Abstract
Background:
This study investigated the impact of seasons with substantial atmospheric pressure change on the occurrence of migraine using large-scale data from a Japanese health insurance claims database matched with meteorological data.
Methods:
This retrospective cohort study used JMDC Claims Data and national meteorological data from Japan. Patients with a diagnostic record of migraine were included and categorized into eight regional subgroups based on the location of the healthcare facility at which they were initially diagnosed with migraine. The time to migraine occurrence, defined as the duration from the first day of each season to the prescription of triptans, was compared between the seasons with the highest and lowest atmospheric pressure change.
Results:
A total of 26,777 individuals were included in this study. Summer showed the lowest atmospheric pressure change across all eight regions. Conversely, winter showed the highest atmospheric pressure change in seven regions, while autumn showed the highest change in one region. No differences were observed in survival curves between the seasons with the highest and lowest atmospheric pressure change in any region. In Cox regression analysis, hazard ratio for the season with the highest atmospheric pressure change was 0.970 (95% CI: 0.951–0.989) in the minimally adjusted model, which included sex and age. Conversely, the fully adjusted model, which incorporated eight covariates, indicated a hazard ratio of 1.294 (95% CI: 1.007–1.663) for the season with the highest atmospheric pressure change.
Conclusion:
This study, using a large Japanese administrative claims database, did not identify a significant association between seasons with substantial atmospheric pressure change and migraine occurrence. Future research should consider examining more granular residential data, beyond the prefecture level, for a more detailed analysis.
Introduction
Migraine is a common condition in the general population, and leads to a significant burden and reduction in quality of life. The prevalence of migraine in Japan has been reported to range from 3.2 to 8.4% (1–3). Migraine is more prevalent in women (1, 3) and is most common in those aged 30–39 years (1). About 70% of individuals with migraine report significant impairment in daily activities (2), and approximately 20% experienced work absences due to headaches over 3 months (3).
The occurrence of migraine has been reported to be associated with various factors, including weather changes, sleep disturbances, medications, smoking, alcohol, stress, and fatigue (4). Other reported triggers include menstruation, volatile organic compounds, certain foods and beverages, and synthetic alkaloids, making the condition multifactorial (5). Among these, the most frequently reported factors are stress, menstrual cycle changes, weather changes, sleep disturbances, alcohol, and specific foods (6).
Several studies have explored the association between weather change and migraine. However, the findings remain controversial, and no clear consensus has been reached. Weather-related factors reported to be associated with migraine include atmospheric pressure, wind force, temperature fluctuations (7), average wind speed (8), humidity and warm climate conditions (9), weather changes, sunlight, cold wind, temperature increase (10), and photophobia (11). In contrast, another report concluded that the impact of weather factors on migraine and headaches is minimal or doubtful (12), while others have found that low atmospheric pressure is not a contributing factor (13, 14). As a result, there is no recognized consensus among experts, and the evidence is not considered definitive.
Populations living in regions with distinct seasonal variations are ideal for studying the relationship between seasons and migraine. Japan, characterized by pronounced seasonal change, significant temperature fluctuations, and large atmospheric pressure shifts, including typhoon effects, offers an optimal setting for such research. Despite extensive studies on weather and migraines globally, few reports have addressed the impact of weather change on migraine onset in Japan. A study in Japan investigated the relationship between migraine and atmospheric pressure using meteorological data and headache diaries from 28 patients, and the results supported an association between weather change and migraine occurrence (15). However, this study had a small sample size and was conducted in a limited region, and the impact of weather change on migraine in Japan remains unclear. A recent report using a Japanese smartphone application found that low pressure, pressure change, high humidity, and rainfall characteristic of Japan’s climate were associated with increased headache frequency (16). However, that study was limited to six regions and did not use medical record-based outcomes, such as claims data. The population included general headache sufferers, many of whom lacked a definitive diagnosis, rather than exclusively representing patients with migraine.
In this study, we aimed to investigate the impact of seasons with substantial atmospheric pressure change on the occurrence of migraine using large-scale data from a Japanese health insurance claims database matched with meteorological data.
Materials and methods
Study design and data source
This is a retrospective cohort study using JMDC Claims Data, which consists of health insurance claims and medical examination data from all the medical institutions in Japan (17), and national meteorological data collected by the Japan Meteorological Agency. The JMDC data enabled us to monitor all medical treatments received by the patients, even across different facilities, as long as they remained under the same health insurance. All patients in the database were younger than 75 years old and were covered by the insurance. Additionally, the Japan Weather Association offers a service called “HealthWeather®” that provides weather data such as temperature, mean atmospheric pressure, maximum and minimum atmospheric pressure, humidity, wind force, and sunlight duration. This data can be integrated with JMDC data for research.
Data from January 1, 2018, to December 31, 2019, were used. Patients were enrolled based on data from January 1, 2019, to December 31, 2019, with data from 2018 serving as the look-back period to assess eligibility.
Study population
Patients continuously registered in the database during the study period from January 1, 2018, to December 31, 2019, with at least one diagnostic record of migraine (ICD10 code: G43) during the look-back period (January 1, 2018, to December 31, 2018) were included. Exclusion criteria included the following: (1) age under 18 years, (2) prescription records for 120 or more triptan tablets (ATC code: N02CC01, N02CC02, N02CC03, N02CC04, N02CC06) during the look-back period, (3) prescription of 120 or more ergotamine tablets during the look-back period, (4) presence of records for comorbidities associated with secondary headaches (ICD10 code; S00-S19, I60-I69, G90-G99, I11-I15, G24, and T918) during the look-back period, and (5) no prescription of triptan medication during the look-back period. Patients prescribed a total of 120 triptan tablets or more annually were excluded to rule out medication-overuse headaches. According to the Japanese headache management guidelines (18), a medication-overuse headache is defined as an “ergotamine-overuse headache” or “triptan-overuse headache” occurring on 10 or more days per month, corresponding to an annual threshold of 120 tablets.
Patients were then classified into subgroups based on the location of the healthcare facility where they were first diagnosed with migraine, corresponding to the eight regions of Hokkaido, Tohoku, Kanto, Chubu, Kinki, Chugoku, Shikoku, and Kyushu.
Study variables
The year 2019 was divided into four seasons: winter (January–March), spring (April–June), summer (July–September), and autumn (October–December). The first day of each season was defined as the index date, and the observation period for each season extended from the index date to the last day of that season. Individuals were enrolled for each season.
Substantial atmospheric pressure change (exposure) was defined as a day when the difference between the highest and lowest atmospheric pressure in the respective region exceeded 5 hPa. We adopted this criterion based on previous research (15) and after considering several alternative definitions, as detailed in Supplementary Table S3. For each season, the number of days meeting this criterion was calculated, and the seasons with the highest and lowest atmospheric pressure change were identified.
The primary outcome of this study was the occurrence of migraine, as evaluated from the index date to the date of the first record for triptan prescription during each season’s observation period. Since this study included patients continuously registered in the database during the study period, the censor date for each season was defined as the last day of the respective season.
The following patient information was collected as covariates: sex, age, female age group, medications used for acute migraine treatment, medications used for migraine prevention, comorbidities that may trigger or exacerbate migraines, and other comorbidities. Details of the codes for medications and diseases are provided in Supplementary material. The following weather covariates were also collected: mean temperature, mean humidity, mean wind force, and sunlight duration.
Statistical analysis
Descriptive statistics for patient characteristics are presented for each regional subgroup. Means and standard deviations (or medians and interquartile ranges) were used to describe continuous variables, while categorical variables were presented as frequencies and percentages.
For each region, the Kaplan–Meier method was used to estimate and plot the incidence-free proportion of migraine (first triptan prescription within the season), with comparison of the seasons with the highest and lowest atmospheric pressure change.
A marginal-structure Cox model was used to calculate the hazard ratio and 95% confidence intervals for the seasons with the highest atmospheric pressure change compared to the seasons with the lowest atmospheric pressure change, with time to the first triptan prescription within the season as the dependent variable. Lin and Wei’s (19) robust sandwich estimator was applied to the covariance matrix. The following covariates were included in the model: sex, age, female age group medications used for acute migraine treatment, medications used for migraine prevention, concomitant medications, comorbidities that may trigger or exacerbate migraines, and other comorbidities. Due to limited meteorological data in certain regions (data on temperature, humidity, wind speed, and sunlight duration were limited), this analysis was conducted on the entire study population without division into regional subgroups.
All analyses were conducted with SAS statistical software version 9.4 (SAS Institute Inc., Cary, NC, United States).
Results
Patient disposition
Figure 1 shows the flow diagram of the study. Of the 5,634,130 individuals enrolled in the JMDC database during the study period, 81,895 had a diagnosis record of migraine in the look-back period. After excluding patients who met the exclusion criteria, the final study population consisted of 26,777 individuals.
Figure 1

Flow diagram.
Patient characteristics
Table 1 shows the patient characteristics stratified by region. The number of patients in each region was as follows: Hokkaido, 519; Tohoku, 1,495; Kanto, 10,868; Chubu, 7,235; Kinki, 3,312; Chugoku, 1,381; Shikoku, 366; and Kyushu, 1,601. Mean age ranged from 40.2 years (SD 11.5) in Hokkaido to 42.2 years (SD 11.2) in Kanto, with all regions showing a concentration of mean age in the early 40s. The percentage of females ranged from 66.9% in Chubu to 75.7% in Shikoku, with all regions showing a majority of females. The proportion of patients with comorbidities that could trigger migraines ranged from 27.1% in Kinki to 32.2% in Shikoku. Specifically, sleep disorders ranged from 13.1% in Tohoku to 17.4% in Chugoku; mood disorders from 10.2% in Tohoku to 14.4% in Kanto; anxiety disorders from 7.0% in Chubu to 10.8% in Tohoku; and dysmenorrhea from 5.8% in Kyushu to 10.4% in Hokkaido. The proportion of patients using migraine prophylactic medications ranged from 32.5% in Shikoku to 39.5% in Hokkaido. The proportion of patients using NSAIDs ranged from 22.2% in Chugoku to 28.7% in Shikoku.
Table 1
| Region | N = 26,777 | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Hokkaido | Tohoku | Kanto | Chubu | Kinki | Chugoku | Shikoku | Kyushu | |||||||||
| Total | 519 | 1,495 | 10,868 | 7,235 | 3,312 | 1,381 | 366 | 1,601 | ||||||||
| Sex, n (%)* | ||||||||||||||||
| Male | 148 | 28.5 | 452 | 30.2 | 3,273 | 30.1 | 2,398 | 33.1 | 949 | 28.7 | 444 | 32.2 | 89 | 24.3 | 433 | 27.0 |
| Female | 371 | 71.5 | 1,043 | 69.8 | 7,595 | 69.9 | 4,837 | 66.9 | 2,363 | 71.3 | 937 | 67.8 | 277 | 75.7 | 1,168 | 73.0 |
| Age, mean (SD) | 40.2 | 11.5 | 40.4 | 11.4 | 42.2 | 11.2 | 41.6 | 11.2 | 42.0 | 11.4 | 41.7 | 11.3 | 40.7 | 11.3 | 41.4 | 11.0 |
| Female age group, n (%)* | ||||||||||||||||
| Male or under 52 years | 449 | 86.5 | 1,317 | 88.1 | 9,191 | 84.6 | 6,192 | 85.6 | 2,798 | 84.5 | 1,186 | 85.9 | 311 | 85.0 | 1,363 | 85.1 |
| Female and equal or over 52 years | 70 | 13.5 | 178 | 11.9 | 1,677 | 15.4 | 1,043 | 14.4 | 514 | 15.5 | 195 | 14.1 | 55 | 15.0 | 238 | 14.9 |
| Comorbidities that may trigger or exacerbate migraines, n (%)* | 153 | 29.5 | 409 | 27.4 | 3,331 | 30.6 | 1,970 | 27.2 | 899 | 27.1 | 429 | 31.1 | 118 | 32.2 | 451 | 28.2 |
| Sleep disorder | 74 | 14.3 | 196 | 13.1 | 1,741 | 16.0 | 989 | 13.7 | 458 | 13.8 | 240 | 17.4 | 57 | 15.6 | 221 | 13.8 |
| Mood disorder | 60 | 11.6 | 152 | 10.2 | 1,565 | 14.4 | 945 | 13.1 | 374 | 11.3 | 191 | 13.8 | 52 | 14.2 | 187 | 11.7 |
| Anxiety disorder | 49 | 9.4 | 161 | 10.8 | 1,074 | 9.9 | 508 | 7.0 | 252 | 7.6 | 111 | 8.0 | 39 | 10.7 | 148 | 9.2 |
| Dysmenorrhea | 54 | 10.4 | 113 | 7.6 | 707 | 6.5 | 436 | 6.0 | 217 | 6.6 | 91 | 6.6 | 24 | 6.6 | 93 | 5.8 |
| Hypothyroidism | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Photosensitivity | 0 | 0.0 | 0 | 0.0 | 2 | 0.0 | 2 | 0.0 | 1 | 0.0 | 0 | 0.0 | 0 | 0.0 | 2 | 0.1 |
| Other comorbidities, n (%)* | 77 | 14.8 | 193 | 12.9 | 1,624 | 14.9 | 902 | 12.5 | 462 | 13.9 | 171 | 12.4 | 58 | 15.8 | 206 | 12.9 |
| Primary Hypertension | 56 | 10.8 | 132 | 8.8 | 1,090 | 10.0 | 688 | 9.5 | 328 | 9.9 | 123 | 8.9 | 45 | 12.3 | 165 | 10.3 |
| Restless Legs Syndrome | 3 | 0.6 | 1 | 0.1 | 43 | 0.4 | 43 | 0.6 | 17 | 0.5 | 9 | 0.7 | 1 | 0.3 | 6 | 0.4 |
| Asthma | 1 | 0.2 | 29 | 1.9 | 17 | 0.2 | 19 | 0.3 | 15 | 0.5 | 8 | 0.6 | 0 | 0.0 | 2 | 0.1 |
| Epilepsy | 26 | 5.0 | 40 | 2.7 | 614 | 5.6 | 193 | 2.7 | 131 | 4.0 | 40 | 2.9 | 14 | 3.8 | 45 | 2.8 |
| Medication used for acute treatment of migraine, n (%)* | 519 | 100.0 | 1,495 | 100.0 | 10,868 | 100.0 | 7,235 | 100.0 | 3,312 | 100.0 | 1,381 | 100.0 | 366 | 100.0 | 1,601 | 100.0 |
| Triptan | 519 | 100.0 | 1,495 | 100.0 | 10,868 | 100.0 | 7,235 | 100.0 | 3,312 | 100.0 | 1,381 | 100.0 | 366 | 100.0 | 1,601 | 100.0 |
| Anxiolytics, Antipsychotics, Anesthetics, Antiemetics | 181 | 34.9 | 486 | 32.5 | 3,401 | 31.3 | 2,223 | 30.7 | 1,115 | 33.7 | 540 | 39.1 | 124 | 33.9 | 544 | 34.0 |
| Acetaminophen, NSAIDs | 418 | 80.5 | 1,124 | 75.2 | 8,364 | 77.0 | 5,534 | 76.5 | 2,542 | 76.8 | 1,098 | 79.5 | 291 | 79.5 | 1,286 | 80.3 |
| Ergotamine | 4 | 0.8 | 16 | 1.1 | 112 | 1.0 | 73 | 1.0 | 28 | 0.8 | 10 | 0.7 | 2 | 0.5 | 11 | 0.7 |
| Steroids | 42 | 8.1 | 127 | 8.5 | 968 | 8.9 | 830 | 11.5 | 223 | 6.7 | 118 | 8.5 | 45 | 12.3 | 91 | 5.7 |
| Others | 59 | 11.4 | 101 | 6.8 | 919 | 8.5 | 551 | 7.6 | 278 | 8.4 | 119 | 8.6 | 21 | 5.7 | 138 | 8.6 |
| Medication used for migraine prevention, n (%)* | 205 | 39.5 | 574 | 38.4 | 4,181 | 38.5 | 2,523 | 34.9 | 1,203 | 36.3 | 538 | 39.0 | 119 | 32.5 | 582 | 36.4 |
| Anti-CGRP Antibodies | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Anti-CGRP Receptor Antibodies | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 | 0 | 0.0 |
| Antiepileptic Drugs | 26 | 5.0 | 123 | 8.2 | 1,239 | 11.4 | 564 | 7.8 | 259 | 7.8 | 137 | 9.9 | 30 | 8.2 | 204 | 12.7 |
| Antidepressants | 57 | 11.0 | 134 | 9.0 | 1,147 | 10.6 | 693 | 9.6 | 301 | 9.1 | 135 | 9.8 | 36 | 9.8 | 138 | 8.6 |
| β Blockers | 9 | 1.7 | 16 | 1.1 | 236 | 2.2 | 135 | 1.9 | 72 | 2.2 | 31 | 2.2 | 16 | 4.4 | 39 | 2.4 |
| Calcium Channel Blockers | 79 | 15.2 | 284 | 19.0 | 1,379 | 12.7 | 928 | 12.8 | 483 | 14.6 | 204 | 14.8 | 30 | 8.2 | 188 | 11.7 |
| ARB/ACE Inhibitors | 17 | 3.3 | 21 | 1.4 | 214 | 2.0 | 117 | 1.6 | 62 | 1.9 | 24 | 1.7 | 5 | 1.4 | 26 | 1.6 |
| Other Concomitant Medications | 88 | 17.0 | 154 | 10.3 | 1,551 | 14.3 | 945 | 13.1 | 422 | 12.7 | 205 | 14.8 | 36 | 9.8 | 233 | 14.6 |
| NSAID | 121 | 23.3 | 382 | 25.6 | 2,745 | 25.3 | 1,810 | 25.0 | 826 | 24.9 | 306 | 22.2 | 105 | 28.7 | 376 | 23.5 |
Patient characteristics of the study population.
*Percentages were calculated using the total number of patients in each group as the denominator.
Seasons with substantial atmospheric pressure change and migraine occurrence
Figure 2 shows Kaplan–Meier curves for the time from the index date to migraine onset (first triptan prescription within the season), stratified by the season of highest and lowest exposure in each region. In all eight regions, summer was the season with the lowest atmospheric pressure change. In Hokkaido, autumn was the season with the highest atmospheric pressure change, whereas in the other seven regions, winter showed the highest atmospheric pressure change. There were no differences in survival curves between exposure groups in any region. At 90 days, the incidence-free proportion of migraine in Hokkaido was 72.3% for the season with the lowest atmospheric pressure change and 69.4% for the season with the highest atmospheric pressure change. Similarly, the proportions were 69.8 and 70.8% in Tohoku; 65.1 and 65.5% in Kanto; 68.5 and 68.3% in Chubu; 67.6 and 68.1% in Kinki; 67.7 and 68.1% in Chugoku; 71.0 and 68.9% in Shikoku; and 68.6 and 67.7% in Kyushu.
Figure 2
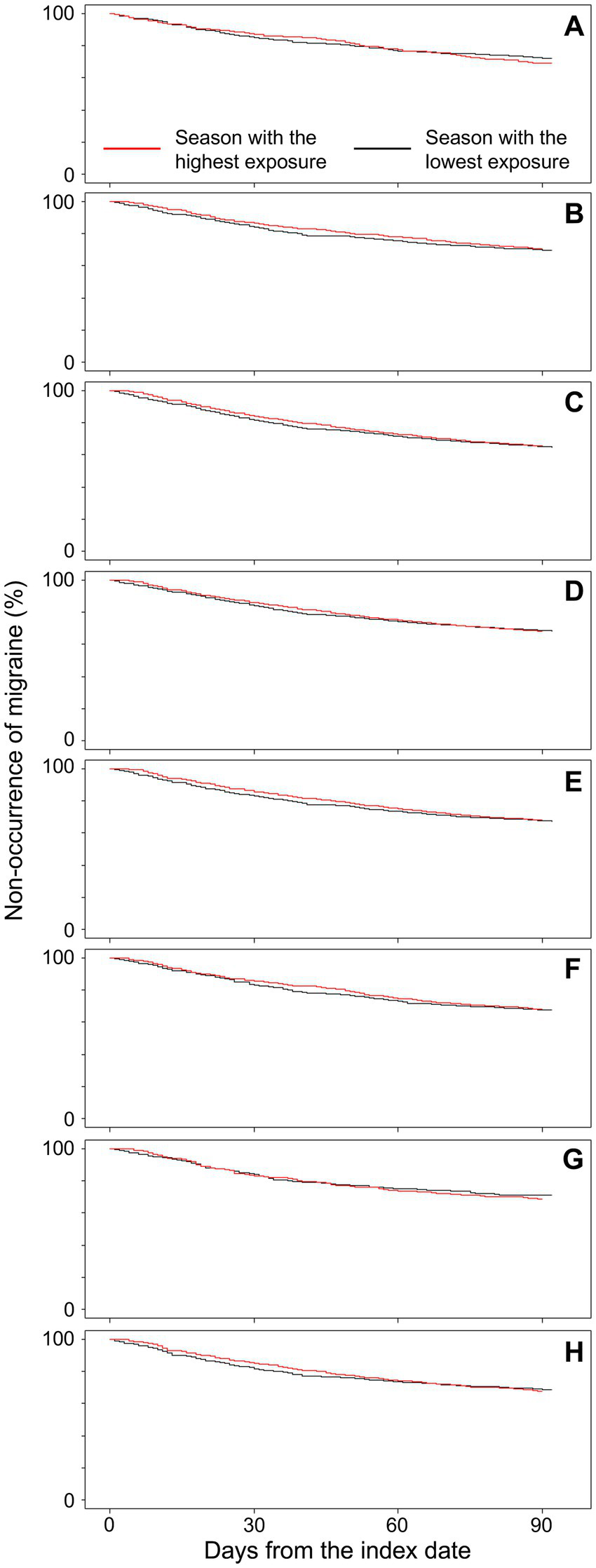
Kaplan Meier plots for the time from the index date to migraine onset (first triptan prescription within the season). (A) Hokkaido (n = 519), (B) Tohoku (n = 1,495), (C) Kanto (n = 10,868), (D) Chubu (n = 7,235), (E) Kinki (n = 3,312), (F) Chugoku (n = 1,381), (G) Shikoku (n = 366), and (H) Kyushu (n = 1,601).
Table 2 shows the results of Cox regression analysis for the entire study population. In the minimally adjusted model (model 1), which included sex and age as covariates, the hazard ratio for the season (exposure variable) was 0.970 (95% CI: 0.951–0.989), and no association was observed between the season and outcome (time to triptan prescription) in models that did not include adjustment for other weather-related variables. In contrast, in model 8, which included sex, age, medication used for migraine prevention, comorbidities that may trigger or exacerbate migraines, other comorbidities, and female’s age group, temperature, humidity, wind force, and sunlight hours as covariates, the hazard ratio for the highest exposure season compared to the lowest exposure season was 1.294 (95% CI: 1.007–1.663). Female sex, use of migraine prophylactic medications, and the presence of comorbidities that could trigger migraines consistently showed higher hazard ratios across all models. In model 8 (the fully adjusted model), the hazard ratios were 1.469 (95% CI: 1.402–1.538), 1.353 (95% CI: 1.300–1.407), and 1.208 (95% CI: 1.159–1.258), respectively.
Table 2
| Variable | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | Model 6 | Model 7 | Model 8 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | HR | 95%CI | |
| Season (ref: season with the lowest atmospheric pressure changes) | 0.970 | 0.951–0.989 | 0.971 | 0.952–0.990 | 0.971 | 0.952–0.990 | 0.971 | 0.952–0.990 | 1.104 | 0.903–1.351 | 1.231 | 0.977–1.551 | 1.230 | 0.975–1.551 | 1.294 | 1.007–1.663 |
| Sex (ref: male) | 1.405 | 1.345–1.467 | 1.402 | 1.343–1.464 | 1.392 | 1.332–1.454 | 1.469 | 1.403–1.539 | 1.470 | 1.403–1.539 | 1.468 | 1.402–1.538 | 1.468 | 1.402–1.538 | 1.469 | 1.402–1.538 |
| Age | 1.031 | 1.029–1.033 | 1.031 | 1.029–1.033 | 1.030 | 1.028–1.032 | 1.035 | 1.033–1.037 | 1.035 | 1.032–1.037 | 1.035 | 1.033–1.037 | 1.035 | 1.033–1.037 | 1.035 | 1.032–1.037 |
| Medication used for migraine prevention (ref: None) | 1.433 | 1.380–1.487 | 1.355 | 1.302–1.409 | 1.352 | 1.300–1.407 | 1.353 | 1.300–1.408 | 1.353 | 1.300–1.407 | 1.353 | 1.300–1.407 | 1.353 | 1.300–1.407 | ||
| Comorbidities that may trigger or exacerbate migraines (ref: None) | 1.210 | 1.162–1.261 | 1.208 | 1.159–1.258 | 1.208 | 1.159–1.258 | 1.208 | 1.159–1.258 | 1.208 | 1.159–1.258 | 1.208 | 1.159–1.258 | ||||
| Other comorbidities (ref: None) | 1.050 | 0.996–1.107 | 1.053 | 0.999–1.110 | 1.053 | 0.999–1.110 | 1.052 | 0.999–1.109 | 1.052 | 0.999–1.109 | 1.052 | 0.999–1.109 | ||||
| Female’s age group (ref: male or under 52 years) | 0.812 | 0.765–0.863 | 0.812 | 0.765–0.863 | 0.813 | 0.765–0.863 | 0.813 | 0.765–0.863 | 0.813 | 0.765–0.863 | ||||||
| Mean temperature | 1.007 | 0.996–1.018 | 1.010 | 0.999–1.021 | 1.010 | 0.999–1.021 | 1.011 | 1.000–1.023 | ||||||||
| Mean humidity | 1.003 | 1.000–1.006 | 1.003 | 1.000–1.006 | 1.005 | 1.000–1.010 | ||||||||||
| Mean wind force | 0.998 | 0.966–1.032 | 1.000 | 0.968–1.034 | ||||||||||||
| Mean sunshine duration | 1.021 | 0.994–1.050 | ||||||||||||||
Adjusted hazard ratios for first triptan prescription within the season: marginal-structure Cox regression analysis.
HR, hazard ratio; CI, confidence interval.
Discussion
This study investigated the association between seasons with substantial atmospheric pressure change and migraine occurrence using a large Japanese administrative claims database and national meteorological data. The results showed no association between seasons with substantial atmospheric pressure change and migraine onset (prescription of triptan) in any of the eight regions of Japan.
One possible explanation for the results of this study was the inability to account for localized meteorological variations at a more granular residential level. Japan’s geography, characterized by its coastal location and mountainous terrain, leads to substantial weather variation even within the same prefecture. Although this study analyzed data at the prefectural level, it lacked more granular information on local weather conditions. This limitation may have contributed to the absence of an association between seasonal change and migraine occurrence. In Cox regression analysis, no association between outcome and exposure was observed in models adjusted for some covariates. In contrast, when weather conditions were included in the fully adjusted model (model 8), the season with the highest atmospheric pressure change showed a statistically significant, although modest, higher hazard for migraine occurrence compared to the season with the lowest atmospheric pressure change. This suggests that within regions with similar weather conditions, the season may be associated with migraine occurrence.
The results of this study may also be partially explained by the influence of other confounding factors. Previous studies have indicated that healthcare-seeking behavior for migraines in Japan is relatively low (1, 2), and triptan prescriptions are typically reserved for more severe migraines (20). Consequently, migraine cases defined using claims data in this study may not have captured mild migraines. Furthermore, the regional disparity in the distribution of specialists in Japan may have influenced the findings of this study by contributing to differences in treatment practices across areas. A previous study in Japan which evaluated migraines using headache diaries supported the association between atmospheric pressure and migraine, presenting findings inconsistent with the current study (15). This also suggests that differences in migraine measurement may have resulted in the current study’s inability to capture patients with milder symptoms. Furthermore, various risk factors associated with migraine have been reported, such as stress, fatigue, menstrual cycle changes, various foods, alcohol, smoking, fasting, premenstrual periods in women, or “letdown” after stress (4, 6). More recently, atopic, psychiatric, sleep, and cardiovascular conditions have also been reported as risk factors (21), as well as hormonal imbalances, genetic and epigenetic influences (22). The current study did not fully account for these factors, which indicates that residual confounding is likely present.
This study builds on previous findings regarding the association between weather conditions and migraine. In geographic regions with marked seasonal variation, such as Japan, recognizing weather change and taking preventive actions to mitigate migraine onset is essential. However, in Japan, this association has only been reported in studies with small sample sizes. This study provides additional information by investigating the association between seasons with substantial atmospheric pressure change and migraine using a large sample size database from Japan. Consistent with previous research, factors such as female sex, the use of migraine prophylactic medications, and the presence of comorbidities that may trigger migraines were also found to be associated with increased migraine risk. However, to clarify the association, further detailed study is considered necessary.
This study has several limitations. First, data on several variables associated with migraine were not available, which suggests the potential for unmeasured confounding. Furthermore, although this study was evaluated over a single year given Japan’s distinct seasonal changes, it could not account for interannual fluctuations of pressure systems, long-term trends in extreme weather events, or delayed biological effects. Second, there is a possibility of outcome misclassification regarding migraine occurrence if triptans were prescribed as preventive medication. However, before the introduction of anti-CGRP antibodies in 2021, there were no well-established preventive treatments for migraines. Therefore, during the study period in 2019, it is likely that the majority of patients were primarily receiving acute-phase treatments. While defining outcomes by triptan prescriptions helps specifically identify migraines (23), this approach limits the sensitivity by not identifying migraine patients who use other treatments. Moreover, the high reliance on over-the-counter (OTC) medications in Japan, as highlighted in previous research (1), further reduced the sensitivity of our data. Third, it is possible that the weather of some patients’ residential areas was misclassified. In this study, regions were categorized based on the location of the medical facility where the patient was treated, which means that if a patient sought care across a prefectural or regional boundary, they might have been classified into a region different from their actual residence. However, since the number of patients who seek care across regions is likely limited, any impact on the results is expected to be minimal. Furthermore, the ecological nature of the prefectural-level meteorological data inherently has a risk of misclassification. Fourth, this study utilized a database based on corporate health insurance, which excludes the elderly and individuals enrolled in the National Health Insurance system, such as the self-employed. Therefore, there are limitations in generalizing the results to the entire population of Japan.
This study, using a large Japanese administrative claims database, did not observe an association between seasons with substantial atmospheric pressure change and migraine occurrence. Although significant results were found in multivariate analyses using national-level average meteorological data, the effect was modest, and region-level examination is considered to be necessary to assess clinical relevance. Future research should consider examining more granular residential data, beyond the prefecture level, for a more detailed analysis, and employing more advanced methodologies.
Statements
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: the data utilized in this study were provided by JMDC Inc. under a licensing agreement. Due to these restrictions, the data are not publicly accessible. For further information regarding access to the dataset, please contact JMDC. Requests to access these datasets should be directed to JMDC Inc., https://www.jmdc.co.jp/inquiry/.
Ethics statement
The studies involving humans were approved by the Ethics Review Committee of the Research Division at Otsuka Pharmaceuticals Co., Ltd. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because informed consent was not required for this study, as the datasets utilized were anonymized.
Author contributions
MT: Writing – review & editing. KH: Writing – review & editing. TN: Writing – review & editing. KY: Writing – review & editing. NN: Writing – original draft, Writing – review & editing. LI: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by Otsuka Pharmaceuticals Co., Ltd., Tokyo, Japan.
Acknowledgments
The authors are grateful to Mr. Tajima from JMDC Inc. for his contribution to the data analysis and to Mr. Terashima from JMDC Inc. for advice on the study design. The authors also thank Ryozo Wakabayashi from Datack Inc. for medical writing support.
Conflict of interest
TN reports grants or contracts: I&H Co., Ltd.; Cocokarafine Group Co., Ltd.; Konica Minolta, Inc.; NTT DATA; consulting fees: Otsuka Pharmaceutical Co.; Takeda Pharmaceutical Co.; Johnson & Johnson K.K.; AstraZeneca plc; payment or honoraria for lectures, presentations, speakers bureaus, manuscript writing or educational events: Pfizer Japan Inc.; MSD K.K.; Chugai Pharmaceutical Co.; Takeda Pharmaceutical Co.; Janssen Pharmaceutical K.K.; Boehringer Ingelheim International GmbH.; Eli Lilly Japan K.K.; Maruho Co., Ltd.; Mitsubishi Tanabe Pharma Co.; Novartis Pharma K.K.; Allergan Japan K.K.; Novo Nordisk Pharma Ltd.; TOA EIYO Ltd.; AbbVie Inc.; ONO PHARMACEUTICAL CO., LTD.; GSK plc; Alexion Pharmaceuticals, Inc.; Kowa Company; Merck Co.; Amicus Therapeutics, Inc.; Merck Co.; Amgen Inc. KY, NN, and LI are Otsuka Pharmaceutical Co., Ltd. (Japan) employees. KH and MT received consulting fees from Otsuka Pharmaceutical Co., Ltd. during the conduct of the study. MT was employed by Canon Marketing Japan Inc.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1600822/full#supplementary-material
References
1.
Sakai F Hirata K Igarashi H Takeshima T Nakayama T Sano H et al . A study to investigate the prevalence of headache disorders and migraine among people registered in a health insurance association in Japan. J Headache Pain. (2022) 23:70. doi: 10.1186/s10194-022-01439-3
2.
Sakai F Igarashi H . Prevalence of migraine in Japan: a Nationwide survey. Cephalalgia. (1997) 17:15–22. doi: 10.1046/j.1468-2982.1997.1701015.x
3.
Takeshima T Ishizaki K Fukuhara Y Ijiri T Kusumi M Wakutani Y et al . Population-based door-to-door survey of migraine in Japan: the Daisen study. Headache. (2004) 44:8–19. doi: 10.1111/j.1526-4610.2004.04004.x
4.
Mayans L . Headache: migraine. FP Essent. (2018) 473:11–6.
5.
Kesserwani H . Migraine triggers: an overview of the pharmacology, biochemistry, atmospherics, and their effects on neural networks. Cureus. (2021) 13:e14243. doi: 10.7759/cureus.14243
6.
Marmura MJ . Triggers, protectors, and predictors in episodic migraine. Curr Pain Headache Rep. (2018) 22:81. doi: 10.1007/s11916-018-0734-0
7.
Scheidt J Koppe C Rill S Reinel D Wogenstein F Drescher J . Influence of temperature changes on migraine occurrence in Germany. Int J Biometeorol. (2013) 57:649–54. doi: 10.1007/s00484-012-0582-2
8.
Akgun N Aciman Demirel E Acikgoz M Celebi U Kokturk F Atasoy HT . The effect of weather variables on the severity, duration, and frequency of headache attacks in the cases of episodic migraine and episodic tension-type headache. Turk J Med Sci. (2021) 51:1406–12. doi: 10.3906/sag-2004-66
9.
Li W Bertisch SM Mostofsky E Buettner C Mittleman MA . Weather, ambient air pollution, and risk of migraine headache onset among patients with migraine. Environ Int. (2019) 132:105100. doi: 10.1016/j.envint.2019.105100
10.
Ying G Fan W Li N Wang J Li W Tan G et al . Clinical characteristics of basilar-type migraine in the neurological Clinic of a University Hospital. Pain Med. (2014) 15:1230–5. doi: 10.1111/pme.12402
11.
Bekkelund SI Muller KI Wilhelmsen A Alstadhaug KB . Photophobia and seasonal variation of migraine in a subarctic population. Headache. (2017) 57:1206–16. doi: 10.1111/head.13131
12.
Zebenholzer K Rudel E Frantal S Brannath W Schmidt K Wober-Bingol C et al . Migraine and weather: a prospective diary-based analysis. Cephalalgia. (2011) 31:391–400. doi: 10.1177/0333102410385580
13.
Bolay H Rapoport A . Does low atmospheric pressure independently trigger migraine?Headache. (2011) 51:1426–30. doi: 10.1111/j.1526-4610.2011.01996.x
14.
Tanik N Sacmaci H Akturk T . The relationship between exposure to hot/cold weather and the clinical features of headaches in patients with migraine and tension-type headaches. Neurol Res. (2020) 42:239–43. doi: 10.1080/01616412.2020.1723300
15.
Kimoto K Aiba S Takashima R Suzuki K Takekawa H Watanabe Y et al . Influence of barometric pressure in patients with migraine headache. Intern Med. (2011) 50:1923–8. doi: 10.2169/internalmedicine.50.5640
16.
Katsuki M Tatsumoto M Kimoto K Iiyama T Tajima M Munakata T et al . Investigating the effects of weather on headache occurrence using a smartphone application and artificial intelligence: a retrospective observational cross-sectional study. Headache. (2023) 63:585–600. doi: 10.1111/head.14482
17.
Nagai K Tanaka T Kodaira N Kimura S Takahashi Y Nakayama T . Data resource profile: Jmdc claims databases sourced from medical institutions. J Gen Fam Med. (2020) 21:211–8. doi: 10.1002/jgf2.367
18.
Headache Clinical Practice Guideline Development Committee . Clinical practice guideline for headache disorders 2021. Japanese Society of Neurology, Japanese Headache Society, Japanese Society of Neurological Therapeutics. Tokyo: Igaku-Shoin (2021).
19.
Lin DY Wei LJ . The robust inference for the cox proportional hazards model. J Am Stat Assoc. (1989) 84:1074–8. doi: 10.2307/2290085
20.
Hirata K Komori M Ueda K Zagar AJ Kim Y Jaffe DH et al . Outcomes and factors associated with insufficient effectiveness of acute treatments of migraine in Japan: results of the observational survey of the epidemiology, treatment, and Care of Migraine (overcome [Japan]) study. Drugs Real World Outcomes. (2023) 10:415–28. doi: 10.1007/s40801-023-00368-0
21.
Terhart M Overeem LH Hong JB Reuter U Raffaelli B . Comorbidities as risk factors for migraine onset: a systematic review and three-level meta-analysis. Eur J Neurol. (2025) 32:e16590. doi: 10.1111/ene.16590
22.
Amiri P Kazeminasab S Nejadghaderi SA Mohammadinasab R Pourfathi H Araj-Khodaei M et al . Migraine: a review on its history, global epidemiology, risk factors, and comorbidities. Front Neurol. (2022) 12:800605. doi: 10.3389/fneur.2021.800605
23.
Yamato K Sano H Hirata K Nakayama T . Validation and comparison of the coding algorithms to identify people with migraine using Japanese claims data. Front Neurol. (2023) 14:1231351. doi: 10.3389/fneur.2023.1231351
Summary
Keywords
migraine, atmospheric pressure change, season, weather, claims database
Citation
Tatsumoto M, Hirata K, Nakayama T, Yamato K, Nakamichi N and Inuyama L (2025) Association between seasons with substantial atmospheric pressure change and migraine occurrence: a retrospective cohort study using Japanese claims data and meteorological data. Front. Neurol. 16:1600822. doi: 10.3389/fneur.2025.1600822
Received
27 March 2025
Accepted
21 July 2025
Published
10 September 2025
Volume
16 - 2025
Edited by
Tim P. Jürgens, University Hospital Rostock, Germany
Reviewed by
Andreia Costa, Centro Hospitalar Universitário de São João (CHUSJ), Portugal
Xin Xiong, Sichuan University, China
Updates
Copyright
© 2025 Tatsumoto, Hirata, Nakayama, Yamato, Nakamichi and Inuyama.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Norihiro Nakamichi, nakamichi.Norihiro@otsuka.jp
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.