Abstract
Lateral semicircular canal peripheral positional vertigo (LC-PPV) is a common condition, even though accurate determination of the affected side remains a diagnostic challenge that is crucial for effective treatment. The aim of this study is to provide a systematic diagnostic approach for lateralization in LC-PPV, based on analysis of endolymphatic flow dynamics elicited by the Bow and Lean test and supine roll test.
Introduction
The sensor for angular head acceleration in the yaw plane is the lateral semicircular canal (LC), which is inclined approximately 30 degrees relative to the horizontal plane. According to Ewald’s second law, ampullopetal endolymphatic flow (toward the ampulla) is excitatory for this canal, whereas ampullofugal flow (away from the ampulla) produces an inhibitory stimulus.
The LC is the second most frequently affected semicircular canal in peripheral positional vertigo (PPV) (1). This variant is characterized by horizontal nystagmus that beats either toward the ground (geotropic) or toward the ceiling (apogeotropic) during positional testing. The initial location of otoliths may be free-floating in the non-ampullary arm of the LC (geotropic variant) or in the ampullary arm or attached to the cupula (apogeotropic variant) (2).
The primary diagnostic test for LC-PPV is the Supine Roll Test (SRT), in which the head is rotated 90 degrees to each side while the patient is on supine position. The direction and intensity of the induced nystagmus are critical for identifying the affected side. In this test, nystagmus typically beats toward the undermost ear in the geotropic variant and toward the uppermost ear in the apogeotropic variant. Additionally, nystagmus is more intense when the head is turned toward the affected side in geotropic LC-PPV and toward the unaffected side in the apogeotropic variant. However, distinguishing subtle differences in nystagmus intensity during the SRT can sometimes be challenging, possibly due to variations in otolith volume or distribution within the canal (3, 4).
The Minimum Stimulus Strategy, first described by Asprella-Libonatti (5), is a stepwise approach based on nystagmus patterns elicited during a sequence of positional tests. This method aims to achieve successful treatment outcomes in the first session while minimizing vertigo symptoms. The Bow and Lean Test is performed with the patient in the seated position, with the head flexed forward and extended backward (6). The direction and intensity of nystagmus observed during this test may serve as key indicators for determining the affected side (7). If there is a horizontal nystagmus during the Bow and Lean Test, we may proceed with the Seated Supine Positioning Test (SSPT) succeeded by the SRT, given the clinical suspicion of LC-PPV. On the other hand, we may continue with the Dix Hallpike test (8) (Figure 1).
Figure 1

Diagnostic algorithm based on variant identification (geotropic vs. apogeotropic) combined with Bow and Lean test findings. BLT, Bow and Lean test; DHT, Dix Hallpike test; Ny, nystagmus; SRT, supine roll test; SSPT, seated supine positioning test.
The objective of this study is to provide practical guidance for diagnosing and identifying the affected side in LC-PPV, based on an analysis of endolymphatic flow dynamics induced by the Bow and Lean Test and the SRT.
Case descriptions
Case 01
Male, 70 years old. Bedside examination at the ENT office with a video-Frenzel-goggle did not exhibited a spontaneous nystagmus with or without visual fixation. Bow test with a left beating nystagmus, Lean test with a right beat nystagmus and SRT with an apogeotropic nystagmus. We were unable to identify the difference in intensity of the nystagmus in the SRT. Therefore, we can assume that the otoliths were located in the ampullary arm of the right LC, because there was an apogeotropic nystagmus in the SRT (ampullary arm) and a right beating nystagmus in the lean test (Right LC) (Supplementary Video 1).
Case 02
Female, 74 years old. Bedside examination at the ENT office with a video-Frenzel-goggle did not exhibited a spontaneous nystagmus with or without visual fixation. Bow test with a right beating nystagmus, Lean test with a left beat nystagmus and SRT with a geotropic nystagmus. We were unable to identify the difference in intensity of the nystagmus in the SRT. Therefore, we can assume that the otoliths were located in the non-ampullary arm of the right LC, because there was a geotropic nystagmus in the SRT (non-ampullary arm) and a right beating nystagmus in the bow test (Right LC) (Supplementary Video 2).
Diagnosis assessment
The diagnosis and determination of the affected side in LC-PPV requires a structured sequence of positional testing. The evaluation begins with the Bow and Lean test performed by sequentially flexing and extending the patient’s head, while seated.
In the geotropic variant (otoliths located in the non-ampullary arm of the LC), the Bow test induces ampullopetal movement of otolithic debris under the gravitational force, generating excitatory endolymphatic flow and consequent nystagmus beating toward the affected side. Conversely, in the apogeotropic variant, the Lean test produces ampullopetal movement, resulting in excitatory flow and nystagmus directed toward the affected side (9, 10) (Figure 2).
Figure 2
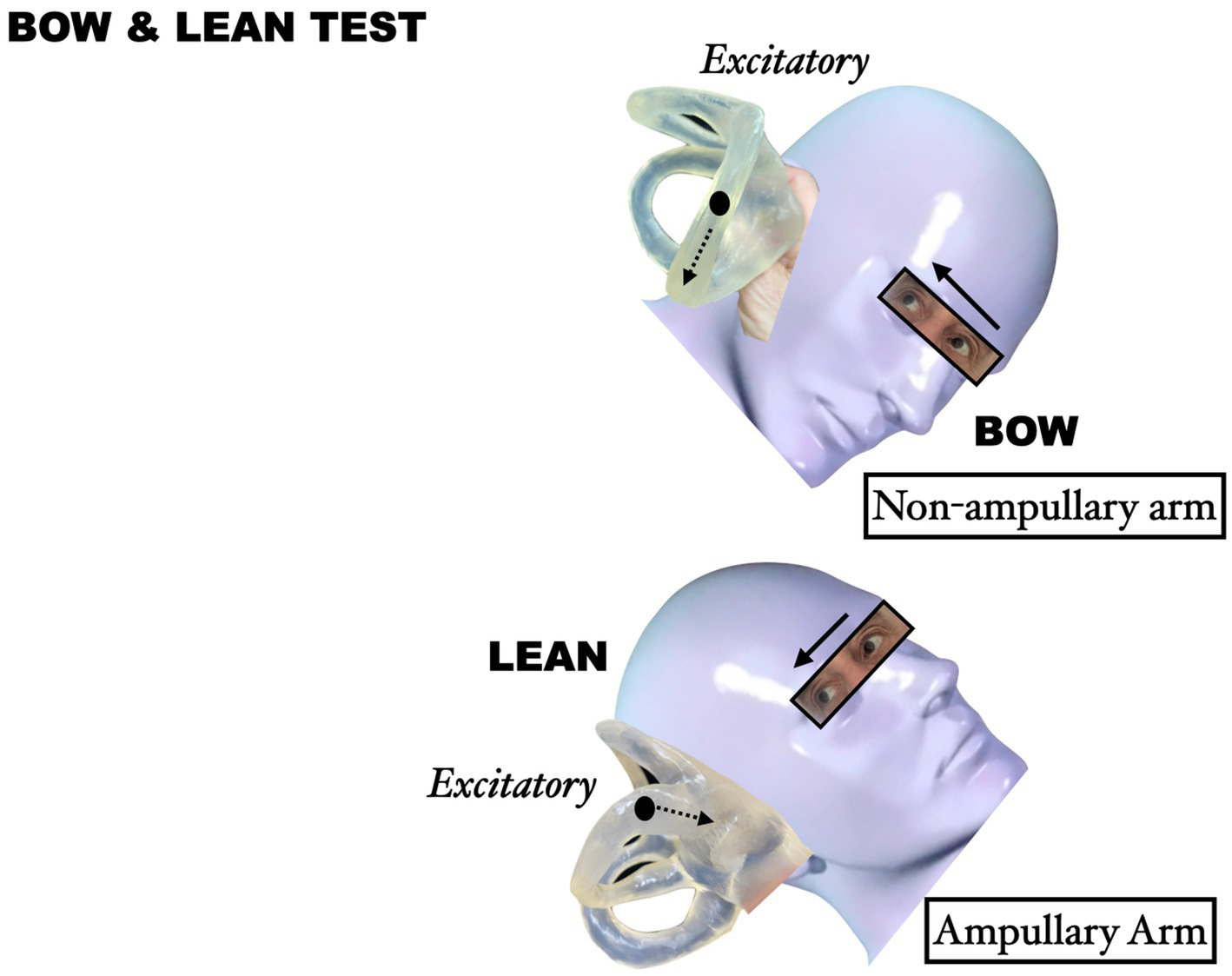
Endolymphatic flow during the Bow and Lean test.
The evaluation continues with the Seated Supine Positioning Test (SSPT), which represents the natural transition between seated and supine positions required for SRT execution. While SSPT alone cannot differentiate between both variants, it provides valuable lateralization clues through characteristic nystagmus patterns, as it elicits nystagmus beating toward the unaffected side in geotropic variant and toward the affected side in apogeotropic variant. Importantly, since patients must be moved to supine position for SRT regardless, SSPT adds negligible additional stimulation while yielding useful diagnostic data.
The diagnostic sequence culminates with the SRT, where 90° head rotations produce direction-changing nystagmus: geotropic variants demonstrate nystagmus beating toward the undermost ear, while apogeotropic variants show nystagmus beating toward the uppermost ear.
Given the occasional difficulty in discerning nystagmus intensity differences during SRT (6, 7), we propose a diagnostic algorithm based on variant identification (geotropic vs. apogeotropic) combined with Bow and Lean test findings. In geotropic LC-PPV, the affected side corresponds to the direction of Bow test-evoked nystagmus. Conversely, in apogeotropic variant, the affected side matches the direction of Lean test-induced nystagmus (7). For instance, right geotropic LC-PPV (non-ampullary arm) manifests as right-beating nystagmus during the Bow test (excitatory stimulus) and geotropic nystagmus in SRT, as demonstrated in Case 02.
Discussion
While less frequently encountered than posterior canal PPV, LC-PPV presents unique diagnostic and therapeutic challenges. Accurate identification of the affected side is crucial for successful treatment outcomes (9, 10). Although the supine roll test (SRT) remains the primary diagnostic tool for LC-PPV, reliance solely on nystagmus intensity differences during SRT may prove diagnostically challenging in certain cases (6, 7).
Complementary diagnostic tools, including pseudo-spontaneous nystagmus evaluation, Bow and Lean test, Seated Supine positioning test (SSPT), and walk-rotate-walk test, have been proposed as valuable adjuncts for lateralization (5, 6, 10, 11). Notably, clinical studies demonstrate that bowing and/or leaning-induced nystagmus can be observed in 70–90% of LC-PPV cases, providing critical diagnostic information when SRT findings are not clear (6, 12).
Based on our understanding of endolymphatic flow dynamics during positional testing, we propose a systematic diagnostic approach incorporating the following principles:
The Bow and Lean test represents a minimally invasive, easily performed diagnostic test.
Excitatory stimuli consistently produce nystagmus beating toward the affected side.
The Bow test elicits an excitatory stimulus in geotropic LC-PPV (7).
The Lean test generates an excitatory stimulus in apogeotropic LC-PPV (7).
These physiological principles support a diagnostic algorithm where SRT determined variant classification (geotropic or apogeotropic) combined with Bow and Lean test nystagmus direction provides reliable information to identify the affected side in LC-PPV. While many LC-PPV cases can be accurately diagnosed through SRT evaluation alone, Bow and Lean test findings serve as valuable confirmatory evidence, enhancing diagnostic certainty.
Conclusion
The Minimum Stimulus Strategy facilitates the application of neurophysiological principles for diagnosing LC-PPV, as it provides multiple concordant data points for lateralization, while maintains patient comfort by minimizing provocative positional tests. Our findings demonstrate that combining variant identification through the Supine Roll Test (geotropic or apogeotropic) with nystagmus direction analysis during the Bow and Lean Test provides a reliable method for determining the affected side in LC-PPV cases, particularly when SRT nystagmus intensity differences are ambiguous.
Statements
Author contributions
FZ: Writing – original draft, Writing – review & editing. BR: Writing – original draft, Writing – review & editing. MC-B: Writing – original draft, Writing – review & editing. RC: Writing – original draft, Writing – review & editing. JM: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1643458/full#supplementary-material
SUPPLEMENTARY VIDEO 1Right apogeotropic LC-PPV.
SUPPLEMENTARY VIDEO 2Right geotropic LC-PPV.
References
1.
Bhandari R Tech B Bhandari A . Prevalence of horizontal canal variant in 3,975 patients with benign paroxysmal positional vertigo: a cross-sectional study. Neurol Clin Pract. (2023) 13:e200191. doi: 10.1212/CPJ.0000000000200191
2.
Li Y Yang X . Design and analysis of HSC-BPPV diagnostic maneuver based on virtual simulation. Front Neurol. (2023) 14:1132343. doi: 10.3389/fneur.2023.1132343
3.
Rajguru SM Ifediba MA Rabbitt RD . Biomechanics of horizontal canal benign paroxysmal positional vertigo. J Vestib Res. (2005) 15:203–14. doi: 10.3233/VES-2005-15404
4.
Rajguru SM Ifediba MA Rabbitt RD . Three-dimensional biomechanical model of benign paroxysmal positional vertigo. Ann Biomed Eng. (2004) 32:831–46. doi: 10.1023/B:ABME.0000030259.41143.30
5.
Asprella Libonati G . Diagnostic and treatment strategy of lateral semicircular canal canalolithiasis. Acta Otorhinolaryngol Ital. (2005) 25:277–83.
6.
Choung YH Shin YR Kahng H Park K Choi SJ . ‘Bow and lean test’ to determine the affected ear of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. (2006) 116:1776–81. doi: 10.1097/01.mlg.0000231291.44818.be
7.
Marcelli V . Nystagmus intensity and direction in bow and lean test: an aid to diagnosis of lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital. (2016) 36:520–6. doi: 10.14639/0392-100X-795
8.
Ramos BF Cal R Mangabeira Albernaz PL Zuma e Maia F . Vertical “pseudospontaneous” nystagmus in a patient with posterior canal BPPV: case report. Acta Oto-laryngologica Case Reports. (2021) 6:116–119. doi: 10.1080/23772484.2021.2008800
9.
Zuma e Maia F Ramos BF Cal R Brock CM Mangabeira Albernaz PL Strupp M . Management of lateral semicircular canal benign paroxysmal positional vertigo. Front Neurol. (2020) 11:1040. doi: 10.3389/fneur.2020.01040
10.
Asprella-Libonati G . Pseudo-spontaneous nystagmus: a new sign to diagnose the affected side in lateral semicircular canal benign paroxysmal positional vertigo. Acta Otorhinolaryngol Ital. (2008) 28:73–8.
11.
Rahko T Kotti V . Walk-rotate-walk test identifies patients responding to Lempert’s maneuver, with benign paroxysmal positional vertigo of the horizontal canal. Eur Arch Otorrinolaringol. (2001) 258:112–5. doi: 10.1007/s004050100329
12.
Lee JB Han DH Choi SJ Park K Park HY Sohn IK et al . Efficacy of the “bow and lean test” for the management of horizontal canal benign paroxysmal positional vertigo. Laryngoscope. (2010) 120:2339–46. doi: 10.1002/lary.21117
Summary
Keywords
benign paroxysmal positional vertigo, lateral canal BPPV, horizontal canal BPPV, apogeotropic nystagmus, geotropic nystagmus
Citation
Zuma E Maia FC, Ramos BF, Castillo-Bustamante M, Cal RV and Madrigal J (2025) Lateral canal peripheral positional vertigo diagnosis: a neurophysiological approach. Front. Neurol. 16:1643458. doi: 10.3389/fneur.2025.1643458
Received
09 June 2025
Accepted
15 July 2025
Published
25 July 2025
Volume
16 - 2025
Edited by
Andrés Soto-Varela, Complejo Hospitalario Universitario de Santiago, Spain
Reviewed by
Juan Carlos Amor-Dorado, Hospital Can Misses, Spain
Updates
Copyright
© 2025 Zuma E Maia, Ramos, Castillo-Bustamante, Cal and Madrigal.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Bernardo Faria Ramos, bernardoframos@gmail.com
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.