- 1Division of Surgical Nursing, Nursing Department, Faculty of Health Sciences, Bayburt University, Bayburt, Türkiye
- 2Division of Surgical Nursing, Nursing Department, Faculty of Health Sciences, Istanbul Aydın University, Istanbul, Türkiye
- 3Department of Medical Biology, Faculty of Medicine, Malatya Turgut Özal University, Malatya, Türkiye
- 4Division of Surgical Nursing, Nursing Department, Faculty of Health Sciences, Kahramanmaraş Sütçü İmam University, Kahramanmaraş, Türkiye
Background: Postoperative kinesiophobia and gastrointestinal (GI) disorders are common and undesirable conditions following orthopedic surgery. Additionally, managing both conditions is crucial for preventing complications and accelerating recovery. The purpose of this study is to investigate the effects of kinesiophobia on GI disorders after lower extremity orthopedic surgery.
Method: This study was conducted with a descriptive and cross-sectional design. The sample consisted of a total of n = 299 patients who underwent orthopedic surgery in their lower extremities at the orthopedics and traumatology clinic of a research and training hospital located in Turkey. A personal information form, the Tampa Scale of Kinesiophobia (TSK), and the Gastrointestinal Symptom Rating Scale (GSRS) were used to collect data, and the obtained data were analyzed using descriptive statistics, one-way analysis of variance (ANOVA), paired-samples t-test, and post hoc tests when necessary.
Results: While 24.4% of the patients were aged 65–74 years, 51.5% were male. The mean total TSK score of the patients was above average (49.36 ± 8.74), while their mean total GSRS score was below average (31.22 ± 11.7). In our study, as kinesiophobia increased, the frequency of bowel movements decreased, and kinesiophobia explained 19.9% of the variance in GI disorders (p < 0.05).
Conclusions: Kinesiophobia is a significant predictor of GI disorders in patients who underwent lower extremity surgery. Returning to normal GI function after surgery is crucial for preventing complications in patients with lower extremity surgery. Uncontrolled kinesiophobia after surgery exacerbates GI disorders. Therefore, early diagnosis and management of both kinesiophobia and GI disorders are necessary for rapid recovery in patients with lower extremity surgery.
Introduction
Orthopedic surgery is considered the most intense procedure in terms of perceived pain during the postoperative period (1). Postoperative pain can lead patients to have anxiety and functional loss, causing kinesiophobia, where they become trapped in a vicious cycle and are unable to overcome this condition (2, 3). Kinesiophobia is an irrational fear that develops resistance to movement as a result of negative emotions such as pain or re-injury (4, 5). It is a psychological response to avoiding the fear of movement (6). While the fear experienced in the initial days after surgery to promote mobility of the operated limb is considered a natural phenomenon, it should be resolved as soon as possible because unresolved fear can turn into chronic kinesiophobia (7).
The incidence of kinesiophobia in orthopedic surgical patients has been reported to reach up to 52.8% (8). The patients who cannot cope with kinesiophobia and exhibit avoidance behavior towards movement may experience physical, physiological, and psychological problems such as depression, obsession, and lack of self-confidence (9–11). In the postoperative period, insufficient mobilization often leads to gastrointestinal (GI) disorders such as abdominal distention and constipation due to venous stasis and thrombus development, urinary retention, tissue integrity impairment, and slowing of peristalsis (12).
A previous study reported that 57.9% of the patients with orthopedic surgery experienced constipation in the period after their operation (13). The effect of early mobilization on GI functions is well-known, and surgical nurses have a responsibility to assess the GI system and perform effective interventions (14, 15). Various diseases have been reported to be associated with kinesiophobia in previous studies, including muscle and bone diseases and Parkinson's, as well as older people suffering from low back pain (16–19). Patients who have had lower extremity surgery may not be able to go to the toilet easily, so they need to ask for help from their companion or nurse. The patients may be embarrassed to say that they want to go to the toilet, which can result in constipation, indigestion, and ileus. The use of antibiotics and other medications after surgery can cause diarrhea. Other possible GI disorders in this patient group are not fully known. This study aimed to examine kinesiophobia and GI disorders in patients who have had lower extremity orthopedic surgery.
The hypotheses of this study are as follows:
H1: There are kinesiophobia and GI disorders in patients who received lower extremity orthopedic surgeries.
H0: Kinesiophobia and GI disorders are not associated with lower extremity orthopedic surgeries.
Materials and methods
Design and sample
This study had a descriptive and cross-sectional research method. The sample of the study consisted of patients who underwent lower extremity surgeries at the orthopedics and traumatology unit of a research and training hospital in eastern Turkey. A power analysis was performed for sample calculation, assuming a 0.05 margin of error and a 95% confidence interval, and a minimum of n = 196 patients were required to participate in the study. Due to possible data loss, this study included a total of n = 299 patients with lower extremity orthopedic surgery.
Inclusion and exclusion criteria
The following criteria were determined for the inclusion of patients in this study (i) having undergone lower extremity surgery at the orthopedics and traumatology unit of the hospital and being on the 2nd, 3rd or 4th postoperative day, (ii) being aged 18 years and above without any communication problems, (iii) providing consent to take part in the study; (iv) having no diagnosed GI disorders/diseases before the surgery. Conditions contradicting the inclusion criteria were considered to be the exclusion criteria. In addition, those with GI disorders before surgery, preoperative disability and permanent physical disabilities, lumbar disc herniation, Parkinson's disease, or other neurological diseases were excluded.
Data collection
The data were collected prospectively by the researchers in face-to-face interviews between February 1, 2022, and August 1, 2022. Each patient provided informed consent in written and verbal form. For patients who were illiterate, the data collection forms were read by the researchers, and the responses of the patients were marked on the form. Patients who were literate filled out the data collection forms by themselves. The data collection process was conducted in patient rooms and took an average of 30 min. Patients who completed 48 h postoperatively (between 48 and 96 h) and were allowed to mobilize by the physician were included in the sample.
Data collection instruments
Data were obtained using a personal information form, the Tampa Scale of Kinesiophobia (TSK), and the Gastrointestinal Symptom Rating Scale (GSRS).
Personal information form
The personal information form was developed by the researchers with expert consultation. It included questions designed to collect information on the socio-demographic characteristics of the patients (age, sex, marital status, occupation, education and income level), and health-related questions.
Gastrointestinal symptom rating scale (GSRS)
The GSRS was created by Revicki et al. (1998) to assess commonly occurring symptoms in gastrointestinal conditions (20). The validity and reliability study of the scale in Turkish was conducted by Turan et al. (2017) (21). The GSRS measures how patients have been feeling in the context of GI disorders in the past week. It consists of 15 items and 5 subscales, namely reflux (2 items), dyspepsia (4 items), diarrhea (3 items), constipation (3 items), and abdominal pain (3 items). Higher GSRS scores show a higher severity of the relevant disorders. Turan et al. reported the Cronbach's alpha internal consistency coefficient of the GSRS to be 0.82. In this study, the Cronbach's alpha coefficient of the scale was determined to be 0.81.
Tampa Scale for Kinesiophobia (TSK)
The TSK was developed by Swinkels-Meewisse et al. (2003) (22). The validity and reliability tests of the TSK in Turkish were performed by Yılmaz et al. (2011) (23). The TSK has 17 items to measure fear of movement, including 4 reverse-scored items (4, 8, 12, and 16). It includes parameters that detect fear or avoidance of injury/reinjury related to work-related activities. It uses a 4-point Likert-type scoring system (1 = strongly disagree, 4 = strongly agree), and its total score varies between 17 and 68. Higher total scores indicate higher levels of kinesiophobia (23).
Statistical analysis
The data that were collected in this study were analyzed using the Statistical Package for the Social Sciences (SPSS) 25.0 IBM (Armonk, NY), and the evaluations included the calculation of descriptive statistics. Prior to the analysis, the Kolmogorov–Smirnov test was utilized to test whether the data were normally distributed. The one-way analysis of variance (ANOVA) and paired-samples t-test methods were used to identify the differences between the scale scores of the patients based on their descriptive characteristics. The Cronbach's alpha internal consistency coefficient, which is used as a measure of reliability, was calculated for the scales. Post hoc analyses were performed to determine the source of differences identified in ANOVA. Linear regression analysis was conducted to determine the predictors of variables among the scale total scores. Pearson correlation test was used to compare the scores of the scale and sub-dimensions. The results of the analyses were interpreted withing a 95% confidence interval and at a significance level of p < 0.05.
Ethical considerations
For conducting the study, necessary legal permissions were received from the Institutional Review Board (IRB) of Turgut Özal Medical Center and the Ethics Committee of İnönü University (Date: 11.01.2022, Decision No: 2022/2954, Number: 01). In accordance with the Declaration of Helsinki, the researcher informed the patients about the study. Those who agreed to take part in the study were included after they provided verbal and written consent.
Results
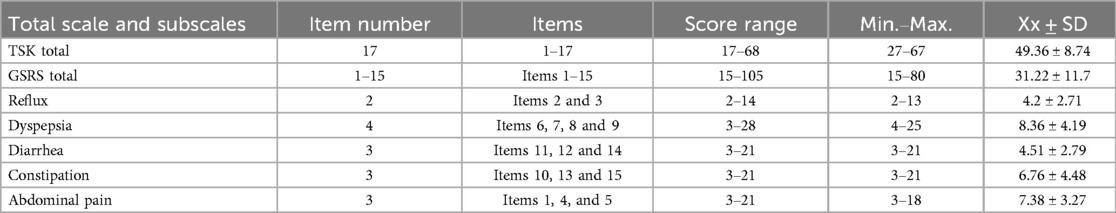
Table 1 presents the sociodemographic characteristics of the patients, as well as their GSRS and TSK mean scores, parametric test results, and post hoc test results. Of the patients, 24.4% were aged between 65 and 74, 51.5% were men, and 79.6% were married. In addition, 20.7% of the patients had tibia fracture surgery, 15.4% had total hip arthroplasty, and 11.4% had femur fracture repair. The percentage of patients who had one bowel movement per day before lower extremity surgery was 70.9%, which decreased to 38.5% after the surgery. The patients aged 75 years and above were more kinesiophobic compared to other age groups, and the retirees were more kinesiophobic compared to other occupational groups. As the TSK scores increased, the frequency of stool after surgery decreased, and this relationship was determined be significant.
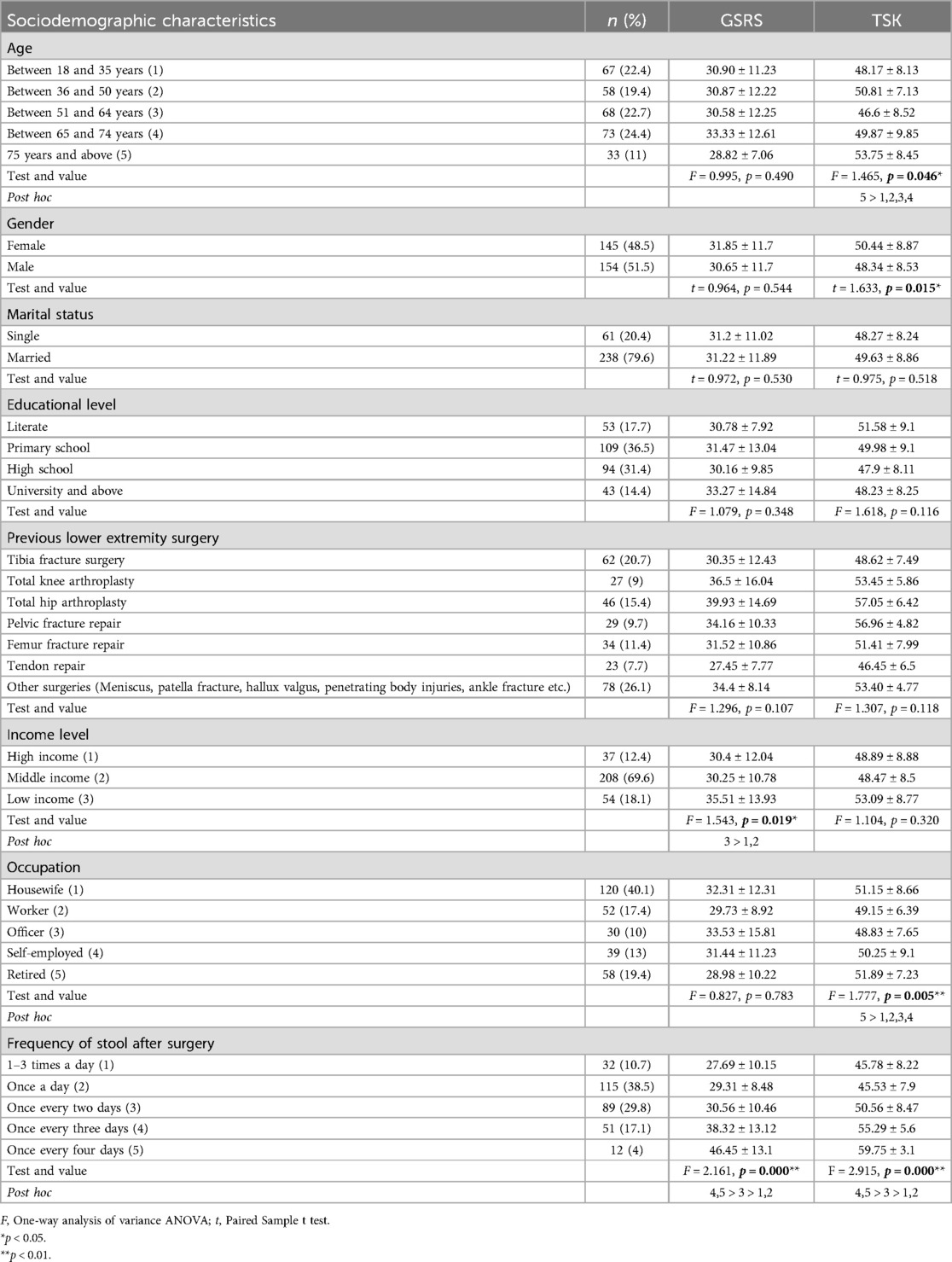
Table 1. Sociodemographic characteristics, GSRS and TSK mean scores, parametric and post hoc tests results for patients with lower extremity surgery (n = 299).
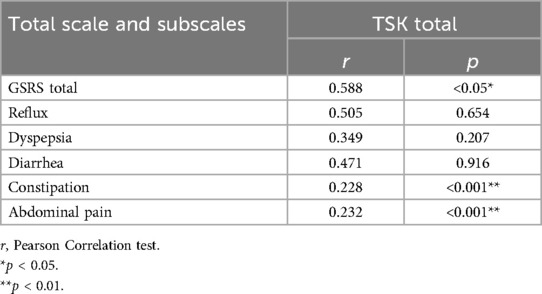
Table 2 shows the patients’ TSK and GSRS mean scores. Their TSK and GSRS total mean scores were 49.36 ± 8.74 and 31.22 ± 11.7, respectively. Their GSRS subscales mean scores were as follows: Reflux 4.2 ± 2.71, Dyspepsia 8.36 ± 4.19, Diarrhea 4.51 ± 2.79, Constipation 6.76 ± 4.48, and Abdominal Pain 7.38 ± 3.27.
Table 3 displays the results of the linear regression analysis including the TSK and GSRS scores of the patients. According to these results, kinesiophobia explained 19.9% of the variance in GI disorders (R-squared = 0.199).
Table 4 shows the correlation analysis between TSK and GSRS. According to the correlation analysis, there was a positive, strong and statistically significant correlation between kinesiophobia and constipation/abdominal pain (p < 0.001). There was a positive, moderate and statistically significant correlation between the total scores of TSK and GSRS (p < 0.05).
Discussion
Kinesiophobia and GI disorders were examined in patients who have had lower extremity orthopedic surgery in this study. Age and gender affected the level of kinesiophobia. Since retired people are generally older people, the effect of employment status on kinesiophobia is an indirect effect. The relationship between kinesiophobia and frequency of stool after surgery was quite interesting, those who had more stool output were less kinesiophobic. Having a stool with someone's help or using a bedpan in bed is a very difficult experience. Patients may have preferred to go to the toilet alone rather than experience this difficulty and may have reduced their kinesiophobia. Every surgical procedure involves a controlled injury. Patients experience postoperative pain associated with surgical incisions. Although postoperative pain can be managed, it is often an inevitable experience (24, 25). Most of the time, patients avoid moving during the postoperative period due to pain. Patients who undergo lower extremity orthopedic surgery experience a high level of kinesiophobia in the early days after surgery (26). Kinesiophobia can lead to several problems in various body systems (12). In this context, kinesiophobia can slow down GI peristalsis and trigger various issues, including constipation (13, 14). From this perspective, it is very important to detect kinesiophobia and GI disorders in patients with lower extremity orthopedic surgery.
In this study, 24.4% of the patients were 65–74 years old, 51.5% were men, 79.6% were married, and 20.7% had tibia fracture surgery. Additionally, the patients aged 75 years and above were more kinesiophobic compared to other age groups, and the retirees were more kinesiophobic compared to other occupational groups. De Vroey et al. found kinesiophobia in patients who underwent lower extremity orthopedic surgery (27). Değirmenci et al. emphasized the development of kinesiophobia due to anesthesia in patients who underwent hip arthroplasty (26). Particularly in the elderly, transitioning to a less active lifestyle and increase in the incidence of falls may cause them to have kinesiophobia after lower extremity orthopedic surgery. The results related to kinesiophobia in the sample in this study are similar to the results of other studies in the literature.
According to these results, kinesiophobia is a predictor for the development of GI disorders, in this context it explained 19.9% of the variance in GI disorders. At the same time, the correlation analysis draws attention to the strong and positive correlation between kinesiophobia and constipation/abdominal pain. Park et al. reported a finding that was similar to ours, stating that the frequency of bowel movements decreased by half after surgery. They also indicated that patients with kinesiophobia and constipation had impaired adaptation to daily life activities (13). The results that were found in our study were in agreement with those in the relevant literature.
Early ambulation and mobilization are of great importance for the return of gastrointestinal activities during the postoperative period (28, 29). Approaches implemented within the Enhanced Recovery After Surgery (ERAS) protocol can eliminate the negative effects of stress responses in surgical patients and enable them to quickly transition to the discharge process. However, kinesiophobic patients tend to hinder this positive progress (14, 30). In the ERAS protocol, it is recommended for surgical patients to mobilize within 24 h at the latest and spend 2 h outside the bed on the day of surgery and 6 h on the following days. Kinesiophobia is one of the important obstacles to postoperative mobilization and can prolong morbidity by triggering GI disorders. Physicians do not want to discharge patients who are not well mobilized, and the treatment and kinesiophobia can reduce compliance of care and treatment.
A statistically significant and moderate level of correlation was identified between kinesiophobic behaviors and GI disorders in this study. Altay and Celenay found a statistically significant relationship between kinesiophobia and GI disorders in patients with migraines (31). Previous studies have noted that kinesiophobia resulted in a slowdown in daily life activities and functions in patients who underwent lower extremity orthopedic surgery (32), decreased their recovery speed (27, 33), and increased their perceived surgical pain (34). Reluctance to mobilize due to kinesiophobia, combined with slow blood circulation caused by anesthesia and physical energy deficiency, can lead to a slowdown in not only GI peristalsis but also other body system functions. This can cause various problems such as atelectasis, deep vein thrombosis, delayed wound healing, and increased stress response (14). Other predictors of postoperative GI disorders include various medication uses (35–37), depression (38), inability to relax (34), surgical pain (24), and infection (39).
In the present study was identified that kinesiophobia as a significant predictor of GI disorders, and these results will increase awareness of kinesiophobia among clinicians. The results of our study are specific to our sample and may not be generalizable to the general public. GI disorders in the patients may be due to their dietary habits, and the patients were still using medications during the postoperative period, which could have triggered their GI disorders. The stress caused by the surgery may have accelerated GI peristalsis, which may have caused diarrhea, poor pain management, and triggered knesiophobia. Pain and stress were not defined in this study. All of these factors can be considered as limitations for our study.
Conclusion
In patients with lower extremity surgery, GI disorders are influenced by kinesiophobia. Early initiation of GI peristalsis after surgery is of great importance in preventing possible complications. Similarly, preventing kinesiophobia can facilitate social integration and shorten the length of hospital stay. Uncontrolled kinesiophobia can increase GI peristalsis, thus encouraging clinicians to use medication methods to ensure peristalsis. This situation requires additional medication use. Therefore, in addition to preventive interventions against kinesiophobia (such as playing calming music, mindfulness interventions, etc.), non-pharmacological methods such as abdominal massage, sufficient dietary fiber intake, liquid diet, and bed mobility exercises should be used to eliminate GI disorders.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by for conducting the study, necessary legal permissions were received from the Institutional Review Board (IRB) of Turgut Özal Medical Center and the Ethics Committee of İnönü University (Date: 11.01.2022, Decision No: 2022/2954, Number: 01). In accordance with the Declaration of Helsinki, the researcher informed the patients about the study. Those who agreed to take part in the study were included after they provided verbal and written consent. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HG: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Project administration, Supervision, Visualization, Writing – original draft, Writing – review & editing. SB: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SS: Conceptualization, Formal analysis, Funding acquisition, Investigation, Methodology, Resources, Writing – original draft, Writing – review & editing. AO: Data curation, Investigation, Software, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Lin CL, Hwang SL, Jiang P, Hsiung NH. Effect of music therapy on pain after orthopedic surgery-a systematic review and meta-analysis. Pain Pract. (2020) 20(4):422–36. doi: 10.1111/papr.12864
2. Filardo G, Merli G, Roffi A, Marcacci T, Berti Ceroni F, Raboni D, et al. Kinesiophobia and depression affect total knee arthroplasty outcome in a multivariate analysis of psychological and physical factors on 200 patients. Knee Surg Sport Traumatol Arthrosc. (2017) 25(11):3417–23. doi: 10.1007/s00167-016-4201-3
3. Cai L, Gao H, Xu H, Wang Y, Lyu P, Liu Y. Does a program based on cognitive behavioral therapy affect kinesiophobia in patients following total knee arthroplasty? A randomized, controlled trial with a 6-month follow-up. J Arthroplasty. (2018) 33(3):704–10. doi: 10.1016/j.arth.2017.10.035
4. Norte GE, Solaas H, Saliba SA, Goetschius J, Slater LV, Hart JM. The relationships between kinesiophobia and clinical outcomes after ACL reconstruction differ by self-reported physical activity engagement. Phys Ther Sport. (2019) 40:1–9. doi: 10.1016/j.ptsp.2019.08.002
5. Duport A, Pelletier R, Martel M, Léonard G. The influence of kinesiophobia and pain catastrophizing on pain-induced corticomotor modulation in healthy participants: a cross sectional study. Neurophysiol Clin. (2022) 52(5):375–83. doi: 10.1016/j.neucli.2022.08.001
6. Theunissen WWES, van der Steen MC, Liu WY, Janssen RPA. Timing of anterior cruciate ligament reconstruction and preoperative pain are important predictors for postoperative kinesiophobia. Knee Surgery, Sport Traumatol Arthrosc. (2020) 28(8):2502–10. doi: 10.1007/s00167-019-05838-z
7. Najafi F, Zare Z, Javad Mortazavi SM, Lundberg M, Shahsavari H. Overcoming fear of movement resulting from knee replacement; strategies used by patients: an interview study. Int J Orthop Trauma Nurs. (2022) 45(July 2021):100904. doi: 10.1016/j.ijotn.2021.100904
8. Morgounovski J, Vuistiner P, Léger B, Luthi F. The fear–avoidance model to predict return to work after an orthopedic trauma. Ann Phys Rehabil Med. (2016) 59:e110–1. doi: 10.1016/j.rehab.2016.07.246
9. Bäck M, Cider Å, Herlitz J, Lundberg M, Jansson B. The impact on kinesiophobia (fear of movement) by clinical variables for patients with coronary artery disease. Int J Cardiol. (2013) 167(2):391–7. doi: 10.1016/j.ijcard.2011.12.107
10. Er G, Angin E. Determining the relationship of kinesiophobia with respiratory functions and functional capacity in ankylosing spondylitis. Med. (2017) 96(29):e7486. doi: 10.1097/MD.0000000000007486
11. Hudes K. The Tampa scale of kinesiophobia and neck pain, disability and range of motion: a narrative review of the literature. J Can Chiropr Assoc. (2011) 55(3):222–32. doi: 10.1097/MD.0000000000007486
12. Yolcu S, Akin S, Durna Z. The evaluation of mobility levels of postoperative patients and associated factors. J Educ Res Nurs. (2016) 13(2):129–38. doi: 10.5222/HEAD.2016.129
13. Park JH, Yun SO, Kim SH, Yu MG, Ham EJ. Constipation in patients following orthopedic surgery: incidence and influencing factors. Korean J Adult Nurs. (2016) 28(6):637–45. doi: 10.7475/kjan.2016.28.6.637
14. Kırtıl I, Kanan N. Effect of early mobilization on gastrointestinal functions after abdominal surgery: systematic review [abdominal cerrahi girişim sonrası erken mobilizasyonun gastrointestinal İşlevlere etkisi: sistematik derleme]. Arch Med Rev J. (2021) 30(3):166–76. doi: 10.17827/aktd.873681
15. Irmak B, Bulut H. Use of non-pharmacological methods to increase intestinal functions after abdominal surgery: what do say evidences?[abdominal cerrahi sonrasında bağırsak fonksiyonlarını artırmada farmakolojik olmayan yöntemlerin kullanımı: kanıtlar ne diyor?]. Istanbul Gelisim Univ J Health Sci. (2021) 14(14):336–50. doi: 10.38079/igusabder.957817
16. Monticone M, Ferrante S, Ambrosini E, Rocca B, Secci C, Foti C. Development of the Tampa scale of kinesiophobia for Parkinson’s disease: confirmatory factor analysis, reliability, validity and sensitivity to change. Int J Rehabil Res. (2015) 38(2):113–20. doi: 10.1097/MRR.0000000000000095
17. Burwinkle T, Robinson JP, Turk DC. Fear of movement: factor structure of the Tampa scale of kinesiophobia in patients with fibromyalgia syndrome. J Pain. (2005) 6(6):384–91. doi: 10.1016/j.jpain.2005.01.355
18. Weiner DK, Haggerty CL, Kritchevsky SB, Harris T, Simonsick EM, Nevitt M, et al. How does low back pain impact physical function in independent, well-functioning older adults? Evidence from the health ABC cohort and implications for the future. Pain Medicine. (2003) 4(4):311–20. doi: 10.1111/j.1526-4637.2003.03042.x
19. Wood DW, Haig AJ, Yamakawa KS. Fear of movement/(re) injury and activity avoidance in persons with neurogenic versus vascular claudication. Spine J. (2012) 12(4):292–300. doi: 10.1016/j.spinee.2012.02.015
20. Revicki DA, Wood M, Wiklund I, Crawley J. Reliability and validity of the gastrointestinal symptom rating scale in patients with gastroesophageal reflux disease. Qual Life Res. (1997) 7(1):75–83. doi: 10.1023/A:1008841022998
21. Turan N, Aşt TA, Kaya N. Reliability and validity of the turkish version of the gastrointestinal symptom rating scale. Gastroenterol Nurs. (2017) 40(1):47–55. doi: 10.1097/SGA.0000000000000177
22. Swinkels-Meewisse EJCM, Swinkels RAHM, Verbeek ALM, Vlaeyen JWS, Oostendorp RAB. Psychometric properties of the Tampa scale for kinesiophobia and the fear-avoidance beliefs questionnaire in acute low back pain. Man Ther. (2003) 8(1):29–36. doi: 10.1054/math.2002.0484
23. Yilmaz OT, Yakut Y, Uygur F, Uluǧ N. Turkish version of the Tampa scale for kinesiophobia and its test-retest reliability. Fiz Rehabil. (2011) 22(1):44–9. Available at: https://dergipark.org.tr/en/download/article-file/138103
24. Eti Aslan F, Kula Şahin S, Seçginli S, Bülbüloğlu S. Patient satisfaction with nursing practices about postoperative pain management: a systematic review. Pain J. (2018) 30(3):105–15. doi: 10.5505/agri.2018.96720
25. Kapikiran G, Bulbuloglu S, Gunes H, Saritas S, Demir B. A randomized controlled trial of reflexology effect after abdominal surgery on patient satisfaction, pain and vital signs. Explore (NY). (2023) 19(4):565–70. doi: 10.1016/j.explore.2022.10.017
26. Degirmenci E, Ozturan KE, Kaya YE, Akkaya A, Yucel İ. Effect of sedation anesthesia on kinesiophobia and early outcomes after total knee arthroplasty. J Orthop Surg. (2020) 28(1):1–6. doi: 10.1177/2309499019895650
27. De Vroey H, Claeys K, Shariatmadar K, Weygers I, Vereecke E, Van Damme G, et al. High levels of kinesiophobia at discharge from the hospital may negatively affect the short-term functional outcome of patients who have undergone knee replacement surgery. J Clin Med. (2020) 9(3):1–12. doi: 10.3390/jcm9030738
28. Wang J, Chen K, Li X, Jin X, An P, Fang Y, et al. Postoperative adverse events in patients with diabetes undergoing orthopedic and general surgery. Med (United States). (2019) 98(14):1–7. doi: 10.1097/MD.0000000000015089
29. Uğurlu AK, Kula Şahin S, Seçginli S, Eti Aslan F. The effect of standing up early in the first 24 hours after surgery on rapid improvement: systematic review, [Ameliyat sonrası İlk 24 saatte erken ayağa kaldırmanın hızlı İyileşmeye etkisi: sistematik derleme]. Turkiye Klinikleri J Nurs Sci. (2017) 9(4):280–8. doi: 10.5336/nurses.2016-53678
30. Wei S, Li L, Yang X, Li X, Jiang Q. Psychological interventions in the pain management after hip and knee arthroplasty: a mini review. Ann Jt. (2020) 5(3):13. doi: 10.21037/aoj.2019.12.06
31. Altay H, Celenay ST. An investigation of the relationship between cutaneous allodynia and kinesiophobia, gastrointestinal system symptom severity, physical activity and disability in individuals with migraine. Korean J Pain. (2023) 36(1):137–46. doi: 10.3344/kjp.22327
32. Dai Y, Chai X, Zhu N, Wang K, Bao W, Zhang X, et al. Analgesia effect of premixed nitrous oxide/oxygen during the rehabilitation after total knee arthroplasty: a study protocol for a randomized controlled trial. Trials. (2019) 20:399. doi: 10.1186/s13063-019-3472-7
33. Güney-Deniz H, Irem Kınıklı G, Çağlar Ö, Atilla B, Yüksel İ. Does kinesiophobia affect the early functional outcomes following total knee arthroplasty? Physiother Theory Pract. (2017) 33(6):448–53. doi: 10.1080/09593985.2017.1318988
34. Cici R, Bulbuloglu S, Kapikiran G. Effect of meditation music and comedy movie interventions on postoperative kinesiophobia and pain in patients undergoing total knee arthroplasty. ANZ J Surg. (2022) 93:302–9. doi: 10.1111/ans.18209
35. Saritaş S, Özdemir A. The effect of immunosuppressant therapy adherence on the comfort of liver transplant recipients. Gastroenterol Nurs. (2021) 44(5):334–40. doi: 10.1097/SGA.0000000000000571
36. Guneş H, Bulbuloglu S, Saritas S. Investigation of adherence to immunosuppressive therapy and spiritual well-being in liver recipients. J Transplant Immunology. (2022) 72:101585. doi: 10.1016/j.trim.2022.101585
37. Çınar F, Bulbuloglu S. The effect of adherence to immunosuppressant therapy on gastrointestinal complications after liver transplantation. J Transplant Immunology. (2022) 71:101554. doi: 10.1016/j.trim.2022.101554
38. Browne JA, Sandberg BF, D'Apuzzo MR, Novicoff WM. Depression is associated with early postoperative outcomes following total joint arthroplasty: a nationwide database study. J Arthroplasty. (2014) 29(3):481–3. doi: 10.1016/j.arth.2013.08.025
Keywords: fear of moving, gastrointestinal disorders, GI symptoms, kinesiophobia, lower extremity, orthopedic surgery, postoperative care
Citation: Gunes H, Bulbuloglu S, Saritas S and Ozdemir A (2025) The effect of kinesiophobia on gastrointestinal disorders in patients with lower extremity orthopedic surgery. Front. Surg. 12:1457474. doi: 10.3389/fsurg.2025.1457474
Received: 30 June 2024; Accepted: 31 March 2025;
Published: 25 April 2025.
Edited by:
Ozgur Karcioglu, University of Health Sciences, TürkiyeReviewed by:
Vitor Marques, Universidade Federal de Goiás, BrazilHugo Sanchez, Universidade Federal de Jataí (UFJ), Brazil
Copyright: © 2025 Gunes, Bulbuloglu, Saritas and Ozdemir. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Semra Bulbuloglu, c2VtcmFidWxidWxvZ2x1QGF5ZGluLmVkdS50cg==
 Huseyin Gunes
Huseyin Gunes Semra Bulbuloglu
Semra Bulbuloglu Serdar Saritas
Serdar Saritas Ahmet Ozdemir
Ahmet Ozdemir