- Department of General Surgery, Sir Run-Run Shaw Hospital, Zhejiang University, Hangzhou, Zhejiang, China
Objectives: The combined technology of laparoscopy, choledochoscope and gastroscope was used in the treatment of gallbladder stones combined with common bile duct stones, which consists of laparoscopic cholecystectomy (LC), laparoscopic common bile duct exploration with primary closure (LCBDE-PC) and combined gastroscopic and choledochoscopic transabdominal nasobiliary drainage (GC-NBD). The clinical effects of the combined technology were evaluated based on hospital stay, hospital costs, postoperative complications, recurrence of stones, and overall patient satisfaction.
Methods: From July 2017 to December 2020, 206 patients with gallbladder stones combined with common bile duct stones were reviewed retrospectively. According to the surgical method, the patients were divided into Triple-Scope group (LC + LCBDE-PC + GC-NBD), (n = 38), ERCP + LC group [endoscopic retrograde cholangiopancreatography (ERCP) followed by LC], (n = 96) and T tube group (LC + LCBDE + T tube drainage), (n = 72). The differences in stone size, hospital stay, hospital cost, postoperative gallstone recurrence rate and postoperative complications were compared among three groups.
Results: No postoperative bile leak occurred in Triple-Scope group, and patients were discharged successfully, and the abdominal drain was removed around 3 days after surgery, and the nasobiliary drainage was removed around 5 days after surgery with a hospital stay of 9.5 ± 2.65 days. The length of hospital stay and hospital cost in the Triple-Scope group were lower than those in the ERCP + LC group (P < 0.01), but not significantly different from those in the T tube group (P > 0.05). The diameter of common bile duct and stone size were significantly larger in the Triple-Scope group and T-tube group than in the ERCP + LC group (P = 0.001; P = 0.004), and the recurrence rate of stones in the Triple-Scope group was not significantly different compared with those in the other two groups (P = 0.43).
Conclusions: For patients with gallbladder stones combined with common bile duct stones, the triple-scope combination is safe and effective with fast recovery, and it is worthy of clinical promotion and application.
Introduction
Gallstones are a common biliary tract disease with an incidence of about 10%, of which 3%–16% may present with concomitant common bile duct (CBD) stones (1–3). In patients with gallbladder stones combined with common bile duct stones, the main surgical options are laparoscopic cholecystectomy combined with laparoscopic common bile duct exploration (LC + LCBDE) or preoperative endoscopic retrograde cholangiopancreatography for removal of common bile duct stones followed by laparoscopic cholecystectomy (ERCP + LC) (4), with both having their own edge (5). It has been shown that with the development of laparoscopic techniques, LC + LCBDE has a smaller stone recurrence rate and less treatment cost than ERCP + LC for patients with gallbladder stones combined with common bile duct stones (1). However, the risk of bile leakage after LCBDE with primary closure (LCBDE-PC) can be as high as 10% even when performed by a skilled surgeon (6). In order to avoid the occurrence of bile leakage, a T-tube is often placed in the common bile duct for drainage, and the T-tube usually needs to be placed for more than 1 month (7, 8), which has a greater impact on the patients' quality of life. Therefore, the search for an innovative minimally invasive procedure based on the LC + LCBDE procedure to reduce or even avoid the occurrence of bile leaks and to make the placement of T-tubes unnecessary for patients has become a common goal pursued by surgeons and patients.
To address the risk of bile leakage after LC + LCBDE-PC, we used an intraoperative protocol of intraoperative nasobiliary drainage placement with a gastroscope combined with a choledochoscope (GC-NBD), which effectively reduced the risk of bile leakage after LC + LCBDE-PC. In this study, we retrospectively analyzed the medical records of 206 patients with gallbladder stones combined with bile duct stones from our hospital between July 2017 and December 2020. We summarized the experience of triple-scope combination (LC + LCBDE-PC + GC-NBD) for gallbladder stones combined with bile duct stones, and compared the outcomes of patients treated with triple-scope combination with those of patients treated with ERCP + LC surgical protocol and LC + LCBDE + T-tube drainage surgical protocol, respectively.
Materials and methods
Study population
We retrospectively analyzed the medical records of patients admitted to Sir Run-Run Shaw Hospital, Zhejiang University from July 2017 to December 2020. Patients were included if they met the following criteria. (1) Age >18 years with a confirmed diagnosis of gallbladder stones combined with common bile duct stones based on preoperative ultrasound or MRCP. (2) Common bile duct diameter ≥10 mm as measured by imaging. (3) No history of malignant tumors of the biliary tract or pancreas. (4) No contraindications to laparoscopy, such as severe cardiopulmonary disease or extensive abdominal adhesions.
Exclusion criteria were as follows: (1) MRCP or ultrasound report containing intrahepatic bile duct stones; (2) The preoperative common bile duct diameter was diagnosed by imaging data to be less than 10 mm; (3) History of malignant tumors of the biliary tract and pancreas; (4) Pregnancy.
Patients were divided into ERCP + LC group, T-tube group and Triple-Scope group according to the surgical procedure. In the ERCP + LC group, ERCP was performed first to remove common bile duct stones, followed by LC during the same hospital admission. The two procedures were typically performed within 24–48 h of each other, depending on the patient's condition and surgical schedule. Patients in the T-tube group underwent LC combined with LCBDE and T tube drainage surgical protocol. Patients in the Triple-Scope group underwent LC, LCBDE-PC and GC-NBD surgical protocol.
Patient data collection
Clinical data were collected from patients including gender, age, imaging data [diameter of common bile duct (cm), maximum diameter of stones (cm), number of stones], preoperative test results (total bilirubin, direct bilirubin, γ-glutamyl transpeptidase, and leukocyte count), surgical procedure, length of stay (days), hospital costs, postoperative complications, and patient satisfaction.
Triple-scope surgical protocol (LC + LCBDE-PC + GC-NBD)
The patient was placed in the supine position after a preoperative fast of 6–8 h. After general anesthesia, the position was adjusted to a head-high to foot-low position of approximately 15°, with the whole body rotated from right to left by approximately 10°, and a sterile towel was laid down. A pneumoperitoneum with a pressure of 12 mmHg was established by making an incision of approximately 10 mm at the infraumbilical margin.
After removal of the gallbladder, a 10-mm longitudinal incision was made in the lower part of the common bile duct, through which a fiberoptic choledochoscope was placed to remove the stones from the common bile duct through a lithotripter basket, or in the case of larger stones, by crushing them with a grasper. After stone extraction, the choledochoscope was reinserted to confirm the patency of the common bile duct and to check that no stones were remained in common bile ducts. A zebra wire was inserted into the common bile duct through an incision below the glabella and through the duodenal papilla to the duodenum. The gastroscope was inserted as usual, and the guide wire was grasped with biopsy forceps and dragged out of the body through the patients' mouth under the gastroscope, through which the nasal bile duct was pushed into the common bile duct. Notably, the nasobiliary drainage tip should be placed more than 1 cm above the common bile duct incision to prevent postoperative bile leakage. The guidewire was removed and the nasobiliary duct was secured beside the patients' ear after confirming its patency by drawing it out of the patients' nasal cavity. The common bile duct was later closed with a full-layer interrupted suture of 4–0 Ethicon absorbable thread with a stitch spacing of 0.3–0.5 cm and a margin of 0.2 cm. Then saline can be injected through the nasobiliary duct or nasocholedochography can be performed to confirm whether the biliary incision was tight. After confirming that the repaired common bile duct was tightly closed, an abdominal drainage tube was placed near the repaired common bile duct and the abdomen was routinely closed.
The nasobiliary tube used in the Triple-Scope procedure had an external diameter of 7 Fr and a length of 150 cm. The tube was placed with its tip positioned at least 1 cm above the common bile duct incision to ensure effective drainage and reduce the risk of bile leakage.
After primary closure of the common bile duct, a saline solution was gently infused through the nasobiliary tube under low pressure. The absence of fluid extravasation at the suture site confirmed the integrity of the closure. If leakage was detected, additional sutures were placed to ensure a watertight closure. This method provided a simple and effective way to verify the adequacy of the repair before completing the surgery.
ERCP + LC protocol
In the ERCP + LC group, patients first underwent ERCP for the removal of common bile duct stones. ERCP was performed under sedation, and a sphincterotomy was typically performed to facilitate stone extraction using a basket or balloon catheter. After successful stone removal, patients underwent LC during the same hospital admission, usually within 24–48 h. This two-stage approach avoids the need for T-tube placement but may be associated with complications such as pancreatitis, cholangitis, or sphincter of Oddi dysfunction (9).
T-tube protocol
In the T-tube group, patients underwent LC combined with LCBDE. After stone extraction, a T-tube was placed in the common bile duct for external drainage. The T-tube was typically left in place for 4–6 weeks postoperatively to ensure adequate biliary decompression and to allow for postoperative cholangiography to confirm the absence of residual stones. Although effective, T-tube drainage is associated with patient discomfort, electrolyte imbalances, and the risk of retrograde infections (10).
Definitions of complications and recurrent stone
Biliary leakage
Defined as the presence of bilirubin-rich fluid in the abdominal drain or imaging evidence of fluid collection with confirmed bile content. Severity is classified as follows. Mild: Asymptomatic, managed conservatively. Moderate: Requires endoscopic or percutaneous intervention. Severe: Necessitates surgical re-intervention or leads to life-threatening complications.
Pancreatitis
Defined as inflammation of the pancreas, diagnosed based on clinical symptoms (e.g., abdominal pain), elevated serum amylase or lipase levels (≥3 times the upper limit of normal), and imaging findings. Severity is graded according to the revised Atlanta classification.
Cholangitis
Defined as an infection of the biliary tract, typically presenting with Charcot's triad (fever, jaundice, and right upper quadrant pain) or Reynolds' pentad (Charcot's triad plus hypotension and altered mental status). Severity is classified based on the Tokyo Guidelines.
Wound infection
Defined as the presence of purulent discharge, erythema, warmth, or tenderness at the surgical site, with or without positive microbiological culture. Severity is categorized as superficial, deep, or organ/space infection.
Recurrent stone
Defined as the reappearance of biliary stones in the gallbladder, bile ducts, or intrahepatic ducts after a confirmed complete clearance, as evidenced by imaging studies (e.g., ultrasound, CT, or MRCP).
Follow-up
All patients were followed up at 1 year postoperatively through telephone interviews, outpatient reviews, and imaging studies (e.g., ultrasound or MRCP), and all patients were followed up until September 2021. The immediate follow-up period (within 30 days postoperatively) focused on detecting early complications such as bile leakage, wound infection, or pancreatitis. Late follow-up (up to 1 year) aimed to identify stone recurrence or biliary stricture. Bile leakage: Detected by abdominal drain output analysis or imaging studies (e.g., CT or ultrasound). Stone recurrence: Confirmed by imaging studies showing new stones in the biliary tract. Other complications: Diagnosed based on clinical symptoms, laboratory tests, and imaging findings.
Statistical analysis
All data were analyzed by SPSS Version 18.0. Age and gender data, preoperative biochemical indexes, common bile duct diameter, number of stones, stone size, length of hospital stay, hospital costs, postoperative complication rate, and patient satisfaction were counted for both groups. The measurement data were described as mean ± standard deviation, and the differences among groups were analyzed by one-way ANOVA. The between-group differences of the count data were tested by chi-square test. Differences among groups were considered statistically significant if P < 0.05.
Results
Pre-operative patient information
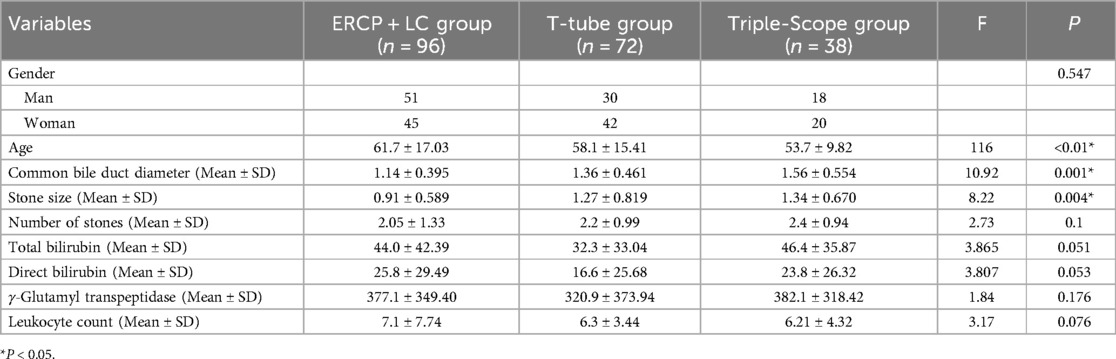
According to the treatment modality, patients who met the enrollment criteria were divided into 3 groups, including 96 patients in the ERCP + LC group, 72 patients in the T-tube group, and 38 patients in the Triple-Scope group, and the baseline characteristics of the included patients were shown in Table 1. There was no significant difference in gender between the Triple-Scope group and the ERCP + LC group (P = 0.547), and the age was younger than that of the ERCP + LC group (P < 0.01). The diameter of common bile duct and stone size were significantly larger in the Triple-Scope group and T-tube group than in the ERCP + LC group (P = 0.001; P = 0.004), and there was no significant difference in the number of stones compared with the ERCP + LC group (P = 0.1). There were no significant differences in total bilirubin, direct bilirubin, γ-glutamyl transpeptidase and leukocyte count in the Triple-Scope group compared with patients in the ERCP + LC group (All P > 0.05).
Treatment results
All patients in the Triple-Scope group successfully completed the expected operation without any reversion to open surgery and no change of T-tube drainage, and the operation time was 130–210 min, with an average of 162.8 ± 78.32 min; the bleeding volume was 5–50 ml, with an average of 38.5 ± 30.62 ml; all patients were discharged without any bile leakage. All patients had their abdominal drains removed 3–5 days after surgery, and their nasobiliary ducts were removed 5–8 days postoperatively. Before removal of the nasobiliary ducts, nasobiliary angiography was performed to confirm that no stones remained and that the contrast agent entered the duodenum successfully.
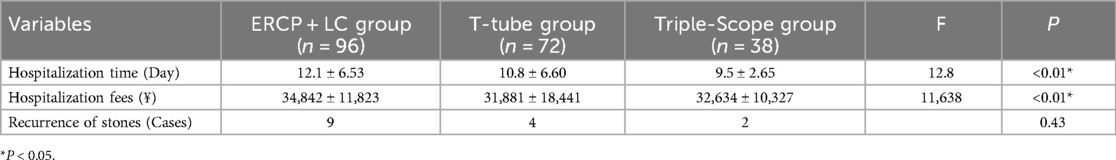
The treatment results of the three groups were shown in Table 2. The length of stay and hospital costs were significantly less in the Triple-Scope group than in the ERCP + LC group (9.5 ± 2.65 days vs. 12.1 ± 6.53 days, P < 0.01; 32,634 ± 10,327 RMB vs. 34,842 ± 11,823 RMB, P < 0.01), and there was no significant difference compared with the T-tube group; the recurrence rate of stones in the Triple-Scope group was not significantly different compared with those in the other two groups (P = 0.43).
Postoperative complications
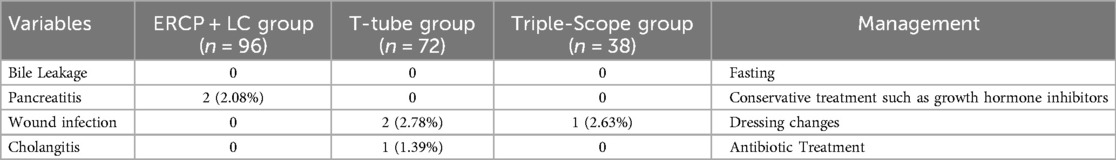
The postoperative complications in the three groups were shown in Table 3. There was no postoperative death in any of the three groups. 2 cases (2.08%) of postoperative pancreatitis occurred in the ERCP + LC group, and the symptoms resolved after 2 weeks of treatment with conservative therapy such as octreotide. In the T-tube group, 2 cases (2.78%) of wound infection and 1 case (1.39%) of biliary duct infection were observed, which were resolved after 1–2 weeks of regular dressing changes and corresponding antibiotic treatment. One case (2.63%) of wound infection occurred in the Triple-Scope group, and the wound was healed after 1 week after regular dressing changes were given.
Satisfaction survey
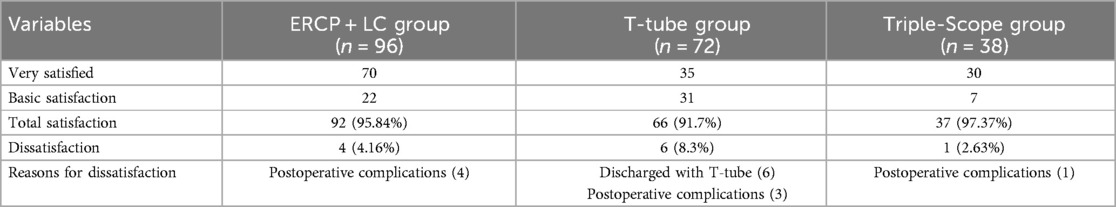
We conducted a satisfaction survey during the postoperative follow-up. Very satisfied and basic satisfaction were defined as total satisfaction. As shown in Table 4, the total satisfaction in the Triple-Scope group and the ERCP + LC group was similar, with individual patients giving unsatisfactory ratings due to the occurrence of postoperative complications, but the T-tube group had the lowest total satisfaction, with three of the unsatisfied patients having reasons related to complications, and the remaining three patients were dissatisfied because postoperative discharge with a T-tube caused some inconvenience to their lives, and it was hoped that improvements could be made.
Discussion
In 1941, Smyth (11) first reported the use of common bile duct exploration for stone extraction and T-tube drainage for the treatment of common bile duct stones. With the advent of laparoscopic techniques, LCBDE has become the mainstream for the treatment of intra- and extrahepatic common bile duct stones. In 1991, LCBDE was first reported in patients with common bile duct stones (12).With the widespread use of LCBDE, postoperative complications due to unskilled operation have gradually decreased (13). Cai et al. (1) showed that compared to ERCP + LC procedure for gallbladder stones combined with common bile duct stones, LC + LCBDE had better treatment results with lower stone recurrence rate, lower hospital cost, and lower length of stay. However, after surgical treatment of LC + LCBDE, patients often need to be discharged with a T-tube, which not only seriously affects their quality of life, but also predisposes them to complications such as water-electrolyte disturbances, massive bile loss, and retrograde infections (10).
ERCP is widely used in the treatment of common bile duct stones (14–17), and the stones in the common bile duct can be removed in advance after preoperative ERCP extraction, and only LC removal of the gallbladder is required for the second-stage surgery. ERCP + LC can avoid the inconvenience of postoperative T-tube placement and the discomfort of skin pruritus caused by T-tube. However, loss of sphincter function after ERCP + LC is often caused by disruption of the integrity of the Oddi's sphincter, which can lead to duodenal reflux, and postoperative complications such as cholangitis or even pancreatitis may also occur (9, 18–20). Moreover, the stones removal rate of ECRP often depends on the proficiency of the endoscopists, and requires the endoscopists' extensive experience in dealing with a variety of complex biliary physiological variants, which often results in complications such as stone remnants for the inexperienced endoscopist.
In contrast to ERCP + LC, the Triple-Scope procedure, which requires a higher level of experience in ERCP operation, uses a choledochoscope that allows stone visualization and other conditions for stone extraction. Meanwhile, the placement of a nasobiliary tube under the gastroscope is simple and convenient compared to the complexity of ERCP. The nasobiliary ducts can be used not only for intraoperative leak detection of the common bile duct suture opening, but also for postoperative drainage and pressure reduction to avoid bile leakage caused by excessive pressure in the common bile duct.
Our findings align with previous studies demonstrating the superiority of LCBDE over ERCP + LC in terms of stone recurrence rates, hospital costs, and length of stay (21). However, the triple-scope technique further improves upon traditional LCBDE by eliminating the need for T-tube drainage, thereby enhancing patient comfort and quality of life. The shorter hospital stay and lower costs observed in the Triple-Scope group compared to the ERCP + LC group underscore the economic and clinical benefits of this approach.
Notably, the triple-scope technique appears to be particularly suitable for patients with larger common bile duct stones or more complex biliary anatomy, as evidenced by the significantly larger stone size and bile duct diameter in the Triple-Scope and T-tube groups. This suggests that the technique may fill an important niche in the management of challenging cases where ERCP may be less effective.
In order to avoid the inconvenience of T-tube drainage, some surgeons have tried LC + LCBDE-PC procedure, but the high incidence of postoperative bile leakage is inevitable. Liu et al. (18) found that the overall incidence of bile leak was 11.3% in 141 patients with common bile duct stones treated with LC + LCBDE-PC procedure, with a significantly higher incidence of 31.6% in patients with common bile duct diameters <1 cm. This showed that the major disadvantage of the LC + LCBDE-PC procedure was the high incidence of bile leakage, which was one of the key factors affecting the success of this procedure.
Compared with LC + LCBDE-PC, the placement of nasobiliary duct in the Triple-Scope procedure not only eliminates the inconvenience of carrying a T-tube after the first-stage bile duct suture, but also improves the safety of the first-stage bile duct suture by avoiding the bile leakage caused by excessive pressure in the bile duct after the suture, which brings a more comfortable and reliable treatment experience for patients. Compared to single-stage laparoscopic cholecystectomy with intraoperative ERCP (LC + IO-ERCP), the Triple-Scope technique offers distinct advantages in managing complex CBD stones. While LC + IO-ERCP avoids nasobiliary drainage, its efficacy heavily depends on endoscopists' expertise and real-time coordination between surgical and endoscopic teams (22). The Triple-Scope approach should be considered due to its direct visualization of stones via choledochoscopy, which is particularly advantageous for large or multiple stones (23).
In this study, we also counted the data of postoperative complications in the three groups of patients. All three groups had individual complications postoperatively, including pancreatitis, wound infection, and cholangitis, with the least postoperative complications (one wound infection) in the Triple-Scope group, which may be related to the smaller number of patients enrolled in the Triple-Scope group. The present study had some limitations with a small sample number, and a large sample is needed for confirmation in the future.
Despite its promising results, this study has several limitations that warrant consideration. First, the retrospective design introduces the potential for selection bias, and the relatively small sample size of the Triple-Scope group limits the generalizability of the findings. Second, the follow-up period may not be sufficient to fully assess long-term outcomes, such as stone recurrence or biliary stricture. Future prospective, randomized controlled trials with larger sample sizes and extended follow-up periods are needed to validate these findings and further refine the indications for the triple-scope technique.
Additionally, future research could explore the integration of advanced imaging modalities, such as intraoperative cholangiography or real-time ultrasound, to enhance the precision of stone clearance and reduce the risk of residual stones. The development of standardized protocols for nasobiliary tube placement and postoperative management could further optimize outcomes and facilitate the broader adoption of this technique.
In conclusion, this retrospective study showed that triple-scope procedure has the advantage of shorter hospital stay and reduced hospital costs compared with ERCP + LC. The triple-scope procedure provided a higher quality of life and treatment experience for patients compared with LC + LCBDE + T-tube drainage procedure. For patients with gallbladder stones combined with common bile duct stones, the triple-scope procedure has the advantages of convenience, safety and comfort, and is a recommended procedure in clinical practice.
Data availability statement
The datasets presented in this study can be found in online repositories. The names of the repository/repositories and accession number(s) can be found below: The data can be uploaded upon reasonable request to corresponding author.
Ethics statement
The studies involving humans were approved by Sir Run-Run Shaw Hospital, Zhejiang University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
HF: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Software, Writing – original draft. WC: Conceptualization, Data curation, Writing – original draft. ZW: Formal analysis, Investigation, Methodology, Software, Writing – original draft. GD: Conceptualization, Data curation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
We are grateful to our colleagues for their assistance in checking the data of the study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
LC, laparoscopic cholecystectomy; LCBDE-PC, laparoscopic common bile duct exploration with primary closure; GC-NBD, combined gastroscopic and choledochoscopic transabdominal nasobiliary drainage; ERCP, Endoscopic retrograde cholangiopancreatography; CBD, Common bile duct.
References
1. Pan L, Chen M, Ji L, Zheng L, Yan P, Fang J, et al. The safety and efficacy of laparoscopic common bile duct exploration combined with cholecystectomy for the management of cholecysto-choledocholithiasis: an up-to-date meta-analysis. Ann Surg. (2018) 268(2):247–53. doi: 10.1097/sla.0000000000002731
2. Dasari BV, Tan CJ, Gurusamy KS, Martin DJ, Kirk G, McKie L, et al. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. (2013) 2013(12):Cd00332718. doi: 10.1002/14651858.CD003327.pub4
3. Pavlidis ET, Pavlidis TE. Current management of concomitant cholelithiasis and common bile duct stones. World J Gastrointest Surg. (2023) 15(2):169–76. doi: 10.4240/wjgs.v15.i2.169
4. Lyu Y, Cheng Y, Li T, Cheng B, Jin X. Laparoscopic common bile duct exploration plus cholecystectomy versus endoscopic retrograde cholangiopancreatography plus laparoscopic cholecystectomy for cholecystocholedocholithiasis: a meta-analysis. Surg Endosc. (2019) 33(10):3275–86. doi: 10.1007/s00464-018-06613-w
5. Zhu J, Li G, Du P, Zhou X, Xiao W, Li Y. Laparoscopic common bile duct exploration versus intraoperative endoscopic retrograde cholangiopancreatography in patients with gallbladder and common bile duct stones: a meta-analysis. Surg Endosc. (2021) 35(3):997–1005. doi: 10.1007/s00464-020-08052-y
6. Kemp Bohan PM, Connelly CR, Crawford J, Bronson NW, Schreiber MA, Lucius CW, et al. Early analysis of laparoscopic common bile duct exploration simulation. Am J Surg. (2017) 213(5):888–94. doi: 10.1016/j.amjsurg.2017.03.011
7. Zhang HW, Chen YJ, Wu CH, Li WD. Laparoscopic common bile duct exploration with primary closure for management of choledocholithiasis: a retrospective analysis and comparison with conventional T-tube drainage. Am Surg. (2014) 80(2):178–81. doi: 10.1177/000313481408000227
8. McNamee MM, Stolz MP, Harvell RT, Staley CA, Green EE, Othman HD, et al. Management of choledocholithiasis in a community hospital: laparoscopic common bile duct exploration versus endoscopic retrograde cholangiopancreatography. Am Surg. (2024) 90(8):2011–3. doi: 10.1177/00031348241241626
9. Wang P, Li ZS, Liu F, Ren X, Lu NH, Fan ZN, et al. Risk factors for ERCP-related complications: a prospective multicenter study. Am J Gastroenterol. (2009) 104(1):31–40. doi: 10.1038/ajg.2008.5
10. Wills VL, Gibson K, Karihaloot C, Jorgensen JO. Complications of biliary T-tubes after choledochotomy. ANZ J Surg. (2002) 72(3):177–80. doi: 10.1046/j.1445-2197.2002.02308.x
11. Smyth MJ. Exploration of the common bile duct for stone. Drainage with T-tube and cholangiography. Br Med J. (1941) 1(4177):111–26.4. doi: 10.1136/bmj.1.4177.111
12. Bagnato J. Laparoscopic common bile duct exploration. J Miss State Med Assoc. (1990) 31(11):361–2.2148604
13. Lin Y, Su Y, Yan J, Li X. Laparoendoscopic rendezvous versus ERCP followed by laparoscopic cholecystectomy in the management of cholecystocholedocholithiasis: a systemic review and meta-analysis. Surg Endosc. (2020) 34(9):4214–24. doi: 10.1007/s00464-020-07698-y
14. Sagami R, Hayasaka K, Ujihara T, Iwaki T, Katsuyama Y, Harada H, et al. Accurate evaluation of residual common bile duct stones by endoscopic ultrasound: a two-step check method for residual stone clearance. Digestion. (2022) 103(3):224–31. doi: 10.1159/000521925
15. AbiMansour JP, Martin JA. Biliary endoscopic retrograde cholangiopancreatography. Gastroenterol Clin North Am. (2024) 53(4):627–42. doi: 10.1016/j.gtc.2024.08.011
16. Li X, Ouyang J, Dai J. Current gallstone treatment methods, state of the art. Diseases. (2024) 12(9):197. doi: 10.3390/diseases12090197
17. Raab S, Jagoditsch A, Kurz F, Pimingstorfer P, Schimetta W, Schöfl R, et al. Comparison of intraoperative versus preoperative ERCP with laparoscopic cholecystectomy for cholecystocholedocholithiasis: a 3-year study at Kepler university hospital. Surg Endosc. (2025) 39(2):1036–42. doi: 10.1007/s00464-024-11438-x
18. Cennamo V, Fuccio L, Zagari RM, Eusebi LH, Ceroni L, Laterza L, et al. Can early precut implementation reduce endoscopic retrograde cholangiopancreatography-related complication risk? Meta-analysis of randomized controlled trials. Endoscopy. (2010) 42(5):381–8. doi: 10.1055/s-0029-1243992
19. Lee KJ, Cho E, Park DH, Cha HW, Koh DH, Lee J, et al. Identification of risk factors associated with post-ERCP pancreatitis in patients with easy cannulation: a prospective multicenter observational study. Gastrointest Endosc. (2024):S0016-5107(24)03728-3. doi: 10.1016/j.gie.2024.11.018
20. Bishay K, Meng ZW, Khan R, Gupta M, Ruan Y, Vaska M, et al. Adverse events associated with endoscopic retrograde cholangiopancreatography: systematic review and meta-analysis. Gastroenterology. (2024) 168(3):568–86. doi: 10.1053/j.gastro.2024.10.033
21. Ricci C, Pagano N, Taffurelli G, Pacilio CA, Migliori M, Bazzoli F, et al. Comparison of efficacy and safety of 4 combinations of laparoscopic and intraoperative techniques for management of gallstone disease with biliary duct calculi: a systematic review and network meta-analysis. JAMA Surg. (2018) 153(7):e181167. doi: 10.1001/jamasurg.2018.1167
22. Zhang D, Dai Z, Sun Y, Sun G, Luo H, Guo X, et al. One-stage intraoperative ERCP combined with laparoscopic cholecystectomy versus two-stage preoperative ERCP followed by laparoscopic cholecystectomy in the management of gallbladder with common bile duct stones: a meta-analysis. Adv Ther. (2024) 41(10):3792–806. doi: 10.1007/s12325-024-02949-z
23. Bass GA, Pourlotfi A, Donnelly M, Ahl R, McIntyre C, Flod S, et al. Bile duct clearance and cholecystectomy for choledocholithiasis: definitive single-stage laparoscopic cholecystectomy with intraoperative endoscopic retrograde cholangiopancreatography versus staged procedures. J Trauma Acute Care Surg. (2021) 90(2):240–8. doi: 10.1097/ta.0000000000002988
Keywords: choledochoscopy, clinical effect, common bile duct stones, gallbladder stones, gastroscopy, laparoscopy
Citation: Fang H, Chen W, Wu Z and Ding G (2025) Comparative analysis of minimally invasive approaches for gallbladder and common bile duct stones: combined endoscopic techniques vs. ERCP with laparoscopic cholecystectomy. Front. Surg. 12:1543205. doi: 10.3389/fsurg.2025.1543205
Received: 11 December 2024; Accepted: 18 April 2025;
Published: 30 April 2025.
Edited by:
Alexander H. Petter-Puchner, Institute for Experimental and Clinical Traumatology (LBG), AustriaReviewed by:
Rossella Palma, Sapienza University of Rome, ItalyAlberto Ferreres, University of Buenos Aires, Argentina
Copyright: © 2025 Fang, Chen, Wu and Ding. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Guoping Ding, ZGluZ3VvcEB6anUuZWR1LmNu
 Haixing Fang
Haixing Fang Wenchao Chen
Wenchao Chen Zhengrong Wu
Zhengrong Wu