- 1Leeds Institute of Medical Research, St James’s University Hospital, University of Leeds, Leeds, United Kingdom
- 2Medical School, Dalhousie University, Halifax, NS, Canada
- 3Thomas Jefferson University, Philadelphia, PA, United States
- 4Faculty of Medicine, Imperial College London, London, United Kingdom
- 5Sheps Health Services, Research Center, University of North Carolina, Chapel Hill, NC, United States
- 6Department of General Surgery, Bradford Teaching Hospitals NHS Foundation Trust, Bradford, United Kingdom
- 7Department of Psychology, Université de Bourgogne, Dijon, France
- 8School of Psychology, University of Leeds, Leeds, United Kingdom
- 9St Mark’s Hospital, London North West University Healthcare NHS Trust, London, United Kingdom
- 10The Royal London Hospital, Barts Health NHS Trust, London, United Kingdom
- 11Department of Health Research, University of York, York, United Kingdom
Background: Mental rehearsal (MR), the deliberate practice of skills specific to a procedure, has been successfully used in sports and music training for decades, but has not been adopted in surgery. This narrative review explores MR's role in surgical training and clinical practice, evaluating its effectiveness in motor skill acquisition, technical and non-technical skill development, and real world clinical implementation. Our aim was to assess MR's impact on both surgical education and clinical performance, while identifying the barriers to its routine adoption in surgical training.
Methods: We searched for relevant studies on the topic and impacts of MR in surgery using the Medline database up to December 2024. A range of studies were included covering mental rehearsal, surgical education, surgical training, and surgical outcomes. The primary outcomes were to provide insights into the mechanisms and implementation of MR in surgery and to assess the potential impact of MR on surgical outcomes.
Results: The narrative review provides scientific insights into the mechanisms of MR in surgery and describes in detail the implementation methodology. The majority of evidence demonstrates that MR is beneficial when used as an adjunct approach to other forms of training. Moreover, there is evidence to support MR as a low-cost and valuable learning technique. Many questions remain regarding training schedules including the optimal duration and nature of the MR sessions, accommodating the surgeon's prior experience, optimal number of repetitions, and addressing the abilities of the participants to perform mental imagery. Most studies have heterogenous methods, diffuse aims and poor descriptions of the specific intervention components. Several studies applied MR in demanding real-life surgical environments and demonstrated feasibility in surgery.
Conclusions: The preliminary findings suggest that MR may improve the performance of operators and operating teams as an efficient adjuvant to traditional surgical skills training methods. More work is needed to better understand how MR interventions can best be implemented to improve training, practice, and outcomes in routine surgical practice.
Introduction
Mental rehearsal (MR) is a cognitive training technique that encompasses both mental and motor imagery (1–3). Mental imagery broadly refers to the simulation of experiences, while motor imagery refers to imagined actions. Neuroscientific evidence suggests that imagined movements engage the same neural networks as executed actions (4), with kinaesthetic imagery adhering to the constraints of human sensorimotor control (5–8). This indicates that MR may produce a similar learning effect to “hands-on” practice through neurocognitive mechanisms. MR offers the opportunity to practice specific procedures or related skills before performing complex tasks on patients, potentially impacting patient outcomes (9).
The two main modalities used in MR are visual and kinaesthetic imagery. Visual imagery involves the mental visualisation of action without explicit physical movement (1–3), whereas the kinaesthetic imagery involves the mental reproduction of movement and actions. Mental images can be formulated in different ways; from direct perceptual information, stored long-term memory, or a combination of both, and can be either generic or specific depending on the context, participants and goals (10). MR may be used by novices and expert operators to advance procedure learning and expertise (11).
Despite growing interest in MR within surgical training, there remain several gaps in the literature. There is no consensus on how best to implement MR in a structured training program, the optimal duration and frequency of sessions, or its long-term impact on surgical performance. Moreover, there is a lack of practical guidance for educators on how to practically integrate MR into surgical curricula. This comprehensive narrative review aims to (i) provide an overview of MR as a motor skill learning method, (ii) evaluate its effectiveness in improving task performance, as measured by assessments of the technical and non-technical skills of the operators and operating teams, and (iii) offer practical recommendations for incorporating MR in surgical training programmes.
Methods
This study is a narrative review aimed at synthesising existing literature on mental rehearsal (MR) in surgical education. The review included five key phases: Identifying the research question, identifying relevant studies, study selection, collating data, and synthesising results.
A structured search was conducted on Medline to identify relevant articles published up to December 2024. The search terms included “mental rehearsal,” “mental imagery,” “surgical training,” and “simulation.” Additional studies were identified through manual searches of reference lists in key articles.
We included studies if they examined the role of MR in surgical training, assessed its impact on technical and non-technical skill acquisition, or provided insights into its implementation. Opinion pieces, conference abstracts, and studies focusing on non-surgical applications of MR were excluded. Given the narrative review design, no formal quality assessment or meta-analysis was conducted. Instead, findings were synthesised thematically to provide an overview of MR's effectiveness and practical applications in surgical education.
Mental rehearsal and motor skill acquisition
Cognitive and motor processes share common features, including an improved performance with practice and a decline with a lack of it. In the initial stages of both imagery practice and motor skills learning, the objectives are identical: to build a mental representation of the task. Feedback plays an essential role in both, leading to automation with repeated practice (4).
The application of MR in surgical training is supported by established theories of motor learning and skill acquisition. Schmidt's schema (12), a classic motor learning theory, emphasises the importance of mentally storing how a task looks, feels, and sounds. This mental storage modifies the feedback processes that are fundamental components of visual and kinaesthetic MR. This suggests that MR may strengthen motor schemas by reinforcing mental representations of key procedural steps. Identifying the learner's mental models—understanding how novices perceive a procedure as compared to experts—has been a common method for preparing MR scripts to train novices (13, 14).
Additionally, Fitts and Posner's Three-Stage Model of Skill Acquisition (15) describes learning in three phases: the cognitive stage (understanding the task), the associative stage (refining movement), and the autonomous stage (performing with minimal cognitive effort). MR aligns particularly well with the cognitive and associative stages, where mental imagery can facilitate the transition from explicit learning to procedural execution.
Experimental evidence indicates that the time required to perform a task mentally is proportional to the time needed for physical performance (16). Visual perception and memory also play a significant role in the quality of mental imagery, affecting the vividness and accuracy of the rehearsed actions (17–20). Motor imagery is also subject to similar computational models as overt motor actions, including alterations in performance caused by sensory feedback and other factors regulating movement response (5, 21–23).
Common cortical and subcortical networks observed by neuroimaging studies demonstrate that MR engages motor-related networks, including the supplementary motor area (24, 25), parietal cortex (26–29), premotor cortex (25, 26, 30), primary motor area (27, 31, 32) and cerebellum (33). Moreover, electroencephalography (EEG) studies demonstrate a substantial overlap in the electrical activity between real and imagined actions (34–36). A source analysis from EEG studies also point to the primary motor structures being implicated in both mental and physical task performance (36). Similarly, potential current signals appear both quantitatively and qualitatively equivalent for imaginary and actual task performance (34, 37).
Beyond motor learning, MR may also optimise cognitive load management and decision-making during surgical tasks. Cognitive Load Theory (38) suggests that MR can reduce extraneous cognitive demands, allowing trainees to allocate more working memory resources to task execution. Furthermore, the Stress Inoculation Model (39) posits that MR under simulated stress conditions may enhance psychological resilience and decision-making under pressure, a crucial factor in high-risk surgical environments (40). These cognitive theories provide additional support for MR's integration into surgical training beyond its effects on motor performance alone. Despite these insights, there is currently no standardised theoretical model guiding MR protocol development or implementation in surgery, leading to variability or lack of its routine use in training approaches.
Preparation, content, and duration of mental rehearsal sessions
The most popular approaches for designing an MR session for surgery are (i) creating a consensus between experts on how the task should be performed (13, 14, 41), (ii) preparing physician/educator-led cognitive task analysis sessions which include a breakdown of the procedure steps in order to facilitate the visualisation process (42–46), or (iii) a combination of the two (47). A consensus is achieved through a series of semi-structured interviews and consequent thematic analysis of their transcripts in search of visual and kinaesthetic cues. This process yields a script that requires subsequent validation (13, 14, 41).
The structure and duration of MR sessions in surgery varies greatly in most studies. Mulla et al. (45) provided medical students with a 25-min one-on-one mental training session with clinical instructors, which included step-by-step descriptions of the motor skills required, relaxation techniques, as well as intrinsic and extrinsic visualisation of the chosen assessment tasks. The students were asked to undergo 15-min daily self-driven practice sessions. In contrast, three RCTs provided a single 30-min session to participants which consisted of psychologist-led relaxation techniques, step-by-step breakdowns of procedures embedded with sensory cues and surgeon-supervised mental imagery rehearsal sessions. Of these, two showed a favourable effect of MR on surgical skills (43, 44) and one study showed no difference (42). Two additional RCTs employed several 30-min MR sessions immediately prior to the surgical procedure. These were based on a MR script that was preceded by relaxation techniques. Both studies showed superior performance in the MR-trained group (13, 14).
Currently, the duration of MR prior to operating is not standardised. An RCT by Cragg et al. (48) spanning four months initially provided a 3-h training session on MR, followed by a practice schedule coupled with a multi-sensory self-evaluation form. At the end of the 2nd month, a 30-min telephone discussion was conducted with further MR advice from a consultant. After the 3rd month participants were instructed to develop a “script” of procedural steps, and after four months a summative 20-min independent session was undertaken before their final assessment. Kaulfuss et al. (49) performed an RCT with medical students who completed a formal training program, received a demonstration by a laparoscopic expert, began 30 min of hands-on training, followed by 60 min of formal theoretical training, and underwent a supervised mental training session prior to two weeks of independent MR. Participants who engaged in MR performed better and faster, and remarkably the skills improvement was noted to last several months. Immenroth et al. (50) offered the longest duration of one-on-one mental training sessions, lasting 90 min. In contrast, some studies planned sessions lasting merely 5 min (51) and 3 min (47) with participants asked to repeat the process several times prior to their assessments.
A systematic review of RCTs by Goble et al. (52) found that in studies where MR groups showed improved outcomes, the median duration of each session was 30 min and the training lasted for a median of 24 days. Notably, it is unclear whether there is a linear relationship between MR duration and surgical performance. Indeed, prolonged motor imagery sessions may have adverse effects on motor performance, due to mental fatigue (53). Alongside delineating an optimal time, the pragmatics of conducting MR in a busy hospital setting with staffing shortages and productivity pressures also need to be considered.
In anticipation of the MR sessions, non-experts must become familiar with the tasks taught (13, 14, 43, 45, 51). Various training techniques have been proposed for this purpose. Eldred-Evans et al. (44) followed Peyton's four-step teaching approach while others trained novices to proficiency before applying the MR intervention (14) or employed expert teaching (42, 43). Once the non-expert surgeon gains a basic understanding of the task, they practise several times during the supervised session(s). At the end of this process, the surgeon may be assessed to ensure their understanding of the task. Equally important, they receive guidance on how to mentally practise, before engaging in a series of supervised or self-driven MR sessions (13, 14, 43–45, 51).
An evaluation may be completed to establish a surgeon's baseline ability to practise mentally, as the capability to mentally reconstruct images varies widely across individuals. A systematic review by Suica et al. (54) identified imagery ability evaluation methods and evaluated their psychometric properties. The best-rated assessments were the Movement Imagery Questionnaire (MIQ) and its iterations (MIQ-R and MIQ-3), and the Vividness of Movement Imagery Questionnaire-2 (VMIQ-2) for evaluation of motor imagery ability. Regarding mental imagery evaluation, only the Sport Imagery Ability Questionnaire (SIAQ) and VVIQ showed sufficient psychometric properties.
Outcome measures to assess mental rehearsal impact
Validated outcome measures are needed to provide meaningful feedback to the learner, in the form of a composite score, an interpretation of results or a risk categorisation of the surgical task. No consensus exists about the most effective outcome measures in the study of MR (55). The most frequently used measure in studies is the overall performance metric. Multiple RCTs have utilised this technique with significant heterogeneity of assessed factors, including a composite of any number of the following: time taken to complete a task, accuracy (44, 45, 47) and rating checklists (13, 14, 41–43, 50, 51). The Objective Structured Assessment of Technical Skill (OSATS) is a validated tool for the assessment of surgical skills (56) and has been implemented in multiple studies assessing MR (13, 50).
An indirect way to assess the MR sessions is through questionnaires (13, 14, 41) addressed to supervising experts or the participating trainees. This method assesses the performance characteristics, and mental characteristics including stress, teamwork, and confidence. Arora et al. (13) applied the validated State-Trait Anxiety-Inventory (STAI) to assess the impact of MR training on the stress levels of novice surgeons completing virtual laparoscopic cholecystectomies. The outcome measures in the literature are frequently limited to short-term performance metrics, with little regard paid to the confounding and potential biasing factors as well as the long-term benefits (55). A lack of consistent outcome measures has limited the use of meta-analysis in assessing the effectiveness of MR in surgery, and larger trials with consistent and validated outcome measures are required (57).
Mental rehearsal for surgical skill acquisition
MR was demonstrated to be effective in teaching both basic technical skills and full procedural tasks across various surgical disciplines. Table 1 provides an overview summary of key studies on MR in surgical training. Studies assessing fundamental surgical skills have demonstrated MR's effectiveness in improving tasks such as suturing and precision cutting. For example, previous studies have used MR to train surgeons in cutting a 44 mm diameter circle from a rubber glove using a box trainer or a virtual reality (VR) simulator (44, 45), opening and closing a midline incision of an anaesthetised rabbit (42, 43), handsewn intestinal anastomosis on bovine intestine (58), or suturing during a laparoscopic Nissen fundoplication on a VR simulator (47). Similarly, MR has been applied to full procedural tasks, including a simulated laparoscopic cholecystectomy on a VR simulator (13, 14), a porcine liver and gallbladder placed in a box trainer (50), laparoscopic jejunojejunostomy (41), and a cricothyroidectomy on a mannequin (51). The diversity in difficulty and subspecialty of the chosen tasks demonstrates that MR can be an effective tool for all training grades and across all surgical specialties.
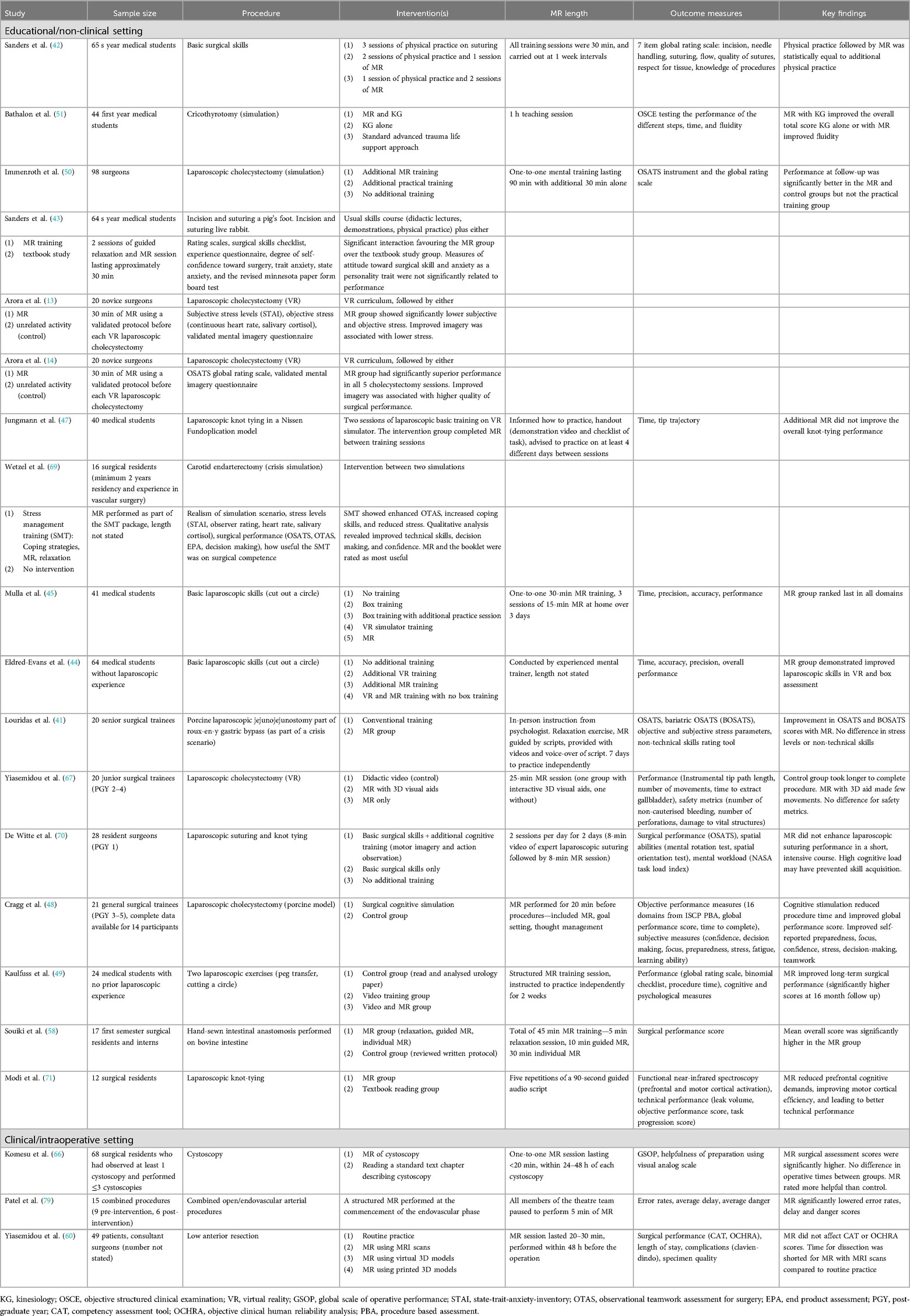
Table 1. Summary of key studies on mental rehearsal (MR) in surgical training, stratified by study setting.
MR can be applied across all levels of competency, from novice learners developing basic technical skills to experienced surgeons refining advanced procedures. For example, junior trainees can rehearse core surgical steps, such as achieving access to the abdominal cavity, while more experienced trainees can practise procedural sequences they have seen but not yet performed (59). Experienced surgeons can utilise MR to rehearse variations that could potentially occur during technically demanding procedures (4, 60). Skervin et al. (61) demonstrated that 91.5% of consultants and surgical trainees incorporate MR informally prior to operating, suggesting that this approach is likely to be widely accepted by trainees and consultants. Interestingly, a 2017 systematic review found that ten out of fourteen trials demonstrated objective improvement in surgical skills, with more obvious benefits to mature surgeons with greater levels of expertise (62). This is in keeping with a review by Anton et al. (63) who highlighted that MR is most useful when applied to surgeons of different experience levels as a supplemental training tool to refine and improve their surgical skills.
Multiple systematic reviews support the efficacy of MR in surgical training. Rao et al. (57) conducted a systematic review of nine randomised controlled trials (RCTs) involving 474 participants, with five trials reporting significant improvement in skill acquisition. These studies examined both basic tasks, such as precision cutting, and full procedures, including laparoscopic cholecystectomy. Assessment tools varied, incorporating objective measures (e.g., checklists, time to complete task, number of instrumental tip movements) alongside non-objective measures. Interestingly, the studies that found neutral outcomes tended to rely on verbal instruction or brief video demonstrations, that featured short MR sessions (≤30 min), and required unsupervised self-rehearsal periods, suggesting that structured, repeated MR sessions may yield better outcomes.
Gabbott et al. (64) conducted a systematic review of eight studies with 268 participants, evaluating MR's impact on teamwork and non-technical skills. While five studies demonstrated improvements in technical performance, only three studies reported a positive impact on teamwork performance. However, the heterogeneity across different scales, outcomes, and outcome measures weakens the inferences from this study. Similarly, Snelgrove and Gabbott (65), reviewed six studies and found that two-thirds of the primary literature supported MR's role in improving both technical and non-technical skills, including surgical movements, communication, and teamwork.
A systematic review by Rajarathnam et al. (55) found that 13 of 19 studies demonstrated improved performance when MR was combined with traditional training. Multiple RCTs have shown that MR is superior to textbook learning in both instructor-assessed and self-assessed technical skills (43, 66). Additionally, Yiasemidou et al. (67) found that MR was superior to video-based learning in improving laparoscopic cholecystectomy skills. Another review looking specifically at MR in orthopaedic surgery included 11 studies and found significant benefits, with cognitive training associated with notably improved surgical performance and increased knowledge when compared with traditional methods of learning, such as textbooks, slide shows, and videos (68).
It should be noted that while there is some evidence to suggest that MR in combination with practical training is beneficial over practical training alone (44), its use as an alternative may be detrimental, with one RCT showing lower operative speed and precision in the MR-trained group as compared to both box trainers and VR simulation (45). However, the study's impact was limited due to methodological limitations and heterogeneity, as well as the lack of large sample sizes and long-term learning assessments.
Arora et al. (13) performed an RCT assessing the stress levels of novice surgeons during simulated laparoscopic cholecystectomies. They found that the group who had undergone prior MR training had significantly lower heart rates, cortisol levels, and self-assessed stress levels as compared to the control group. Wetzel et al. (69) demonstrated similar results, while additionally identifying increased teamwork in the MR group. However, De Witte et al. (70) demonstrated an increase in cognitive load in MR study participants leading to detrimental learning outcomes when compared with those trained with traditional teaching methods alone.
A recent study by Modi et al. (71) used functional near-infrared spectroscopy (fNIRS) to assess the impact of MR on prefrontal and motor cortical activation during a laparoscopic knot-tying task. The authors demonstrated that mental rehearsal (MR) can enhance surgical skill acquisition by reducing prefrontal cognitive load, increasing motor cortical activation, and improving technical performance. The MR participants had better suture quality (lower leak volume, p = 0.019) and higher objective performance scores (p = 0.043) as compared to a textbook reading control group. These findings support the neurocognitive benefits of MR in optimising surgical task execution.
Mental rehearsal compared against simulation training
MR sessions can be conducted in various settings, either independently or as an adjunct to simulation-based training. Simulation is a well-established tool in surgical education and is widely recognised as an effective adjunct to traditional training (72). However, a frequent criticism of the current simulation approaches in surgery is the inability to fully replicate the experience of conducting a surgical operation and the limited ability to show lasting behaviour change outcomes (73). While simulation actively engages trainees with physical models, VR systems, or cadaveric specimens, mental rehearsal (MR) relies solely on cognitive imagery, allowing surgeons to visualise procedural steps, anticipate challenges, and engage sensory cues without physical execution of movements. Some hybrid models integrate MR with simulation, but these should be distinguished from pure MR techniques.
Unlike simulation, MR is not limited to visual reconstruction alone, but also engages auditory (74), olfactory (75), and haptic (76) imagery, potentially providing a more holistic representation of the real-world theatre environment. This cognitive flexibility makes MR particularly valuable for preparing surgeons to manage anatomical variations and intraoperative decision-making. For example, during a laparoscopic cholecystectomy, MR can be used to mentally reconstruct the dissection of Calot's triangle, allowing the surgeon to anticipate anatomical variations (e.g., proximal bifurcation of the cystic artery), and the potential associated complications (e.g., common bile duct injury).
Another key advantage of MR is its accessibility and cost-effectiveness. Simulation often requires expensive equipment, dedicated facilities, and instructor time, making widespread adoption challenging (72, 77). In contrast, MR has minimally associated costs and can be performed anytime, anywhere, making it universally accessible (55). While supervised MR sessions may enhance learning, they can also be effectively practised independently after initial training (13, 14). However, it is worth noting that unsupervised simulation training has been shown to yield less behaviour modification and performance improvement as compared to structured guidance (78), a factor that should be explored further in MR research.
MR has broad applications in surgical training. Experienced surgeons can use it to refine techniques for complex procedures (60). For others, it may be a cost-effective way of maintaining basic technical skills whilst on a career break or for clinician scientists who divide their time between research and surgery. Additionally, simulation and likely MR are useful for shortening the surgeon's learning curve for an operation (4), thus reinforcing patient safety by allowing surgeons to rehearse critical steps before performing them in real world settings. Given its flexibility, MR represents a valuable complement to simulation-based training, providing an alternative when physical simulation is unavailable and enhancing cognitive preparedness for surgery.
Implementation in a real-world surgical environment
The integration of MR in a real-world clinical setting is challenged by time limitations and the lack of consultant supervision given the growing demand for service provision. Studies that have implemented MR in actual surgical environments (as opposed to simulation-based training) suggest that MR can be performed pre-operatively to enhance technical preparedness, decision-making, and efficiency, without causing delays in surgical care and productivity (60, 66, 79). However, the majority of MR research remains focused on educational and training settings, with fewer studies evaluating its impact on live surgical performance.
Yiasemidou et al. (60) compared MR combined with virtual and physical patient-specific anatomical models and Magnetic Resonance Imaging (MRI) to routine preparation prior to surgery. The study recruited expert surgeons, who performed MR prior to commencing minimally invasive low anterior resections; the MR session focused on the pelvic dissection part of the procedure only. The primary outcome was the quality of the surgery. The study demonstrated no differences between the groups, and undertaking MR caused no delays in surgery. The only significant difference the authors found was the reduction in idle time during surgery for the group that performed MR using pre-operative MRIs as visual modalities.
Patel et al. (79) assessed error incidence before and after implementing a structured MR prior to the endovascular phase of combined open/endovascular arterial procedures. A trained observer assessed 15 combined procedures over a period of six weeks. Two blinded assessors carefully examined surgical event logs for technical errors. When they identified errors, these were categorised based on type, potential to harm the patient (danger), and potential to disrupt the procedure (delay). After conducting nine procedures, a focus group introduced a structured MR before the endovascular phase for the subsequent six combined procedures. The goal was to improve the surgical process and potentially reduce surgical errors and prevent patient harm. The error patterns were compared before and after the implementation of the MR technique to measure the impact of the MR intervention. After the application of MR, the error rates during the endovascular phase significantly decreased as compared to the rates before the intervention. Additionally, both the danger and delay scores were reduced (1.2 errors per dangerous event and 1.3 errors per delayed event, respectively) in comparison to the scores before the MR. The authors concluded that the MR may reduce the frequency and severity of surgical errors and patient harm.
Komesu et al. (66) assessed whether MR prior to cystoscopy can improve surgical performance. The authors conducted an RCT involving multiple centres. Residents with ≤3 previous cystoscopies were randomly assigned to two different preparation methods before the surgery: one group received preoperative mental imagery sessions, while the other group read a book chapter that described a cystoscopy. The primary focus of the study was to compare the surgical performance scores between the two groups. Additionally, they also measured the operative times and collected feedback from surgical residents about how they perceived the helpfulness of their preparation methods. A total of 68 residents participated in the randomisation process, with 33 assigned to the imagery group and 35 to the control group. The two groups were similar in terms of age, cystoscopic procedure experience, residency year level, and gender distribution. The residents who underwent mental imagery sessions before the surgery achieved surgical assessment scores that were 15.9% higher compared to the control group, with the difference statistically significant (p = 0.03). Furthermore, the residents who received the mental imagery preparation rated it as significantly more helpful as compared to the control group. However, there were no significant differences in the operative times between the two groups.
A qualitative study by Jolly et al. (80) explored ten Australian general surgery trainees' perceptions of MR using semi-structured interviews. All trainees reported using MR before operations, but this was informal and unstructured. The study highlighted that MR could address key challenges in surgical education, including reducing anxiety, improving communication, and enhancing training during periods of reduced clinical exposure. Participants supported the formal integration of MR into surgical curricula, with a preference for online training resources to mitigate time constraints. Standardisation of training was seen as a major benefit, although concerns were raised about variability in surgical techniques. The study concluded that mental training has the potential to supplement existing surgical education and should be implemented through a structured, accessible format to optimise trainee preparedness.
Discussion
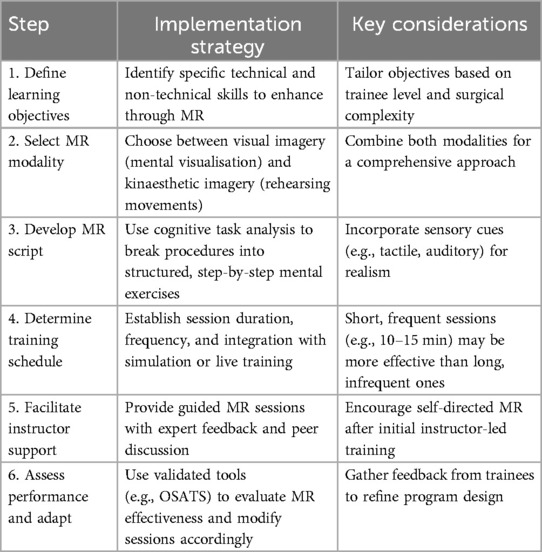
Our comprehensive review provides a practical guide and support for the effective integration of MR in surgical training and the ongoing maintenance of surgical competency. We propose a structured, stepwise approach to facilitate its adoption, outlining key steps for implementation (Table 2), and ensuring that MR is tailored to learners' and training program needs while complementing existing training modalities. We highlight several successful strategies across different experience levels, assessed through various learning and clinical outcomes. A critical question remains: how can MR be effectively implemented in real-world surgical environments without disrupting patient care or busy clinical workflows?
We found that MR is a more accessible and potentially more cost-effective technique than existing educational training such as simulation and reading of scientific materials. These findings raise a series of questions about why MR has not been routinely embedded in surgical curricula. What are effective guidelines for how best to embark on embedding MR in training contexts? What curricula design models are most effective from a pedagogical perspective? We highlight the merits of MR, while attempting to make the case to the surgical community on the need for the surgical community to seriously support implementing MR as an effective, inexpensive surgical competency training approach.
A key distinction in the MR literature is its application in controlled training environments vs. real-world surgical settings. In training settings, MR is primarily used as a cognitive and motor skill acquisition tool, helping trainees develop technical proficiency, procedural understanding, and confidence before hands-on practice. Studies conducted in simulation-based settings have reported improvements in task execution speed, error reduction, and stress management following MR interventions. However, the transition from training to real-world implementation is poorly defined, and the use of MR in surgical environments remains limited and inconsistent.
Real-world studies have focused on assessing MR's impact on intraoperative workflow, decision-making efficiency, and patient safety. These studies suggest that preoperative MR may enhance intraoperative efficiency, reduce idle time, and lower surgical error rates. However, due to limited sample sizes and variability in study design, it remains unclear whether MR consistently translates into improved postoperative outcomes and patient safety. There is currently no standardised protocol for implementing MR in surgical settings, and further research is required to evaluate its feasibility, scalability, and long-term impact on surgical outcomes and hospital workflow.
Unlike learning-focused studies, implementation research studies have primarily been descriptive rather than analytical, making it difficult to assess the true feasibility and long-term impact of MR in surgical practice. There are several variables that require calibration before MR is widely endorsed for effective implementation. For instance, the success of MR is highly associated with the expertise of the participants (81–83), therefore the duration and nature of the MR sessions may vary according to the surgeon's experience, support and competency levels. The MR sessions for non-experts should include a familiarisation stage with the procedure or task, followed by an assessment to ensure understanding. Expert surgeons can omit this step and instead focus on full sensory engagement and continuous repetition in a personally chosen environment to achieve optimal results. MR has been shown to increase movement accuracy (84, 85) and quality (86), however, the number of repetitions necessary for learning surgical procedures is unknown and needs to be evaluated through robust research. The variance in baseline ability to perform MR should also be addressed. Could the discrepancy in MR outcome results be due to the diverse MR baseline ability of the participants? Assessing baseline ability through validated questionnaires and through focus groups, as well as ethnographic observations to help determine the optimal MR method (visual, haptic, or other) for each surgeon. A personalised, targeted approach will enhance surgeon engagement, MR outcomes and improve their skill acquisition.
Limitations
It is important to acknowledge the limitations associated with our review. First, the evidence base on MR remains heterogeneous, with significant variability in study designs, outcome measures, and intervention protocols, making direct comparisons challenging. Most studies have focused on short-term performance metrics, with few evaluating long-term skill retention or clinical outcomes. Second, there is a lack of standardized pedagogical models guiding MR implementation, leading to inconsistencies in training approaches across studies. Third, from a methodological perspective, this review was narrative rather than systematic, meaning that the search strategy, study selection, and data synthesis were not conducted using formal systematic review methodology. While the narrative review approach allows for a broad and flexible synthesis of MR applications, it does not provide a meta-analysis or formal quality appraisal of included studies. Finally, many of the studies done on MR impact assume fixed external team and hospital environments, and yet other unmeasured changes such as staffing and workflow changes might have impacted the studies putative benefits.
Future directions
Future research should seek to integrate validated skill acquisition models and surgical performance theories to improve the design, consistency, and reproducibility of MR interventions. The current variability in MR protocols, training duration, and outcome measures highlights the need for a standardised framework that can be applied across different surgical specialties and levels of expertise. In addition, more robust studies are needed to determine the long-term impacts of MR on surgical performance and patient outcomes, particularly in real-world settings. While existing evidence suggests MR can enhance technical proficiency and decision-making, few studies have assessed its sustained effects on skill retention, intraoperative efficiency, and postoperative complications.
Prospective, multicentre trials and longitudinal studies are needed to explore how MR influences surgeon competencies over time, how it integrates with existing training methods, and whether its benefits translate into improved patient care. Furthermore, research is needed to focus on addressing the logistical and practical challenges of implementing MR in high-pressure surgical environments, ensuring that it can be seamlessly incorporated into routine practice without disrupting workflow or increasing cognitive load. Future studies can help establish MR as a reliable, evidence-based training tool that can optimise both learning outcomes and clinical performance in surgery.
Conclusions
Our review explored the neurocognitive mechanisms underlying mental rehearsal (MR), its current applications in surgical education, and its potential future role in optimising surgical performance and patient outcomes. MR offers promising benefits for surgeon training by enhancing both technical and non-technical skills, improving cognitive preparedness, and may serve as a cost-effective adjunct to traditional training methods. More work is needed to bridge the gaps between theory and practice, requiring a continuous loop of knowledge generation, dissemination, and uptake on how best to provide surgical training under real world conditions. Our paper provides a training framework for integrating MR more effectively into surgical training. Future research is needed on standardising training protocols, novel study designs that improve statistical and logistical efficiency, and evaluating long-term patient and learner outcomes to maximise MR effectiveness in surgical education.
Author contributions
JW: Data curation, Visualization, Writing – original draft, Writing – review & editing. BH: Writing – original draft, Writing – review & editing. PBar: Data curation, Formal analysis, Methodology, Project administration, Writing – original draft, Writing – review & editing. PBan: Writing – original draft, Writing – review & editing. AM: Writing – original draft, Writing – review & editing. FL: Writing – original draft, Writing – review & editing. FM: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. DJ: Writing – original draft, Writing – review & editing. DM: Writing – original draft, Writing – review & editing. MY: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Resources, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The publication fees for this article are kindly provided by the University of York
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Jackson PL, Lafleur MF, Malouin F, Richards C, Doyon J. Potential role of mental practice using motor imagery in neurologic rehabilitation. Arch Phys Med Rehabil. (2001) 82:1133–41. doi: 10.1053/apmr.2001.24286
2. Jeannerod M. Mental imagery in the motor context. Neuropsychologia. (1995) 33:1419–32. doi: 10.1016/0028-3932(95)00073-C
3. Bernardi NF, De Buglio M, Trimarchi PD, Chielli A, Bricolo E. Mental practice promotes motor anticipation: evidence from skilled music performance. Front Hum Neurosci. (2013) 7:451. doi: 10.3389/fnhum.2013.00451
4. Hall JC. Imagery practice and the development of surgical skills. Am J Surg. (2002) 184:465–70. doi: 10.1016/S0002-9610(02)01007-3
5. Decety J, Jeannerod M, Prablanc C. The timing of mentally represented actions. Behav Brain Res. (1989) 34:35–42. doi: 10.1016/S0166-4328(89)80088-9
6. Decety J, Jeannerod M. Mentally simulated movements in virtual reality: does fitts’s law hold in motor imagery? Behav Brain Res. (1995) 72:127–34. doi: 10.1016/0166-4328(96)00141-6
7. Decety J, Grèzes J. Neural mechanisms subserving the perception of human actions. Trends Cogn Sci. (1999) 3:172–8. doi: 10.1016/S1364-6613(99)01312-1
8. Rodrigues EC, Lemos T, Gouvea B, Volchan E, Imbiriba LA, Vargas CD. Kinesthetic motor imagery modulates body sway. Neuroscience. (2010) 169:743–50. doi: 10.1016/j.neuroscience.2010.04.081
9. Wong AH, Ahmed RA, Ray JM, Khan H, Hughes PG, McCoy CE, et al. Supporting the quadruple aim using simulation and human factors during COVID-19 care. Am J Med Qual. (2021) 36:73–83. doi: 10.1097/01.JMQ.0000735432.16289.d2
10. Pearson DG, Deeprose C, Wallace-Hadrill SMA, Heyes SB, Holmes EA. Assessing mental imagery in clinical psychology: a review of imagery measures and a guiding framework. Clin Psychol Rev. (2013) 33:1–23. doi: 10.1016/j.cpr.2012.09.001
11. Causer J, Barach P, Williams AM. Expertise in medicine: using the expert performance approach to improve simulation training. Med Educ. (2014) 48:115–23. doi: 10.1111/medu.12306
12. Schmidt RA. A schema theory of discrete motor skill learning. Psychol Rev. (1975) 82:225–60. doi: 10.1037/h0076770
13. Arora S, Aggarwal R, Moran A, Sirimanna P, Crochet P, Darzi A, et al. Mental practice: effective stress management training for novice surgeons. J Am Coll Surg. (2011) 212:225–33. doi: 10.1016/j.jamcollsurg.2010.09.025
14. Arora S, Aggarwal R, Sirimanna P, Moran A, Grantcharov T, Kneebone R, et al. Mental practice enhances surgical technical skills: a randomized controlled study. Ann Surg. (2011) 253:265–70. doi: 10.1097/SLA.0b013e318207a789
16. Shepard RN, Cooper LA. Mental Images and Their Transformations. Cambridge, MA: MIT Press (1982). p. 364. Available at: https://psycnet.apa.org/fulltext/1986-97354-000.pdf
17. Kosslyn SM, Thompson WL, Ganis G. The Case for Mental Imagery. USA: Oxford University Press (2006). p. 248.
18. Goodale MA. Image and brain: the resolution of the imagery debate. J Cogn Neurosci. (1995) 7:415–20. doi: 10.1162/jocn.1995.7.3.415
19. Zimmermann-Schlatter A, Schuster C, Puhan MA, Siekierka E, Steurer J. Efficacy of motor imagery in post-stroke rehabilitation: a systematic review. J Neuroeng Rehabil. (2008) 5:8. doi: 10.1186/1743-0003-5-8
20. Annett J. Motor imagery: perception or action? Neuropsychologia. (1995) 33:1395–417. doi: 10.1016/0028-3932(95)00072-B
21. Jeannerod M, Frak V. Mental imaging of motor activity in humans. Curr Opin Neurobiol. (1999) 9:735–9. doi: 10.1016/S0959-4388(99)00038-0
22. Frak V, Paulignan Y, Jeannerod M. Orientation of the opposition axis in mentally simulated grasping. Exp Brain Res. (2001) 136:120–7. doi: 10.1007/s002210000583
23. Allami N, Brovelli A, Hamzaoui EM, Regragui F, Paulignan Y, Boussaoud D. Neurophysiological correlates of visuo-motor learning through mental and physical practice. Neuropsychologia. (2014) 55:6–14. doi: 10.1016/j.neuropsychologia.2013.12.017
24. Lotze M, Montoya P, Erb M, Hülsmann E, Flor H, Klose U, et al. Activation of cortical and cerebellar motor areas during executed and imagined hand movements: an fMRI study. J Cogn Neurosci. (1999) 11:491–501. doi: 10.1162/089892999563553
25. Naito E, Kochiyama T, Kitada R, Nakamura S, Matsumura M, Yonekura Y, et al. Internally simulated movement sensations during motor imagery activate cortical motor areas and the cerebellum. J Neurosci. (2002) 22:3683–91. doi: 10.1523/JNEUROSCI.22-09-03683.2002
26. Gerardin E, Sirigu A, Lehéricy S, Poline JB, Gaymard B, Marsault C, et al. Partially overlapping neural networks for real and imagined hand movements. Cereb Cortex. (2000) 10:1093–104. doi: 10.1093/cercor/10.11.1093
27. Nair DG, Purcott KL, Fuchs A, Steinberg F, Kelso JAS. Cortical and cerebellar activity of the human brain during imagined and executed unimanual and bimanual action sequences: a functional MRI study. Brain Res Cogn Brain Res. (2003) 15:250–60. doi: 10.1016/S0926-6410(02)00197-0
28. Sirigu A, Duhamel JR, Cohen L, Pillon B, Dubois B, Agid Y. The mental representation of hand movements after parietal cortex damage. Science. (1996) 273:1564–8. doi: 10.1126/science.273.5281.1564
29. Wolbers T, Weiller C, Büchel C. Contralateral coding of imagined body parts in the superior parietal lobe. Cereb Cortex. (2003) 13:392–9. doi: 10.1093/cercor/13.4.392
30. Binkofski F, Amunts K, Stephan KM, Posse S, Schormann T, Freund HJ, et al. Broca’s region subserves imagery of motion: a combined cytoarchitectonic and fMRI study. Hum Brain Mapp. (2000) 11:273–85. doi: 10.1002/1097-0193(200012)11:4%3C273::AID-HBM40%3E3.0.CO;2-0
31. Porro CA, Francescato MP, Cettolo V, Diamond ME, Baraldi P, Zuiani C, et al. Primary motor and sensory cortex activation during motor performance and motor imagery: a functional magnetic resonance imaging study. J Neurosci. (1996) 16:7688–98. doi: 10.1523/JNEUROSCI.16-23-07688.1996
32. Roth M, Decety J, Raybaudi M, Massarelli R, Delon-Martin C, Segebarth C, et al. Possible involvement of primary motor cortex in mentally simulated movement: a functional magnetic resonance imaging study. Neuroreport. (1996) 7:1280–4. doi: 10.1097/00001756-199605170-00012
33. Munzert J, Lorey B, Zentgraf K. Cognitive motor processes: the role of motor imagery in the study of motor representations. Brain Res Rev. (2009) 60:306–26. doi: 10.1016/j.brainresrev.2008.12.024
34. Beisteiner R, Höllinger P, Lindinger G, Lang W, Berthoz A. Mental representations of movements. Brain potentials associated with imagination of hand movements. Electroencephalogr Clin Neurophysiol. (1995) 96:183–93. doi: 10.1016/0168-5597(94)00226-5
35. Cunnington R, Iansek R, Bradshaw JL, Phillips JG. Movement-related potentials associated with movement preparation and motor imagery. Exp Brain Res. (1996) 111:429–36. doi: 10.1007/BF00228732
36. Caldara R, Deiber M-P, Andrey C, Michel CM, Thut G, Hauert C-A. Actual and mental motor preparation and execution: a spatiotemporal ERP study. Exp Brain Res. (2004) 159:389–99. doi: 10.1007/s00221-004-2101-0
37. Caspers H, Speckmann EJ, Lehmenkühler A. DC potentials of the cerebral cortex. Seizure activity and changes in gas pressures. Rev Physiol Biochem Pharmacol. (1987) 106:127–78. doi: 10.1007/BFb0027576
38. Sweller J. Cognitive load during problem solving: effects on learning. Cogn Sci. (1988) 12:257–85. doi: 10.1207/s15516709cog1202_4
39. Meichenbaum D, Cameron R. Stress inoculation training. In: Meichenbaum D, Jaremko ME, editors. Stress Reduction and Prevention. Boston, MA: Springer US (1989). p. 115–54.
40. Ignacio J, Scherpbier A, Dolmans D, Rethans J-J, Liaw SY. Mental rehearsal strategy for stress management and performance in simulations. Clin Simul Nurs. (2017) 13:295–302. doi: 10.1016/j.ecns.2017.04.005
41. Louridas M, Bonrath EM, Sinclair DA, Dedy NJ, Grantcharov TP. Randomized clinical trial to evaluate mental practice in enhancing advanced laparoscopic surgical performance. Br J Surg. (2015) 102:37–44. doi: 10.1002/bjs.9657
42. Sanders CW, Sadoski M, Bramson R, Wiprud R, Van Walsum K. Comparing the effects of physical practice and mental imagery rehearsal on learning basic surgical skills by medical students. Am J Obstet Gynecol. (2004) 191:1811–4. doi: 10.1016/j.ajog.2004.07.075
43. Sanders CW, Sadoski M, van Walsum K, Bramson R, Wiprud R, Fossum TW. Learning basic surgical skills with mental imagery: using the simulation centre in the mind. Med Educ. (2008) 42:607–12. doi: 10.1111/j.1365-2923.2007.02964.x
44. Eldred-Evans D, Grange P, Cheang A, Yamamoto H, Ayis S, Mulla M, et al. Using the mind as a simulator: a randomized controlled trial of mental training. J Surg Educ. (2013) 70:544–51. doi: 10.1016/j.jsurg.2013.04.003
45. Mulla M, Sharma D, Moghul M, Kailani O, Dockery J, Ayis S, et al. Learning basic laparoscopic skills: a randomized controlled study comparing box trainer, virtual reality simulator, and mental training. J Surg Educ. (2012) 69:190–5. doi: 10.1016/j.jsurg.2011.07.011
46. Saab SS, Bastek J, Dayaratna S, Hutton E, Salva CR. Development and validation of a mental practice tool for total abdominal hysterectomy. J Surg Educ. (2017) 74:216–21. doi: 10.1016/j.jsurg.2016.10.005
47. Jungmann F, Gockel I, Hecht H, Kuhr K, Räsänen J, Sihvo E, et al. Impact of perceptual ability and mental imagery training on simulated laparoscopic knot-tying in surgical novices using a nissen fundoplication model. Scand J Surg. (2011) 100:78–85. doi: 10.1177/145749691110000203
48. Cragg J, Mushtaq F, Lal N, Garnham A, Hallissey M, Graham T, et al. Surgical cognitive simulation improves real-world surgical performance: randomized study. BJS Open. (2021) 5:zrab003. doi: 10.1093/bjsopen/zrab003
49. Kaulfuss JC, Kluth LA, Marks P, Grange P, Fisch M, Chun FKH, et al. Long-term effects of mental training on manual and cognitive skills in surgical education—a prospective study. J Surg Educ. (2021) 78:1216–26. doi: 10.1016/j.jsurg.2020.11.005
50. Immenroth M, Bürger T, Brenner J, Nagelschmidt M, Eberspächer H, Troidl H. Mental training in surgical education: a randomized controlled trial: a randomized controlled trial. Ann Surg. (2007) 245:385–91. doi: 10.1097/01.sla.0000251575.95171.b3
51. Bathalon S, Dorion D, Darveau S, Martin M. Cognitive skills analysis, kinesiology, and mental imagery in the acquisition of surgical skills. J Otolaryngol. (2005) 34:328. doi: 10.2310/7070.2005.34506
52. Goble MSL, Raison N, Mekhaimar A, Dasgupta P, Ahmed K. Adapting motor imagery training protocols to surgical education: a systematic review and meta-analysis. Surg Innov. (2021) 28:329–51. doi: 10.1177/1553350621990480
53. Rozand V, Lebon F, Stapley PJ, Papaxanthis C, Lepers R. A prolonged motor imagery session alter imagined and actual movement durations: potential implications for neurorehabilitation. Behav Brain Res. (2016) 297:67–75. doi: 10.1016/j.bbr.2015.09.036
54. Suica Z, Behrendt F, Gäumann S, Gerth U, Schmidt-Trucksäss A, Ettlin T, et al. Imagery ability assessments: a cross-disciplinary systematic review and quality evaluation of psychometric properties. BMC Med. (2022) 20:166. doi: 10.1186/s12916-022-02295-3
55. Rajaratnam V, Rahman NA, Omar UF, Ng HJH. Mental practice in surgical training. Bull R Coll Surg Engl. (2021) 103:403–8. doi: 10.1308/rcsbull.2021.145
56. Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. (1997) 84:273–8. doi: 10.1046/j.1365-2168.1997.02502.x
57. Rao A, Tait I, Alijani A. Systematic review and meta-analysis of the role of mental training in the acquisition of technical skills in surgery. Am J Surg. (2015) 210:545–53. doi: 10.1016/j.amjsurg.2015.01.028
58. Souiki T, Benzagmout M, Alami B, Ibn Majdoub K, Toughrai I, Mazaz K, et al. Impact of mental imagery on enhancing surgical skills learning in novice’s surgeons: a pilot study. BMC Med Educ. (2021) 21:545. doi: 10.1186/s12909-021-02987-z
59. Cosman PH, Sirimanna P, Barach P. Building surgical expertise through the science of continuous learning and training. In: Sanchez JA, Barach P, Johnson JK, Jacobs JP, editors. Surgical Patient Care. Cham: Springer International Publishing (2017). p. 185–204.
60. Yiasemidou M, Mushtaq F, Basheer M, Galli R, Panagiotou D, Stock S, et al. Patient-specific mental rehearsal with three-dimensional models before low anterior resection: randomized clinical trial. BJS Open. (2021) 5:zraa004. doi: 10.1093/bjsopen/zraa004
61. Skervin AL, Scott HJ. Mental rehearsal: a useful simulation adjunct to surgical training. Surgeon. (2021) 19:e423–9. doi: 10.1016/j.surge.2020.12.007
62. Davison S, Raison N, Khan MS, Dasgupta P, Ahmed K. Mental training in surgical education: a systematic review. ANZ J Surg. (2017) 87:873–8. doi: 10.1111/ans.14140
63. NE A, Bean EA, Hammonds SC, Stefanidis D. Application of mental skills training in surgery: a review of its effectiveness and proposed next steps. J Laparoendosc Adv Surg Tech A. (2017) 27:459–69. doi: 10.1089/lap.2016.0656
64. Gabbott B, Tennent D, Snelgrove H. Effect of mental rehearsal on team performance and non-technical skills in surgical teams: systematic review. BJS Open. (2020) 4:1062–71. doi: 10.1002/bjs5.50343
65. Snelgrove H, Gabbott B. Critical analysis of evidence about the impacts on surgical teams of “mental practice” in systematic reviews: a systematic rapid evidence assessment (SREA). BMC Med Educ. (2020) 20:221. doi: 10.1186/s12909-020-02131-3
66. Komesu Y, Urwitz-Lane R, Ozel B, Lukban J, Kahn M, Muir T, et al. Does mental imagery prior to cystoscopy make a difference? A randomized controlled trial. Am J Obstet Gynecol. (2009) 201:218.e1–9. doi: 10.1016/j.ajog.2009.04.008
67. Yiasemidou M, Glassman D, Mushtaq F, Athanasiou C, Williams M-M, Jayne D, et al. Mental practice with interactive 3D visual aids enhances surgical performance. Surg Endosc. (2017) 31:4111–7. doi: 10.1007/s00464-017-5459-3
68. Anderson MJJ, deMeireles AJ, Trofa DP, Kovacevic D, Ahmad CS, Lynch TS. Cognitive training in orthopaedic surgery. J Am Acad Orthop Surg Glob Res Rev. (2021) 5:e21. doi: 10.5435/JAAOSGlobal-D-21-00021
69. Wetzel CM, George A, Hanna GB, Athanasiou T, Black SA, Kneebone RL, et al. Stress management training for surgeons-a randomized, controlled, intervention study. Ann Surg. (2011) 253:488–94. doi: 10.1097/SLA.0b013e318209a594
70. De Witte B, Di Rienzo F, Martin X, Haixia Y, Collet C, Hoyek N. Implementing cognitive training into a surgical skill course: a pilot study on laparoscopic suturing and knot tying. Surg Innov. (2018) 25:625–35. doi: 10.1177/1553350618800148
71. Modi HN, Osborne-Grinter M, Patel R, Darzi A, Leff DR, Singh H. Investigating the impact of mental rehearsal on prefrontal and motor cortical haemodynamic responses in surgeons using optical neuroimaging. Front Hum Neurosci. (2024) 18:1386005. doi: 10.3389/fnhum.2024.1386005
72. Stefanidis D, Sevdalis N, Paige J, Zevin B, Aggarwal R, Grantcharov T, et al. Association for surgical education simulation committee. Simulation in surgery: what’s needed next? Ann Surg. (2015) 261:846–53. doi: 10.1097/SLA.0000000000000826
73. McCaskie AW, Kenny DT, Deshmukh S. How can surgical training benefit from theories of skilled motor development, musical skill acquisition and performance psychology? Med J Aust. (2011) 194:463–5. doi: 10.5694/j.1326-5377.2011.tb03062.x
74. Cotter KN. Mental control in musical imagery: a dual component model. Front Psychol. (2019) 10:1904. doi: 10.3389/fpsyg.2019.01904
75. Stevenson RJ, Case TI. Olfactory imagery: a review. Psychon Bull Rev. (2005) 12:244–64. doi: 10.3758/BF03196369
76. Jüttner M, Rentschler I. Imagery in multi-modal object learning. Behav Brain Sci. (2002) 25:197–8. doi: 10.1017/S0140525X0238004X
77. Meling TR, Meling TR. The impact of surgical simulation on patient outcomes: a systematic review and meta-analysis. Neurosurg Rev. (2021) 44:843–54. doi: 10.1007/s10143-020-01314-2
78. Cole SJ, Mackenzie H, Ha J, Hanna GB, Miskovic D. Randomized controlled trial on the effect of coaching in simulated laparoscopic training. Surg Endosc. (2014) 28:979–86. doi: 10.1007/s00464-013-3265-0
79. Patel SR, Gohel MS, Hamady M, Albayati MA, Riga CV, Cheshire NJW, et al. Reducing errors in combined open/endovascular arterial procedures: influence of a structured mental rehearsal before the endovascular phase. J Endovasc Ther. (2012) 19:383–9. doi: 10.1583/11-3785R.1
80. Jolly S, Asokan G. Mental training in general surgery: a qualitative review of Australian trainee perceptions. ANZ J Surg. (2024) 94:63–7. doi: 10.1111/ans.18620
81. Fourkas AD, Bonavolontà V, Avenanti A, Aglioti SM. Kinesthetic imagery and tool-specific modulation of corticospinal representations in expert tennis players. Cereb Cortex. (2008) 18:2382–90. doi: 10.1093/cercor/bhn005
82. Jeannerod M, Decety J, Michel F. Impairment of grasping movements following a bilateral posterior parietal lesion. Neuropsychologia. (1994) 32:369–80. doi: 10.1016/0028-3932(94)90084-1
83. Reed CL. Chronometric comparisons of imagery to action: visualizing versus physically performing springboard dives. Mem Cognit. (2002) 30:1169–78. doi: 10.3758/BF03213400
84. Pascual-Leone A, Nguyet D, Cohen LG, Brasil-Neto JP, Cammarota A, Hallett M. Modulation of muscle responses evoked by transcranial magnetic stimulation during the acquisition of new fine motor skills. J Neurophysiol. (1995) 74:1037–45. doi: 10.1152/jn.1995.74.3.1037
85. Yágüez L, Nagel D, Hoffman H, Canavan AG, Wist E, Hömberg V. A mental route to motor learning: improving trajectorial kinematics through imagery training. Behav Brain Res. (1998) 90:95–106. doi: 10.1016/S0166-4328(97)00087-9
Keywords: education, surgery, simulation, mental rehearsal (MR), training
Citation: Walshaw J, Huo B, Barach P, Banks P, McClean A, Lebon F, Mushtaq F, Jayne D, Miskovic D and Yiasemidou M (2025) Embedding mental rehearsal in surgery: a comprehensive review of the evidence. Front. Surg. 12:1524468. doi: 10.3389/fsurg.2025.1524468
Received: 7 November 2024; Accepted: 9 May 2025;
Published: 13 June 2025.
Edited by:
Theodoros Michelakos, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Anastasios Karneris, National and Kapodistrian University of Athens, GreeceNathan Coppersmith, Yale-New Haven Hospital, United States
Aysel Doğan, Toros University, Türkiye
Wei Li, Southern Medical University, China
Copyright: © 2025 Walshaw, Huo, Barach, Banks, McClean, Lebon, Mushtaq, Jayne, Miskovic and Yiasemidou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Marina Yiasemidou, bWFyaW5heWlhc2VtaWRvdUBnbWFpbC5jb20=
 Josephine Walshaw
Josephine Walshaw Bright Huo2
Bright Huo2 Paul Barach
Paul Barach Adam McClean
Adam McClean Florent Lebon
Florent Lebon Faisal Mushtaq
Faisal Mushtaq Marina Yiasemidou
Marina Yiasemidou