Abstract
Background:
Laminoplasty has been widely used for the treatment of multilevel degenerative cervical myelopathy (DCM). However, patients often experience persistent axial symptoms, which affect post-operative functional rehabilitation. This study aims to explore the intrinsic connection between the pre-operative structural and functional status of the cervical spine and the post-operative functional rehabilitation of patients undergoing laminoplasty, providing a theoretical basis for individualized rehabilitation strategies for specific populations.
Methods:
A retrospective analysis was conducted on the clinical data of patients who underwent laminoplasty and received inpatient rehabilitation treatment. Pre-operative and 3-month post-operative visual analog scale (VAS) score, modified Japanese orthopedic association (mJOA) score, and neck disability index (NDI) score were collected, and correlation analyses were performed with pre-operative cervical flexion and extension range of motion (ROM), cervical muscle strength, and the functional cross-sectional area (fCSA) of posterior cervical muscles measured by magnetic resonance imaging (MRI).
Results:
Among the 30 included patients, 17 were males and 13 were females with an average age of 59.70 ± 8.41 years, the follow-up period is 3 months. Correlation analysis revealed that pre-operative cervical extension muscle strength was weakly positively correlated with the post-operative VAS score (r = 0.364, p = 0.048) and was moderately positively correlated with the NDI score (r = 0.448, p = 0.013). The regression analysis results showed that extension strength had a significant and positive independent predictive effect on post-operative VAS score (β = 0.256, p = 0.025) and NDI score (β = 0.789, p = 0.024). For the sum of posterior cervical muscles, pre-operative fCSA of the right multifidus (MF) was weakly negatively correlated with the post-operative NDI score (r = −0.369, p = 0.045).
Conclusion:
Our result suggested that stronger pre-operative cervical extension strength may be important predictors of post-operative functional rehabilitation in patients after laminoplasty, especially in terms of axial symptoms.
1 Introduction
Degenerative cervical myelopathy (DCM) is a variety of age-related and genetically associated pathologies, including cervical spondylotic myelopathy, degenerative disc disease, and ligamentous aberrations such as ossification of the posterior longitudinal ligament (1). It is understood that DCM is the most common cause of non-traumatic spinal cord impairment worldwide, literatures reported that the incidence were estimated to occur in 24.2% of asymptomatic/subclinical adults (2, 3). The most consistent feature of DCM is the progression of symptoms rather than the symptoms present. The most common presenting symptom is paraesthesia in the hands which can easily be misdiagnosed. Late-stage presentation of DCM includes motor loss, paralysis and loss of sphincter control (4). Given the natural history of a stepwise deterioration, treatment strategy favors surgical intervention (5), with 1.6 per 100,000 people requiring surgery in their lifetime (6).
Laminoplasty is a posterior decompressive surgery and has been widely used for the treatment of multilevel DCM (7). The long-term clinical follow-up results show that the patients' neurological functions can achieve a relatively ideal recovery after laminoplasty (8, 9), however, post-operative complications such as axial symptoms, C5 palsy and cervical kyphosis seriously affecting the overall efficacy and the rehabilitation process (10–12). To address this surgical dilemma, previous studies have reported modified surgical techniques that maximally preserve the spinal-muscle-ligament stabilizing structures (13–15). In particular, persistent axial pain can be a major cause of dissatisfaction after surgery, even in patients with excellent neurological recovery (16). Therefore, people have come to realize the significance of post-operative rehabilitation treatment for cervical spine function. Some researchers, including those from our research team, have reported the rehabilitation effects of early cervical range of motion (ROM) and resistance muscle strength training for patients after laminoplasty (17–19).
Advancements in clinical decision-making, surgical techniques, and perioperative rehabilitation have allowed doctors to manage increasingly complex cervical spine cases. Continued teamwork is required on the part of orthopedics, rehabilitation physicians, rehabilitation therapists, and nurses to take this access forward. Compared to surgical techniques, the post-operative rehabilitation treatment for cervical spine function has developed slowly, indicating that there are still many overlooked treatment details that we have not addressed. In previous studies, we adopt a team approach for early rehabilitation in patients after laminoplasty, and demonstrated its efficacy in improving quality of life in specific populations (18). However, it still failed to solve the problem that we are most concerned about, namely the therapeutic effect on post-operative axial symptoms. Naghdi et al. (20) discovered that morphological characteristics of pre-operative posterior cervical muscles might be important predictors of functional recovery and post-surgical outcomes in patients with DCM. Therefore, we conducted a retrospective analysis of the clinical data of the patients, attempting to identify the intrinsic connection between pre-operative structural-functional status of cervical spine and post-operative function rehabilitation in patients after laminoplasty. We hypothesized that pre-operative cervical spine function will be associated with post-operative axial symptoms and functional scores. The study aimed to discover potential intervention timing and treatment methods, in order to provide theoretical basis for individualized rehabilitation strategies for specific populations.
2 Methods
2.1 Study design and participants
We conducted a single-center retrospective study at Peking University Third Hospital, involving 30 patients who underwent laminoplasty and received inpatient rehabilitation treatment after surgery from February 2018 to February 2020. The follow-up period is 3 months. Inclusion criteria: (1) a clear diagnosis of DCM based on medical history, symptoms, signs, and imaging findings; (2) patients who underwent open-door laminoplasty preservation of unilateral (right side) musculo-ligamentous complex by the same surgeon at Peking University Third Hospital (21); (3) age ≥18 years; (4) patients completed a 7-day inpatient rehabilitation treatment from the third day after surgery; (5) complete clinical and follow-up data. Exclusion criteria: (1) Patients with major organic lesions, including cardiac and pulmonary dysfunction, tumors, stroke, Parkinson's disease, etc.; (2) patients who underwent secondary cervical spine surgery during the follow-up period; (3) patients with fractures and severe osteoporosis.
2.2 Sample size determination
This study was a exploratory, single-center retrospective study. During the research design phase, we discovered that for patients who undergone laminoplasty, few studies have explored the relationship between cervical pre-operative function and post-rehabilitative function. So there was a lack of previous research data to estimate the effect size for conducting a priori sample size calculation. Therefore, we adopted a feasibility sample size design and included all consecutive cases that met all inclusion and exclusion criteria during the study period from February 2018 to February 2020, a total of 30 cases.
2.3 Rehabilitation during hospitalization
Patients received rehabilitation treatment in hospital for 7 days under the guidance of a professional team composed of rehabilitation doctors, physiotherapists, occupational therapists, and nurses. The treatment was based on Chinese expert consensus on the implementation of enhanced recovery after surgery in posterior cervical spine surgery (22). From the third day after surgery, the training was conducted for approximately 60 min each time, twice a day, and based on the patients' functional performance to adjust the exercise prescription. The nerve function training of the limbs and hands includes proprioceptive neuromuscular facilitation practices, muscle strength training and hand function training, up to 30 min at a time (Figure 1). Training on transfers, balance and gait up to 20 min at a time (Figure 2). If the neck pain was mild, perform cervical function training includes cervical range of motion training and isometric muscle strength training, the training lasts no more than 20 min (Figure 3). After the 7-day rehabilitation treatment was completed, we provided patients with a home-based rehabilitation programme that includes cervical spine function training, according to their functional impairments. Patients were discharged from the hospital and started a daily rehabilitation exercise at home.
Figure 1
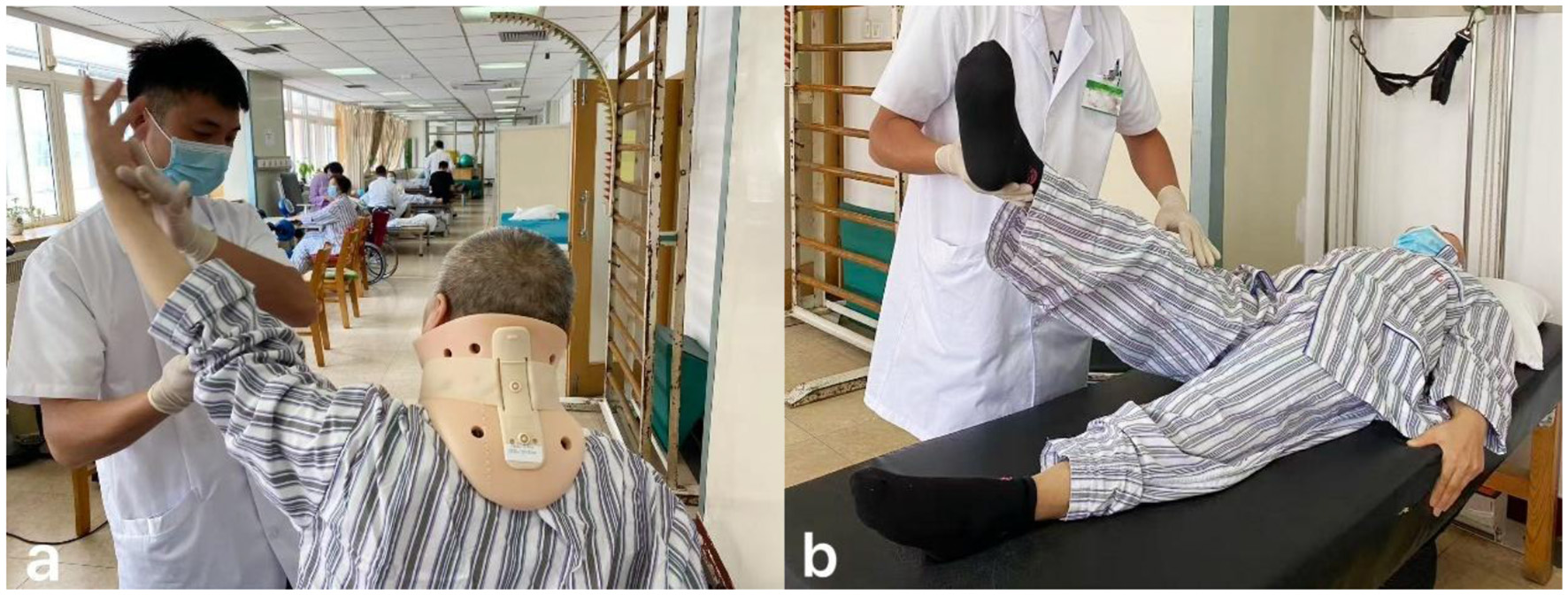
(a) Upper limb motor function training. (b) Lower limb motor function training.
Figure 2

(a) Visual feedback-assisted standing balance training. (b) Walking aid-assisted standing balance training.
Figure 3

(a) Active cervical rotation range of motion training. (b) Cervical extension resistance isometric muscle strength training.
2.4 Data collection
Information was extracted from the hospital's electronic medical record system and the collected patient follow-up case report forms. The data collected included: (1) basic information: gender, age, surgical segment, longest follow-up time; (2) visual analog scale (VAS) score: a total score of 10 points, with a higher score indicating more severe pain; (3) modified Japanese orthopedic association (mJOA) score: a total score of 17 points, with a higher score indicating better neurological function. This is currently a widely used evaluation index for cervical spinal cord function (23); (4) neck disability index (NDI): a total score of 50 points, with a higher score indicating worse cervical spine function, and its reliability and validity have been effectively verified (24); (5) cervical range of motion (ROM) and muscle strength: using Multi-Cervical Unit (MCU, BTE Technologies, Inc, Hanover, MD) for cervical flexion and extension ROM and isometric muscle strength tests (25, 26), recording cervical flexion ROM, extension ROM, flexion strength and extension strength (Figure 4); (6) functional cross-sectional area (fCSA) of posterior cervical muscles: patients underwent 3.0T magnetic resonance imaging (MRI, GE Signa HDxt 3.0T) before surgery, and the images were stored in the hospital's Picture Archiving and Communication System (PACS, United Imaging Medical Technology Co., Ltd., Shanghai, China). The intervertebral disc cross-sectional T2-weighted images of the C3/4, C4/5, C5/6, and C6/7 segments were downloaded to the computer, and two physicians simultaneously used the ImageJ system (Version 1.54p, National Institutes of Health, Bethesda, Maryland) for measurement, and took the average value. Four areas within the cross-sectional muscle were selected and the signal values were measured. The maximum value among them was selected as the threshold to distinguish normal muscle tissue from fat tissue. The cross-sectional areas (CSA) of the multifidus (MF), semispinalis cervicis (SC), semispinalis capitis (SCap), and splenius capitis (SpC) on both sides were obtained, and the fatty infiltration (FI) was calculated based on the measured muscle threshold, and the fCSA was calculated as fCSA = CSA × (1-FI) (27) (Figure 5).
Figure 4

The Multi-Cervical Unit (MCU, BTE Technologies, Inc, Hanover, MD) is a biomechanical system designed to measuring the active range of motion of the neck and the isometric strength of neck muscles. The unit is equipped with an armchair that rotates 90° for measurement of lateral flexions, with adjustable seat height, lumbar support and armrests, and a shoulder restraint system to secure the subject within the seat in order to isolate the cervical spine during testing. It also contains a unique head assembly system (movable inner and outer head brace) designed to cause the subject's head to move safely in different planes.
Figure 5
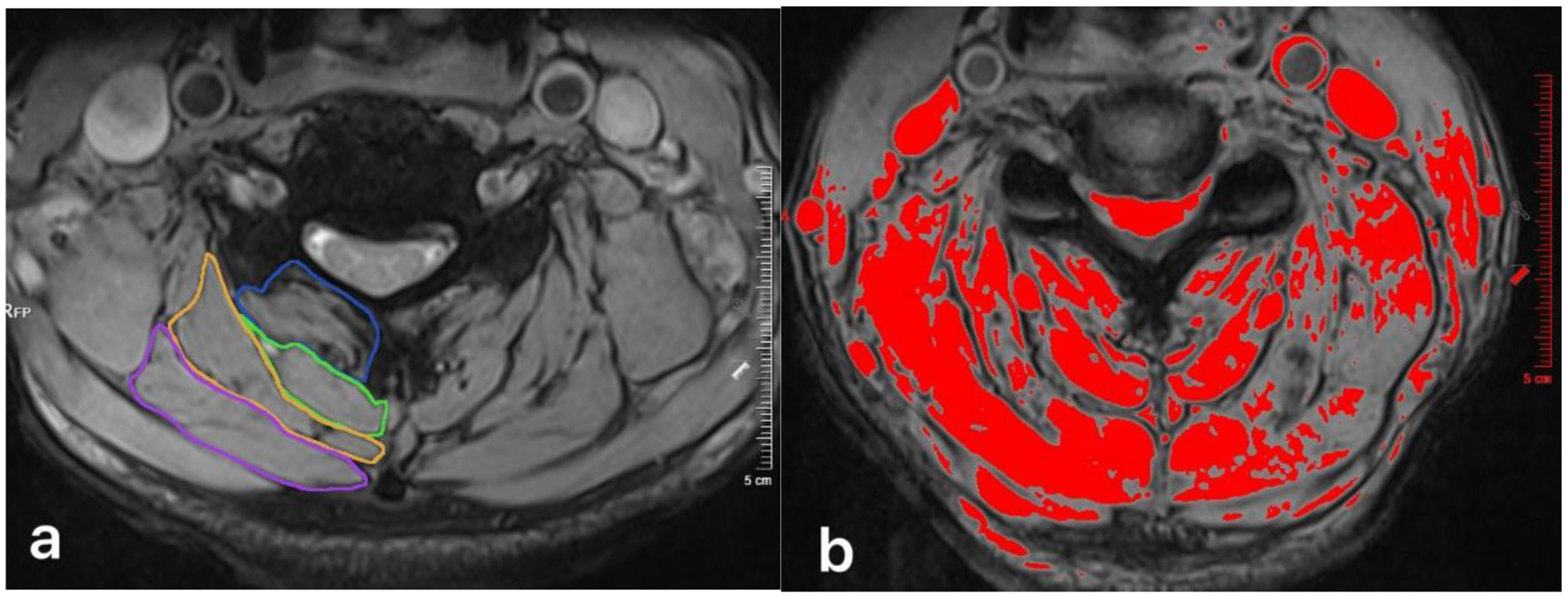
(a) Measurement of pre-operatively total CSA at C4/5 level for the multifidus (MF, blue circle), semispinalis cervicis (SC, green circle), semispinalis capitis (SCap, orange circle), and splenius capitis (SpC, pink circle). (b) Thresholding technique was used to mark the pre-operative FI and calculate the fCSA.
This study collected the VAS scores, mJOA scores and NDI scores of the patients before and 3 months after laminoplasty. It also conducted a correlation analysis between pre-operative cervical spine function and post-rehabilitative functional scores.
2.5 Statistical analysis
All the statistical analyses were performed using SPSS version 27.0 (IBM Corp., Armonk, NY, United States). The Shapiro–Wilk test was used to assess the normality of the data distribution. Normally distributed continuous variables are presented as the mean ± standard deviation (SD) and non-normally distributed continuous variables are expressed as medians with ranges. Categorical variables are reported as frequencies and percentages [n (%)]. Paired sample t-test was used to compare pre-operative and post-operative index. The Pearson correlation coefficients were calculated and multivariate linear regression analysis was used to assess the linear correlation between pre-operative and post-operative target, with a significance level set at p ≤ 0.05.
3 Results
3.1 Clinical features
A total of 30 patients who underwent laminoplasty and received inpatient rehabilitation treatment were included in this study. No serious complications such as nerve injury, post-operative infection, or poor wound healing occurred in any of the patients during the follow-up period. The average age was 59.70 ± 8.41 years, including 17 (56.7%) male and 13 (43.3%) female. Among them, 20 (66.7%) underwent C3-C7 segment open-door laminoplasty, and 10 (33.3%) underwent non- C3-C7 segment open-door laminoplasty. Within the group there was no significant difference in the VAS scores before and 3 months after surgery (p > 0.05), while there were significant differences in the mJOA scores and NDI scores within the group before and 3 months after surgery (p ≤ 0.05). The average pre-operative cervical flexion ROM was 36.7° ± 9.5°, the extension ROM was 37.8° ± 9.5°, and the flexion muscle strength was 8.1 ± 4.3 lbs, the extension muscle strength was 11.0 ± 5.8 lbs (Table 1).
Table 1
| Variables | Total | ||
|---|---|---|---|
| Age; mean+SD | 59.70 ± 8.41 | ||
| Gender | |||
| Male; n (%) | 17 (56.7) | ||
| Female; n (%) | 13 (43.3) | ||
| Surgical segment; n (%) | |||
| C3-C7 | 20 (66.7) | ||
| Non C3-C7 | 10 (33.3) | ||
| Obsevation index | Pre-operation | Post-operation | p-Value |
| VAS; mean + SD | 2.6 ± 2.2 | 3.2 ± 2.3 | 0.262 |
| mJOA; mean + SD | 13.4 ± 2.1 | 14.6 ± 2.0 | 0.008 |
| NDI; mean + SD | 7.2 ± 7.2 | 10.1 ± 6.9 | 0.050 |
| Flexion ROM; mean + SD, degrees | 36.7 ± 9.5 | ||
| Extension ROM; mean + SD, degrees | 37.8 ± 9.5 | ||
| Flexion strength; mean + SD, lbs | 8.1 ± 4.3 | ||
| Extension strength; mean + SD, lbs | 11.0 ± 5.8 |
Baseline characteristics and clinical features of patients.
Statistically significant values are in bold (p ≤ 0.05).
Table 2 presented the measurement values and sum values of posterior cervical muscles' fCSA on both sides of each cervical segment before surgery. The measurement of posterior cervical muscles included MF, SC, Scap, and SpC.
Table 2
| Surgical segment | Cervical muscle | Side | C3/4 | C4/5 | C5/6 | C6/7 | Sum |
|---|---|---|---|---|---|---|---|
| fCSA, cm2 | MF | Left | 1.22 ± 0.39 | 1.26 ± 0.44 | 1.27 ± 5.83 | 1.57 ± 0.59 | 5.33 ± 1.66 |
| Right | 1.29 ± 0.38 | 1.20 ± 0.46 | 1.15 ± 0.44 | 1.50 ± 0.44 | 5.11 ± 1.38 | ||
| SC | Left | 0.99 ± 0.44 | 0.88 ± 0.52 | 0.72 ± 0.38 | 0.59 ± 0.30 | 3.17 ± 1.17 | |
| Right | 1.05 ± 0.42 | 0.78 ± 0.42 | 0.59 ± 0.34 | 0.62 ± 0.31 | 3.03 ± 1.07 | ||
| Scap | Left | 1.97 ± 1.19 | 1.80 ± 1.01 | 1.32 ± 0.79 | 1.31 ± 0.68 | 6.40 ± 3.18 | |
| Right | 1.54 ± 1.07 | 1.53 ± 1.14 | 1.06 ± 0.66 | 1.13 ± 0.67 | 5.25 ± 3.17 | ||
| SpC | Left | 1.39 ± 1.17 | 1.64 ± 1.24 | 1.74 ± 1.20 | 1.53 ± 1.17 | 6.30 ± 3.94 | |
| Right | 1.01 ± 0.70 | 1.12 ± 0.83 | 1.37 ± 1.07 | 1.21 ± 0.84 | 4.70 ± 2.94 |
Pre-operative posterior cervical muscles fCSA index.
Sum, calculate the sum value of posterior cervical muscles from segments C3 to C7.
3.2 Correlation analysis
The correlation analysis showed that there was no correlation between the pre-operative cervical flexion ROM, extension ROM, flexion muscle strength and the post-operative 3-month observation indicators (p > 0.05). The pre-operative cervical extension muscle strength was weakly positively correlated with the post-operative VAS score (r = 0.364, p = 0.048) and was moderately positively correlated with the NDI score (r = 0.448, p = 0.013), however there was no correlation with the mJOA score (p > 0.05; Table 3).
Table 3
| Observation index | VAS | mJOA | NDI | |||
|---|---|---|---|---|---|---|
| r -value | p -Value | r -value | p -Value | r -value | p -Value | |
| Flexion ROM | 0.001 | 0.996 | −0.141 | 0.457 | 0.160 | 0.397 |
| Extension ROM | 0.259 | 0.167 | 0.183 | 0.332 | 0.111 | 0.561 |
| Flexion strength | 0.144 | 0.448 | 0.008 | 0.966 | 0.214 | 0.256 |
| Extension strength | 0.364 | 0.048 | −0.111 | 0.558 | 0.448 | 0.013 |
Correlation analysis of post-operative observation index and pre-operative cervical spine function.
Statistically significant values are in bold (p ≤ 0.05).
To further verify whether extension strength was an independent predictor of VAS score and NDI score, we conducted a multiple linear regression analysis. Under the condition of controlling for flexion ROM, extension ROM, and flexion strength, we evaluated the independent impact of extension strength on post-operative indicators. The regression analysis results showed that extension strength had a significant and positive independent predictive effect on post-operative VAS score (β = 0.256, p = 0.025) and NDI score (β = 0.789, p = 0.024), indicating that extension strength was a potential independent predictor of VAS score and NDI score after surgery (Table 4).
Table 4
| Observation index | Variant | SE | β (95%CI) | t-value | p-Value |
|---|---|---|---|---|---|
| VAS | Constant | 1.810 | |||
| Flexion ROM | 0.054 | −0.093 (−0.204, 0.018) | −1.733 | 0.095 | |
| Extension ROM | 0.051 | 0.083 (−0.022, 0.187) | 1.621 | 0.118 | |
| Flexion strength | 0.137 | −0.157 (−0.440, 0.126) | −1.142 | 0.264 | |
| Extension strength | 0.107 | 0.256 (0.036, 0.476) | 2.392 | 0.025 | |
| NDI | Constant | 5.538 | |||
| Flexion ROM | 0.165 | −0.033 (−0.373, 0,306) | −0.203 | 0.841 | |
| Extension ROM | 0.156 | −0.016 (−0.337,0.305) | −0.100 | 0.921 | |
| Flexion strength | 0.42 | −0.397 (−1.263, 0.469) | −0.944 | 0.354 | |
| Extension strength | 0.327 | 0.789 (0.114, 1.463) | 2.409 | 0.024 |
Multiple linear regression analysis of pre-operative cervical spine function predicting post-operative observation index.
SE, Standard error; CI, Confidence interval.
Statistically significant values are in bold (p ≤ 0.05).
Table 5 presented the correlation analysis results between the pre-operative sum values of posterior cervical muscles' fCSA on the left and right sides and the post-operative observation indicators. The results showed that for the sum of posterior cervical muscles, pre-operative fCSA of the right MF was weakly negatively correlated with the post-operative NDI score (r = −0.369, p = 0.045). The fCSA of other posterior cervical muscles did not show a correlation with the post-operative 3-month observation indicators (p > 0.05).
Table 5
| Observation index | Cervical muscle | Side | VAS | mJOA | NDI | |||
|---|---|---|---|---|---|---|---|---|
| r -Value | p -Value | r -value | p -Value | r -Value | p -Value | |||
| fCSA-Sum | MF | Left | −0.144 | 0.448 | 0.021 | 0.910 | −0.300 | 0.107 |
| Right | −0.103 | 0.588 | 0.105 | 0.582 | −0.369 | 0.045 | ||
| SC | Left | −0.039 | 0.837 | −0.161 | 0.394 | −0.146 | 0.442 | |
| Right | 0.045 | 0.813 | −0.338 | 0.067 | −0.124 | 0.515 | ||
| Scap | Left | −0.108 | 0.570 | −0.156 | 0.410 | −0.124 | 0.514 | |
| Right | −0.152 | 0.423 | −0.212 | 0.261 | −0.101 | 0.595 | ||
| SpC | Left | −0.025 | 0.896 | −0.188 | 0.319 | −0.135 | 0.475 | |
| Right | −0.052 | 0.786 | −0.109 | 0.565 | 0.063 | 0.741 | ||
Correlation analysis of post-operative observation index and pre-operative cervical spine fCSA index.
Sum, calculate the sum value of posterior cervical muscles from segments C3 to C7. Statistically significant values are in bold (p ≤ 0.05).
4 Discussion
The laminoplasty is one of the standard surgical procedures for treatment of multilevel DCM, its clinical efficacy has been widely recognized. However, due to the dissection of muscles during the exposure of the surgical area, posterior cervical surgery has a significant negative impact on the posterior cervical muscles. In this study, all patients underwent single-door laminoplasty with the preservation of the right musculo-ligamentous complex. Previous studies have confirmed that this surgical method has long-term stable efficacy (28), and the cervical curvature can be maintained well. However, there are still problems such as decreased cervical mobility and atrophy of the posterior cervical muscles, which are difficulties in the post-operative rehabilitation of patients (27). To solve this difficult clinical problem, our research team, based on conventional rehabilitation treatment, added early post-operative rehabilitation training targeting cervical function, including active cervical ROM exercises and isometric muscle strength exercises of the neck. However, the above treatments did not show the advantages in rapidly relieving post-operative axial symptoms in the clinical follow-up (18).
This study appeared to indicate that cervical extension strength is a potential independent predictor of VAS score and NDI score after surgery. However, the result suggested that the better the pre-operative cervical extension strength, the more severe the axial symptoms would be after laminoplasty. It is contrary to conventional understanding and previous research trends. Through further literatures review, we found that previous researchers' exploration of cervical spine function was often based on analysis of surgical-related structural indicators such as changes in cervical curvature (29–31). Better cervical spine function can lead to a more stable post-operative structure and result in better objective measurement indicators. However, post-operative neck pain is a subjective sensation for patients and often has no direct correlation with objective measurement indicators, and is influenced by various factors (16). Beneck et al. (32) believed that in the early post-operative period, the accumulation of lactic acid in muscle tissue will stimulate the nerve endings, thereby causing local muscle pain. Damaged soft tissues and impaired blood circulation both lead to the accumulation of inflammatory mediators in the surgical area. This local accumulation stimulates the peripheral terminals of primary sensory neurons and increases sensitivity to pain, resulting in obvious pain manifestations (33). In addition, atrophied neck muscles have a situation of denervation (34), patients with poor cervical extension strength before surgery may experience less post-operative pain than others. Uehara et al. (17) discovered that change in the VAS of axial pain from before surgery to 3 months after surgery showed a greater decreased neck extension muscle strength resulting in severer axial pain. Therefore, considering the damage that laminoplasty may cause to posterior cervical muscle of the patients, it was observed that patients with better pre-operative cervical extension strength showed a significant decrease in muscle strength after surgery. The accumulation of inflammatory substances stimulates nerve endings, which may lead to more obvious axial symptoms. It is undeniable that the number of cases included in this study is limited. Therefore, the result of this study need to be further validated and analyzed through prospective large-sample studies.
Based on the results of MRI, correlation analysis showed that for the sum of posterior cervical muscles, pre-operative fCSA of the right MF was weakly negatively correlated with the post-operative NDI score, but we did not find a correlation with other observation indicators. Therefore, our study did not indicate a correlation between pre-operative fCSA and post-operative functional indicators. Naghdi et al. (20) conducted a correlation analysis on the pre-operative cervical spine MRI measurement values and post-operative indicators of 171 patients, and discovered the predictive value of the pre-operative morphology characteristics of cervical posterior muscles for post-operative function. Wong et al. (35) revealed that the pre-operative asymmetry of cervical muscles from C5 to C7 segments was a risk factor for adjacent segment disease after anterior cervical discectomy and fusion. The above studies confirmed the predictive value of pre-operative measurements of the posterior cervical muscles, therefore further prospective study can be designed to increase imaging measurement indicators of cervical posterior muscles, in order to explore their impact on post-operative function.
This study is the first to explore correlation between pre-operative cervical spine function and post-rehabilitation function after laminoplasty. The result appeared to indicate that cervical extension strength is a potential independent predictor of post-operative axial symptoms. For patients with stronger cervical extension strength, their post-operative pain can be quite obvious due to more pronounced muscle weakness and sensitization of pain perception. This might be a problem that we had overlooked before. Therefore, pain management after surgery is crucial for early rehabilitation exercises. Nie et al. (19) discovered that for patients with post-operative axial symptoms after cervical surgery, both peripheral and central pain sensitization exist. Compared with cervical range of motion training, progressive resistance cervical muscle strength training can reduce pain sensitization and reduce the occurrence of post-operative axial symptoms. Their study suggests that we need to further refine our existing post-operative cervical spine function training program, focusing on cervical muscle strength training as the key component of functional exercises, which might effectively alleviate post-operative pain. Additionally, we can also apply physical agents therapy such as transcutaneous electrical nerve stimulation (36), low-frequency ultrasound therapy (37), and high-intensity laser therapy (38) to relieve post-operative pain. Our study offered a new perspective for improving the axial symptoms of patients after laminoplasty. However, as it was a retrospective study with a limited sample size, our research results still require further experimental verification.
5 Conclusion
Our result suggested that stronger pre-operative cervical extension strength may be important predictors of post-operative functional rehabilitation in patients after laminoplasty, especially in terms of axial symptoms.
6 Limitations
This study is a retrospective study, which has several limitations such as numerous confounding factors, incomplete data, and resulting in a relatively small sample size. The single-center design and limited sample size may have reduced statistical power, potentially obscuring the significance of certain clinical indicators. In addition, the collection of the observation indicators in this study was mainly focused on 3 months after the surgery. Further, collection of long-term post-operative indicators is required.
Statements
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Research Ethics Committee of Peking University Third Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
ZZ: Conceptualization, Data curation, Investigation, Writing – original draft, Writing – review & editing. YZ: Data curation, Investigation, Writing – original draft, Writing – review & editing. HZ: Data curation, Writing – original draft. MZ: Methodology, Writing – review & editing. YY: Methodology, Writing – review & editing. ZL: Investigation, Writing – original draft. JT: Investigation, Writing – original draft. GC: Funding acquisition, Methodology, Project administration, Writing – review & editing. TL: Funding acquisition, Methodology, Project administration, Writing – review & editing. FZ: Methodology, Project administration, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The special fund of the National Clinical Key Specialty Construction Program, P. R. China (2022), and National Key Research and Development Program of China (No. 2018YFF0301104).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1.
Hejrati N Moghaddamjou A Marathe N Fehlings MG . Degenerative cervical myelopathy: towards a personalized approach. Can J Neurol Sci. (2021) 49:729–40. doi: 10.1017/cjn.2021.214
2.
Banerjee A Mowforth OD Nouri A Budu A Newcombe V Kotter MRN et al . The prevalence of degenerative cervical myelopathy-related pathologies on magnetic resonance imaging in healthy/asymptomatic individuals: a meta-analysis of published studies and comparison to a symptomatic cohort. J Clin Neurosci. (2022) 99:53–61. doi: 10.1016/j.jocn.2022.03.002
3.
Smith SS Stewart ME Davies BM Kotter MRN . The prevalence of asymptomatic and symptomatic spinal cord compression on magnetic resonance imaging: a systematic review and meta-analysis. Glob Spine J. (2021) 11:597–607. doi: 10.1177/2192568220934496
4.
Lannon M Kachur E . Degenerative cervical myelopathy: clinical presentation, assessment, and natural history. J Clin Med. (2021) 10:3626. doi: 10.3390/jcm10163626
5.
Saunders LM Sandhu HS McBride L Maniarasu VS Taylor S Dhokia R . Degenerative cervical myelopathy: an overview. Cureus. (2023) 15:e50387. doi: 10.7759/cureus.50387
6.
Ost K Jacobs WB Evaniew N Cohen-Adad J Anderson D Cadotte DW . Spinal cord morphology in degenerative cervical myelopathy patients; assessing key morphological characteristics using machine vision tools. J Clin Med. (2021) 10:892. doi: 10.3390/jcm10040892
7.
Liang Z Xu G Liu T Zhong Y Mo F Li Z . Quantitatively biomechanical response analysis of posterior musculature reconstruction in cervical single-door laminoplasty. Comput Methods Prog Biomed. (2023) 233:107479. doi: 10.1016/j.cmpb.2023.107479
8.
Takeshima Y Matsuoka R Nakagawa I Nishimura F Nakase H . Surgical outcome of laminoplasty for cervical spondylotic myelopathy in an elderly population - potentiality for effective early surgical intervention: a meta-analysis. Neurol Med Chir. (2017) 57:366–73. doi: 10.2176/nmc.ra.2016-0302
9.
Veeravagu A Azad TD Zhang M Li A Pendharkar AV Ratliff JK et al . Outcomes of cervical laminoplasty-population-level analysis of a national longitudinal database. J Clin Neurosci. (2018) 48:66–70. doi: 10.1016/j.jocn.2017.10.089
10.
Zuo KK Qin W Miao Y Zhu L . Analysis of risk factors of axial neck pain in posterior cervical single-door laminoplasty from the perspective of cervical sagittal plane. Front Surg. (2022) 9:973924. doi: 10.3389/fsurg.2022.973924
11.
Levi DJ Brusko GD Levi AD Wang MY . Does hinge sidedness influence laterality of C5 palsy after expansile open-door cervical laminoplasty?Neurosurg Focus. (2023) 55:E6. doi: 10.3171/2023.6.FOCUS23297
12.
Ren HL Shen X Ding RT Cai HB Zhang GL . Preoperative range of motion in extension may influence postoperative cervical kyphosis after laminoplasty. Spine. (2023) 48:1308–16. doi: 10.1097/BRS.0000000000004610
13.
Chen C Yang C Yang S Gao Y Zhang Y Wu X et al . Clinical and radiographic outcomes of modified unilateral open-door laminoplasty with posterior muscle-ligament complex preservation for cervical spondylotic myelopathy. Spine. (2019) 44:1697–704. doi: 10.1097/BRS.0000000000003158
14.
Sun Y . The application of the concept of minimal invasive spine surgery in the development and innovation of cervical expansive laminoplasty. Zhonghua Wai Ke Za Zhi. (2023) 61:645–9. doi: 10.3760/cma.j.cn112139-20230402-00134
15.
Qu L Li Z Wang X Yuan L Li C . Axial symptoms after conventional and modified laminoplasty: a meta-analysis. World Neurosurg. (2023) 180:112–22. doi: 10.1016/j.wneu.2023.09.086
16.
Kimura A Endo T Inoue H Seichi A Takeshita K . Impact of axial neck pain on quality of life after laminoplasty. Spine. (2015) 40:E1292–8. doi: 10.1097/BRS.0000000000001167
17.
Uehara T Tsushima E Yamada S Kimura S Satsukawa Y Yoshihara A et al . A randomized controlled trial for the intervention effect of early exercise therapy on axial pain after cervical laminoplasty. Spine Surg Relat Res. (2022) 6:123–32. doi: 10.22603/ssrr.2021-0110
18.
Zhang ZZ Chu HL Liu XX Zhou MW Zhou FF . Application of early intensive rehabilitation in enhanced recovery after surgery protocol after laminoplasty: a mixed methods research. Chin J Rehabil Theory Pract. (2024) 30:468–78. doi: 10.3969/j.issn.1006-9771.2024.04.013
19.
Nie C Chen K Zhu YU Song H Lyu F Jiang J et al . Comparison of time-dependent resistance isometric exercise and active range of motion exercise in alleviating the sensitization of postoperative axial pain after cervical laminoplasty. Musculoskelet Sci Pract. (2022) 62:102669. doi: 10.1016/j.msksp.2022.102669
20.
Naghdi N Elliott JM Weber MH Fehlings MG Fortin M . Cervical muscle morphometry and composition demonstrate prognostic value in degenerative cervical myelopathy outcomes. Front Neurol. (2023) 14:1209475. doi: 10.3389/fneur.2023.1209475
21.
Lin S Zhou F Sun Y Chen Z Zhang F Pan S . The severity of operative invasion to the posterior muscular-ligament complex influences cervical sagittal balance after open-door laminoplasty. Eur Spine J. (2015) 24:127–35. doi: 10.1007/s00586-014-3605-3
22.
Zhou FF Han B Liu N Yuan L Tian J Li L et al . Expert consensus on ERAS protocol of posterior cervical spine surgery. Chin J Bone Joint Surg. (2019) 12:498–508. doi: 10.3969/j.issn.2095-9958.2019.07.03
23.
Yee TJ Upadhyaya C Coric D Potts EA Bisson EF Turner J et al . Correlation of the Modified Japanese Orthopedic Association with functional and quality-of-life outcomes after surgery for degenerative cervical myelopathy: a quality outcomes database study. Neurosurgery. (2022) 91:952–60. doi: 10.1227/neu.0000000000002161
24.
Saltychev M Widbom-Kolhanen SS Pernaa KI . Sex-related differential item functioning of neck disability index. Disabil Rehabil. (2023) 20:1–7. doi: 10.1080/09638288.2023.2180545
25.
Chiu TT Sing KL . Evaluation of cervical range of motion and isometric neck muscle strength: reliability and validity. Clin Rehabil. (2002) 16:851–8. doi: 10.1191/0269215502cr550oa
26.
Arvanitidis M Mak HHK Martinez-Valdes E Barbero M Falla D . Validation of a novel device for assessing neck muscle strength. Arch Physiother. (2025) 15:148–57. doi: 10.33393/aop.2025.3476
27.
Xia T Sun Y Wang SB Zhang FS Zhang L Pan SF et al . Effect on the morphological change in the posterior cervical muscle of laminoplasty with preservation of unilateral musculo-ligamentous complex in the treatment of patients with ossification of the posterior longitudinal ligament. Chin J Spine Spinal Cord. (2020) 30:212–8. doi: 10.3969/j.issn.1004-406X.2020.03.05
28.
Chen X Zhuang YF Sun Y Wang SB Zhang FS Pan SF et al . The mid-to-long term efficacy of open-door laminoplasty for cervical ossification of posterior longitudinal ligament. Chin J Spine Spinal Cord. (2015) 25:1057–62. doi: 10.3969/j.issn.1004-406X.2015.12.01
29.
Lin S Lin T Wu Z Chen G Shangguan Z Wang Z et al . Does the asymmetry and extension function of the preoperative cervical paraspinal extensor predict postoperative cervical sagittal deformity in patients who undergo modified laminoplasty?Spine J. (2022) 22:1953–63. doi: 10.1016/j.spinee.2022.07.099
30.
Hu W Li S Shi H Li Y Qiu J Zhou J et al . Preoperative decreased hounsfield unit values of cervical vertebrae and the relative cross-sectional area of flexion/extension paraspinal muscles are novel risk factors for the loss of cervical lordosis after open-door laminoplasty. J Clin Med. (2023) 12:2119 doi: 10.3390/jcm12062119
31.
Niu Y Lv Q Gong C Duan D Zhou Z Wu J . Predictive effect of cervical sagittal parameters and corresponding segmental paravertebral muscle degeneration on the occurrence of cervical kyphosis following cervical laminoplasty. World Neurosurg. (2023) 175:e723–9. doi: 10.1016/j.wneu.2023.04.011
32.
Beneck GJ Kulig K . Multifidus atrophy is localized and bilateral in active persons with chronic unilateral low back pain. Arch Phys Med Rehabil. (2012) 93:300–6. doi: 10.1016/j.apmr.2011.09.017
33.
Latremoliere A Woolf CJ . Central sensitization: a generator of pain hypersensitivity by central neural plasticity. J Pain. (2009) 10:895–926. doi: 10.1016/j.jpain.2009.06.012
34.
Naghdi N Elliott JM Weber MH Fehlings MG Fortin M . Morphological changes of deep extensor neck muscles in relation to the maximum level of cord compression and canal compromise in patients with degenerative cervical myelopathy. Glob Spine J. (2024) 14:1184–92. doi: 10.1177/21925682221136492
35.
Wong AYL Harada G Lee R Gandhi SD Dziedzic A Espinoza-Orias A et al . Preoperative paraspinal neck muscle characteristics predict early onset adjacent segment degeneration in anterior cervical fusion patients: a machine-learning modeling analysis. J Orthop Res. (2021) 39:1732–44. doi: 10.1002/jor.24829
36.
Megía García Á Serrano-Muñoz D Bravo-Esteban E Ando Lafuente S Avendaño-Coy J Gómez-Soriano J . Analgesic effects of transcutaneous electrical nerve stimulation (TENS) in patients with fibromyalgia: a systematic review. Aten Primaria. (2019) 51:406–15. doi: 10.1016/j.aprim.2018.03.010
37.
Honaker JS Forston MR Davis EA Weisner MM Morgan JA Sacca E . The effect of adjunctive noncontact low frequency ultrasound on deep tissue pressure injury. Wound Repair Regen. (2016) 24:1081–8. doi: 10.1111/wrr.12479
38.
Yilmaz M Tarakci D Tarakci E . Comparison of high-intensity laser therapy and combination of ultrasound treatment and transcutaneous nerve stimulation on cervical pain associated with cervical disc herniation: a randomized trial. Complement Ther Med. (2020) 49:102295. doi: 10.1016/j.ctim.2019.102295
Summary
Keywords
degenerative cervical myelopathy, laminoplasty, posterior cervical muscles, functional rehabilitation, axial symptoms
Citation
Zhang Z, Zhao Y, Zhao H, Zhou M, Yang Y, Luo Z, Tong J, Cui G, Li T and Zhou F (2025) Impact of pre-operative cervical spine function on post-operative functional rehabilitation in patients after laminoplasty. Front. Neurol. 16:1706836. doi: 10.3389/fneur.2025.1706836
Received
16 September 2025
Accepted
03 November 2025
Published
26 November 2025
Volume
16 - 2025
Edited by
Ye Li, Hong Kong Polytechnic University, Hong Kong SAR, China
Reviewed by
Mingzhen Li, China-Japan Friendship Hospital, China
Chaofan Han, Capital Medical University, China
Updates
Copyright
© 2025 Zhang, Zhao, Zhao, Zhou, Yang, Luo, Tong, Cui, Li and Zhou.
This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guoqing Cui, drcuiguoqing1964@126.com; Tao Li, tobetheone@126.com; Feifei Zhou, zhoufeifei@bjmu.edu.cn
†These authors have contributed equally to this work
Disclaimer
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article or claim that may be made by its manufacturer is not guaranteed or endorsed by the publisher.