- 1Shanghai University of Traditional Chinese Medicine, Shanghai, China
- 2Department of Orthopedic Surgery, Guanghua Hospital Affiliated to Shanghai University of Traditional Chinese Medicine, Shanghai, China
Objective: To compare the early clinical outcomes of posterior cruciate ligament-retaining (CR) and posterior stabilized (PS) knee prostheses in total knee arthroplasty for patients with rheumatoid arthritis.
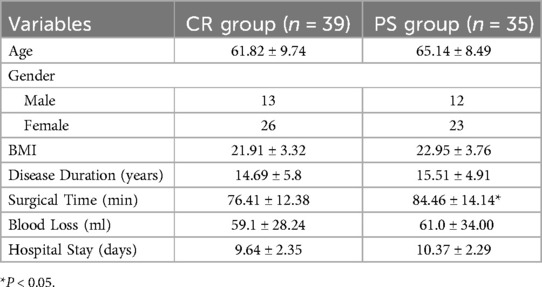
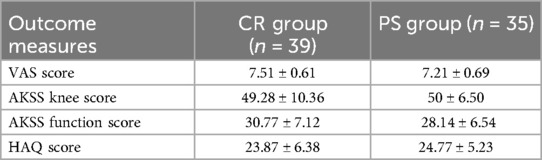
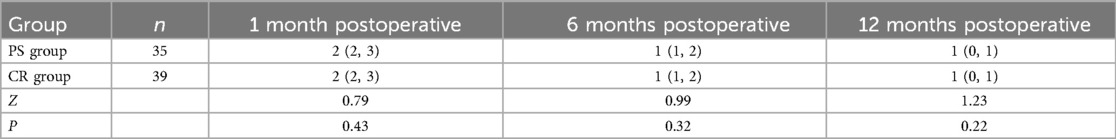
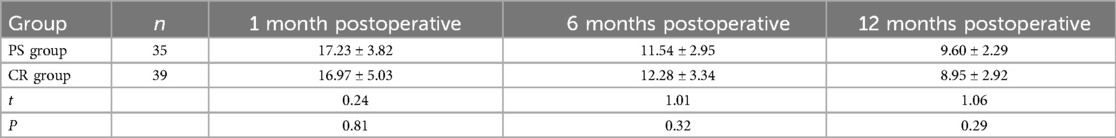
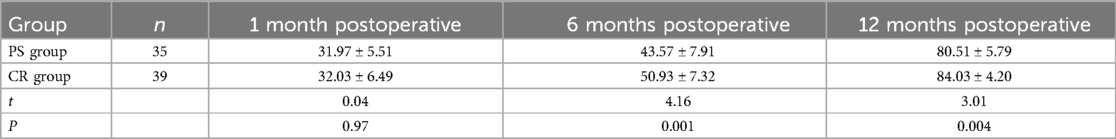
Methods: A retrospective analysis was conducted on 74 patients with rheumatoid arthritis (RA) who underwent unilateral total knee arthroplasty (TKA) from January 2021 to December 2022. Among these, 39 patients received CR prostheses (CR group), while 35 received PS prostheses (PS group). Data on operation time, intraoperative blood loss, hospital stay, preoperative and postoperative Visual Analogue Scale (VAS) scores, American Knee Society Score (AKSS), Functional Joint Score-12 (FJS-12) scores, Health Assessment Questionnaire scores (HAQ) and postoperative complications were recorded and compared between the two groups.
Results: All 74 patients successfully completed the surgery without complications. The average operation time for the CR group was shorter than that of the PS group, with no statistically significant differences in intraoperative blood loss or hospital stay. Both groups showed improved postoperative AKSS scores, VAS scores, and HAQ Scores compared to preoperative levels. Between-group comparisons showed no statistical differences in postoperative AKSS, VAS, HAQ scores. However, the CR group had significantly higher FJS-12 scores at 6 and 12 months postoperatively compared to the PS group.
Conclusion: Both CR and PS prostheses can achieve good clinical outcomes in TKA for RA patients. Compared to PS prostheses, CR prostheses may provide better knee proprioception postoperatively, as indicated by higher FJS-12 scores at 6 and 12 months postoperatively.
1 Introduction
Rheumatoid arthritis (RA) is a systemic autoimmune disease characterized by chronic, symmetrical inflammation of multiple joints and extra-articular manifestations, with an estimated global incidence of about 0.2% (1). Knee joints, being the largest and most complex synovial joints, are frequently affected in RA. Patients with RA affecting the knee often suffer from pain and functional limitations due to synovial hyperplasia, cartilage degradation, and joint deformities. Total knee arthroplasty (TKA), a highly successful procedure, remains the most effective surgical option for RA patients when conservative treatments are ineffective (2, 3). Patients with rheumatoid arthritis often present with severe knee joint destruction and deformities. Additionally, the risk of postoperative knee joint infection and prosthesis loosening is significantly higher than in osteoarthritis, necessitating individualized surgical strategies and precise perioperative management.
Currently, TKA predominantly uses posterior cruciate ligament-retaining (CR) and posterior stabilized (PS) prostheses. Studies have demonstrated that both CR and PS prostheses can significantly improve knee function, alleviate pain, and boost quality of life (4). Given the scarcity of research on prosthesis selection in RA patients, this retrospective study aims to compare the early clinical outcomes of CR and PS prostheses following TKA for RA patients.
2 Materials and methods
2.1 General information
A retrospective analysis was conducted on RA patients who underwent TKA from January 2021 to December 2022. Patients were divided into CR and PS groups based on the type of knee prosthesis used, which was determined according to the surgeon's clinical judgment, considering factors such as preoperative ligament integrity, bone quality, joint deformity, and intraoperative stability assessment. This study did not employ randomization or blinding due to its retrospective design.
2.2 Inclusion and exclusion criteria
2.2.1 Inclusion criteria
Diagnosed with RA according to the 2010 criteria of the American College of Rheumatology (ACR)/European League Against Rheumatism (EULAR) and categorized as Steinbrocker grade III or IV, with ineffective conservative treatment and clear surgical indications;
Patients undergoing unilateral knee surgery for the first time;
Varus or valgus deformity less than 15°;
No anesthesia contraindications, ASA classification of I or II, with signed informed consent.
2.2.2 Exclusion criteria
Patients with severe knee instability requiring constrained prostheses or extended stems;
Patients with severe complications requiring reoperation;
Incomplete clinical and imaging follow-up data.
2.3 Perioperative management of antirheumatic medications
For patients receiving conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) and glucocorticoids preoperatively, these medications should be continued perioperatively without dosage adjustments. For patients taking targeted synthetic disease-modifying antirheumatic drugs (tsDMARDs) before surgery, the medication should be discontinued at least three days prior to the procedure. For patients on biological disease-modifying antirheumatic drugs (bDMARDs), all biologics should be stopped preoperatively and resumed only after proper wound healing and confirmation of no infection at both surgical and non-surgical sites, typically around two weeks postoperatively (5).
2.4 Preoperative evaluation
All patients underwent a comprehensive physical examination and imaging assessments, including standing, lateral, and patellar views of the knee joint, as well as full-length lower limb x-rays and MRI scans. PCL injuries were classified into four grades based on MRI findings (6, 7):
Grade 0: No significant signal change in PCL; intact structure with no signs of congestion or edema around the ligament.
Grade 1: Increased signal on T1 and T2 sequences within the ligament, but intact fibers, with no changes in shape, thickness, or length, and damage area <1/2.
Grade 2: High signal changes on T1 and T2 sequences, with thickening, swelling, or hemorrhage, irregular or partially discontinuous fibers, damage area ≥1/2.
Grade 3: Significant signal enhancement on MRI, with ligament discontinuity, retraction, or wavy or clumped morphology, indicating complete rupture.
For patients with no PCL injury on physical examination and MRI grading of 0 or 1, CR prostheses were used if the PCL was intact during surgery; otherwise, PS prostheses were chosen. For those with PCL laxity and MRI grading of 2 or 3, PS prostheses were applied (8).
2.5 Follow-up and outcome measures
Follow-up was conducted preoperatively and at 1, 6, and 12 months postoperatively. Outcome measures included AKSS score, VAS score, HAQ score, FJS-12 score, and any postoperative complications. AKSS is a comprehensive knee evaluation scale proposed by the American Knee Society in 1989, which includes knee pain scores (Knee Score) and functional ability scores (Function Score). VAS is widely used for pain assessment, reflecting subjective pain severity. HAQ (Health Assessment Questionnaire), evaluates daily life status in RA patients, where higher scores indicate lower health status (9). FJS-12, introduced by Behrend et al. in 2012 (10), assesses joint awareness in patients with prosthetic knees; higher scores indicate better knee proprioception, making it widely used for evaluating post-TKA recovery and quality of life (11).
2.6 Statistical analysis
Data were analyzed using SPSS 26.0 (IBM, USA). The Shapiro–Wilk test assessed normality. Data following normal distribution were presented as mean ± standard deviation, with paired t-tests for within-group comparisons. Data with non-normal distribution were shown as median (interquartile range) and analyzed using the Mann–Whitney U test. P < 0.05 was considered statistically significant.
3 Results
3.1 General results
A total of 74 patients were included, with 39 in the CR group (26 females and 13 males) and 35 in the PS group (23 females and 12 males). Baseline characteristics were comparable between the two groups, with no statistically significant differences except for the operation time. Detailed information is shown in Table 1. All patients successfully completed the surgery without significant postoperative complications. Representative case images are shown in Figures 1, 2.
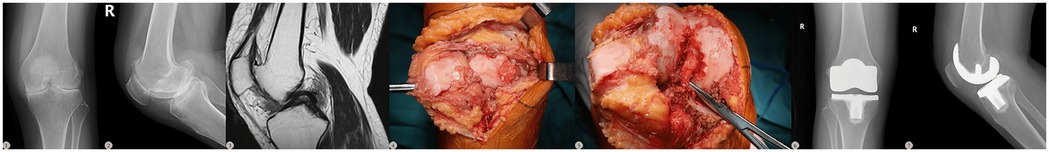
Figure 1. A 59-year-old female with a 13-year history of rheumatoid arthritis (RA). Preoperative imaging and intraoperative exploration revealed an intact and stable PCL, prompting the selection of a CR prosthesis for TKA. ①–②: the preoperative x-ray findings, ③: the preoperative MRI results, ④–⑤: the intraoperative exploration, ⑥–⑦: the postoperative follow-up x-ray results.
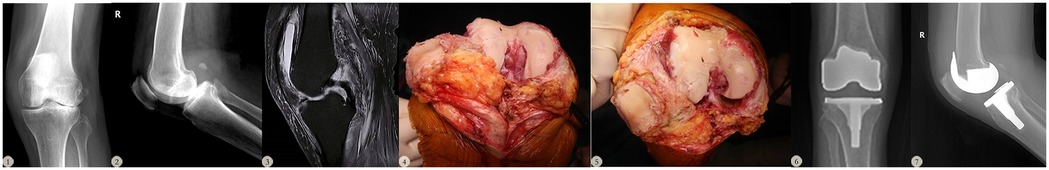
Figure 2. A 70-year-old female with a 31-year history of rheumatoid arthritis (RA). Preoperative imaging and intraoperative exploration revealed an incomplete and unstable PCL, prompting the selection of a PS prosthesis for TKA. ①–②: the preoperative x-ray findings, ③: the preoperative MRI results, ④–⑤: the intraoperative exploration, ⑥–⑦: the postoperative follow-up x-ray results.
3.2 Follow-up results
The study results showed that the preoperative VAS score for the PS group was 7.21 ± 0.69, and for the CR group, it was 7.51 ± 0.61. The preoperative AKSS Knee Score was 50 ± 6.50 in the PS group and 49.28 ± 10.36 in the CR group, while the preoperative AKSS Function Score was 28.14 ± 6.54 in the PS group and 30.77 ± 7.12 in the CR group. The preoperative HAQ Score was 24.77 ± 5.23 in the PS group and 23.87 ± 6.38 in the CR group, shown in Table 2.
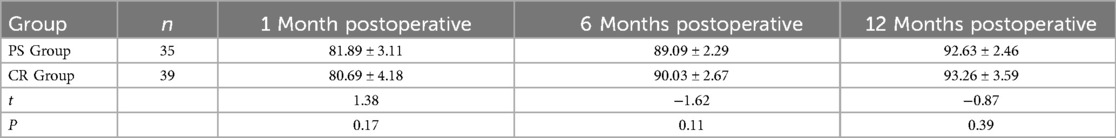
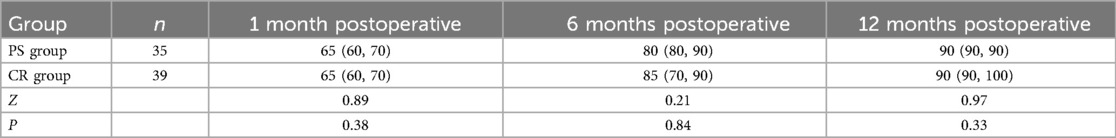
At 1 month postoperatively, the VAS score was 2.20 ± 0.63 in the PS group and 2.44 ± 1.05 in the CR group. At 6 months, the VAS score decreased to 1.36 ± 0.56 in the PS group and 1.23 ± 0.77 in the CR group. By 12 months, the VAS score further decreased to 0.61 ± 0.62 in the PS group and 0.46 ± 0.65 in the CR group. At 1 month postoperatively, the AKSS Knee Score was 81.89 ± 3.11 and the Function Score was 63.00 ± 6.99 in the PS group, while in the CR group, the Knee Score was 80.69 ± 4.18 and the Function Score was 64.87 ± 9.14. At 6 months, the AKSS Knee Score in the PS group increased to 89.09 ± 2.29, with a Function Score of 83.14 ± 7.68; in the CR group, the Knee Score was 90.03 ± 2.67 and the Function Score was 81.15 ± 11.09. By 12 months, the AKSS Knee Score reached 92.63 ± 2.46 in the PS group with a Function Score of 90.86 ± 5.07, while in the CR group, the Knee Score was 93.26 ± 3.59 and the Function Score was 92.05 ± 7.41.For the HAQ Score, the PS group recorded 17.23 ± 3.82 at 1 month, 11.54 ± 2.9 at 6 months, and 9.6 ± 2.29 at 12 months postoperatively. In the CR group, the HAQ Score was 16.97 ± 5.03 at 1 month, 12.28 ± 3.34 at 6 months, and 8.95 ± 2.92 at 12 months. For the FJS-12 Score, the PS group had 31.97 ± 5.51 at 1 month, 43.57 ± 7.91 at 6 months, and 80.51 ± 5.79 at 12 months; the CR group had 32.03 ± 6.49 at 1 month, 50.93 ± 7.32 at 6 months, and 84.03 ± 4.20 at 12 months, shown in Figure 3.
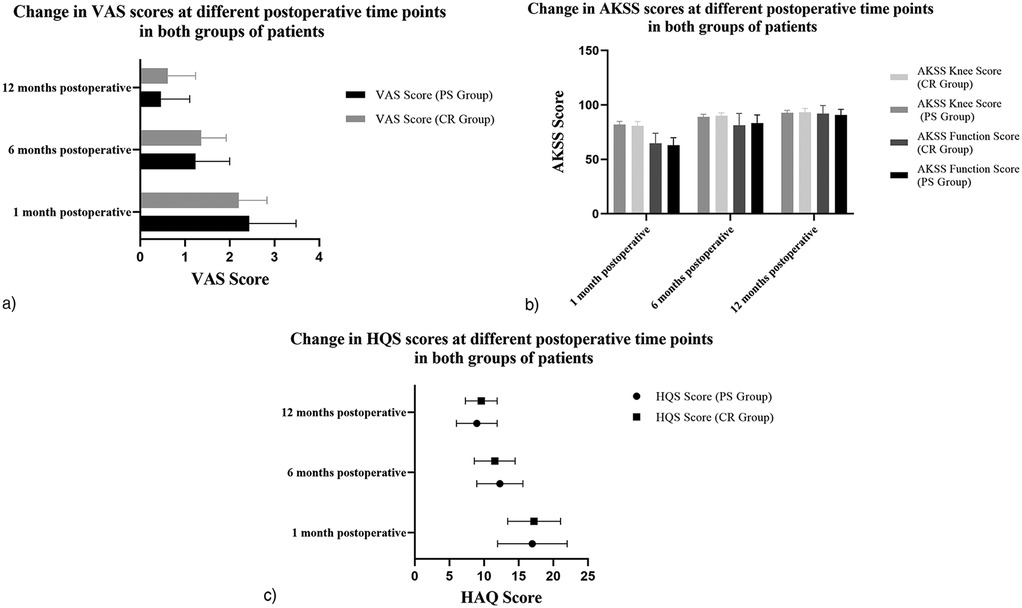
Figure 3. Changes in outcome measures at different time points after surgery in Two patient groups (a: VAS score, b: AKSS score, c: HAQ score).
Postoperative VAS and HAQ scores in both groups were significantly lower than preoperative scores, while AKSS scores were higher, with statistically significant differences (P < 0.05). Between-group comparisons showed no statistically significant differences in VAS, AKSS, or HAQ scores at any postoperative time points, shown in Tables 3–6. However, at 12 months postoperatively, the CR group had significantly higher FJS-12 scores compared to the PS group, shown in Table 7.
4 Discussion
Total knee arthroplasty (TKA) is currently the primary surgical treatment for advanced rheumatoid arthritis (RA) patients, as it can effectively relieve knee pain, improve mobility, and significantly enhance quality of life (12). However, there is still no consensus on whether to preserve the posterior cruciate ligament (PCL) in RA patients undergoing TKA. Some researchers argue that due to the inflammatory nature of RA, the functionality of the PCL may not be reliable as the disease progresses, and using a posterior cruciate ligament-retaining (CR) prosthesis could lead to postoperative posterior instability and increase the risk of revision surgery (13). Other studies, however, have demonstrated that the long-term survival rates of CR prostheses in RA patients are comparable to those of posterior-stabilized (PS) prostheses, with a low incidence of posterior instability (14). Since RA is characterized by bone destruction, RA patients undergoing TKA tend to be younger on average than osteoarthritis patients (15). For relatively younger RA patients, preserving more native soft tissue and bone mass may better maintain joint function postoperatively (16). Designed for bone preservation and low constraint, CR prostheses are considered more suitable than PS prostheses for RA patients with osteoporosis and higher activity demands (17).
Using a CR prosthesis in TKA can simplify the intercondylar bone resection, reduce operation time and intraoperative blood loss, and require less release of posterior soft tissue (16, 17). Long-term follow-up studies by Ricardo et al. (18) found no significant differences in pain scores between CR and PS groups, with similar rates of residual pain and swelling at the final follow-up. Another randomized study by Clark et al. (19) of 143 patients over more than two years showed no significant differences in functional scores or range of motion between the two prostheses. Similarly, long-term studies by Lauren et al. (20) and Ricardo et al. (18) over 10 years revealed similar AKSS and functional scores in both groups. In a large cohort study of 11,606 knee replacements, Rand et al. (17) concluded that posterior cruciate ligament-retaining prostheses had a long lifespan in elderly female patients with inflammatory arthritis. Our study corroborates these findings, with one-year follow-up showing significant improvements in AKSS, VAS, and HAQ score, in both CR and PS groups compared to preoperative levels, with no significant differences in scores between groups. No complications such as posterior instability, prosthesis loosening, infection, or fractures occurred during follow-up.
Compared to PS prostheses, CR prostheses retain the PCL, which can support femoral rollback mechanics, potentially providing a greater range of flexion postoperatively (21). Additionally, retaining the PCL can enhance joint mobility postoperatively (22). Hina et al. (23) found that in patients with preoperative varus deformity, 60% of those who received CR prostheses retained similar kinematics pre- and postoperatively, whereas only 25% of those with PS prostheses did, demonstrating that the PCL plays a crucial role in coronal knee stability postoperatively, aligning more closely with normal knee kinematics. An anatomical study by Kennedy et al. (24) on cadaver knee specimens also showed that the PCL's anterolateral and posteromedial bundles limit posterior tibial translation during knee flexion. Comparative studies on PS and CR prosthesis designs (25–27) indicate similar outcomes in mobility, aseptic loosening, polyethylene wear, and stability; however, Conditt et al. (28) reported that the cam mechanism in PS prostheses cannot fully replicate the function of the PCL, particularly in high-demand activities such as deep flexion, squatting, and kneeling. Thus, CR prostheses with PCL retention may offer better mobility and satisfaction in certain movements postoperatively compared to PS prostheses without PCL retention (8). FJS-12 scores showed no significant difference between groups at 1 month postoperatively, but the CR group exhibited better joint awareness than the PS group at 6 and 12 months. This may be due to some damage to the peripheral proprioceptive receptors during intraoperative release of the PCL and that occurs in the early postoperative period when the tissues are in a period of repair. As soft tissue and proprioceptive receptors heal by 6 months, the CR prosthesis, with its superior biological compatibility, provides better subjective movement sensation, enhancing joint awareness (29).
Additionally, Liu et al. (26) suggested that RA patients may have moderate to severe flexion contracture or PCL dysfunction, potentially requiring conversion from a CR to a PS prosthesis during surgery. Our study excluded patients with severe preoperative knee varus/valgus deformity or flexion contracture >10°, and we carefully assessed PCL integrity through repeated physical exams and MRI evaluation, along with intraoperative testing and PCL preservation (30). As a result, none of the CR group patients required conversion to a PS prosthesis due to PCL rupture or dysfunction intraoperatively.Our findings indicate that both CR and PS prostheses provide good postoperative outcomes for RA patients undergoing TKA. However, compared to PS prostheses, CR prostheses may offer better knee proprioception in the early postoperative period. We recommend careful evaluation of PCL integrity before and during surgery; RA patients with PCL damage should consider PS prostheses, while CR prostheses are more suitable for patients with an intact PCL and high functional demands for joint mobility postoperatively.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Shanghai Guanghua Hospital of Integrated Traditional Chinese and Western Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HD: Conceptualization, Writing – original draft. DH: Data curation, Writing – original draft. NM: Data curation, Writing – original draft. CG: Formal analysis, Writing – original draft. JY: Formal analysis, Writing – original draft. GO: Validation, Writing – original draft.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was supported by the Changning District Health and Wellness Committee Scientific Research Project (20214Y021) and Changning District Science and Technology Commission Scientific Research Project (CNKW2022Y22).
Acknowledgments
The authors thank all their colleagues for their kind help and all patients for their cooperation with our work.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
TKA, total knee arthroplasty; VAS, visual analog scale; AKSS, American Knee Society Score; RA, Rheumatoid arthritis; CR, posterior cruciate ligament-retaining; PS, posterior stabilized; HAQ, Health Assessment Questionnaire; FJS, forgotten joint score; EULAR, European League Against Rheumatism; ACR, American College of Rheumatology; ASA, American society of Aneshesiologists; PCL, posterior cruciate ligament.
References
1. Black RJ, Cross M, Haile LM, Culbreth GT, Steinmetz JD, Hagins H, et al. Global, regional, and national burden of rheumatoid arthritis, 1990–2020, and projections to 2050: a systematic analysis of the global burden of disease study 2021. Lancet Rheumatol. (2023) 5(10):e594–610. doi: 10.1016/S2665-9913(23)00211-4
2. American Joint Replacment Registry (AJRR). The tenth annual report of the AJRR on hip and knee arthroplasty. Am Acad Orthopaedic Surgeeons. (2023):1–125.
3. Cordtz R, Odgaard A, Kristensen LE, Overgaard S, Dreyer L. Risk of medical complications following total hip or knee arthroplasty in patients with rheumatoid arthritis: a register-based cohort study from Denmark. Semin Arthritis Rheum. (2020) 50:30–5. doi: 10.1016/j.semarthrit.2019.06.007
4. Yamashita F, Funakoshi N, Mori D, Kizaki K. Long-term outcomes and duration of outdoor ambulation following primary total knee arthroplasty in patients with rheumatoid arthritis. J Orthop Sci. (2022) 27:414–9. doi: 10.1016/j.jos.2021.01.014
5. Goodman SM, Springer BD, Chen AF, Davis M, Fernandez DR, Figgie M, et al. 2022 American college of rheumatology/American association of hip and knee surgeons guideline for the perioperative management of antirheumatic medication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty. J Arthroplasty. (2022) 37(9):1676–83. doi: 10.1016/j.arth.2022.05.043
6. Predeep Kumar VM, Karuppal R. Comparison between clinical, magnetic resonance imaging, and arthroscopic findings in meniscal and cruciate ligament injuries: a cross-sectional study. (2022) 19(3):137–41.
7. Brown JS, Mogianos K, Roemer FW, Isacsson A, Kumm J, Frobell R, et al. Clinical, patient-reported, radiographic and magnetic resonance imaging findings 11 years after acute posterior cruciate ligament injury treated non-surgically. BMC Musculoskelet Disord. (2023) 24(1):365. doi: 10.1186/s12891-023-06480-0
8. Nolan P, O’Sullivan M, Gorman Á, Eustace S, Mohammad A, Sheehan E. Evaluating posterior cruciate ligament integrity in inflammatory arthritis patients prescribed biologic agents: a radiological case-control study. Cureus. (2021) 13(2):e13160. doi: 10.7759/cureus.13160
9. Taylor WJ, Parekh K. Rasch analysis suggests that health assessment questionnaire II is a generic measure of physical functioning for rheumatic diseases: a cross-sectional study. (2018) 16(1).
10. Behrend H, Zdravkovic V, Giesinger JM, Giesinger K. Joint awareness after ACL reconstruction: patient-reported outcomes measured with the forgotten joint score-12. Knee Surg Sports Traumatol Arthrosc. (2017) 25(5):1454–60. doi: 10.1007/s00167-016-4357-x
11. Londhe SB, Shah R, Shah MY, Doshi AP, Londhe SS, Subhedar K, et al. Discrepant histological diagnoses affects the near term FJS-12 and could be one of the causes of unhappy TKR patient. Orthop J Sports Med. (2020) 8(9 suppl7):2325967120S00531. doi: 10.1177/2325967120S00531
12. Kobayashi S, Niki Y, Harato K, Nagura T, Nakamura M, Matsumoto M. Rheumatoid arthritis patients achieve better satisfaction but lower functional activities as compared to osteoarthritis patients after total knee arthroplasty. J Arthroplasty. (2018) 34(3):478–482.e1. doi: 10.1016/j.arth.2018.11.003
13. Waslewski G-L, Marson B-M, Benjamin J-B. Early, incapacitating instability of posterior cruciate ligament-retaining total knee arthroplasty. (1998):763–7.9802661
14. Meding JB, Keating EM, Ritter MA, Faris PM, Berend ME. Long-term followup of posterior-cruciate-retaining TKR in patients with rheumatoid arthritis. Clin Orthop Relat Res. (2004) 428:146–52. doi: 10.1097/01.blo.0000147134.52561.64
15. Lee JK, Kee YM, Chung HK, Choi CH. Long-term results of cruciate-retaining total knee replacement in patients with rheumatoid arthritis: a minimum 15-year review. Cma Joule Inc. (2015) 58(3):193–7. doi: 10.1503/cjs.012014
16. Jinseok K, Wooseong J, Sung-Won L. Effect of rheumatoid arthritis on primary total knee arthroplasty and revision arthroplasty. S550.
17. Rand JA, Trousdale RT, Ilstrup DM, Harmsen WS. Factors affecting the durability of primary total knee prostheses. J Bone Joint Surg Am. (2003) 85(2):259–65. doi: 10.2106/00004623-200302000-00012
18. Serna-Berna R, Lizaur-Utrilla A, Vizcaya-Moreno MF, Miralles Muñoz FA, Gonzalez-Navarro B, Lopez-Prats FA. Cruciate-retaining vs posterior-stabilized primary total arthroplasty. Clinical outcome comparison with a Minimum follow-up of 10 years. J Arthroplasty. (2018) 33(8):2491–5. doi: 10.1016/j.arth.2018.02.094
19. Clark CR, Rorabeck CH, MacDonald S, MacDonald D, Swafford J, Cleland D. Posterior-stabilized and cruciateretaining total knee replacement. Clin Orthop Relat Res. (2001) 392:208–12. doi: 10.1097/00003086-200111000-00025
20. Beaupre LA, Sharifi B, Johnston DWC. A randomized clinical trial comparing posterior cruciate-stabilizing vs posterior cruciate-retaining prostheses in primary total knee arthroplasty: 10-year follow-up. (2017) 32(3):818–23.27693054
21. Song SJ, Park CH, Bae DK. What to know for selecting cruciate-retaining or posterior-stabilized total knee arthroplasty. (2019) 11(2):142.31156764
22. Sierra RJ, Berry DJ. Surgical technique differences between posterior-substituting and cruciate-retaining total knee arthroplasty. (2008) 23(7):20–3.18701240
23. Hino K, Oonishi Y, Kutsuna T, Watamori K, Iseki Y, Kiyomatsu H, et al. Preoperative varus-valgus kinematic pattern throughout flexion persists more strongly after cruciate-retaining than after posterior-stabilized total knee arthroplasty. Knee. (2016) 23(4):637–41. doi: 10.1016/j.knee.2015.11.015
24. Kennedy NI, Wijdicks CA, Goldsmith MT, Michalski MP, Devitt BM, Engebretsen L, et al. Kinematic analysis of the posterior cruciate ligament, part 1: the individual and collective function of the anterolateral and posteromedial bundles. Am J Sports Med. (2013) 41(12):2828–38. doi: 10.1177/0363546513504287
25. Guven MF, Karaismailoglu B, Kara E, Ahmet SH, Guler C, Tok O, et al. Does posterior cruciate ligament sacrifice influence dynamic balance after total knee arthroplasty? Comparison of cruciate-retaining and cruciate-substituting designs in bilaterally operated patients. J Orthopaedic Surg. (2021) 29(3):23094990211061610. doi: 10.1177/23094990211061610
26. Wang Y, Zhang L, Lin J, Xing D, Liu Q, Zhou D. Preoperative factors predicting the preservation of the posterior cruciate ligament in total knee arthroplasty. Orthop Surg. (2022) 14(9):2203–9. doi: 10.1111/os.13439
27. Amirjanova VN, Makarov MA, Karateev AE, Khramov AE, Maglevanyi SV, Rozov AV, et al. Updated American college of rheumatology/American association of hip and knee surgeons guideline for the perioperative management of antirheumatic medication in patients with rheumatic diseases undergoing elective total hip or total knee arthroplasty 2022. Rheumatol Sci Pract. (2023) 61(3):260–7. doi: 10.47360/1995-4484-2023-260-267
28. Conditt MA, Noble PC, Bertolusso R, Woody J, Parsley BS. The PCL significantly affects the functional outcome of total knee arthroplasty. J Arthroplasty. (2004) 19(7 Suppl 2):107–12. doi: 10.1016/j.arth.2004.06.006
29. Bieganowski T, Fiedler B, Singh V, Karlin E, Anil U, Rozell JC, et al. Does retention of the posterior cruciate ligament lead to a more “forgotten joint” following total knee arthroplasty? Surg Technol Int. (2022) 40:329–34. doi: 10.52198/22.STI.40.OS1538
Keywords: rheumatoid arthritis, total knee arthroplasty, CR prosthesis, PS prosthesis, retrospective study
Citation: Ding H, Han D, Ma N, Gao C, Yao J and Ouyang G (2025) Comparison of early clinical outcomes between CR and PS prostheses in total knee arthroplasty for rheumatoid arthritis patients - a retrospective cross-sectional study. Front. Surg. 12:1522588. doi: 10.3389/fsurg.2025.1522588
Received: 4 November 2024; Accepted: 3 April 2025;
Published: 6 May 2025.
Edited by:
Bernardo Innocenti, Université libre de Bruxelles, BelgiumReviewed by:
Filippo Maria Anghilieri, San Leopoldo Mandic Hospital, ItalyAshok Kumar Banskota, Hospital and Rehabilitation Centre for Disabled Children, Nepal
Copyright: © 2025 Ding, Han, Ma, Gao, Yao and Ouyang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guilin Ouyang, b3lnbG1kQGhvdG1haWwuY29t
†These authors have contributed equally to this work
 Haoyuan Ding
Haoyuan Ding Dapeng Han2,†
Dapeng Han2,† Nanshan Ma
Nanshan Ma