- 1Faculty of Medicine, Cairo University, Cairo, Egypt
- 2Al Jahra Hospital, Al Jahra, Kuwait
- 3Department of Public Health, Al-Qassim Health Cluster, Buraydah, Saudi Arabia
- 4King Abdulaziz Medical City, Riyadh, Saudi Arabia
- 5Internal Medicine Department, Mubarak Al-kabeer Hospital, Jabriyah, Kuwait
- 6College of Medicine, Alfaisal University, Riyadh, Saudi Arabia
- 7Riyadh Second Health Cluster, Riyadh, Saudi Arabia
- 8King Salman Specialist Hospital, Hail Health Cluster, Hail, Saudi Arabia
- 9Sheikh Jaber Al-Ahmad Al-Sabah Hospital, Kuwait City, Kuwait
- 10University of Jeddah, Jeddah, Saudi Arabia
- 11Faculty of Medicine, Tabuk University, Tabuk, Saudi Arabia
- 12Faculty of Medicine, University of Khartoum, Khartoum, Sudan
- 13Faculty of Pharmacy Umm Al-Qura University, Makkah, Saudi Arabia
- 14Faculty of Medicine and Health Sciences, Seiyun University, Seiyun, Yemen
- 15Almana General Hospital, Dammam, Saudi Arabia
Background: Psychological stress has been increasingly recognized as a potential risk factor for stroke, but the strength and consistency of this association remained uncertain. This systematic review and meta-analysis aims to determine the overall association between broad psychological stress and broad stroke risk.
Methodology: Systematic searches of PubMed, Scopus, Web of Science, and OVID databases from 1990 to March of 2025. These searches utilized a strategy combining subject headings and keywords related to psychosocial risk factors and stroke. Twenty-eight studies met inclusion criteria (23 prospective cohort and 5 case-control), comprising over 950,000 participants. We excluded studies involving participants with a history of depression. Stroke was broadly defined to include ischemic, hemorrhagic, subarachnoid, TIA, and unspecified subtypes.
Results: Our meta-analysis of 23 prospective cohort studies found that individuals exposed to psychological stress had a 46% higher risk of experiencing stroke (HR = 1.46; 95% CI: 1.29–1.66; P < 0.01). Initial analysis revealed substantial heterogeneity (I2 = 82%), which was significantly reduced to 39% (HR = 1.45; 95% CI: 1.32–1.59; P = 0.02) after a sensitivity analysis. Analysis of five case-control studies yielded a pooled odds ratio (OR) of 1.10 (95% CI: 1.01–1.20; P < 0.01), also indicating a modest but significant elevation in stroke risk; however, heterogeneity remained high (I2 = 92%). Sex-stratified analysis showed comparable increases in stroke risk for males (HR = 1.33; 95% CI: 1.19–1.49) and females (HR = 1.44; 95% CI: 1.07–1.95), with no statistically significant subgroup difference (P = 0.61).
Conclusion: Psychological stress is significantly associated with an increased risk of fatal stroke, though publication bias and study heterogeneity highlight the need for cautious interpretation. Further research should aim to address methodological variability and selective reporting to refine our understanding of this relationship.
Introduction
Stroke continues to be an important cause of mortality and disability in adulthood, weighing heavily on public health (1). Global estimates indicate that approximately 12 million people suffered a first-ever stroke in 2021, suggesting a rise in incidence partly attributed to the aging population and the presence of risk factors (1). Well-established risk factors for adult stroke include hypertension and smoking, diabetes, and other vascular risk factors (1). In recent years, psychosocial stress has been offered as a potential modifiable risk factor for stroke (2). Large international studies suggest that psychosocial factors might account for a large proportion of stroke risk. For instance, the INTERSTROKE case-control study attributed almost 17% of population stroke risk to psychosocial stressors (with an odds ratio of approximately 2.2 for high stress) (3). This emerging evidence outlines the impact of psychosocial environment on cardiovascular health.
Psychosocial stress arises essentially from one's interaction with social, environmental, or psychological domains. It encompasses various exposures, such as job stress, financial strain, and emotional distress due to major life events (4), Common stressors include job strain, social isolation, caregiver stress, and interpersonal conflicts (5). The stressors act on the hypothalamic-pituitary-adrenal axis to trigger cortisol, inflammatory markers, and sympathetic activity, implicating them in vascular dysfunction (6). A biologically plausible mechanism for stress contributing to stroke is its ability to raise blood pressure, enhance platelet aggregation, and accelerate atherosclerosis (7). As further mechanisms, it is also likely to increase adverse behavior, such as smoking, poor diet, and limited physical activity, thus indirectly increasing stroke risk. The recent INTERSTROKE study recognized psychosocial stress as a major risk factor for stroke, independent of confounders (3).
A meta-analysis published in 2015 synthesized results from 14 observational studies and found an overall significant positive association between psychosocial stress and risk of stroke (8). This meta-analysis found elevated odds of stroke among individuals with high stress, specifically related to general work-related stress and life event-related stress. Since 2015, many high-quality studies have emerged that were not included in earlier reviews; parameters of stress such as chronic perceived stress, occupational stress, and environmental strain were studied in diverse populations (9–13). These newer studies have addressed gaps as stroke subtypes, dose-response relationships, and stress in the absence of clinical anxiety or depression. An updated meta-analysis is therefore called for to consider this new evidence while at the same time updating the combined effect estimates and assessing heterogeneity over study designs and stress types.
It is also worth mentioning that another meta-analysis, published in 2017, found confirmation for the association across different populations and types of stress (14). However, that study had a different exclusion criteria than the one we aim to focus on. Unlike the 2017 meta-analysis, our study excludes individuals with clinical depression in a similar way to the 2015 study (8, 14). This is done in order to minimize confounding, as depression is an independent risk factor for stroke with distinct biological and behavioral mechanisms. This approach allows for a more accurate estimation of the direct association between pychosocial stress and stroke risk.
Hence, this systematic review and meta-analysis examines the expanded and most recent evidence base in order to sharpen our definition of psychosocial stress in relation to stroke risk and offer updated information to guide clinical and public health interventions. Additionally, we seek to synthesize results obtained from observational studies to aid in determining whether psychosocial stress is a significant risk factor of stroke in adults through a meta-analysis that investigates the various aspects of stress exposures (e.g., psychological, financial, work) in relation to all types of stroke, such as ischemic and hemorrhagic subtypes, as well as TIAs in the absence of depression history. Furthermore, Our study divided the participants into males and females to take into account the physiological, as well as psychological differences that determine the impact of stress on both males and females and their biological response to it (11, 15).
Methodology
This systematic review and meta-analysis was conducted and reported in adherence to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) (16) and MOOSE (Meta-analyses Of Observational Studies in Epidemiology) guidelines (17).
Study strategy
We conducted Systematic searches of published papers indexed in PubMed, Scopus, Web of Science and OVID Databases between 1990 and March 2025 using a strategy combining selected subject headings and keywords relating to psychosocial risk factors and stroke. A combination search of subject terms was applied. Subject terms included: (“psychosocial stress” OR “psychological stress” OR “mental stress” OR “work stress” OR “chronic stress” OR “job strain” OR “social stress” OR “life stress” OR “stressful life events” OR “emotional stress”) AND (“stroke” OR “cerebrovascular accident” OR “cerebral infarction” OR “ischemic stroke” OR “hemorrhagic stroke” OR “transient ischemic attack” OR “cerebral hemorrhage”) Manual searching of relevant systematic reviews and the reference lists of included studies was also conducted. Only English language studies were included.
Study selection and eligibility criteria
Studies included in the meta-analysis met the following criteria: (1) Observational studies (prospective cohort or case–control designs). (2) Contained evidence of psychological stress exposure (e.g., self-reported psychological stress, job strain, emotional stress, and socioeconomic hardship), which were either self-reported or measured using validated tools. (3) Primary studies used adjusted models to control for confounders. Studies were excluded if: (1) they reported any history of depression (2) They were review articles, editorials, letters, or abstracts without full-text articles. Stroke was defined broadly to include ischemic, hemorrhagic, subarachnoid, TIA and unspecified subtypes. Four reviewers independently screened titles and abstracts, and bibliographic records were retrieved where available. Full-text articles of potentially relevant studies were retrieved, their eligibility was assessed by four reviewers using the predetermined inclusion criteria. Conflicts were resolved through discussion by two reviewers.
Data extraction
Four reviewers extracted data independently using review-specific extraction tool. Data extracted included details of study design; total number of participants; inclusion and exclusion criteria; conclusion; stroke outcomes; history of co-morbidities including stroke, myocardial infarction, diabetes mellitus, hypertension, depression; type of psychosocial exposure; name of the exposure as mentioned in included studies; type of confounders in adjusted model.
Quality appraisal and risk of bias assessment
Three reviewers independently assessed the quality of each study by using the Newcastle-Ottawa Quality Assessment Scales for Cohort Studies and Case–Control Studies. We graded the selection of participants, assessed exposure and outcome measurements, comparability and control of confounding factors. The maximum total score that could be received is 9 points.
Data synthesis
Pooled effect estimates were calculated using random-effects meta-analysis models to account for between-study variability. For prospective cohort studies, hazard ratios (HRs) were synthesized to evaluate the association between psychological stress and stroke risk, while odds ratios (ORs) were pooled for case–control studies. Heterogeneity was assessed using the I2 statistic and Chi-square test, with values over 50% indicating substantial inconsistency. Sensitivity analysis was performed to explore the impact of individual studies on overall heterogeneity. Specifically, studies contributing to high heterogeneity were systematically excluded, and the pooled estimates were recalculated to evaluate robustness. Subgroup analyses were conducted based on sex to assess potential differences in stroke risk associated with psychological stress among males and females. Additionally, separate synthesis was performed for studies reporting on fatal stroke outcomes. Publication bias was assessed both visually using funnel plots and statistically through Egger's regression test. A significant result from this test was used to indicate the potential presence of small-study effects or selective reporting.
Results
Search results
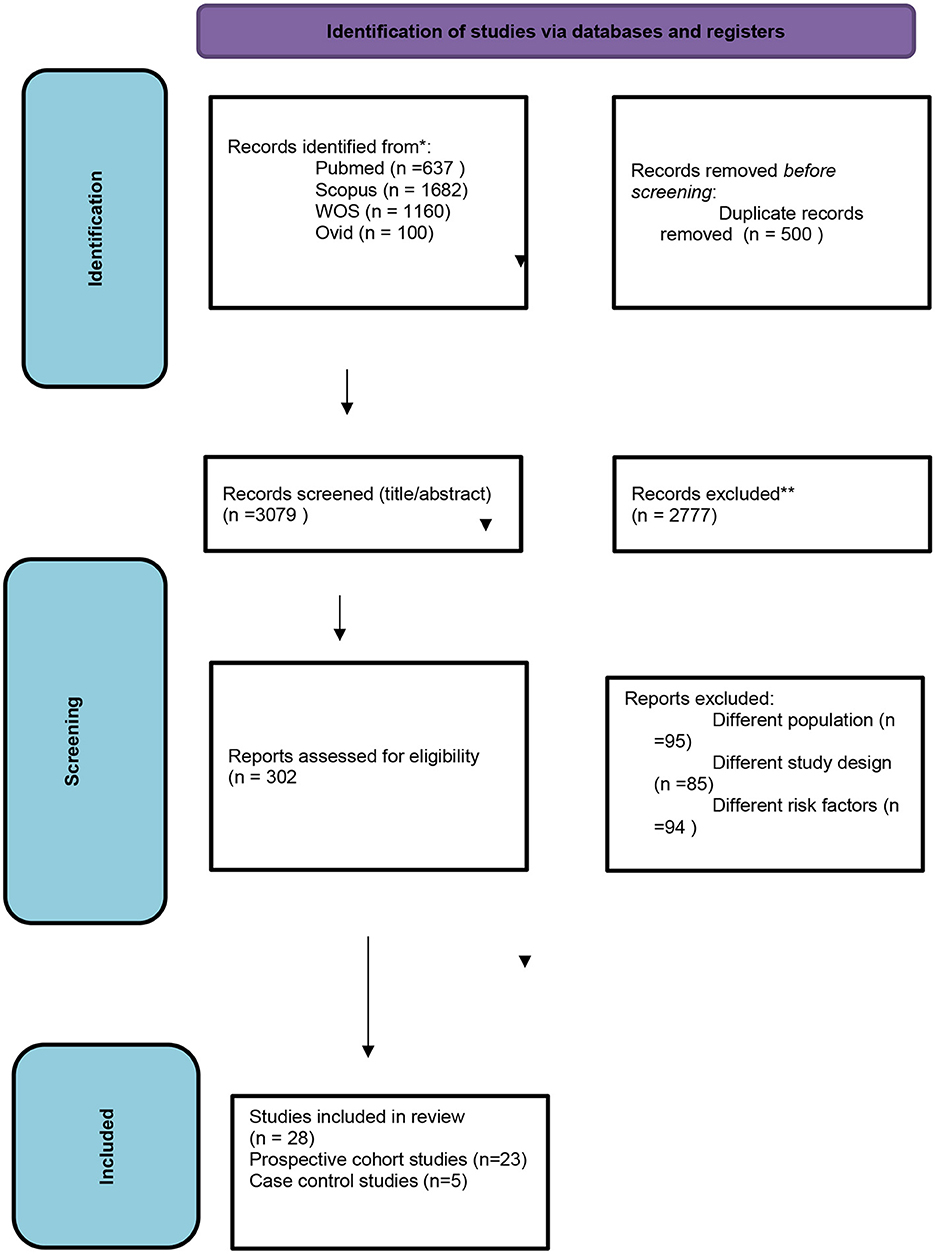
Our primary literature search identified 3,579 records sourced as follows: 637 from PubMed, 1,160 from WOS, 1,682 from Scopus, and 100 from Ovid. Following eliminating duplicates, 3,079 articles underwent screening at the title/abstract level. After screening titles and abstracts, 302 manuscripts remained. Upon conducting the full-text screening, 274 articles were excluded, resulting in a total of 28 studies that fulfilled our inclusion criteria (Figure 1).
Baseline characteristics
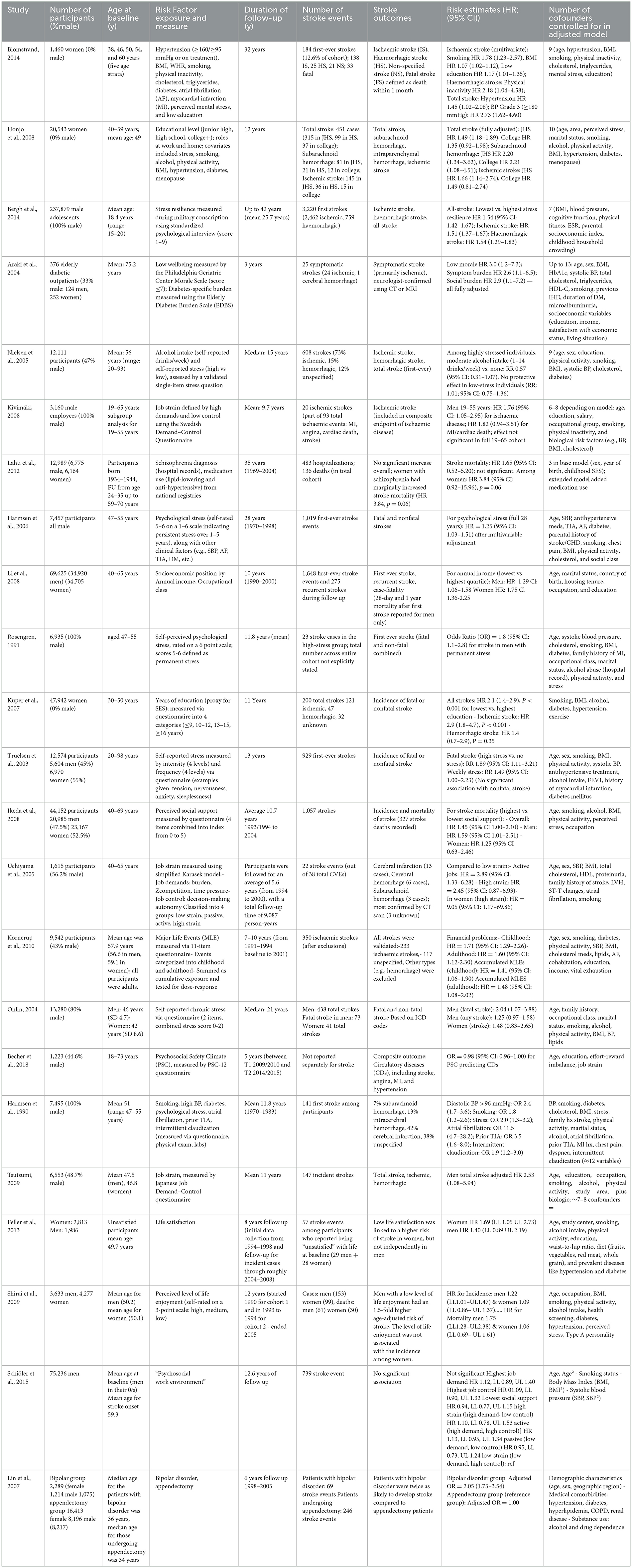
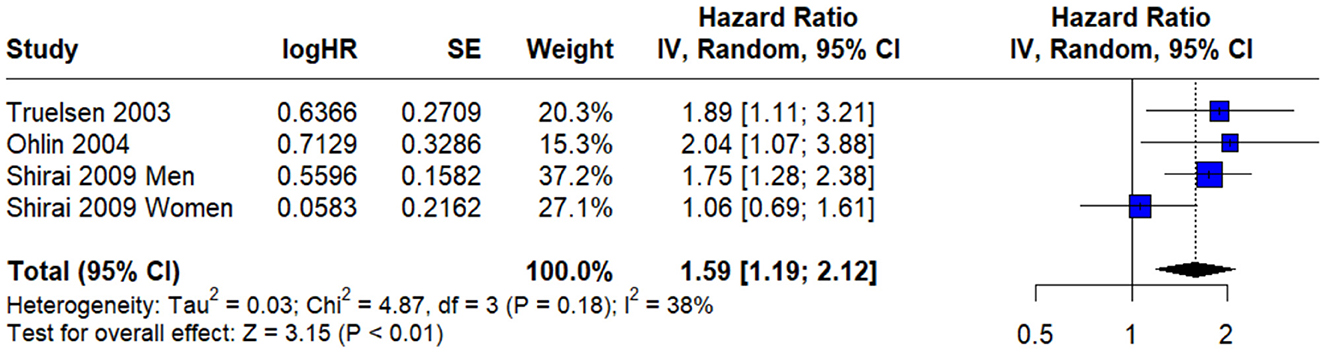
Out of the 28 studies included, 23 were prospective cohort studies and 5 were case–control studies, collectively encompassing a population of over 950,000 participants. The vast majority of these studies were conducted in Europe and Asia, with additional contributions from the United States, Russia, and Australia. Sample sizes ranged dramatically—from small, focused groups of under 400 participants [e.g., (18)] to large national cohorts exceeding 237,000 individuals [e.g., (19)].
Participants varied widely by demographic, clinical, and occupational background. Cohorts included male adolescents undergoing military conscription, older adults with diabetes, hypertensive workers, individuals with psychiatric disorders, and ethnically diverse stroke patients in case–control settings. Most studies focused on mid- to late-adulthood, though several included younger populations starting from 18 or 20 years of age.
Psychological stress exposure was defined through various lenses—occupational stress (e.g., job strain or workplace environment), emotional resilience, life satisfaction, educational or socioeconomic hardship, and psychosocial adversity. While some studies relied on single-item self-report tools, others used structured interviews or validated psychosocial scales.
Stroke outcomes included ischemic, hemorrhagic, subarachnoid hemorrhage, and total or unspecified stroke. The outcome was confirmed through medical records, imaging, national health registries, or death certificates. Ischemic stroke was the most commonly reported subtype across the studies, though many included combined or multiple stroke types (Tables 1, 2).
Quality assessment
In this systematic review, to ensure the accuracy of assessing the validity of the included studies, we used the Newcastle–Ottawa Scale (NOS) for the cohort and case-control studies. This scale evaluates the studies across categories: selection (up to 4 stars), comparability (up to 2 stars), and outcome (up to 3 stars). Among the 23 cohort studies, 17 were classified as low risk, 3 as moderate risk, and 3 as high risk. For the 5 case-control studies, all were low risk except one that showed moderate risk. A detailed summary of the results is provided in Tables 3, 4.
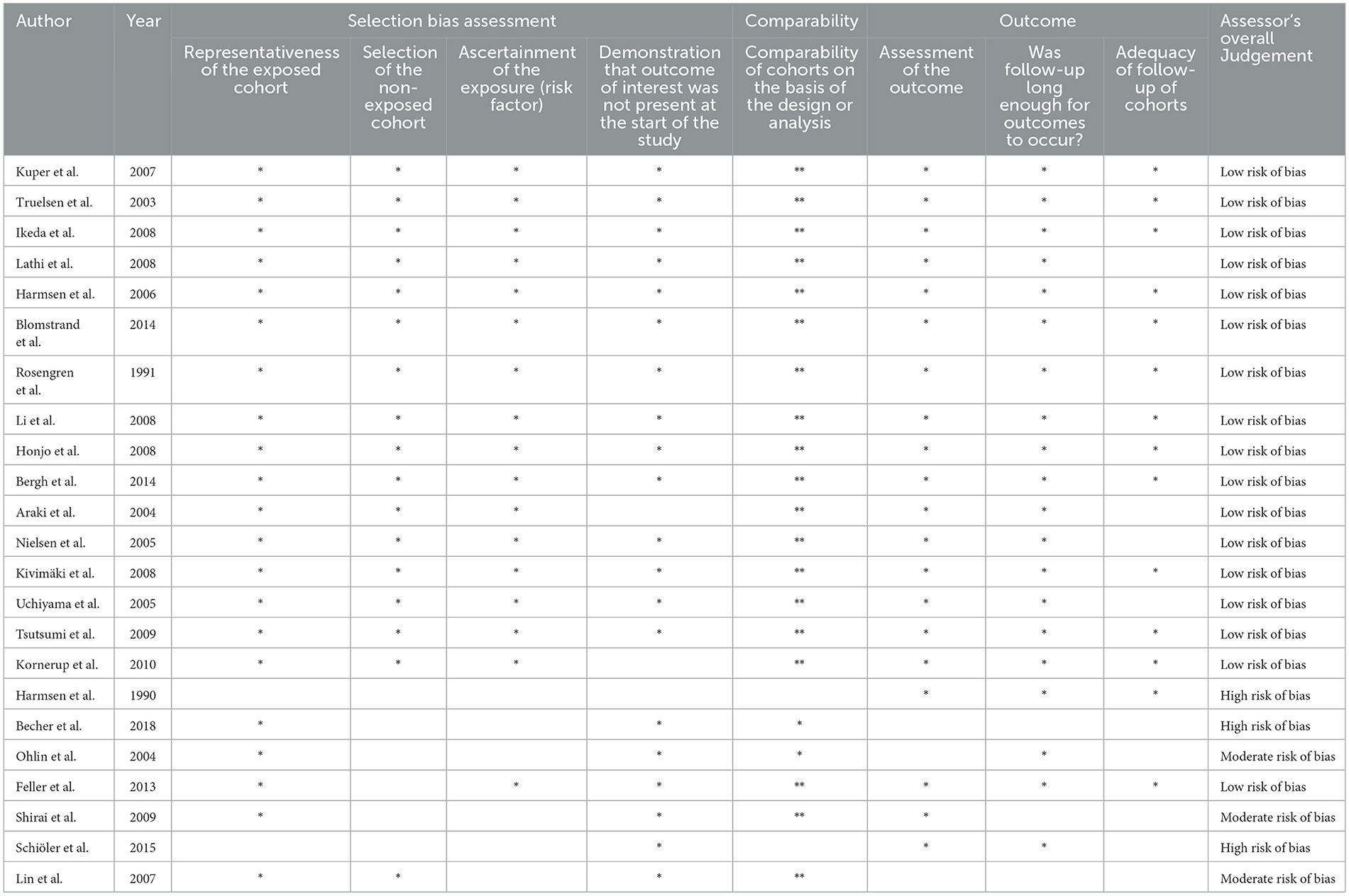
Table 3. Summary table of ROB assessment using the Newcastle-Ottawa Quality Assessment Scale for Cohort studies.
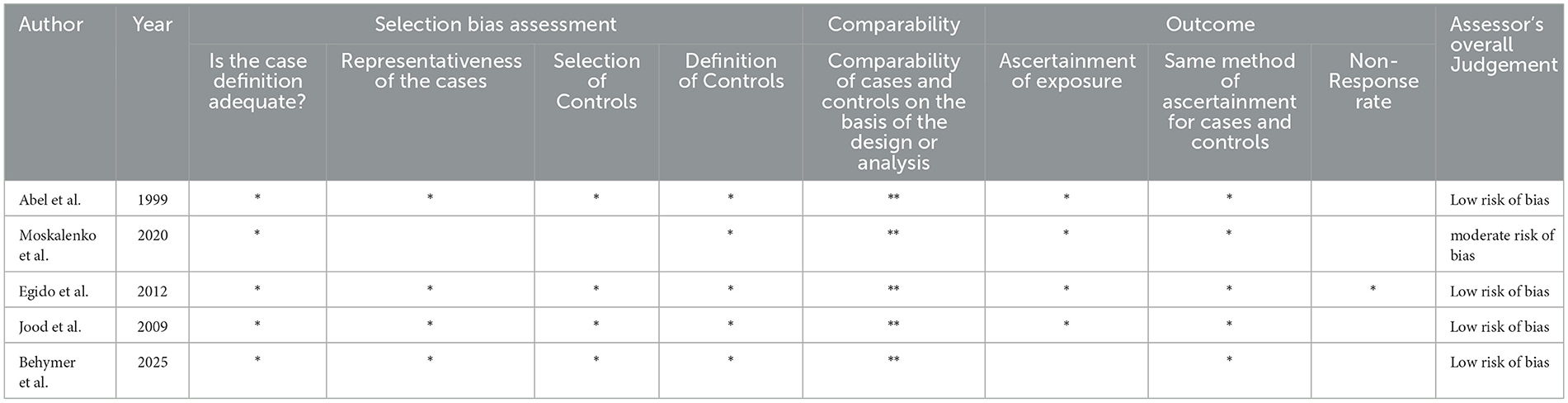
Table 4. Summary table of ROB assessment using the Newcastle-Ottawa Quality Assessment Scale for Case-Conrol studies.
Psychological stress
The meta-analysis of 23 prospective cohort studies produced a pooled hazard ratio (HR) of 1.46 (95% CI: 1.29–1.66; P < 0.01), indicating that individuals exposed to psychological stress had a 46% higher risk of experiencing stroke compared to those without such exposure. However, this association was accompanied by substantial statistical heterogeneity (I2 = 82%), as shown in Figure 2.
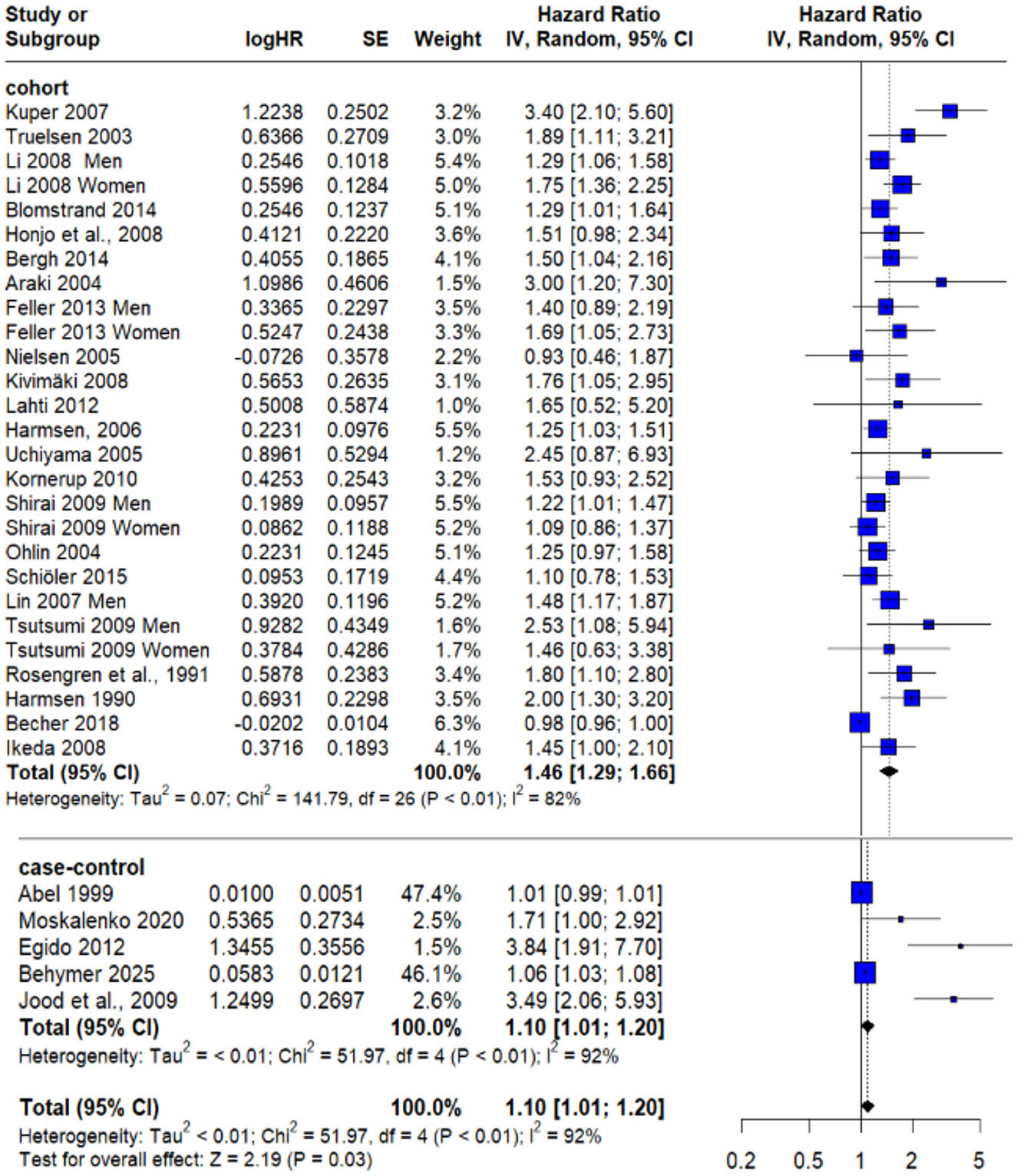
Figure 2. Forest plot of overall pooled effect estimate for risk of any type of stroke in subjects exposed to psychological stress.
To assess the robustness of this finding and identify potential sources of heterogeneity, a sensitivity analysis was conducted. By excluding Becher et al. (20)—which was identified as a likely contributor to variability—the recalculated pooled HR was 1.45 (95% CI: 1.32–1.59; P = 0.02). Importantly, this adjustment reduced heterogeneity to 39% as demonstrated in Figure 3, thereby improving the consistency of the included studies and strengthening confidence in the observed relationship between psychological stress and stroke risk.
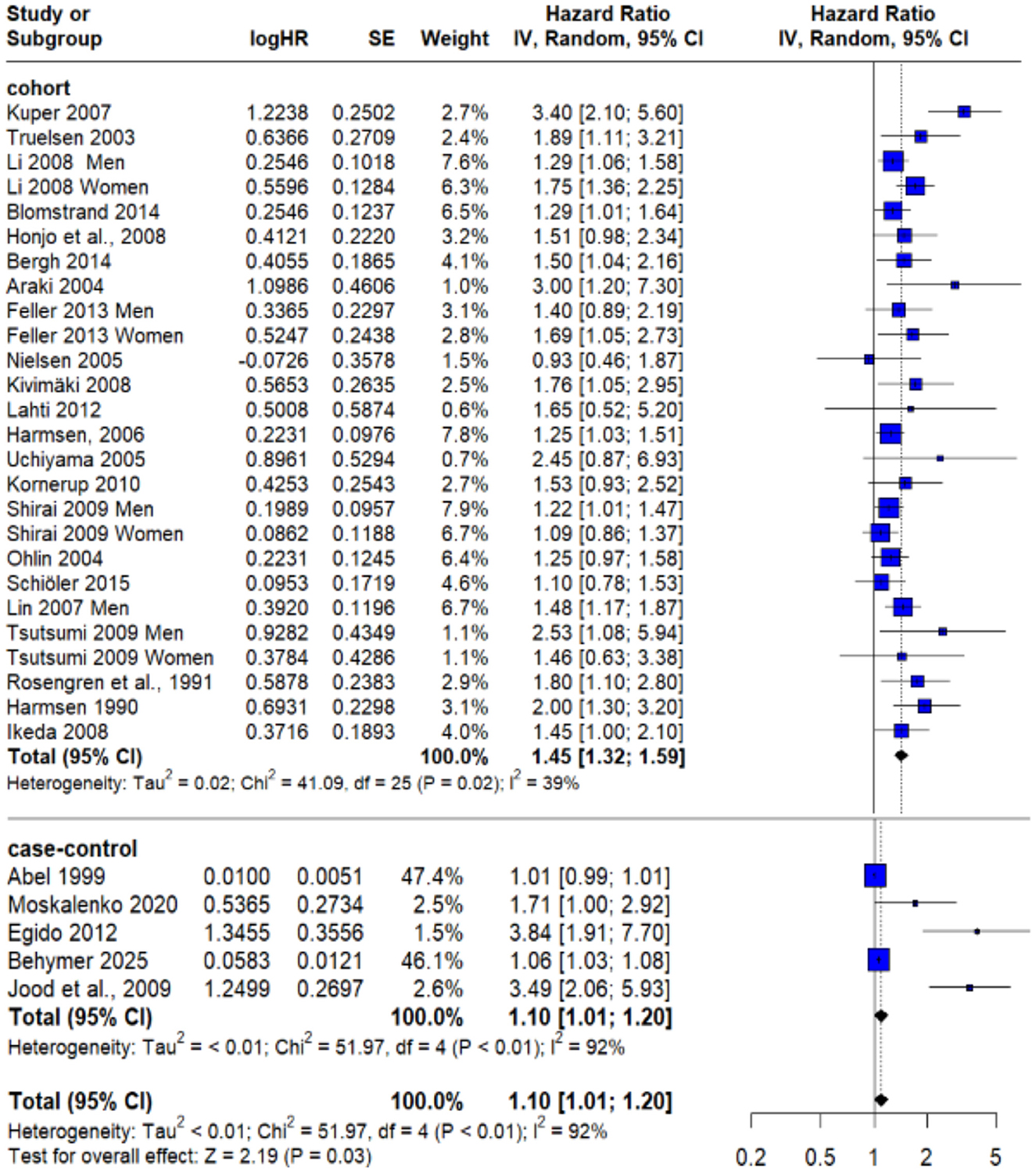
Figure 3. Sensitivity analysis after excluding Becher et al. (20).
In parallel, analysis of five case–control studies yielded a pooled odds ratio (OR) of 1.10 (95% CI: 1.01–1.20; P < 0.01) as shown in Figure 2, also pointing to a modest but statistically significant elevation in stroke risk among individuals with psychological stress. Nonetheless, heterogeneity remained high in this group (I2 = 92%) and couldn't be solved.
Stratified risk analysis by sex and stroke mortality
Five studies provided data for males and females separately, allowing for a comparative analysis of the association between psychological stress and stroke risk in men and women. Among male participants, the pooled hazard ratio (HR) for stroke associated with psychological stress was 1.33 (95% CI: 1.19–1.49), reflecting a statistically significant increase in risk. Notably, the heterogeneity across these studies was negligible (I2 = 0%), suggesting high methodological and population consistency within this subgroup (Figure 4).
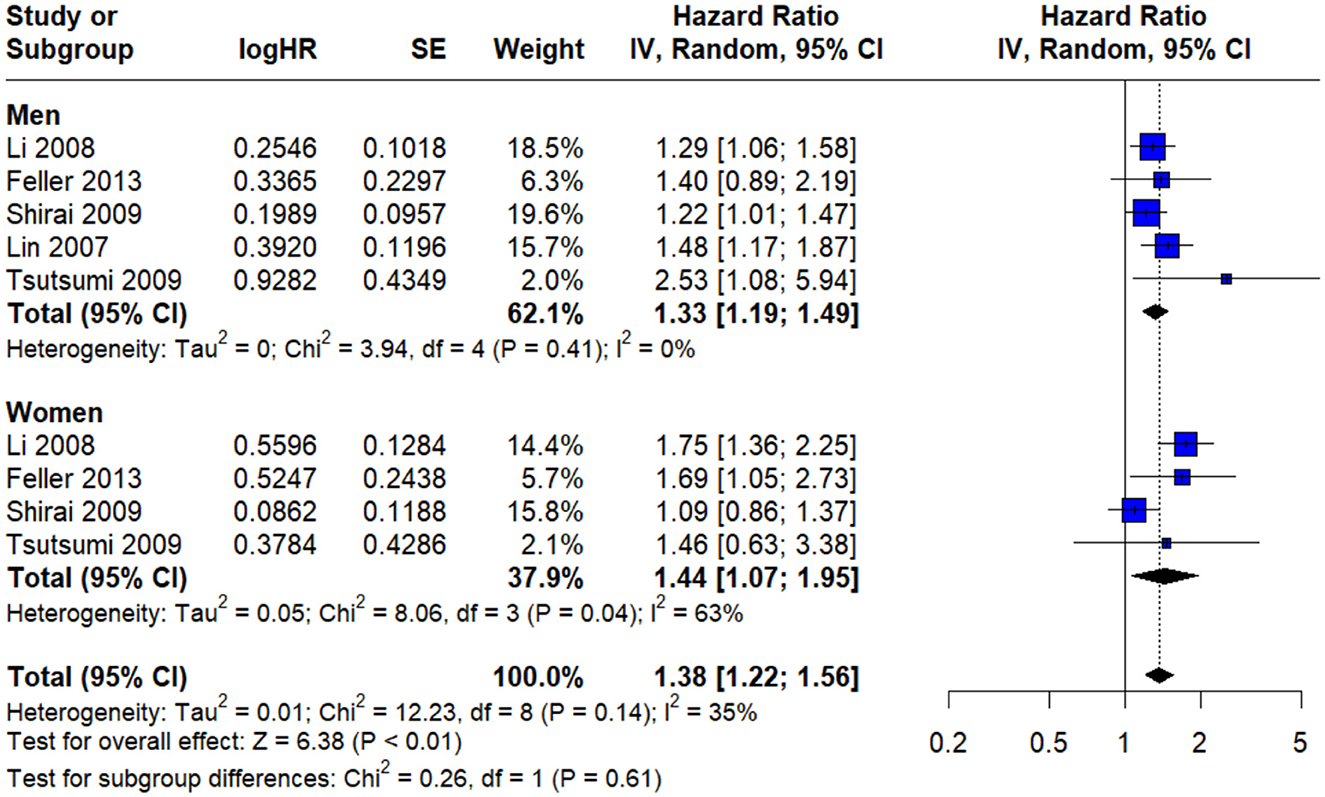
Figure 4. Gender subgroup allowing for a comparative analysis of the association between psychological stress and stroke risk in men and women.
Conversely, the analysis of female participants yielded a pooled HR of 1.44 (95% CI: 1.07–1.95), indicating a slightly stronger association. However, this estimate was accompanied by moderate heterogeneity (I2 = 63%). Despite the numerical difference in risk magnitude between men and women, the test for subgroup difference did not reach statistical significance (P = 0.61), suggesting that psychological stress exerts a comparable impact on stroke risk across males and females (Figure 4).
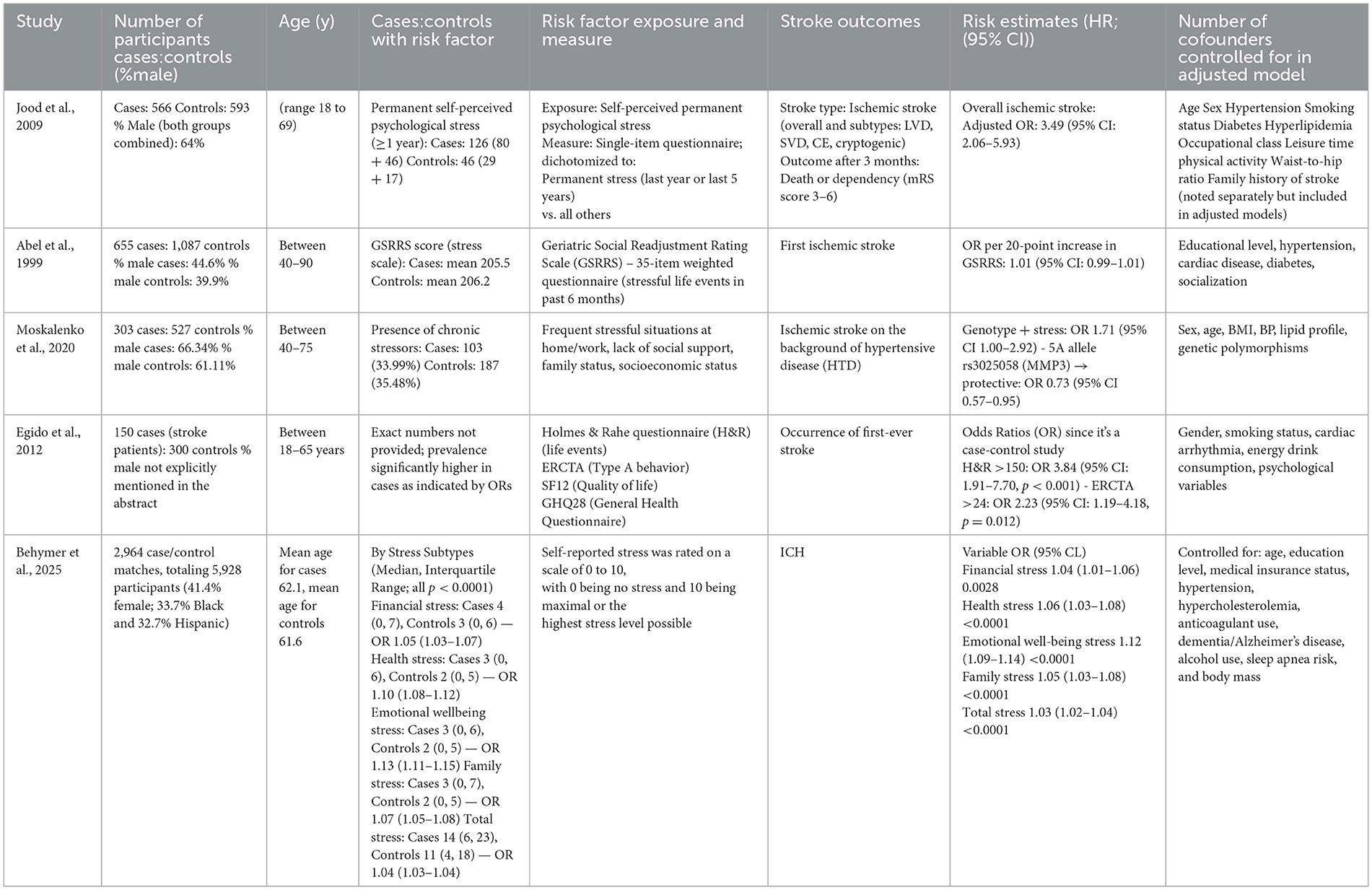
Three prospective cohort studies that specifically reported on fatal stroke events, the pooled hazard ratio (HR) was found to be 1.59 (95% CI: 1.19–2.12). This suggests that individuals experiencing psychological stress may have a 59% higher risk of dying from stroke, compared to their non-stressed counterparts accompanied by moderate heterogeneity (I2 = 38%) (Figure 5).
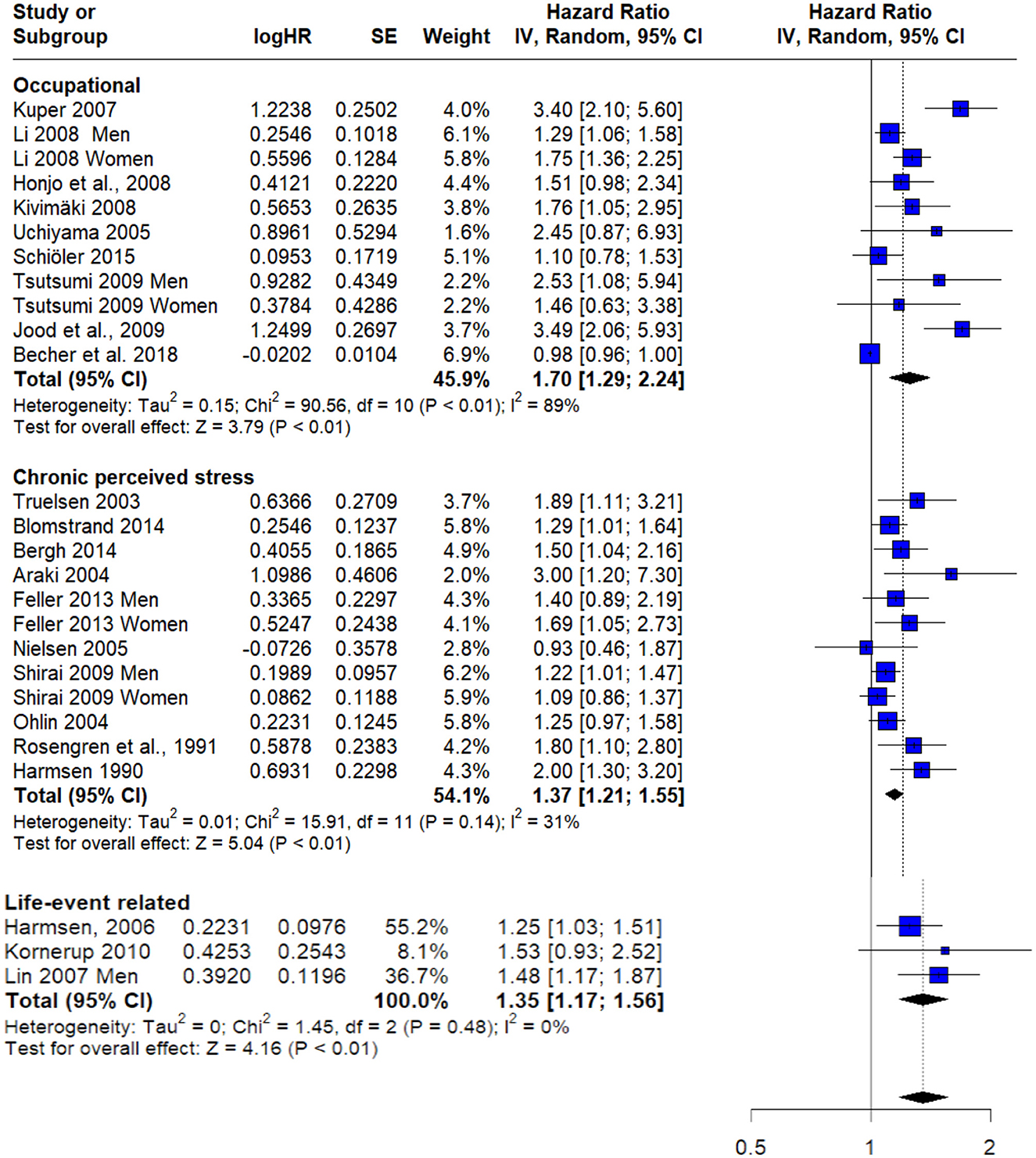
Stratified risk analysis by type of stress
Subgroup analysis revealed a statistically significant elevated risk among individuals exposed to occupational stress, with a pooled hazard ratio (HR) of 1.70 (95% CI: 1.29–2.24; I2 = 89%). Similarly, individuals experiencing chronic perceived stress demonstrated a significantly increased risk, with a pooled HR of 1.37 (95% CI: 1.21–1.55; I2 = 31%). Life-event related stressors were also associated with a higher risk, with a pooled HR of 1.35 (95% CI: 1.17–1.56; I2 = 0%) (Figure 6).
Co-founder adjustment
All 28 studies included in the analysis implemented multivariable models to control for potential confounding factors. Adjustment for age, smoking status, body mass index (BMI), and hypertension was reported in every study, providing a consistent baseline across the dataset.
In addition to these core variables, 25 studies adjusted for diabetes mellitus (18–40, 43), and 21 incorporated alcohol consumption as a covariate (9, 20, 22, 23, 25–27, 30–32, 34, 36, 39–41). Physical activity was included in the adjustment models of 21 studies (18, 20, 22, 23, 25–28, 30–36, 38–40), while blood lipid parameters, including serum cholesterol, were controlled for in 18 (20–23, 25–27, 30–33, 36, 38, 40, 41). These adjustments reflect a high level of methodological rigor in accounting for lifestyle and metabolic stroke risk factors.
Social determinants of health were also systematically considered. Specifically, 25 studies adjusted for socioeconomic indicators, including education, occupational status, or income level [all except (9, 40, 41)], recognizing their potential confounding influence in both psychological stress exposure and stroke risk. Additionally, 6 studies incorporated marital status or family structure as contextual variables reflecting social support (19, 20, 25, 28, 31, 35).
The consistency and breadth of confounder control across the included studies enhance the internal validity of the observed associations. While some variation in covariate selection reflects differences in study populations and data availability, the majority of studies demonstrated comprehensive methodological approaches to isolating the independent effect of psychological stress on stroke outcomes.
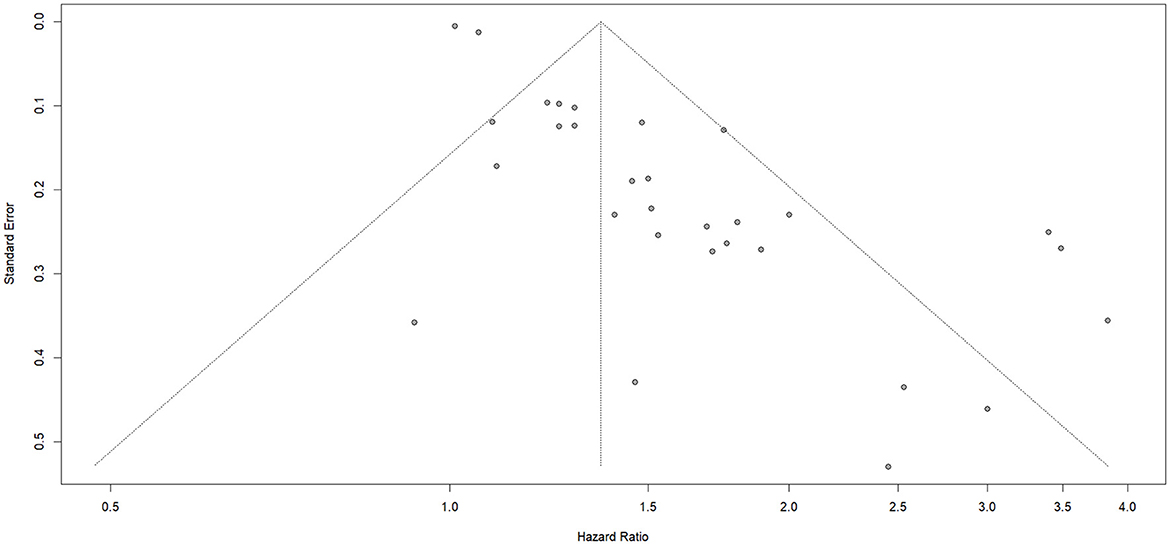
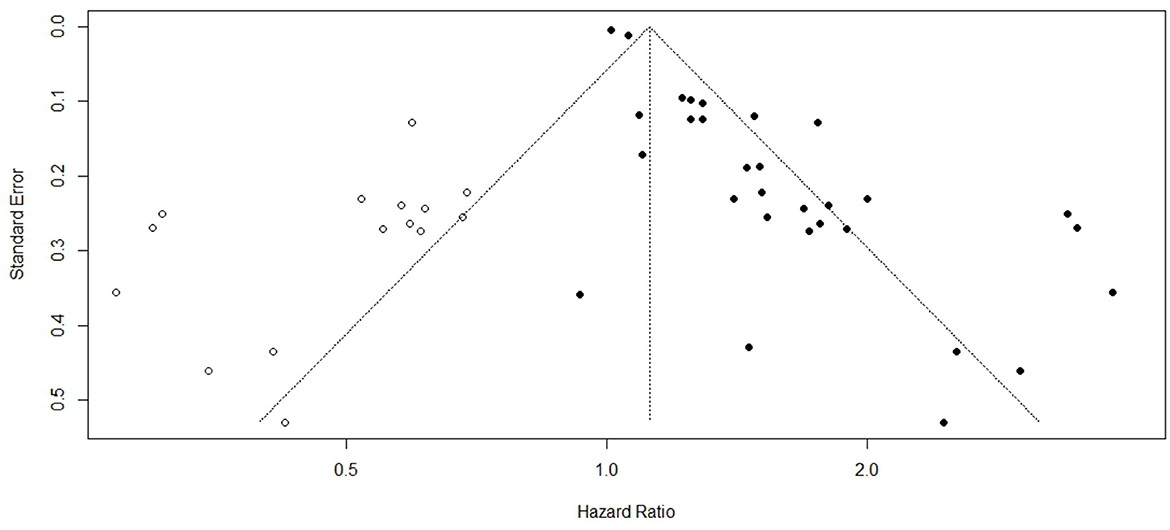
Publication bias
The potential for publication bias was examined to evaluate the reliability and completeness of the pooled estimates. Visual inspection of the funnel plot revealed noticeable asymmetry, suggesting the possibility of small-study effects or selective publication of positive findings. In order to statistically assess this visual impression, Egger's regression test was performed. The test yielded a highly significant result (p < 0.0001), confirming the presence of potential publication bias across the included studies (Figure 7). This result implies that smaller or non-significant studies may be underrepresented in the meta-analysis, potentially inflating the pooled estimates. To verify the validity of the study results, correction using Duval and Tweedie's trim-and-fill method was used. The corrected pooled hazard ratio (HR) obtained using the trim-and-fill method was 1.12 (95 % CI: 1.04-1.20; P = 0.002), which represented a reduction from the original hazard ratio of 1.46; however, the increase in risk of stroke in individuals experiencing psychological stress still statistically significant (Figure 8).
Discussion
Our systematic review and meta-analysis included 28 studies, 23 were prospective cohort studies and 5 were case–control studies, collectively encompassing a population of over 950,000 participants. We aim to assess the overall association between psychological stress and stroke risk across prospective cohort and case-control studies.
Our meta-analysis of prospective cohort studies found a 46% higher risk of stroke linked to psychological stress. This aligns with the findings from a recent systematic review and meta-analysis on psychosocial risk factors for stroke reported that “psychological factors” increased stroke risk by 39% (14). The consistent findings across studies strengthen the evidence that psychological stress is an independent and significant risk factor for stroke. Also, a meta-analysis using individual-level data that specifically focused on “job strain,” a widely studied measure of work-related stress, found a 24% higher risk of ischemic stroke after adjusting for age and sex (42). Given that occupational stress, including job strain, was one of the “various lenses” through which psychological stress exposure was defined in the current meta-analysis, this supports the link between work-related stressors and ischemic stroke. However, it is important to note that Becher et al. (20) was identified as a major source of heterogeneity. Therefore, a sensitivity analysis was performed after excluding this study. The observed heterogeneity can likely be explained by the relatively small sample size, the short follow-up duration, and the low incidence of circulatory diseases (i.e., stroke and myocardial infarction), which accounted for only about 8% of the total study population (20).
Conversely, the analysis of the five case-control studies included in our meta-analysis revealed a statistically significant 10% higher odds of experiencing stroke when exposed to psychological stress. However, the heterogeneity remained high in the analysis of case-control studies reflecting a weaker consistency and greater variability across studies. For example, in a case-control study (23) strong links between specific stress indicators have been found, where individuals with Holmes & Rahe values greater than 150 had 3.84 times the odds of developing an ischemic stroke and those with type A behavior had a 2.23 times the odds of having a stroke (23). Similarly, another case-control study (29), found that individuals who reported self-perceived psychological stress had 3.49 times the odds of developing an ischemic stroke (29). This observed discrepancy between the stronger associations reported in some individual case-control studies and the modest pooled effect from our meta-analysis warrants further critical examination. This could be explained by methodological variations in research design, including the vulnerability of case-control designs to recall bias, where stroke survivors may remember stressful experiences more easily than healthy controls
Given the variability in stress definitions and measurement tools across the included studies, we conducted subgroup analyses based on the type of stressor. Stress exposure was categorized into three groups: occupational stress, life-event-related stress, and chronic perceived stress. Our findings indicated that all stressor categories were significantly associated with stroke risk, with occupational stress showing the highest relative risk, followed by chronic perceived and life-event-related stress.
Furthermore, Our meta-analysis provided valuable sex-stratified findings, showing that psychological stress is significantly associated with increased odds of stroke in both sexes, with slight differences. Whereas for males we found a 33% higher odds of experiencing stroke when exposed to psychological stress, with no heterogeneity suggesting a consistent effect size across studies involving male participants. For females we found a 44% increased odds of stroke in the presence of psychological stress, but with moderate heterogeneity implying more variation across studies involving female participants. However, in our study the differences between the two sexes are statistically not significant, which indicate that psychological stress poses a comparable risk of stroke across sexes. Our findings are not consistent with the literature, where a meta-analysis conducted in 2015 concluded that females with perceived psychological stress have a 90% increased risk of stroke, whereas in males the risk is 24%, with females showing a greater vulnerability to stress-related stroke (8). This inconsistency between our findings and the 2015 meta-analysis could be due to differences in the effect estimates (e.g., odds ratios vs. hazard ratios), differences in the inclusion and selection criteria, or the definition and measurement of stress or the inconsistencies in the specific confounders adjusted for across studies. Furthermore, while our study suggests similar odds of stroke across sexes, we must consider the greater heterogeneity observed in female data which may have diluted the strength of the association. Also, not having a subgroup difference in our study does not exclude the possibility of sex-related association to higher vulnerability to stroke related to psychological stress.
A critical finding of our meta-analysis is the observed association between psychological stress and fatal stroke events. The pooled analysis from three prospective cohort studies indicated that individuals experiencing psychological stress had a 59% higher risk of dying from stroke (HR = 1.59; 95% CI: 1.19–2.12), with moderate heterogeneity suggesting some variability across studies. However, this result should be interpreted with caution due to the limited number of studies contributing to this analysis, which may reduce the precision and generalizability of the pooled estimate. Despite this, the direction of association aligns with previous literature. For example, a 2015 meta-analysis of 14 studies found that perceived psychological stress is associated with a 45% increased risk of fatal stroke (8) and the INTERSTROKE study reports similar findings of higher risk of all types of stroke, including fatal strokes when reporting high levels of self perceived psychological stress (2).
Additionally, Our meta-analysis identified a significant potential for publication bias, indicated by a noticeable asymmetry in the funnel plot and confirmed by a highly significant result from Egger's regression test (p < 0.0001). This finding implies the possibility of small-study effects or selective publication, where smaller studies with non-significant or negative findings may be underrepresented in the published literature and in the meta-analysis.
The observed publication bias suggests that the actual impact of psychological stress on stroke risk could be smaller than what the results show, especially since studies with little or no association may not have been published or included. This bias reflects a broader challenge in scientific publishing, where studies with statistically significant results are often more likely to be published, which can skew the overall evidence base. Despite this possibility for inflation, the consistent direction of the effect across multiple studies still carry a considerable weight to the conclusion that psychological stress is a risk factor for stroke.
Clinical and practical applicability of findings
Findings in our meta-analysis highlights the importance of psychological stress as a modifiable risk factor for stroke. These findings suggest that clinical protocols for stroke prevention need to incorporate more than the traditional focus of cardiovascular risk factors and consider a systematic assessment and management of psychological stress. The numerically stronger association observed in women, even if not statistically significant in subgroup analysis, warrants specific attention. It suggests that stress management interventions might be particularly beneficial or need to be tailored for female patients, given findings in other studies that showed higher stress associations with stroke in women. Also, future research should investigate the specific mechanisms by which psychological stress impacts stroke severity and mortality, potentially through the examination of biomarkers related to inflammation, coagulation, or neurovascular integrity, and further explore the role of stress-related behaviors and access to healthcare in mediating these effects.
Limitations
This meta-analysis has several limitations that should be considered when interpreting its findings.
First, there was considerable variability in how perceived psychosocial stress was measured, and a lack of a clear, specific, or standardized assessment. Additionally, no available data indicated whether stress levels remained consistent throughout the follow-up period, limiting our ability to distinguish between ongoing chronic stress and acute, short-term exposures. Furthermore, the use of single item self reported tools in some studies can affect the accuracy of the reported stress exposure leading to an increase in the risk of bias and subjectivity. Second, the observational nature of the both cohort and case-control studies can have few limitations of their own, although they show associations between stress and stroke, they can't prove a direct cause linking the two. Also, the presence of multiple confounders made it more complicated to isolate the effects of stress from other coexisting risk factors which may contribute to stroke risk.
Third, High statistical heterogeneity was observed, suggesting notable differences among study populations, methodologies, and stress definition making it difficult to achieve generalized conclusions. While we explored potential sources of heterogeneity through subgroup analyses, this variability makes it difficult to draw universally generalized conclusions from the pooled estimates alone.
Finally, the inclusion criteria, which sometimes involved selecting populations based on specific age, gender, or geographic regions, limit the overall generalizability of our findings
Restricting the inclusion criteria to studies that are only in English-language may have excluded other valuable research. Moreover, Egger's regression test showed potential publication bias, suggesting that smaller or non-significant studies might have been underrepresented, which could result in artificially higher pooled results.
Strengths
Key strengths of this meta-analysis are the inclusion of a large sample of over 950,000 individuals which enhances both the generalizability and statistical reliability of the results. Furthermore, an extensive literature search was conducted across multiple databases, which was crucial in limiting the omission of relevant studies.
Another notable strength was the extensive adjustment for multiple confounders within the included studies, such as age, BMI, smoking, hypertension, diabetes, alcohol consumption, physical activity, blood lipids, and socioeconomic indicators. This adjustment increases confidence in establishing an independent association between stress and stroke, supporting that the association observed is not an artifact of differences in health characteristics or demographics.
Future directions
To further advance the understanding of the relationship between psychological stress and stroke, future research should aim to address the limitations identified in this meta-analysis. Specifically, developing Standardized, consistent, validated tools for measuring perceived psychosocial stress are essential. as this will help researchers in achieving valid comparisons and identifying aspects of stress associated with the increased risk of stroke. Implementing regular and repeated measurements of perceived stress throughout the follow-up period, rather than a single baseline measurement would provide valuable insight into whether chronic, cumulative, or fluctuating stress exposure is most strongly associated with stroke occurrence. Further Broader inclusion criteria will help in highlighting cultural differences in how psychosocial stress is experienced and its effects on health thereby increasing the generalizability and relevance of future research findings.
Conclusion
Our meta-analysis confirms a consistent association between psychosocial stress and stroke incidence, with prospective studies showing approximately a 50% higher risk and case–control studies supporting this relationship. Although the increased risk was observed in both women and men, the slightly higher—but not statistically significant—odds among women warrant further investigation. Importantly, while our analysis also indicated an association between higher stress levels and fatal stroke events, this result should be interpreted cautiously due to the small number of available studies contributing to that estimate and the potential influence of publication bias. Overall, these findings emphasize the need to incorporate stress assessment and management into comprehensive stroke prevention and public health strategies.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
MK: Conceptualization, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. AAla: Conceptualization, Data curation, Project administration, Visualization, Writing – original draft, Writing – review & editing. GF: Conceptualization, Methodology, Writing – original draft, Writing – review & editing. AM: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. BT: Data curation, Methodology, Writing – original draft, Writing – review & editing. FA: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. MB: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. SAl: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. HA: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. HH: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. AAlq: Conceptualization, Data curation, Methodology, Writing – original draft, Writing – review & editing. SAh: Methodology, Writing – original draft, Writing – review & editing. SH: Writing – original draft, Writing – review & editing. OB-S: Writing – original draft, Writing – review & editing. DM: Methodology, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Feigin VL, Brainin M, Norrving B, Martins SO, Pandian J, Lindsay P, et al. World stroke organization: global stroke fact sheet 2025. Int J Stroke. (2025) 20:132–44. doi: 10.1177/17474930241308142
2. Reddin C, Murphy R, Hankey GJ, Judge C, Xavier D, Rosengren A, et al. Association of psychosocial stress with risk of acute stroke. JAMA Net Open. (2022) 5:e2244836. doi: 10.1001/jamanetworkopen.2022.44836
3. O'Donnell MJ, Chin SL, Rangarajan S, Xavier D, Liu L, Zhang H, et al. Global and regional effects of potentially modifiable risk factors associated with acute stroke in 32 countries (INTERSTROKE): a case-control study. Lancet. (2016) 388:761–75. doi: 10.1016/S0140-6736(16)30506-2
4. Ganster DC, Rosen CC. Work stress and employee health. J Manage. (2013) 39:1085–122. doi: 10.1177/0149206313475815
5. Kivimäki M, Kawachi I. Work stress as a risk factor for cardiovascular disease. Curr Cardiol Rep. (2015) 17:74. doi: 10.1007/s11886-015-0630-8
6. Schneiderman N, Ironson G, Siegel SD. Stress and health: psychological, behavioral, and biological determinants. Ann Rev Clin Psychol. (2005) 1:607–28. doi: 10.1146/annurev.clinpsy.1.102803.144141
7. Rosengren A, Hawken S, Ôunpuu S, Sliwa K, Zubaid M, Almahmeed WA, et al. Association of psychosocial risk factors with risk of acute myocardial infarction in 11 119 cases and 13 648 controls from 52 countries (the INTERHEART study): case-control study. Lancet. (2004) 364:953–62. doi: 10.1016/S0140-6736(04)17019-0
8. Booth J, Connelly L, Lawrence M, Chalmers C, Joice S, Becker C, et al. Evidence of perceived psychosocial stress as a risk factor for stroke in adults: a meta-analysis. BMC Neurol. (2015) 15:233. doi: 10.1186/s12883-015-0456-4
9. Behymer TP, Sekar P, Demel SL, Aziz YN, Coleman ER, Williamson BJ, et al. Psychosocial stress and risk for intracerebral hemorrhage in the ERICH (Ethnic/Racial Variations of Intracerebral Hemorrhage) study. J Am Heart Assoc. (2025) 14:e024457. doi: 10.1161/JAHA.121.024457
10. Khan M, Wasay M, O'Donnell MJ, Iqbal R, Langhorne P, Rosengren A, et al. Risk factors for stroke in the young (18–45 Years): a case-control analysis of INTERSTROKE data from 32 Countries. Neuroepidemiology. (2023) 57:275–83. doi: 10.1159/000530675
11. Kutal S, Tulkki LJ, Sarkanen T, Redfors P, Jood K, Nordanstig A, et al. Association between self-perceived stress and cryptogenic ischemic stroke in young adults. Neurology. (2025) 104:e213369. doi: 10.1212/WNL.0000000000213369
12. Maalouf E, Hallit S, Salameh P, Hosseini H. Depression, anxiety, insomnia, stress, and the way of coping emotions as risk factors for ischemic stroke and their influence on stroke severity: a case–control study in Lebanon. Front Psychiatry. (2023) 21:14. doi: 10.3389/fpsyt.2023.1097873
13. Sarfo FS, Ovbiagele B, Gebregziabher M, Akpa O, Akpalu A, Wahab K, et al. Unraveling the risk factors for spontaneous intracerebral hemorrhage among West Africans. Neurology. (2020) 94:e998–e1012. doi: 10.1212/WNL.0000000000009056
14. Lightbody C, Clegg A, Patel K, Lucas J, Storey H, Hackett M, et al. Systematic review and meta-analysis of psychosocial risk factors for stroke. Semin Neurol. (2017) 37:294–306. doi: 10.1055/s-0037-1603758
15. Mazure CM, Weinberger AH, Pittman B, Sibon I, Swendsen J. Gender and stress in predicting depressive symptoms following stroke. Cerebr Dis. (2014) 38:240–6. doi: 10.1159/000365838
16. Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA (2020) statement: an updated guideline for reporting systematic reviews. BMJ. (2021) 29:n71. doi: 10.1136/bmj.n71
17. Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D. Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA. (2000) 283:2008. doi: 10.1001/jama.283.15.2008
18. Araki A, Murotani Y, Kamimiya F, Ito H. Low well-being is an independent predictor for stroke in elderly patients with diabetes mellitus. J Am Geriatr Soc. (2004) 52:205–10. doi: 10.1111/j.1532-5415.2004.52055.x
19. Bergh C, Udumyan R, Fall K, Nilsagård Y, Appelros P, Montgomery S. Stress resilience in male adolescents and subsequent stroke risk: cohort study. J Neurol Neurosurg Psychiatry. (2014) 85:1331–6. doi: 10.1136/jnnp-2013-307485
20. Becher H, Dollard M, Smith P, Li J. Predicting circulatory diseases from psychosocial safety climate: a prospective cohort study from Australia. Int J Environ Res Public Health. (2018) 15:415. doi: 10.3390/ijerph15030415
21. Abel GA, Chen X, Boden-Albala B. Sacco RalphL. Social readjustment and ischemic stroke: lack of an association in a multiethnic population. Neuroepidemiology. (1999) 18:22–31. doi: 10.1159/000026192
22. Cook NR. Joint effects of sodium and potassium intake on subsequent cardiovascular disease. Arch Intern Med. (2009) 169:32. doi: 10.1001/archinternmed.2008.523
23. Egido JA, Castillo O, Roig B, Sanz I, Herrero MR, Garay MT, et al. Is psycho-physical stress a risk factor for stroke? A case-control study. J Neurol Neurosurg Psychiatry. (2012) 83:1104–11. doi: 10.1136/jnnp-2012-302420
24. Feller S, Teucher B, Kaaks R, Boeing H, Vigl M. Life satisfaction and risk of chronic diseases in the european prospective investigation into cancer and nutrition (EPIC)-Germany Study. PLoS One. (2013) 8:e73462. doi: 10.1371/journal.pone.0073462
25. Harmsen P, Rosengren A, Tsipogianni A, Wilhelmsen L. Risk factors for stroke in middle-aged men in Göteborg, Sweden. Stroke. (1990) 21:223–9. doi: 10.1161/01.STR.21.2.223
26. Harmsen P, Lappas G, Rosengren A, Wilhelmsen L. Long-term risk factors for stroke. Stroke. (2006) 37:1663–7. doi: 10.1161/01.STR.0000226604.10877.fc
27. Honjo K, Iso H, Inoue M, Tsugane S. Education, social roles, and the risk of cardiovascular disease among middle-aged Japanese Women. Stroke. (2008) 39:2886–90. doi: 10.1161/STROKEAHA.108.514067
28. Ikeda A, Iso H, Kawachi I, Yamagishi K, Inoue M, Tsugane S. Social support and stroke and coronary heart disease. Stroke. (2008) 39:768–75. doi: 10.1161/STROKEAHA.107.496695
29. Jood K, Redfors P, Rosengren A, Blomstrand C, Jern C. Self-perceived psychological stress and ischemic stroke: a case-control study. BMC Med. (2009) 7:53. doi: 10.1186/1741-7015-7-53
30. Kivimaki M, Theorell T, Westerlund H, Vahtera J, Alfredsson L. Job strain and ischaemic disease: does the inclusion of older employees in the cohort dilute the association? The WOLF Stockholm Study. J Epidemiol Commun Health. (2008) 62:372–4. doi: 10.1136/jech.2007.063578
31. Kornerup H, Osler M, Boysen G, Barefoot J, Schnohr P, Prescott E. Major life events increase the risk of stroke but not of myocardial infarction: results from the Copenhagen City Heart Study. Eur J Cardio Prevent Rehab. (2010) 17:113–8. doi: 10.1097/HJR.0b013e3283359c18
32. Kuper H, Adami HO, Theorell T, Weiderpass E. The socioeconomic gradient in the incidence of stroke. Stroke. (2007) 38:27–33. doi: 10.1161/01.STR.0000251805.47370.91
33. Lahti M, Tiihonen J, Wildgust H, Beary M, Hodgson R, Kajantie E, et al. Cardiovascular morbidity, mortality and pharmacotherapy in patients with schizophrenia. Psychol Med. (2012) 42:2275–85. doi: 10.1017/S0033291712000396
34. Li C, Hedblad B, Rosvall M, Buchwald F, Khan FA, Engström G. Stroke incidence, recurrence, and case-fatality in relation to socioeconomic position. Stroke. (2008) 39:2191–6. doi: 10.1161/STROKEAHA.107.507756
35. Moskalenko MI, Ponomarenko IV, Polonikov AV, Zhernakova NI, Efremova OA, Churnosov MI. The role of stress factors and genetic predisposition in the development of stroke in patients with essential hypertension. Zh Nevrol Psikhiatr Im S S Korsakova. (2019) 119:11. doi: 10.17116/jnevro201911903211
36. Nielsen NR, Truelsen T, Barefoot JC, Johnsen SP, Overvad K, Boysen G, et al. Is the effect of alcohol on risk of stroke confined to highly stressed persons? Neuroepidemiology. (2005) 25:105–13. doi: 10.1159/000086352
37. Öhlin B. Chronic psychosocial stress predicts long-term cardiovascular morbidity and mortality in middle-aged men. Eur Heart J. (2004) 25:867–73. doi: 10.1016/j.ehj.2004.03.003
38. Truelsen T, Nielsen N, Boysen G, Grønbæk M. Self-reported stress and risk of stroke. Stroke. (2003) 34:856–62. doi: 10.1161/01.STR.0000062345.80774.40
39. Uchiyama S, Kurasawa T, Sekizawa T, Nakatsuka H. Job strain and risk of cardiovascular events in treated hypertensive japanese workers: hypertension follow-up group study. J Occup Health. (2005) 47:102–11. doi: 10.1539/joh.47.102
40. Lin HC, Tsai SY, Lee HC. Increased risk of developing stroke among patients with bipolar disorder after an acute mood episode: a six-year follow-up study. J Affect Disord. (2007) 100:49–54. doi: 10.1016/j.jad.2006.09.016
41. Shirai K, Iso H, Ohira T, Ikeda A, Noda H, Honjo K, et al. Perceived level of life enjoyment and risks of cardiovascular disease incidence and mortality. Circulation. (2009) 120:956–63. doi: 10.1161/CIRCULATIONAHA.108.834176
42. Fransson EI, Nyberg ST, Heikkilä K, Alfredsson L, Bjorner JB, Borritz M, et al. Job strain and the risk of stroke. Stroke. (2015) 46:557–9. doi: 10.1161/STROKEAHA.114.008019
Keywords: stress, stroke, psychosocial, meta-analysis, observational studies
Citation: Khalifa MA, Alardhi AS, Alharbi GFS, Mousa M. Alzahrani A, Taqi BA, Alsalman FS, Basher G. Albalawi M, Alzahrani SA, Abul HH, Hassan HS, Alqarni ADN, Ahmed SSK, Hegazy SM, Bin-Sahel OHA and Mohamed DA (2025) Psychosocial stress and stroke risk: meta-analysis of observational studies. Front. Neurol. 16:1669925. doi: 10.3389/fneur.2025.1669925
Received: 20 July 2025; Accepted: 10 October 2025;
Published: 06 November 2025.
Edited by:
Patricia Pia Wadowski, Medical University of Vienna, AustriaReviewed by:
Nour S. Erekat, Jordan University of Science and Technology, JordanAna Isabel Fumagalli, Sanatorio Parque Rosario Argentina, Argentina
Copyright © 2025 Khalifa, Alardhi, Alharbi, Mousa M. Alzahrani, Taqi, Alsalman, Basher G. Albalawi, Alzahrani, Abul, Hassan, Alqarni, Ahmed, Hegazy, Bin-Sahel and Mohamed. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mostafa A. Khalifa, bW9zdGFmYWtoYWxpZmEyODJAZ21haWwuY29t
†ORCID: Mostafa A. Khalifa orcid.org/0009-0009-7199-3939
Albandari Sultan Alardhi orcid.org/0009-0008-9680-8608
Ghadah Faleh S. Alharbi orcid.org/0009-0000-7616-1431
Abdulmajeed Mousa M. Alzahrani orcid.org/0000-0001-7954-5107
Batoul Ali Taqi orcid.org/0009-0009-4181-1858
Falwah Sami Alsalman orcid.org/0009-0007-1182-7934
Mohand Basher G. Albalawi orcid.org/0000-0001-5485-5029
Saleh Ahmed Alzahrani orcid.org/0009-0001-7358-2588
Hessah Haji Abul orcid.org/0009-0006-6480-9054
Hayat Safwat Hassan orcid.org/0009-0001-5004-7021
Ashwaq Dhafer N. Alqarni orcid.org/0009-0004-7069-7648
Shaima ShamsEldeen KhalfAllah Ahmed orcid.org/0009-0000-1853-8720
Sarah M. Hegazy orcid.org/0009-0009-8928-7987
Omer Hussein Alwi Bin-Sahel orcid.org/0009-0007-7657-2418
Dalia Abdalla Mohamed orcid.org/0009-0007-9676-9859
 Mostafa A. Khalifa
Mostafa A. Khalifa Albandari Sultan Alardhi2†
Albandari Sultan Alardhi2† Ghadah Faleh S. Alharbi
Ghadah Faleh S. Alharbi Falwah Sami Alsalman
Falwah Sami Alsalman Saleh Ahmed Alzahrani
Saleh Ahmed Alzahrani Hessah Haji Abul
Hessah Haji Abul Omer Hussein Alwi Bin-Sahel
Omer Hussein Alwi Bin-Sahel