- 1National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion, Tianjin, China
- 2First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Tianjin, China
- 3Tianjin University of Traditional Chinese Medicine, Tianjin, China
- 4Shanghai University of Traditional Chinese Medicine, Shanghai, China
Objective: Antagonistic muscles rehabilitation training has been extensively utilized in the rehabilitation of patients with spastic hemiplegia. With the increasing acceptance and application of acupuncture, numerous scholars have discovered that incorporating electroacupuncture combined with antagonistic muscles rehabilitation training can enhance the treatment for spastic hemiplegia after stroke. The objective of this study is quantify the clinical efficacy of electroacupuncture in treating spastic hemiplegia after stroke on the basis of antagonistic muscles rehabilitation training, provide insights for future clinical treatments and scientific investigations related to spastic hemiplegia.
Methods: We searched eight Chinese and English databases to identify clinical randomized controlled trials investigating the efficacy of electroacupuncture antagonistic muscles combined with rehabilitation training for the treatment of spastic hemiplegia after stroke. The search period extended from the inception of each database up to April 4, 2025. Two researchers independently reviewed the literatures, extracted relevant data, and assessed the risk of bias using the Cochrane Risk of Bias Tool.
Results: A total of 8 literatures were selected from an initial pool of 1,680 for the purpose of meta-analysis. The findings indicated that the combination of electroacupuncture antagonistic muscles with rehabilitation training significantly alleviates muscle spasms in hemiplegic limbs [MD = –0.52,95%CI (−0.91, −0.13), p = 0.36, I2 = 0%, Z = 2.6, p < 0.05], enhances daily living capabilities [MD = 6.31,95%CI (3.91,8.71), p = 0.02, I2 = 59%, Z = 5.15, p < 0.05], improve motor function [MD = 9.9,95%CI (8.25,11.55), p = 0.2, I2 = 33%, Z = 11.75, p < 0.05]. Furthermore, we discovered that when the wave type and frequency of electroacupuncture are low frequency intermittent waves, electroacupuncture antagonistic muscles combined with rehabilitation training can effectively improve the lower limb motor function of hemiplegic patients. [MD = 10.52,95%CI (8.66,12.37), p = 0.89, I2 = 0%, Z = 11.11, p < 0.05], and electroacupuncture combined with Bobath technique is better than combined with conventional rehabilitation training.
Conclusion: The integration of electroacupuncture treatment with antagonist muscle rehabilitation training can effectively alleviate muscle spasms, reduce muscle tension, and enhance lower limb motor function as well as daily living abilities.
1 Introduction
Stroke ranks as the second leading cause of death globally (1). Research indicates that approximately one in four individuals globally will experience a stroke (2), and the population affected by strokes is increasing each year (3). When hemorrhage or infarction occurs in the cerebral cortex, internal capsule or basal ganglia, the damage to the cortical-reticular projection neurons, along with heightened excitability of the pontine reticular spinal cord bundle and diminished inhibitory influence from the medullary reticular spinal cord bundle, results in an increased excitability of the spinal cord motor neurons (4, 5), the patients will exhibit static deformities as well as joint contractures associated with static deformity (6), According to statistical data, approximately 17.0 to 42.6% of stroke patients are likely to experience spastic hemiplegia (7), The spasticity of the limbs may be more pronounced in younger patients (8). Although spasmodic muscles can sustain the tone of the limbs to facilitating standing and walking, prolonged limb spasms may lead to permanent joint contractures and muscle atrophy. Therefore, if the spasmodic condition of the limb is not addressed in time, it will lead to increased pessimism among patients. This not only diminishes their adherence to rehabilitation efforts but also reduces the capacity for participation in daily activities and social engagement (9, 10), placing significant strains on healthcare systems and socio-economic structures (11).
The patients diagnosed with spastic hemiparesis primarily exhibit spasticity in the flexor muscles of the upper limbs, as well as spasticity in the extensor muscles of the lower limbs (12), spasticity is observed in the flexor muscle groups located on the anterior and medial aspects of the upper limbs. This includes muscles such as the pectoralis major, latissimus dorsi, vastus lateralis, brachialis, brachioradialis, and rotator cuff muscles responsible for elbow flexion. In addition, spasticity affects muscle groups in the lower extremities, primarily within the anterior-inferior thigh region and posterior calf area. This encompasses muscles such as the quadriceps, adductor group, gastrocnemius, and soleus (13). During treatment, it is essential to harmonize the tone of both active and antagonist muscle groups. This involves enhancing the lateral extensor muscle groups of the upper extremity while simultaneously strengthening the flexor muscle groups of the lower extremity. Such an approach promotes the emergence of limb separation movements and facilitates the establishment of normal movement patterns. Various rehabilitation modalities—including occupational therapy, plyometrics, and joint mobility training—can significantly improve the function of passive structures such as bone assemblies, joint surfaces, and ligaments, as well as active structures like muscle-tendon complexes. These interventions address issues related to mechanical alignment or kinematic alignment anomalies, thereby increasing antagonist muscle strength and inhibiting pathological reflexes. While straightforward rehabilitation training can effectively alleviate limb spasticity, it necessitates significant investment in healthcare personnel, funding, and equipment. Furthermore, in low-income countries and regions, patients may be reluctant to engage with treatment due to the prolonged duration of therapy, slow progress in results, and high associated costs.
With the growing interdisciplinary connections and the recent integration of therapeutic approaches, the efficacy of acupuncture in conjunction with modern rehabilitation techniques for treating post-stroke hemiplegia has increasingly emerged as a prominent area of research (14). Due to its simplicity and efficacy (15), acupuncture is endorsed by the World Health Organization as a complementary and alternative treatment for stroke and its sequelae (16). The application of electroacupuncture, a therapeutic approach that incorporates pulsed electrical stimulation alongside the deqi from millimeter acupuncture (17), offers several advantages. These include precise parameter settings, quantifiable intensity and frequency of stimulation, and consistent levels of acupuncture intervention. Such characteristics can significantly aid in the formulation of a clinically standardized treatment strategy for spastic hemiparesis following stroke. It has been demonstrated that electroacupuncture induces excitatory contractions by stimulating the active muscle, leading to impulse signals being transmitted to the spinal cord via type Ia afferent nerves. This process facilitates the inhibition of corresponding antagonist muscles and alleviates muscle spasms (18). In accordance with the principles of human biomechanics, the movement patterns and neuroanatomical considerations associated with spastic limbs, electroacupuncture antagonist muscles combined with rehabilitation training can significantly enhance limb function and improve daily living capabilities. Furthermore, research has demonstrated that acupuncture can treat spastic hemiparesis through various mechanisms, including improving blood perfusion, reducing neuroinflammation, regulating neuroplasticity (19), remodeling corticospinal tracts, repairing descending motor pathways (20, 21), inhibiting the release and transport of excitatory neurotransmitters to prevent neuronal excitotoxicity (22, 23), decreasing the excitability of spinal cord anterior horn motoneurons, and modifying muscle structure to improve muscular motility in multiple ways (24). The purpose of this paper is to conduct a meta-analysis of the improvement of electroacupuncture antagonistic muscles combined with rehabilitation training on patients with hemiplegia after stroke.to provide the foundation for future in-depth investigations into the effects of electroacupuncture antagonist muscles alongside rehabilitation training therapy on limb function recovery post-stroke. This study has been registered in PROSPERO (No: CRD420251045251).
2 Methods
2.1 Study selection
We searched across eight Chinese and English databases, including PubMed, Cochrane Library, Embase, Web of Science, China Biology Medicine disc (CBM), China National Knowledge Infrastructure (CNKI), China Science Periodical Database (CSPD), and the Chinese Citation Database (CCD). The search period for each database extended from its inception until April 4, 2025. The languages utilized in the search were restricted to Chinese and English. The search strategy employed a combination of subject terms and free-text keywords. The Chinese search terms included “spastic hemiplegia,” “hemiplegia,” “hemiplegia with stroke,” “hemiplegia with hemiparesis,” “post-stroke hemiplegia,” “dystonia enhancement,” “electro-acupuncture,” “electro-acupuncture interventions,” “acupuncture plus electro-acupuncture,” “electro-acupuncture stimulation,” “conventional electro-acupuncture,” “electro-acupuncture treatment,” as well as various forms of randomized controlled trials such as RCTs and related terminology. The English search terms comprised “hemiplegia,” “hemiplegias,” “electroacupuncture,” “randomized controlled trial,” “randomized,” and “placebo.” To develop effective search strategies tailored to the specific requirements and characteristics of different databases in both languages, we applied the PICOS principle while combining spastic hemiplegia subject terms with relevant free-text keywords. This approach aimed to yield comprehensive primary literature on the topic. All search strategies were finalized following multiple iterations of searches. We imported the retrieved titles of Chinese and English literature into NoteExpress software to assess their weights and eliminate duplicates. Two researchers independently reviewed the titles and abstracts, manually re-evaluated the weights, and screened the literatures according to predefined inclusion criteria. Subsequently, both researchers independently downloaded the literatures that met these criteria, read the full texts, and conducted a further screening based on the same inclusion standards. Ultimately, we determined which pieces of literature would be included in our study. Finally, both researchers cross-verified their screening processes; in cases of discrepancies, they engaged in discussions until reached agreement.
2.2 Inclusion criteria
2.2.1 Type of article
Randomized controlled clinical trials of electroacupuncture antagonistic muscles combined with rehabilitation training in the treatment of spastic hemiplegia after stroke.
2.2.2 Research participants
Diagnosed with cerebral infarction or cerebral hemorrhage in Western medicine; accompanied by limb motor dysfunction; there are no restrictions regarding age, gender, or race.
2.2.3 Intervention
The observation group received electroacupuncture antagonist muscles, in conjunction with rehabilitation training and basic treatment. In contrast, the control group underwent rehabilitation training along with basic treatment. Both groups followed an identical course of treatment. The conventional basic treatment employed in Western medicine encompassed antiplatelet aggregation therapy, antihypertensive measures, lipid-lowering interventions, and enhancements to cerebral metabolism, among others. The dosage and duration of these treatments were not subject to restrictions.
2.2.4 Quality assessment criteria
The methodological quality of the included studies was assessed using the Cochrane Collaboration’s risk of bias tool (Risk of Bias Tool). This evaluation encompassed seven key items: randomized sequence generation (selection bias), allocation concealment (selection bias), blinding of subjects and investigators (implementation bias), blinding of outcome evaluators (measurement bias), incomplete outcome data (loss to follow-up bias), selective reporting of outcomes (reporting bias), and other biases. Each item was classified as “low risk,” “unclear,” or “high risk.” To ensure the integrity and quality of the literatures, two independent investigators evaluated the risk of bias for each study. They subsequently discussed their findings and reached a consensus regarding the overall assessment of risk.
2.2.5 Criteria for exclusion
(1) Duplicate literatures; (2) Systematic reviews, commentaries, letters, meeting abstracts, and research protocols; (3) Literatures derived from non-randomized controlled trials; (4) Interventions that do not align with the study criteria; (5) Absence of relevant outcome indicators or inability to extract valid data; (6) Literatures for which the full text is inaccessible; (7) Non clinical trials.
2.2.6 Data extraction
Two researchers independently entered the information from the final included literatures into Microsoft Excel, following the data extraction form. They subsequently cross-checked the entered data with each other and engaged in discussions to resolve any discrepancies. The extracted data encompassed: (1) the name of the researcher, title of the literature, year of publication, sample size, shedding rates, adverse reactions, and other relevant details; (2) patient demographics including age, gender, duration of disease, duration of treatment, interventions administered, controls utilized; and (3) assessments regarding the risk of bias in randomized controlled trials. (4) The outcome measures included the primary endpoint: overall clinical effectiveness, and secondary endpoints such as the simplified Fugl-Meyer motor function rating scale. Additionally, the assessment tools utilized were the Fugl-Meyer Assessment (FMA), Barthel Index (BI), and Modified Ashworth Scale (MAS). In cases where study data were inadequately described or information was lacking in the literature, we were contacted via email for clarification; otherwise, those literatures were excluded from consideration.
2.2.7 Statistical analysis
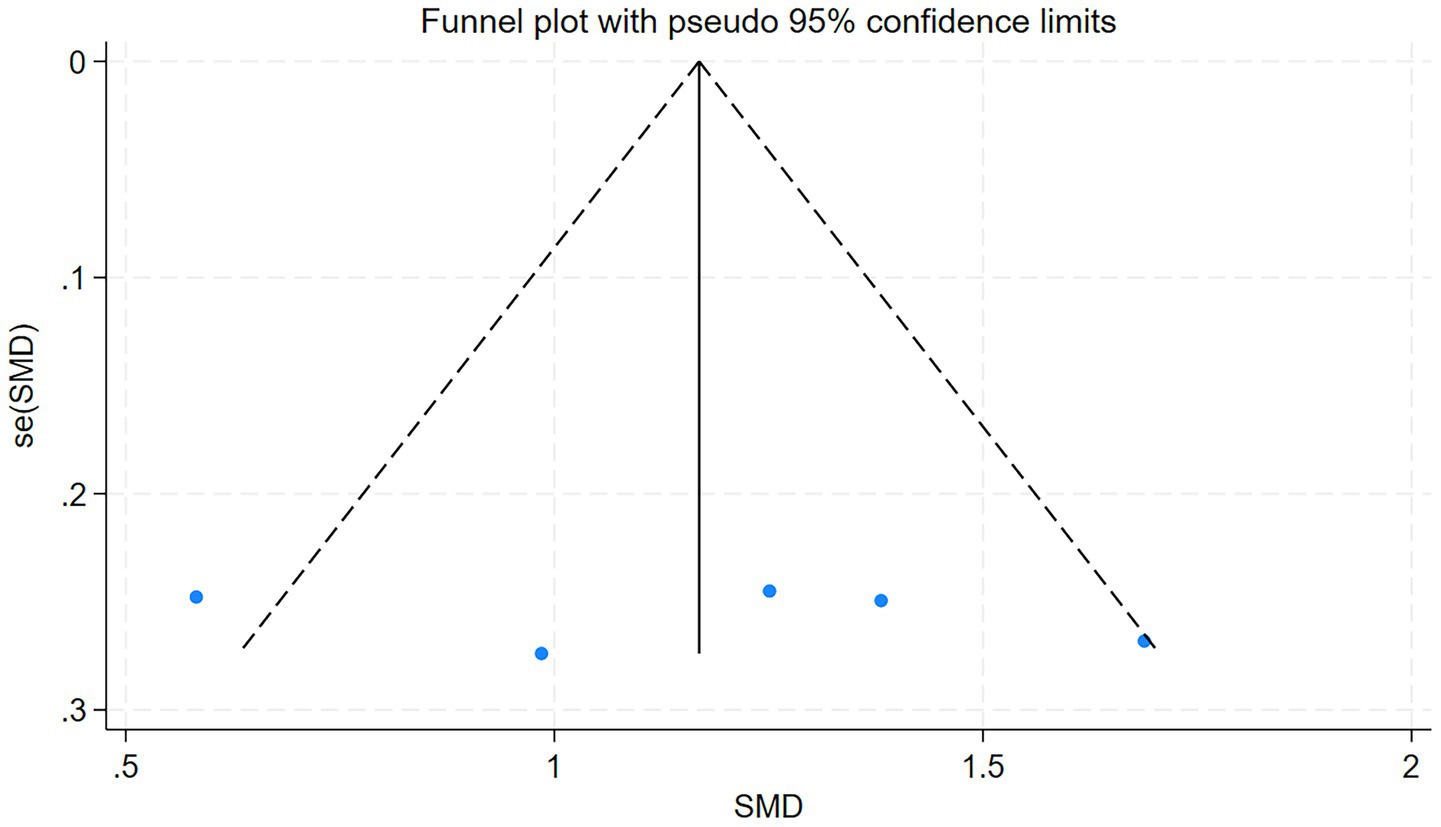
The software package provided by the Cochrane Collaboration (Review Manager 5.3) was utilized for conducting heterogeneity tests, evaluating publication bias, performing subgroup analyses, and executing sensitivity analyses. Measurement data were analyzed using mean difference (MD), expressed with a 95% confidence interval (CI), along with the I2 test to assess heterogeneity. When the statistical results indicated low heterogeneity (0% ≤ I2 < 49%), a fixed-effects model was employed; conversely, when inter-study heterogeneity was substantial (I2 ≥ 50%), a random-effects model was applied to aggregate effect sizes. Additionally, we examined the sources of heterogeneity and conducted subgroup analyses based on potential factors contributing to this variability (rehabilitation measures, duration of treatment, disease duration). Sensitivity analysis was performed as necessary to evaluate the robustness of combined effect size estimates in light of study outcomes. In cases where excessive heterogeneity precluded identification of its source, descriptive analysis was adopted instead. Funnel plots were drawn for the main outcome indicators to assess publication bias.
3 Results
3.1 Literature search
The results yielded a total of 1,680 relevant pieces of literature. Specifically, there were 17 literatures identified in PubMed, 21 literatures in the Cochrane Library, 22 literatures in Embase, 7 literatures in Web of Science, 279 literatures in CBM, 400 literatures in CNKI, 758 literatures in CSPD, and 176 literatures in CCD. Following a thorough review using NoteExpress software and manual verification for duplicates, we excluded a total of 603 duplicate entries. Additionally, we eliminated 258 literatures based on an assessment of their titles and abstracts. After reviewing the full texts, we further excluded: 786 literatures due to mismatches with study content, 19 literatures because of discrepancies regarding interventions, 2 literatures from low-quality journals, 3 literatures that lacked target parameters, and finally, 1 literature was removed due to data duplication. Ultimately, eight studies were included in the final selection process (25–32). The screening process is illustrated in Figure 1.
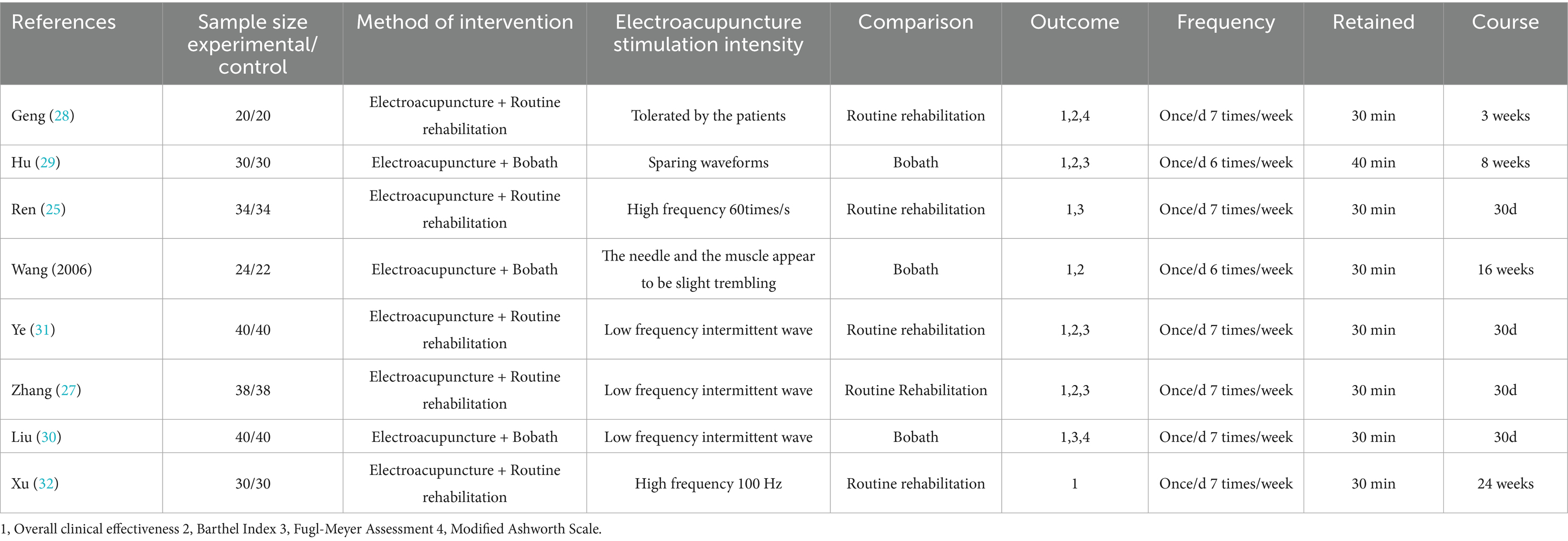
3.2 Fundamental characteristics of the included literature
We included a total of 8 randomized controlled trials, comprising 2 dissertations and 6 published papers. There are 584 cases, with 293 participants in the intervention group and 291 participants in the control group. The smallest sample size among the studies was 40 cases, while the largest was 80 cases. Six studies reported on the waveforms and frequencies associated with electroacupuncture; all eight studies documented treatment duration, which ranged from a minimum of 3 weeks to a maximum of 16 weeks. The included studies featured two types of rehabilitation therapies: five focused on conventional rehabilitation training and three utilized the Bobath technique. The fundamental characteristics of these studies are presented in Table 1.
3.3 Evaluation results of the methodological quality of the included studies
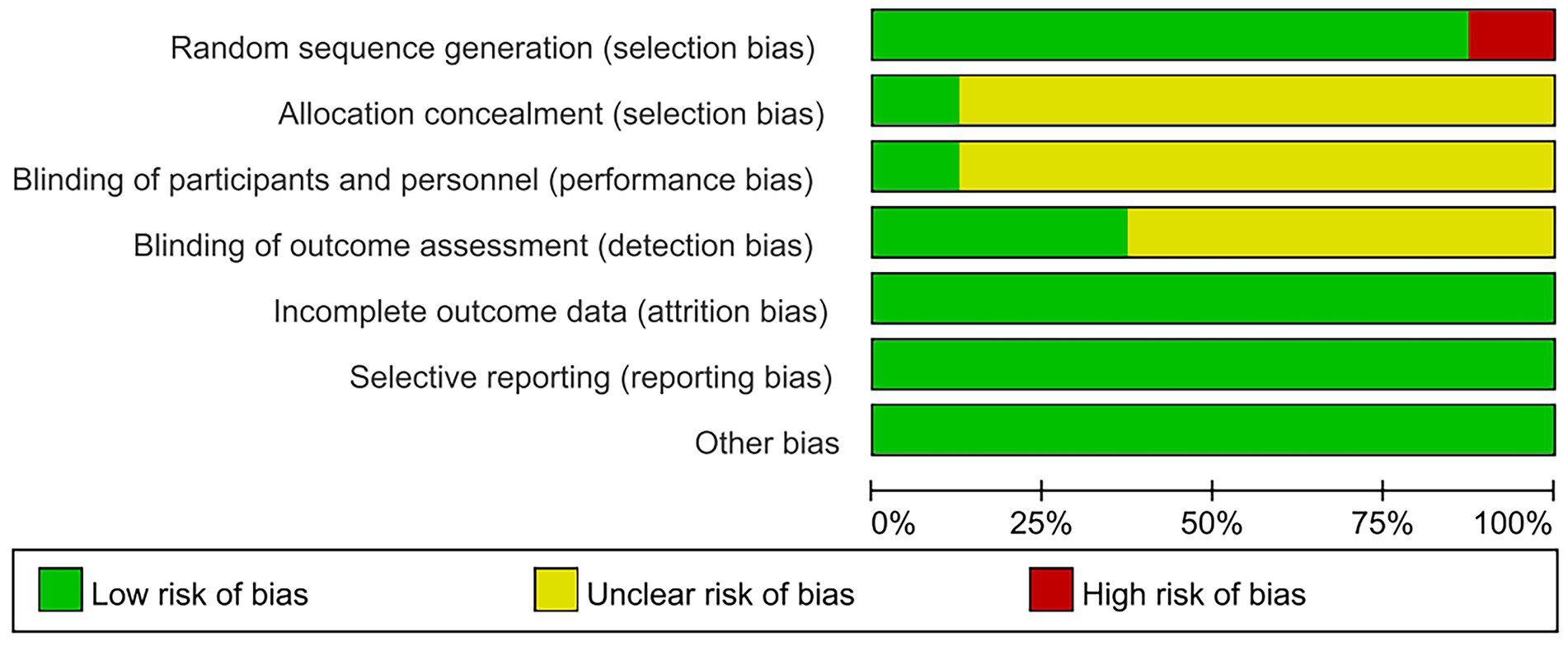
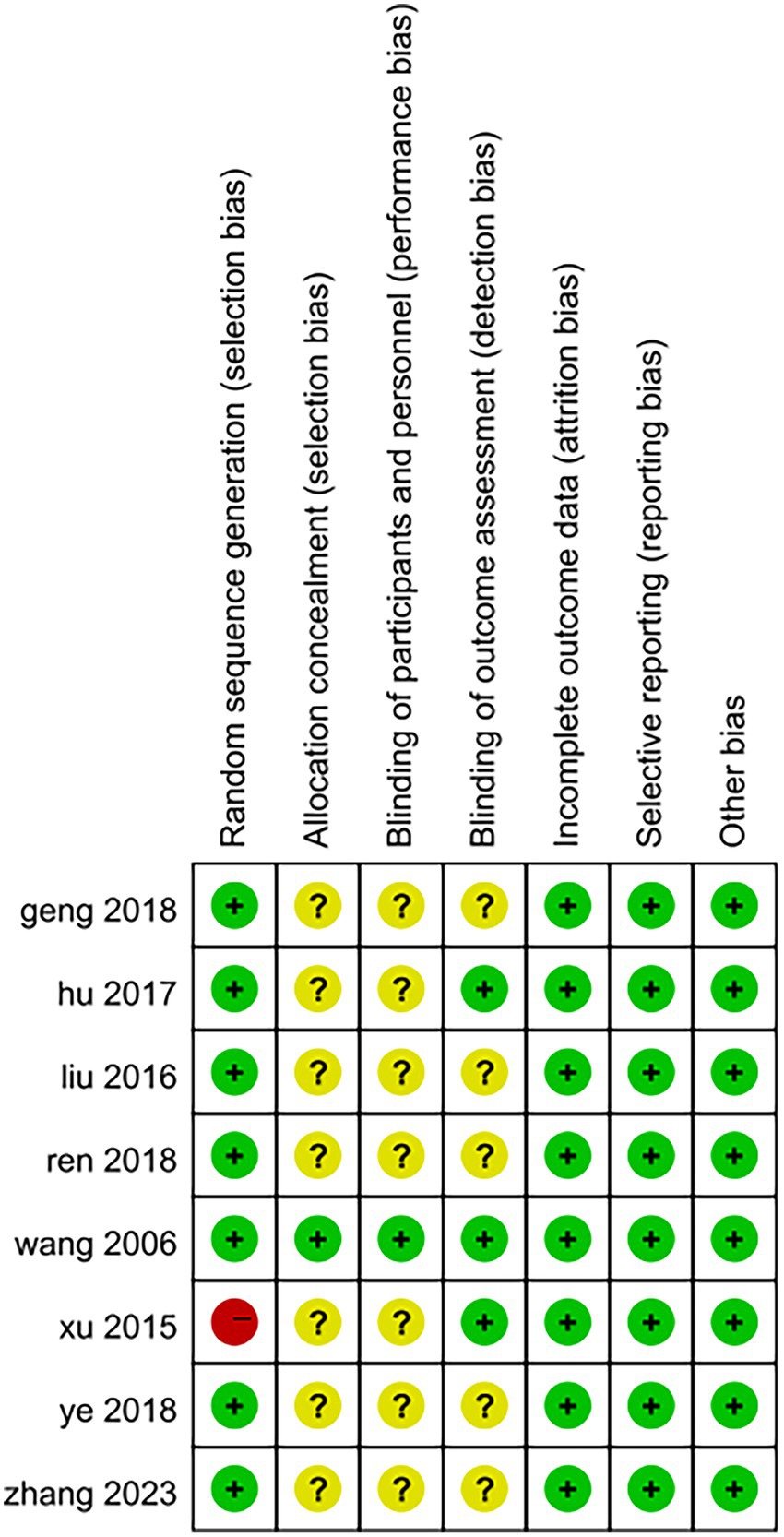
The quality of the included studies was evaluated according to Cochrane criteria: (1) Random sequence generation: three studies utilized randomized numeric tables (29–31), two employed randomized sampling (25, 27), and one study implemented randomized serial numbers (26); One study (28) merely mentioned randomization without specifying the method of allocation; however, the baseline characteristics in terms of demographic information and clinical features among the included subjects were comparable, leading to an assessment of “low risk.” Conversely, one study (32) grouped patients based on their order of hospital attendance, which constituted a semi-randomized approach and was assessed as “high risk.” (2) Allocation concealment: one study (26) reported on allocation concealment and was therefore rated as “low risk,” while seven studies did not provide this information, resulting in an assessment of “unclear.” (3) Blinding of outcome assessors: three studies (26, 29, 32) blinded outcome assessors and were classified as “low risk”; five studies did not specify whether blinding occurred for outcome assessors and were deemed “unclear.” (4) Blinding of the included population and experimental personnel: One study (26) implemented blinding for both the included population and experimental personnel, resulting in an assessment of “low risk.” In contrast, seven studies did not specify whether blinding was applied to the included population and experimental personnel; therefore, these were assessed as having an “unclear” risk. (5) Completeness of outcome data: One study (26) reported instances of dislodgement and loss to follow-up. Specifically, one patient experienced dislodgement and subsequently lost to follow-up (the exact reason remains unknown), while another patient was excluded from the results due to the use of muscarinic agents during the treatment period. Conversely, seven studies reported no occurrences of dislodgement or loss to follow-up; all were deemed complete and assessed as “low risk.” (6) Selective Reporting: The results section of all studies in the literature aligns with the methodology section. Given that there is no evidence of selective reporting, this aspect has been assessed as presenting a “low risk.” (7) Other Sources of Bias: All studies was standardized, and demographic data along with clinical characteristics of all patients were comparable at baseline. Furthermore, no other sources of bias that could potentially affect the results were identified; therefore, this risk has also been evaluated as “low.” The outcomes of the risk of bias assessment for the included studies are presented in Figures 2, 3.
3.4 Results of the meta-analysis
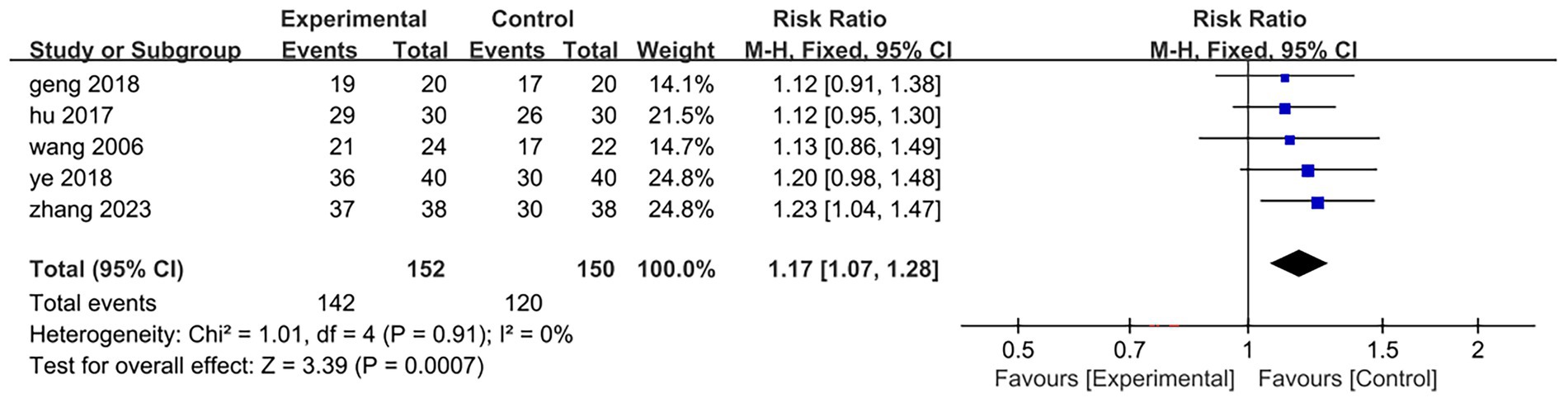
3.4.1 Overall clinical effectiveness
Five of the eight included studies (26–29, 31) reported overall clinical efficacy rates, encompassing a total sample size of 302 cases: 152 in the treatment group and 150 in the control group. The results of the heterogeneity test indicated p = 0.91 and I2 = 0%, suggesting that the heterogeneity among the literatures included in this analysis was not statistically significant. Consequently, a fixed-effect model was employed to combine effect sizes. The meta-analysis results revealed a relative risk (RR) of 1.17 with a 95% confidence interval (CI) ranging from 1.07 to 1.28, demonstrating statistical significance (Z = 3.39, p = 0.0007 < 0.001). This indicates that the overall clinical efficacy for patients in the treatment group surpassed that of those in the control group; specifically, electroacupuncture intervention targeting antagonist muscles combined with rehabilitation training proved more effective than rehabilitation training alone[RR = 1.17,95%CI(1.07,1.28), Z = 3.39, p = 0.0007 < 0.001]. Detailed results are illustrated in Figure 4.
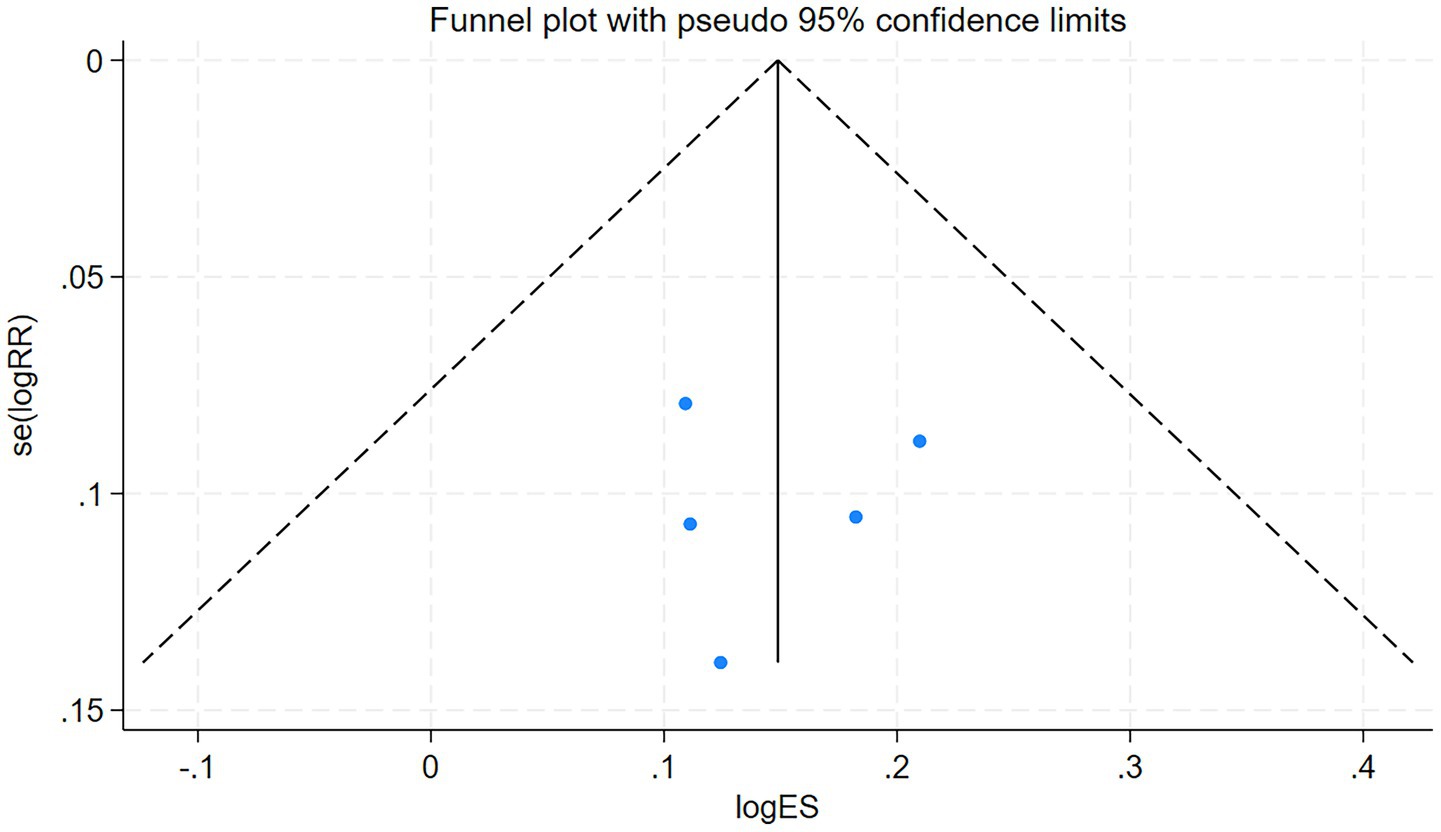
3.4.2 Assessments for bias
The total clinical efficacy rate of the included studies serves as the primary index. The funnel plot derived from the five studies included in this analysis was evaluated using Stata 18, the outcome of the test is p = 0.936 (p > 0.05). This indicates that the funnel plot is symmetrical and free from publication bias. The detailed results are presented in Figure 5.
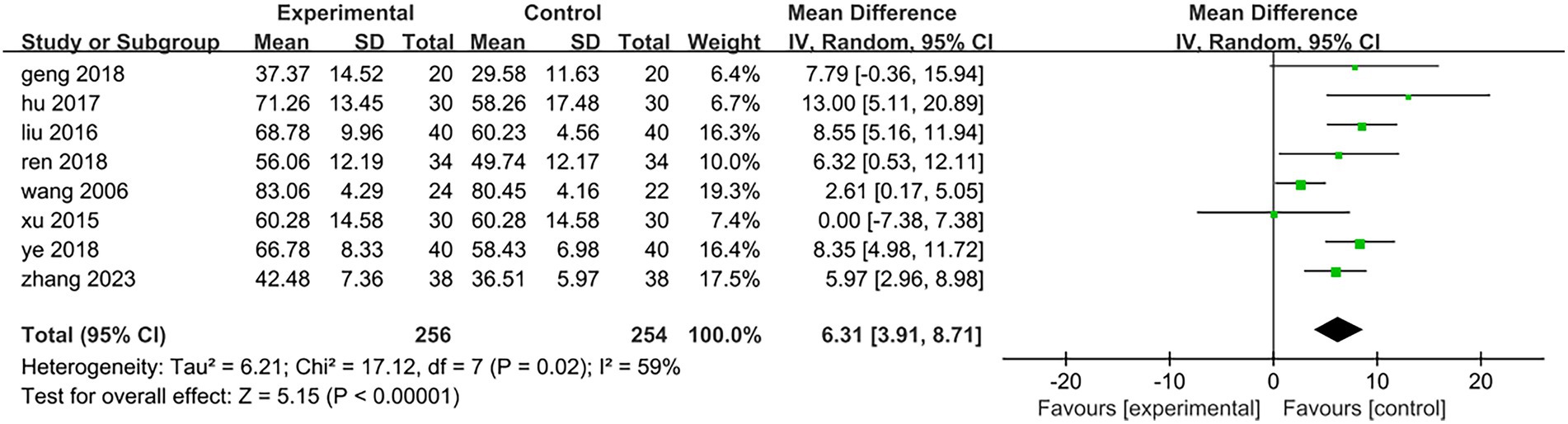
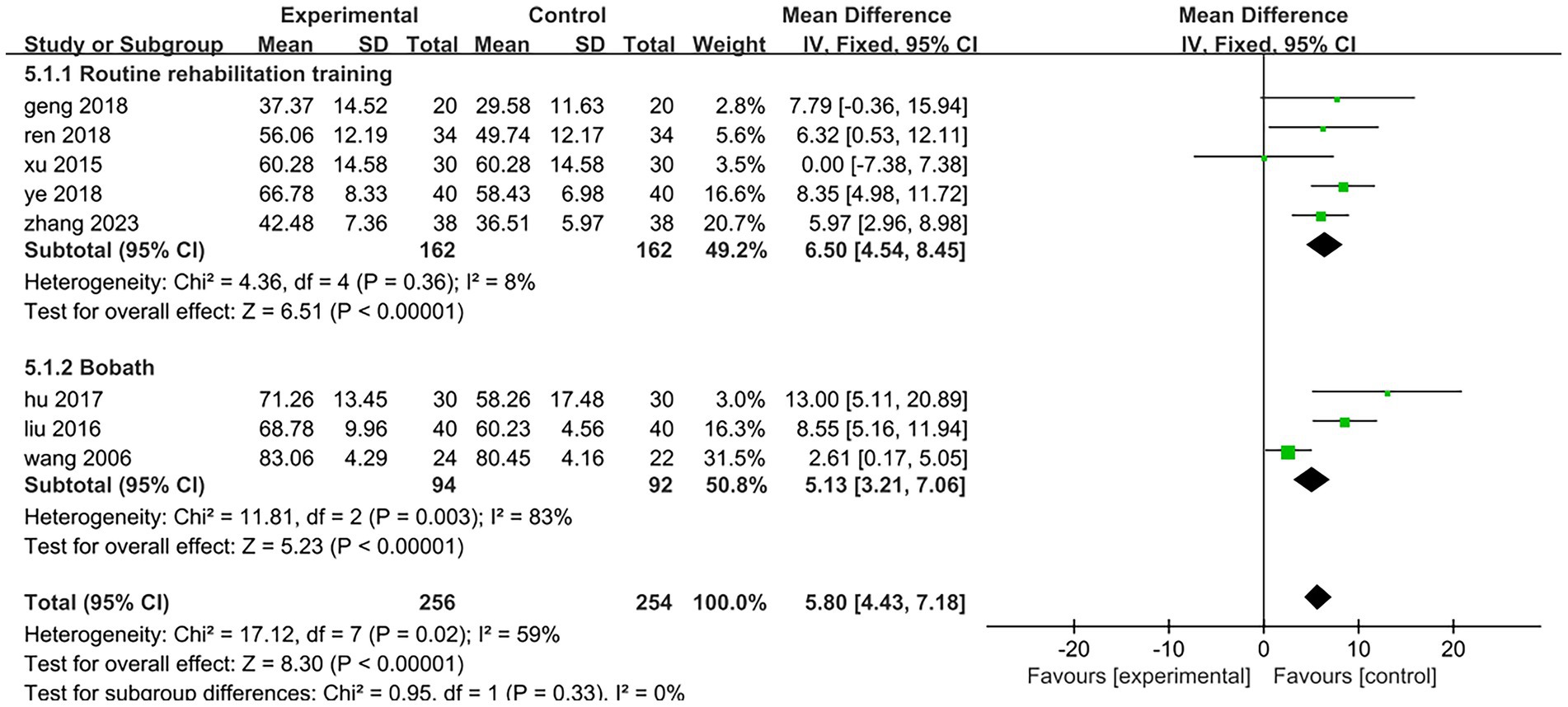
3.4.3 Barthel index
All eight included studies assessed the improvement in daily mobility between the two groups before and after treatment. Four studies utilized the Barthel Index, while the other four employed the Modified Barthel Index. The total number of participants was 510, with 256 in the treatment group and 254 in the control group. The heterogeneity test yielded a result of p = 0.02 and I2 = 59%, indicating a high degree of heterogeneity; thus, a random effects model was applied for analysis. The meta-analysis revealed a mean difference (MD) of 6.31 with a 95% confidence interval (CI) ranging from 3.91 to 8.71, which was statistically significant (Z = 5.15, p < 0.05). This suggests that electroacupuncture targeting antagonist muscles combined with rehabilitation training can effectively enhance patients’ daily living abilities [MD = 6.31,95%CI (3.91,8.71), Z = 5.15, p < 0.05], as illustrated in Figure 6. To analyze the rehabilitation interventions within subgroups, five studies (25, 27, 28, 31, 32) involving a total of 324 cases employed conventional rehabilitation training. The results of the heterogeneity test indicated p = 0.36 and I2 = 8%, suggesting low heterogeneity. Consequently, data were combined using a fixed-effect model. The meta-analysis revealed a mean difference (MD) of 6.5 with a 95% confidence interval (CI) ranging from 4.54 to 8.45, which was statistically significant (Z = 6.51, p < 0.01). These findings suggest that electroacupuncture antagonist muscles in conjunction with routine rehabilitation training significantly enhances the daily living abilities of hemiplegic patients [MD = 6.5,95%CI (4.54,8.45), Z = 6.51, p < 0.01]; specific results are illustrated in Figure 7. The rehabilitation interventions in three studies (26, 29, 30) employed the Bobath technique. The heterogeneity test yielded a result of p < 0.01 and I2 = 83%, indicating substantial heterogeneity; specific results are illustrated in Figure 7. In one study (26) (Wang, 2006, n = 46), the data recording period was extended to 16 weeks, which was longer than the treatment duration in the other two trials. Upon excluding this study from the heterogeneity analysis, we found that p = 0.31 and I2 = 3%, suggesting low levels of heterogeneity. For the remaining two studies (29, 30) (n = 140), data were combined using a fixed-effects model for meta-analysis. The results indicated a mean difference (MD) of 9.24 with a confidence interval (CI) of 95% (6.13,12.36), achieving statistical significance (Z = 5.81, p < 0.01). This suggests that within an eight-week period, electroacupuncture antagonist muscles in conjunction with the Bobath technique is effective in enhancing daily living abilities among hemiplegic patients [MD = 9.24,95%CI (6.13,12.36), Z = 5.81, p < 0.01]; detailed findings are presented in Figure 8.
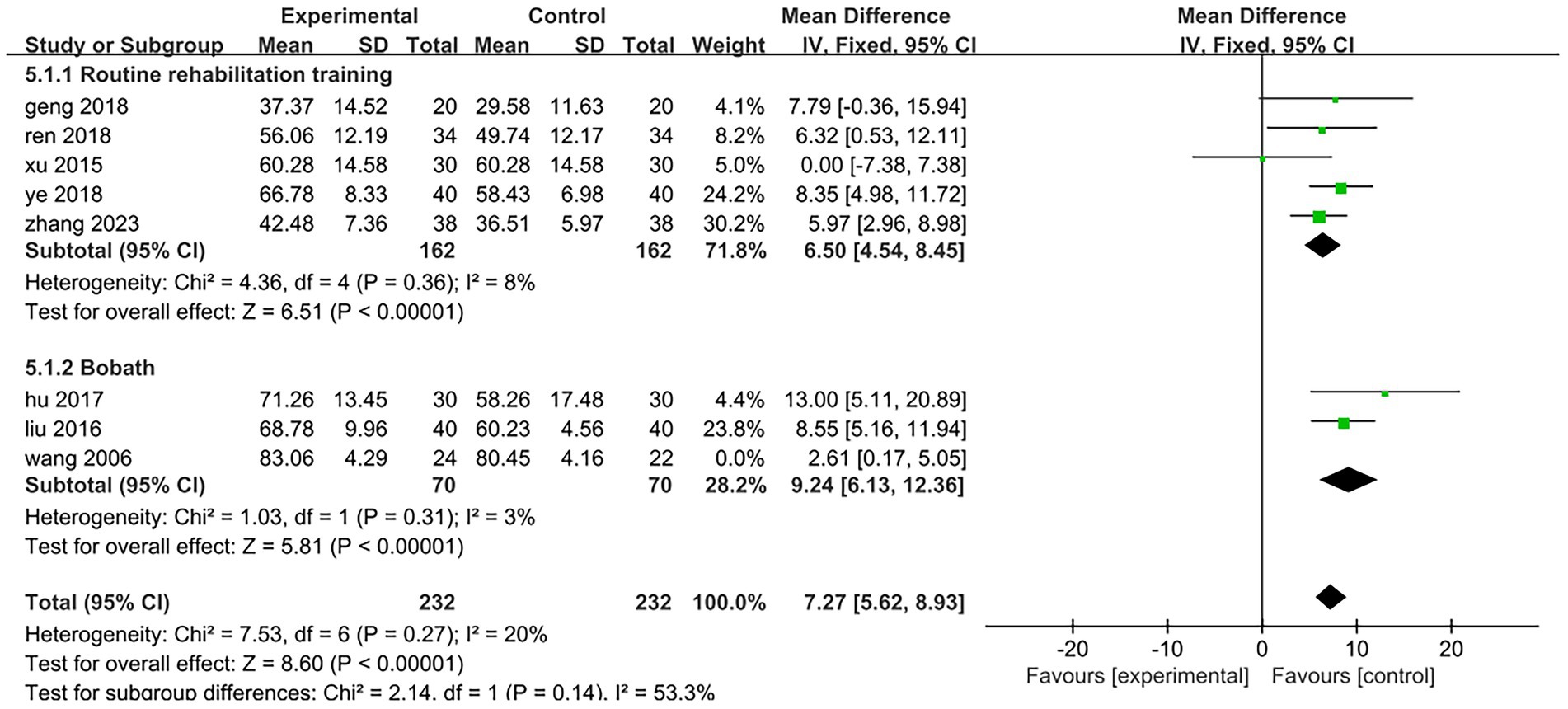
Figure 8. Forest plot of the subgroup analysis of electroacupuncture antagonistic muscles combined with Bobath technique.
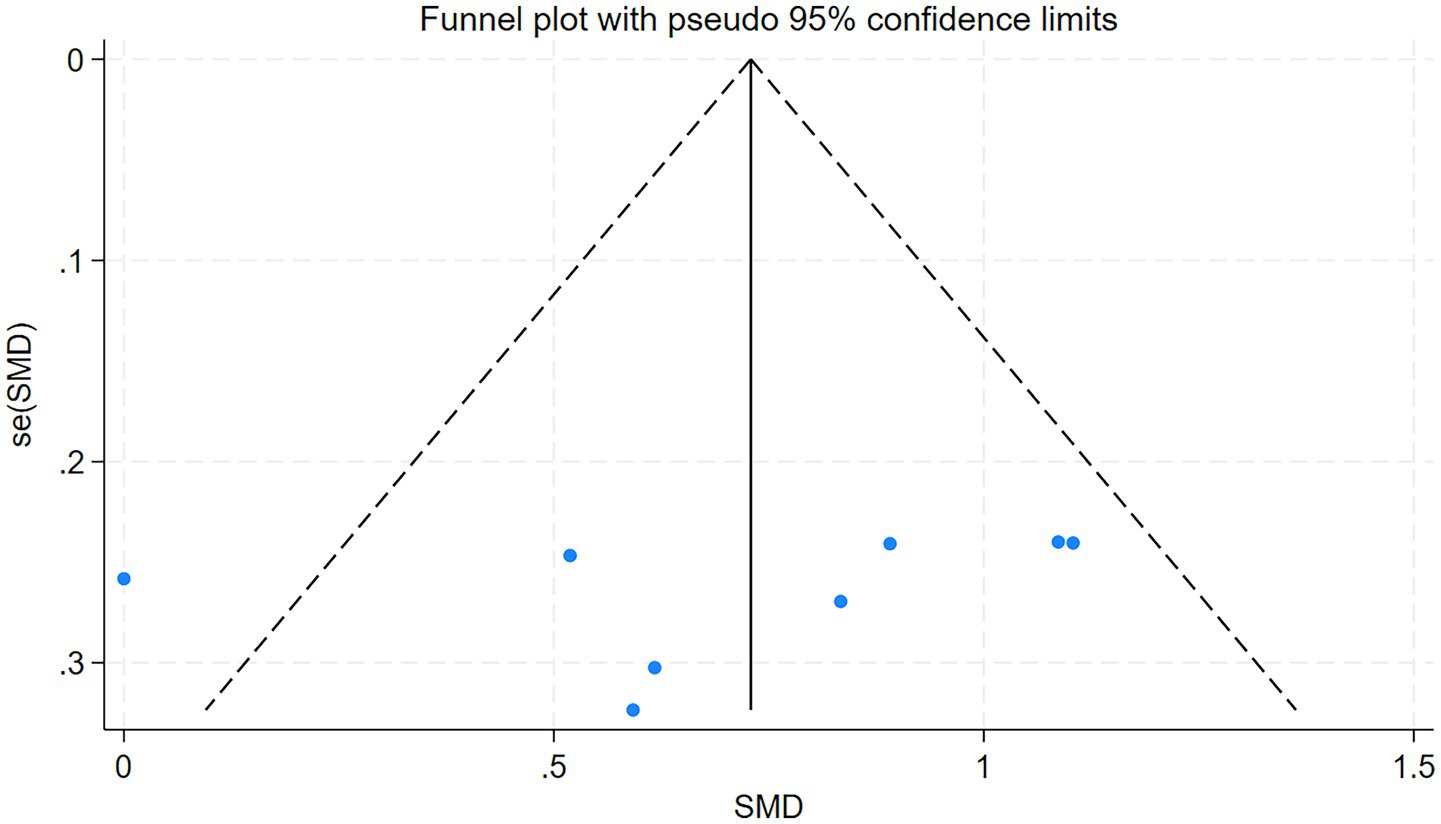
3.4.4 Assessments for bias
The funnel plot was drawn by Stata18 to test the 8 articles included in this study, p = 0.421 > 0.05, suggesting that there was no publication bias. The detailed results are presented in Figure 9.
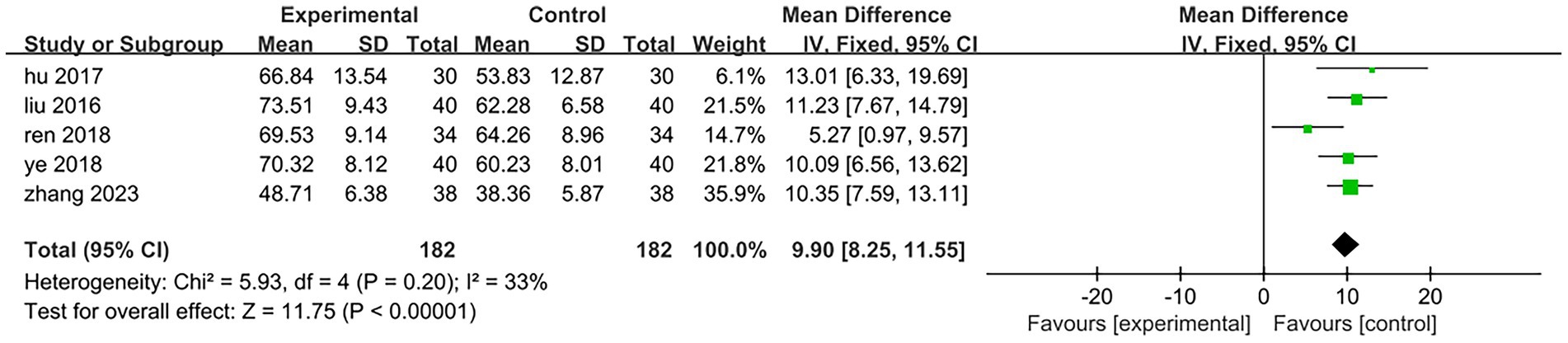
3.4.5 Fugl-Meyer assessment
Five of the eight included studies assessed motor function. Three studies (25, 27, 31) utilized the Fugl-Meyer Motor Function Rating Scale, while two studies (29, 30) employed the Simplified Fugl-Meyer Motor Function Rating Scale. The total sample size comprised 182 participants, with 91 in the treatment group and 91 in the control group. The results of the heterogeneity test indicated p = 0.2 and I2 = 33%, suggesting that there was minimal statistical heterogeneity among the included literatures; thus, a fixed effect model was applied for analysis. The meta-analysis revealed a mean difference (MD) of 9.9 with a 95% confidence interval (CI) ranging from (8.25 to 11.55), which was statistically significant (Z = 11.75, p < 0.05). This indicates that patients in the treatment group exhibited superior lower limb motor function compared to those in the control group. It can be concluded that electroacupuncture targeting antagonist muscles combined with rehabilitation training significantly enhanced patients’ lower limb motor function relative to controls [MD = 9.9,95%CI (8.25,11.55), Z = 11.75, p < 0.05]; specific results are illustrated in Figure 10. One of the studies (25) (Ren 2018, 68 cases) included patients with a longer disease duration compared to those in other studies. Additionally, the rehabilitation training implemented in this trial is a personalized rehabilitation program, resulting in low consistency regarding the content of the rehabilitation training among the included patients. After excluding this study, the results of the heterogeneity test indicated p = 0.87 and I2 = 0%, suggesting that the heterogeneity among the remaining four studies included in this analysis was statistically insignificant. The specific results are illustrated in Figure 11. In the three studies analyzed, the electroacupuncture employed consisted of low-frequency intermittent waves. The parameters for electroacupuncture interventions—including the number of sessions, retention time, and treatment duration—were consistent across all studies. The heterogeneity test yielded p = 0.89 and I2 = 0%, indicating that there was minimal statistical heterogeneity among the three papers included in this analysis. The results of the meta-analysis demonstrated a mean difference (MD) of 10.52 with a 95% confidence interval (CI) ranging from 8.66 to 12.37, which is statistically significant (Z = 11.11, p < 0.05). This suggests that low-frequency intermittent wave electroacupuncture combined with rehabilitation training can effectively enhance lower limb motor function in hemiplegic patients on a daily basis [MD = 10.52,95%CI (8.66,12.37), Z = 11.11, p < 0.05]. Specific results are illustrated in Figure 12.
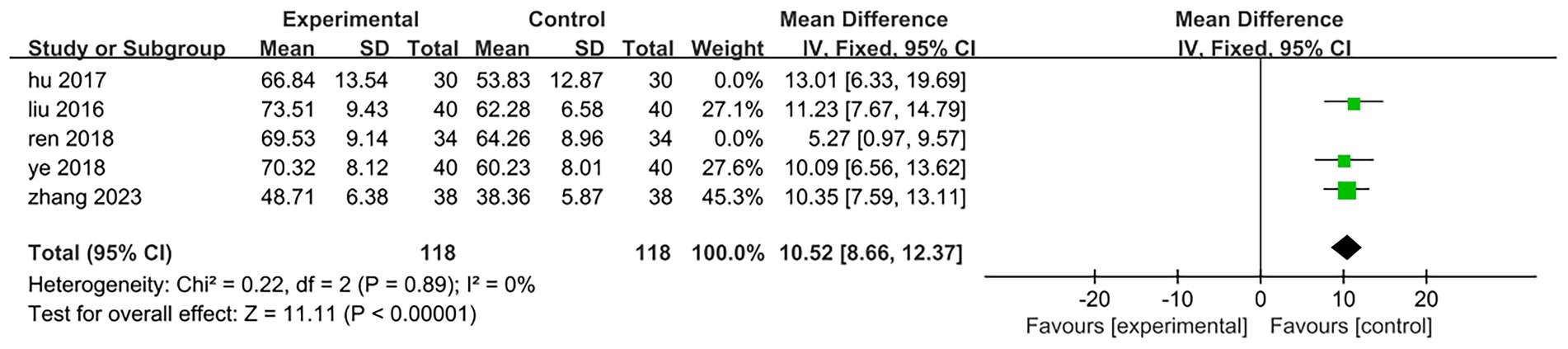
Figure 12. Forest plot of the low-frequency intermittent wave electroacupuncture antagonistic muscle combined with rehabilitation training to improve lower limb motor function.
3.4.6 Assessments for bias
The funnel plot was drawn by Stata18 to test the 5 articles included in this study, p = 0.674 > 0.05, suggesting that there was no publication bias. The detailed results are presented in Figure 13.
3.4.7 Modified Ashworth scale
There are two studies (28, 30) among the eight included in this review that assessed the improvement in limb spasticity before and after treatment in both groups. The total sample size comprised 120 cases, with 60 participants in the treatment group and 60 in the control group. The results of the heterogeneity test indicated p = 0.36 and I2 = 0%, suggesting that there was no statistically significant heterogeneity among the included studies; thus, a fixed-effect model was employed for analysis. The meta-analysis revealed a mean difference (MD) of −0.52 with a 95% confidence interval (CI) ranging from −0.91 to −0.13, which was statistically significant (Z = 2.6, p = 0.009 < 0.05). This finding indicates that electroacupuncture combined with antagonist muscle rehabilitation training can effectively improve limb spasticity in patients with hemiplegia [MD = –0.52,95%CI(−0.91,–0.13), Z = 2.6, p < 0.05]. The specific results are illustrated in Figure 14.
3.4.8 Security analysis
None of the eight studies reported any adverse effects, and the incidence of such effects is found to be low. One study (26) did mention instances of dislodgement and missed appointments; specifically, one patient experienced dislodgement and subsequently lost to follow-up (the exact cause remains unknown), while another patient was removed from the study due to the muscle relaxant during treatment.
4 Discussion
There remain areas for improvement in this study: (1) We have observed that low-frequency intermittent waveforms can effectively alleviate spasticity; however, the sample size of our study is limited. Future research should involve multi-center and large-sample studies to explore the differences in efficacy among various waveforms and frequencies in the treatment of hemiplegia. This will help confirm the optimal clinical conditions for different waveform frequencies in relation to Brunnstrom stage, as well as clarify protocols for spasticity staging corresponding to specific waveforms, frequencies, and intensities of electroacupuncture. (2) The literatures included in this study discusses electroacupuncture treatment following the sensation of deqi; however, only one study (29) provided the description of the performance of deqi. Furthermore, none of the studies elaborated on the specific techniques employed to achieve acupuncture deqi, as the experience of deqi primarily relies on patients’ subjective perceptions. There is considerable variability in how different patients perceive deqi (33), In future research, it is essential to standardize various factors related to needling operations, including frequency, duration, direction, and depth. Additionally, integrating multimodal perception fusion technologies and incorporating visual parameters such as needle movement amplitude alongside tactile characteristics like finger pressure (34) will help mitigate the impact of subjective variables associated with manipulation on test outcomes. (3) The primary outcome indicators included in this study exhibit a high degree of subjectivity (35), which results in a lack of standardization in the evaluation of clinical efficacy. Additionally, there is a scarcity of original data available for homogeneity analysis. In future research, objective indicators such as the touchdown area and maximum pressure peak across various regions of the plantar surface can be measured to assess the coordinated function of foot internal and external rotation, as well as lower limb skeletal joints. This approach will enable a scientific and objective evaluation of patients’ stride frequency, stride length, and support time. (4) The patients included in this study were all of the Asians, which is characterized by certain geographical limitations. With the gradual global acceptance of acupuncture and moxibustion (36), it is essential to conduct relevant randomized controlled trials involving different races in the future. Furthermore, the therapeutic effects of electroacupuncture antagonistic muscles combined with rehabilitation training should be extended to a broader patient population worldwide. Additionally, establishing a database for regional spastic paralysis across various regions will provide valuable data support for clinical treatment and scientific research. (5) The findings of this study indicate that electroacupuncture interventions antagonistic muscles can significantly alleviate spasm symptoms in patients. However, electroacupuncture can be applied to antagonistic muscles through various approaches, including the selection of starting and ending points of these muscles, tendon nodes, muscle movement points, and corresponding acupoints based on the specific antagonistic muscles involved (37). Nevertheless, the differences in efficacy and treatment mechanisms among these diverse intervention methods remain unclear. (6) This meta-analysis demonstrates that electroacupuncture combined with Bobath technique results in better outcomes than electroacupuncture combined with the conventional rehabilitation training. However, it is important to note that the sample size of patients included in this study is limited. Future research should focus on multi-center large-sample randomized controlled trials to further investigate the differences in efficacy of electroacupuncture combined with different rehabilitation training approaches to provide high-quality evidence. (7) Due to variations in the random allocation methods employed in the included studies, confounding factors such as demographic and disease characteristics may emerge. Furthermore, considering the difficulty of implementing a double-blind design in clinical studies of acupuncture, making it difficult to maintain blinding for participants, experimenters, and outcome assessors. This situation can lead to potential assessment bias from outcome evaluators. Additionally, it is difficult to quantify and exclude the influence of acupuncture placebo effects on participants and researchers. The limited sample sizes further restrict the statistical power of study findings, thereby increasing the likelihood that results may be affected by chance or outliers. All included studies were conducted at single centers involving Asian participants; thus, they do not adequately represent patients with spastic hemiplegia from other regions, which limits the generalizability of these findings. Moreover, the short duration of interventions is insufficient for effectively evaluating both long-term efficacy and safety of electroacupuncture combined with rehabilitation training for spastic hemiplegia post-stroke—this includes potential delayed adverse reactions. Future research should be designed as rigorous multicenter randomized controlled trials with large sample sizes. Stratified randomization methods should be utilized to group participants based on age, gender, and disease severity prior to their random assignment into intervention and control groups; this will help ensure balanced baseline characteristics such as age and disease severity. It is essential to select objective outcome measures that are resistant to interference while employing ANCOVA for correcting baseline values during statistical analyses. Additionally, extending both treatment duration and follow-up periods appropriately is necessary to elucidate the long-term efficacy and safety of electroacupuncture combined with rehabilitation training in treating spastic hemiplegia after stroke.
5 Suggestions for future development direction
(1) Due to physical dysfunction, social role change and other reasons, hemiplegic patients will face the pressure of economic burden (38), family burden and self-cognitive burden during the rehabilitation period, resulting in decreased happiness and increased loneliness (39). Effective emotional support and psychological counseling (such as Swanson care theory) can effectively alleviate depression (40), foster positive life experiences, enhance quality of life, and facilitate disease recovery. Research indicates that acupuncture may inhibit neuronal excitotoxicity by reducing glutamate (Glu) expression in the cerebral cortex while promoting gamma-aminobutyric acid (GABA) expression. This regulation of the ‘GABA-Glu’ balance can improve muscle spasms. The disruption of Glu/GABA homeostasis across various brain regions is recognized as a contributing factor to severe depressive disorders (41) and plays a role in the mechanisms underlying antidepressant efficacy (42). Therefore, in the future, it should carry out high-quality randomized controlled trials to explore the effect of electroacupuncture antagonistic muscle on patients with spastic hemiplegia and depression by improving ‘GABA-Glu ‘imbalance. (2) At present, the mechanism of electroacupuncture antagonistic muscles in the treatment of spastic hemiplegia predominantly is a single-mechanism approach. It is essential to investigate the effects of various parameters associated with antagonistic muscles electroacupuncture on different biological indices within the human body. This exploration should integrate techniques such as acupuncture manipulation quantification (43), modern systems biology, and mechanical biology. For instance, studies could focus on synaptic structure reconstruction (44), neuronal growth factor (NGF) (45), brain-derived neurotrophic factor (BDNF) (46), F wave and H reflex assessments related to spinal anterior horn motor neuron excitability during cross-inhibition, pro-vascular endothelial growth factor (VEGF) (47), inflammatory factors including TNF, IL-6, and NF-κB signaling pathways. Additionally, it is important to examine biological characteristics such as spastic muscle fiber thickness, muscle bundle length, pinnate angle, and the proportion of type I/II muscle fibers post-acupuncture (48, 49), By integrating insights from the central nervous system, peripheral nervous system, blood circulation system, skeletal muscular system, and neuro-immune-endocrine system, we can elucidate the theoretical connotation underlying acupuncture’s local-central-target organ-peripheral correlation effect. (3) Spastic hemiplegia can be categorized into various forms, including hand dysfunction, upper limb spastic hemiplegia, lower limb spastic hemiplegia, and foot drop. Currently, there is no systematic treatment protocol for selecting wave patterns and parameters of antagonistic muscles in different regions of the hands, feet, upper limbs, and lower limbs. In the future, the multi-center large-sample randomized controlled trials should be carried out to determine the guidance scheme for the selection of parameters such as wave mode and frequency of antagonistic muscle muscles in different parts of the hand, foot, upper and lower limbs.
6 Conclusion
The findings of this meta-analysis indicate that the integration of electroacupuncture treatment with antagonist muscle rehabilitation training can effectively alleviate muscle spasms, reduce muscle tension, and enhance lower limb motor function as well as daily living abilities. Although the improvement in various indicators was more pronounced in the treatment group compared to the control group, confounding factors, selection bias, and inherent limitations hinder a definitive interpretation of the safety and efficacy of electroacupuncture combined with rehabilitation training for spastic hemiplegia following stroke. This study offers preliminary evidence regarding the potential safety and efficacy of electroacupuncture in conjunction with antagonist muscle rehabilitation training for patients experiencing spastic hemiplegia post-stroke. Consequently, the findings of this study should be regarded as preliminary and exploratory; further validation through large-scale, long-term randomized controlled trials is essential.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author/s.
Author contributions
JL: Writing – original draft. XM: Writing – original draft. YH: Writing – original draft. HJ: Writing – original draft. JYZ: Writing – original draft. JYS: Writing – original draft. JSZ: Writing – original draft. MZ: Writing – original draft. FC: Writing – original draft. SD: Writing – original draft. JWS: Writing – review & editing. ZM: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by The National Key R&D Program of China (No. 2018YFC1706001, 2010CB530506), Open Project of National Clinical Research Center for Chinese Medicine Acupuncture and Moxibustion (Grant No. NCRCOP2023001, NCRCOP2023003, NO. NCRCOP2024001), Tianjin Science and Technology Plan Project (24ZYJDSY00260, 24ZYJDSY00270), National Natural Science Foundation of China (NO. 82374560), Science and Technology Project of Haihe Laboratory of Modern Chinese Medicine(24HHZYSS00012), The Science & Technology Development Fund of Tianjin Education Commission for Higher Education (2022KJ170) and the First Teaching Hospital of Tianjin University of Traditional Chinese Medicine, Exploration and Innovation Project (No. XB2024002).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1634845/full#supplementary-material
References
1. Kuriakose, D, and Xiao, Z. Pathophysiology and treatment of stroke: present status and future perspectives. Int J Mol Sci. (2020) 21:7609. doi: 10.3390/ijms21207609
2. Watkins, DA. Policy priorities for preventing stroke-related mortality and disability worldwide. Lancet Neurol. (2023) 22:1096–8. doi: 10.1016/S1474-4422(23)00387-3
3. Baylan, S, Griffiths, S, Grant, N, Broomfield, NM, Evans, JJ, and Gardani, M. Incidence and prevalence of post-stroke insomnia: a systematic review and meta-analysis. Sleep Med Rev. (2020) 49:101222. doi: 10.1016/j.smrv.2019.101222
4. Pan, L, Jin, J, Huang, R, Wang, W, and Chen, Q. Application of transcranial Doppler in prognosis assessment of nerve function in patients with acute cerebral infarction after intracranial mechanical thrombectomy. Zhonghua Wei Zhong Bing Ji Jiu Yi Xue. (2020) 32:835–9. doi: 10.3760/cma.j.cn121430-20200410-00281
5. Gerard, EF, and R, MJSJ. Poststroke Spasticity Management. (2012) 43:3132–6. doi: 10.1161/strokeaha.111.639831
6. Sainz-Pelayo, MP, Albu, S, Murillo, N, and Benito-Penalva, J. Spasticity in neurological pathologies. An update on the pathophysiological mechanisms, advances in diagnosis and treatment. Rev Neurol. (2020) 70:453–60. doi: 10.33588/rn.7012.2019474
7. Schinwelski, MJ, Sitek, EJ, Waz, P, and Slawek, JW. Prevalence and predictors of post-stroke spasticity and its impact on daily living and quality of life. Neurol Neurochir Pol. (2019) 53:449–57. doi: 10.5603/PJNNS.a2019.0067
8. Nam, KE, Lim, SH, Kim, JS, Hong, BY, Jung, HY, Lee, JK, et al. When does spasticity in the upper limb develop after a first stroke? A nationwide observational study on 861 stroke patients. J Clin Neurosci. (2019) 66:144–8. doi: 10.1016/j.jocn.2019.04.034
9. Ewing, AC, Li, Y, Chen, X, Gallis, J, Su, K, Turner, EL, et al. Stroke and activity limitation in Chinese adults 65 years or older. Disabil Health J. (2023) 16:101452. doi: 10.1016/j.dhjo.2023.101452
10. Reinkensmeyer, DJ, Farrens, AJ, and Kamper, DG. Facilitating limb movement after stroke. Nat Med. (2023) 29:535–6. doi: 10.1038/s41591-023-02233-7
11. Collaborators, GBDS. Global, regional, and national burden of stroke, 1990-2016: a systematic analysis for the global burden of disease study 2016. Lancet Neurol. (2019) 18:439–58. doi: 10.1016/S1474-4422(19)30034-1
12. Brown, DA, Kautz, SA, and Dairaghi, CA. Muscle activity adapts to anti-gravity posture during pedalling in persons with post-stroke hemiplegia. Brain. (1997) 120:825–37. doi: 10.1093/brain/120.5.825
13. Schillebeeckx, F, De Groef, A, De Beukelaer, N, Desloovere, K, Verheyden, G, and Peers, K. Muscle and tendon properties of the spastic lower leg after stroke defined by ultrasonography: a systematic review. Eur J Phys Rehabil Med. (2021) 57:495–510. doi: 10.23736/s1973-9087.20.06462-x
14. Renming, LM, Kywe, AA, Weiting, L, Maryam, Z, and Shapour, JJJIM. Does acupuncture at motor-related acupoints affect corticospinal excitability? A systematic review and meta-analysis. J Integrat Med. (2025) 23:113–25. doi: 10.1016/j.joim.2025.02.004
15. Fan, W, Kuang, X, Hu, J, Chen, X, Yi, W, Lu, L, et al. Acupuncture therapy for poststroke spastic hemiplegia: a systematic review and meta-analysis of randomized controlled trials. Complement Ther Clin Pract. (2020) 40:101176. doi: 10.1016/j.ctcp.2020.101176
16. Jiang, H, Zhang, C, Lin, M, Yin, Y, Deng, S, Liu, W, et al. Deciphering the mechanistic impact of acupuncture on the neurovascular unit in acute ischemic stroke: insights from basic research in a narrative review. Ageing Res Rev. (2024) 101:102536. doi: 10.1016/j.arr.2024.102536
17. Zhang, J, Zhu, L, and Tang, Q. Electroacupuncture with rehabilitation training for limb spasticity reduction in post-stroke patients: a systematic review and meta-analysis. Top Stroke Rehabil. (2021) 28:340–61. doi: 10.1080/10749357.2020.1812938
18. Huang, L, Yi, L, Huang, H, Zhan, S, Chen, R, and Yue, Z. Corticospinal tract: a new hope for the treatment of post-stroke spasticity. Acta Neurol Belg. (2024) 124:25–36. doi: 10.1007/s13760-023-02377-w
19. Zhang, J, Lu, C, Wu, X, Nie, D, and Yu, H. Neuroplasticity of acupuncture for stroke: an evidence-based review of MRI. Neural Plast. (2021) 2021:1–14. doi: 10.1155/2021/2662585
20. Zhang, K, Jiang, M, and Fang, Y. The Drama of Wallerian degeneration: the cast, crew, and script. Annu Rev Genet. (2021) 55:93–113. doi: 10.1146/annurev-genet-071819-103917
21. Qian, Y, Xie, B, and Yan, X. Clinical observation on the effect of acupuncture on corticospinal tract and motor function in patients with ischemic stroke. Zhong Guo Zhong Yi Yao Xian Dai Yuan Cheng Jiao Yu. (2024) 22:133–6.
22. Liu, CH, Liao, WL, Su, SY, Chen, WL, and Hsieh, CL. Electroacupuncture in the Contralesional hemisphere improves neurological function involving GABA in ischemia-reperfusion injury rats. Evid Based Complement Alternat Med. (2021) 2021:5564494. doi: 10.1155/2021/5564494
23. Prager, EM, Bergstrom, HC, Wynn, GH, and Braga, MF. The basolateral amygdala gamma-aminobutyric acidergic system in health and disease. J Neurosci Res. (2016) 94:548–67. doi: 10.1002/jnr.23690
24. Aze, OD, Ojardias, E, Akplogan, B, Giraux, P, and Calmels, P. Structural and pathophysiological muscle changes up to one year after post-stroke hemiplegia: a systematic review. Eur J Phys Rehabil Med. (2023) 59:474–87. doi: 10.23736/S1973-9087.23.07844-9
25. Ren, H. Clinical study of high frequency electroacupuncture combined with rehabilitation training in the treatment of upper limb muscle tension enhancement after stroke Liaoning University of Traditional Chinese Medicine (2018).
26. Wang, Q. Clinical study on complex facilitation technique of electro-acupuncturing antagonistic muscle Acupoint in treating Extremital spasm caused by cerebral infarction hemiplegia Chengdu University of Traditional Chinese Medicine (2006).
27. Zhang, Y. Observation on the effect of Electroacupuncture at antagonistic muscle Acupoints combined with rehabilitation training in the treatment of stroke hemiplegic spasm. China Practical Medicine. (2023) 18:153–5.
28. Geng, H, and Cheng, C. Clinical observation on Electroacupuncture antagonistic muscle combined with rehabilitation therapy for post-stroke muscle tension enhancement. Clin J Chin Med. (2018) 10:70–2.
29. Hu, D, Zhao, M, and Li, X. Clinical study on Electroacupuncture combined with rehabilitation training in the treatment of hemiplegic spasticity after stroke. J Clin Acupunct Moxibust. (2017) 33:26–9.
30. Liu, M, Li, Z, and Ma, H. Clinical evaluation of Electroacupuncture antagonistic muscle Acupoints combined with rehabilitation training in the treatment of stroke hemiplegic spasm. J Clin Acupunct Moxibust. (2016) 32:8–10.
31. Ye, J, Wu, D, and Jin, Y. Clinical observation of Electroacupuncture stimulating antagonistic muscle side Acupoints combined with rehabilitation training in the treatment of patients with increased muscle tension after stroke. J Emergen Trad Chin Med. (2018) 27:2200–2.
32. Xu, H., Clinical efficacy of electroacupuncture combined with rehabilitation training in the treatment of upper limb muscle spasticity after apoplexy. World Chin Med, (2015). (0): p. 974–975
33. Yeung, A, and Mischoulon, D. Effects of Electroacupuncture for depression-related insomnia. JAMA Netw Open. (2022) 5:e2220573. doi: 10.1001/jamanetworkopen.2022.20573
34. Su, C, Wang, C, Gou, S, Chen, J, Tang, W, and Liu, C. An action recognition method for manual acupuncture techniques using a tactile array finger cot. Comput Biol Med. (2022) 148:105827. doi: 10.1016/j.compbiomed.2022.105827
35. Aloraini, SM, Gaverth, J, Yeung, E, and MacKay-Lyons, M. Assessment of spasticity after stroke using clinical measures: a systematic review. Disabil Rehabil. (2015) 37:2313–23. doi: 10.3109/09638288.2015.1014933
36. Liu, B, Chen, B, Guo, Y, and Tian, L. Acupuncture – a national heritage of China to the world: international clinical research advances from the past decade. (2021) 1:65–73. doi: 10.1097/hm9.0000000000000017
37. Qian, X, Ma, LX, Sun, TY, Mu, JD, Zhang, Z, Yu, WY, et al. Practical value and thought on "co-regulation of body and mind" in treatment of post-stroke spasticity with acupuncture. Zhongguo Zhen Jiu. (2022) 42:803–6. doi: 10.13703/j.0255-2930.20210718-k0003
38. Hotter, B, Padberg, I, Liebenau, A, Knispel, P, Heel, S, Steube, D, et al. Identifying unmet needs in long-term stroke care using in-depth assessment and the post-stroke checklist - the managing aftercare for stroke (MAS-I) study. Eur Stroke J. (2018) 3:237–45. doi: 10.1177/2396987318771174
39. Yang, X, Fengyi, W, Yi, C, Lin, Q, Yang, L, Xize, L, et al. Effects of robot-assisted upper limb training combined with functional electrical stimulation in stroke patients: study protocol for a randomized controlled trial. Trials. (2024) 25:355. doi: 10.1186/s13063-024-08199-2
40. Zafari, M, Sadeghipour Roudsari, M, Yarmohammadi, S, Jahangirimehr, A, and Marashi, T. Investigating the relationship between spiritual well-being, resilience, and depression: a cross-sectional study of the elderly. Psychogeriatrics. (2023) 23:442–9. doi: 10.1111/psyg.12952
41. Fogaca, MV, and Duman, RS. Cortical GABAergic dysfunction in stress and depression: new insights for therapeutic interventions. Front Cell Neurosci. (2019) 13:87. doi: 10.3389/fncel.2019.00087
42. Marwaha, S, Palmer, E, Suppes, T, Cons, E, Young, AH, and Upthegrove, R. Novel and emerging treatments for major depression. Lancet. (2023) 401:141–53. doi: 10.1016/S0140-6736(22)02080-3
43. Shi, X. Study of the relationship between acupuncture dose and effect. Acupuncture and Herbal Medicine. (2021) 1:3–9. doi: 10.1097/hm9.0000000000000009
44. Zheng, Y, Qin, Z, Tsoi, B, Shen, J, and Zhang, ZJ. Electroacupuncture on trigeminal nerve-innervated Acupoints ameliorates Poststroke cognitive impairment in rats with middle cerebral artery occlusion: involvement of neuroprotection and synaptic plasticity. Neural Plast. (2020) 2020:1–13. doi: 10.1155/2020/8818328
45. Pang, Q, Zhang, H, Chen, Z, Wu, Y, Bai, M, Liu, Y, et al. Role of caveolin-1/vascular endothelial growth factor pathway in basic fibroblast growth factor-induced angiogenesis and neurogenesis after treadmill training following focal cerebral ischemia in rats. Brain Res. (2017) 1663:9–19. doi: 10.1016/j.brainres.2017.03.012
46. Chen, S, Wang, H, Xu, H, Zhang, Y, and Sun, H. Electroacupuncture promotes axonal regrowth by attenuating the myelin-associated inhibitors-induced RhoA/ROCK pathway in cerebral ischemia/reperfusion rats. Brain Res. (2020) 1748:147075. doi: 10.1016/j.brainres.2020.147075
47. Geiseler, SJ, and Morland, C. The Janus face of VEGF in stroke. Int J Mol Sci. (2018) 19:1362. doi: 10.3390/ijms19051362
48. Son, J, Rymer, WZ, and Lee, SSM. Limited fascicle shortening and fascicle rotation may be associated with impaired voluntary force-generating capacity in pennate muscles of chronic stroke survivors. Clin Biomech (Bristol). (2020) 75:105007. doi: 10.1016/j.clinbiomech.2020.105007
49. Battaglia, M, Cosenza, L, Scotti, L, Bertoni, M, Polverelli, M, Loro, A, et al. Triceps Surae muscle characteristics in spastic hemiparetic stroke survivors treated with botulinum toxin type a: clinical implications from ultrasonographic evaluation. Toxins (Basel). (2021) 13:889. doi: 10.3390/toxins13120889
Keywords: spastic hemiplegia, antagonistic muscles, rehabilitation training, systematic review, meta-analysis, electroacupuncture
Citation: Liu J, Meng X, He Y, Jiang H, Zhang J, Shi J, Zhang J, Zhang M, Cai F, Deng S, Shi J and Meng Z (2025) Clinical efficacy of electroacupuncture antagonistic muscles combined with rehabilitation training in the treatment of spastic hemiplegia after stroke: a systematic review and meta-analysis of randomized controlled trials. Front. Neurol. 16:1634845. doi: 10.3389/fneur.2025.1634845
Edited by:
António Moreira, Instituto Politécnico de Santarém-ESDRM, PortugalReviewed by:
Xun Luo, Kerry Rehabilitation Medicine Research Institute, ChinaQinwei Fu, McMaster University, Canada
Copyright © 2025 Liu, Meng, He, Jiang, Zhang, Shi, Zhang, Zhang, Cai, Deng, Shi and Meng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jiangwei Shi, YWN1c3RvbmVAMTYzLmNvbQ==; Zhihong Meng, cHJvZm1lbmd6aGlob25nQDE2My5jb20=
†These authors have contributed equally to this work and share first authorship
 Jingyue Liu
Jingyue Liu Xiang Meng
Xiang Meng Yana He
Yana He Hailun Jiang
Hailun Jiang Jieying Zhang
Jieying Zhang Jinyuan Shi
Jinyuan Shi Jingshu Zhang
Jingshu Zhang Menglong Zhang
Menglong Zhang Fei Cai
Fei Cai Shizhe Deng
Shizhe Deng Jiangwei Shi
Jiangwei Shi Zhihong Meng
Zhihong Meng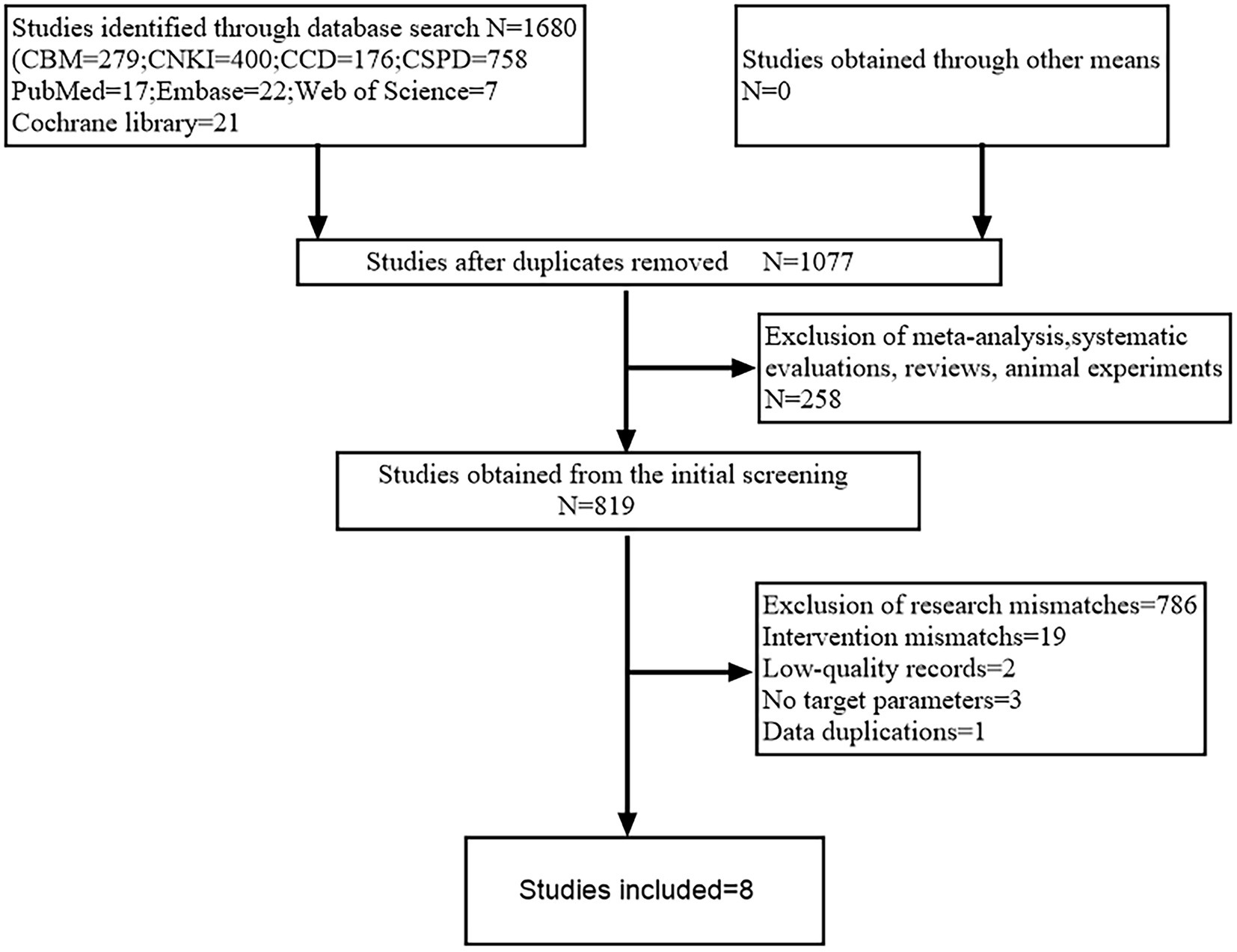
![Forest plot comparing experimental and control groups across five studies, showing mean differences with 95% confidence intervals. Studies favor the experimental group, with a total mean difference of 10.70 [8.91, 12.48]. Heterogeneity is low (Chi² = 0.72, df = 3, I² = 0%).](https://www.frontiersin.org/files/Articles/1634845/fneur-16-1634845-HTML/image_m/fneur-16-1634845-g011.jpg)
![Forest plot showing mean differences between experimental and control groups for two studies: Geng 2018 and Liu 2016. Geng 2018 shows a mean difference of -0.83, and Liu 2016 shows -0.41. The overall effect has a mean difference of -0.52 with a 95% confidence interval of [-0.91, -0.13]. Heterogeneity analysis shows Chi² = 0.85, df = 1, p = 0.36, and I² = 0%. The test for overall effect has Z = 2.60, p = 0.009.](https://www.frontiersin.org/files/Articles/1634845/fneur-16-1634845-HTML/image_m/fneur-16-1634845-g014.jpg)