- Department of Urology, The General Hospital of Fujian Energy Group, Fuzhou, Fujian, China
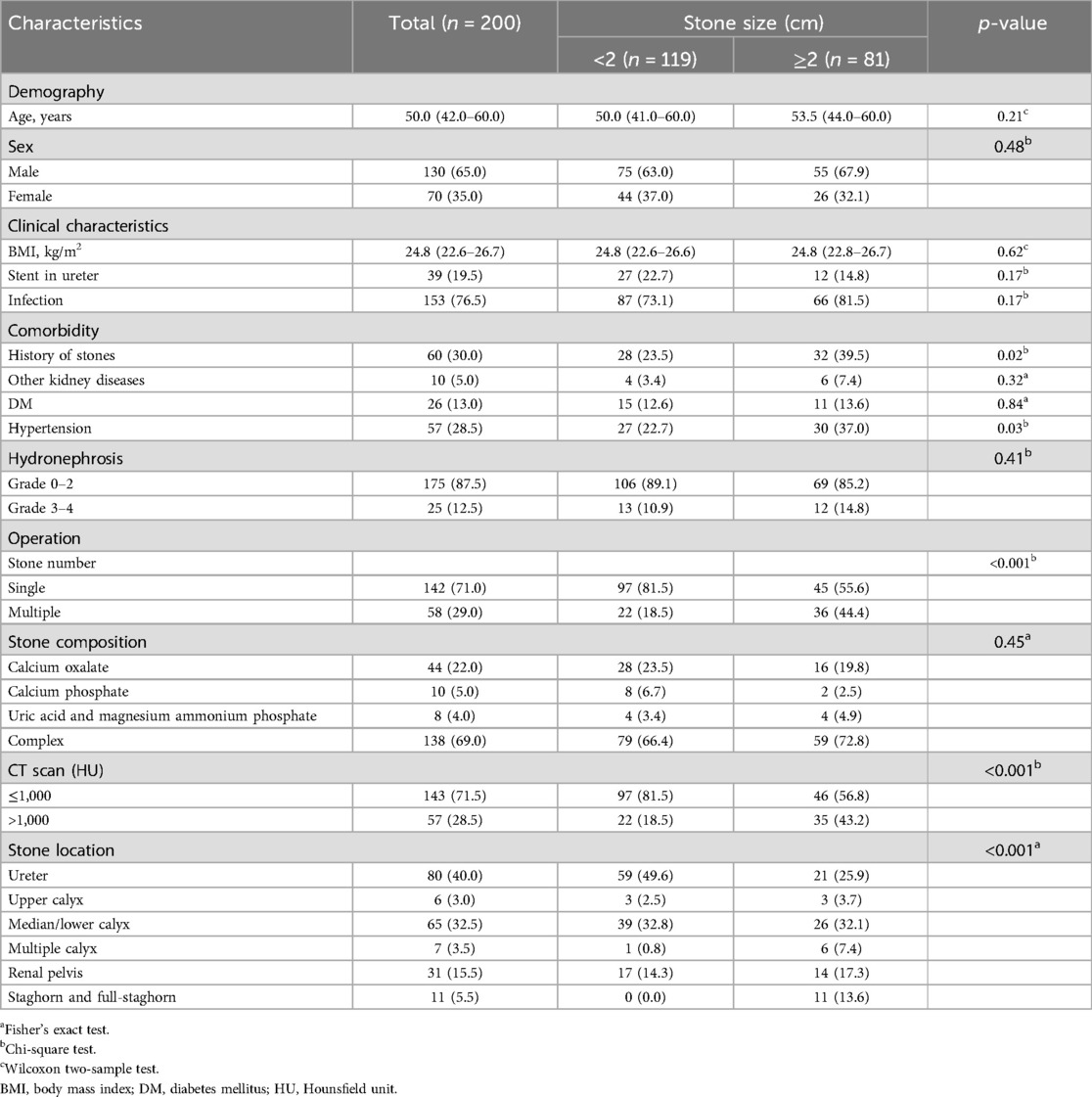
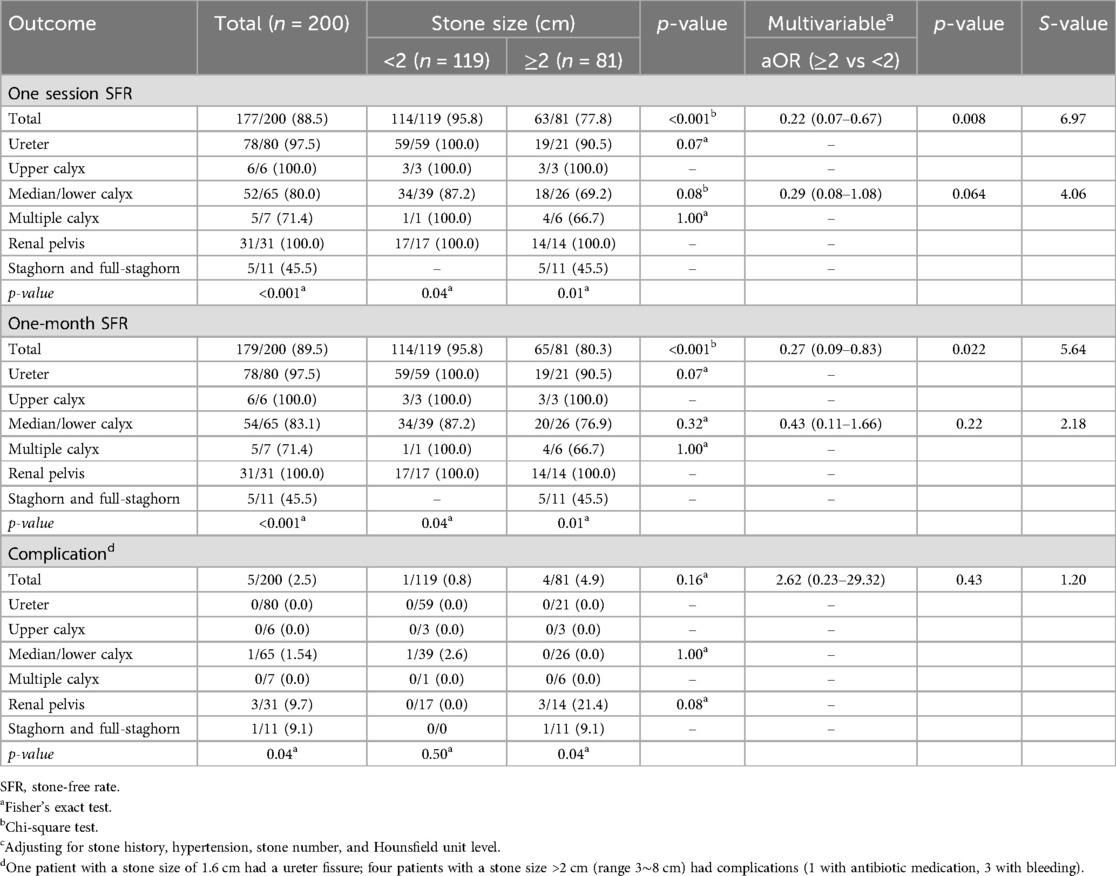
Suctioning Flexible Ureteroscopy with Intelligent Pressure Control (SFUI) has the advantage of automatically capturing and breaking urinary tract calculi while maintaining renal pelvic pressure stability. This retrospective study aimed to evaluate the efficacy of SFUI in treating upper urinary tract calculi of large sizes. A total of 200 patients with upper urinary tract calculi who underwent SFUI treatment in a single location from 2020 to 2021 were included. Outcomes were a one-session stone-free rate (SFR), one-month SFR, and complications within 4 weeks after SFUI classified by Clavien-Dindo grades. Patients’ median age was 50.0 years and a majority (65%) was males. Among them, 119 patients had small calculi (<2 cm) and 81 patients had large calculi (≥ 2 cm); 1 (0.8%) patient in the small calculi group, and 4 (4.9%) patients in the large calculi group had complications ≥ Grade II. Multivariable analysis showed that the large calculi group had significantly lower odds ratio for total one-session SFR [adjusted odds ratio (aOR): 0.22, 95% confidence interval (CI): 0.07–0.67, p = 0.008, S-value = 6.97] and one-month SFR (aOR: 0.27, 95% CI: 0.09–0.83, p = 0.022, S-value = 5.64) compared to the small calculi group, whereas calculi size was not associated with complication rate (aOR: 2.62, 95% CI: 0.23–29.32, p = 0.43, S-value = 1.20). In conclusions, SFUI is safe and effective for immediate stone removal after surgery. The very low complication rate benefits fast recovery, especially for patients with large calculi.
Introduction
Urinary tract calculi are primarily managed using minimally invasive methods such as ureteroscopy lithotripsy and percutaneous nephrolithotomy (PCNL), with the choice of treatment depending on patient factors, stone size, equipment, and expertise (1). Flexible ureteroscopy lithotripsy (FURL) is widely used for small renal stones due to its high stone-free rates (SFRs) and low complication rates (2–7). However, the high perfusion rate during FURL can lead to elevated renal pelvic pressure and backflow (8), which may result in complications like postoperative fever and systemic inflammatory response syndrome (9, 10).
As stone size increases, SFRs for FURL decrease significantly (2, 7). For renal stones ≥ 2 cm, the American Urological Association (AUA) and the European Association of Urology (EAU) recommend PCNL as the first-line treatment choice (11, 12). Despite the existing guidelines, controversy remains regarding the optimal treatment for larger stones, particularly those between 2 and 3 cm. While PCNL achieves a high SFR with effective immediate stone removal, it is associated with higher complication rates and longer hospital stays compared to FURL (4, 6, 7, 13, 14). FURL, though less invasive, is still questioned for its efficacy in larger stones, with limited high-quality evidence to support its use for this subset of patients. Previous meta-analyses documented that while FURL is generally safe and effective, it has significantly lower SFRs compared to PCNL for stones larger than 2 cm (15, 16). Thus, there is a need for treatment methods that achieve high SFRs while minimizing complications, especially for larger stones.
Suctioning Flexible Ureteroscopy with Intelligent Pressure Control (SFUI), a new variation of FURL, has demonstrated high lithotripsy efficacy and low complication rates (2%–5%) in patients with upper urinary tract calculi and a solitary kidney (17–19). However, current studies have not adequately explored this relatively newer technique. Therefore, there is a pressing need for further investigation to address the gaps in evidence regarding SFUI. This retrospective cohort study aimed to confirm the safety and effectiveness of SFUI in treating large calculi in different locations of the upper urinary tract, providing data to guide clinical decision-making and potentially bridge the gap between FURL and PCNL for larger stones.
Methods
Study design and patient selection criteria
This retrospective cohort study reviewed the medical records of patients who underwent SFUI surgery at the Department of Urology, General Hospital of Fujian Energy Group, China, between July 2020 and August 2021. Inclusion criteria were: (1) a diagnosis of urinary tract calculi; and (2) a comprehensive diagnostic work-up, including medical history, routine preoperative exams, and laboratory tests such as urinalysis, urine culture, blood tests, renal function assessment, and imaging studies. No specific exclusion criteria were applied. The study protocol was reviewed and approved by the Institutional Review Board of our institution, and informed consent was waived due to the retrospective nature of the study.
Operative procedure
Before the operation, a thorough assessment of the patient's history of urinary stones will be conducted, including whether the stones are primary or recurrent and the presence of ureteral stenosis. Before the operation, CT plain scan with 3D reconstruction and x-rays were used to assess the size and volume of the stones. x-rays were used to confirm stone radiopacity, establish a baseline image, and assess whether the stone could be monitored postoperatively using x-ray, which involves lower radiation exposure.
All surgeries were performed by the same surgeon with the SFUI system. The SFUI system contained a patented irrigation and suctioning platform (Patent No. ZL201420055766.5) and ureteral access sheath (Patent No. 201420055134.9) (Figure 1A–D) (17–19). The ureteral access sheath (outer diameter: F14.9; diameter of the working channel: F12; length 35–45 cm) has a pressure-sensitive tip. The very advantage of the SFUI system is keeping renal pelvic pressure (RPP) stable during operation, which is achieved by precisely regulating infusion flow and controlling the vacuum suctioning through computerized real-time recording and monitoring of RPP with a pressure feedback system (17–19).
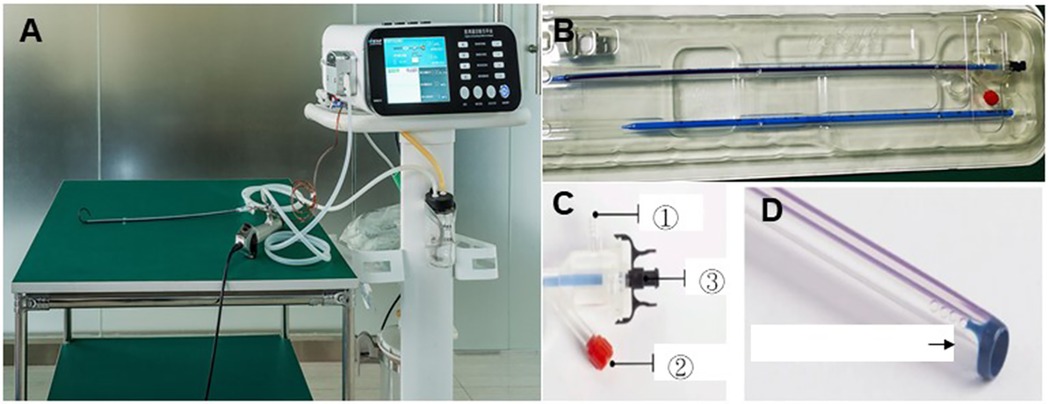
Figure 1. The SFUI system. (A) A patented irrigation and suction platform, consisting of a main control unit, an infusion device, a suctioning device, and a pressure feedback unit. The perfusion flow, pressure control value, and pressure limit value (30 mmHg) can be monitored on the main control unit during surgery. (B) A UAS with a transparent pressure-sensitive tip. The UAS has (C) one pressure sensor in the front end and (D) two connection channels at the back end, ① to vacuum device with suction effect and ② to pressure monitoring feedback device. ③ is the connecting channel to a flexible ureteroscope. UAS, ureteral access sheath.
The whole operative procedure has been described previously (17–19). Briefly, patients were in the oblique supine lithotomy position with the diseased side upward under general anesthesia (Figure 1E). Ureteroscopy was performed with a semi-rigid 8/9.8F ureteroscope (Richard Wolf, Germany) with a flexible 0.032-inch guidewire (Innovel, China) inserted into the renal collecting system. The ureteral access sheath was inserted into the proximal ureter along the guidewire without fluoroscopic guidance, and then a disposable flexible ureteroscope (Pusen, China) was inserted into the sheath for a comprehensive inspection of the delivery location of the transparent sheath between the renal pelvis and ureter.
The pressure sensory and suctioning channels were connected to the irrigation and suctioning platform when the transparent sheath reached the targeted position. Perfusion flow was set at 50–150 ml/min. RPP control value was set at −15∼−5 mmHg. The upper-limit value was set at 30 mmHg. The stone was broken by a holmium laser (Raykeen, China) at 0.8–1.2 J/pulse with a frequency of 20–30 Hz (energy ranged from 16 to 36 Watts). During lithotripsy, the scope body was moved back and forth slightly to facilitate suctioning out the small gravel particles, while gravel particles larger than the sheath gap but smaller than the ureteral access sheath were suctioned out by withdrawing the scope intermittently without the need for stone basketing. For patients in whom the indwelling ureteral access sheath was not successful, a 7F Double-J ureteral stent (Asymchem Inc., China) was placed for 2 weeks to facilitate the UAS placement for flexible ureteroscopy. Considering that the mucosa of the ureter may be hurt by repeated suction of stone fragments, a 7F Double-J ureteral stent was placed at the end of the operation and remained indwelling for 4 weeks to protect the ureter. Patients were followed at 4 weeks after the operation.
Not all patients successfully had an introducer sheath placed on the first attempt. Approximately 13% required the placement of a double J tube for two weeks before undergoing surgery due to initial placement failure.
Postoperatively, routine color Doppler ultrasound examinations at 3 and 6 months will be conducted to evaluate changes in hydronephrosis and assess for any postoperative ureteral stenosis, ensuring timely intervention if needed.
Clinical outcomes
The primary outcomes were the SFRs at one session and at one month after surgery. The secondary outcome was complications classified by Clavie-Dindo grade (20, 21) within 4 weeks after surgery. Stone size was determined by the maximal length shown in the KUB x-ray or CT image. For multiple stones, the sum of the maximal length of all stones was calculated. Stone-free was defined as no residual stone or left residual stone < 4 mm in size recognized by KUB x-ray images. Based on the Chinese Guideline for Diagnosis of Urology and Male Diseases 2019, intense follow-up is allowed for residual stones ≦4 mm without obstruction or infection.
Statistical analysis
To compare different groups, categorical variables are presented as N (%) and performed by the Chi-square test or Fisher's exact test, as appropriate. When more than 20% of cells have expected frequencies < 5, we used Fisher's exact test because applying the approximation method is inadequate (22). The normality of continuous data was examined by the Shapiro–Wilk test. Continuous variables with normal distribution are presented as mean ± standard deviation (SD) and performed by Student's t-test; non-normally distributed data are presented as median (interquartile range, 25th-75th percentile, IQR) and performed by the Wilcoxon rank-sum test. Adjusted odds ratios (aOR) and 95% confidence intervals (CI) were calculated for outcomes adjusted for p-value < 0.15 in univariate analysis using multiple logistic regression analysis. p-value < 0.05 was considered statistically significant. We also provided the S-value (the Shannon information, surprisal, or self-information), which is a logarithmic transformation of the P-value: S-value = − log2 (p-value) for the logistic regression model. The 95% CI includes the range of values which are compatible with the data, that is, statistical testing of values provides no > 4.32 bits (S-value > 4.32) of information against them assuming the background assumptions are correct. All statistical analyses were performed using SAS 9.4 statistical software (SAS Institute, Inc., Cary, NC, USA).
Results
Characteristics of the patients
A total of 200 patients were included, of whom 119 patients had stones <2 cm and 81 had stones ≥2 cm. Table 1 shows patients' baseline demographic and clinical characteristics. Patients' median age was 50.0 years. Most patients were male (65.0%). Among all patients, the main location of stones was the ureter (40.0%), median/lower calyx (32.5%), and renal pelvis (15.5%). Patients with stones ≥2 cm had significantly higher proportions of a history of stones (39.5% vs. 23.5%, p = 0.02), hypertension (37.0% vs. 22.7%, p = 0.03), multiple stones (44.4% vs. 18.5%, p < 0.001) and stones >1000 HU on CT scan (43.2% vs. 18.5%, p < 0.001) compared to those with stones <2 cm. In the <2 cm stone group, stones were primarily located in the ureter (49.6%) and the middle/lower calyx (32.5%), whereas in the ≥2 cm stone group, stones were predominantly found in the middle/lower calyx (32.1%). No significant differences were found in age, sex, BMI, stone composition, or hydronephrosis between the two groups.
Associations between stone size, location, and SFRs
Table 2 shows the univariate and multivariate analyses of outcomes between the two groups. Overall, total one-session SFR and one-month SFR were significantly associated with stone size (both p < 0.001) and stone location (both p < 0.001). Regarding stone size, stones in the upper calyx and renal pelvis had 100% one-session SFR in both groups, however, staghorn and full-staghorn stones in the size > 2 cm group had low one-session SFRs of 45%. One-session SFR and one-month SFRs were significantly associated with stone location in both groups (p = 0.04 for stone <2 cm and p = 0.01 for stone >2 cm).
Postoperative complications occurred in only 5 patients. One patient with a 1.6 cm stone located in the middle/lower calyx developed a ureteral fissure, likely due to a thin ureter and the placement of the ureteral access sheath. Among the four patients with a stone size > 2 cm who experienced postoperative complications, one developed a urinary tract infection that required intravenous antibiotic treatment (Clavien-Dindo Grade II), and three experienced gross haematuria without hemodynamic instability. The haematuria resolved spontaneously with conservative management and did not require transfusion or additional interventions (Clavien-Dindo Grade I). The total complication rate was 0.8% for stones <2 cm and 4.9% for stones >2 cm (p = 0.16). The complication rate was significantly associated with stone location when stones were >2 cm (p = 0.04). Stones located in the renal pelvis had the highest percentage of complications (21.4%), followed by the location of staghorn and full-staghorn stones (9.1%).
After adjusting for history of stones, hypertension, stone number, and Hounsfield unit level, patients with stone size ≥ 2 cm had significantly lower odds of total one-session SFR (aOR: 0.22, 95% CI: 0.07–0.67, p = 0.008, S-value = 6.97) and one-month SFR (aOR: 0.27, 95% CI: 0.09–0.83, p = 0.022, S-value = 1.20) than those with stone size < 2 cm. Stone location was not associated with complications (aOR: 0.16, 95% CI: 0.23–23.32, p = 0.43, S-value = 1.20).
Discussion
The present study revealed the high safety and efficacy of SFUI. For stones <2 cm, the total one-session SFR was 95.8% with a complication rate of 0.8%; for stones ≥2 cm, the total one-session SFR was 77.8% with a low complication rate of 4.9%. The low complication rate benefits the fast recovery of patients with large urinary tract calculi.
FURL treatment was reported to have a one-session SFR of 76%-90% for stones ≤2 cm with a complication rate of 6%-7% (2–7, 23, 24), and the SFR decreases to ∼60% for stones of 2–3 cm (25, 26). PCNL was reported to have SFRs higher than 85% with complication rates of 7%-12% for stones <2 cm, and SFRs of 76%-89% with a high complication rate of 10%-25% for stones >2 cm (4–7, 13, 14, 25, 27). The high complication rate of PCNL compared to FURL also leads to significantly longer hospital stays (4, 6, 7). Chen et al. (18) showed that SFUI has a shorter mean operative time, higher stone-free rate, and lower complication rate compared to FURL in cleaning kidney stones <2 cm, while no significant differences were found in postoperative hospital stays between SFUI and FURL (18). Another study showed that SFUI displayed shorter postoperative hospitalization and lower complication rate, including fewer patients needing pain medication and less bleeding compared to mini-invasive PCNL in treating kidney stones of 2–3 cm, while no significant differences were found in stone-free rates and mean operative times between SFUI and PCNL (28). Overall, SFUI displays a better one-session SFR than FURL for stones >2 cm and lower complication rates than PCNL, supporting a favorable option for fast recovery in patients with upper urinary tract calculi of larger size. The intelligence system automatically searched and broke large stones into tiny fragments for direct expulsion. The ability to break and immediately expel stone fragments is the main advantage of the SFUI system, making it markedly different from conventional FURL. In our study, all procedures were performed by a single experienced endourologist, which likely minimized variability related to operator experience. However, previous research has indicated that outcomes may still be influenced by the learning curve, particularly in mastering suction control and sheath positioning (29). Future multicenter studies involving multiple operators are warranted to better quantify the learning curve and its potential impact on clinical outcomes.
Results of the present study showed that SFR is lower in medial/low calyx compared to other locations, and it decreases as stone size increases. Two retrospective studies with small cohorts reported one-session SFRs of 75%–90% with retrograde ureteroscopy and ∼90% with PCNL for lower calyceal stones of 1–2 cm (23, 24). The priority for treating lower calyceal stones is PCNL, while stones <1.5 cm have a better chance for better SFRs with ureteroscopy (30). Meanwhile, staghorn stones are usually large and occupy a large proportion of the renal pelvis. PCNL combined with URL for residual stone cleaning is an option for treating staghorn stones with good final SFR (31, 32). However, the reported one-session SFR with a single PCNL treatment is 55%–60% for staghorn stones, with a high complication rate of ∼30% (33–35,36,37). Regarding the high complication rate of PCNL in treating staghorn stones, SFUI with multiple procedures may be an appropriate alternative consideration.
The SFUI system uses a special ureteral sheath with a pressure monitor on the original flexible scope. The price of this sheath is similar to that of the commonly used flexible ureteroscope sheath without a pressure monitor, making it highly economical and cost-effective. Although special surgical equipment for SFUI is required, the price is not high. Most medical institutions can afford it. Considering that most urinary calculi can be removed without major complications, SFUI is a good choice for both patients and hospitals.
Limitations
This study has several limitations. First, the absence of a control group undergoing other surgical treatments and the potential influence of unmeasured confounders are major limitations. Second, as a single-center retrospective study, there is a risk of selection bias, potential information bias, and reliance on existing records, which may impact patient recruitment and data analysis, thereby limiting the generalizability of the findings to other institutions or populations. Operation time was not reported. Although the SFUI system can maintain a relatively stable low-pressure state in the kidney, prolonged indwelling of the guide sheath may compress the ureter and cause ureteral injury, particularly in patients with ureteral stenosis, potentially leading to postoperative ureteral strictures. Additionally, longer operative times may increase the risk of other complications, such as lower limb thrombosis. Moreover, stone complexity was not graded using Guy's score due to incomplete anatomical data in some imaging records, which limited our ability to apply the scoring system consistently across all patients and may reduce the granularity of outcome interpretation. Another imitation is the lack of systematically recorded quantitative urine culture data, which may limit the ability to fully assess preoperative urinary infection status. Further prospective studies are highly recommended to specifically address these concerns and provide a more comprehensive analysis, including a direct comparison with PCNL.
Conclusions
SFUI system is safe and effective for immediate stone-free. The high SFR and very low complication rate benefit fast recovery, especially for patients with large calculi in the middle/lower calyx and renal pelvis.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the study protocol was reviewed and approved by the Institutional Review Board of the General Hospital of Fujian Energy Group. The ethics committee of the General Hospital of Fujian Energy Group waived the need for informed consent because of the retrospective study design. All methods were carried out according to relevant guidelines and regulations. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants’ legal guardians/next of kin because the ethics committee of the General Hospital of Fujian Energy Group waived the need for informed consent because of the retrospective study design.
Author contributions
WC: Conceptualization, Formal analysis, Project administration, Supervision, Writing – original draft. BZ: Data curation, Methodology, Writing – original draft. XL: Data curation, Formal analysis, Methodology, Writing – original draft. XG: Investigation, Methodology, Software, Writing – review & editing. ZZ: Methodology, Resources, Software, Writing – review & editing. YL: Investigation, Methodology, Resources, Writing – review & editing. HZ: Investigation, Methodology, Resources, Writing – review & editing. JY: Investigation, Methodology, Software, Writing – review & editing. GZ: Investigation, Methodology, Software, Writing – review & editing. WB: Investigation, Methodology, Software, Writing – review & editing. YuL: Methodology, Resources, Validation, Visualization, Writing – review & editing. YiL: Conceptualization, Data curation, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Hiller SC, Ghani KR. Frontiers of stone management. Curr Opin Urol. (2020) 30(1):17–23. doi: 10.1097/mou.0000000000000698
2. Cohen J, Cohen S, Grasso M. Ureteropyeloscopic treatment of large, complex intrarenal and proximal ureteral calculi. BJU Int. (2013) 111(3 Pt B):E127–131. doi: 10.1111/j.1464-410X.2012.11352.x
3. Breda A, Angerri O. Retrograde intrarenal surgery for kidney stones larger than 2.5 cm. Curr Opin Urol. (2014) 24(2):179–83. doi: 10.1097/mou.0000000000000030
4. Zhang Y, Yu CF, Jin SH, Zhu H, Na YQ. A prospective comparative study between minimally invasive percutaneous nephrolithotomy in supine position and flexible ureteroscopy in the management of single large stone in the proximal ureter. Urology. (2014) 83(5):999–1002. doi: 10.1016/j.urology.2013.11.034
5. Schoenthaler M, Wilhelm K, Hein S, Adams F, Schlager D, Wetterauer U, et al. Ultra-mini PCNL versus flexible ureteroscopy: a matched analysis of treatment costs (endoscopes and disposables) in patients with renal stones 10–20 mm. World J Urol. (2015) 33(10):1601–5. doi: 10.1007/s00345-015-1489-4
6. Jiao B, Lai S, Xu X, Zhang M, Diao T, Zhang G. The efficacy of flexible ureteroscopy lithotripsy and miniaturized percutaneous nephrolithotomy for the treatment of renal and proximal ureteral calculi of ≤2 cm: a retrospective study. Medicine (Baltimore). (2019) 98(11):e14535. doi: 10.1097/md.0000000000014535
7. Rao P, Li J, Shen S, Zhao H. A research on flexible ureteroscope lithotripsy versus percutaneous nephrolithotomy for upper urinary tract calculi. Int J Clin Exp Med. (2020) 13:1115–22.
8. Shao Y, Shen ZJ, Zhu YY, Sun XW, Lu J, Xia SJ. Fluid-electrolyte and renal pelvic pressure changes during ureteroscopic lithotripsy. Minim Invasive Ther Allied Technol. (2012) 21(4):302–6. doi: 10.3109/13645706.2011.595419
9. De La Rosette J, Denstedt J, Geavlete P, Keeley F, Matsuda T, Pearle M, et al. The clinical research office of the endourological society ureteroscopy global study: indications, complications, and outcomes in 11,885 patients. J Endourol. (2014) 28(2):131–9. doi: 10.1089/end.2013.0436
10. Zhong W, Leto G, Wang L, Zeng G. Systemic inflammatory response syndrome after flexible ureteroscopic lithotripsy: a study of risk factors. J Endourol. (2015) 29(1):25–8. doi: 10.1089/end.2014.0409
11. Assimos D, Krambeck A, Miller NL, Monga M, Murad MH, Nelson CP, et al. Surgical management of stones: american urological association/endourological society guideline, PART I. J Urol. (2016) 196(4):1153–60. doi: 10.1016/j.juro.2016.05.090
12. Türk C, Petřík A, Sarica K, Seitz C, Skolarikos A, Straub M, et al. EAU Guidelines on interventional treatment for urolithiasis. Eur Urol. (2016) 69(3):475–82. doi: 10.1016/j.eururo.2015.07.041
13. Elsheemy MS, Elmarakbi AA, Hytham M, Ibrahim H, Khadgi S, Al-Kandari AM. Mini vs standard percutaneous nephrolithotomy for renal stones: a comparative study. Urolithiasis. (2019) 47(2):207–14. doi: 10.1007/s00240-018-1055-9
14. Güler A, Erbin A, Ucpinar B, Savun M, Sarilar O, Akbulut MF. Comparison of miniaturized percutaneous nephrolithotomy and standard percutaneous nephrolithotomy for the treatment of large kidney stones: a randomized prospective study. Urolithiasis. (2019) 47(3):289–95. doi: 10.1007/s00240-018-1061-y
15. Kang SK, Cho KS, Kang DH, Jung HD, Kwon JK, Lee JY. Systematic review and meta-analysis to compare success rates of retrograde intrarenal surgery versus percutaneous nephrolithotomy for renal stones >2 cm: an update. Medicine (Baltimore). (2017) 96(49):e9119. doi: 10.1097/md.0000000000009119
16. Chung DY, Kang DH, Cho KS, Jeong WS, Jung HD, Kwon JK, et al. Comparison of stone-free rates following shock wave lithotripsy, percutaneous nephrolithotomy, and retrograde intrarenal surgery for treatment of renal stones: a systematic review and network meta-analysis. PLoS One. (2019) 14(2):e0211316. doi: 10.1371/journal.pone.0211316
17. Deng X, Song L, Xie D, Fan D, Zhu L, Yao L, et al. A novel flexible ureteroscopy with intelligent control of renal pelvic pressure: an initial experience of 93 cases. J Endourol. (2016) 30(10):1067–72. doi: 10.1089/end.2015.0770
18. Chen H, Song LM, Liu TR, Zhong JQ, Zhu LF, Yao L, et al. Clinical applications of intelligent pressure control flexible ureteroscope for the treatment of renal calculi ≤2 cm. Zhonghua Wai Ke Za Zhi. (2018) 56(10):772–5. doi: 10.3760/cma.j.issn.0529-5815.2018.10.014
19. Gao X, Zhang Z, Li X, Cai W, Zheng B, Lu Y, et al. High stone-free rate immediately after suctioning flexible ureteroscopy with intelligent pressure-control in treating upper urinary tract calculi. BMC Urol. (2022) 22(1):180. doi: 10.1186/s12894-022-01126-0
20. Clavien PA, Sanabria JR, Strasberg SM. Proposed classification of complications of surgery with examples of utility in cholecystectomy. Surgery. (1992) 111(5):518–26.1598671
21. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. (2004) 240(2):205–13. doi: 10.1097/01.sla.0000133083.54934.ae
22. Kim HY. Statistical notes for clinical researchers: chi-squared test and fisher’s exact test. Restor Dent Endod. (2017) 42(2):152–5. doi: 10.5395/rde.2017.42.2.152
23. Bozkurt OF, Resorlu B, Yildiz Y, Can CE, Unsal A. Retrograde intrarenal surgery versus percutaneous nephrolithotomy in the management of lower-pole renal stones with a diameter of 15 to 20 mm. J Endourol. (2011) 25(7):1131–5. doi: 10.1089/end.2010.0737
24. Aboutaleb H, El-Shazly M, Badr Eldin M. Lower pole midsize (1–2 cm) calyceal stones: outcome analysis of 56 cases. Urol Int. (2012) 89(3):348–54. doi: 10.1159/000341557
25. Zhang Y, Wu Y, Li J, Zhang G. Comparison of percutaneous nephrolithotomy and retrograde intrarenal surgery for the treatment of lower calyceal calculi of 2–3cm in patients with solitary kidney. Urology. (2018) 115:65–70. doi: 10.1016/j.urology.2017.11.063
26. Li Z, Lai C, Shah AK, Xie W, Liu C, Huang L, et al. Comparative analysis of retrograde intrarenal surgery and modified ultra-mini percutaneous nephrolithotomy in management of lower pole renal stones (1.5–3.5cm). BMC Urol. (2020) 20(1):27. doi: 10.1186/s12894-020-00586-6
27. Bozzini G, Aydogan TB, Müller A, Sighinolfi MC, Besana U, Calori A, et al. A comparison among PCNL, miniperc and ultraminiperc for lower calyceal stones between 1 and 2cm: a prospective, comparative, multicenter and randomised study. BMC Urol. (2020) 20(1):67. doi: 10.1186/s12894-020-00636-z
28. Chen H, Qiu X, Du C, Xie D, Liu T, Wang G, et al. The comparison study of flexible ureteroscopic suctioning lithotripsy with intelligent pressure control versus minimally invasive percutaneous suctioning nephrolithotomy in treating renal calculi of 2 to 3 cm in size. Surg Innov. (2019) 26(5):528–35. doi: 10.1177/1553350619849782
29. Mazzon G, Claps F, Germinale F, Brusa D, Choong S, Caruso A, et al. Learning curve for endoscopic combined intra-renal surgery using vacuum-assisted device. Urol Int. (2023) 107(4):413–21. doi: 10.1159/000528785
30. Boonyapalanant C, Saksirisampant P, Taweemonkongsap T, Leewansangtong S, Srinualnad S, Chotikawanich E. Factors impacting stone-free rate after retrograde intrarenal surgery for calyceal diverticular calculi. Res Rep Urol. (2020) 12:345–50. doi: 10.2147/rru.s265959
31. Chen L, Sha ML, Li D, Zhuo J, Jiang CY, Zhu YP, et al. Treatment for residual stones using flexible ureteroscopy and holmium laser lithotripsy after the management of complex calculi with single-tract percutaneous nephrolithotomy. Lasers Med Sci. (2017) 32(3):649–54. doi: 10.1007/s10103-017-2162-5
32. Leng S, Xie D, Zhong Y, Huang M. Combined single-tract of minimally percutaneous nephrolithotomy and flexible ureteroscopy for staghorn calculi in oblique supine lithotomy position. Surg Innov. (2018) 25(1):22–7. doi: 10.1177/1553350617741023
33. El-Nahas AR, Eraky I, Shokeir AA, Shoma AM, El-Assmy AM, El-Tabey NA, et al. Factors affecting stone-free rate and complications of percutaneous nephrolithotomy for treatment of staghorn stone. Urology. (2012) 79(6):1236–41. doi: 10.1016/j.urology.2012.01.026
34. Atmoko W, Birowo P, Rasyid N. Factors affecting stone free rate of primary percutaneous nephrolithotomy on staghorn calculi: a single center experience of 15 years. F1000Res. (2016) 5:2106. doi: 10.12688/f1000research.9509.2
35. Choi SW, Bae WJ, Ha US, Hong SH, Lee JY, Kim SW, et al. Prognostic impact of stone-scoring systems after percutaneous nephrolithotomy for staghorn calculi: a single center’s experience over 10 years. J Endourol. (2016) 30(9):975–81. doi: 10.1089/end.2016.0188
36. Deng XL, Song LM, Xie DH, Zhu LF, Yao L, Huang JR, et al. Suctioning flexible ureteroscopy with automatic control of renal pelvic pressure, a porcine model. Int J Clin Exp Med. (2016) 9:6563–8.
Keywords: Clavien-Dindo classification, stone-free rate, suctioning flexible ureteroscopy with intelligent pressure control, upper urinary tract calculi, calculi
Citation: Cai W, Zheng B, Li X, Gao X, Zhang Z, Lu Y, Zhao H, You J, Zheng G, Bao W, Lai Y and Lv Y (2025) Clinical advantages of suctioning flexible ureteroscopy with intelligent pressure control on treating large upper urinary tract calculi. Front. Surg. 12:1554964. doi: 10.3389/fsurg.2025.1554964
Received: 3 January 2025; Accepted: 19 June 2025;
Published: 2 July 2025.
Edited by:
Panagiotis Mourmouris, Metropolitan Hospital, GreeceReviewed by:
Beata Jurkiewicz, Medical Centre for Postgraduate Education, PolandLuca Ongaro, Royal Free Hospital, United Kingdom
Han Chu, Anhui Provincial Children's Hospital, China
Copyright: © 2025 Cai, Zheng, Li, Gao, Zhang, Lu, Zhao, You, Zheng, Bao, Lai and Lv. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yisong Lv, MzI5MTI2MzBAcXEuY29t
†These authors share first authorship
 Weiping Cai
Weiping Cai Bin Zheng
Bin Zheng Xinwei Li
Xinwei Li Xingjian Gao
Xingjian Gao Zedong Zhang
Zedong Zhang Hualong Zhao
Hualong Zhao Gangfeng Zheng
Gangfeng Zheng Yisong Lv
Yisong Lv