Abstract
Backgrounds:
In clinical practice, many patients cannot undergo inpatient rehabilitation in hospitals for extended periods due to personal financial constraints, as well as China’s health insurance policy. They are often forced to terminate their rehabilitation training during the prime recovery phase. This makes tele-rehabilitation-based, home-based rehabilitation particularly important.
Purpose:
This retrospective cohort study aimed to compare the efficacy of tele-rehabilitation-based task-oriented training (TOT) versus face-to-face task-oriented training and conventional tele-neurofacilitation techniques.
Methods:
Patients who met the criteria were assigned to either the telerehabilitation group, the FTF group, or the Tele-Control group while receiving standardized rehabilitation treatment and education. Moreover, the Tele-Rehab group underwent tele-rehabilitation-based task-oriented training, the FTF group underwent face-to-face task-oriented training, and the Tele-Control Group underwent tele-rehabilitation-based conventional neurofacilitation techniques. The main evaluation indices were the Fugl-Meyer Assessment Upper Extremity Scale (FMA-UE), Wolf Motor Function Test (WMFT), and Action Research Arm Test (ARAT). Secondary outcome indicators were Instrumental Activities of Daily Living (IADL). All patients underwent 3 weeks of treatment.
Results:
In total, 79 participants completed the trial: Tele-rehab group (n = 23), FTF group (n = 28), and Tele-Control group (n = 28). Improvements in FMA-UE, WMFT, ARAT, and IADL were found in all three groups (p<0.05). The mean change in FMA-UE was 9.4 in the Tele-rehab group, 6.4 in the FTF group, and 6.7 in the Tele-control group. The mean difference between the Tele-Rehab and FTF groups was 3.0, and the mean difference between the Tele-Rehab and Tele-Control groups was 2.7, with the upper limit of the 95% confidence interval not exceeding the margin of non-inferiority. Non-inferiority was demonstrated, as the 95% CI did not cross the margin in FMA-UE difference scores before and after the intervention in the Tele-rehab group compared with the FTF group (p > 0.05), nor in the FTF group compared with the Tele-Control group before and after the intervention (p > 0.05). The 95% CI for FMA-UE improvement between Tele-rehab TOT and face-to-face TOT was [−0.81, 7.39], not exceeding the non-inferiority margin of 12.4.
Conclusion:
Task-oriented training and remote traditional neurofacilitation techniques for tele-rehabilitation of stroke patients can enhance upper limb motor function and improve quality of daily life with comparable efficacy to face-to-face task-oriented training. Therefore, telerehabilitation is a method that is not inferior to conventional rehabilitation and deserves to be used and promoted in homebound patients.
1 Introduction
Stroke is a common cerebrovascular disease, comprising ischemic stroke (80%) and hemorrhagic stroke (20%) (1). Approximately 60–80% of stroke survivors experience motor dysfunction (2, 3), with upper limb impairment being particularly prevalent (4). This impairment not only hinders daily activities and reduces quality of life (5–7) but also imposes significant economic burdens on families and society (8). Stroke patients in the early stage of stroke are usually in the hospital under the guidance of a rehabilitation therapist, and since most stroke patients still have functional impairment after discharge from the hospital (9), they need to undergo continuous rehabilitation training. However, routine rehabilitation training in hospitals is difficult for some patients, which is often related to treatment resources (transport, professionals (10), funding sources), etc., which will also affect subsequent recovery. Therefore, exploring rational training methods and effective training modalities is necessary (11, 12).
Tele-rehabilitation (TR) refers to the provision of rehabilitation services through the use of telecommunication devices such as mobile phones, computers, and tablets in combination with information and modern communication technologies (13). TR is a promising model that features remotely managed treatment, effectively expanding service accessibility and treatment modalities, which compensates for the lack of rehabilitation treatments received by the patient due to the high cost, the scarcity of professional treatment staff, and the lack of transport (14). In addition, there have been several studies pointing out the good efficacy of, such as in 2018, Huidi Tchero et al. showed that TR is comparable to conventional care in terms of improving patients’ quality of life and other aspects, as well as lower costs (15). However, there are some limitations due to the lack of close guidance from professionals, such as a recent Meta-analysis indicated that the efficacy of TR was comparable to that of conventional rehabilitation, but patients undergoing TR tended to have poorer adherence due to differences in training schedules and conditions, etc. (13). Meanwhile, another meta-analysis showed low evidence that remote self-rehabilitation efficacy is comparable to face-to-face conventional efficacy (16).
Task-oriented training (TOT) is a neuroscience-based intervention (17) that has been used in the rehabilitation of stroke patients (18), which focuses on the repetition of multiple explicit active training sessions (19). Relevant literature suggests that TOT is effective in improving motor and functional recovery by incorporating principles of neuroplasticity (20, 21). Similarly, Annick et al. stated in a systematic evaluation that task-oriented training consists of 15 components, some of which improve patients’ ability to remember learned motor performance (22). However, most TOT is currently performed by professionals in a defined clinic or research setting (23), which limits its applicability to some extent. Neurofacilitation techniques are commonly used for CNS injuries, including the Bobath technique, the Brunnstrom technique, and the PNF technique. Neurofacilitation techniques emphasize the stimulation and modulation of neurons in the motor pathway through different methods, which have a wide range of clinical applicability and a high degree of patient cooperation.
Current applications of TR in stroke rehabilitation remain debated. While studies confirm its non-inferiority to conventional care (15), recent systematic reviews note significant adherence and technical standardization challenges (13). In rural China, <30% of patients access TR due to uneven healthcare resources and digital disparities (24), underscoring the need for context-specific protocol optimization. Crucially, no studies have compared TR-delivered task-oriented training (TOT) against neurofacilitation techniques using non-inferiority designs—a gap this study addresses.
To further compare the efficacy of TR combined with task-oriented training and Neurofacilitation techniques, this study, therefore, used a non-inferiority design to compare the effects of task-oriented training with TR, face-to-face task-oriented training, and conventional neurofacilitation techniques treatments on upper limb dysfunction after stroke.
2 Methods
2.1 Study design
This non-inferiority trial utilized a retrospective cohort design based on historical data from patients who received different interventions. Eighty-nine stroke patients with upper limb motor dysfunction who attended the Department of Rehabilitation Medicine of Yuebei People’s Hospital from January 2021 to June 2024 were selected. Depending on the type of intervention, the researchers assigned patients to 3 groups (Grouping based on historical data). Each patient had to receive standardized rehabilitation treatment and education simultaneously. The Ethics Committee of Yuebei People’s Hospital approved the study under No. KY-2022-101. Considering the type of retrospective study, the right to exemption from informed consent was obtained after ethics committee approval. The ethics committee granted a waiver of informed consent under the condition that all data were anonymized and retrospectively analyzed without compromising patient privacy (e.g., deletion of name, medical record number, etc). Assignments between groups are grouped according to the historical events that have been accomplished.
2.2 Eligible criteria
Inclusion criteria were: (1) first onset; (2) all patients with ischaemic or hemorrhagic stroke meeting the diagnostic criteria established by the Fourth National Academic Conference on Cerebrovascular Disease and confirmed by MRI or CT; (3) functional motor disorders of the upper limb and hand on the hemiplegic side; (4) stable vital signs, and duration of the disease between 3 and 24 months; (5) age between 18 and 75 years old; (6) upper limb Functional Brunnstorm stage 1 to 4; (7) clear consciousness, no serious cognitive impairment, no auditory or visual impairment; (8) Walking ability: Functional Ambulation Category≥3. (9) Ashworth spasticity scores: I+- II (1.5–2).
Exclusion criteria were: (1) aphasia, apraxia, lateral neglect; (2) cognitive dysfunction: mini-mental state examination (MMSE) score <24 points (secondary school level or above), illiteracy <17 points; (3) severe spasticity of the upper limbs, Ashworth > 3; (4) previous other brain diseases or history of brain surgery; (5) other causes of severe spasticity of the upper limbs or upper limb dysfunction; (6) unstable condition or vital organ failure, malignant tumor; (7) inability to cooperate with the completion of the MRI examination, etc.; (8) women during pregnancy.
2.3 Interventions
The Tele-Rehab group underwent task-oriented training guidance as the treatment method of TR therapy, the FTF group receives face-to-face task-oriented training and rehabilitation therapy, and the Tele-Control group receives standardized self-guided neurofacilitation exercises via a pre-recorded video platform, with weekly check-ins to ensure protocol adherence (see Table 1). The duration of each treatment in each group was 1 h per day, 6 days per week for 3 weeks. Total dose: 1 h/day, 6 days/week × 3 weeks (18 h total).
Table 1
| Group | Content | Delivery mode | Intensity/Parameters | Progression |
|---|---|---|---|---|
| Tele-Rehab | Task-oriented training (e.g., cup grasping, drawer pushing, turning keys) | Synchronous video (WeChat); real-time correction; household items used | 60 min/session; 6 sessions/week; 3 weeks | Task complexity ↑ weekly based on performance |
| FTF | Identical TOT tasks with standardized equipment (pegboards, weight disks) | In-clinic 1:1 sessions; standardized equipment | Identical to Tele-Rehab | Identical progression |
| Tele-Control | Neurofacilitation (Brunnstrom staging: passive ROM → active-assisted exercises) | Asynchronous videos; weekly check-ins; caregiver supervision | 60 min/session; 6 sessions/week | Resistance ↑ weekly based on performance |
Intervention protocols.
2.4 Study procedures
The Tele-Rehab group requires the patients to carry out targeted, targeted, and systematic upper limb task-oriented training at home under the remote guidance of the therapist. The FTF group was treated by a therapist in an occupational therapist for face-to-face, task-oriented training. In the Tele-Control group, patients were asked to carry out upper limb rehabilitation therapy at home on their own. Quality control: Dual camera angles (wide + close-up), therapist error screening every 15 min, daily video logs, therapist video audits (exercises with >30% deviation triggered in-person reassessment).
2.5 Outcome measures
After randomized grouping, patients were evaluated and followed up by the therapist at baseline (before treatment), after treatment, or before discharge.
2.5.1 Main evaluation indicators
2.5.1.1 Fugl-Meyer Assessment Upper Extremity Scale (FMA-UE)
The FMA-UE assesses the recovery of the shoulder, forearm, elbow, wrist, and hand. The specific assessment consists of 33 items, each of which is scored on three levels: 2 for full conduction, 1 for partial conduction, and 0 for no conduction. With a maximum score of 66 and a minimum of 0, the scale has high reliability and validity, with higher final scores indicating better function (25, 26).
2.5.1.2 Wolf Motor Function Test (WMFT)
The WMFT-FAS assesses upper limb motor function and consists of 15 items ranging from simple forearm touching to a table to complex card flipping, etc. A score of 0 indicates that the affected side cannot be used, and a score of 5 indicates full ability to perform the task. The scale has high reliability and validity, with higher final scores indicating better function (27).
2.5.1.3 Action Research Arm Test (ARAT)
The ARAT assesses the activity and participation of the upper extremity. The specific assessment consists of 19 items, each of which consists of four components: grasping, grip strength, pinching, and gross motor. Each item is scored from 0 to 3, with 0 indicating no movement and 3 indicating full completion. The maximum score is 57. The scale has high reliability and validity, with higher final scores indicating better functioning.
2.5.2 Secondary outcome indicators
The Internal Activities of Daily Living (IADL) assesses the patient’s functional independence. The specific questionnaire consists of eight components: responsibility for taking medication, ability to handle finances, preparing food, using the telephone, shopping, doing housework, washing personal clothes, and using transport. The scale has high reliability and validity, with higher total scores indicating better independence.
2.6 Statistical analysis
The analysis included measures such as median (IQR) for continuous variables and frequencies and percentages for categorical variables. Group comparisons for continuous variables were performed using the Wilcoxon rank-sum test or the Kruskal-Wallis test. For comparison between groups of categorical data, we used the Fisher exact test for expected frequencies <5; otherwise, we used the Chi-squared test.
The efficacy evaluation is mainly based on the concept of double difference. Analysis of variance (ANOVA) was used to compare the change (gain) in each outcome indicator before and after treatment between groups. Home-based TR training was considered non-inferior to face-to-face task-oriented training during hospitalization if the upper limit of the 95% confidence interval (CI) for the difference in FMA-UE gain before and after the two treatments was not greater than the noninferiority margin. The non-inferiority margin was set at 12.4, which has been reported to be the minimum clinically important difference (MCID) for FMA-UE in stroke patients (28, 29). Although not directly validated in our cohort, this threshold aligns with clinical relevance, and prior studies were also referenced (28, 29). Priori sample size calculation was performed based on the non-inferiority margin (MCID = 12.4), with an assumed standard deviation of 8.8 (from pilot data), alpha = 0.05, and power = 80%, yielding a required sample size of 25 per group. Post-hoc power analysis confirmed 78.5% power - above the 75% minimum recommended for non-inferiority trials (25, 26), the final sample size (n = 79) met this requirement.
Subgroup analyses were performed to examine differences across subgroups (gender, stroke type, and lesion side) and whether there is any difference in efficacy, the least squares mean and its confidence interval based on the ANOVA model and the p-value showing the interaction can help to determine the difference between different groups, so we selected the FMA as an outcome indicator to draw the forest plot for subgroup analysis. In our study, all statistical analyses were performed using the R software (version 4.2.2).
3 Results
A total of 96 stroke patients were recruited, 10 patients were excluded for various reasons, 86 people were categorized into three groups because of the different types of intervention, of which 7 without data and withdrew from the study. A total of 79 subjects completed the trial (see Figure 1 for the inclusion flowchart), and no adverse reactions were reported. General information, including mean age, MMSE scores, effective duration of intervention, gender, stroke type, and site of injury, was statistically analyzed across the three groups, and the differences were not statistically significant (p > 0.05). There was a significant difference in the disease duration among the three groups (p<0.001), with the Tele-Rehab group having the longest disease duration, followed by the Tele-Control group, and the shortest being the FTF group, we used ANCOVA to correct for differences in disease duration. The detailed results are shown in Table 2.
Figure 1
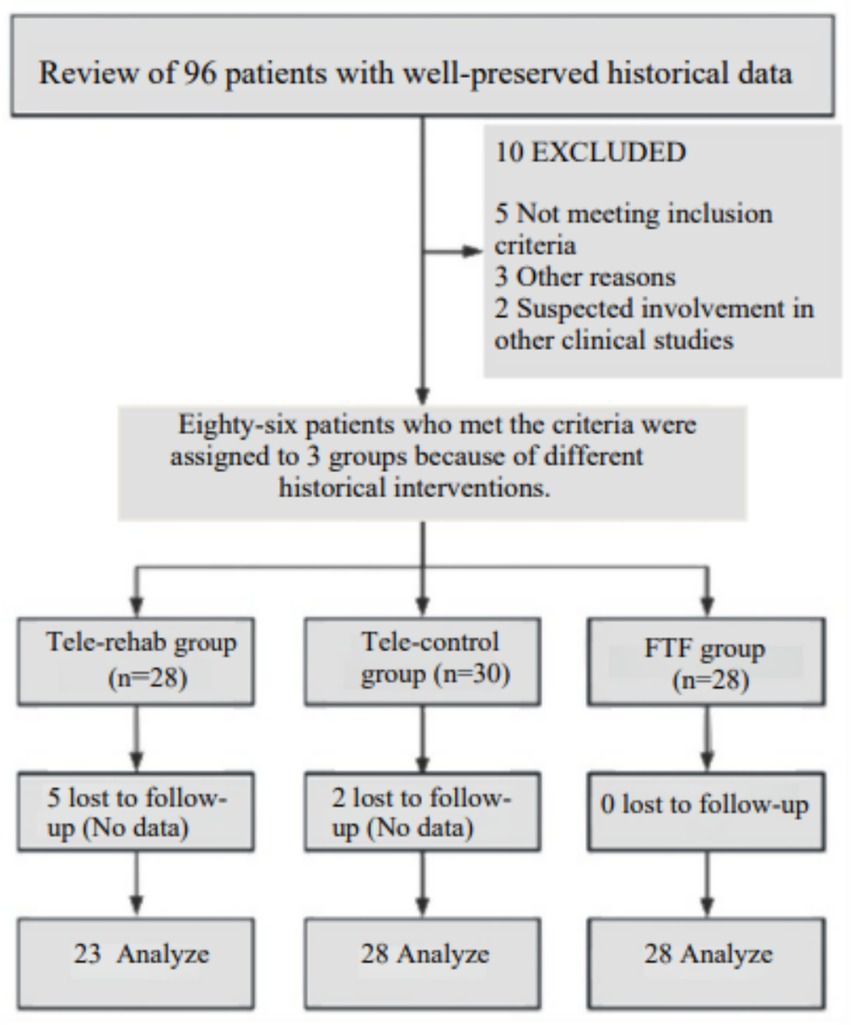
Patients recruitment flowchart.
Table 2
| Characteristic | Group | p-value | ||
|---|---|---|---|---|
| Tele-Control, N = 281 | FTF, N = 281 | Tele-Rehab, N = 231 | ||
| Age | 57 (47, 66) | 60 (53, 63) | 60 (50, 63) | 0.6462 |
| MMSE | 27.5 (25.5, 30.0) | 27.5 (23.8, 30.0) | 26.0 (24.5, 30.0) | 0.6422 |
| Disease duration (days) | 47 (41, 62) | 29 (21, 44) | 70 (48, 140) | <0.0012 |
| Treatment time | 32.0 (28.0, 32.3) | 29.5 (25.8, 31.0) | 30.0 (29.0, 31.0) | 0.1122 |
| Sex | 0.7333 | |||
| Female | 8 (28.6%) | 10 (35.7%) | 6 (26.1%) | |
| Male | 20 (71.4%) | 18 (64.3%) | 17 (73.9%) | |
| Stroke type | 0.1133 | |||
| Hemorrhage | 10 (35.7%) | 8 (28.6%) | 13 (56.5%) | |
| Infarction | 18 (64.3%) | 20 (71.4%) | 10 (43.5%) | |
| Lesion side | 0.9723 | |||
| Left | 15 (53.6%) | 15 (53.6%) | 13 (56.5%) | |
| Right | 13 (46.4%) | 13 (46.4%) | 10 (43.5%) | |
| FAC | 0.8093 | |||
| FAC-3 | 9 (32.1%) | 7 (25.0%) | 5 (21.7%) | |
| FAC-4 | 13 (46.4%) | 17 (60.7%) | 13 (56.5%) | |
| FAC-5 | 6 (21.4%) | 4 (14.3%) | 5 (21.7%) | |
| Ashworth spasticity | 0.0963 | |||
| I+ | 10 (35.7%) | 12 (42.9%) | 15 (65.2%) | |
| II | 18 (64.3%) | 16 (57.1%) | 8 (34.8%) | |
Patient demographics and baseline characteristics.
1 Median (IQR); n (%); 2 Kruskal-Wallis rank sum test; 3 Pearson's Chi-squared test.
FAC, Functional Ambulation Category.
3.1 Major outcomes
Before treatment, the scores of the three groups of patients were compared; the differences were not statistically significant (p > 0.05) and were comparable. After treatment, we found that the scores of the Tele-Rehab group, the FTF group, and the Tele-Control group were significantly improved compared with those of the pre-treatment group (p > 0.05). Detailed results are shown in Table 3. The non-inferiority results showed (see Table 4) that the FMA-UE scores of the Tele-Rehab group were non-inferior to those of the FTF group and the Tele-Control group after the treatment, and the difference between the pre-and post-treatment values was also non-inferior to those of the other two groups. The 95% CI for the difference in change between FMA-UE treatment in the test and FTF groups did not exceed a non-inferiority margin of 12.4, indicating that treatment in the test group was non-inferior to that in the FTF group (mean [SD] of 9.4 (8.80) in the test group and 6.4 (7.52) in the FTF group; mean difference between groups: 3.29; 95% confidence interval: (−0.81, 7.39)). The 95% CI for the difference in change between the Tele-rehab and Tele-Control groups, and the FTF and Tele-Control groups also did not exceed a non-inferiority margin of 12.4. The Tele-Rehab group showed a numerically greater improvement in FMA-UE compared to both the FTF and Tele-Control groups, although the difference did not reach statistical superiority (p > 0.05).
Table 3
| Characteristic | Group | p-value | |||
|---|---|---|---|---|---|
| Tele-Control, N = 281 | FTF, N = 281 | Tele-Rehab, N = 231 | |||
| FMA | Baseline | 16 (9, 38) | 20 (6, 37) | 29 (11, 45) | 0.6832 |
| Post-treatment | 28 (13, 50) | 31 (12, 43) | 35 (21, 55) | 0.4992 | |
| WOLF | Baseline | 7 (5, 23) | 12 (2, 22) | 20 (7, 30) | 0.5202 |
| Post-treatment | 17 (11, 35) | 16 (7, 36) | 26 (14, 39) | 0.5202 | |
| ARAT | Baseline | 3 (3, 12) | 4 (3, 11) | 3 (3, 13) | 0.8202 |
| Post-treatment | 8 (3, 26) | 6 (3, 20) | 6 (4, 25) | 0.6792 | |
| IADL | Baseline | 9.0 (6.0, 13.3) | 8.0 (6.0, 11.0) | 10.0 (6.0, 11.0) | 0.3802 |
| Post-treatment | 10.5 (8.0, 13.3) | 9.0 (7.0, 11.3) | 12.0 (8.5, 14.0) | 0.1032 | |
Comparison between groups before and after treatment.
FMA, Fugl-Meyer Assessment Upper Extremity Scale; WOLF, Wolf Motor Function Test; ARAT, Action Research Arm Test; IADL, Instrumental Activities of Daily Living; Tele-Control, Tele-Control; FTF, Face to Face; Tele-Rehab, Tele-rehabilitation.
Table 4
| Group | Baseline | Post-treatment-FMA | Change from baseline | ||||
|---|---|---|---|---|---|---|---|
| N | Mean (SD) | N | Mean (SD) | N | Mean (SD) | LS Mean (95% CI) a | |
| FTF | 28 | 24.9 (19.48) | 28 | 31.2 (19.58) | 28 | 6.4 (7.52) | 6.31 (3.52, 9.10) |
| Tele-Control | 28 | 25.1 (20.49) | 28 | 31.8 (20.18) | 28 | 6.7 (6.28) | 6.62 (3.83, 9.41) |
| Tele-Rehab | 23 | 28.1 (18.62) | 23 | 37.6 (18.67) | 23 | 9.4 (8.80) | 9.61 (6.52, 12.69) |
| Pairwise comparison | Difference in LS Mean (95% CI) a | p-value |
|---|---|---|
| (Tele-Control) - FTF | 0.31 (−3.58, 4.19) | 0.987 |
| (Tele-Rehab) - FTF | 3.29 (−0.81, 7.39) | 0.263 |
| (Tele-Rehab) - (Tele-Control) | 2.99 (−1.11, 7.08) | 0.332 |
Effectiveness analysis.
a Based on an ANCOVA model after adjusting baseline FMA. ANCOVA, Analysis of Covariance; CI, Confidence Interval; LS, Least Squares; SD, Standard Deviation.
For the primary outcome (FMA-UE), the 95% CI of the between-group difference [−0.81, 7.39] did not cross the non-inferiority margin (12.4). The upper limit (7.39) was 5.01 points below the MCID - exceeding FMA-UE’s typical standard error of measurement (SEM = 3.2 points (24)). Sensitivity analysis using bias-corrected bootstrapping yielded consistent results (95% CI: −0.75 to 7.31).
3.2 Secondary outcomes
The difference in IADL scores among the three groups before treatment was not statistically significant (p > 0.05) and was comparable. For secondary outcomes (WMFT, ARAT, IADL): Group differences had narrower CIs (e.g., WMFTΔ: 95% CI [−1.22, 5.18]) due to lower variability (SD < 6.0). No significant interactions were found in subgroup analyses (all p > 0.10), suggesting consistent effects despite group size differences. Demonstrates that the primary concern (wide CI) was isolated to FMA-UE and did not affect other outcomes, highlights internal consistency of results.
3.3 Subgroup analyses
Subgroup analyses of FMA, the primary outcome indicator, were conducted at the end of treatment to assess the impact of gender, stroke type, and stroke site on outcomes. It was found that efficacy was not affected by gender, stroke type and stroke site. Specifically, see Figure 2.
Figure 2
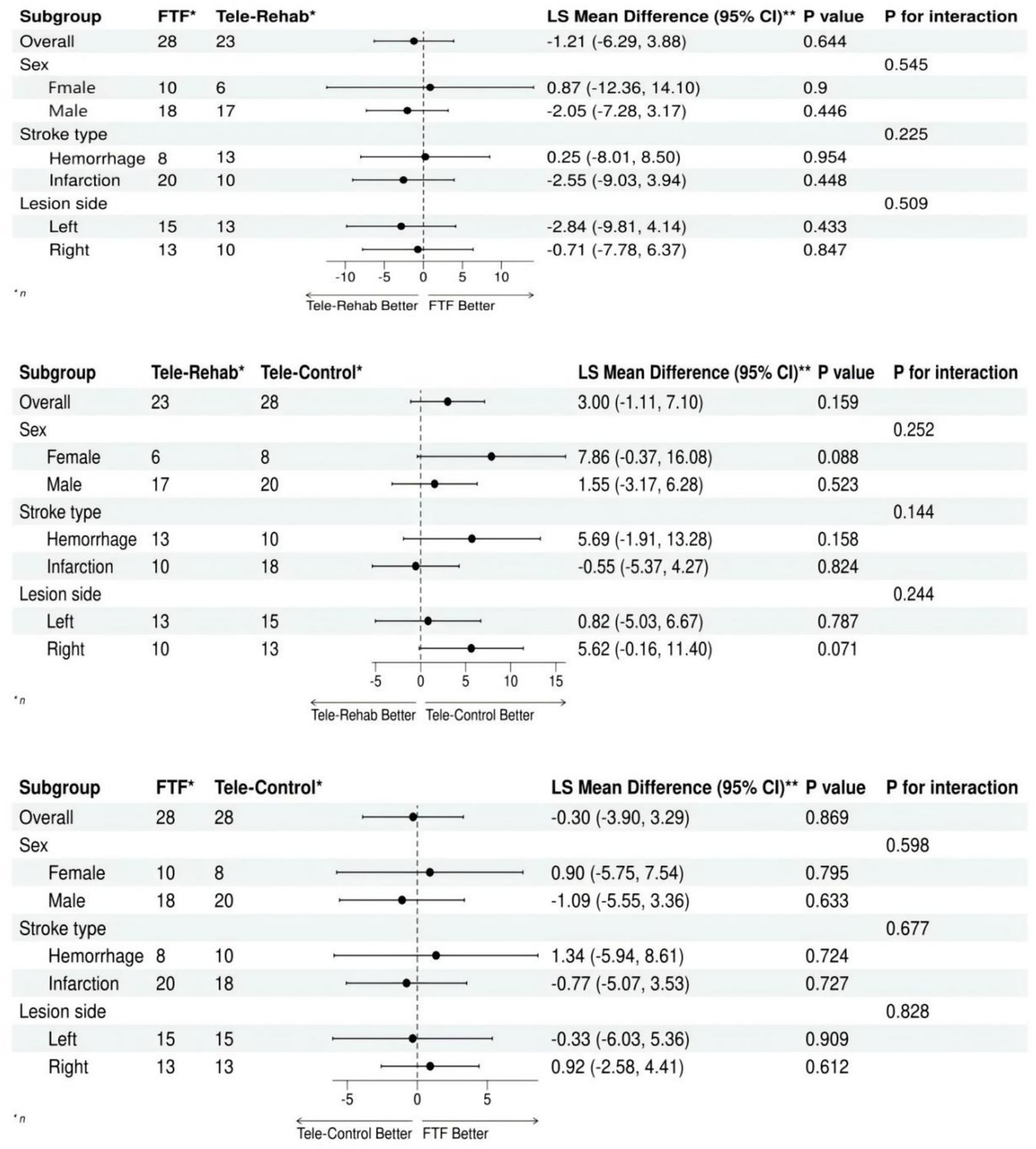
Forest plot of subgroup analysis for FMA-UE.
4 Discussion
The results of this study found that the scores of all groups were higher after the treatment than before the treatment, in which the difference between the pre and post-test scores of the Tele-Rehab group was not inferior to that of the conventional and Tele-Control groups. The above results suggest that TR or face-to-face combined with task-oriented training or tele-conventional neurological easing techniques can improve the upper limb motor function and daily living ability of stroke patients.
Stroke often affects the control ability of some areas of the brain due to the death of brain cells (30), which leads to some functional impairment after a period of rehabilitation (31), upper limb motor dysfunction is often more serious than the lower limb (32), and upper limb motor dysfunction has a great impact on the quality of life (33, 34), so there is an urgent need for highly operable and effective training programs (35). Recent studies have further demonstrated that changes in cortical-muscular coupling in stroke patients are significantly associated with clinical function scores (e.g., FMA-UE), which provides physiological evidence that task-oriented training improves motor function through neuroplasticity mechanisms (36).
Our TR-TOT adherence rate (92%) exceeded the 78% reported in Tchero et al.’s study (15), likely due to hybrid synchronous-asynchronous supervision (real-time correction + weekly audits). The FMA-UE improvement (∆9.4) aligns with Cramer et al.’s home-based telerehabilitation trial (∆8.7) (10), but contrasts with Laver et al.’s finding of superior clinic-based outcomes (9). This discrepancy may stem from our ecologically valid tasks (e.g., cup grasping) versus standardized equipment training. Notably, TR neurofacilitation (∆6.7) showed comparable efficacy to face-to-face TOT (∆6.4), supporting Chen et al.’s (25) assertion. Self-guided protocols suffice for structured techniques like Brunnstrom. From the perspective of training modality, we found that TR combined with task-oriented training could improve patients’ ability to perform daily living activities, and the Mean (SD) of the difference between pre-and post-FMA-UE scores, which was not inferior to task-oriented training performed face-to-face. Statistically corrected results support non-inferiority despite potential confounders (e.g., environmental differences). It cannot be denied that TR, as a means of providing online services for rehabilitation (27), is non-inferior to face-to-face rehabilitation training, and the results are independent of gender, type of lesion, and lesion location. In addition, TR has the characteristics of low cost and is not affected by geography (24). Consequently, with the popularity of the technology and the individualization of the training intensity, etc., it may be widely applied to stroke patients who require long-term rehabilitation training.
From the perspective of training methods, we found that both remote task-oriented training and conventional neural facilitation techniques can improve upper limb function in stroke patients, and the efficacy of both is comparable. Task-oriented training emphasizes a task-oriented strategy, which aims to train patients toward a certain goal through targeted and repetitive training (37) and to provide certain incentives (38), as well as to develop their ability to adapt to different environments (22, 39). Neurofacilitation techniques are based on physiological and developmental theories to restore motor function, emphasizing the therapist’s skills and the patient’s cooperation usually without incentives. The results of this study show that task-oriented training and conventional neuro-easy techniques are equally effective in restoring upper limb function in stroke patients, suggesting that patients can choose the appropriate method according to their needs and acceptability. The results of this study may be related to the differences arising from the patients’ degree of self-management and training standardization. Finally, most of the patients only trained for about 1 month, after which there was no follow-up, which could be followed up to observe the long-term efficacy of the different groups. TR-TOT’s non-inferiority may stem from: (1) Neuroplasticity: Home-environment training promotes skill generalization (40); (2) Self-efficacy: Patient autonomy enhances engagement (41, 42); (3) It’s also a dual cognitive + motor training (43), essentially a clinical application of ecological validity, − embedding rehabilitation scenarios into real-life environments and bridging the gap between traditional training and life practice.
This study has several limitations. First, the relatively small sample size (n = 79) may restrict the generalizability of findings and reduce statistical power to detect subtle differences between groups. Second, the non-inferiority margin (12.4 points on FMA-UE) was adopted from prior literature but lacked direct validation in our population, potentially affecting interpretation. The smaller sample in the Tele-Rehab group (n = 23) reduced precision for FMA-UE comparisons, as reflected in the wider confidence interval (−0.81 to 7.39). While statistically adequate for non-inferiority conclusions (power = 78.5%), future trials should recruit ≥35 participants per group to achieve 90% power and narrower CIs. Third, the 3-week intervention period and absence of long-term follow-up limit conclusions about sustained treatment effects. Fourth, while randomization was implemented, baseline disease duration differed significantly across groups (p < 0.001), introducing potential confounding. Additionally, TR protocols relied on patient self-reporting for adherence monitoring, and environmental factors (e.g., home setup quality) were not systematically controlled. Although disease duration differed significantly across groups, we adjusted for this variable in the ANCOVA model to minimize potential confounding. Finally, the single-center design and specific cultural context of China’s healthcare system may limit cross-regional applicability. The greater numerical improvement suggests that future studies need to further validate its potential benefits. Future research could incorporate emerging temporal-guided adaptive graph learning techniques (44) to more accurately identify patients’ coordinated movement patterns to optimize personalized tele-rehabilitation programs. There is also a trend toward combining neuromodulation techniques (45, 46) or home virtual reality (47), Constraint-induced movement therapy (48), and so on.
The efficacy of TR combined with task-oriented training is no less than that of face-to-face task-oriented training, and also the effectiveness of task-oriented training is comparable to that of neural efficiency training, with significant improvement in both upper limb dysfunction remaining in post-stroke patients and in reduced ability to perform activities of daily living.
5 Conclusion
This study has demonstrated that TR combined with task-oriented training is feasible and non-inferior to for upper limb dysfunction in stroke patients and that both task-oriented training and neural facilitation techniques are effective in promoting upper limb functional recovery in stroke patients. Many studies have indicated that a certain amount of dysfunction may still exist even months after stroke. If the TR platform can be improved and optimized in the future, this will be a great benefit to society and families.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
The studies involving humans were approved by the Ethics Committee of Yuebei People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
XH: Conceptualization, Data curation, Formal analysis, Writing – original draft, Writing – review & editing. HC: Investigation, Methodology, Project administration, Resources, Writing – original draft, Writing – review & editing. XB: Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. JL: Data curation, Methodology, Supervision, Writing – original draft, Writing – review & editing. XL: Formal analysis, Project administration, Validation, Writing – original draft, Writing – review & editing. JC: Data curation, Methodology, Supervision, Writing – original draft, Writing – review & editing. ZL: Conceptualization, Methodology, Software, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Shaoguan City Health and Wellness Research Project: No. Y23014.
Acknowledgments
We would like to thank all the staff involved in the Yuebei People’s Hospital for their support and help in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Boursin P Paternotte S Dercy B Sabben C Maïer B . Semantics, epidemiology and semiology of stroke. Soins. (2018) 63:24–7. doi: 10.1016/j.soin.2018.06.008
2.
Tater P Pandey S . Post-stroke movement disorders: clinical spectrum, pathogenesis, and management. Neurol India. (2021) 69:272–83. doi: 10.4103/0028-3886.314574
3.
Fu J Zeng M Shen F Cui Y Zhu M Gu X et al . Effects of action observation therapy on upper extremity function, daily activities and motion evoked potential in cerebral infarction patients. Medicine. (2017) 96:e8080. doi: 10.1097/MD.0000000000008080
4.
Persson HC Alt Murphy M Danielsson A Lundgren-Nilsson Å Sunnerhagen KS . A cohort study investigating a simple, early assessment to predict upper extremity function after stroke - a part of the SALGOT study. BMC Neurol. (2015) 15:92. doi: 10.1186/s12883-015-0349-6
5.
Lin S-H Yang T-R Chuang IC Chen C-L Wu C-Y . Upper extremity motor abilities and cognitive capability mediate the causal dependency between somatosensory capability and daily function in stroke individuals. Sci Rep. (2022) 12:690. doi: 10.1038/s41598-021-04491-2
6.
Lee D-H Lee J-H . A study on the physical therapy approach for improving the upper extremity function of spastic ischemic stroke patients. Int J Adv Nurs Educ Res. (2019) 4:7–12. doi: 10.21742/ijaner.2019.4.3.02
7.
Zhang LJ Wen X Peng Y Hu W Liao H Liu ZC et al . Effectiveness of the A3 robot on lower extremity motor function in stroke patients: a prospective, randomized controlled trial. World J Clin Cases. (2024) 12:5523–33. doi: 10.12998/wjcc.v12.i24.5523
8.
Perera KS de Boasquevisque D Rao-Melacini P Taylor A Cheng A Hankey GJ et al . Evaluating rates of recurrent ischemic stroke among young adults with embolic stroke of undetermined source. JAMA Neurol. (2022) 79:450. doi: 10.1001/jamaneurol.2022.0048
9.
Laver KE Adey-Wakeling Z Crotty M Lannin NA George S Sherrington C . Telerehabilitation services for stroke. Cochrane Database Syst Rev. (2020) 2020:255. doi: 10.1002/14651858.CD010255.pub3
10.
Cramer SC Dodakian L Le V See J Augsburger R McKenzie A et al . Efficacy of home-based Telerehabilitation vs in-clinic therapy for adults after stroke: a randomized clinical trial. JAMA Neurol. (2019) 76:1079–87. doi: 10.1001/jamaneurol.2019.1604
11.
Peng Y Wang J Liu Z Zhong L Wen X Wang P et al . The application of brain-computer Interface in upper limb dysfunction after stroke: a systematic review and Meta-analysis of randomized controlled trials. Front Hum Neurosci. (2022) 16:798883. doi: 10.3389/fnhum.2022.798883
12.
Wen X Li L Li X Zha H Liu Z Peng Y et al . Therapeutic role of additional Mirror therapy on the recovery of upper extremity motor function after stroke: a single-blind, randomized controlled trial. Neural Plast. (2022) 2022:1–9. doi: 10.1155/2022/8966920
13.
Everard G Declerck L Detrembleur C Leonard S Bower G Dehem S et al . New technologies promoting active upper limb rehabilitation after stroke: an overview and network meta-analysis. Eur J Phys Rehabil Med. (2022) 58:530–48. doi: 10.23736/S1973-9087.22.07404-4
14.
Knepley KD Mao JZ Wieczorek P Okoye FO Jain AP Harel NY . Impact of Telerehabilitation for stroke-related deficits. Telemed J E Health. (2021) 27:239–46. doi: 10.1089/tmj.2020.0019
15.
Tchero H Tabue Teguo M Lannuzel A Rusch E . Telerehabilitation for stroke survivors: systematic review and Meta-analysis. J Med Internet Res. (2018) 20:e10867. doi: 10.2196/10867
16.
Everard G Luc A Doumas I Ajana K Stoquart G Edwards MG et al . Self-rehabilitation for post-stroke motor function and activity-a systematic review and Meta-analysis. Neurorehabil Neural Repair. (2021) 35:1043–58. doi: 10.1177/15459683211048773
17.
Rowe VT Neville M . Client perceptions of task-oriented training at home: "I forgot I was sick". OTJR. (2018) 38:190–5. doi: 10.1177/1539449218762729
18.
da Silva ESM Ocamoto GN Santos-Maia GLD de Fátima Carreira Moreira Padovez R Trevisan C de Noronha MA et al . The effect of priming on outcomes of task-oriented training for the upper extremity in chronic stroke: a systematic review and meta-analysis. Neurorehabil Neural Repair. (2020) 34:479–504. doi: 10.1177/1545968320912760
19.
Alsubiheen AM Choi W Yu W Lee H . The effect of task-oriented activities training on upper-limb function, daily activities, and quality of life in chronic stroke patients: a randomized controlled trial. Int J Environ Res Public Health. (2022) 19:4125. doi: 10.3390/ijerph192114125
20.
Pimentel Piemonte ME Okamoto E . Improvement in gait performance after training based on declarative memory cues in patients with Parkinsons disease: a randomized clinical trial. J Novel Physiother. (2015) 5:277. doi: 10.4172/2165-7025.1000277
21.
Kleim JA Jones TA . Principles of experience-dependent neural plasticity: implications for rehabilitation after brain damage. J Speech Lang Hear Res. (2008) 51:S225–39. doi: 10.1044/1092-4388(2008/018)
22.
Timmermans AAA Spooren AIF Kingma H Seelen HAM . Influence of task-oriented training content on skilled arm-hand performance in stroke: a systematic review. Neurorehabil Neural Repair. (2010) 24:858–70. doi: 10.1177/1545968310368963
23.
Lang CE Strube MJ Bland MD Waddell KJ Cherry-Allen KM Nudo RJ et al . Dose response of task-specific upper limb training in people at least 6 months poststroke: a phase II, single-blind, randomized, controlled trial. Ann Neurol. (2016) 80:342–54. doi: 10.1002/ana.24734
24.
Chen Y Abel KT Janecek JT Chen Y Zheng K Cramer SC . Home-based technologies for stroke rehabilitation: a systematic review. Int J Med Inform. (2019) 123:11–22. doi: 10.1016/j.ijmedinf.2018.12.001
25.
Chen J Sun D Zhang S Shi Y Qiao F Zhou Y et al . Effects of home-based telerehabilitation in patients with stroke. Neurology. (2020) 95:821. doi: 10.1212/WNL.0000000000010821
26.
Sveen U Bautz-Holter E Sødring KM Wyller TB Laake K . Association between impairments, self-care ability and social activities 1 year after stroke. Disabil Rehabil. (1999) 21:372–7. doi: 10.1080/096382899297477
27.
Wolf SL Catlin PA Ellis M Archer AL Morgan B Piacentino A . Assessing Wolf Motor function test as outcome measure for research in patients after stroke. Stroke. (2001) 32:1635–9. doi: 10.1161/01.STR.32.7.1635
28.
Hiragami S Inoue Y Harada K . Minimal clinically important difference for the Fugl-Meyer assessment of the upper extremity in convalescent stroke patients with moderate to severe hemiparesis. J Phys Ther Sci. (2019) 31:917–21. doi: 10.1589/jpts.31.917
29.
Maeda H Hishikawa N Sawada K Sakurai M Ohashi S Mikami Y . Wearable integrated volitional control electrical stimulation device as treatment for paresis of the upper extremity in early subacute stroke patients: a randomized controlled non-inferiority trial. Arch Phys Med Rehabil. (2024) 105:227–34. doi: 10.1016/j.apmr.2023.08.031
30.
Morone G Cocchi I Paolucci S Iosa M . Robot-assisted therapy for arm recovery for stroke patients: state of the art and clinical implication. Expert Rev Med Devices. (2020) 17:223–33. doi: 10.1080/17434440.2020.1733408
31.
Winstein CJ Stein J Arena R Bates B Cherney LR Cramer SC et al . Guidelines for adult stroke rehabilitation and recovery. Stroke. (2016) 47:98. doi: 10.1161/STR.0000000000000098
32.
Moon J-H Cho H-Y Hahm S-C . Influence of electrotherapy with task-oriented training on spasticity, hand function, upper limb function, and activities of daily living in patients with subacute stroke: a double-blinded, randomized, controlled trial. Healthcare. (2021) 9:987. doi: 10.3390/healthcare9080987
33.
Inatomi Y Nakajima M Yonehara T Ando Y . Ipsilateral hemiparesis in ischemic stroke patients. Acta Neurol Scand. (2017) 136:31–40. doi: 10.1111/ane.12690
34.
Qu Q Lin Y He Z Fu J Zou F Jiang Z et al . The effect of applying robot-assisted task-oriented training using human-robot collaborative interaction force control technology on upper limb function in stroke patients: preliminary findings. Biomed Res Int. (2021) 2021:1–8. doi: 10.1155/2021/9916492
35.
Mayo NE . Stroke rehabilitation at home. Stroke. (2016) 47:1685–91. doi: 10.1161/STROKEAHA.116.011309
36.
Wang X Li W Song R Ao D Hu H Li L . Corticomuscular coupling alterations during elbow isometric contraction correlated with clinical scores: an fNIRS-sEMG study in stroke survivors. IEEE Trans Neural Syst Rehabil Eng. (2025) 33:696–704. doi: 10.1109/TNSRE.2025.3535928
37.
He Y-Z Huang Z-M Deng H-Y Huang J Wu J-H Wu J-S . Feasibility, safety, and efficacy of task-oriented mirrored robotic training on upper-limb functions and activities of daily living in subacute poststroke patients: a pilot study. Eur J Phys Rehabil Med. (2024) 59:660–8. doi: 10.23736/S1973-9087.23.08018-8
38.
Jeong S Chung Y . Task-oriented training with abdominal drawing-in maneuver in sitting position for trunk control, balance, and activities of daily living in patients with stroke: a pilot randomized controlled trial. Healthcare. (2023) 11. doi: 10.3390/healthcare11233092
39.
Li Y Lian Y Chen X Zhang H Xu G Duan H et al . Effect of task-oriented training assisted by force feedback hand rehabilitation robot on finger grasping function in stroke patients with hemiplegia: a randomised controlled trial. J Neuroeng Rehabil. (2024) 21:77. doi: 10.1186/s12984-024-01372-3
40.
Zich C Debener S Schweinitz C Sterr A Meekes J Kranczioch C . High-intensity chronic stroke motor imagery neurofeedback training at home: three case reports. Clin EEG Neurosci. (2017) 48:403–12. doi: 10.1177/1550059417717398
41.
Bandura A Adams NE Beyer J . Cognitive processes mediating behavioral change. J Pers Soc Psychol. (1977) 35:125–39. doi: 10.1037/0022-3514.35.3.125
42.
Bandura A . Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. (1977) 84:191–215. doi: 10.1037/0033-295X.84.2.191
43.
Yang Z-Q Wei M-F Chen L Xi J-N . Research progress in the application of motor-cognitive dual-task training in rehabilitation of walking function in stroke patients. J Neuro-Oncol. (2023) 11:100028. doi: 10.1016/j.jnrt.2022.100028
44.
Li L Zhang M Chen Y Wang K Zhou G Huang Q . Tagl: temporal-guided adaptive graph learning network for coordinated movement classification. IEEE Trans Ind Inform. (2024) 20:12554–64. doi: 10.1109/TII.2024.3423311
45.
Cheng JL Tan C Liu HY Han DM Liu ZC . Past, present, and future of deep transcranial magnetic stimulation: a review in psychiatric and neurological disorders. World J Psychiatry. (2023) 13:607–19. doi: 10.5498/wjp.v13.i9.607
46.
Fan P Wu C Liu B . Ischemic stroke treatment by vagus nerve stimulation: a comprehensive review of mechanisms, clinical efficacy, and future directions. J Neuro-Oncol. (2025) 13:100209. doi: 10.1016/j.jnrt.2025.100209
47.
Hussain MA Waris A Gilani SO Mushtaq S Pujari AN Khan NB et al . Virtual reality as a non-conventional rehabilitation for stroke: a comprehensive review. J Neuro-Oncol. (2024) 12:100135. doi: 10.1016/j.jnrt.2024.100135
48.
Shamweel H Gupta N . Constraint-induced movement therapy through telerehabilitation for upper extremity function in stroke. J Neuro-Oncol. (2024) 12:100108. doi: 10.1016/j.jnrt.2024.100108
Summary
Keywords
stroke, telerehabilitation, task-oriented training, clinical trials, upper limb dysfunction
Citation
Hong X, Cha H, Bao X, Luo J, Li X, Cheng J and Liu Z (2025) Task-oriented telerehabilitation for upper limb functional recovery after stroke: a retrospective cohort study. Front. Neurol. 16:1611565. doi: 10.3389/fneur.2025.1611565
Received
14 April 2025
Accepted
12 August 2025
Published
21 August 2025
Volume
16 - 2025
Edited by
Wenxin Niu, Tongji University, China
Reviewed by
Le Li, Northwestern Polytechnical University, China
Klara Novotna, Charles University, Czechia
Updates
Copyright
© 2025 Hong, Cha, Bao, Luo, Li, Cheng and Liu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jinling Cheng, jl1472582022@163.com; Zicai Liu, 1454262065@qq.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.