- Department of Neurosurgery, The First Affiliated Hospital of Harbin Medical University, Harbin, Heilongjiang, China
Background and purpose: Tandem occlusion is a significant risk factor for poor outcomes following intravenous thrombolysis. The necessity of bridging therapy [intravenous thrombolysis prior to mechanical thrombectomy (MT)] for patients with tandem occlusion remains controversial. This study assessed the safety and efficacy of direct MT vs. bridging therapy in patients with tandem occlusions in the anterior circulation.
Methods: This retrospective study enrolled patients with anterior circulation tandem occlusions treated with either direct mechanical thrombectomy (MT-alone group) or intravenous alteplase thrombolysis followed by MT (bridging group) between January 2019 and March 2022. The primary outcome was prespecified as a favorable outcome [modified Rankin Scale (mRS) score of 0–2] at 90 days. Secondary outcomes included successful reperfusion, overall mortality at 90 days, and rates of symptomatic intracranial hemorrhage (SICH) and asymptomatic intracranial hemorrhage (aSICH).
Results: A total of 110 patients were enrolled, with 49 in the MT-alone group and 61 in the bridging group. A favorable outcome (mRS score of 0–2) at 90 days was achieved in 25 patients (51.0%) in the MT-alone group and in 34 patients (55.7%) in the bridging group, showing no significant difference between the groups, with an adjusted odds ratio (aOR) of 1.17 (95% CI, 0.47–2.90; P = 0.743). The incidence of aSICH was higher in the bridging group than in the MT-alone group [31.1% vs. 14.3%; aOR, 2.86 (95% CI, 1.04–7.88); P = 0.042]. Rates of successful reperfusion, overall mortality at 90 days, and SICH were similar between the groups. Multivariate analysis showed that a lower baseline National Institutes of Health Stroke Scale (NIHSS) score (P = 0.005), intraprocedural tirofiban administration (P = 0.012), and internal carotid artery stent implantation (P = 0.040) were associated with a favorable outcome at 90 days.
Conclusion: This study found no evidence that prior intravenous thrombolysis affects clinical or imaging outcomes in patients with acute ischemic stroke due to anterior circulation tandem occlusions after endovascular thrombectomy. Bridging therapy may be associated with an increased rate of aSICH. Intraprocedural tirofiban administration, stent implantation, and a lower baseline NIHSS score were associated with favorable outcomes.
1 Introduction
Anterior circulation tandem occlusion was defined as an intracranial anterior circulation large vessel occlusion [distal intracranial internal carotid artery (ICA) or M1-M2 segment of the middle cerebral artery] along with ipsilateral high-grade cervical ICA stenosis or occlusion (complete occlusion or stenosis ≥90% as per the North American Symptomatic Carotid Endarterectomy Trial) (1–3). Anterior circulation tandem occlusion occurs in approximately 15%–20% of patients with acute ischemic stroke (4). Due to its complex pathophysiology, managing such lesions presents a significant clinical challenge. Tandem occlusion is a notable risk factor for poor outcomes following intravenous thrombolysis (1, 5), and published studies have demonstrated the safety and efficacy of endovascular mechanical thrombectomy (MT) for tandem occlusion (1–4). For patients with acute large artery anterior circulation stroke, multiple studies have reported the benefits of bridging therapy (intravenous thrombolysis prior to MT) (6–10). However, recent studies suggest that, for patients with acute large vessel occlusive stroke, direct mechanical thrombectomy may be non-inferior to bridging therapy in terms of recanalization and outcomes (10, 11). Previous randomized controlled studies, however, did not specifically describe or summarize outcomes for patients with tandem lesions, leaving a lack of sufficient evidence on whether anterior circulation tandem occlusions benefit from bridging therapy (11–13). This retrospective study aimed to compare clinical outcomes in patients with anterior circulation tandem occlusions treated with bridging therapy vs. those treated with MT alone.
2 Materials and methods
2.1 Study design and patients
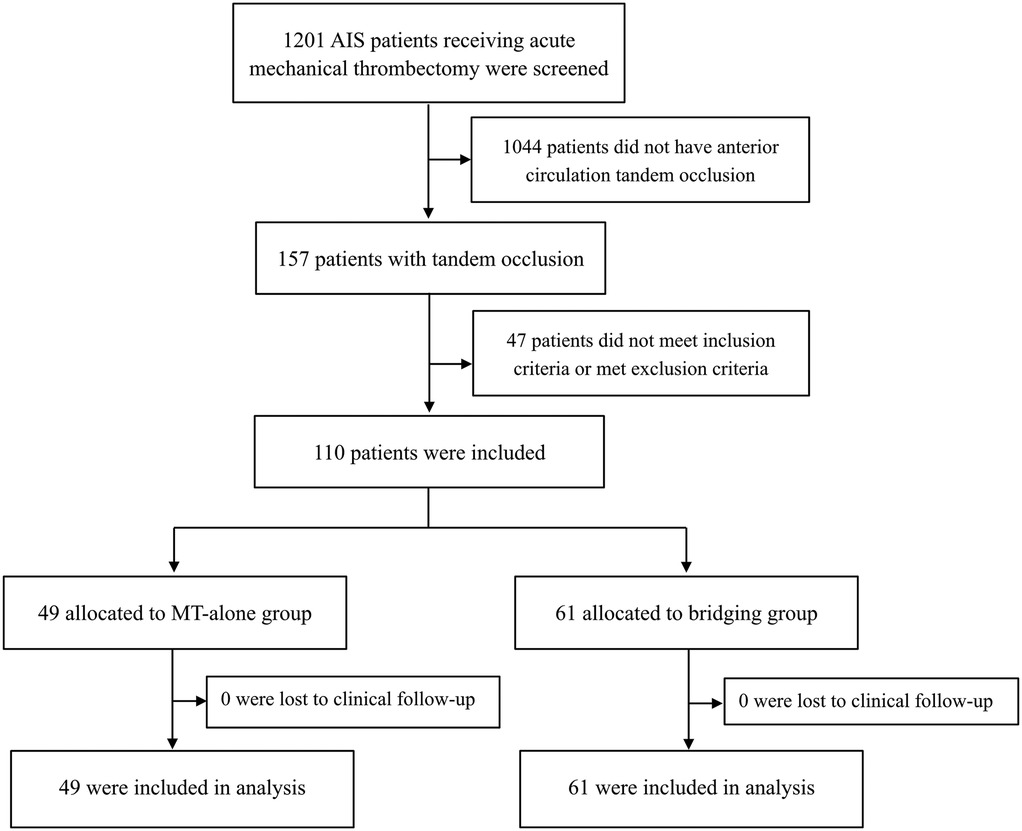
This retrospective, observational cohort study assessed the safety and efficacy of direct MT vs. bridging therapy in patients with anterior circulation tandem occlusions from the First Affiliated Hospital of Harbin Medical University between January 2019 and March 2022. We screened 1,201 patients with acute anterior circulation stroke who had received endovascular treatment. Among them, 110 patients with tandem occlusions meeting the inclusion criteria were enrolled in our study. The patients included in the study received either MT alone (MT-alone group) or intravenous alteplase followed by MT (bridging group).
To be eligible for inclusion in this study, the patients had to meet the following inclusion criteria: (1) patients were 18 years of age or older; (2) had disabling symptoms, defined as a National Institutes of Health Stroke Scale (NIHSS) score ≥6 (13); (3) based on non-contrast computed tomography (CT), patients with an Alberta Stroke Program Early CT Score (ASPECTS) ≥6; (4) patients with anterior circulation tandem occlusions as shown on computed tomographic angiography (CTA) or digital subtraction angiography (DSA), that could be treated with intravenous alteplase within 4.5 h after symptom onset; (5) patients receiving intravenous thrombolysis met the indications for alteplase administration, with no contraindications; (6) all patients received endovascular treatment within 6 h of acute stroke onset. Patients were excluded from the study if they met any of the following exclusion criteria: (1) angiographic results after thrombolysis indicated vascular recanalization without the need for further endovascular intervention; (2) patients received intra-arterial alteplase or urokinase as rescue therapy after reperfusion failure; (3) patients with an mRS score >2 before symptom onset; (4) patients who received treatment with other intravenous thrombolytic drugs, such as urokinase, were excluded to reduce the potential impact on the outcomes. The study flowchart is shown in Figure 1. Our study was approved by the Ethics Committee of the first affiliated hospital of Harbin medical university and the informed consent was waived.
2.2 Data collection
Baseline characteristics, including age, sex, and medical history, were recorded for each patient. Baseline stroke severity was assessed using the NIHSS score. The extent of early cerebral ischemia on baseline CT was measured with the ASPECTS score. Time intervals from stroke onset to groin puncture and to reperfusion were also documented. The location of arterial occlusion was identified using CTA or DSA [internal carotid artery (ICA) or M1 and M2 segments of the middle cerebral artery (MCA)]. Recanalization was measured by the expanded Thrombolysis in Cerebral Infarction (eTICI) score [ranging from 0 (no reperfusion) to 3 (complete reperfusion)] on the final DSA after the procedure, with successful recanalization defined as eTICI 2b-3. Postprocedural symptomatic intracranial hemorrhage (SICH) and asymptomatic intracranial hemorrhage (aSICH) were recorded, and hemorrhage was classified according to the Heidelberg criteria (14). Functional outcomes at 90 days post-stroke were evaluated by neurointerventionists during routine follow-up visits using the modified Rankin Scale (mRS) score. If a patient was unable to return to the hospital, outcomes were assessed through a standardized telephone interview.
2.3 Treatment
According to international guidelines, patients in the bridging group received alteplase at a total dose of 0.9 mg/kg within 4.5 h of symptom onset (10% administered as an intravenous bolus and the remaining 90% as an intravenous infusion over 1 h). The infusion could be completed during endovascular treatment. For endovascular mechanical thrombectomy, patients were positioned supine, and either local or general anesthesia was administered based on the patient's cooperation and vascular condition. Cerebral angiography was first performed to assess the site of vascular occlusion and primary compensatory flow. The loach guide wire guided the 8F guide catheter (Boston Scientific, USA) and the intermediate catheter to the vicinity of the affected common carotid artery bifurcation. The intermediate catheter was initially advanced through the severe stenosis or occlusion in the ICA's proximal segment. If unsuccessful, a microcatheter and micro guide wire were used to navigate the ICA under roadmap guidance. Following percutaneous transluminal angioplasty of the ICA, the intermediate catheter was passed through the stenotic or occluded segment, and intracranial vascular thrombectomy and recanalization were performed using standard techniques. After intracranial vessel recanalization, patients were monitored for 20 min, with the degree of stenosis assessed via common carotid artery angiography to determine the need for carotid stent implantation.
2.4 Outcomes
The primary outcome was prespecified as a favorable outcome (mRS score of 0–2) at 90 days. Secondary outcomes included successful reperfusion (eTICI score of 2b-3) at the procedure's end, incidence of SICH and aSICH, and overall mortality at 90 days.
2.5 Statistical analyses
Continuous variables following a normal distribution were described as mean ± standard deviation (SD), while non-normally distributed data were represented by median and interquartile range (IQR). Categorical variables were presented as numbers with percentages. For continuous variables, independent sample t-tests or Mann–Whitney U-tests were used according to data distribution, and Fisher's exact test and chi-square test were used for categorical variables. The association between treatment methods and outcomes was expressed as an odds ratio (OR) with adjustments for confounders, estimated by a multivariate logistic regression model. Outcomes were calculated with a 95% confidence interval (CI), and variables with P < 0.1 in the univariate analysis were included in the model. Given the number of events, variables were selected cautiously for model entry. All regression results presented both unadjusted and adjusted OR (aOR) values. Statistical analyses were performed using SPSS 22.0 software (IBM), with P < 0.05 considered statistically significant.
3 Results
3.1 Study population
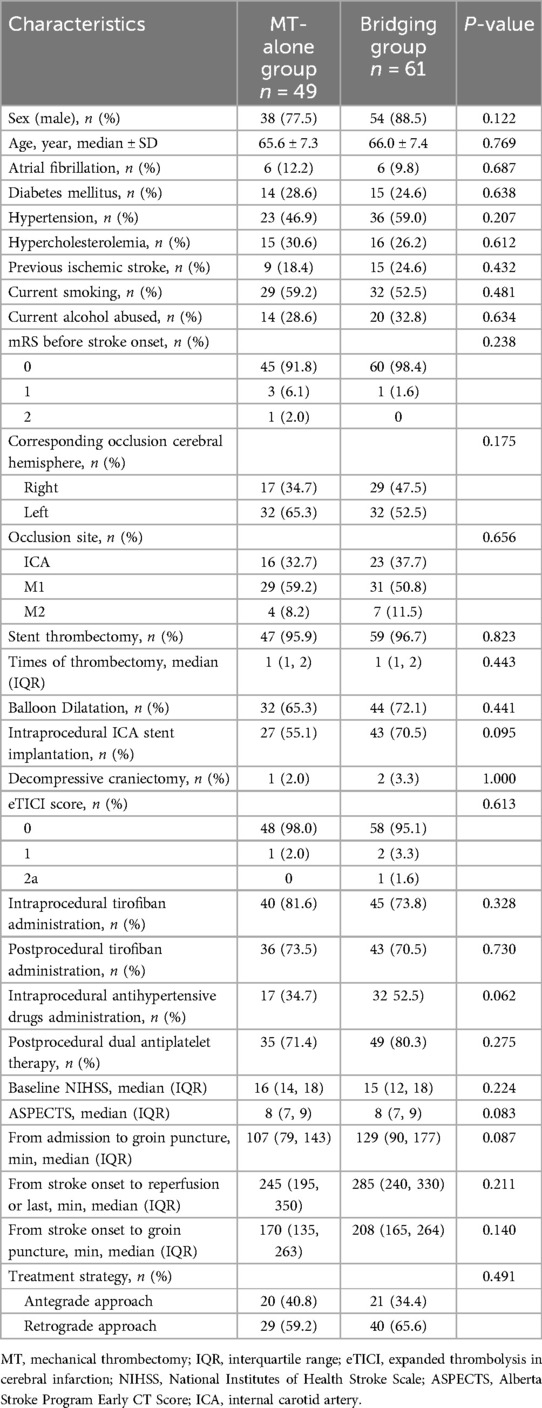
A total of 110 patients were included in the study, with 49 patients assigned to direct mechanical thrombectomy (MT-alone group) and 61 patients to intravenous alteplase followed by MT (bridging group). Key baseline characteristics were as follows: the mean age was 65.6 ± 7.3 years in the MT-alone group and 66.0 ± 7.4 years in the bridging group; baseline median NIHSS scores were 16 (IQR 14–18) and 15 (IQR 12–18), respectively; baseline median ASPECT scores were 8 (IQR 7–9) for both groups. Table 1 presents detailed baseline characteristics for both groups, with no statistically significant differences between them.
3.2 Procedure-related data
After perfusion, cervical ICA stenting was performed in 27 (55.1%) patients in the MT-alone group and 43 (70.5%) in the bridging group. The median time from admission to groin puncture was 107 min (IQR 79–143) in the MT-alone group and 129 min (IQR 90–177) in the bridging group. The median time from stroke onset to reperfusion was 245 min (IQR 195–350) for the MT-alone group and 285 min (IQR 240–330) for the bridging group. The median time from stroke onset to groin puncture was 170 min (IQR 135–263) for the MT-alone group and 208 min (IQR 165–264) for the bridging group. Tirofiban was administered intraprocedurally in 40 (81.6%) patients in the MT-alone group and in 45 (73.8%) patients in the bridging group. Post-procedure, tirofiban was administered to 36 (73.5%) patients in the MT-alone group and 43 (70.5%) patients in the bridging group. A total of 28 (57.1%) patients in the MT-alone group and 43 (70.5%) patients in the bridging group received intraprocedural ICA stent implantation. Postprocedural dual antiplatelet therapy was administered to 35 (71.4%) patients in the MT-alone group and 49 (80.3%) patients in the bridging group. Balloon dilatation was performed in 76 patients: 32 (65.3%) in the MT-alone group and 44 (72.1%) in the bridging group. In terms of thrombectomy methods, 47 (95.9%) patients in the MT-alone group and 59 (96.7%) in the bridging group received stent thrombectomy.
3.3 Primary outcomes
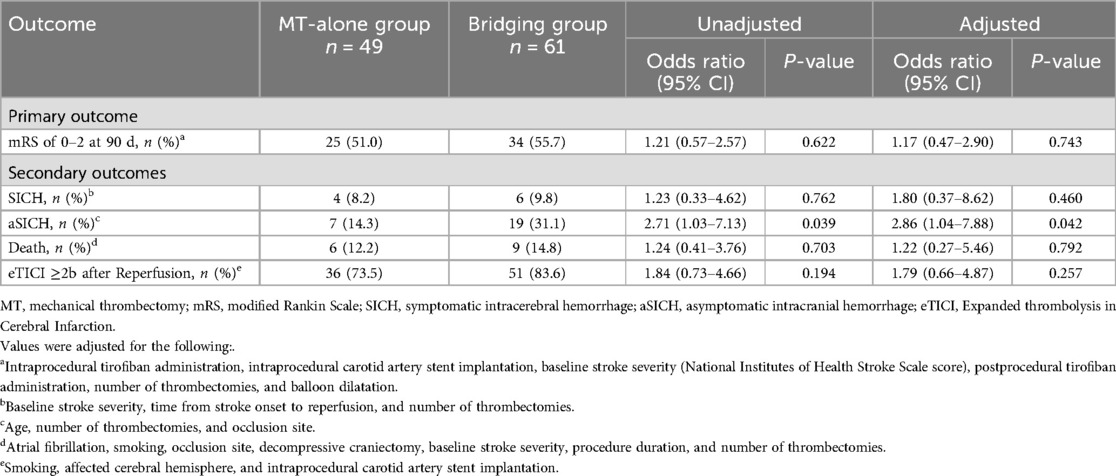
The mRS score at 90 days was comparable between the bridging and MT-alone groups (P = 0.579) (Figure 2). A favorable outcome (mRS of 0–2) at 90 days was observed in 25 (51.0%) patients in the MT-alone group and 34 (55.7%) patients in the bridging group, showing no significant difference between the groups (P = 0.622) with an unadjusted OR of 1.21 (95% CI, 0.57–2.57). Multivariate analysis found no association between prior intravenous alteplase administration and 90-day functional outcomes in patients with anterior circulation tandem occlusions after adjusting for confounding variables, yielding an aOR of 1.17 (95% CI, 0.47–2.90; adjusted P = 0.743) (Table 2).
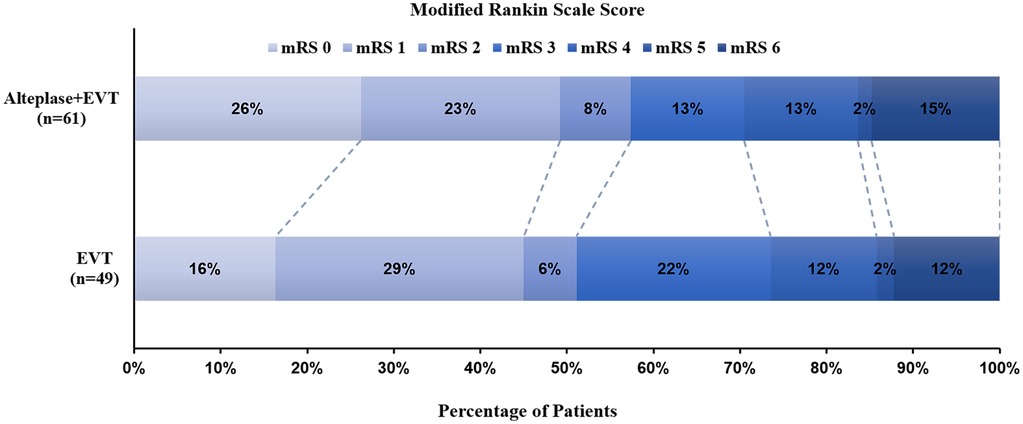
Figure 2. Distribution of modified rankin scale (mRS) scores at 90 days post-treatment. Scores range from 0 to 6, with (0) indicating no symptoms; (1) no significant disability; (2) mild disability (patient can manage self-care independently but cannot perform all previous activities); (3) moderate disability (patient requires some assistance but can walk unassisted); (4) moderately severe disability (patient cannot attend to physical needs or walk without assistance); (5) severe disability (patient requires constant care and attention); and (6) death. The mRS scores at 90 days were comparable between the MT-alone group and the bridging group (P = 0.579).
A subgroup analysis of the primary outcome was conducted using multivariate logistic regression, evaluating intra- or postprocedural tirofiban administration, intravenous alteplase administration before MT, intraprocedural stent implantation, baseline NIHSS score, time from stroke onset to reperfusion, number of thrombectomies, balloon dilation, and procedure duration. Results indicated that intraprocedural tirofiban administration (OR = 4.19, 95% CI, 1.37–12.77; P = 0.012), intraprocedural stent implantation (OR = 2.65, 95% CI, 1.05–6.70; P = 0.040), and baseline NIHSS score (OR = 0.85, 95% CI, 0.76–0.95; P = 0.005) were associated with a favorable outcome at 90 days (Figure 3).
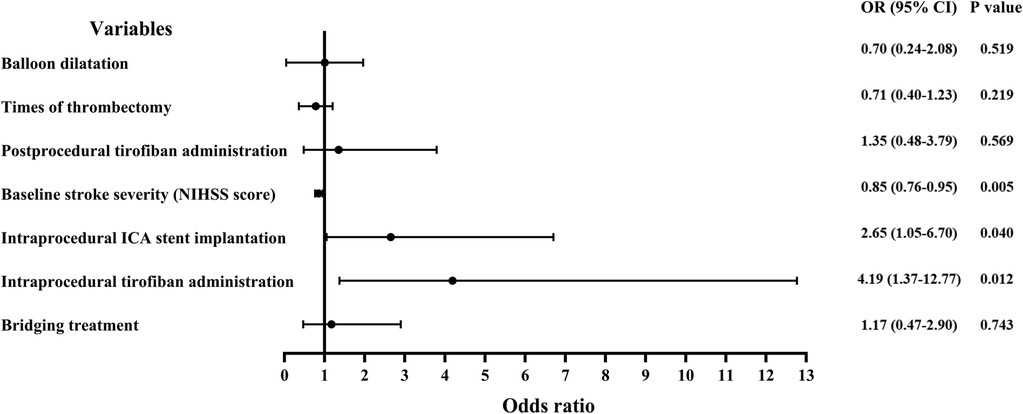
Figure 3. Forest plots demonstrating risk factors for a favorable outcome (mRS score of 0–2) at 90 days post-treatment. OR, odds ratio; ICA, internal carotid artery; NIHSS, National Institutes of Health Stroke Scale.
3.4 Secondary outcomes
The rate of aSICH was higher in the bridging group than in the MT-alone group, with an aSICH rate of 14.3% in the MT-alone group vs. 31.1% in the bridging group, resulting in an aOR of 2.86 (95% CI, 1.04–7.88; adjusted P = 0.042). The rate of SICH was similar between groups (8.9% vs. 9.8%; aOR = 1.80, 95% CI, 0.37–8.62; adjusted P = 0.460). The 90-day mortality rate was 12.2% in the MT-alone group and 14.8% in the bridging group, with no significant difference (aOR = 1.22, 95% CI, 0.27–5.46; adjusted P = 0.792). The successful recanalization rate was numerically higher in the bridging group (83.6% vs. 73.5%; aOR = 1.79, 95% CI, 0.66–4.87; adjusted P = 0.257), though this difference was not statistically significant.
4 Discussion
Our study found no evidence that prior intravenous alteplase administration before MT influenced the 90-day outcomes of patients with acute ischemic stroke due to anterior circulation tandem occlusions. However, we observed that bridging therapy was associated with an increased rate of aSICH following the procedure. Although this study did not demonstrate a significant improvement in functional outcomes, MT alone appeared to yield nominally better efficacy outcomes compared to combination therapy.
Previous studies comparing the safety and efficacy of bridging therapy vs. MT alone have reported conflicting results, creating uncertainty regarding the benefits of intravenous thrombolysis before MT (6–10). Recent RCTs, however, have provided robust evidence for the non-inferiority of MT alone compared to combined intravenous alteplase and MT (11, 13). The DIRECT-MT (Endovascular Thrombectomy with or without Intravenous Alteplase in Acute Stroke) trial (11) and the DEVT (Direct Endovascular Thrombectomy vs. Combined IVT and Endovascular Thrombectomy for Patients with Acute Large Vessel Occlusion in the Anterior Circulation) trial (13) demonstrated that MT alone was not inferior to bridging therapy in terms of 90-day neurological function outcomes. Conversely, the SKIP (Effect of Mechanical Thrombectomy Without vs. With Intravenous Thrombolysis on Functional Outcome Among Patients with Acute Ischemic Stroke) trial (12) failed to demonstrate non-inferiority regarding favorable functional outcomes in patients treated with endovascular thrombectomy with or without intravenous alteplase in acute large vessel occlusion stroke. The inconsistency among these RCTs remains unexplained, and all three trials lack specific outcome data for patients with tandem occlusion.
Tandem occlusion is a known risk factor for poor outcomes following intravenous thrombolysis (1, 5). It remains uncertain whether patients with tandem occlusion should undergo intravenous thrombolysis before endovascular treatment. Previous animal studies have shown that downstream microvascular thrombosis is common in large artery occlusion and that early administration of alteplase may improve outcomes post-recanalization by reducing fibrinogen-dependent platelet aggregation (15). Pikija et al. (16) conducted a retrospective study on patients who underwent endovascular therapy for tandem occlusion in acute ischemic stroke, finding that intravenous t-PA administration was associated with a favorable outcome at three months (OR 12.0, 95% CI 1.0–144.4). Similarly, results from Anadani et al. (17) indicated that patients who received intravenous thrombolysis before MT had higher rates of favorable outcomes and successful reperfusion. However, our study yielded conflicting results, with comparable 90-day mRS scores between the bridging and MT-alone groups. This discrepancy may stem from differences in patient selection criteria; studies that included MT alone for patients outside the time window or contraindicated for alteplase may have experienced higher unfavorable outcome rates.
In our study, the overall ICH rate was comparable to that in published trials (11–13). However, regarding secondary safety outcomes, we found that aSICH rates were significantly higher in patients who received intravenous alteplase, with 14.3% in the MT-alone group vs. 31.1% in the bridging group, while SICH rates did not significantly differ between the two groups. The SKIP trial similarly found a lower rate of any ICH in the MT-alone group compared to the combined group (12). Alteplase administration is known to increase the risk of ICH compared to placebo or open control in patients with acute ischemic stroke, potentially leading to more than a five-fold increase in hemorrhage frequency (18). This may explain the higher frequency of aSICH observed in our study. Van Kranendonk et al. (19) demonstrated that hemorrhagic transformation is associated with functional outcomes following acute ischemic stroke. Thus, both SICH and aSICH remain critical and warrant vigilance. Moreover, while the bridging group demonstrated a numerically higher rate of successful reperfusion (eTICI ≥2b) compared to the MT-alone group, this difference did not reach statistical significance (P = 0.257). Preclinical studies have established that downstream microvascular thrombosis represents a pathognomonic feature of large artery occlusion, with early alteplase administration demonstrating improved post-recanalization outcomes via fibrinogen-mediated attenuation of platelet aggregation (15). The technical complexity of endovascular thrombectomy in tandem lesions carry risks of post-recanalization re-occlusion, where pre-treatment with rt-PA thrombolysis might provide protective benefits against re-occlusion. Nevertheless, our findings provide no conclusive evidence that bridging treatment enhances post-thrombectomy favorable recanalization rates, warranting validation through larger multicenter cohorts.
We observed that intraprocedural tirofiban administration was associated with favorable 90-day outcomes. Tirofiban has been shown to be safe and effective in endovascular treatments for cerebrovascular diseases, including ruptured and unruptured aneurysms, symptomatic intracranial atherosclerotic stenosis, and acute ischemic stroke (20–23). As a glycoprotein IIb/IIIa inhibitor, tirofiban acts quickly post-administration, and platelet function can be promptly reversed after discontinuing the infusion. Tirofiban administration may prevent thrombus formation and reduce ischemic events (22). Additionally, our study indicated that intraprocedural stent implantation was linked to a higher favorable outcome rate at 90 days. Acute stent implantation for extracranial carotid stenosis is a crucial management approach for tandem lesions in acute ischemic stroke and may enhance clinical outcomes (24). The benefit of acute stent implantation may relate to improved intracranial vascular perfusion post-implantation (22, 24). Acute stent implantation for extracranial carotid stenosis can also stabilize the unstable plaques in the proximal carotid artery, preventing their detachment and subsequent thromboembolic events in distal vessels. Additionally, this approach provides a more favorable vascular pathway for endovascular treatment of distal occlusions, allowing the micro-guidewire and microcatheter to reach the distal occluded vessel under direct visualization, thereby mitigating ischemic events caused by vascular dissection and endothelial injury to some extent.
This study has several limitations. Our sample size was relatively small, resulting in wide confidence intervals when analyzing patient outcomes and reducing the statistical power. Additionally, our study was retrospective and non-randomized, with potential biases (e.g., selection bias) that are unavoidable in retrospective studies. In our study, we did not compare the possible impacts of other intravenous thrombolytic drugs on the outcomes, such as tenecteplase. The absence of comparative analysis between intravenous thrombolysis alone and endovascular therapy regarding safety and efficacy in anterior circulation tandem occlusion also represents a limitation of our study. Moreover, although we used a multivariate analysis model to adjust for primary and secondary outcomes to minimize confounding factor influence, residual confounding factors may still affect our findings. Therefore, a prospective, randomized controlled trial would be valuable.
5 Conclusion
Our findings indicated that prior intravenous alteplase administration did not impact the clinical or imaging outcomes of patients with acute ischemic stroke due to anterior circulation tandem occlusions, as reflected by similar mRS scores at 90 days. Bridging therapy, however, was associated with a higher rate of aSICH. Favorable outcomes were associated with intraprocedural tirofiban administration, stent implantation, and a lower baseline NIHSS score.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The Ethics Committee of the first affiliated hospital of Harbin medical university. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because The retrospective data collected in this study were all obtained from the medical information system, and no additional tests or examinations were required.
Author contributions
ZY: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Visualization, Writing – original draft. GZ: Conceptualization, Data curation, Formal analysis, Project administration, Writing – original draft. QW: Conceptualization, Data curation, Formal analysis, Writing – original draft. YZ: Data curation, Investigation, Project administration, Writing – original draft. SX: Conceptualization, Data curation, Methodology, Project administration, Writing – original draft. HS: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Supervision, Validation, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by National Health Commission Capacity Building and Continuing Education Center (GWJJQ2023100102), the Research and Innovation Fund of the First Affiliated Hospital of Harbin Medical University (2023M35), Young Teachers' Research Foundation Capacity Enhancement Project in Guangxi Universities (No. 2025KY0515) and Guangxi Natural Science Foundation Project (No. 2025GXNSFHA069158).
Acknowledgments
Thanks to the patients from the First Affiliated Hospital of Harbin Medical University who participated in this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Feil K, Herzberg M, Dorn F, Tiedt S, Küpper C, Thunstedt DC, et al. Tandem lesions in anterior circulation stroke. Stroke. (2021) 52(4):1265–75. doi: 10.1161/strokeaha.120.031797
2. Marko M, Cimflova P, Poppe AY, Kashani N, Singh N, Ospel J, et al. Management and outcome of patients with acute ischemic stroke and tandem carotid occlusion in the Escape-Na1 trial. J Neurointerv Surg. (2022) 14(5):429–33. doi: 10.1136/neurintsurg-2021-017474
3. Anadani M, Marnat G, Consoli A, Papanagiotou P, Nogueira RG, Siddiqui A, et al. Endovascular therapy of anterior circulation tandem occlusions. Stroke. (2021) 52(10):3097–105. doi: 10.1161/strokeaha.120.033032
4. Poppe AY, Jacquin G, Roy D, Stapf C, Derex L. Tandem carotid lesions in acute ischemic stroke: mechanisms, therapeutic challenges, and future directions. Am J Neuroradiol. (2020) 41(7):1142–8. doi: 10.3174/ajnr.A6582
5. Rubiera M, Ribo M, Delgado-Mederos R, Santamarina E, Delgado P, Montaner J, et al. Tandem internal carotid artery/middle cerebral artery occlusion. Stroke. (2006) 37(9):2301–5. doi: 10.1161/01.STR.0000237070.80133.1d
6. Gariel F, Lapergue B, Bourcier R, Berge J, Barreau X, Mazighi M, et al. Mechanical thrombectomy outcomes with or without intravenous thrombolysis. Stroke. (2018) 49(10):2383–90. doi: 10.1161/strokeaha.118.021500
7. Mistry EA, Mistry AM, Nakawah MO, Chitale RV, James RF, Volpi JJ, et al. Mechanical thrombectomy outcomes with and without intravenous thrombolysis in stroke patients. Stroke. (2017) 48(9):2450–6. doi: 10.1161/strokeaha.117.017320
8. Fischer U, Kaesmacher J, Mendes Pereira V, Chapot R, Siddiqui AH, Froehler MT, et al. Direct mechanical thrombectomy versus combined intravenous and mechanical thrombectomy in large-artery anterior circulation stroke. Stroke. (2017) 48(10):2912–8. doi: 10.1161/strokeaha.117.017208
9. Broeg-Morvay A, Mordasini P, Bernasconi C, Bühlmann M, Pult F, Arnold M, et al. Direct mechanical intervention versus combined intravenous and mechanical intervention in large artery anterior circulation stroke. Stroke. (2016) 47(4):1037–44. doi: 10.1161/strokeaha.115.011134
10. Weber R, Nordmeyer H, Hadisurya J, Heddier M, Stauder M, Stracke P, et al. Comparison of outcome and interventional complication rate in patients with acute stroke treated with mechanical thrombectomy with and without bridging thrombolysis. J Neurointerv Surg. (2017) 9(3):229–33. doi: 10.1136/neurintsurg-2015-012236
11. Yang P, Zhang Y, Zhang L, Zhang Y, Treurniet KM, Chen W, et al. Endovascular thrombectomy with or without intravenous alteplase in acute stroke. N Engl J Med. (2020) 382(21):1981–93. doi: 10.1056/NEJMoa2001123
12. Suzuki K, Matsumaru Y, Takeuchi M, Morimoto M, Kanazawa R, Takayama Y, et al. Effect of mechanical thrombectomy without vs with intravenous thrombolysis on functional outcome among patients with acute ischemic stroke. JAMA. (2021) 325(3):244–53. doi: 10.1001/jama.2020.23522
13. Zi W, Qiu Z, Li F, Sang H, Wu D, Luo W, et al. Effect of endovascular treatment alone vs intravenous alteplase plus endovascular treatment on functional independence in patients with acute ischemic stroke. JAMA. (2021) 325(3):234–43. doi: 10.1001/jama.2020.23523
14. von Kummer R, Broderick JP, Campbell BCV, Demchuk A, Goyal M, Hill MD, et al. The Heidelberg bleeding classification. Stroke. (2015) 46(10):2981–6. doi: 10.1161/strokeaha.115.010049
15. Desilles J-P, Loyau S, Syvannarath V, Gonzalez-Valcarcel J, Cantier M, Louedec L, et al. Alteplase reduces downstream microvascular thrombosis and improves the benefit of large artery recanalization in Stroke. Stroke. (2015) 46(11):3241–8. doi: 10.1161/strokeaha.115.010721
16. Pikija S, Magdic J, Sztriha LK, Killer-Oberpfalzer M, Bubel N, Lukic A, et al. Endovascular therapy for tandem occlusion in acute ischemic stroke: intravenous thrombolysis improves outcomes. J Clin Med. (2019) 8(2):228. doi: 10.3390/jcm8020228
17. Anadani M, Marnat G, Consoli A, Papanagiotou P, Nogueira RG, Spiotta AM, et al. Endovascular therapy with or without intravenous thrombolysis in acute stroke with tandem occlusion. J Neurointerv Surg. (2022) 14(4):314–20. doi: 10.1136/neurintsurg-2020-017202
18. Hacke W, Donnan G, Fieschi C, Kaste M, von Kummer R, Broderick JP, et al. Association of outcome with early stroke treatment: pooled analysis of Atlantis, ecass, and ninds rt-pa stroke trials. Lancet. (2004) 363(9411):768–74. doi: 10.1016/s0140-6736(04)15692-4
19. van Kranendonk KR, Treurniet KM, Boers AMM, Berkhemer OA, van den Berg LA, Chalos V, et al. Hemorrhagic transformation is associated with poor functional outcome in patients with acute ischemic stroke due to a large vessel occlusion. J Neurointerv Surg. (2019) 11(5):464–8. doi: 10.1136/neurintsurg-2018-014141
20. Yan Y, He X, Fang Y, Xu Y, Hong B, Liu J, et al. The safety and efficacy of low-dosage tirofiban for stent-assisted coiling of ruptured intracranial aneurysms. Neurosurg Rev. (2020) 44(4):2211–8. doi: 10.1007/s10143-020-01398-w
21. Wu Q, Shao Q, Li L, Liang X, Chang K, Li T, et al. Prophylactic administration of tirofiban for preventing thromboembolic events in flow diversion treatment of intracranial aneurysms. J Neurointerv Surg. (2021) 13(9):835–40. doi: 10.1136/neurintsurg-2020-016878
22. Garayzade R, Berlis A, Schiele S, Ertl M, Schneider H, Müller G, et al. Efficacy and safety outcomes for acute ischemic stroke patients treated with intravenous infusion of tirofiban after emergent carotid artery stenting. Clin Neuroradiol. (2024) 34(1):163–72. doi: 10.1007/s00062-023-01350-7
23. Zhang J, Huang X, Wang G, Wang X, Zhang T, Wang D, et al.Efficacy and safety of tirofiban before stenting for symptomatic intracranial atherosclerotic stenosis: a randomized clinical trial. Neurology. (2024) 102(7):e209217. doi: 10.1212/WNL.0000000000209217
Keywords: direct mechanical thrombectomy, acute ischemic stroke, intravenous alteplase, anterior circulation, tandem occlusion
Citation: Yang Z, Zhang G, Wu Q, Zhu Y, Xu S and Shi H (2025) Direct mechanical thrombectomy vs. intravenous alteplase plus mechanical thrombectomy in acute ischemic stroke with anterior circulation tandem occlusions. Front. Surg. 12:1536912. doi: 10.3389/fsurg.2025.1536912
Received: 29 November 2024; Accepted: 7 April 2025;
Published: 22 April 2025.
Edited by:
Xuesong Bai, Capital Medical University, ChinaReviewed by:
Rick Gill, Loyola University Chicago, United StatesAleksandras Vilionskis, Vilnius University, Lithuania
Copyright: © 2025 Yang, Zhang, Wu, Zhu, Xu and Shi. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huaizhang Shi, aHVhaXpoYW5nc2hpQDE2My5jb20=
†These authors have contributed equally to this work
 Zhonghui Yang
Zhonghui Yang Guang Zhang
Guang Zhang Qiaowei Wu
Qiaowei Wu Yujing Zhu
Yujing Zhu Shancai Xu
Shancai Xu Huaizhang Shi
Huaizhang Shi