Abstract
Background:
Migraine is a common disabling neurological disorder that affects the quality of human daily life and mental health, potentially leading to disability and imposing a substantial disease burden. There is currently a lack of literature analysis on the global burden and changing trends of migraines. Therefore, this study is of great significance for the development of effective management and prevention strategies for migraine by analyzing the global burden of migraine and its changing trends.
Methods:
We obtained data on the incidence, prevalence, and disability-adjusted life years (DALYs) of migraine by region and year from the Global Burden of Disease Study 2021 (GBD 2021). The estimated annual percentage change (EAPC) and 95% confidence interval (CI) were used to evaluate the time trend of disease burden, and factors that may affect the EAPC were analyzed. The burden of migraine was analyzed based on the Socio-demographic Index (SDI). Frontier analysis was used to visually demonstrate the burden of development levels in various regions, and the trends of migraine incidence, prevalence, and DALYs over the next decade were predicted.
Results:
In 2021, the global number of prevalent cases, incident cases, and DALYs for migraine were 1.158 billion, 90.18 million, and 43.38 million, compared with 1990, the percentage changes were 58, 42, and 58%, respectively. In 2021, the age-standardized incidence rate (ASIR), age-standardized prevalence rate (ASPR), and age-standardized DALY rate (ASDR) of migraine were the highest in areas with high SDI. Its prevalence, incidence, and DALYs were 15365.1, 1222.5, and 573.6 per 100,000 people. From 1990 to 2021, the ASDR showed an upward trend globally and in all regions, among which ASIR and ASPR in global, China, East Asia, high, high-middle SDI regions were on the rise, while they showed a downward trend in low, low-middle SDI regions. Frontier analysis showed that areas with high SDI generally had greater potential for improvement. We used a predictive model to estimate that ASIR, ASPR, and ASDR of migraine were all on the rise.
Conclusion:
From 1990 to 2021, the global burden of migraine has increased significantly, especially in middle SDI region. This study highlights the importance of tailored interventions aimed at addressing migraine and thus contributing to the achievement of the Sustainable Development Goals set by the World Health Organization.
1 Introduction
Migraine is a common chronic neurovascular dysfunction disease, ranking as the third most disabling condition in the nervous system (1). It is characterized by recurrent unilateral or bilateral pulsatile pain, sensitivity to sound and light stimuli, accompanied by nausea, vomiting, and other symptoms. It has a high recurrence rate, affecting the quality of human daily life and mental health, and can even lead to disability in severe cases. Migraine demonstrates established comorbidities with anxiety, depression, and sleep disorders, while significantly elevating the risk of cognitive dysfunction and cardiovascular/cerebrovascular diseases (2). Furthermore, evidence confirms associations with increased susceptibility to asthma, stroke, and other pain-related conditions (3, 4). These factors collectively establish migraine as a substantial public health challenge that inflicts considerable patient suffering and imposes major socioeconomic burdens (3).
The Global Burden of Disease Study 2021 (GBD 2021) provides the latest data on migraine diseases covering 204 countries and regions worldwide from 1990 to 2021 (5). This latest iteration incorporates expanded data sources and methodological refinements that enhance estimation accuracy. While the GBD 2019 report highlighted migraine’s significant contribution to disability-adjusted life years (DALYs), particularly among the 10–49 age group where it represents a leading cause of disability (6). For the diagnosis and treatment of migraine, the ideal situation is to follow internationally recognized recommendations and establish a layered medical service provision structure. However, in reality, significant obstacles are encountered. In most countries around the world, headache patients fail to receive standardized treatment due to insufficient medical system resources. Furthermore, the COVID-19 pandemic has further exacerbated these inequalities (7). Therefore, this study analyzes the incidence, prevalence, and DALYs of migraine through GBD 2021, predicts its trend, and aims to comprehensively evaluate the global disease burden of migraine from 1990 to 2021. Compared with previous GBD studies, this study integrates more available data sources and provides more accurate estimation results through improved methodology. It is expected to serve as an important extension and supplement to the aforementioned research, helping healthcare workers to have a deeper understanding of migraine and providing a scientific basis for policymakers to improve resource allocation and develop effective health strategies.
Building upon previous important work documenting migraine burden, the evolving data landscape and global context necessitate continued assessment. The Global Burden of Disease Study 2021 provides updated estimates through 2021, capturing the initial phase of the COVID-19 pandemic—a crucial period for understanding this global health crisis’s impact on chronic disease management, including migraine (8). While confirming established patterns of migraine burden from earlier reports, our study extends this work by systematically examining heterogeneity in disease burden across Socio-demographic Index (SDI) regions and projecting future trends using frontier analysis. Through extended temporal analysis (1990–2021) and SDI-stratified interpretation, our findings provide updated epidemiological evidence with enhanced granularity to inform targeted migraine prevention and control strategies globally.
2 Methods
2.1 Disease definition and data sources
According to the GBD 2021, migraine is defined as a disabling primary headache disorder characterized by recurrent moderate to severe pulsatile unilateral headache. In GBD 2021, we do not distinguish between migraine with aura and migraine without aura because most epidemiological studies only report overall migraine data. If a patient’s symptoms meet the five diagnostic criteria proposed by the International Classification of Headache Disorders, Third Edition (ICHD-3), they can be diagnosed with migraine. According to the 9th and 10th editions of the International Classification of Diseases (ICD), migraine is represented by codes 346–346.93 and G43-G43.919, respectively (5).
This study used anonymized data from the GBD 2021, a comprehensive database covering the impact of 371 diseases, 88 risk factors, and injuries in 5 Socio-demographic Index (SDI) groups and 204 countries and regions. The information is available at the following URL: http://ghdx.healthdata.org/gbd-results-tool. Detailed information on relevant data, methods, and statistical modeling can be found in previous reports (8). We obtained migraine incidence, prevalence, and DALYs data by region and year from the GBD 2021. The estimated annual percentage change (EAPC) and 95% confidence interval (CI) were used to evaluate the time trend of disease burden. The migraine related burden was analyzed based on the Socio-demographic Index (SDI), a comprehensive indicator that measures education, economy, and fertility levels, emphasizing the interconnection between social development and population health outcomes. Frontier analysis was further applied to evaluate the relationship between migraine burden and socio-demographic development. Subsequently, we extracted the corresponding predicted population to forecast the global migraine age-standardized incidence rate (ASIR), age-standardized prevalence rate (ASPR), and age-standardized DALY rate (ASDR) for the next 10 years.
2.2 Statistical analysis
This study calculated the EAPC to describe the ASR trend of migraine burden. If both the EAPC value and the lower limit of its 95% confidence interval are greater than 0, it indicates an upward trend in ASR. If these values are less than 0, it indicates a downward trend. If the EAPC is equal to 0, it indicates a constant trend. All data analyses in this study were performed in R software (version 4.2.2) and RStudio, and a p-value <0.05 was considered statistically significant.
3 Results
3.1 Global level
Globally, there has been a significant increase in the number of prevalent cases, incident cases, and DALYs for migraine. For instance, migraine prevalent cases rose from 732.56 million in 1990 to 1.15843 billion in 2021, representing a 58% increase. The number of incident cases rose from 63.5 million in 1990 to 90.18 million in 2021, representing a 42% increase. Similarly, DALYs cases rose from 27.41 million in 1990 to 43.38 million in 2021, also a 58% increase (Tables 1–3 and Figure 1). The global prevalence rate, incidence rate, and DALYs rate of migraine have all climbed from 1990 to 2021, with EAPC of 0.05 (95% CI: 0.04–0.06), 0.05 (95% CI: 0.03–0.07), and 0.04 (95% CI: 0.04–0.04) respectively. This indicates a persistent and profound increase in the global burden of migraine.
Table 1
| Number | Location | Number (1990) | ASR per 100,000 (1990) | Number (2021) | ASR per 100,000 (2021) | EAPC (CI) |
|---|---|---|---|---|---|---|
| 1 | China | 133474536.5 (114199443.7–153482597.7) | 10948.5 (9428.8–12586.1) | 184752280.1 (160836524.7–213633958.3) | 11777.5 (10137.6–13538.6) | 0.24 (0.23–0.24) |
| 2 | East Asia | 138666855.2 (118605236.2–159459078.7) | 10993.2 (9469–12636.8) | 191704023.9 (166846937.8–221713278.7) | 11798.4 (10162.5–13,567) | 0.23 (0.23–0.23) |
| 3 | Global | 732564462.7 (624559243.9–847058436.3) | 14027.6 (12063.4–16078.1) | 1158432823.8 (995861966.4–1331312506.1) | 14246.5 (12194.1–16378.7) | 0.05 (0.03–0.07) |
| 4 | High SDI | 142911565.2 (124064905–163809089.4) | 15286.9 (13196.4–17504.2) | 175424403.7 (153279198.8–201,895,737) | 15365.1 (13250.3–17765.4) | 0.01 (−0.13–0.14) |
| 5 | High-middle SDI | 146640057.8 (125805580.8–168593873.1) | 13250.6 (11372.4–15230.6) | 191802656.3 (167163077.2–220,197,711) | 13502.7 (11610.1–15484.7) | 0.06 (0.06–0.07) |
| 6 | Low SDI | 54342303.5 (45978743.5–63691837.1) | 12809.1 (10955.4–14788.5) | 129654870.3 (109563874.3–152432455.6) | 12,809 (10909.3–14754.4) | 0 (−0.03–0.02) |
| 7 | Low-middle SDI | 157234783.9 (133322760.3–182843387.7) | 14823.8 (12712.9–17056.2) | 288676927.2 (246439632.7–332108194.8) | 14,787 (12677.1–16,979) | −0.01 (−0.05–0.03) |
| 8 | Middle SDI | 230715534.9 (195772574.5–267365243.4) | 13590.8 (11682.7–15580.9) | 371941648.1 (319831620.3–426895953.9) | 14344.2 (12233.4–16477.3) | 0.18 (0.16–0.19) |
Global and regions prevalence of migraine from 1990 to 2021.
Table 2
| Number | Location | Number (1990) | ASR per 100,000 (1990) | Number (2021) | ASR per 100,000 (2021) | EAPC (CI) |
|---|---|---|---|---|---|---|
| 1 | China | 11518097.6 (10091942.1–13156841.9) | 917.3 (808.4–1,037) | 13047220.7 (11597731.5–14698852.1) | 975.6 (862.3–1102.1) | 0.2 (0.19–0.2) |
| 2 | East Asia | 11956378.8 (10465336.6–13649232.3) | 921 (810.9–1041.6) | 13524742.6 (12000699.7–15250401.1) | 976.9 (863.3–1,104) | 0.19 (0.19–0.19) |
| 3 | Global | 63496590.8 (55194751.5–72208003.4) | 1136.9 (995.1–1287.8) | 90183386.9 (78857600.5–101838162.5) | 1153.2 (1006.1–1304.5) | 0.05 (0.04–0.06) |
| 4 | High SDI | 10193796.2 (8908219.3–11542805.2) | 1200.5 (1044.7–1359.7) | 11294915.5 (9902278.8–12786995.5) | 1222.5 (1070.6–1388.6) | 0.05 (−0.08–0.17) |
| 5 | High-middle SDI | 11546733.7 (10130462.1–13148277.8) | 1056.8 (920.6–1201.7) | 13060790.8 (11423422.8–14774640.4) | 1087.1 (951.7–1233.3) | 0.09 (0.06–0.13) |
| 6 | Low SDI | 5490327.4 (4696368.4–6408793.2) | 1047.9 (909–1192.8) | 12662944.1 (10811145–14650313.1) | 1,046 (905.2–1193.5) | −0.01 (−0.03–0.02) |
| 7 | Low-middle SDI | 15222630.5 (13175203.1–17497048.4) | 1220.6 (1066.8–1377.8) | 24656879.9 (21420024.1–27993901.8) | 1213.3 (1057.8–1372.5) | −0.02 (−0.06–0.01) |
| 8 | Middle SDI | 20983717.3 (18289662.7–23872475.4) | 1129.4 (987.4–1,276) | 28437798.3 (25055734.6–32051775.7) | 1173.2 (1027.7–1322.8) | 0.13 (0.06–0.2) |
Global and regions incidence of migraine from 1990 to 2021.
Table 3
| Number | Location | Number (1990) | ASR per 100,000 (1990) | Number (2021) | ASR per 100,000 (2021) | EAPC (CI) |
|---|---|---|---|---|---|---|
| 1 | China | 5028787.5 (767668.5–11262271.4) | 413 (66.2–911) | 6988198.6 (1133318.7–15186289.3) | 443.7 (66.9–971.7) | 0.23 (0.23–0.23) |
| 2 | East Asia | 5223002.7 (792490.7–11671556.1) | 414.5 (65.9–912.6) | 7248392.4 (1171602.6–15744802.5) | 444.3 (66.8–971.8) | 0.22 (0.22–0.23) |
| 3 | Global | 27412196.3 (4076605–60325805.8) | 526.8 (83.4–1145.9) | 43378889.8 (6732642.2–95079454.1) | 532.7 (80.6–1167.7) | 0.04 (0.04–0.04) |
| 4 | High SDI | 5,376,701 (896805.6–11550290.6) | 573.4 (91.4–1243.2) | 6613112.3 (1212857.1–14047722.3) | 573.6 (89.8–1,236) | −0.01 (−0.1–0.08) |
| 5 | High-middle SDI | 5657198.1 (1090025.3–12056696.2) | 511.7 (99.7–1085.8) | 7409676.3 (1474226.7–15665836.9) | 517.6 (92.9–1103.3) | 0.04 (0.01–0.07) |
| 6 | Low SDI | 1989610.8 (284626.4–4460947.3) | 472.4 (76.2–1018.8) | 4782245.5 (672592.6–10758550.4) | 475.2 (76.4–1031.5) | 0.02 (0.01–0.03) |
| 7 | Low-middle SDI | 5750275.1 (691692.1–12804149.2) | 543.9 (73.7–1198.3) | 10,617,257 (1368932.8–23440099.6) | 544.2 (73.9–1201.9) | 0 (−0.03–0.03) |
| 8 | Middle SDI | 8611314.2 (1117747.6–19168775.6) | 508.5 (72.1–1119.5) | 13921317.3 (2023382.9–30,544,094) | 535.9 (74.8–1178.3) | 0.17 (0.15–0.19) |
Global and regions DALYs of migraine from 1990 to 2021.
Figure 1

Global map of ASIR, ASPR, and ASDR of migraine for 204 countries and regions in 2021 (A: ASIR, B: ASPR, C: ASDR).
In East Asia, prevalent cases rose from 138.67 million in 1990 to 191.7 million in 2021, representing a 38% increase. In China, the number rose from 133.47 million to 184.75 million, representing a 38% increase. Incident cases In East Asia rose from 11.96 million in 1990 to 13.52 million in 2021, representing a 13% increase. Specifically, in China, the number rose from 11.52 million to 13.05 million, also representing a 13% increase. DALYs cases in East Asia rose from 5.22 million to 7.25 million, representing a 39% increase, while in China, they rose from 5.03 million to 6.99 million, also representing a 39% increase. China, accounting for approximately 85% of the total population in East Asia, mirrors the regional trends in disease burden. The EAPC for incidence rate, prevalence rate, and DALYs rate in East Asia were 0.19 (95% CI: 0.19–0.19), 0.23 (95% CI: 0.23–0.23), and 0.22 (95% CI: 0.22–0.23) respectively, while in China, they were 0.20 (95% CI: 0.19–0.20), 0.24 (95% CI: 0.23–0.24), and 0.23 (95% CI: 0.23–0.23), indicating a significant rise in disease burden in both East Asia and China.
3.2 SDI regional level
In 2021, the highest numbers of prevalent, incident, and DALY cases of migraine were observed in regions with middle SDI, reaching 371941648.1 (95% CI: 319831620.3–426895953.9), 28437798.3 (95% CI: 25055734.6–32051775.7), and 13921317.3 (95% CI: 2023382.9–30,544,094) respectively. These cases accounted for approximately 30% of the global total. In 2021, the ASPR, ASIR, and ASDR of migraine were highest in high SDI regions (Tables 1–3). The prevalence, incidence, and DALYs rates were 15365.1, 1222.5, and 573.6 per 100,000 people, respectively. Significant percentage changes were observed in the number of prevalent and incident cases in Low-middle SDI regions, but the prevalence and incidence rates showed a downward trend. The largest percentage changes were seen in low SDI regions (around 130–140%), while the smallest changes occurred in high SDI regions (around 11–23%). Notably, from 1990 to 2021, middle SDI regions experienced rapid growth in prevalence, incidence, and DALY rates, with EAPC of 0.18 (95% CI: 0.16–0.19), 0.13 (95% CI: 0.06–0.2), and 0.17 (95% CI: 0.15–0.19) respectively. Additionally, in 2021, middle SDI regions exhibited relatively higher prevalence, incidence, and DALYs. Therefore, middle SDI regions have the highest number of migraine cases, with the fastest growth rate compared to 1990, resulting in the highest EAPC for these rates.
3.3 Factors influencing the EAPC in the burden of migraine disease
To better interpret the GBD2021 for migraine, this study analyzed factors that could potentially affect the EAPC, including ASIR, ASPR, and ASDR (Figure 2). As shown in Figure 2A, the relationship between EAPC and ASR is not a simple linear correlation. In 1990, there was a significant positive correlation between EAPC and ASIR, ASPR, and ASDR (r = 0.5872, 0.6385, 0.6731, p-values <0.05). However, in 2021, although there was a moderate correlation between EAPC and ASR (r = 0.4128, 0.4557, 0.4968), the p-value was greater than 0.05, indicating that this correlation was not statistically significant (Figure 2B).
Figure 2

Correlation of ASIR, ASPR, and ASDR for migraine with EAPC in 1990 and 2021 (A: 1990, B: 2020, from left to right, ASIR, ASPR, and ASDR).
3.4 The correlation between the burden of migraine and SDI
In 2021, a positive correlation was observed between the prevalence, incidence, and DALY rates of migraine and the SDI. As economic conditions improved, the overall disease burden showed an upward trend. Specifically, when the SDI value ranged from 0.625 to 0.75, the ASIR burden of migraine exhibited a decline, followed by a significant increase in disease burden alongside rising SDI. Similarly, the ASPR demonstrated a downward trend when the SDI value was between 0.625 and 0.7, with a subsequent continuous escalation in disease burden. The ASDR also showed a downward trend when the SDI value was between 0.6 and 0.7. Notably, the ASIR burden of migraine exceeded expectations in Belgium, Italy, Spain, Brazil, and Paraguay, while it was lower than anticipated in Somalia, Djibouti, Ethiopia, and Singapore (Figure 3).
Figure 3

ASPR, ASIR, and ASDR by SDI of migraine in 204 countries and regions (A: ASPR, B: ASIR, and C: ASDR).
3.5 Frontier analysis of ASPR, ASIR, and ASDR for migraine in 2021
This study employs frontier analysis to illustrate the health gains across countries or regions with varying levels of development from 1990 to 2021. The findings reveal the unrealized health gains in countries or regions due to various reasons (such as policies, health systems, environmental factors, etc.) that have prevented them from fully utilizing their potential and achieving optimal health improvements. In 2021, the ASPR, ASIR and ASDR burden, as well as effective disparities, progressively increased with the SDI development across countries or regions with different sociodemographic levels (Figure 4). Generally, as sociodemographic development progresses, effective disparities among countries or regions have widened, indicating that countries or regions with a higher SDI have greater potential for burden improvement. There is still room for improvement in achieving health equity, effectively implementing disease prevention and management, and enhancing the quality of health services.
Figure 4

Frontier analysis of ASPR, ASIR, and ASDR for migraine based on SDI in 2021 (A: ASPR, B: ASIR, and C: ASDR).
3.6 Future predictions of the global disease burden of migraine
This study presents the predicted trends for the future burden of migraine. The findings reveal an upward trajectory in the ASPR, ASIR, and ASDR of migraine globally. Specifically, the ASPR is expected to rise significantly from 2022 to 2025, followed by a steady but continued increase between 2025 and 2031 (Figure 5A). Similarly, the ASIR demonstrates a notable upward trend from 2022 to 2025, with a period of stabilization between 2025 and 2028, subsequently resuming its upward climb (Figure 5B). Regarding the ASDR, a significant increase is anticipated from 2022 to 2025, followed by a slight decrease and then a leveling off between 2028 and 2031 (Figure 5C).
Figure 5
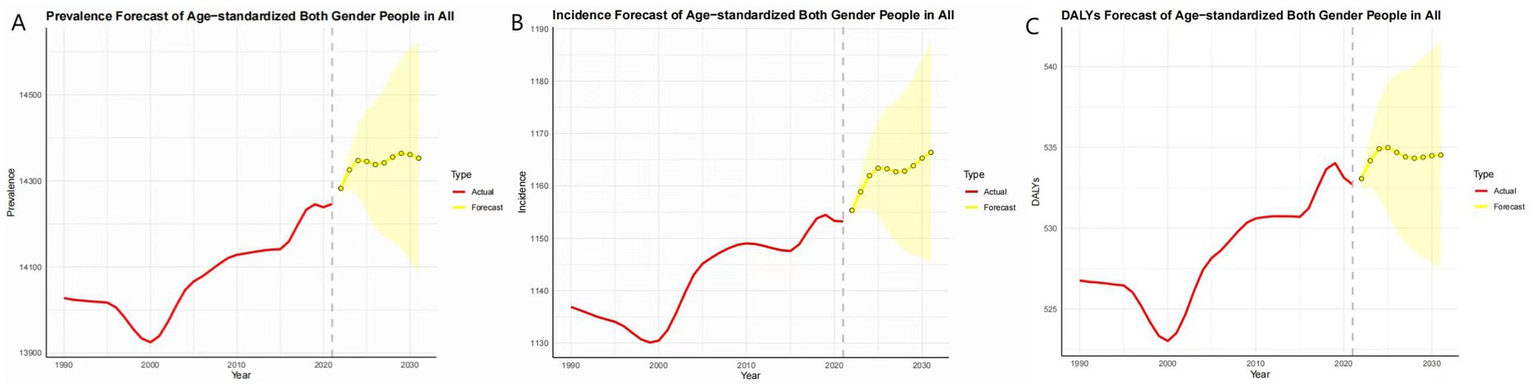
Trend of ASPR, ASIR, and ASDR for migraine from 2021 to 2031 (A: ASPR, B: ASIR, and C: ASDR).
4 Discussion
Our analysis reveals distinct patterns of migraine burden across the socioeconomic spectrum. While high-SDI regions exhibited the highest ASIR, ASPR, and ASDR, it is the middle-SDI regions that emerge as the epicenter of the growing epidemic, bearing the highest absolute number of cases and demonstrating the most rapid growth in ASRs. This divergence highlights the complex interplay between development, healthcare access, and disease risk. This pattern of increasing burden in developing regions aligns with the concept of the ‘fourth stage of epidemiologic transition’, characterized by the rising prominence of non-fatal but disabling chronic conditions as societies develop (9). Our findings that migraine burden escalates specifically in middle-SDI settings are consistent with broader empirical evidence of complex health transitions in low- and middle-income countries (10). This transition is particularly evident for neurological disorders, which are now recognized as a leading and growing cause of disability worldwide, especially in developing regions (11). The rapid urbanization and adoption of lifestyle-related risk factors in these transitioning economies, which are well-established drivers of chronic disease mortality and morbidity (12), likely represent key mechanisms underlying the observed rise in migraine incidence and burden. However, ASIR and ASPR showed a downward trend in low and low-middle SDI regions. Despite the sharp increase in global migraine cases over the past 31 years, ASIR, ASPR, and ASDR did not demonstrate a rapid growth trend. This slow growth is consistent with our findings for the EAPC.
SDI is a composite index based on the total fertility rate of women under 25, lag-distributed income, and average education level among those aged 15 and above (13). Our study suggests that regions with high SDI levels have the highest ASR for migraine, while middle SDI regions bear the highest number of cases, EAPC, and percentage change in case counts. This could be attributed to the rapid urbanization and modernization processes in middle-income regions, accompanied by higher work stress, faster-paced lifestyles, and rapid changes in the social environment. These factors include sedentary lifestyles, stress, lack of physical activity, excessive use of medications and electronic devices, and deteriorating sleep patterns (14). Additionally, with the improvement of healthcare systems in middle-income countries, the diagnosis rate of migraine has increased. Enhanced public health awareness has led to greater recognition and acceptance of migraine, resulting in more people seeking medical help and consequently, an increase in diagnosed migraine cases (15). This contributes to the rise in migraine prevalence, case counts, and ASR. Furthermore, our study observed significant growth in the number of affected and incident cases in low-middle and low SDI regions, but the ASPR, and ASIR declined. This trend may be associated with the increasing proportion of the older adult population in these regions (16). It is worth noting that changes in ASR and EAPC in low, low-middle, and middle SDI regions are expected to impose a growing burden on individuals and society due to population growth and rising global SDI levels.
Furthermore, the COVID-19 pandemic has acted as a major disruptor, likely exacerbating both the global burden of migraine and inequities in its management. Healthcare resources worldwide were diverted toward pandemic response, leading to widespread interruptions in non-urgent medical services. A study conducted in Spain detailed severe disruptions to headache care, including cancellation of outpatient visits, delays in diagnosis, and interruptions in essential treatments (17). Global surveys by the World Health Organization further confirm that such service disruptions were particularly acute in resource-limited settings, with low and middle-income countries experiencing more severe and prolonged impacts on non-urgent medical care (18). Consequently, the pandemic has probably contributed to substantial underdiagnosis, which masks the true incidence of the disease, and has worsened management of existing cases. The lack of timely and standardized treatment likely increased patient disability, a effect ultimately reflected in rising disability-adjusted life years (DALYs). The rapid adoption of telemedicine, while serving as a critical solution, has exhibited substantial disparities in effectiveness across different Socio-demographic Index (SDI) settings, thereby creating a “digital divide” (19). Barriers to access, which include geographical isolation, socioeconomic disadvantage, and inadequate digital infrastructure (20, 21), have posed particularly severe challenges for patients with significant physical or mental disabilities (22). Thus, the pandemic has intensified the current management challenges and underscored the imperative for establishing more resilient and equitable healthcare systems.
The notably rapid increase in migraine burden in middle-SDI regions, as highlighted by our study, likely stems from a dual dynamic: a genuine rise in incidence coupled with major improvements in case ascertainment. The improvement in ascertainment can be primarily attributed to enhanced financial capacity resulting from socioeconomic development, which directly addresses the predominant structural barrier to healthcare access in resource-limited settings, namely financial difficulty (23, 24). Empirical evidence from India provides robust support for this mechanism, demonstrating that a health insurance scheme for the impoverished significantly increased outpatient service utilization (25). Consequently, as economic barriers are removed, patient behavior shifts decisively from endurance to active healthcare use. This behavioral shift, reinforced by growing health awareness, fundamentally alters care-seeking patterns for conditions like migraine (26). Leading to the identification of a substantial pre-existing burden. Concurrently, health system strengthening in these regions, particularly investments in primary health care, has improved the diagnostic capacity for chronic diseases at the grassroots level. Migraine is recognized to be substantially under-diagnosed globally, and the World Health Organization has explicitly identified training primary care physicians as a key strategy to address this problem. Studies confirm that introducing diagnostic guidelines and tools in primary care settings can effectively correct the under-recognition and misdiagnosis of headache disorders (27). Together, these factors systematically uncover a substantial pre-existing burden of migraine that was previously overlooked by the healthcare system.
Simultaneously, the rapid urbanization and lifestyle transitions characteristic of middle-SDI regions represent a contributing factor to a true increase in migraine incidence. World Health Organization reports indicate that urbanization promotes increased risk for various non-communicable diseases. Within this epidemiological shift, increased population exposure to psychosocial stress, sedentary behavior, and dietary changes, all of which are established as modifiable risk factors for migraine (28, 29), is likely instrumental. Consequently, the observed escalation in burden likely reflects both improved detection of pre-existing cases and a genuine rise in disease incidence driven by these risk environments, underscoring the dual challenge faced by health systems in transitioning economies.
This study indicates that the prevalence, incidence, and DALY rates of migraine showed an overall upward trend with economic improvement in 2021. Generally, countries with higher SDI tend to have more advanced healthcare systems and higher patient engagement. Additionally, factors such as the transition from traditional to industrialized diets, increased exposure to environmental pollution, and lifestyle changes (e.g., reduced physical activity) may contribute to the rising risk of chronic diseases (30, 31). In countries with higher SDI, the larger proportion of the older adult population may lead to an increased disease burden of migraine. Therefore, regions with higher SDI should prioritize measures to reduce specific risk factors associated with migraine and improve early screening and treatment.
We should focus on frontier countries with lower SDI, as frontier analysis reveals their excellent performance despite limited resources. The practices and models adopted by these countries can serve as valuable references for other resource-limited countries facing heavy burdens. Conversely, some high SDI countries and regions, such as Belgium, Germany, and San Marino, have shown poor performance, indicating that other factors have outweighed the health benefits brought by development. Future research needs to further explore the driving factors in leading countries and the obstacles faced by lagging countries.
The pattern of a markedly rapid increase in migraine burden observed in middle- and high-middle SDI regions, as illustrated by China, is likely generalizable to a broader range of countries undergoing similar developmental transitions. Our analysis pinpoints a turning point at an SDI of approximately 0.75, beyond which the age-standardized rates of migraine resume a pronounced upward trend. This pattern of co-evolution between non-communicable disease risk and developmental level aligns with the broader framework established by the Global Burden of Disease study (13). This SDI threshold can serve as a predictive tool, indicating that countries approaching or newly entering this high-risk range are likely to encounter an increasing burden of migraine. This pattern is particularly relevant for a cohort of nations experiencing sustained socioeconomic growth, including Indonesia, India, Vietnam, Peru, and Colombia. Many of these countries, classified by the World Bank as middle- and upper-middle-income economies (32), represent the next group likely to confront this challenge. These nations embody the epidemiologic transition, which is the characteristic shift in population disease burden that accompanies societal development (33).
5 Limitations
This study still faces some limitations. Firstly, our research is based on secondary data analysis from the GBD study. Insufficient registration of migraine cases in certain underdeveloped areas may lead to underestimation, despite the use of robust statistical methods to mitigate this effect. Misdiagnosis or missed diagnosis due to limited health resources remains a possibility. Secondly, data from various countries inevitably leads to quality inconsistencies, such as measurement biases, reporting delays, or disease misclassification. While the predictive model provides a general outline of future trends, it cannot offer precise forecasts. Finally, the issue of GBD data lag arises because current estimates are calculated based on past trends and covariates (34). To address the limitations of the GBD study, more international collaborations should be encouraged, including annual data searches with partners from various countries and the incorporation of case data from a wider range of sources. Additionally, the detailed data cleaning, correction, and smoothing procedures developed by GBD collaborators are effective measures to overcome these limitations. Ultimately, we need to translate research findings into practical actions, such as formulating public policies and providing references for future studies.
6 Conclusion
In summary, migraine represents a significant global public health issue. This study has found that the burden of migraine among the global population has increased significantly from 1990 to 2021, particularly in regions with middle SDI. Our research underscores the importance of tailored interventions aimed at addressing migraine, thereby contributing to the achievement of the Sustainable Development Goals set by the World Health Organization. The formulation and implementation of scientifically effective public health policies, along with the enhancement of health education and medical services, are crucial in reducing the burden of migraine.
Statements
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Ethics statement
Ethical review and approval was not required for the study on human participants in accordance with the local legislation and institutional requirements. Written informed consent from the patients/participants or patients/participants’ legal guardian/next of kin was not required to participate in this study in accordance with the national legislation and the institutional requirements.
Author contributions
YL: Conceptualization, Investigation, Methodology, Writing – original draft. Q-yL: Conceptualization, Investigation, Methodology, Writing – original draft. LG: Conceptualization, Investigation, Methodology, Writing – original draft. YY: Conceptualization, Software, Visualization, Writing – original draft. C-dW: Conceptualization, Data curation, Formal Analysis, Software, Writing – original draft. Z-wG: Conceptualization, Data curation, Formal Analysis, Software, Writing – original draft. JS: Project administration, Resources, Supervision, Validation, Writing – review & editing. X-yL: Funding acquisition, Project administration, Resources, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was funded by the Shanghai Hongkou District Science and Technology Committee Major Project Hongwei (No. 2301-02), National TCM Advantageous Specialty Construction Project (20240511), and New Technology Research and Transformation of Shanghai Municipal Health Commission (No. 2024ZZ2067).
Acknowledgments
We express our sincere gratitude to the Global Burden of Disease Study 2021 collaborators for their valuable contributions and efforts. The authors would like to thank all the researchers in our working group.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
GBD 2021 Nervous System Disorders Collaborators . Global, regional, and national burden of disorders affecting the nervous system, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet Neurol. (2024) 23:344–81. doi: 10.1016/S1474-4422(24)00038-3
2.
Huang L Juan Dong H Wang X Wang Y Xiao Z . Duration and frequency of migraines affect cognitive function: evidence from neuropsychological tests and event-related potentials. J Headache Pain. (2017) 18:54. doi: 10.1186/s10194-017-0758-6
3.
Cohen F Brooks CV Sun D Buse DC Reed ML Fanning KM et al . Prevalence and burden of migraine in the United States: a systematic review. Headache. (2024) 64:516–32. doi: 10.1111/head.14709
4.
Vetvik KG MacGregor EA . Sex differences in the epidemiology, clinical features, and pathophysiology of migraine. Lancet Neurol. (2017) 16:76–87. doi: 10.1016/S1474-4422(16)30293-9
5.
GBD 2021 Diseases and Injuries Collaborators . Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2133–61. doi: 10.1016/S0140-6736(24)00757-8
6.
Vos T Lim SS Abbafati C Abbas KM Abbasi M Abbasifard M et al . Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1204–22. doi: 10.1016/S0140-6736(20)30925-9
7.
Tana C Raffaelli B Souza MNP de la Torre ER Massi DG Kisani N et al . Health equity, care access and quality in headache-part 1. J Headache Pain. (2024) 25:12. doi: 10.1186/s10194-024-01712-7
8.
GBD 2021 Causes of Death Collaborators . Global burden of 288 causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet. (2024) 403:2100–32. doi: 10.1016/S0140-6736(24)00367-2
9.
Olshansky SJ Ault AB . The fourth stage of the epidemiologic transition: the age of delayed degenerative diseases. Milbank Q. (1986) 64:355–91. doi: 10.2307/3350025
10.
McKeown RE . The epidemiologic transition: changing patterns of mortality and population dynamics. Am J Lifestyle Med. (2009) 3:19S–26S. doi: 10.1177/1559827609335350
11.
GBD 2016 Neurology Collaborators . Global, regional, and national burden of neurological disorders, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. (2019) 18:459–80. doi: 10.1016/S1474-4422(18)30499-X
12.
Yusuf S Joseph P Rangarajan S Islam S Mente A Hystad P et al . Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. (2020) 395:795–808. doi: 10.1016/S0140-6736(19)32008-2
13.
Wang H Abbas KM Abbasifard M Abbasi-Kangevari M Abbastabar H Abd-Allah F et al . Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950–2019: a comprehensive demographic analysis for the Global Burden of Disease Study 2019. Lancet. (2020) 396:1160–203. doi: 10.1016/S0140-6736(20)30977-6
14.
Leonardi M Raggi A . A narrative review on the burden of migraine: when the burden is the impact on people’s life. J Headache Pain. (2019) 20:41. doi: 10.1186/s10194-019-0993-0
15.
Steiner TJ Stovner LJ Jensen R Uluduz D Katsarava Z . Migraine remains second among the world's causes of disability, and first among young women: findings from GBD2019. J Headache Pain. (2020) 21:137. doi: 10.1186/s10194-020-01208-0
16.
GBD 2019 Ageing Collaborators . Global, regional, and national burden of diseases and injuries for adults 70 years and older: systematic analysis for the global burden of disease 2019 study. BMJ. (2022) 376:e068208. doi: 10.1136/bmj-2021-068208
17.
López-Bravo A García-Azorín D Belvís R González-Oria C Latorre G Santos-Lasaosa S et al . Impact of the COVID-19 pandemic on headache management in Spain: an analysis of the current situation and future perspectives. Neurologia. (2020) 35:372–80. doi: 10.1016/j.nrl.2020.05.006
18.
World Health Organization . (2021). Second round of the national pulse survey on continuity of essential health services during the COVID-19 pandemic. Available online at: https://www.who.int/publications/i/item/WHO-2019-nCoV-EHS-continuity-survey-2021.1. (Accessed October 9, 2025)
19.
Cheshmehzangi A Zou T Zhang Y Chen H Su Z Dawodu A et al . Commentary: reflecting on the neglected digital divide barriers of telemedicine during COVID-19. Front Public Health. (2022) 10:915401. doi: 10.3389/fpubh.2022.915401
20.
Nakayama LF Binotti WW Link Woite N Fernandes CO Alfonso PG Celi LA et al . The digital divide in Brazil and barriers to telehealth and equal digital health care: analysis of internet access using publicly available data. J Med Internet Res. (2023) 25:e42483. doi: 10.2196/42483
21.
Chang JE Lai AY Gupta A Nguyen AM Berry CA Shelley DR . Rapid transition to telehealth and the digital divide: implications for primary care access and equity in a post-COVID era. Milbank Q. (2021) 99:340–68. doi: 10.1111/1468-0009.12509
22.
Bhaskar S Nurtazina A Mittoo S Banach M Weissert R . Editorial: telemedicine during and beyond COVID-19. Front Public Health. (2021) 9:662617. doi: 10.3389/fpubh.2021.662617
23.
Shang XT Wei ZH . Socio-economic inequalities in health among older adults in China. Public Health. (2023) 214:146–52. doi: 10.1016/j.puhe.2022.11.013
24.
Alamneh TS Teshale AB Yeshaw Y Alem AZ Ayalew HG Liyew AM et al . Socioeconomic inequality in barriers for accessing health care among married reproductive aged women in sub-Saharan African countries: a decomposition analysis. BMC Womens Health. (2022) 22:130. doi: 10.1186/s12905-022-01716-y
25.
Karan A Yip W Mahal A . Extending health insurance to the poor in India: an impact evaluation of Rashtriya Swasthya Bima Yojana on out of pocket spending for healthcare. Soc Sci Med. (2017) 181:83–92. doi: 10.1016/j.socscimed.2017.03.053
26.
Cai J Li Y Li R Coyte PC . Has socioeconomic inequality in perceived access to health services narrowed among older adults in China?BMC Health Serv Res. (2024) 24:1077. doi: 10.1186/s12913-024-11510-1
27.
Kernick D Stapley S Hamilton W . GPs’ classification of headache: is primary headache underdiagnosed?Br J Gen Pract. (2008) 58:102–4. doi: 10.3399/bjgp08X264072
28.
Woldeamanuel YW Cowan RP . The impact of regular lifestyle behavior in migraine: a prevalence case-referent study. J Neurol. (2016) 263:669–76. doi: 10.1007/s00415-016-8031-5
29.
Buse DC Reed ML Fanning KM Bostic RC Lipton RB . Demographics, headache features, and comorbidity profiles in relation to headache frequency in people with migraine: results of the American Migraine Prevalence and Prevention (AMPP) study. Headache. (2020) 60:2340–56. doi: 10.1111/head.13966
30.
Dai X Gakidou E Lopez AD . Evolution of the global smoking epidemic over the past half century: strengthening the evidence base for policy action. Tob Control. (2022) 31:129–37. doi: 10.1136/tobaccocontrol-2021-056535
31.
Afshin A Forouzanfar MH Reitsma MB Sur P Estep K Lee A et al . Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med. (2017) 377:13–27. doi: 10.1056/NEJMoa1614362
32.
The World Bank . World Bank country and lending groups. Washington, DC: The World Bank (2024).
33.
Bennett JE Stevens GA Mathers CD Bonita R Rehm J Kruk ME et al . NCD countdown 2030: worldwide trends in non-communicable disease mortality and progress towards sustainable development goal target 3.4. Lancet. (2018) 392:1072–88. doi: 10.1016/S0140-6736(18)31992-5
34.
Kluth LA Fajkovic H Xylinas E Crivelli JJ Passoni N Rouprêt M et al . Female gender is associated with higher risk of disease recurrence in patients with primary T1 high-grade urothelial carcinoma of the bladder. World J Urol. (2013) 31:1029–36. doi: 10.1007/s00345-012-0996-9
Summary
Keywords
migraine, disease burden, frontier analysis, trends, GBD 2021
Citation
Lu Y, Li Q-y, Gan L, You Y, Wang C-d, Guo Z-w, Shi J and Liu X-y (2025) The global and regional burden and trends of migraine from 1990 to 2021: Global Burden of Disease Study 2021. Front. Neurol. 16:1686288. doi: 10.3389/fneur.2025.1686288
Received
19 August 2025
Accepted
17 October 2025
Published
03 November 2025
Volume
16 - 2025
Edited by
Claudia Altamura, Fondazione Policlinico Campus Bio-Medico, Italy
Reviewed by
Sonia Santos Lasaosa, Lozano Blesa University Clinical Hospital, Spain
Kazumasa Saigoh, Kindai University Hospital, Japan
Updates
Copyright
© 2025 Lu, Li, Gan, You, Wang, Guo, Shi and Liu.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jun Shi, shijundoctor@163.com; Xiao-ying Liu, 303425290@qq.com
†These authors share first authorship
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.