- Department of Orthopaedics, Taizhou School of Clinical Medicine, The Affiliated Taizhou People’s Hospital of Nanjing Medical University, Nanjing Medical University, Taizhou, Jiangsu, China
Bilateral medial third clavicle fractures are very rare, with only very few cases reported in the literature. The mechanism underlying this type of fracture is often complex, and so far, its treatment remains controversial. We report a case of bilateral medial third clavicle fractures after a traffic accident. X-ray showed dislocation of bilateral medial third clavicles. The patient was cured by surgery and instrument fixation. Both clavicles were fixed using an inverted anatomic locking plate. The patient had excellent shoulder function after 2 years of surgery. Clavicle stability is necessary for normal shoulder function, and surgical fixation is becoming a trend for displaced medial third clavicle fractures. In this study, we reported a patient with bilateral clavicle fractures of the medial third who was treated by surgery and achieved excellent shoulder movement. An inverted anatomic locking plate is an effective internal fixation material for treating this type of fracture.
Introduction
Clavicle fracture is very common in clinical practice, accounting for nearly 4% of all human bone fractures and up to 44% of all fractures of the shoulder girdle (1). However, medial third clavicle fracture is rare, accounting for less than 2%–3% of all clavicle fractures (2, 3). They are associated with multisystem injury, high energy trauma, and death (3). Furthermore, bilateral medial clavicle fractures are even rarer, and so far, only a few cases have been reported in the literature, accounting for less than 0.5% of all clavicle fractures (4). Most of the previous studies have suggested that non-operative treatment has been advocated as the golden standard for medial clavicle fractures due to the lack of specifically designed instruments and complex anatomical structures (5–7). However, conservative treatment of displaced sternal end fracture is often unsatisfactory with symptomatic injury and a nearly 15% nonunion (8). As previous studies have indicated unsatisfactory shoulder function and a high non-union rate among displaced fractures, surgery is increasingly used for medial clavicle fractures and various surgical methods have been proposed in this regard (3, 6, 9). In this report, we present a case of bilateral medial clavicle fractures treated by operation. The patient's management and postoperative functional status were assessed.
Case presentation
A 56-year-old male was immediately transferred to our hospital following a serious traffic accident. He was riding on an electric bicycle and had a frontal collision against a telephone pole. Because of this accident, he suffered from multiple injuries, including the left fourth rib bone cortex distorted, minor pneumothorax, right-side pleural effusion, and bilateral medial third clavicle fractures. No other complications were found.
X-ray of the shoulder girdle exhibited a minimal displacement of both fractures (Figure 1). Considering his multiple injuries, conservative treatment was temporarily proposed. Both clavicles were immobilized by collar and cuff slings and the thorax was secured with a rib strap. After one week of observation, the patient still complained about serious pain around both clavicles and could not passively move the shoulder joint. A computed tomography (CT) scan was arranged to reveal the displacement and shortening of bilateral medial clavicle fractures (Figures 2A–C). The left clavicle fit type 1B2 and the right fit type 1B1 according to Edinburgh's classification. The examination also showed that pneumothorax and pleural effusion were stable and only needed conservative treatment.

Figure 1. Anterior-posterior clavicle radiograph showing fresh bilateral fractures of medial clavicle.
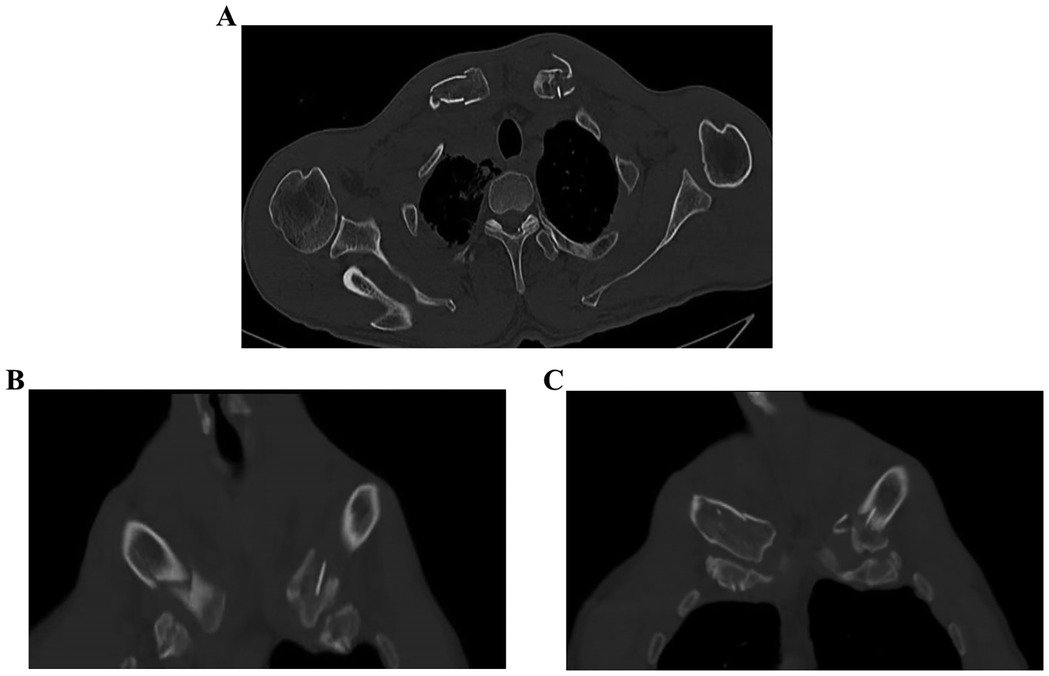
Figure 2. Ct image of bilateral medial clavicles showing complete displacement and shortening. (A–C) Are patient CT image of bilateral medial clavicles.
Considering the displacement and intra-articular fracture, the patient finally underwent surgery and fixation with the instrument. Lateral locking clavicle plates (Double Medical, China) and reversed implantation were used to fix both clavicles. As the sternal end of the clavicle has a similar angulation and surface as the lateral, the inverted implantation is an ideal implant for facture fixation. The variable-angle screw holes located at the end of lateral locking plates were placed toward the medial clavicle; thus, screws could pass through and fix the medial-end fragments of the clavicle. The sternal end fragment was fixed by the 2.7 mm locking screw and the other side of the plate was fixed with the 3.5 mm locking screw. The surgery was conducted under general anesthesia and the shoulder was placed slightly high in the supine position. The fracture of the clavicle was exposed gently without periosteal damage. Then the medial fragment was fixed temporarily with Kirschner wire, and locking screws was used to fix the fracture. When plating, the fragment was fixed with locking screws that passed through the unilateral cortex because of adjacent major thoracic vessels such as the aorta and vena cava. Then, remove the temporarily fixed Kirschner wire and the surgical wound was carefully sutured. The same surgery was performed on both sides. The postoperative radiograph showed that the implants were in good positions (Figure 3A). After the surgery, both shoulders were allowed progressive functional exercise and active and passive movements of the shoulder started after 3 weeks. Two months after the surgery, the patient felt no pain during active movement. After six months, the patient had a good recovery and full range of motion. At eight months, CT scan revealed the union of both fractures (Figures 3B,C). The patient obtained the excellent function of the shoulder (Figures 4A–C) and returned to his daily activities. After two years of the surgery, we evaluated the shoulder function based on the Disabilities of the Arm, Shoulder, and hand (DASH) score. The result was 5.0 and there was no obvious hardware irritation. Informed consent was obtained from this patient and this study was approved by the TaiZhou People's Hospital Clinic Research Ethic Committee (KY 2022-113-01).
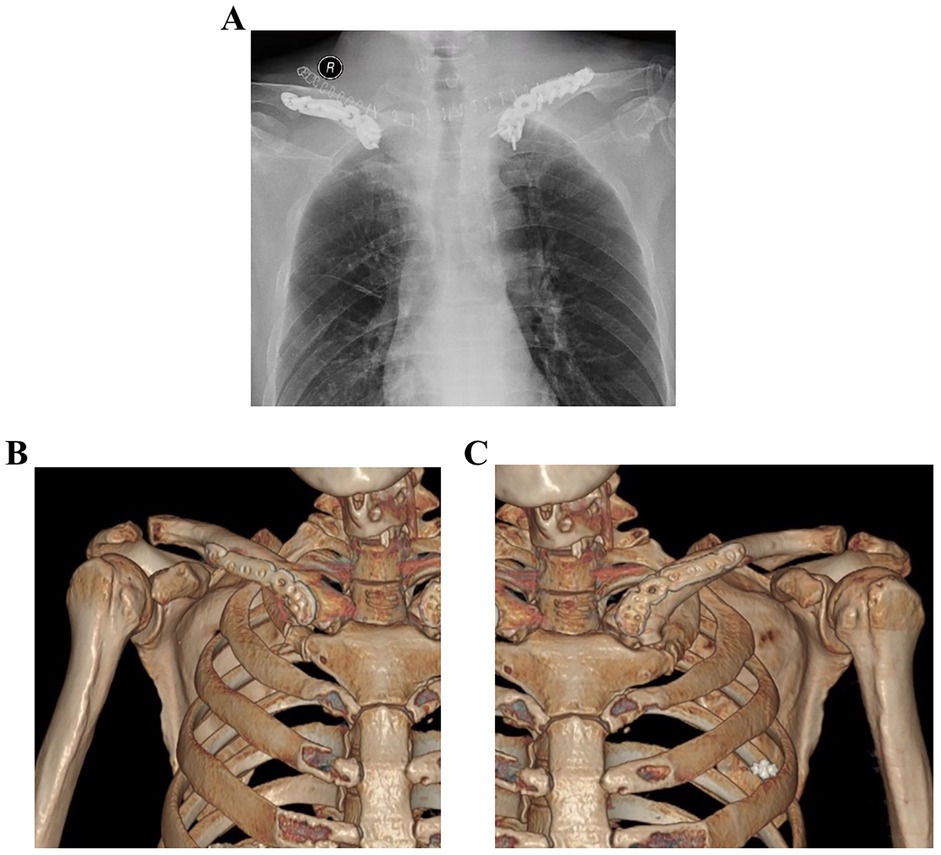
Figure 3. Postsurgical radiograph scans and CT scans. (A) Postsurgical radiograph demonstrating restoration of shoulder length after reduction and internal fixation with an inverted anatomic locking plate; (B,C) at eight months, CT scan revealed the union of both fractures.
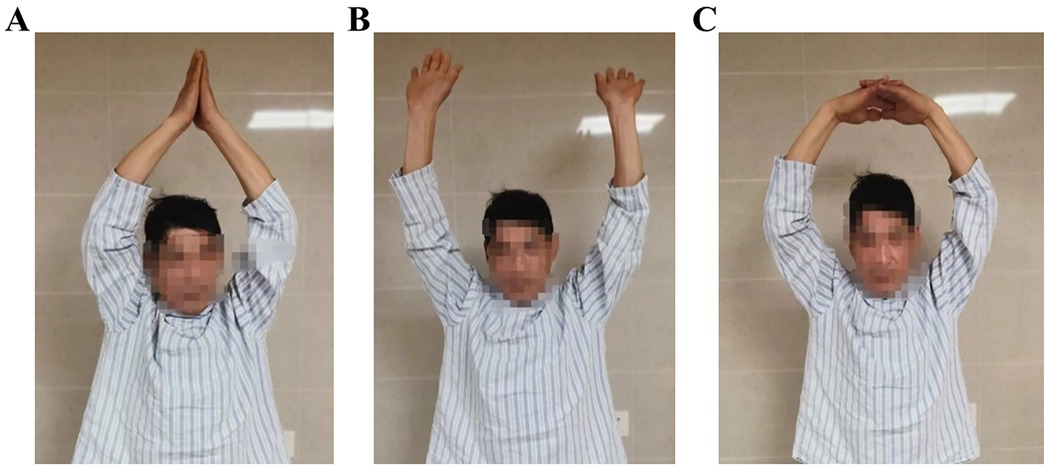
Figure 4. Free and full movement of the shoulder joints was achieved one year after the surgery. (A–C) Are patient activities.
Discussion
Bilateral clavicle fractures are rare. Most of the previously reported bilateral clavicle fractures were bilateral mid-range fractures or distal clavicle fractures (10–12). Bilateral medial clavicle fractures are even rarer, with only a few cases reported. Medial clavicle fractures are a special subgroup of clavicle fractures. The most common patients are middle-aged men experiencing traffic accidents. The high frequency of chest trauma (49%) and segmental fractures (9%) implies an association with high-energy trauma (3). The mechanism of this injury is complex including a motor vehicle or motorbike accident (36%) followed by sports (25%) and bicycle (23%) injuries (13). And it is usually associated with multi-organ and severe injuries and death (9, 14). This study reported a patient with bilateral fractures of the medial clavicle. The damage was mainly caused by strong violence directly affecting the chest.
Traditionally, non-surgical treatment is considered the gold standard for treating medical clavicle fractures. Undisplaced sternal end fractures warrant conservative treatment, and only few or no residual symptoms is occurred and the incidence of non-union for conservative treatment is less than 1% (15). Even in patients with significantly displaced fractures (6). However, the latest studies imply that conservative treatment of displaced medial clavicle fracture is often unsatisfactory. Displacement of sternal end clavicle fracture is most commonly defined in the literature using Throckmorton (>10 mm displacement) classification system (16). Following an average of three years non-operative management, the delayed union rate was 20% for displaced medial clavicle fracture (6, 17). Previous studies have found that 28% of patients who undergo non-surgical treatment may experience moderate-to-severe pain during follow-up (18). Robinson et al. showed that the non-union rate of non-displaced medial clavicle fracture is nearly 6.3% at 24 weeks after conservative treatment, while the proportion of displaced fractures is up to 14.3% (8). Salipas et al. found that only 45.8% of all patients undergoing non-surgical treatment achieve a good recovery. Of 7 patients with fracture displacement of more than 10 mm, 2 patients underwent surgery because of delayed union (6). Although, conservative management is still the major therapies, surgical treatment has recently been recommended for displaced medical clavicle fractures.
Surgical treatment of medial-end clavicle fracture is extremely challenging because of the complex anatomy and the limited options available for reliable internal fixation of the small medial fragment. Surgeries adjacent to the sternum can impose the risk of iatrogenic damage to the surrounding vasculature (19–21). As there is no special internal fixation for medial clavicle fracture, various implants have been used for fixation. There are three main ways of fragment fixation, including instrument plating (88%), suture (9%), and cerclage wires (3%) (2). Gill et al. used a modified hook plate and osteosynthesis, and the patient achieved a satisfactory shoulder function after a sixteen-month follow-up (22). A study found that displaced medial-end clavicle fracture can be fixed with an internal instrument with a union rate of 100% and a full range of motion at 12 months follow-up (23). However, implants have not been designed to fix the medial clavicle fracture. Most of the relevant studies are case reports, and there is no consensus on the optimal instrument for internal fixation. We used reversed lateral clavicle plates to fix medial clavicle fractures on both sides. The same surgical method was used in previous studies. Wang et al. published a patient with an extra-articular fracture of a medical clavicle who was treated with an inverted lateral clavicle locking plate. After 12 months of follow-up, the patient achieved satisfactory shoulder function and returned to daily activity (24). Bakir et al. used the same method to fix partial intra-articular fractures and achieved a good recovery (25). Liu et al. used the same method for 11 patients diagnosed with the medial-end clavicle, with no neurovascular injuries or internal fixation failures and good functional scores of the shoulder (26). It was found that fixation with lateral locking clavicle plates placed in reverse direction is a reliable and effective treatment for medial clavicle fractures.
However, we did not find any studies using inverted anatomic locking plates to fix bilateral medial clavicle fractures. We presented a patient with medial clavicle fractures on both sides. We followed the patient's postoperative functional status, and the subjective outcomes and satisfaction were measured.
In general, bilateral medial clavicle fractures are rare. Surgical treatment of displaced medial clavicle fractures using inverted plate has been reported as the optimal method to achieve rapid recovery with few complications. Therefore, the inverted anatomic locking plate can be used to cure this injury, even in patients with bilateral medial fractures. In the future, more studies should be conducted to validate our findings.
Conclusion
Bilateral fractures of the medial clavicle are rare, with only very few cases reported in the literature. Our patient underwent surgery to insert an inverted anatomic locking plate, and the follow-up demonstrated complete fracture union and good functional recovery.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Affiliated Taizhou People's Hospital of Nanjing Medical University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
JT: Writing – original draft. MZ: Writing – original draft. QY: Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Varelas N, Joosse P, Zermatten P. Operative treatment of an atypical segmental bipolar fracture of the clavicle. Arch Trauma Res. (2015) 4(4):e29923. doi: 10.5812/atr.29923
2. Kang LX, Faulkner HJ, Howard WH, Low AK. Displaced medial clavicle fractures: a systematic review of outcomes after nonoperative and operative management. JSES Int. (2023) 7(1):79–85. doi: 10.1016/j.jseint.2022.09.010
3. Asadollahi S, Bucknill A. Acute medial clavicle fracture in adults: a systematic review of demographics, clinical features and treatment outcomes in 220 patients. J Orthop Traumatol. (2019) 20(1):24. doi: 10.1186/s10195-019-0533-3
4. Kihlström C, Möller M, Lönn K, Wolf O. Clavicle fractures: epidemiology, classification and treatment of 2 422 fractures in the Swedish Fracture Register; an observational study. BMC Musculoskelet Disord. (2017) 18(1):82. doi: 10.1186/s12891-017-1444-1
5. van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg. (2012) 21:423–9. doi: 10.1016/j.jse.2011.08.053
6. Salipas A, Kimmel LA, Edwards ER, Rakhra S, Moaveni AK. Natural history of medial clavicle fractures. Injury. (2016) 47:2235–9. doi: 10.1016/j.injury.2016.06.011
7. Gleich J, Helfen T, Lampert C. Treatment concepts for the medial clavicle and the sternoclavicular joint. Unfallchirurgie (Heidelb). (2024) 127:783–7. doi: 10.1007/s00113-024-01461-x
8. Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. (2004) 86:1359–65. doi: 10.2106/00004623-200407000-00002
9. Frima H, Houwert RM, Sommer C. Displaced medial clavicle fractures: operative treatment with locking compression plate fixation. Eur J Trauma Emerg Surg. (2020) 46(1):207–13. doi: 10.1007/s00068-018-1024-6
10. Zhang YF, Zhang LF, Zhou YJ. Bilateral symmetrical distal clavicle fractures (neer type II): a case of rare injury. J Back Musculoskelet Rehabil. (2023) 36(3):773–7. doi: 10.3233/BMR-220245
11. Vellingiri K, Seenappa H. Bilateral clavicle fractures—a rare injury. Cureus. (2020) 12(11):e11449. doi: 10.7759/cureus.11449
12. Lakhotia D, Khatri K, Sharma V, Farooque K, Sharma S. Bilateral clavicle fractures: a report of three cases. J Clin Diagn Res. (2016) 10(6):RR01–3. doi: 10.7860/JCDR/2016/17236.8007
13. Feng WL, Cai X, Li SH, Li ZJ, Zhang K, Wang H, et al. Balser plate stabilization for traumatic sternoclavicular instabilities or medial clavicle fractures: a case series and literature review. Orthop Surg. (2020) 12:1627–34. doi: 10.1111/os.12726
14. Lindsey MH, Grisdela P, Lu L, Zhang D, Earp B. What are the functional outcomes and pain scores after medial clavicle fracture treatment? Clin Orthop Relat Res. (2021) 479(11):2400–7. doi: 10.1097/CORR.0000000000001839
15. Robinson CM. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. (1998) 80-B:476–84. doi: 10.1302/0301-620X.80B3.0800476
16. Van Tongel A, Toussaint A, Herregods S, Van Damme S, Marrannes J, De Wilde L. Anatomically based classification of medial clavicle fractures. Acta Orthop Belg. (2018) 84:62–7.30457501
17. Nowak J, Holgersson M, Larsson S. Sequelae from clavicular fractures are common: a prospective study of 222 patients. Acta Orthop. (2005) 76(4):496–502. doi: 10.1080/17453670510041475
18. Throckmorton T, Kuhn JE. Fractures of the medial end of the clavicle. J Shoulder Elbow Surg. (2007) 16(1):49–54. doi: 10.1016/j.jse.2006.05.010
19. Xie WP, Zhang YK, Chen YH, Wang SL, Xu HH, Bi RX. A novel surgical method for treating medial-end clavicle fractures. Exp Ther Med. (2018) 16(6):5390–3. doi: 10.3892/etm.2018.6870
20. Sidhu VS, Hermans D, Duckworth DG. The operative outcomes of displaced medial-end clavicle fractures. J Shoulder Elbow Surg. (2015) 24(11):1728–34. doi: 10.1016/j.jse.2015.04.011
21. Titchener A, See A, Van Rensburg L, Tytherleigh-Strong G. Displaced medial end clavicular fractures treated with an inverted distal clavicle plate contoured through 90 degrees. J Shoulder Elbow Surg. (2019) 28(4):e97–103. doi: 10.1016/j.jse.2018.08.047
22. Gille J, Schulz A, Wallstabe S, Unger A, Voigt C, Faschingbauer M. Hook plate for medial clavicle fracture. Indian J Orthop. (2010) 44(2):221–3. doi: 10.4103/0019-5413.61768
23. Low AK, Duckworth DG, Bokor DJ. Operative outcome of displaced medial-end clavicle fractures in adults. J Shoulder Elbow Surg. (2008) 17(5):751–4. doi: 10.1016/j.jse.2008.01.139
24. Wang Y, Jiang J, Dou B, Zhang P. Inverted distal clavicle anatomic locking plate for displaced medial clavicle fracture. Arch Orthop Trauma Surg. (2015) 135(9):1241–5. doi: 10.1007/s00402-015-2259-x
25. Bakir MS, Merschin D, Unterkofler J, Guembel D, Langenbach A, Ekkernkamp A, et al. Injuries of the medial clavicle: a cohort analysis in a level-I-trauma-center. Concomitant injuries. Management. Classification. Chirurgia (Bucur). (2017) 112(5):594. doi: 10.21614/chirurgia.112.5.586
Keywords: bilateral medial clavicle fracture, incision and internal fixation, case report, inverted anatomic locking plate, shoulder function
Citation: Tong J, Zhang M and Yu Q (2025) Bilateral clavicle fractures of the medial third treated by inverted anatomic locking plates: a case report. Front. Surg. 12:1562213. doi: 10.3389/fsurg.2025.1562213
Received: 17 January 2025; Accepted: 28 April 2025;
Published: 13 May 2025.
Edited by:
Wenqi Song, Shanghai Jiao Tong University, ChinaReviewed by:
Gergo Jozsa, University of Pécs, HungarySungho Lee, Cheju Halla University, Republic of Korea
Copyright: © 2025 Tong, Zhang and Yu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qing Yu, eXVxaW5neDE5Y3Nna0AxNjMuY29t
 Jian Tong
Jian Tong Qing Yu
Qing Yu