Abstract
Objective:
To analyze the temporal changes in ischemic stroke incidence and prevalence and their correlations with age, period, and birth cohort from 1990 to 2021 in Finland, Korea, Singapore and China, and to predict the trends of incidence and number of cases in 2036.
Methods:
The data from the Global Burden of Disease (GBD) 2021 database were used. The effects of age, period and birth cohort on the incidence of ischemic stroke were sorted out by age-period-cohort (APC) modeling. Bayesian Age-Period-Cohort (BAPC) modeling was used to predict the incidence rates of different sex and age groups in 2036.
Results:
The global all-age disability-adjusted life year (DALY) rate of ischemic stroke decreased by 34.90% between 1990 and 2021, with the highest disease burden in China, especially in males. Whereas, Singapore, South Korea, and Finland were lower than the global average. The APC model showed that the incidence increased significantly with the increase of age. Compared with China, the age of high incidence in Singapore, South Korea and Finland has moved forward. In terms of period effect, there were fluctuations across the countries. Although China is less affected by the cyclical effect, the overall burden is increased. In the cohort effect, the incidence of Singapore, Finland, and Korea showed a “U-shape,” while China's prevalence continued to decline. Projections for the next 15 years indicate that the incidence rates in Finland, Korea, and Singapore will remain low, whereas China may continue to increase. By 2036, it could reach nearly 200 per 100,000 people, and the uncertainty is greater, so it needs to focus on prevention and control.
Conclusion:
The burden of disease for ischemic stroke has been declining in all four countries from 1990 to 2021, but it has been rising in recent years and is expected to continue to rise over the next 15 years.
Introduction
Ischemic stroke represents a major global public health challenge, characterized by high incidence, recurrence rates, disability, mortality and substantial economic costs (1). According to the Global Burden of Disease (GBD) 2019 study, ischemic stroke accounted for approximately 6.55 million deaths worldwide (2), establishing it as a leading cause of death and long-term disability, surpassed only by cardiovascular diseases and cancer (3). Although recent decades have seen advancements in prevention, diagnosis, and treatment, which led to declining mortality in some regions (4, 5), the overall burden of ischemic stroke continues to rise globally. This rise is largely driven by lifestyle changes and aging populations, particularly in developing countries (6, 7).
A thorough understanding of the evolving epidemiology of ischemic stroke is essential for facilitating early risk screening, acute treatment, sustained rehabilitation, and effective management of risk factors. It also supports policymakers in developing targeted strategies to alleviate pressure on healthcare systems.
Significant regional variations exist in the burden of ischemic stroke, reflecting differences in healthcare access, socioeconomic conditions, and geographic factors (2, 8, 9). For instance, countries such as Finland, South Korea, Singapore, and China differ considerably in economic development and health infrastructure, contributing to divergent trends in the prevalence and incidence of ischemic stroke (10–13). These differences underscore the need for country-specific analyses of disease burden.
Using data from GBD 2021, this study examines the temporal trends and geographical distribution of ischemic stroke in Finland, South Korea, Singapore, and China. In addition, we employ the Bayesian Age-Period-Cohort (BAPC) model to forecast incidence rates in these countries over the next 15 years. Our aim is to elucidate regional disparities in disease burden and contributing factors, thereby informing the development of tailored prevention and management strategies for ischemic stroke.
Methods
Data sources
This study is based on a secondary analysis of the GBD2021 dataset from the Global Health Data Exchange (GHDx) in Global Burden of Disease (GBD) covering 371 disease burdens in 204 countries and territories around the world from 1990 to 2021. The data was extracted on the fifteenth of November 2024. Over the subsequent month, the data underwent analysis and processing, culminating in the completion of the relevant charts.
The Global Burden of Disease (GBD) 2021 provides the distribution of diseases and injuries and their burdens over time, age, sex, and geography, while continuously updated databases allow for precise assessment of risk factor exposures, associations with health risks, and shares in the burden of disease (14). However, traditional epidemiological methods do not accurately analyze the correlates contributing to the disparities, whereas the BAPC model is based on an integrated nested Laplace approximation, which approximates the marginal posterior distributions and avoids the mixing and convergence problems introduced by the Markov chain Monte Carlo sampling technique traditionally used for Bayesian methods. The excellent predictive performance of the model has been verified. Therefore, the present study provides an in-depth analysis through the age-period-cohort (APC) model to clarify that these factors influence the epidemiology of ischemic stroke (15).
Case definitions and data collection
In GBD 2021, ischemic stroke was defined using the International Classification of Diseases (ICD), including the 9th (ICD-9: 433-435.9, 437.0-437.2, 437.4-437.9) and 10th (ICD-10: G45-G46.8, I63-I63.9, I65-I66.9, I67.2- I67.848, I69.3-I69.4) (16). This study collected the data on the number of disability-adjusted life years (DALYs), all-age disability-adjusted life year (DALY) rates, and age-standardized DALY rates attributable to ischemic stroke globally and within the four countries listed above, covering age groups ranging from 0 to over 95 during the period 1990 to 2021. In this article, DALY is defined as the sum of the number of life years lost due to premature death from ischemic stroke and the number of life years lived in the disabled state, and is used to assess the burden of the disease on the overall population. The all-age DALY rate represents the total burden per year per population without age adjustment, calculated as the total number of DALYs in a given year divided by the total population during the same period. It reflects the crude disease burden affecting the entire population.
Statistical methods and data analysis
All data were processed by R software (version 4.2.1). To estimate 95% uncertainty intervals (UI), the analysis was based on the intrinsic characteristics of the GBD database such as model selection, parameter estimation and data quality. These intervals were calculated by generating 1,000 samples after simulation, and the upper and lower limits correspond to the 2.5 and 97.5 percentiles of the results distribution, respectively. In addition, due to the data update of GBD 2021 version, the socio-demographic index (SDI) was introduced for these four countries as an important variable for the analysis in this study. The detailed methodology and modeling approach used in GBD 2021 were described in other publications (14, 17, 18). The data used in this study were anonymized and publicly accessible, and informed consent waiver approval was obtained from the University of Washington Institutional Review Board.
SDI
The sociodemographic index (SDI) is a composite indicator developed by GBD researchers that is closely related to the burden of disease and health of a population. It calculates the geometric mean of three indices normalized between 0 and 1: the total fertility rate of the population under 25 years of age (TFU25), the average years of schooling of individuals aged 15 years and older (EDU15+), and the per capita lagged-distributed income (LDI) A value of 0 for the SDI represents the lowest level of development in terms of health-related aspects, while a value of 1 represents the most developed level. In the 2021 SDI, all countries were categorized into five categories based on SDI: low SDI: < 0.47; medium-low SDI: 0.47–0.62; medium SDI: 0.62–0.71; medium-high SDI: 0.71–0.81; and high SDI: > 0.81 (19). This study measures the level of development of these four countries through SDI.
Age-period-cohort analysis
This study used age-period-cohort modeling analysis to assess the impact of age, period, and cohort effects on ischemic stroke incidence, prevalence, and DALY trends. The model independently estimates the coefficients of the effects of age, period, and cohort effects by using the Intrinsic Estimator (IE) subalgorithm. The IE method employs principal component regression techniques, and the robustness of its statistical properties has been validated in several modeling studies (20, 21). In this study, age was divided into one cohort for every 5 years of age, the period was divided into 6 cohorts (one cohort for every 5 years), and the data for the year in the middle of each cohort were used as the incidence of ischemic stroke during that period (22). A total of 25 birth cohorts were obtained (see Supplementary Table 1 for a detailed schematic). Incidence, prevalence and relative risk (RR) of DALY were obtained by transforming the natural logarithm of the effect coefficients. Finally, age-period-cohort analysis was performed using the Age Period Cohort Analysis Tool. Additionally, Bayesian Age-Period-Cohort (BAPC) (Version number: 0.0.36) analysis was performed in R language using BAPC and Integrated Nested Laplace Approximations (INLA) (Version number: 25.02.10) packages to predict the prevalence rates for different gender and age groups from 2022 to 2036.
Results
DALYs for ischemic stroke in 4 countries in 2021
In 2021, the global rate of all-age DALYs for ischemic stroke was 837.36 (95% UI 763.73–904.98) per 100,000 people, which was a reduction from 1,286.31 per 100,000 people (95% UI 1,195.19–1,376.06) in 1990. And of the 4 countries of interest, China had the highest ischemic stroke burden, with an overall level of 1180.98 (95% UI 1009.70–1356.67) per 100,000 people, especially for the male group of 1518.49 per 100,000 people. The DALY value for Singapore was relatively low, with an overall level of 205.84 (95% UI 174.50–237.16). And excluding China, the rates of DALYs in the remaining 3 countries were significantly lower than the global average (Table 1; Figure 1).
Table 1
| Location_name | Sex_name | Val | Upper | Lower | UI |
|---|---|---|---|---|---|
| Global | Male | 975.30 | 1069.81 | 885.61 | 975.30 (885.61, 1069.81) |
| Female | 719.52 | 791.64 | 642.82 | 719.52 (642.82, 791.64) | |
| Both | 837.36 | 904.98 | 763.73 | 837.36 (763.73, 904.98) | |
| Finland | Male | 406.70 | 448.27 | 364.40 | 406.70 (364.40, 448.27) |
| Female | 312.94 | 349.48 | 269.98 | 312.94 (269.98, 349.48) | |
| Both | 357.84 | 397.54 | 314.38 | 357.84 (314.38, 397.54) | |
| Republic of Korea | Male | 608.95 | 688.27 | 532.61 | 608.95 (532.61, 688.27) |
| Female | 371.47 | 436.46 | 298.91 | 371.47 (298.91, 436.46) | |
| Both | 473.65 | 540.18 | 401.60 | 473.65 (401.60, 540.18) | |
| China | Male | 1518.49 | 1819.06 | 1243.01 | 1518.49 (1243.01, 1819.06) |
| Female | 921.94 | 1107.52 | 760.75 | 921.94 (760.75, 1107.52) | |
| Both | 1180.98 | 1356.67 | 1009.70 | 1180.98 (1009.70, 1356.67) | |
| Singapore | Male | 220.69 | 256.34 | 185.50 | 220.69 (185.50, 256.34) |
| Female | 189.60 | 217.58 | 160.58 | 189.60 (160.58, 217.58) | |
| Both | 205.84 | 237.16 | 174.50 | 205.84 (174.50, 237.16) |
DALYs for ischemic stroke in 4 countries in 2021.
Figure 1

DALYs by all age groups globally and in China, South Korea, Finland, and Singapore.
Age-Period-Cohort analysis of ischemic stroke incidence
The Age-Period-Cohort (APC) model was employed to dissect the trends in ischemic stroke incidence into age, period, and cohort effects, providing insights beyond the crude temporal changes. The detailed data for the APC analysis results are provided in Supplementary Tables 2–6.
Age effects
The age effects, which represent the intrinsic risk of disease associated with each age group, exhibited a consistent pattern across Finland, Korea, and Singapore. The relative risk (expressed as logarithmic incidence rate ratios) was significantly below the reference level in the 0–20 age group. This risk increased steadily with age, peaking around the 50-year-old age group. In contrast, China displayed a distinct pattern, where the relative risk remained below the reference level until approximately 40 years of age before rising sharply to peak at around 80 years of age. Moreover, there is a marked trend toward younger age groups experiencing high incidence rates, with the age range shifting from the elderly population (65–94 years) toward middle-aged individuals (40–64 years) (Figure 2). These findings confirm that the biological risk of ischemic stroke is predominantly concentrated in middle-aged and elderly populations in all studied countries.
Figure 2
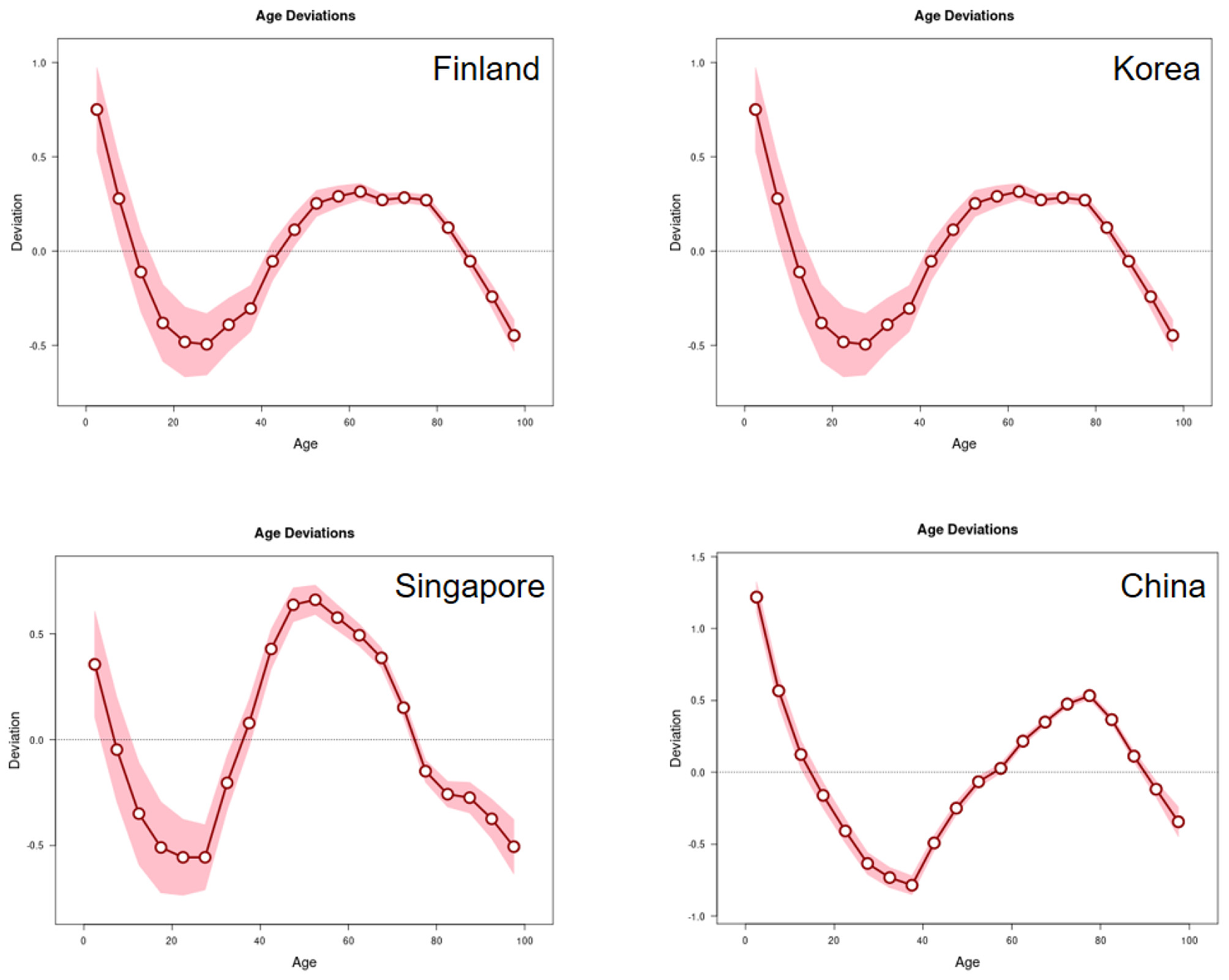
Impact of the age effect on the incidence of IS in Finland, Korea, Singapore and China.
Period effects
The period effects, reflecting the influence of external factors affecting all age groups simultaneously at specific points in time, showed distinct fluctuations across the four countries (Figure 3). A notable increase in relative risk was observed between 1995 and 2000 in Finland, Korea, and Singapore. However, since approximately 2010, only Finland demonstrated a significant declining period effect. In China, the period effects remained relatively stable throughout the study duration, indicating that the incidence rate in China has been less influenced by the broad temporal factors (e.g., population-wide changes in healthcare or policy) that affected the other nations.
Figure 3
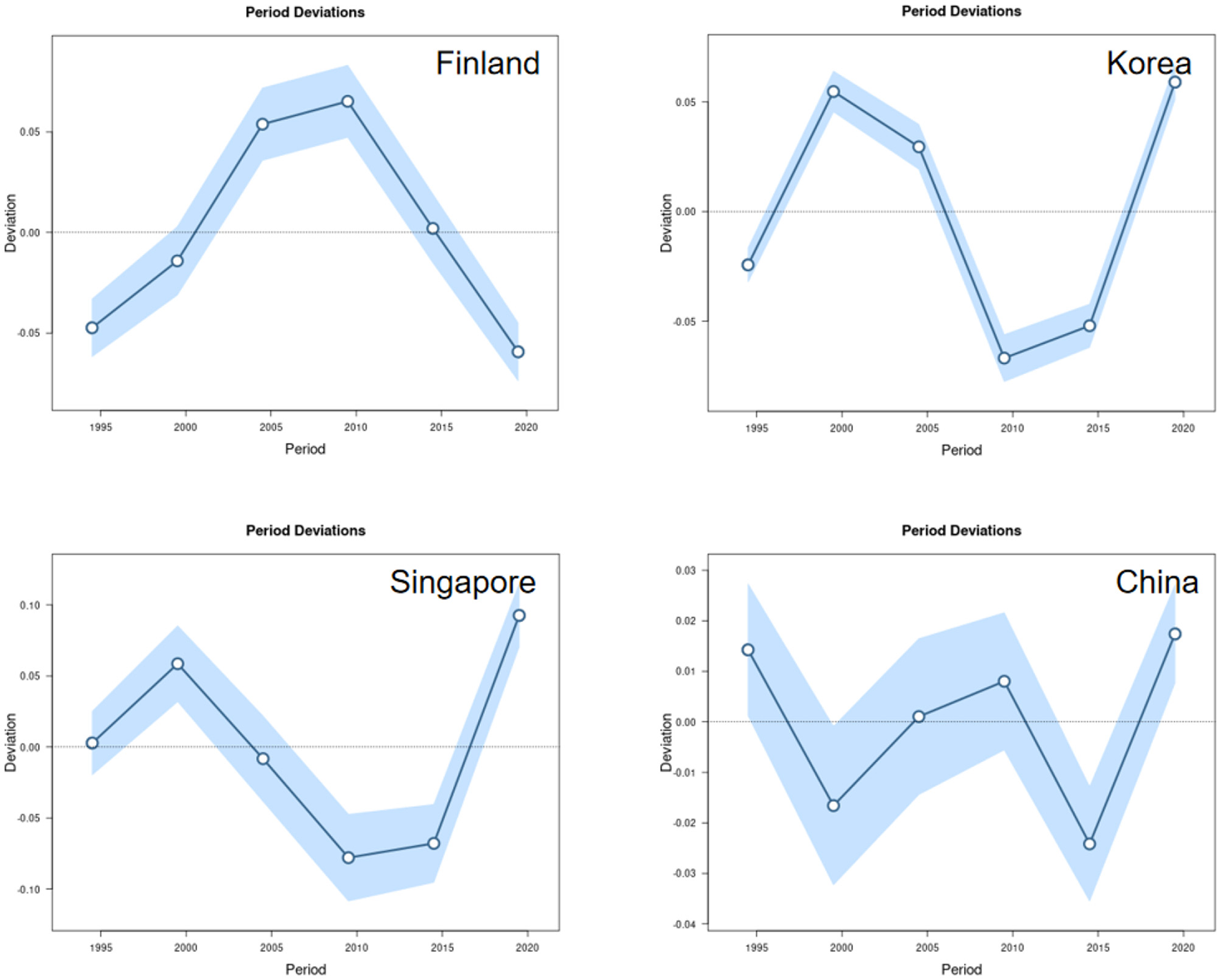
Impact of period effects on the incidence of IS in Finland, Korea, Singapore and China.
Cohort effects
The cohort effects, indicating the lifetime risk characteristic of specific birth cohorts, revealed important trends in disease risk across generations. The birth cohort deviations for Finland, Korea, and Singapore exhibited a pronounced “U-shaped” pattern. This indicates that earlier and later birth cohorts experience a higher relative risk of ischemic stroke compared to those born in the middle decades (e.g., around 1940–1960) (Supplementary Table 1). Conversely, China's cohort effects showed a generally consistent trend of gradual improvement, with later birth cohorts exhibiting a lower relative risk than their predecessors (Figure 4).
Figure 4
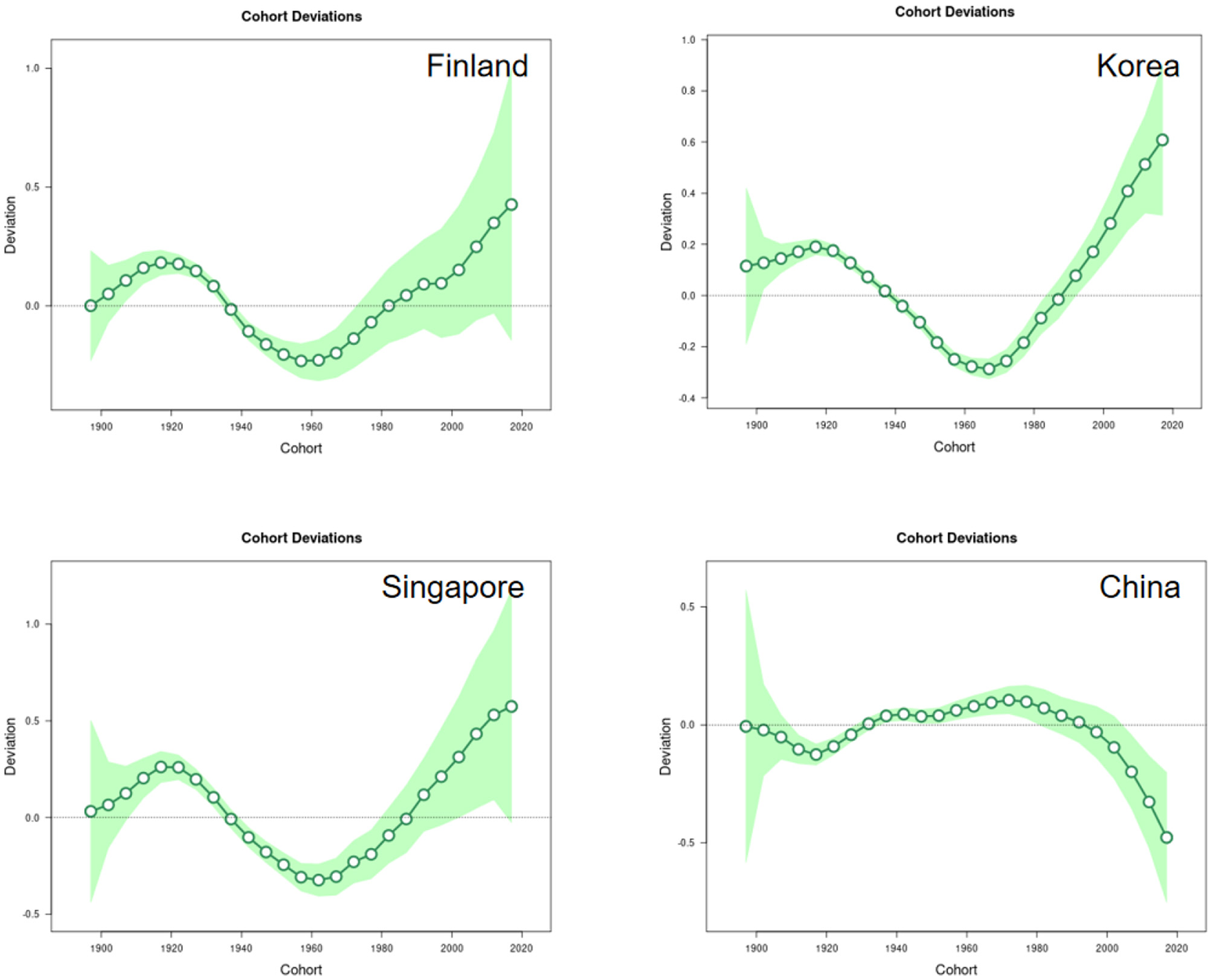
Impact of cohort effects on the incidence of IS in Finland, Korea, Singapore and China.
Future projections of ischemic stroke in 4 countries
The observed trends in age-standardized incidence rates (ASIR) of ischemic stroke from 1990 to 2021, along with projections to 2036, varied substantially among the countries (Figure 5).
Figure 5

Future projections of ischemic stroke of Finland, Korea, Singapore and China.
Finland: The ASIR displayed a steady decreasing trend from nearly 200 to approximately 100 per 100,000 people. Projections indicate that this decline is plateauing, with the future rate stabilizing around 100 per 100,000. The uncertainty interval for this projection was relatively narrow (95% UI: 40.12 to 119.59), suggesting stable and reliable estimates.
Korea and Singapore: Both countries experienced a dramatic decline in ASIR between 1990 and 2010. In Korea, the rate fell from 300 to below 150 per 100,000, while in Singapore, it decreased from 250 to about 100 per 100,000. Projections for both nations suggest that this downward trend has halted, with incidence rates stabilizing near 100 per 100,000.
China: In contrast, the ASIR in China showed a gradual but persistent increase from about 100 to nearly 150 per 100,000. Projections indicate a continuation of this upward trajectory, with the rate potentially reaching 200 per 100,000 by 2036. The uncertainty interval for this projection was wide (95% UI: 131.29 to 348.36), indicating greater uncertainty in future estimates.
Discussion
This study utilized the Global Burden of Disease (GBD) database to analyze temporal trends in the incidence, prevalence, and disability-adjusted life years (DALYs) of ischemic stroke in Finland, South Korea, Singapore, and China between 1990 and 2021. It employed age-period-cohort (APC) models to explore age, period, and cohort effects, and utilized Bayesian age-period-cohort (BAPC) models to forecast future incidence trends over the next 15 years. Results indicate that China bears a significantly higher stroke burden than other nations, with incidence rates exhibiting a persistent upward trajectory. Conversely, Finland, South Korea, and Singapore demonstrate relatively lower burdens, characterized by declining or stable incidence trends. Furthermore, age effects reveal a marked increase in ischemic stroke incidence with advancing age, alongside a trend toward younger age groups in China. Period and cohort effects further elucidate the dynamic shifts in stroke burden across countries and their potential drivers.
Although the global average age-standardized incidence rate declined during this period, it has rebounded in recent years and is projected to continue rising over the next 15 years. This reversal may partly relate to rapid global economic development, which has substantially enhanced healthcare standards and public health awareness in some nations. This progress enables governments to establish comprehensive healthcare systems and implement effective public health interventions, such as risk factor management, early disease screening, and prevention (23, 24). However, the global rebound may be linked to population aging, increased chronic disease burden, and changing lifestyles (25–28). Ischemic stroke is a complex cerebrovascular disorder whose pathophysiological mechanisms primarily involve reduced cerebral blood flow, vascular endothelial dysfunction, inflammatory responses, thrombosis, and neuronal injury (29). Research indicates that regional disparities in stroke burden may be closely linked to the prevalence of these mechanisms and the distribution of associated risk factors. For instance, persistent exposure to high-salt diets, high smoking rates, and inadequate management of hypertension are all factors strongly associated with increased risks of vascular endothelial dysfunction and thrombosis (30–33). Moreover, aging is a significant driver of rising stroke incidence, with rapid population aging potentially exacerbating the stroke burden further (34).
Concurrently, substantial variations between nations underscore the complexity of the epidemiological profile of ischemic stroke. These disparities across countries and regions may stem from differences in socioeconomic development, public health policies, cultural practices, and lifestyles. Nations should enhance collaboration and exchange experiences in prevention and treatment to mitigate the multidimensional burden of this disease.
By analyzing the age-period-cohort model, we can further explore the specific reasons for these differences.
From an age perspective, global averages and distribution curves across four countries reveal that the incidence of ischemic stroke increases significantly with age, rising from around 20 years and peaking around 60 years. Concurrently, the elderly population exhibits the highest age-standardized prevalence rates, age-standardized incidence rates, and age-standardized disability-adjusted life years (DALYs). This phenomenon aligns with established associations between age and ischemic stroke risk (35).
The heightened disease burden among the elderly may stem from the cumulative effects of long-term risk factors and the gradual manifestation of degenerative changes within the cerebrovascular system. The most characteristic pathological alterations include reduced arterial wall elasticity and impaired vascular endothelial cell regulatory function (36, 37).
Moreover, in developed nations, the age range for high incidence of ischaemic stroke has progressively shifted from the traditional elderly cohort (65–94 years) toward middle-aged individuals (40–64 years). This trend likely arises from increasing exposure among middle-aged adults to risk factors historically associated with older age groups, such as hypertension, coronary heart disease, diabetes mellitus, hypercholesterolemia, and impaired glucose tolerance (38). Addressing this trend, future research should further analyze specific drivers in the middle-aged population (e.g., hypertension control and lifestyle modifications) and incorporate scenario-based predictive analyses with covariates (e.g., smoking prevalence, dietary patterns, physical activity levels) to generate more policy-relevant outcomes. Concurrently, enhanced early screening and health education for middle-aged individuals should be prioritized, alongside lifestyle interventions (such as exercise and healthy diets) to effectively reduce stroke risk.
From a period perspective, economic globalization has facilitated the dissemination of advanced medical technologies and health-conscious lifestyles, contributing to an overall downward trend in incidence rates. However, fluctuations in period bias curves across nations may correlate with economic factors and public health events; for instance, financial crises may induce heightened stress and deteriorating lifestyles, thereby elevating stroke risk (39–42). Moreover, public health crises (such as the COVID-19 pandemic) may further exacerbate ischemic stroke risk by altering population behaviors (e.g., increased sedentary lifestyles, dietary deterioration). These period effects underscore the necessity for health policy implementation to account for socioeconomic shifts impacting population health.
Notably, declining ischemic stroke incidence in certain countries correlates closely with specific public health policies. For instance, China's incidence reduction between 1995 and 2000 may relate to the successful implementation of national salt reduction campaigns and health education initiatives (43); while Finland's decline since 2010 may be closely linked to reduced smoking rates (44). Future research should further explore the long-term effects of these policy drivers and conduct scenario-based predictive analyses incorporating relevant covariates (e.g., hypertension, diabetes, air pollution) to generate more policy-relevant estimates. Furthermore, it is recommended to assess the calibration and uncertainty of predictive models through post-prediction and a posteriori forecasting checks, thereby enhancing the precision and efficacy of policy interventions.
From a cohort perspective, cohort bias exhibits significant variations across nations. Finland, South Korea, and Singapore demonstrate a characteristic “U-shaped” trend in cohort bias, where bias initially declines before increasing. This pattern reflects the combined effects of healthcare standards, economic and social development, and population aging on incidence rates. South Korea's increasing cohort bias may correlate with its advancing population aging (45). In contrast, China's cohort bias exhibits an overall trend of gradual improvement, indicating that public health interventions and rising living standards positively contribute to reducing ischemic stroke risk (46).
Regarding cohort effects, future research should further explore differences in health behaviors, healthcare resource accessibility, and socioeconomic status across cohorts (47–51). For instance, more in-depth analysis could be conducted on health behaviors (such as dietary patterns and exercise habits) and the distribution of healthcare resources within urban and rural cohorts (28, 30, 52). Furthermore, it is recommended to integrate data on specific subtypes of ischemic stroke (29) to examine the long-term impact of different cohorts on future disease burden, thereby providing more targeted evidence for policy formulation.
Future projections indicate that incidence rates in Finland and Singapore will continue to decline and remain at low levels, whereas China may experience a gradual increase due to population aging and rising chronic diseases (53). The growing burden of chronic conditions such as hypertension and diabetes are likely to be a primary driver of rising ischemic stroke incidence in China (54). In response to this trend, it is recommended to strengthen comprehensive chronic disease management, including multidisciplinary collaboration and community health services (55–57). Furthermore, health education for the elderly population should be enhanced to encourage healthy behaviors and regular medical check-ups. International cooperation also holds significant importance in reducing the burden of ischemic stroke. By sharing successful experiences (such as Finland's smoking rate control and Singapore's health management) (58, 59), countries can collectively address the challenges posed by the burden of ischemic stroke.
This Global Burden of Disease (GBD) study offers a valuable macro-level assessment of the global ischemic stroke burden. By integrating diverse data sources and employing rigorous modeling, it illuminates overall trends and key risk factors, providing a crucial evidence base for understanding global disease patterns and filling knowledge gaps, especially in data-scarce regions. However, the findings must be interpreted with caution due to several limitations.
These limitations primarily lie in three areas. First, the heavy reliance on heterogeneous secondary data may lead to underestimation of the true burden in low- and middle-income countries and introduce compositional bias. The modeling approach itself, while advanced, depends on assumptions and statistical imputation, introducing uncertainty. The absence of sensitivity analysis further limits the ability to assess the robustness of the estimates (2). Secondly, the analysis lacks depth and specificity; it cannot classify strokes into etiological subtypes (e.g., TOAST criteria), examine the compounding effects of risk factors, or account for the influence of existing national stroke prevention and management strategies (5). Thirdly, the study period coincides with the COVID-19 pandemic, which likely confounded trends through increased thrombotic events and widespread healthcare disruptions.
In conclusion, while this study provides an essential macro-perspective on long-term, large-scale trends, its limitations necessitate cautious interpretation of specific regional or national estimates. Future research should aim to incorporate higher-quality primary data, conduct subtype-specific analyses, perform sensitivity analyses, and integrate assessments of healthcare policies. Additionally, moving beyond the current model's projections, which may not capture future disruptive events, by leveraging individual-level data and alternative modeling techniques (e.g., machine learning) would be valuable for exploring specific drivers (e.g., socioeconomic factors, biomarkers) and informing targeted interventions.
Conclusions
Although the global average age-standardized incidence rate declined between 1990 and 2021, it has shown an upward trend in recent years and is likely to continue to rise over the next 15 years. Significant differences in age-standardized incidence rates of ischemic stroke between Finland, Korea, Singapore and China may be attributed to differences in the level of economic development, healthcare conditions and demographics of each country. Using an age-period-cohort model, this study provides trends in the incidence of ischemic stroke and provides a basis for the development of targeted prevention and management strategies in each country.
Statements
Data availability statement
The original contributions presented in the study are included in the article/Supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving human participants were reviewed and approved by the Ethics Committee of the School of Nursing, Jilin University, Changchun, China. Written informed consent from the patients/participants or patients/participants' legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
JZ: Writing – original draft, Writing – review & editing. BZ: Data curation, Writing – original draft, Writing – review & editing. KW: Software, Visualization, Writing – review & editing. LZ: Supervision, Writing – review & editing. ZX: Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the green seedling program of China-Japan Union Hospital (Grant Number: 2024QM17).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fneur.2025.1651799/full#supplementary-material
References
1.
Fagin VL Norrving B Mensah GA . Global burden of stroke. Circ Res. (2017) 120:439–48. 10.1161/CIRCRESAHA.116.308413
2.
GBD 2019 Stroke Collaborators . Global, regional, and national burden of stroke and its risk factors, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet Neurol. (2021) 20:795–820. 10.1016/S1474-4422(21)00252-0
3.
Lavine SD Cockroft K Hoh B Bambakidis N Khalessi AA Woo H et al . Training guidelines for endovascular ischemic stroke intervention: an international multi- society consensus document. AJNR Am J Neuroradiol. (2016) 37:E31–4.
4.
Katan M Luft A . Global burden of stroke. Semin Neurol. (2018) 38:208–11 10.1055/s-0038-1649503
5.
Ma Q Li R Wang L Yin P Wang Y Yan C et al . Temporal trend and attributable risk factors of stroke burden in China, 1990-2019: an analysis for the Global Burden of Disease Study 2019. Lancet Publ Health. (2021) 6:e897–906. 10.1016/S2468-2667(21)00228-0
6.
Feigin VL Krishnamurthi RV Parmar P Norrving B Mensah GA Bennett DA et al . Update on the global burden of ischemic and hemorrhagic stroke in 1990-2013: the GBD 2013 study. Neuroepidemiology. (2015) 45:161–76 10.1159/000441085
7.
Global, regional, and and national burden of stroke, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016 . Lancet Neurol. (2019) 18:439–58. 10.1016/S1474-4422(19)30034-1
8.
Ding Q Liu S Yao Y Liu H Cai T Han L . Global, regional, and national burden of ischemic stroke, 1990–2019. Neurology. (2022) 98:e279–90. 10.1212/WNL.0000000000013115
9.
Cheng F Cheng P Xie S Wang H Tang Y Liu Y et al . Epidemiological trends and age-period-cohort effects on ischemic stroke burden across the BRICS-plus from 1992 to 2021. BMC Public Health. (2025) 25:137. 10.1186/s12889-025-21310-9
10.
Hyvrinen M Qiao Q Tuomilehto J Söderberg S Eliasson M Stehouwer CDA . The difference between acute coronary heart disease and ischemic stroke risk with regard to gender and age in Finnish and Swedish populations. J Intern Med. (2010) 268:371–80. 10.1111/j.1747-4949.2010.00423.x
11.
Jung SH . Correction: Stroke rehabilitation fact sheet in Korea. Ann Rehabil Med. (2022) 46:108. doi: 10.5535/arm.22001.e. Erratum for: Ann Rehabil Med. (2022) 46:1–8. 10.5535/arm.22001
12.
Lee J Kang DW Kwon SU Kim JS . Stroke statistics in Korea: part I. Epidemiol Risk Fact J Stroke. (2016) 18:2–15. 10.5853/jos.2013.15.1.2
13.
Sacco RL Kasner SE Broderick JP Caplan LR Connors JJ Culebras A et al . An updated definition of stroke for the 21st century: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. (2013) 44:2064–89. 10.1161/STR.0b013e318296aeca
14.
Diseases GBD Injuries C . Global incidence, prevalence, years lived with disabil- ity (YLDs), disability-adjusted life- years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 sub national locations, 1990- 2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2133–61. 10.1016/S0140-6736(24)00757-8
15.
Holford TR . Age–Period–Cohort analysis. Encycl Biostat. (2005) B2A03003. 10.1002/0470011815.b2a03003
16.
Global Burden of Disease Study 2021 . (GBD 2021) Socio-Demographic-Index (SDI)1950–2021. Available online at: https://ghdx.healthdata.org/record/global-burden-disease-study-2021-gbd-2021-socio-demographic-index-sdi-1950%E2%80%932021 (Accessed September 10, 2024).
17.
Schumacher AE Kyu HH Aali A Abbafati C Abbas J Abbasgholizadeh R et al . Global age-sex-specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:1989–2056. 10.1016/S0140-6736(24)00476-8
18.
Naghavi M Ong KL Antony CM Aravkin AY Arndt MB Basting AV et al . Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2100–32. 10.1016/S0140-6736(24)00367-2
19.
Brauer M Roth GA Aravkin AY Zheng P Afshin A Ahmad N et al . Global burden and strength of evidence for 88 risk factors in 204 countries and 811 subnational locations,1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2162–203. 10.1016/S0140-6736(24)00933-4
20.
Luo L . Assessing validity and application scope of the intrinsic estimator approach to the age-period-cohort problem. Demography. (2013) 50:1945–67. 10.1007/s13524-013-0243-z
21.
Wenjiang JF Peter H . Asymptotic properties of estimators in age-period-cohort analysis. Stat Probab Lett. (2006) 76:1925–9. 10.1016/j.spl.2006.04.051
22.
Chen X Sun Y Li Z Yu B Gao G Wang P . Historical trends in suicide risk for the residents of mainland China: APC modeling of the archived national suicide mortality rates during 1987–2012. Soc Psychiatry Psychiatr Epidemiol. (2019) 54:99–110. 10.1007/s00127-018-1593-z
23.
Pandian JD Gall SL Kate MP Silva GS Akinyemi RO Ovbiagele BI et al . Prevention of stroke: a global perspective. Lancet. (2018) 392:1269–78. 10.1016/S0140-6736(18)31269-8
24.
Chimatiro GL Rhoda AJ . Scoping review of acute stroke care management and rehabilitation in low and middle-income countries. BMC Health Serv Res. (2019) 19:789. 10.1186/s12913-019-4654-4
25.
Huang Y Lee D . Association between physical activity behaviors and hypertension with comorbid multiple chronic diseases in South Korean middle-aged and elderly: an analysis based on association rule. BMC Public Health. (2025) 25:1586. 10.1186/s12889-025-22806-0
26.
Liang D Guan Q Huang M He Y Ou Y Chen M et al . Changing trends of disease burden of stroke from 1990 to 2019 and its predictions among the Chinese population. Front Neurol. (2023) 14:1255524. 10.3389/fneur.2023.1255524
27.
Zhou M Wang H Zeng X Yin P Zhu J Chen W et al . Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. (2019) 394:1145–58. 10.1016/S0140-6736(19)30427-1
28.
Zhang X Ye WQ Xin XK Gao YJ Yang F . Global, regional, and national burden of stroke attributable to diet high in sodium from 1990 to 2019: a systematic analysis from the global burden of disease study 2019. Front Neurol. (2024) 15:1437633. 10.3389/fneur.2024.1437633
29.
Feske SK . Ischemic stroke. Am J Med. (2021) 134:1457–64. 10.1016/j.amjmed.2021.07.027
30.
Schmidt-Pogoda A Strecker JK Liebmann M Massoth C Beuker C Hansen U et al . Dietary salt promotes ischemic brain injury and is associated with parenchymal migrasome formation. PLoS ONE. (2018) 13:e0209871. 10.1371/journal.pone.0209871
31.
Ishida M Sakai C Kobayashi Y Ishida T . Cigarette smoking and atherosclerotic cardiovascular disease. J Atheroscler Thromb. (2024) 31:189–200. 10.5551/jat.RV22015
32.
Fan J Li X Yu X Liu Z Jiang Y Fang Y et al . Global burden, risk factor analysis, and prediction study of ischemic stroke, 1990-2030. Neurology. (2023) 101:e137–50. 10.1212/WNL.0000000000207387
33.
Webb AJS Werring DJ . New insights into cerebrovascular pathophysiology and hypertension. Stroke. (2022) 53:1054–64. 10.1161/STROKEAHA.121.035850
34.
Gou R Luo C Liang X Qin S Wu H Li B et al . Elderly stroke burden: a comprehensive global study over three decades. Front Aging. (2025) 6:1489914. 10.3389/fragi.2025.1489914
35.
Bengtsson VW Persson GR Berglund J Renvert S . Carotid calcifications in panoramic radiographs are associated with future stroke or ischemic heart diseases: a long-term follow-up study. Clin Oral Invest. (2019) 23:1171–9. 10.1007/s00784-018-2533-8
36.
Ovbiagele B Nguyen-Huynh MN . Stroke epidemiology: advancing our understanding of disease mechanism and therapy. Neurotherapeutics. (2011) 8:319–29. 10.1007/s13311-011-0053-1
37.
Purnell C Gao S Callahan CM Hendrie HC . Cardiovascular risk factors and incident Alzheimer disease: a systematic review of the literature. Alzheimer Dis Assoc Disord. (2009) 23:1–10. 10.1097/WAD.0b013e318187541c
38.
Rahman A-N . High prevalence of metabolic risk factors for cardiovascular diseases among Saudi population, aged 30–64 years. Int J Cardiol. (1997) 62:227–35. 10.1016/S0167-5273(97)00268-4
39.
Yang H An R Clarke CV Shen J . Impact of economic growth on physical activity and sedentary behaviors: a systematic review. Public Health. (2023) 215:17–26. 10.1016/j.puhe.2022.11.020
40.
Cuevas García-Dorado S Cornselsen L Smith R Walls H . Economic globalization, nutrition and health: a review of quantitative evidence. Glob Health. (2019) 15:15. 10.1186/s12992-019-0456-z
41.
Gupta S Methuen C Kent P Chatain G Christie D Torales J et al . Economic development does not improve public mental health spending. Int Rev Psychiatry. (2016) 28:415–9. 10.1080/09540261.2016.1210582
42.
Wu Y Chen X Hu S Zheng H Chen Y Liu J et al . The impact of potentially modifiable risk factors for stroke in a middle-income area of China: a case-control study. Front Public Health. (2022) 10:815579. 10.3389/fpubh.2022.815579
43.
Hipgrave DB Chang S Li X Wu Y . Salt and sodium intake in China. JAMA. (2016) 315:703–5. 10.1001/jama.2015.15816
44.
Dai X Gakidou E Lopez AD . Evolution of the global smoking epidemic over the past half century: strengthening the evidence base for policy action. Tob Control. (2022) 31:129–37. 10.1136/tobaccocontrol-2021-056535
45.
Statistics Korea . Special Estimate of the Future Population between 2017 and 2067. Daejeon: Statistics Korea (2019).
46.
Wang C Rao K Wu S Liu Q . Health care in China: improvement, challenges, and reform. Chest. (2013) 143:524–31. 10.1378/chest.12-1839
47.
Strilciuc S Grad DA Radu C Chira D Stan A Ungureanu M et al . The economic burden of stroke: a systematic review of cost of illness studies. J Med Life. (2021) 14:606–19. 10.25122/jml-2021-0361
48.
Wang S Shen B Wei L Wu M Wang J . Association between socioeconomic status and prognosis after ischemic stroke in South China. Neurol Res. (2019) 41:916–22. 10.1080/01616412.2019.1630165
49.
Chen X Zheng J Wang J Wang H Shi H Jiang H et al . Global burden and cross-country inequalities in stroke and subtypes attributable to diet from 1990 to 2019. BMC Public Health. (2024) 24:1813. 10.1186/s12889-024-19337-5
50.
Palm F Pussinen PJ Aigner A Becher H Buggle F Bauer MF et al . Association between infectious burden, socioeconomic status, and ischemic stroke. Atherosclerosis. (2016) 254:117–23. 10.1016/j.atherosclerosis.2016.10.008
51.
Zhang R Han L Xu S Jiang G Pu L Liu H . Relationship between socioeconomic status and stroke: an observational and network Mendelian randomization study. J Stroke Cerebrovasc Dis. (2024) 33:108097. 10.1016/j.jstrokecerebrovasdis.2024.108097
52.
McDonnell MN Hillier SL Judd SE Yuan Y Hooker SP Howard VJ . Association between television viewing time and risk of incident stroke in a general population: results from the REGARDS study. Prev Med. (2016) 87:1–5. 10.1016/j.ypmed.2016.02.013
53.
Han Y Hu Y Yu C Guo Y Pei P Yang L et al . Lifestyle, cardiometabolic disease, and multimorbidity in a prospective Chinese study. Eur Heart J. (2021) 42:3374–84. 10.1093/eurheartj/ehab413
54.
Richards A Jackson NJ Cheng EM Bryg RJ Brown A Towfighi A et al . Derivation and application of a tool to estimate benefits from multiple therapies that reduce recurrent stroke risk. Stroke. (2020) 51:1563–9. 10.1161/STROKEAHA.119.027160
55.
Lawrence M Pringle J Kerr S Booth J Govan L Roberts NJ . Multimodal secondary prevention behavioral interventions for TIA and stroke: a systematic review and meta-analysis. PLoS ONE. (2015) 10:e0120902. 10.1371/journal.pone.0120902
56.
Heron N Kee F Mant J Reilly PM Cupples M Tully M et al . Stroke prevention rehabilitation intervention trial of exercise (SPRITE) - a randomised feasibility study. BMC Cardiovasc Disord. (2017) 17:290. 10.1186/s12872-017-0717-9
57.
Towfighi A Cheng EM Ayala-Rivera M Barry F McCreath H Ganz DA et al . Effect of a coordinated community and chronic care model team intervention vs usual care on systolic blood pressure in patients with stroke or transient ischemic attack: the SUCCEED randomized clinical trial. JAMA Netw Open. (2021) 4:e2036227. 10.1001/jamanetworkopen.2020.36227
58.
GBD 2021 . Stroke Risk Factor Collaborators. Global, regional, and national burden of stroke and its risk factors, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. (2024) 23:973–1003. 10.1016/S1474-4422(24)00369-7
59.
GBD 2021 . Tobacco Forecasting Collaborators. Forecasting the effects of smoking prevalence scenarios on years of life lost and life expectancy from 2022 to 2050: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Public Health. (2024) 9:e729–44. 10.1016/S2468-2667(24)00166-X
Summary
Keywords
ischemic stroke, epidemiology, burden of disease, Bayesian Age-Period-Cohort model, disease prediction
Citation
Zhang J, Zhao B, Wang K, Zhao L and Xu Z (2025) Age-Period-Cohort analysis and 2036 projections of the burden of ischemic stroke in Finland, Korea, Singapore and China, 1990–2021. Front. Neurol. 16:1651799. doi: 10.3389/fneur.2025.1651799
Received
07 July 2025
Accepted
14 October 2025
Published
03 November 2025
Volume
16 - 2025
Edited by
Kaijian Hou, Shantou University, China
Reviewed by
Yingxin Yu, Chinese PLA General Hospital, China
Kerollos Abdelsayed, Minneapolis Heart Institute Foundation (MHIF), United States
Updates
Copyright
© 2025 Zhang, Zhao, Wang, Zhao and Xu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhongxin Xu xuzhongxin@jlu.edu.cn
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.