- 1Department of Woman, Child and General and Specialized Surgery, University of Campania “Luigi Vanvitelli”, Naples, Italy
- 2Gynecology and Obstetrics Unit, Department of Human Pathology of Adult and Childhood “G. Barresi”, University of Messina, Messina, Italy
- 3Department of General Surgery and Medical Surgical Specialties, University of Catania, Catania, Italy
Objectives: This study aims to compare the outcomes of laparoscopic colposuspension sec Shull (LCSS) and laparoscopic colposacropexy (LCSP) with and without the addition of cystopexy for the treatment of pelvic organ prolapse (POP) in terms of postoperative complications, recurrence rates, and overall effectiveness.
Materials and methods: A retrospective case-control analysis was conducted on women treated for grade 3–4 POP-Q uterine prolapse at the Academic Departments of Gynaecology and Obstetrics of “G. Martino” of Messina, Italy, and “L. Vanvitelli” of Napoli, Italy, between November 2020 and February 2022. Group A consisted of patients who underwent laparoscopic hysterectomy followed by LCSS or LCSP without cystopexy. At the same time, Group B included patients who had the same procedures with the addition of cystopexy. Data on complications were collected using the Clavien-Dindo classification, and prolapse recurrence was monitored according to the POP-Q system. Statistical analysis was performed using Fisher's exact, Chi-squared, and Wilcoxon rank-sum tests.
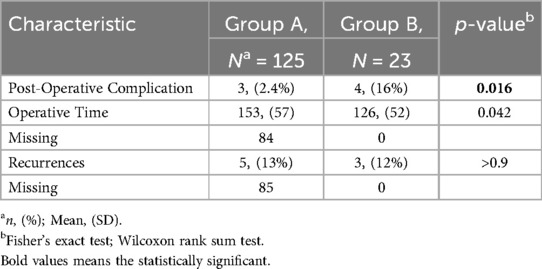
Results: A total of 148 patients were included, with 125 in Group A and 23 in Group B. Group B showed a significantly higher rate of postoperative complications (16%) compared to Group A (2.4%) (p = 0.016), with an Odds Ratio of 7.62 (95% CI 1.59–36.51, p = 0.0017). No significant difference between the groups was found in the recurrence rate of prolapse at 24 months (p > 0.9).
Conclusion: Adding cystopexy to LCSS or LCSP increases the risk of postoperative complications without reducing prolapse recurrence rates. Further research is needed to identify patients who may benefit from cystopexy and to evaluate its impact on stress incontinence and patient satisfaction.
Highlights
Comparison of LCSS and LCSP with and without cystopexy for pelvic organ prolapse showed a significant increase in postoperative complications with cystopexy (16% vs. 2.4%). No significant difference was found in prolapse recurrence rates at 24 months.
Introduction
Pelvic Organ Prolapse (POP) represents a significant health concern for women, affecting both their quality of life and daily functioning. It is estimated that 40% of women suffer from POP, particularly those over 50 years old, with a peak in incidence in women between 60 and 69 years old (1–3). Various non-surgical and surgical interventions have been developed to address POP and improve overall quality of life. Among the surgical options, the laparoscopic ones have gained prominence due to their minimally invasive nature, increased visualization of anatomic structures, and decreased risk of intraoperative complications such as ureteral damage (4–9). Laparoscopic colposuspension sec Shull (LCSS) and laparoscopic Colposacropexy (LCSP) are among the most commonly performed laparoscopic surgical interventions for POP (10, 11). LCSS is a technique that involves suspending the vaginal apex high to the uterosacral ligaments to restore the normal position of the vaginal vault and support the pelvic organs. On the other hand, LCSP entails attaching the vaginal vault to the promontories of the sacrum using a mesh, which provides robust support and solves the prolapse. Both procedures are used to resolve central compartment prolapse. Often, it is associated with anterior compartment prolapse, with varying degrees of cystocele. For this reason, cystopexy surgeries can often be combined to resolve anterior compartment defects as well. Moreover, cystopexy can also be performed to prevent stress incontinence that may develop after surgery for POP (12–16). Despite the efficacy of both procedures with or without the addition of cystopexy, comparative studies on outcomes of these two approaches exploring long-term durability of repairs, recurrence rates and complications remain underexplored. The aim of the present study is to fill this gap by comparing LCSS and LCSP without cystopexy to LCSS and LCSP with cystopexy to provide comprehensive insights on the postoperative outcomes that will guide the surgeon on clinical decision-making and will help to optimize patient care in the management of pelvic organ prolapse.
Materials and methods
The present study is a retrospective case-control analysis carried out on women surgically treated for grade 3–4 POP-Q Uterine prolapse at the Academic Department of Gynaecology and Obstetrics of Azienda Ospedaliera Policlinico Universitario “G. Martino” of Messina, Italy, and at Azienda Ospedaliera Universitaria “L. Vanvitelli” of Napoli, Italy, between November 2020 and February 2022. Patients' data were retrieved from hospital medical records. All the patients were treated with laparoscopic hysterectomy followed by laparoscopic colpo-sacropexis (LCSP) or high uterosacral ligament suspension (LCSS) without other prolapse correction (Group A) and LCSP/LCSS associated with cystopexy for anterior defect (Group B). Urodynamic tests eventually confirmed concomitant urinary tract symptoms. All patients underwent a total hysterectomy in accordance with the clinical protocols of the recruiting centers. Additionally, all enrolled patients underwent urodynamic testing within 60 days prior to surgery.
In accord with the clinical practice of the institutions involved, cystopexy has been associated in cases of grade 2 or higher median cystocele with symptomatic repercussions by the patient or alterations reported on urodynamic tests. All included patients were treated surgically by 3 surgeons: CR, MT, and SC. All included surgeons have more than 5 years' experience in both vaginal and laparoscopic surgery for urodynamic correction. All patients are managed according to standardized clinical protocols with bladder catheter removal 48 h after surgery, bladder physiotherapy for the next 12 h, and discharge without complications on the third postoperative day. No antibiotic therapy in addition to preoperative prophylaxis is performed in the absence of complications. The timing of follow-up visits was set at 1, 3, 6, 12, and 24 months after surgery. Any complication in the first 30 days after surgery was recorded and classified according to the Clavien-Dindo classification (17). Also, prolapse recurrences were taken under control during Follow-ups.
Recurrence of anatomical prolapse was defined as any compartment descent stage II according to the POP-Q system (18).
Technique
The LCSP and LCSS techniques were performed laparoscopically with 3 standard 5-mm accesses in the pelvis and 10-mm transumbilical optics. All patients under study underwent hysterectomy prior to colposuspension following the steps described by Gueli Alletti et al. (11). LCSP was performed according to the steps described by Henniger et al. in 2015 (19, 20), and LCSS followed the steps described by Restaino et al. in 2016 (21). Cystopexy was, on the other hand, performed vaginally with colpoincision and raffia of the bladder fascia with natural vaginal tissue repair technique (NVTR) (22).
Statistical analysis
The primary endpoint was the rate of post-operative complications in the first 30 days. The null hypothesis (H0) of the primary endpoint of the study is devised as no difference in the prevalence of post-operative complications in the first 30 days in patients undergoing laparoscopic hysterectomy for uterine prolapse with colposuspension, compared to the same technique combined with cystopexy, (H0: π-π1 = 0; one-way). To test H0, the significance level α was set = 0.05. Fisher's exact test and Chi- squared test were used to calculate p in comparing dichotomous variables and Wilcoxon's test in the case of ordinal variables. Rejection of H0 for p ≤ α. The parameter of the presence or absence of postoperative complications in the first 30 days was estimated as a dichotomous prevalence variable. The effect of the addition of cystopexy on postoperative complications was expressed as an Odds Ratio (OR) with a 95% confidence interval. Quantitative variables such as age and BMI were expressed as medians. R software version 4.2.3 was used for statistical analysis.
Handling of missing data and sensitivity analysis
Missing data were addressed using multiple imputation techniques, ensuring the preservation of statistical power and reducing potential bias. The imputed values were cross-validated using complete case analysis to verify consistency. Sensitivity analyses involved excluding extreme values, testing alternative statistical models, and assessing subgroup-specific trends.
Ethical or institutional review board approval
The study was conducted in two university clinics where all patients treated must sign a dedicated consent for anonymous data processing. According to the regulations in force in the state where the study was conducted, no IRB is required due to the study's retrospective nature.
Results
148 patients were included in the study and divided into two groups: 125 women who underwent Laparoscopic hysterectomy plus laparoscopic colposuspension (LCSP/LCSS) were included in Group A; 23 patients who were treated with the same technique with the addition of cystopexy formed Group B. Table 1 describes the main characteristics of the groups.
The two groups were homogeneous regarding parity, BMI, Stamey Score, Age and prevalence of previous surgery. Data concerning previous laparotomy showed a statistical difference (12% Group B vs. 0% Group A; p = 0.004) in favor of Group B. Moreover, LCSP was statistically more frequent in Group A (71.2% vs. 21.7%; p < 0.001).
Outcomes
Operative time was comparable in the two groups (p = 0.042): mean surgery length is 153 min in LCSP or LCSS (data concerning 84 procedures are missing) and 126 min in colposuspension associated with cystopexy. The primary endpoint was the evaluation of post-operative complications. The post-operative complications rate in Group A was 2.4% compared to 16% in Group B (p = 0.016). Only 3 complications occurred in Group A and 4 in Group B. Adding cystopexy at the time of colposuspension resulted in a statistically significant Odds Ratio of 7.62 (95% CI 1.59–36.51; p = 0.017) to develop post-operative complications in the early 30 days. The secondary outcome was the recurrence rate of prolapse at 24 months. Group A presented a recurrence rate of 13% compared to 12% of Group B (p > 0.9). Surgical Outcomes are summarized in Table 2.
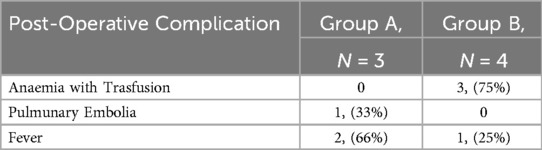
The types of complications are summarized in Table 3.
As reported in the previous paragraph, group A reported 3 complications: 1 case (33%) of pulmonary embolism and 2 cases (66%) of fever. On the other hand, group B reported 4 cases of postoperative complications: 3 patients had post-operative anemia with the necessity of blood transfusion (75%), and 1 patient had a post-operative fever (25%).
Discussion
Main findings
The present retrospective study demonstrates that adding cystopexy to LCSP or LCSS at the time of uterine prolapse treatment increases on 7 times the risk of postoperative complications in the early 30 days after surgery. The operation time seems to be slightly longer in group A (without cystopexy). However, the results of this outcome are weakened by a high presence of missing data and also could be attributed to the higher percentage of LCSP in group A. Moreover, cystopexy was not found to decrease the rate of prolapse recurrence when combined with LCSP or LCSS.
Interpretation of results and clinical significance
Despite the common use of cystopexy, there are only a few studies on its precise indications and post- operative complication rates.
As already demonstrated, the key advantage of the laparoscopic approach for POP treatment is the magnified view of the operative field, which facilitates easier dissection and a more precise suture placement, thus helping minimize potential damage to the ureter. These benefits align with existing literature demonstrating minimal ureteric injury rates associated with this laparoscopic procedure (6, 7, 23, 24).
Otherwise, it is used in continent women at the time of surgical correction of POP to prevent genuine stress after corrective surgery for urogenital prolapse (24). In particular, Fianu et al. showed that 16% of their patients developed stress incontinence following anterior colporrhaphy (14), and Stanton et al. (13) reported an incidence of 11%. In contrast, Colombo et al. (25) observed an overall incidence of 8% of significant stress incontinence that required further treatment in two cases. The underlying causes of genuine stress incontinence following prolapse surgery remain not fully understood. In the literature (13), no differences have been found in age, parity, weight, and past pelvic surgery between the subjects who remained continent postoperatively and those who did not. In addition, it has been shown that the addition of hysterectomy does not affect postoperative outcomes in the case of surgery for urodynamic correction, as long as the surgery is not related to other clinical conditions that may alter pelvic structures (26–28). Postoperative bladder neck descent because of ineffective urethorvescical junction stabilization, and/or periuretral fibrosis with urethral denervation seem to be direct consequences of stress incontinence after POP surgery (13, 29). Our research group has previously shown that corrective surgery with a purely laparoscopic approach has an increased risk of symptom recurrence and organ prolapse (30). We believe that the occurrence of stress incontinence after prolapse surgery may have a multifactorial origin. For this reason, although the preventive execution of cystopexy could play a fundamental role in reducing this undesirable outcome, it must be remembered that cystopexy is not free from potential postoperative complications. Therefore, a careful selection of patients who could genuinely benefit from this procedure should be conducted to avoid adding unnecessary risks.
Strengths and limitations
A major strength of the present study is its focus on cystopexy and its association with postoperative outcomes. Indeed, there are only a few studies in the literature regarding cystopexy, and most are outdated or in non-English language (23). Moreover, the cystopexy technique is never described in a standardized way. Nevertheless, all patients reported in the study underwent the same cystopexy methods by the Natural Vaginal Tissue repair technique. Hence, we believe that our work, besides presenting new data on the increased postoperative complications in patients undergoing cystopexy, also plays a fundamental role in highlighting the need for further studies helping in a better selection of patients.
A limitation of the present study is its retrospective nature, which limits the ability to establish causality and resulted in an abundance of “missing data” in the sample characteristics. This may limit the reproducibility of the study and its translation into clinical practice. Moreover, we have no data on post-surgical stress incontinence in the two groups with/without cystopexy, which is usually one of the main indications for cystopexy after surgery for POP (23). Hence, we would expect results in favor of adding the procedure routinely to prevent this unpleasant outcome. Moreover, since POP significantly impacts patients' quality of life, data on subjective patient satisfaction after surgical correction of POP would be needed, but they are still missing. Finally, laparoscopic and vaginal techniques involve two different skills, which may not coexist in the same operator (4, 31).
Therefore, the higher complication rate might be operator-dependent. Designs of prospective studies may clarify these doubts.
Conclusions
In conclusion, it seems that patients undergoing cystopexy after surgical correction of POP are at increased risk of serious post-operative complications. However, there are no data concerning patient satisfaction and the occurrence of post-surgical stress incontinence. Hence, further studies are surely needed to better select patients who may truly benefit from cystopexy after surgical correction of POP.
Data availability statement
All data and the methodological process for their calculation can be supplied under explicit request to the corresponding author and provided as an “.R” file.
Ethics statement
Ethical approval was not required for the study involving humans in accordance with the local legislation and institutional requirements. Written informed consent to participate in this study was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and the institutional requirements. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CR: Conceptualization, Formal analysis, Methodology, Project administration, Software, Supervision, Validation, Writing – original draft, Writing – review & editing. GA: Data curation, Investigation, Writing – original draft. PR: Writing – review & editing, Data curation, Formal analysis. GS: Writing – review & editing, Writing – original draft. MT: Writing – review & editing, Supervision, Validation, Visualization. SC: Writing – original draft, Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Campagna G, Vacca L, Panico G, Vizzielli G, Caramazza D, Zaccoletti R, et al. Laparoscopic high uterosacral ligament suspension vs. lparoscopic sacral colpopexy for pelvic organ prolapse: a case-control study. Front Med (Lausanne). (2022) 9:853694. doi: 10.3389/fmed.2022.853694
2. Handa VL, Garrett E, Hendrix S, Gold E, Robbins J. Progression and remission of pelvic organ prolapse: a longitudinal study of menopausal women. Am J Obstetr Gynecol. (2004) 190:27–32. doi: 10.1016/j.ajog.2003.07.017
3. Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. (2013) 24:1783–90. doi: 10.1007/s00192-013-2169-9
4. La Verde M, Riemma G, Tropea A, Biondi A, Cianci S. Ultra-minimally invasive surgery in gynecological patients: a review of the literature. Updates Surg. (2022) 74:843–55. doi: 10.1007/s13304-022-01248-y
5. Filmar GA, Fisher HW, Aranda E, Lotze PM. Laparoscopic uterosacral ligament suspension and sacral colpopexy: results and complications. Int Urogynecol J. (2014) 25:1645–53. doi: 10.1007/s00192-014-2407-9
6. Rardin CR, Erekson EA, Sung VW, Ward RM, Myers DL. Uterosacral colpopexy at the time of vaginal hysterectomy: comparison of laparoscopic and vaginal approaches. J Reprod Med. (2009) 54:273–80.19517690
7. Turner LC, Lavelle ES, Shepherd JP. Comparison of complications and prolapse recurrence between laparoscopic and vaginal uterosacral ligament suspension for the treatment of vaginal prolapse. Int Urogynecol J. (2016) 27:797–803. doi: 10.1007/s00192-015-2897-0
8. Vallabh-Patel V, Saiz C, Salamon C. Subjective and objective outcomes of robotic and vaginal high uterosacral ligament suspension. Female Pelvic Med Reconstr Surg. (2016) 22:420–4. doi: 10.1097/SPV.0000000000000306
9. Vacca L, Lucidi A, Panico G, Campagna G, Restaino S, Ercoli A, et al. Laparoscopic high uterosacral ligament suspension (modified shull technique): a case series and a step by step description of surgical procedure. Eur J Obstet Gynecol Reprod Biol. (2020) 253:83–9. doi: 10.1016/j.ejogrb.2020.07.031
10. Riemma G, Pasanisi F, Reino A, Solazzo MC, Ronsini C. Robotic single-site hysterectomy in gynecologic benign pathology: a systematic review of the literature. Medicina (Kaunas). (2023) 59(2):411. doi: 10.3390/medicina59020411
11. Gueli Alletti S, Restaino S, Finelli A, Ronsini C, Lucidi A, Scambia G, et al. Step by step total laparoscopic hysterectomy with uterine arteries ligation at the origin. J Minim Invasive Gynecol. (2020) 27(1):22–3. doi: 10.1016/j.jmig.2019.06.001
12. Hodgkinson CP. Stress urinary incontinence-1970. Am J Obstet Gyneco1. (1970) 108:1141–68. doi: 10.1016/0002-9378(70)90467-9
13. Stanton SL, Hilton I’, Norton C, Cardozo L. Clinical and urodynamic effects of anterior colporrhaphy and vaginal hysterectomy for prolapse with and without incontinence. Br J Obstet Gynaecol. (1982) 89(6):459–63. doi: 10.1111/j.1471-0528.1982.tb03637.x
14. Fianu S, Kjaeldgaard A, Larsson B. Preoperative screening for latent stress incontinence in women with cystocele. Neurourol Urodynam. (1985) 4:7.
15. Raz S, Klutke CG, Golomb J. Four corner bladder and urethral suspension for moderate cystocele. J Urol. (1989) 142(3):712–5. doi: 10.1016/s0022-5347(17)38863-8
17. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. (2009) 250(2):187–96. doi: 10.1097/SLA.0b013e3181b13ca2
18. Riss P, Dwyer PL. The POP-Q classification system: looking back and looking forward. Int Urogynecol J. (2014) 25(4):439–40. doi: 10.1007/s00192-013-2311-8
19. Henninger V, Reisenauer C, Brucker SY, Rall K. Laparoscopic nerve-preserving colposacropexy for surgical management of neovaginal prolapse. J Pediatr Adolesc Gynecol. (2015) 28(5):e153–5. doi: 10.1016/j.jpag.2014.12.005
20. Arcieri M, Morlacco A, Montebelli F, Mancini M, Soligo M, Restaino S, et al. Sacrocolpopexy after sub-total hysterectomy vs. sacral hysteropexy for advanced urogenital prolapse: a propensity-matched study. Int J Gynaecol Obstet. (2023) 163(3):847–53. doi: 10.1002/ijgo.14959
21. Restaino S, Ronsini C, Finelli A, Santarelli A, Scambia G, Fanfani F. Laparoscopic approach for shull repair of pelvic floor defects. J Minim Invasive Gynecol. (2018) 25(6):954. doi: 10.1016/j.jmig.2017.12.016
22. Campagna G, Pedone Anchora L, Panico G, Caramazza D, Arcieri M, Cervigni M, et al. Titanized polypropylene mesh in laparoscopic sacral colpopexy. Int Urogynecol J. (2020) 31(4):763–8. doi: 10.1007/s00192-019-04146-x
23. Houlihan S, Kim-Fine S, Birch C, Tang S, Brennand EA. Uterosacral vault suspension (USLS) at the time of hysterectomy: laparoscopic versus vaginal approach. Int Urogynecol J. (2019) 30:611–21. doi: 10.1007/s00192-018-3801-5
24. Barbier HM, Smith MZ, Eto CU, Welgoss JA, Von Pechmann W, Horbach N, et al. Ureteral compromise in laparoscopic versus vaginal uterosacral ligament suspension: a retrospective cohort. Female Pelvic Med Reconstr Surg. (2015) 21:363–8. doi: 10.1097/SPV.0000000000000202
25. Colombo M, Maggioni A, Zanetta G, Vignali M, Milani R. Prevention of postoperative urinary stress incontinence after surgery for genitourinary prolapse. Obstet Gynecol. (1996) 87(2):266–71. doi: 10.1016/0029-7844(95)00378-9
26. Ronsini C, Fumiento P, Iavarone I, Greco PF, Cobellis L, De Franciscis P. Liquid biopsy in endometriosis: a systematic review. Int J Mol Sci. (2023) 24(7):6116. doi: 10.3390/ijms24076116
27. Tius V, Arcieri M, Taliento C, Pellecchia G, Capobianco G, Simoncini T, et al. Laparoscopic sacrocolpopexy with concurrent hysterectomy or uterine preservation: a metanalysis and systematic review. Int J Gynaecol Obstet. (2025) 168(2):456–71. doi: 10.1002/ijgo.15891
28. Iavarone I, Greco PF, La Verde M, Morlando M, Torella M, de Franciscis P, et al. Correlations between gut microbial composition, pathophysiological and surgical aspects in endometriosis: a review of the literature. Medicina (Kaunas, Lithuania). (2023) 59(2):347. doi: 10.3390/medicina59020347
29. Tanagho EA. Effect of hysterectomy and periurethral surgery on urethrovesical function. In: Ostergard DR, editor. Gynecologic Urology and Urodynamics. 2nd ed. Baltimore: Williams & Wilkins (1985). p. 537–44.
30. Ronsini C, Vitale C, Romeo P, Sarpietro G, Torella M, Cianci S. Laparoscopic shull technique for uterine prolapse and risk of recurrences: a retrospective comparison with vaginal hysterectomy. Int Urogynecol J. (2025) 36(1):197–203. doi: 10.1007/s00192-024-05997-9
Keywords: pelvic organ prolapse, laparoscopic colposuspension, shull technique, natural vaginal tissue repair, cystopexy
Citation: Ronsini C, Andreoli G, Torella M, Romeo P, Sarpietro G and Cianci S (2025) Cystopexy raises the post-operative complication rate during laparoscopic hysterectomy for uterine prolapse. Front. Surg. 12:1488775. doi: 10.3389/fsurg.2025.1488775
Received: 30 August 2024; Accepted: 16 April 2025;
Published: 30 April 2025.
Edited by:
Menelaos Zafrakas, International Hellenic University, GreeceReviewed by:
Giuseppe Vizzielli, University of Udine, ItalyFederico Romano, University of Trieste, Italy
Copyright: © 2025 Ronsini, Andreoli, Torella, Romeo, Sarpietro and Cianci. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Carlo Ronsini, Y2FybG8ucm9uc2luaTkwQGdtYWlsLmNvbQ==
 Carlo Ronsini
Carlo Ronsini Giada Andreoli1
Giada Andreoli1 Giuseppe Sarpietro
Giuseppe Sarpietro