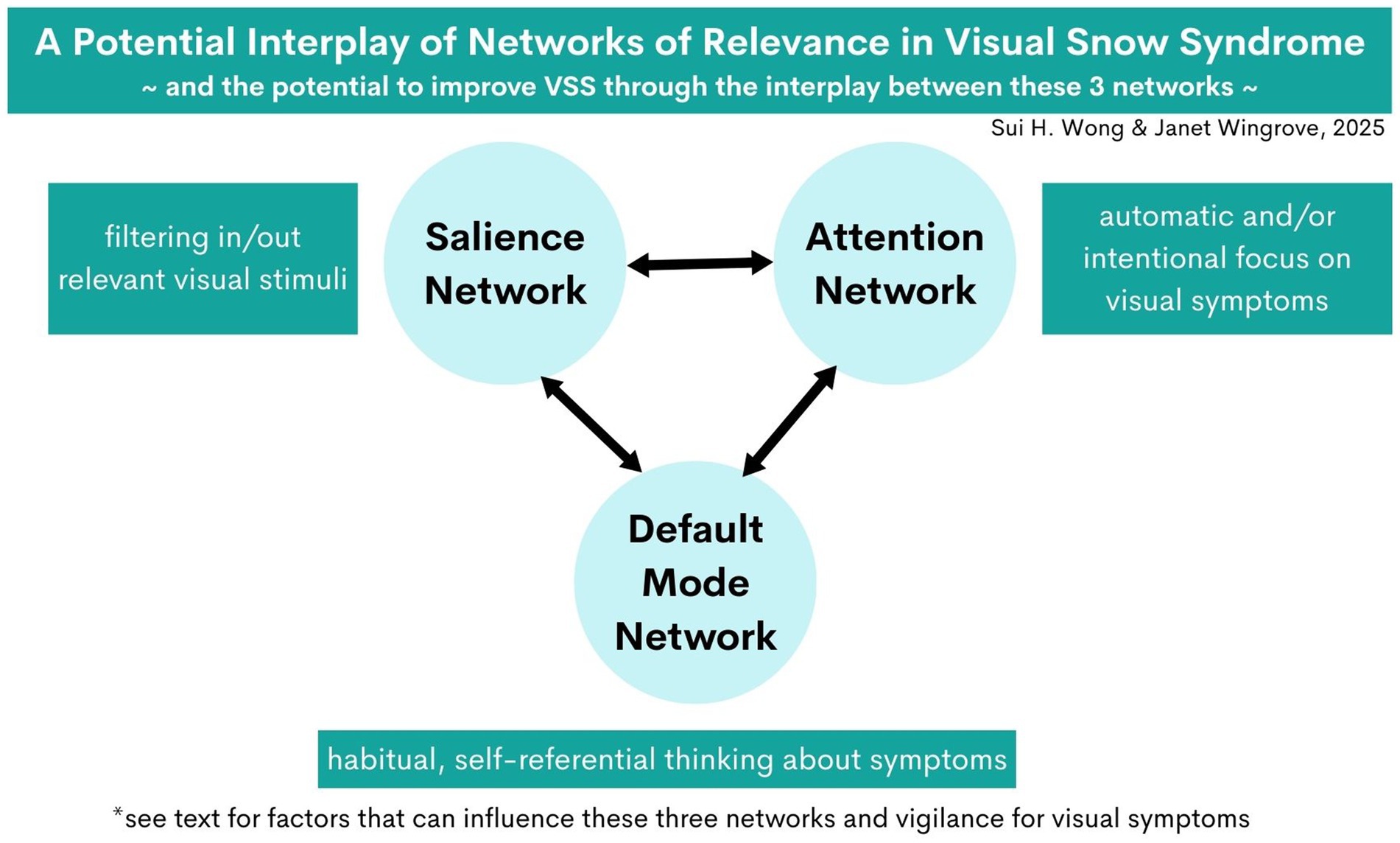
Figure 1. A potential interplay of networks of relevance in Visual Snow Syndrome (VSS), and the potential to improve VSS through the interplay between these three networks.
BOX 1. Holistic model of therapeutic approaches to support people with VSS
*These approaches can support neuroplasticity and modulating the heightened visual networks in VSS. NB: see full text for discussions and references.
Attentional processes in VSS and the role of mindfulness
VSS is a brain network disorder (2). Current evidence implicates three key networks: the salience network (SN), default mode network (DMN), and thalamocortical circuits (5–7). These networks play crucial roles in attention regulation, vigilance maintenance, and the processing of emotional and behavioral responses (8–11).
Considering VSS through the lens of attention theory provides valuable insights into symptom perpetuation and potential therapeutic approaches. An established model of the attentional system considers three main components: alerting; orienting; and executive control (12, 13). Alerting refers to achieving and maintaining a state of heightened sensitivity to incoming stimuli. Orienting involves selecting specific information from sensory input. Executive control is responsible for monitoring and resolving conflicts among thoughts, feelings, and responses.
Attention is a selective process that allows us to focus on specific stimuli while filtering out irrelevant information (13, 14). This can be influenced by factors including self-relevance (15) and stimulus selection for the promotion of survival and wellbeing (14).
The selection process operates through a combination of automatic and controlled mechanisms (12, 13). Automatic processes occur rapidly and without conscious effort, while controlled processes are deliberate and require conscious awareness. However, newer research suggests that these two processes can become more flexible and context-dependent, contrary to classical theories that portrayed them as a rigid distinction (16).
This potential for flexibility can help us understand the experience of VSS in some people, e.g., symptom monitoring which become more automatic over time; and the potential for therapeutic advances, e.g., changing automatic processes to become more deliberate with mindfulness practices, thereby an opportunity for change and neuroplasticity to improve VSS.
VSS symptoms may perpetuate through an interplay between the salience and attentional networks, with influence by the thalamocortical circuits. Disruptions to these lead to an increased awareness of visual symptoms that would normally be “filtered out.” The visual phenomenon experienced in VSS can be transiently noticed as a normal phenomenon and “filtered out” as insignificant in non-VSS sufferers. However, this “filtering out” process can be affected by various factors such as migraines, sleep deprivation, anxiety or stress (17–20).
The pathophysiological cascade in VSS may begin with an increased awareness of a range of visual phenomena, leading to attentional orientation toward these phenomena. This initial awareness of visual symptoms then leads on to an orienting of attention to visual symptoms, which can become more automatic, if unmanaged.
This process can become self-perpetuating through two mechanisms:
i. threat attribution: interpreting the symptoms as a source of threat because of the way they interfere with current tasks, or because of the perception that they signify potential dangers such as blindness;
ii. monitoring behavior: e.g., to check if the symptoms are getting worse or better; to describe them to healthcare practitioners; or to get a diagnosis.
The presence of co-morbid health anxiety may further perpetuate this orienting of attention to visual symptoms. The concept that VSS is perpetuated by maladaptive attentional processes is not yet well established in the literature and is based on our perspective with the rationale outlined above. This concept has been shaped by our discussions with people about the onset of their VSS symptoms, their initial reactions, and subsequent monitoring habits. We are currently undertaking a qualitative study to further understand this and will be publishing the results in due course.
Heightened vigilance and attention
This heighted awareness of VSS symptoms may be linked with a heightened vigilance to threat. This heightened vigilance and may explain the broader phenomenology of VSS beyond visual disturbances, such as anxiety, feeling of disconnection from oneself or reality, and cognitive difficulties (4).
Additionally, aversion to VSS symptoms may lead to deliberate efforts to ignore or suppress them, which may further impair attentional control (17, 21). This further perpetuates a cycle of heightened vigilance: visual symptoms worsen anxiety, mood and sleep, which in turn affects the salience network function, further impairing perceptual filtering and leading to increased symptom awareness.
Research in cognitive psychology has shown that attention allocation is significantly influenced by personal relevance and perceived threat (22). This is relevant in VSS, as the persistent and intrusive nature of VSS symptoms carry high personal relevance and potential threat value, further creating challenges for attention regulation.
Traditional advice to “ignore” symptoms contradicts basic attention mechanisms, as the skills required such as disengaging from visual stimuli and focus-switching (12, 13) become especially challenging when symptoms are persistent and perceived as threatening.
This is where mindfulness-based approaches can play a crucial role in the treatment of VSS, by directly addressing these attentional challenges. Rather than attempting to suppress symptom awareness, mindfulness practices help break the cycle of heightened vigilance and symptom perpetuation in VSS by modifying fundamental attention processes. This approach enhances attention regulation capabilities while developing non-reactive awareness.
Mindfulness and MBCT-vision for VSS
Mindfulness is defined as “the awareness that arises from paying attention in a particular way; on purpose, in the present moment and non-judgmentally.” (23). Mindfulness practices often incorporate the qualities of non-judgment, kindness, curiosity, friendliness and openness (24, 25).
MBCT-vision is a mindfulness-based intervention delivered as a structured group-learning program over 8 weeks. MBCT-vision is a modification of the Mindfulness-Based Cognitive Therapy (MBCT) program created by Segal, Williams, Teasdale (26), built on the Mindfulness-Based Stress Reduction (MBSR) program created by Kabat-Zinn (23).
In the MBCT program, participants learn a repertoire of mindfulness practices, structured around weekly themes with practices that include sitting, movement and informal practices during daily activities. Each theme builds on the next over 8 weeks. In addition to mindfulness skills, participants learn meta-cognitive skills, e.g., awareness of thought patterns that may be affecting their wellbeing.
The groups meet once weekly for 8 weeks and are given daily home practices in between group meetings. The group meetings include guided mindfulness practices and structured discussions about their daily home practices, facilitating experiential and reflective learning.
In developing a mindfulness-based intervention for VSS, we chose MBCT as the base structure, due to extensive research on MBCT as a clinical intervention. MBCT has been studied in numerous clinical trials and is recommended by the National Institute of Clinical Excellent in the United Kingdom for preventing recurrent depression (27). Additionally, MBCT has been shown to be effective in health anxiety (28), which in our experience may also be co-existent in VSS.
We modified MBCT into MBCT-vision for the treatment of VSS, by removing structured discussions about preventing depression. Instead, we included discussions about VSS; mindfulness and other lifestyle modifications for improving resilience and wellbeing (detailed further below); and guidance on modifications to mindfulness practices due to VSS symptoms where necessary.
Practices are taught as described in the original MBCT program, which includes body scan, focus on breath, mindful movement (similar to certain practices of Tai Chi or Yoga), and a technique called “3-step breathing space” which is a three step process of being aware of body sensations, emotions, thoughts, situation; followed by anchoring on the breath; and expanding awareness and attention to the wider present moment again. We also added additional sensory tactile practices such as tapping of the body to help with anchoring to the present moment, alongside the wider principles of breath and body, which we find particularly useful in the context of depersonalization symptoms.
Mechanisms of mindfulness in VSS
The mindfulness practices taught in MBCT-vision help participant become better at noticing the connections between their body sensations, emotions, and thought processes.
Mindfulness practices can create a shift in how individuals relate to their symptoms by working with the attentional and emotional salience of VSS experiences. Mindfulness-based interventions have been shown to enhance attentional control and emotional regulation (29), allowing individuals with VSS to relate to their symptoms in a less reactive and more accepting manner.
By cultivating non-judgmental awareness and the ability to observe symptoms without automatically engaging with them, mindfulness may help reduce the distress associated with VSS and improve overall quality of life (23). This approach acknowledges the difficulty of “ignoring” symptoms while providing practical tools for managing attention and emotional responses to VSS experiences.
Mindfulness skills allow people with Visual Snow Syndrome (VSS) to:
• Practice disengaging attention from one stimulus and redirecting it to another, enhancing attentional flexibility (25).
• Increase awareness of attentional processes, including recognizing patterns of conscious, deliberate monitoring of symptoms and learning to disengage from this habitual focus (24).
• Cultivate the ability to bring other aspects of experience, particularly body sensations and other senses, into the foreground of awareness. This practice can create conditions for VSS symptoms to recede into the background of perception (30).
• Recognize habitual patterns of aversion toward symptoms and understand their consequences. This awareness allows individuals to develop a more balanced relationship with their VSS experiences (31).
• Learn to allow VSS symptoms to be present without excessive attachment (treating them as overly important) or aversion (responding with fear or tension). This approach fosters a more accepting and less reactive stance toward symptoms (23).
These mindfulness skills collectively contribute to a more adaptive way of relating to VSS symptoms, potentially reducing their impact on daily life and well-being.
Group learning in MBCT-vision
The cognitive skills that participants develop through reflective learning during group discussions, help them identify patterns that may be perpetuating their symptoms. These discussions, when anchored in the experience of mindfulness practices, are integral to the process of changing their relationship to VSS.
Participants learn to observe their thoughts, emotions, and bodily sensations related to VSS with increased awareness and objectivity. This metacognitive perspective allows them to recognize automatic patterns of reactivity and develop more adaptive responses to their symptoms.
Moreover, the group setting provides a unique therapeutic environment. Feeling understood by the facilitators and sharing experiences with other participants who face similar challenges can significantly contribute to reducing the sense of threat associated with VSS symptoms. This shared understanding and validation can help normalize the experience of VSS and reduce the anxiety and isolation often associated with the condition.
The combination of mindfulness practices, cognitive skills, and group support creates a comprehensive approach to managing VSS symptoms. This multifaceted intervention aims to not only alleviate symptoms but also improve overall quality of life by fostering a more accepting and less reactive relationship with VSS experiences.
Neuroplasticity and the default mode network with MBCT-vision in VSS
The approach of anchoring in mindful mind–body practices helps participants develop a sense of psychological safety, as part of the process of settling and reducing heightened vigilance.
The default mode network (DMN) is part of the vigilance system (32) and can be modified with mindfulness practices (33). This could be the process underlying the changes on fMRI following MBCT-vision in our recent study (5). We speculate that this could also link in with a recent neuroimaging study showing reduced serotonergic and glutaminergic connectivity in VSS (34), as both serotonin and glutamine neurotransmitters are involved in DMN (35).
A regular practice is recommended to promote long lasting changes in neural networks (29), which is what we encourage participants to do after the MBCT-vision program. Our feasibility study showed that self-reported outcome using a 0–10 visual analog scale was more significant at 3 months compared to 1 week following the MBCT-vision program (5). However, the limitation was that it was an open-label study. We are therefore currently delivering an RCT.
Our current RCT includes a secondary outcome measure at 1-year. We notice that with regular practice, participants become more skilled at reducing reactivity to their visual symptoms, have more agency and skill to shift their attention as needed.
Toward a holistic, person-centered approach
Our treatment approach in MBCT-vision includes discussions on lifestyle measures that improves attentional control and executive function, i.e., improving the above-mentioned concept of the “filter.” Lifestyle modifications discussed include sleep hygiene, physical activity, nutrition, limiting excessive caffeine or alcohol, and stress management. These adjunctive topics covered in group discussions, while mindfulness remains the main focus of MBCT-vision.
The complex interplay between VSS and comorbid conditions necessitates a comprehensive treatment approach. Disruptions to the Salience Network, Thalamocortical Circuits, and Default Mode Network may be exacerbated by conditions such as migraine, anxiety, and sleep disorders (17–20). Therefore, effective management of these comorbidities becomes integral to VSS treatment success.
We advocate a holistic and personalized approach in the support of people with VSS. Our clinical experience suggests that some individuals benefit from personalized therapeutic support before engaging in group-based interventions. Individual therapy, particularly incorporating somatic or mind–body practices, can prepare participants for optimal engagement with the MBCT-vision program. This staged approach acknowledges the diverse needs of individuals with VSS and allows for appropriate therapeutic tailoring.
By simultaneously addressing network dysfunction, attention regulation, and contributing factors, this comprehensive framework aims to modify both symptoms and their underlying mechanisms, potentially leading to sustained improvement in clinical outcomes.
Future directions
The emerging understanding of VSS as a network disorder, combined with preliminary evidence for mindfulness-based interventions, opens several promising avenues for future research.
Our ongoing randomized controlled trial, which includes a qualitative sub-study with structured interviews, will provide valuable insights into both the efficacy of MBCT-vision and the lived experience of participants. The upcoming publication of these findings will help refine our theoretical framework and treatment approach.
Critical areas for future investigation include the optimization of mindfulness-based interventions for VSS, lifestyle-based interventions, identification of predictive factors for treatment response, and exploration of potential synergies between MBCT-vision and other therapeutic modalities. Furthermore, research into interventions of shorter duration, which include a focus on the fears and experiences of living with VSS could be helpful.
Additionally, research examining the neurobiological and attentional mechanisms underlying mindfulness effects in VSS, particularly through advanced neuroimaging techniques and attention tasks, may reveal new therapeutic targets and guide treatment refinement.
We suggest that studies showing changes in visual networks in VSS (2, 34, 36) are likely a downstream effect of the salience, attention and default mode networks for the above-mentioned reasons. Therefore studies focusing on the latter networks will be of particular relevance.
The development of effective treatments for VSS requires a continued commitment to rigorous research methodology while maintaining sensitivity to individual patient needs. As our understanding of VSS pathophysiology and the role of attention networks continues to evolve, integration of these insights with clinical observations will be crucial for advancing therapeutic approaches. Through this combined basic science and clinical research agenda, we aim to enhance our ability to provide effective, personalized care for individuals living with VSS. We continue in our endeavors with our current RCT, due to complete in 2027; and future related work.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
SW: Conceptualization, Writing – original draft, Writing – review & editing. JW: Conceptualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. We have received VSS research funding from Visual Snow Initiative, EyeHope, and GSTT charity. The publication cost for this article was funded by the Visual Snow Initiative.
Acknowledgments
We thank past and present participants of our Mindfulness and VSS research studies for their contribution to research; research funding that enabled our research to date, from Visual Snow Initiative, EyeHope, and GSTT charity.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The handling editor GP declared a shared affiliation with the author(s) SW at the time of review.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Bessero, A-C, and Plant, GT. Should “visual snow” and persistence of after-images be recognised as a new visual syndrome? J Neurol Neurosurg Psychiatry. (2014) 85:1057–8. doi: 10.1136/jnnp-2013-306827
2. Aeschlimann, SA, Klein, A, and Schankin, CJ. Visual snow syndrome: recent advances in understanding the pathophysiology and potential treatment approaches. Curr Opin Neurol. (2024) 37:283–8. doi: 10.1097/WCO.0000000000001258
3. White, OB, Clough, M, McKendrick, AM, and Fielding, J. Visual snow: visual misperception. J Neuroophthalmol. (2018) 38:514–21. doi: 10.1097/WNO.0000000000000702
4. Solly, EJ, Clough, M, Foletta, P, White, OB, and Fielding, J. The psychiatric symptomology of visual snow syndrome. Front Neurol. (2021) 12:703006. doi: 10.3389/fneur.2021.703006
5. Wong, SH, Pontillo, G, Kanber, B, Prados, F, Wingrove, J, Yiannakas, M, et al. Visual snow syndrome improves with modulation of resting-state functional MRI connectivity after mindfulness-based cognitive therapy: an open-label feasibility study. J Neuroophthalmol. (2024) 44:112–8. doi: 10.1097/WNO.0000000000002013
6. Puledda, F, Ffytche, D, Lythgoe, DJ, O’Daly, O, Schankin, C, Williams, SCR, et al. Insular and occipital changes in visual snow syndrome: a BOLD fMRI and MRS study. Ann Clin Transl Neurol. (2020) 7:296–306. doi: 10.1002/acn3.50986
7. Lauschke, JL, Plant, GT, and Fraser, CL. Visual snow: a thalamocortical dysrhythmia of the visual pathway? J Clin Neurosci. (2016) 28:123–7. doi: 10.1016/j.jocn.2015.12.001
8. Menon, V, and Uddin, LQ. Saliency, switching, attention and control: a network model of insula function. Brain Struct Funct. (2010) 214:655–67. doi: 10.1007/s00429-010-0262-0
9. Halassa, MM, and Sherman, SM. Thalamocortical circuit motifs: a general framework. Neuron. (2019) 103:762–70. doi: 10.1016/j.neuron.2019.06.005
10. Zhou, K, Zhu, L, Hou, G, Chen, X, Chen, B, Yang, C, et al. The contribution of thalamic nuclei in salience processing. Front Behav Neurosci. (2021) 15:634618. doi: 10.3389/fnbeh.2021.634618
11. Furutachi, S, Franklin, AD, Aldea, AM, Mrsic-Flogel, TD, and Hofer, SB. Cooperative thalamocortical circuit mechanism for sensory prediction errors. Nature. (2024) 633:398–406. doi: 10.1038/s41586-024-07851-w
12. Posner, MI, and Petersen, SE. The attention system of the human brain. Annu Rev Neurosci. (1990) 13:25–42.
13. Petersen, SE, and Posner, MI. The attention system of the human brain: 20 years after. Annu Rev Neurosci. (2012) 35:73–89. doi: 10.1146/annurev-neuro-062111-150525
14. Anderson, BA. A value-driven mechanism of attentional selection. J Vis. (2013) 13:7. doi: 10.1167/13.3.7
15. Svensson, S, Golubickis, M, Johnson, S, Falbén, JK, and Macrae, CN. Self-relevance and the activation of attentional networks. Q J Exp Psychol. (2023) 76:1120–30. doi: 10.1177/17470218221112238
16. Fabio, RA, Caprì, T, and Romano, M. From controlled to automatic processes and back again: the role of contextual features. Eur J Psychol. (2019) 15:773–88. doi: 10.5964/ejop.v15i4.1746
17. Paczynski, M, Burton, AM, and Jha, AP. Brief exposure to aversive stimuli impairs visual selective attention. J Cogn Neurosci. (2015) 27:1172–9. doi: 10.1162/jocn_a_00768
18. Ma, N, Dinges, DF, Basner, M, and Rao, H. How acute total sleep loss affects the attending brain: a meta-analysis of neuroimaging studies. Sleep. (2015) 38:233–40. doi: 10.5665/sleep.4404
19. Geng, H, Li, X, Chen, J, Li, X, and Gu, R. Decreased intra- and inter-salience network functional connectivity is related to trait anxiety in adolescents. Front Behav Neurosci. (2015) 9:350. doi: 10.3389/fnbeh.2015.00350
20. Androulakis, XM, Rorden, C, Peterlin, BL, and Krebs, K. Modulation of salience network intranetwork resting state functional connectivity in women with chronic migraine. Cephalalgia. (2017) 38:1731–741. doi: 10.1177/0333102417748570
21. Kim, H, and Anderson, BA. How does the attention system learn from aversive outcomes? Emotion. (2021) 21:898–903. doi: 10.1037/emo0000757
22. Yiend, J. The effects of emotion on attention: a review of attentional processing of emotional information. Cognit Emot. (2010) 24:3–47. doi: 10.1080/02699930903205698
23. Kabat-Zinn, J. Mindfulness-based interventions in context: past, present, and future. Clin Psychol Sci Pract. (2003) 10:144–56. doi: 10.1093/clipsy.bpg016
24. Shapiro, SL, Carlson, LE, Astin, JA, and Freedman, B. Mechanisms of mindfulness. J Clin Psychol. (2006) 62:373–86. doi: 10.1002/jclp.20237
25. Bishop, SR, Lau, M, Shapiro, S, Carlson, L, Anderson, ND, Carmody, J, et al. Mindfulness: a proposed operational definition. Clin Psychol Sci Pract. (2004) 11:230–41. doi: 10.1093/clipsy.bph077
26. Segal, ZV, Williams, M, and Teasdale, J. Mindfulness-based cognitive therapy for depression. Second ed. New York: The Guilford Press (2018).
27. National Institute of Clinical Excellence (NICE) NICE guidelines NG222. Depression in adults: treatment and management NICE (2022). Available at: https://www.nice.org.uk/guidance/ng222
28. McManus, F, Surawy, C, Muse, K, Vazquez-Montes, M, and Williams, JMG. A randomized clinical trial of mindfulness-based cognitive therapy versus unrestricted services for health anxiety (hypochondriasis). J Consult Clin Psychol. (2012) 80:817–28. doi: 10.1037/a0028782
29. Tang, Y-Y, Hölzel, BK, and Posner, MI. The neuroscience of mindfulness meditation. Nat Rev Neurosci. (2015) 16:213–25. doi: 10.1038/nrn3916
30. Farb, NAS, Segal, ZV, and Anderson, AK. Mindfulness meditation training alters cortical representations of interoceptive attention. Soc Cogn Affect Neurosci. (2013) 8:15–26. doi: 10.1093/scan/nss066
31. Teasdale, JD, Moore, RG, Hayhurst, H, Pope, M, Williams, S, and Segal, ZV. Metacognitive awareness and prevention of relapse in depression: empirical evidence. J Consult Clin Psychol. (2002) 70:275–87. doi: 10.1037/0022-006X.70.2.275
32. Bogler, C, Vowinkel, A, Zhutovsky, P, and Haynes, JD. Default network activity is associated with better performance in a vigilance task. Front Hum Neurosci. (2017) 11:623. doi: 10.3389/fnhum.2017.00623
33. Bremer, B, Wu, Q, Mora Álvarez, MG, Hölzel, BK, Wilhelm, M, Hell, E, et al. Mindfulness meditation increases default mode, salience, and central executive network connectivity. Sci Rep. (2022) 12:13219. doi: 10.1038/s41598-022-17325-6
34. Puledda, F, Dipasquale, O, Gooddy, BJM, Karsan, N, Bose, R, Mehta, MA, et al. Abnormal glutamatergic and serotonergic connectivity in visual snow syndrome and migraine with Aura. Ann Neurol. (2023) 94:873–84. doi: 10.1002/ana.26745
35. von Düring, F, Ristow, I, Li, M, Denzel, D, Colic, L, Demenescu, LR, et al. Glutamate in salience network predicts BOLD response in default mode network during salience processing. Front Behav Neurosci. (2019) 13:232. doi: 10.3389/fnbeh.2019.00232
Keywords: visual snow syndrome, mindfulness, attention network, salience network, default mode network, lifestyle intervention, mindfulness-based intervention
Citation: Wong SH and Wingrove J (2025) Mindfulness and MBCT-vision (mindfulness-based cognitive therapy modified for visual symptoms) for visual snow syndrome: a therapeutic perspective. Front. Neurol. 16:1596642. doi: 10.3389/fneur.2025.1596642
Edited by:
Gordon Plant, University College London, United KingdomReviewed by:
Arnold Jonathan Wilkins, University of Essex, United KingdomAxel Petzold, NHS England, United Kingdom
Copyright © 2025 Wong and Wingrove. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sui H. Wong, c3Vpd29uZ0Bkb2N0b3JzLm9yZy51aw==
 Sui H. Wong
Sui H. Wong Janet Wingrove5
Janet Wingrove5