- 1Department of Orthopaedic Surgery, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Shanghai Key Laboratory of Orthopaedic Implants, Shanghai Ninth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 3Department of Orthopaedic Surgery, Shanghai Sixth People’s Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 4Department of Orthopaedic Surgery, Fengcheng Hospital of Fengxian District, Shanghai, China
Cervical andersson lesions (ALs) are rare in patients with ankylosing spondylitis (AS), and even more rare in patients with simultaneous superior cervical atlantoaxial fracture and dislocation. Here, we present a case of C1 Jefferson fracture (C1 bilateral posterior arch fracture), C2 odontoid, lateral mass, vertebral fracture (nonclassic C2 hangman fracture), traumatic posterior atlantoaxial dislocation (AAD) and C6/C7 AL in a long-standing AS cervical spine. The patient with traumatic AS-related cervical fractures underwent a two-stage surgery. The stage I surgery involved a posterior atlantoaxial reduction and fixation surgery combined with C5/C6/T1/T2 posterior pedicle screw fixation plus C6/C7 decompression. One week later, C6/C7 anterior cervical corpectomy decompression and fusion (ACCF) with long anterior plate stabilization combined with iliac crest bone graft transplantation was performed for stage II surgery. The patient recovery observed during follow-up was satisfactory. Nine-month postoperative radiological images revealed fracture union of the upper and lower cervical spine with optimal reduction of the atlantoaxial segment. In conclusion, lower cervical ALs with simultaneous upper cervical C1/C2 fractures in the AS are very rare. Posterior C1-C2 fixation combined with C6-C7 AL corpectomy/fusion and posterior pedicle screw fixation may offer a desirable alternative approach for this complex case of cervical trauma. During treatment, complete decompression, effective reduction, and potent stabilization can comprehensively improve the clinical prognosis.
Introduction
Ankylosing spondylitis (AS) is characterized by inflammatory ossification of the fusion between the sacroiliac joint and ankylosed spinal ligaments and presents as a stiff spine and osteoporosis (1). Therefore, patients with AS inevitably incur spinal fractures, which can be caused by even trivial traumatic impacts. Andersson lesions (ALs), known as erosive vertebral or discovertebral lesions in AS, are characterized by consistent spinal fracture nonunion, spondylodiscitis and pseudarthrosis (2). ALs are commonly found in the thoracic and lumbar regions of the spine rather than in the lower cervical spine (3, 4). This was partially due to the reduced mechanical stress in the cervical spine compared with that in the thoracolumbar skeleton. In addition, acute injury to the C1/C2 complex poses a potentially life-threatening challenge to the spine cord, resulting in severe neurological sequelae derived from unstable upper atlantoaxial joints. Very few studies have reported upper C1/C2 trauma with AS (5–7), and there are even few cases in which lower AL simultaneously presents with upper atlantoaxial fracture in a single patient. Herein, we describe the case in which a patient with AS was sent to our hospital after falling from a motorcycle during a collision. CT revealed a C1 Jefferson fracture (C1 bilateral posterior arch fracture), C2 odontoid fracture, lateral mass, vertebral fracture (nonclassic C2 hangman fracture), traumatic posterior atlantoaxial dislocation (AAD) and C6/C7 AL in the long-standing AS spine. Upon further history questioning, the patient recalled persistent neck pain after a previous fall two years ago but did not previously seek medical assistance. To the best of our knowledge, this is the first report that covers both the lower C6/C7 AL and upper C1/C2 AL fractures in the ankylosed spine. We aimed to identify the significant correlation between spinal stability and both C1/C2 and C6/C7 injuries by elucidating their clinical and treatment characteristics, aiming to provide a deeper understanding of cervical spine stability, especially in patients with AS.
Patient characteristics
Descriptions
A 49-year-old man experienced occipitocervical junction pain with restricted cervical range of motion while falling during a motorcycle collision. Significant numbness was found in both upper limbs, with reduced bilateral biceps and intrinsic hand muscle strength, especially in the left upper arm. The Lhermitte sign was positive when he bent his neck or rolled over on both sides, radiating from the neck to the planta pedis. The diagnosis of AS was established five years prior, but the patient failed to take proper medication regularly. He had experienced an accident two years prior, which was followed by consistent neck discomfort. However, he did not seek medical assistance during that period and played basketball several times.
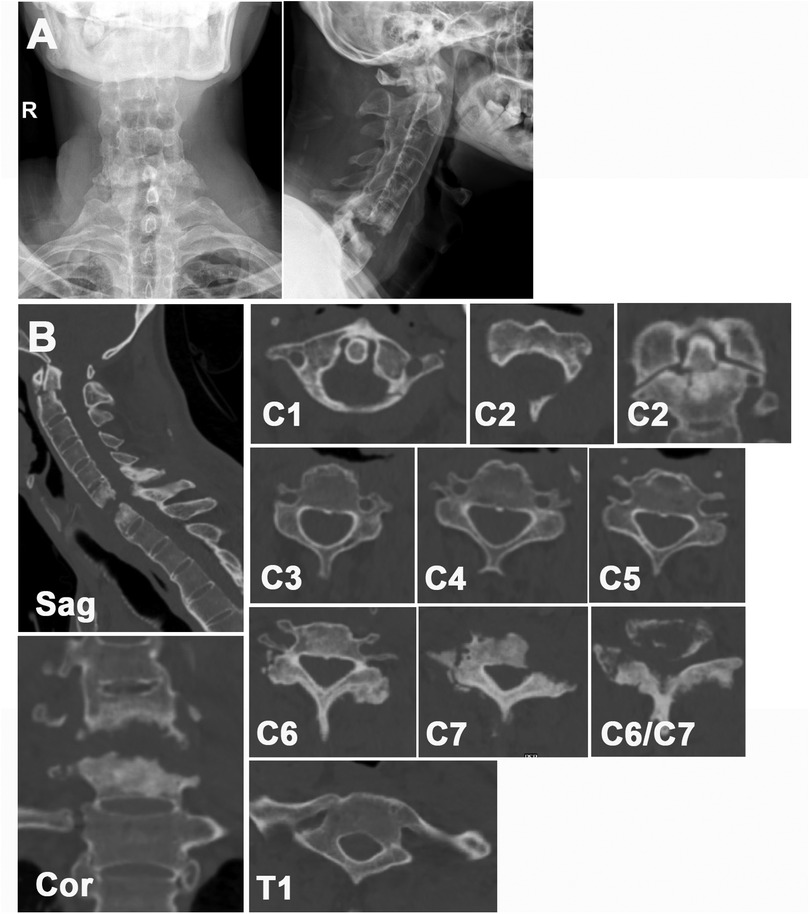
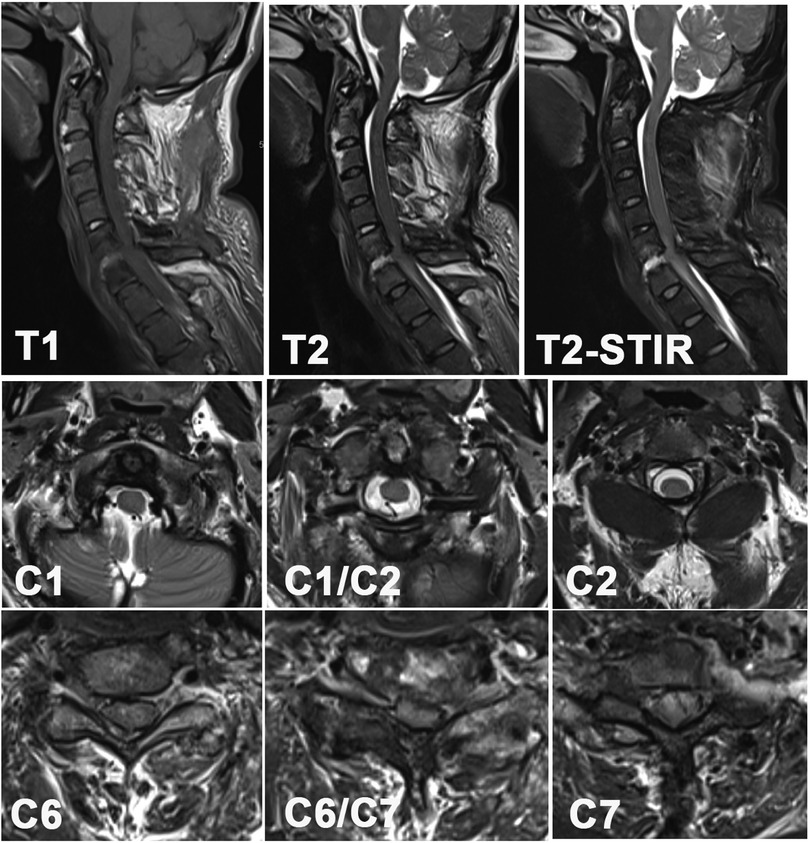
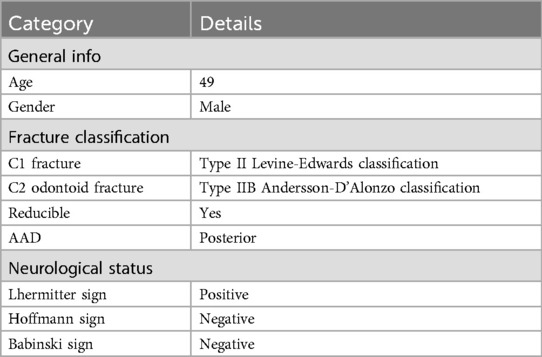
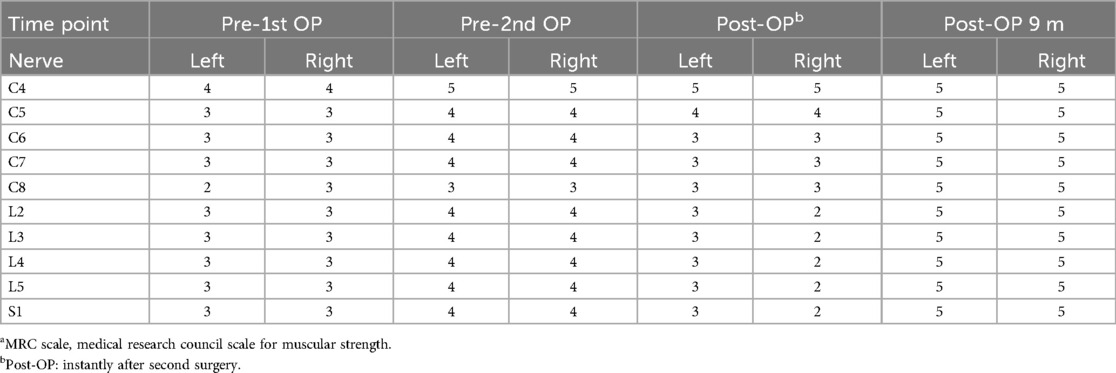
The characteristics of the patient are listed in Tables 1–3. The x-ray image revealed a bamboo-like ankylosed cervical spine (Figure 1A). A CT scan revealed the detailed characteristics of both the superior and inferior cervical fractures (Figure 1B). The C1 fracture was identified as a Jefferson fracture with bilateral posterior arch fracture, which was classified as type II Levine-Edwards classification with traumatic posterior AAD. The C2 vertebra suffers from odontoid fracture (type IIB Andersson-D'Alonzo classification) and lateral mass fracture of the vertebral wall (nonclassic C2 hangman fracture (8). Herein, the C6/C7 segment exhibited osteolysis combined with sclerosis in the upper and lower endplates, with the disappearance of the normal C6/C7 intervertebral structure. This process was followed by further destruction of the C6/C7 bony vertebrae. MRI (Figure 2) revealed vertebral edema in the C2 odontoid and vertebral walls. Additionally, the increase in the T2 signal was concentrated at the C6/C7 intervertebral level. The spinous process and supraspinous ligaments were injured, which was exemplified by the enhanced T2 intensity from C2 to the C7 posterior ligament complex (PLC). More importantly, the stenotic spinal cord was evidently compressed in the C6/C7 segment with diffuse intradural hyperintensity, which explained the reduced muscular strength and sensation in the extremities.
Surgery
Because this patient suffered from two separate traumas that contributed to the C1/C2 fracture and C6/C7 AL, both superior and inferior cervical lesions required sufficient decompression to rescue neurologic deficits as well as potent fixation to restore spinal stability via two sequential surgical operations. The initial surgery was posterior atlantoaxial reduction and fixation surgery combined with C5/C6/T1/T2 posterior pedicle screw fixation plus C6/C7 decompression. One week later, C6/C7 anterior cervical corpectomy decompression and fusion (ACCF) with long anterior plate stabilization combined with iliac crest bone graft transplantation was performed as a second surgery.
After the first posterior surgery, the patient experienced rapid neurologic recovery of limb numbness and weakness compared with his preoperative symptoms. However, after the second anterior surgery, the patient experienced a transient decrease in limb muscular strength, especially in the right lower limb (2/5). We considered that during the second C6/C7 ACCF surgery, because there was a large amount of fibrous scar tissue in the C6/C7 intervertebral space, which was accompanied by an unclear intervertebral structure and the formation of numerous osteophytes in the front edge of the adjacent upper and lower vertebral endplates, no obvious bony structures were observed in the posterior wall of the C6 and C7 vertebral bodies. The scar fibrous tissue was closely adherent to the dural sac and was not clearly and thoroughly separated. Hence, during the decompression process, inevitable disturbance may occur to the spinal cord, which can lead to the transient aggravation of neurologic symptoms. Subsequently, the patient received low-dose methylprednisolone and mannitol dehydration treatment. The patient's neurologic symptoms significantly improved within three days. His muscular strength of the left lower limb increased to 4/5. During the follow-up, he received regular NSAIDs treatment.
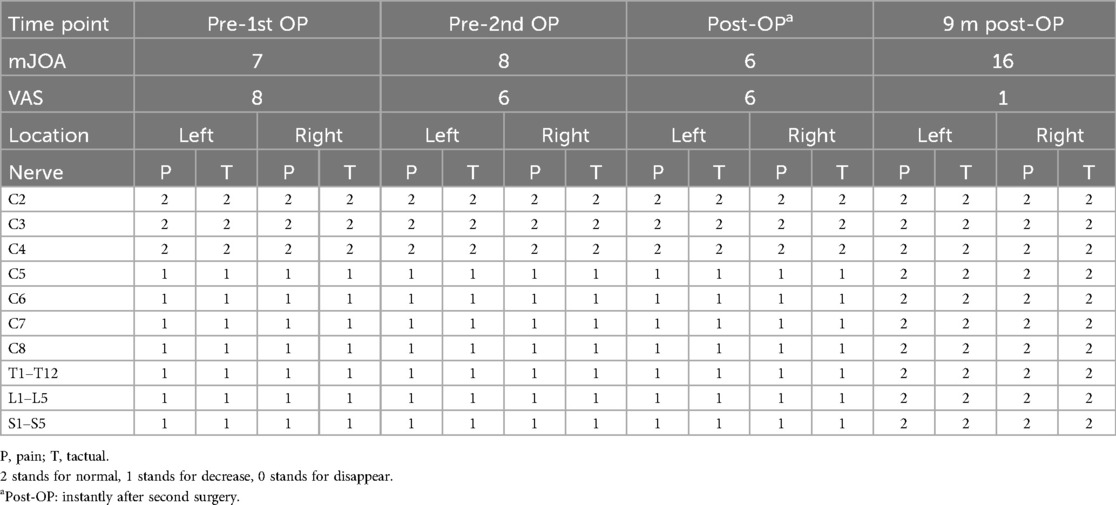
The final postoperative x-ray is shown in Figure 3A. Postoperative CT images (Figure 3B) demonstrated the precise implantation of each pedicle screw and the stable support of the anterior iliac crest bone graft. Figure 3C shows the bone healing observed after 9 months of follow-up. The AAD was corrected, and the stenotic C6/C7 lesion was decompressed sufficiently. After nine months of follow-up, the patient remained neurologically intact with no evident neck or limb discomfort. No other complication occurred during the rest follow-up period. He was able to walk freely without any brace help. The postoperative VAS score was 1, and the mJOA score was 16 compared with 8 and 7 preoperatively.

Figure 3. (A) postoperative cervical x-ray image. (B) Postoperative cervical CT image 2 days after surgery. (C) Postoperative cervical sagittal CT image 9 months after surgery showing healing of the odontoid fracture and bone fusion after C6 iliac bone transplantation.
Discussion
The unique feature of our patient was that he incurred two significant traumas. After the first trauma, cervical spinal stability was maintained partially by relying on fibrous union until the second severe trauma occurred two years later. These two separate falls cause lower and upper cervical fractures, respectively. Approximately 14% of AS patients clinically suffer from AS fracture (9), while only 1.5% progress to persistent AL bone nonunion (10). Altered biomechanics increase the risk of spinal fracture, thereby contributing to the progression of AL by persistently increasing vertebral/discovertebral stress and stimulating discitis/spondylodiscitis (11). Herein, the etiologies of AL varied. It can be classified as traumatic or inflammatory, which manifests as early spondylodiscitis or late pseudarthrosis, respectively (3). More importantly, the rigidity and fragility of the fused AS spine can act as a brittle plaster rather than an elastic spring, which is especially vulnerable to the uneven distribution of mechanical impact (12, 13). Therefore, even trivial mechanical stress can lead to severe loss of spinal stability, with 58% of patients being diagnosed with devastating neurologic sequalae (14). Spinal cord injury can be caused by instability of the cervical spine or direct stenotic compression of the bone fracture. Surgical approaches were thereby employed to resolve the spinal cord stimulation, reestablish the spinal curvature and restore normal neurologic functionality (15). Herein, preoperative MR revealed significant spinal cord compression at the stenotic C1/C2 and C6/C7 levels, indicating that the proper reduction and fixation of the responsible segments was indispensable for alleviating clinical symptoms. With regards to the AL, we chose C6/C7 ACCF with long anterior plate stabilization and iliac crest bone graft transplantation to debride the proliferative inflammatory tissue and reconstruct the immobilizer vertebral column. Additionally, posterior C5-T2 pedicle screw fixation assisted in maintaining cervical spine stability.
The common site of AL in AS patients is the thoracic and lumbar spine, especially in the thoracolumbar transition area (T10-L2) (16, 17); few studies have reported cervical AL, which is relatively rare (18), not to mention the concomitant occurrence of both cervical AL and C1 Jefferson fractures and C2 odontoid fractures. Peng (18) reported a 78-year-old AS patient suffered from C5/6 and C6/7 AL who received one stage anterior-posterior approach. The follow-up results showed the desirable relief of limb pain and movement. Since both C1–C2 dislocation and C6/C7 AL contributed to severe cervical instability, the use of a nonoperative treatment algorithm was not sufficient to correct the dynamic cervical imbalance. To date, numerous treatment modalities are used for restoring the cervical spine. Previously, transoral decompression, followed by posterior fixation or anterior fixation, was used to manage cervical sagittal alignment (19). However, due to the presence of multiple surgical incisions and the associated risk of infection, this combined surgical approach is not frequently employed in clinical practice. Eun (20) et al. presented a case of type II odontoid fracture with AAD in an AS patient who was treated with cervical reduction and occipito-cervical fusion (OCF) from C0-C4. Prognosis evaluation showed the satisfied recovery at 3 years postoperatively. Miao et al. also reported a series of cases of C2 odontoid fracture of the AS spine with posterior OCF and autologous bone transplantation, showing that the fracture union and dislocation were reduced (5). Mika et al. (21) revisited the MRI results of 20 AS cervical fracture patients and showed that only two patients suffered from both odontoid fracture and C1 Jefferson fracture. However, the researchers did not mention their corresponding treatment approaches. In addition, anterior odontoid screw fixation was employed to restore the cervical curvature in C2 odontoid fracture patients with AS, demonstrating the relief of neck symptoms with the retention of neck rotation functionality (22). Therefore, the surgical approach for treating cervical fractures in AS patients is controversial. Compared with lateral mass screws, posterior C1/C2 pedicle screw fixation for atlantoaxial immobilization can significantly decrease the postoperative NDI score with more efficient anti-pullout efficacy (23). More importantly, posterior C1/C2 pedicle screw fixation can be removed after fracture union, leading to the effective retention of neck rotary function. Compared with C1/C2 fixation without fusion, conventional C1/C2 fixation and iliac bone transplantation/fusion significantly reduced atlantoaxial rotation, leading to incongruous neck stiffness and discomfort (24). Additionally, anterior C1/C2 fixation was not applicable in our case of atlantoaxial fracture. The appropriate placement of anterior odontoid screws was challenging due to the traumatic kyphosis of the cervical spine as well as the osseous anterior longitudinal ligament (ALL). In contrast, with proper operative traction and reduction, posterior atlantoaxial fixation and fusion can satisfactorily meet the requirements for C1/C2 fracture healing (25). However, whether OCF with long-segment fixation or C1/C2 fusion with short-segment fixation results in atlantoaxial fracture of the AS spine remains debatable. Miao et al. (5) showed that OCF from C0-C4 posterior fixation can result in optimal atlantoaxial fracture union. This approach was not applicable in our patient due to the lower C6/C7 AL. The potential long-segment fixation from C0-C4 may have led to the new initiation of AL in the transition area between C0-C4 and C5-T2 after even trivial trauma. More importantly, the application of osteogenic agents and anti-osteoporosis remedies may serve as potent accelerators for bone fracture healing (26). Hence, individualized surgical fracture treatment is recommended based on diverse traumatic patterns, bone density and surgeon judgment.
Herein, our manuscript is the first to describe the combined occurrence of both upper C1/C2 fractures and AADs with C6/C7 ALs in AS patients. In addition, subsequent cervical reduction and posterior/anterior fixation and fusion resulted in desirable relief of cervical symptoms, as indicated by improvements in the VAS and mJOA scores. Our case provides an essential reference for multiple cervical injuries in AS patients. Extensive stenotic decompression and robust cervical stability are crucial for the treatment of multiple cervical traumas, especially in AS. However, when performing the fixation approach and fusion segment selection, various aspects should be considered individually and comprehensively.
Conclusion
Our review revealed a combination of superior atlantoaxial fracture (C1 Jefferson fracture and C2 type II odontoid fracture) with an inferior C6/C7 Andersson lesion in the rigid spine of the AS. Posterior C1/C2 fixation combined with C6/C7 AL corpectomy/fusion and posterior pedicle screw fixation could serve as a desirable alternative approach for this complex case of cervical trauma. During treatment, complete decompression, effective reduction, and potent stabilization can comprehensively improve the clinical prognosis.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics review committee of Shanghai Ninth People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
HQ: Writing – original draft. XC: Data curation, Writing – original draft. HT: Writing – review & editing. CZ: Writing – review & editing. XS: Writing – review & editing. JZ: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by Shanghai Municipal Health Commission (2020040329).
Acknowledgments
We thank all the staff in Orthopaedic Department of Shanghai Ninth Hospital. This study was approved by the ethics review committee of Shanghai Ninth People's Hospital.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Mauro D, Thomas R, Guggino G, Lories R, Brown MA, Ciccia F. Ankylosing spondylitis: an autoimmune or autoinflammatory disease? Nat Rev Rheumatol. (2021) 17(7):387–404. doi: 10.1038/s41584-021-00625-y
2. Sun X, Qiao H, Cheng X, Tian H, Shen K, Jin W, et al. Case report: identifying andersson-like lesions in diffuse idiopathic skeletal hyperostosis. Front Endocrinol (Lausanne). (2021) 12:766209. doi: 10.3389/fendo.2021.766209
3. Bron JL, de Vries MK, Snieders MN, van der Horst-Bruinsma IE, van Royen BJ. Discovertebral (andersson) lesions of the spine in ankylosing spondylitis revisited. Clin Rheumatol. (2009) 28(8):883–92. doi: 10.1007/s10067-009-1151-x
4. Park YS, Kim JH, Ryu JA, Kim TH. The andersson lesion in ankylosing spondylitis: distinguishing between the inflammatory and traumatic subtypes. J Bone Joint Surg Br. (2011) 93(7):961–6. doi: 10.1302/0301-620X.93B7.26337
5. Miao J, Chen Y, Zhang B, Li T, Luo Y, Shi L, et al. Surgical treatment for odontoid fractures in patients with long-standing ankylosing spondylitis: a report of 3 cases and review of the literature. World Neurosurg. (2018) 116:88–93. doi: 10.1016/j.wneu.2018.05.055
6. Hamilton MG, MacRae ME. Atlantoaxial dislocation as the presenting symptom of ankylosing spondylitis. Spine (Phila Pa 1976). (1993) 18:2344–6. doi: 10.1097/00007632-199311000-00037
7. Thompson GH, Khan MA, Bilenker RM. Spontaneous atlantoaxial subluxation as a presenting manifestation of juvenile ankylosing spondylitis. A case report. Spine (Phila Pa 1976). (1982) 7:78–9. doi: 10.1097/00007632-198200710-00014
8. Li G, Wang Q. Detailed observation of anatomical location and pattern in hangman’s fracture based on computed tomography three-dimensional reconstruction. J Orthop Surg Res. (2023) 18:136. doi: 10.1186/s13018-023-03622-x
9. Feldtkeller E, Vosse D, Geusens P, van der Linden S. Prevalence and annual incidence of vertebral fractures in patients with ankylosing spondylitis. Rheumatol Int. (2006) 26(3):234–9. doi: 10.1007/s00296-004-0556-8
10. Pai SN, Kailash K, Jayabalan V, Ganesan S. Andersson lesion in ankylosing spondylitis. BMJ Case Rep. (2022) 15(2):1–2. doi: 10.1136/bcr-2021-248542
11. Kim DH, Kim SW, Lee SM. Complete fusion of three lumbar vertebral bodies in ankylosing spondylitis. Korean J Neurotrauma. (2020) 16:105–9. doi: 10.13004/kjnt.2020.16.e1
12. Einsiedel T, Schmelz A, Arand M, Wilke H, Gebhard F, Hartwig E, et al. Injuries of the cervical spine in patients with ankylosing spondylitis: experience at two trauma centers. J Neurosurg Spine. (2006) 5(1):33–45. doi: 10.3171/spi.2006.5.1.33
13. Shen FH, Samartzis D. Surgical management of lower cervical spine fracture in ankylosing spondylitis. J Trauma. (2006) 61:1005–9. doi: 10.1097/01.ta.0000208125.63010.04
14. Westerveld LA, van Bemmel JC, Dhert WJ, Oner FC, Verlaan JJ. Clinical outcome after traumatic spinal fractures in patients with ankylosing spinal disorders compared with control patients. Spine J. (2014) 14(5):729–40. doi: 10.1016/j.spinee.2013.06.038
15. Zhang X, Wang Y, Wu B, Hu W, Zhang Z, Wang Y. Treatment of andersson lesion-complicating ankylosing spondylitis via transpedicular subtraction and disc resection osteotomy, a retrospective study. Eur Spine J. (2016) 25(8):2587–95. doi: 10.1007/s00586-015-4213-6
16. Hu X, Kong Y, Li B. Andersson lesion in the thoracic spine. J Clin Rheumatol. (2021) 27:e258. doi: 10.1097/RHU.0000000000001402
17. Li WF, Zhang MQ, Ren CQ, Sun Y. Ankylosing spondylitis complicating with a thoracolumbar andersson lesion: a case report. Asian J Surg. (2023) 46(12):5749–50. doi: 10.1016/j.asjsur.2023.08.122
18. Peng YJ, Zhou Z, Wang QL, Liu XF, Yan J. Ankylosing spondylitis complicated with andersson lesion in the lower cervical spine: a case report. World J Clin Cases. (2022) 10(11):3533–40. doi: 10.12998/wjcc.v10.i11.3533
19. Di Lorenzo N. Transoral approach to extradural lesions of the lower clivus and upper cervical spine: an experience of 19 cases. Neurosurgery. (1989) 24:37–42. doi: 10.1227/00006123-198901000-00006
20. Eun J, Oh Y. Traumatic lateral atlantoaxial dislocation combined with a type II odontoid fracture in a patient with ankylosing spondylitis: a case report. Medicine (Baltimore). (2022) 101:e30912. doi: 10.1097/MD.0000000000030912
21. Koivikko MP, Koskinen SK. MRI of cervical spine injuries complicating ankylosing spondylitis. Skeletal Radiol. (2008) 37:813–9. doi: 10.1007/s00256-008-0484-x
22. Shen T, Zhao X, Huang Y, Shang H. Type II odontoid fracture in an ankylosing spondylitis patient: successful treatment by anterior odontoid screw fixation. Asian J Surg. (2022) 45(11):2590–1. doi: 10.1016/j.asjsur.2022.06.012
23. Ibrahim Y, Li H, Zhao G, Yuan S, Zhao Y, Liu W, et al. Posterior temporary C1-2 pedicle screws fixation for the treatment of unstable C1-2 Complex fractures: minimum of 2-year follow-up. Global Spine J. (2023) 13(6):1522–32. doi: 10.1177/21925682211039186
24. Guo Q, Zhang M, Wang L, Lu X, Guo X, Ni B. Comparison of atlantoaxial rotation and functional outcomes of two nonfusion techniques in the treatment of Anderson-D'Alonzo type II odontoid fractures. Spine (Phila Pa 1976). (2016) 41(12):E751–8. doi: 10.1097/BRS.0000000000001370
25. Frangen TM, Zilkens C, Muhr G, Schinkel C. Odontoid fractures in the elderly: dorsal C1/C2 fusion is superior to halo-vest immobilization. J Trauma. (2007) 63(1):83–9. doi: 10.1097/TA.0b013e318060d2b9
Keywords: andersson lesion, ankylosing spondylitis, atlantoaxial fracture, spinal stability, cervical surgery
Citation: Qiao H, Cheng X, Tian H, Zhao C, Sun X and Zhao J (2025) Lower cervical C6/C7 andersson lesion with upper cervical C1/C2 fracture in ankylosing spondylitis: a case report and literature review. Front. Surg. 12:1568553. doi: 10.3389/fsurg.2025.1568553
Received: 30 January 2025; Accepted: 12 May 2025;
Published: 27 May 2025.
Edited by:
Siying Song, Massachusetts General Hospital and Harvard Medical School, United StatesReviewed by:
Fulvio Tartara, University Hospital of Parma, ItalyShaocheng Liu, Capital Medical University, China
Qihan Guo, Capital Medical University, China
Copyright: © 2025 Qiao, Cheng, Tian, Zhao, Sun and Zhao. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Changqing Zhao, emhhb2NxOWhvc3BpdGFsQDE2My5jb20=; Xiaojiang Sun, c3hqNjAzQDEyNi5jb20=
 Han Qiao
Han Qiao Xiaofei Cheng
Xiaofei Cheng Haijun Tian
Haijun Tian Changqing Zhao
Changqing Zhao Xiaojiang Sun
Xiaojiang Sun Jie Zhao
Jie Zhao