- Neurosurgical Intensive Care Unit, Nanjing Drum Tower Hospital Affiliated to Nanjing University Medical School, Nanjing City, Jiangsu, China
Objectives: This study aimed to evaluate the psychological outcomes and changes in health-related quality of life (HRQOL) in Chinese patients with Moyamoya disease (MMD) following revascularization procedures.
Methods: A total of 68 patients diagnosed with MMD and who underwent revascularization at Nanjing Drum Tower Hospital between January 2023 and January 2024 were retrospectively analyzed. Neuropsychological assessments, including the Trail Making Test, Chapuis Maze, Digit D2, Symptom Checklist-90 (SCL-90), Beck Depression Inventory-II (BDI-II), and the 36-item Short Form Health Survey (SF-36), were administered preoperatively and postoperatively at 3 months and 1 year. Statistical analysis was performed using SPSS version 29.0, with appropriate parametric or non-parametric tests applied based on data distribution.
Results: Baseline characteristics revealed no significant differences between the Unremarkable and Impaired groups, confirming comparability. Postoperative improvements were observed in HRQOL across multiple domains, particularly in patients with preoperative impairments. Significant improvements were seen in physical functioning, general health, physical pain, emotional role function, and vitality (P < 0.05). Psychological outcomes also showed significant improvements, with reductions in aggressiveness, anxiety, and somatization (P < 0.001). Depression scores significantly decreased in 29.4% of patients (P < 0.001), and executive function, as measured by TMTA, TMTB, and Digit D2, also showed significant improvements in the impaired group (P < 0.001). However, patients without preoperative impairments exhibited no significant changes in any of the assessed domains.
Conclusion: Revascularization significantly improves both psychological outcomes and HRQOL in Chinese patients with MMD, particularly in those with preoperative impairments. These findings highlight the importance of surgical intervention in enhancing both cognitive and psychological functioning in this patient population. Further prospective studies are warranted to confirm these results and explore long-term benefits.
1 Introduction
Moyamoya disease (MMD) is a chronic cerebrovascular disorder marked by progressive stenosis of the internal carotid arteries, leading to the formation of fragile collateral vessels in response to impaired blood flow (1, 2). Predominantly affecting East Asian populations, including Chinese individuals, MMD is associated with an increased risk of transient ischemic attacks (TIA), ischemic strokes, and intracerebral hemorrhage (3, 4). In addition to these serious physical consequences, MMD often results in significant cognitive impairment, emotional distress, and diminished health-related quality of life (HRQOL) (5, 6).
Revascularization surgery, specifically aimed at restoring cerebral perfusion and mitigating the risk of ischemic events, has been widely endorsed as the primary therapeutic approach for MMD (7). Studies have consistently demonstrated its efficacy in significantly reducing stroke recurrence (7, 8). However, recent research has increasingly focused on the broader neuropsychological and HRQOL outcomes following revascularization (9, 10). Cognitive impairments in MMD patients, particularly in domains such as executive function, attention, and memory, are prevalent due to chronic cerebral hypoperfusion (11). These deficits often exacerbate psychological issues, including depression, anxiety, and emotional instability, which are commonly reported in both pediatric and adult populations (6). While the surgical intervention successfully improves cerebral blood flow and reduces the risk of recurrent ischemic events, its effects on neurocognitive recovery are variable. Research indicates that cognitive function can improve post-surgery, especially in younger patients or those who undergo early intervention (9). However, long-term cognitive outcomes remain mixed, with some patients continuing to experience deficits in higher-order cognitive processes (10). Additionally, neuroimaging studies have shown that even after revascularization, regions of the brain previously affected by ischemia may not fully recover, leading to persistent cognitive challenges (12).
HRQOL in MMD patients is also notably impacted by both physical symptoms, such as fatigue and recurrent strokes, and cognitive and emotional challenges (13, 14). Post-revascularization HRQOL assessments show improvements in physical function, but mental health outcomes remain inconsistent (15). This underscores the importance of a multidisciplinary treatment approach for MMD, integrating cognitive rehabilitation and psychological interventions alongside surgery. However, the research specifically evaluating psychological outcomes and HRQOL changes following revascularization remains sparse, particularly in Chinese MMD patients. While many studies have focused on surgical and neurological outcomes, the effects of revascularization on cognitive function, emotional well-being, and overall quality of life in this demographic are underexplored. Considering the high prevalence of MMD in East Asian populations and the unique cultural and social factors influencing psychological health (3, 14, 16), it is essential to investigate these outcomes in Chinese patients.
This study aims to address this significant gap in the literature by systematically evaluating the psychological outcomes and HRQOL changes in Chinese MMD patients following revascularization surgery. Through detailed pre- and post-operative neuropsychological assessments, the study seeks to provide insights into the cognitive and emotional recovery associated with surgical intervention. By focusing on this understudied population, the research highlights the broader therapeutic potential of revascularization, offering important implications for improving overall patient management and quality of life in Chinese MMD patients.
2 Methods
2.1 Participants enrollment
This study retrospectively identified a group of Chinese patients diagnosed with MMD who subsequently underwent revascularization procedures. Patients were consecutively enrolled from the Nanjing Drum Tower Hospital Affiliated to Nanjing University Medical School between January 2023 and January 2024. A total of 68 participants met the eligibility criteria and were included in the final analysis. Selection criteria were based on established clinical and imaging guidelines. Specifically: (1) Clinical criteria: Patients exhibited ischemic symptoms [e.g., transient ischemic attack (TIA) or stroke] or progressive cognitive decline associated with MMD. (2) Imaging criteria: Diagnosis was confirmed via cerebral angiography, demonstrating progressive stenosis or occlusion of the internal carotid artery with characteristic collateral vessel formation. Additional evaluations, including functional MRI and H₂¹⁵O-PET with acetazolamide challenge, were used to assess cerebral perfusion status and determine surgical candidacy. Patients were excluded if they had secondary Moyamoya syndrome, severe comorbid conditions limiting surgery, or incomplete follow-up data. These criteria ensured a well-defined study population while maintaining clinical relevance. The study was approved by the Ethics Committee of the Nanjing Drum Tower Hospital Affiliated to Nanjing University Medical School. This study received ethics committee approval, ensuring compliance with ethical guidelines. Due to its retrospective design, obtaining individual informed consent was not feasible, and a waiver was granted per institutional and national regulations. To protect privacy, all data were anonymized before analysis, adhering to the Declaration of Helsinki. While informed consent was waived, patient rights remained safeguarded. In future studies, we recognize the value of prospective designs to obtain explicit consent and enhance ethical compliance. To ensure sufficient statistical power, we conducted a post-hoc power analysis. Based on observed effect sizes (Cohen's d ranging from 0.57 to 4.59), the required sample sizes to achieve 80% power varied between 3 and 26 participants, except for Chapuis Maze, which exhibited a negligible effect size. Given that our study included 68 participants, the power is more than sufficient for detecting significant changes in key outcomes. However, for detecting very small effects, particularly in spatial memory (Chapuis Maze), a much larger sample may be required in future research.
2.2 Neuropsychological assessments
Certified neuropsychologists conducted assessments covering executive function, psychological well-being, depression, and health-related quality of life (HRQOL). The NPAs included the Trail Making Test A (TMTA) and B (TMTB) for executive function, Chapuis Maze (CM) for spatial navigation, and Digit D2 (D2) for attention and processing speed. Psychological outcomes were measured with the Symptom Checklist-90 (SCL-90), depression with the Beck Depression Inventory-II (BDI-II), and HRQOL with the 36-item Short Form Health Survey (SF-36). The cutoff values of function impairment are defined based on previous report (17, 18). Preoperative imaging used cerebral panangiography, functional MRI, and H2 15 O-PET with acetazolamide challenge to assess disease severity and cerebral perfusion. Multiterritorial revascularization was performed in stages as needed. Postoperative assessments, including MRI, occurred 3 months after surgery, and follow-up assessments were conducted at 1 year to assess cognitive and psychological changes.
2.3 Statistical analysis
The data analysis and statistical evaluations were conducted using the latest version of SPSS software (SPSS 29.0). To determine whether the parametric data conformed to a normal distribution, the Shapiro–Wilk test was applied. For data that adhered to parametric assumptions, a paired t-test was performed with a 95% confidence interval. For non-parametric data, the Wilcoxon signed-rank test was employed. The significance level was set at 0.05 for all statistical analyses.
3 Results
3.1 Baseline characteristics
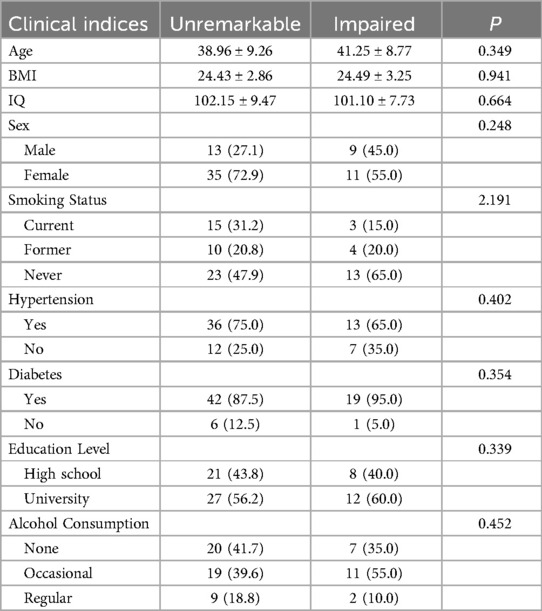
Baseline characteristics showed no significant differences between the Unremarkable and Impaired groups, confirming comparability (Table 1). The mean age was 38.96 ± 9.26 years in the Unremarkable group and 41.25 ± 8.77 years in the Impaired group (P = 0.349), with similar BMI (24.43 ± 2.86 vs. 24.49 ± 3.25, P = 0.941) and IQ (102.15 ± 9.47 vs. 101.10 ± 7.73, P = 0.664). Sex distribution was female-dominant in both groups (72.9% vs. 55.0%, P = 0.248). Current smoking was lower in the Impaired group (15.0%) than in the Unremarkable group (31.2%), while non-smoking rates were higher (65.0% vs. 47.9%) (P = 2.191). Hypertension (P = 0.402) and diabetes (P = 0.354) were evenly distributed. Education levels were comparable, with 43.8% vs. 40.0% having a high school education (P = 0.339). Alcohol consumption patterns were similar (P = 0.452), with occasional drinking more common in the Impaired group (55.0% vs. 39.6%). Overall, the lack of significant differences (P > 0.05) confirms well-matched groups, ensuring a valid comparison of postoperative outcomes.
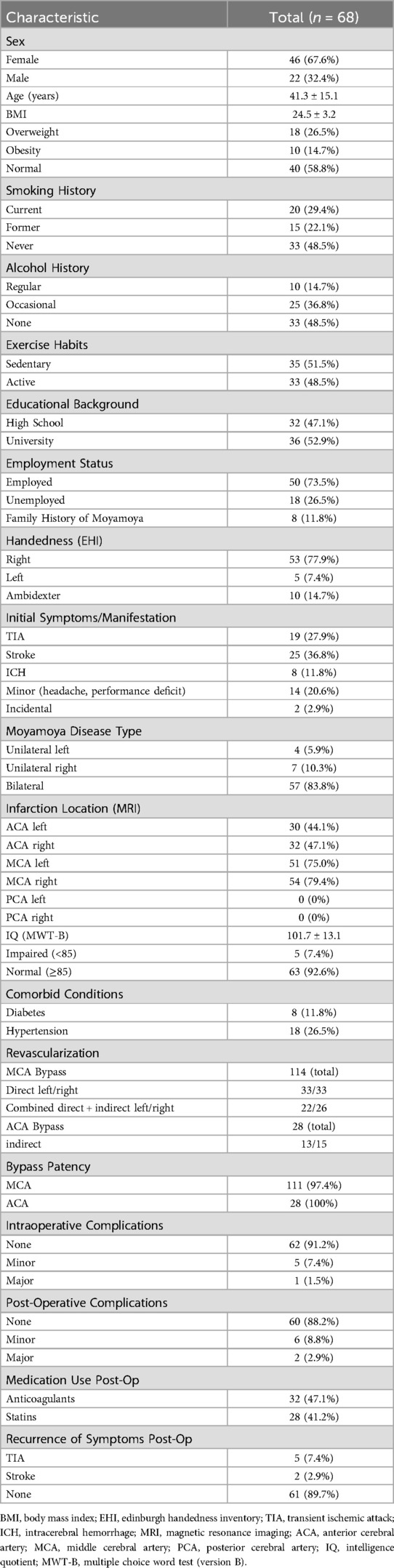
Preoperative characteristics revealed that 67.6% of the cohort were female, with an average age of 41.3 years (SD = 15.1). BMI categorized 26.5% of patients as overweight, 14.7% as obese, and 58.8% with normal weight. Smoking was active in 29.4%, with 22.1% as former smokers, and 48.5% as non-smokers. Alcohol consumption was regular in 14.7%, occasional in 36.8%, and absent in 48.5%. Physical inactivity was noted in 51.5%, and 52.9% had university degrees. Employment status showed 73.5% employed. Initial symptoms included TIA (27.9%), stroke (36.8%), ICH (11.8%), and minor symptoms (20.6%). Imaging revealed bilateral moyamoya in 83.8%. A total of 114 MCA bypasses and 28 ACA bypasses were performed with high patency. Postoperative outcomes were favorable, with 88.2% having no complications, and limited recurrence of TIA (7.4%) and stroke (2.9%). Detailed information was shown in Table 2.
3.2 Postoperative improvements in health-related quality of life evaluated by SF-36
Following revascularization, significant improvements in health-related quality of life (HRQOL) were observed across multiple domains in Chinese patients with moyamoya disease, as measured by the SF-36 scale. Among those classified as impaired preoperatively, physical functioning improved in 27.9% of patients, with scores rising from −2.59 ± 0.45 to −1.06 ± 0.50 (P < 0.05). General health also showed a notable increase, with scores improving from −2.89 ± 0.83 to −1.02 ± 1.04 in 47.1% of impaired patients (P < 0.05). Physical pain and physical role function improved significantly in 22.1% and 41.2% of patients with impairments, respectively, with physical pain scores improving from −1.94 ± 0.30 to −0.50 ± 0.43 (P < 0.05), and physical role function showing substantial gains from −2.29 ± 0.43 to −0.84 ± 0.50 (P < 0.05). Psychological well-being and emotional role function similarly showed improvements, with psychological well-being scores rising in 33.8% of impaired patients from −2.06 ± 0.35 to −0.59 ± 0.46 (P < 0.05), and emotional role function improving in 36.8% of patients from −3.18 ± 0.46 to −1.50 ± 0.64 (P < 0.05). Social functioning improved in 27.9% of those classified as impaired, with scores rising from −2.58 ± 0.24 to −1.12 ± 0.38 (P < 0.05), while vitality saw the greatest enhancement, with scores increasing from −1.33 ± 0.21 to −0.04 ± 0.41 in 38.2% of impaired patients (P < 0.05). In contrast, patients classified as unremarkable preoperatively did not exhibit significant changes postoperatively. Detailed information is presented in Table 3.
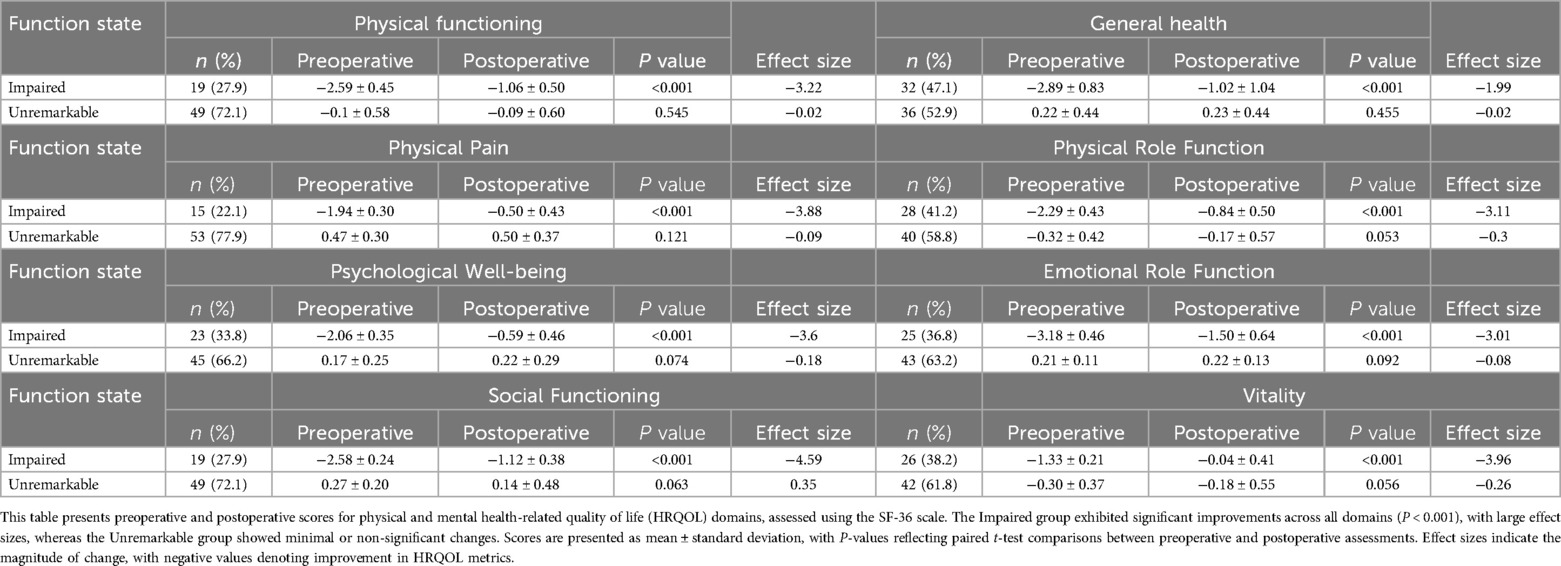
Table 3. Postoperative improvements in health-related quality of life (HRQOL) in Chinese patients with moyamoya disease, evaluated by the SF-36 scale.
3.3 Postoperative improvements in health-related quality of life evaluated by SCL-90
Meanwhile, significant improvements in psychological outcomes were observed after revascularization, as measured by the SCL-90 scale. Among patients classified as impaired preoperatively, aggressiveness improved in 19.1%, with scores decreasing from 66.26 ± 2.91 to 64.21 ± 2.85 (P < 0.001). Anxiety also showed a notable decrease in 29.4% of impaired patients, with scores improving from 67.23 ± 4.33 to 64.30 ± 4.63 (P < 0.001). Obsessiveness and paranoid thinking demonstrated similar improvements. Obsessed patients (39.7%) showed a decrease in scores from 65.91 ± 1.45 to 62.00 ± 2.97 (P < 0.001), while those with paranoid thinking (8.8%) improved from 62.02 ± 0.95 to 58.50 ± 4.25 (P = 0.05). Insecurity improved in 7.4% of patients, with scores dropping from 67.94 ± 1.82 to 65.47 ± 3.55, which is not statistically significant (P = 0.05). Somatization showed a marked decrease in 32.4% of impaired patients, with scores improving from 64.16 ± 2.62 to 56.61 ± 3.56 (P < 0.001). Psychoticism improved significantly in 41.2% of patients, with scores decreasing from 63.33 ± 1.72 to 56.09 ± 2.09 (P < 0.001). Phobic-anxiety showed a slight improvement in 22.1% of patients, with scores decreasing from 65.91 ± 2.60 to 64.18 ± 3.46, though this change was not statistically significant (P = 0.051). In contrast, patients classified as unremarkable preoperatively showed no significant changes postoperatively. Detailed information was presented in Table 4.
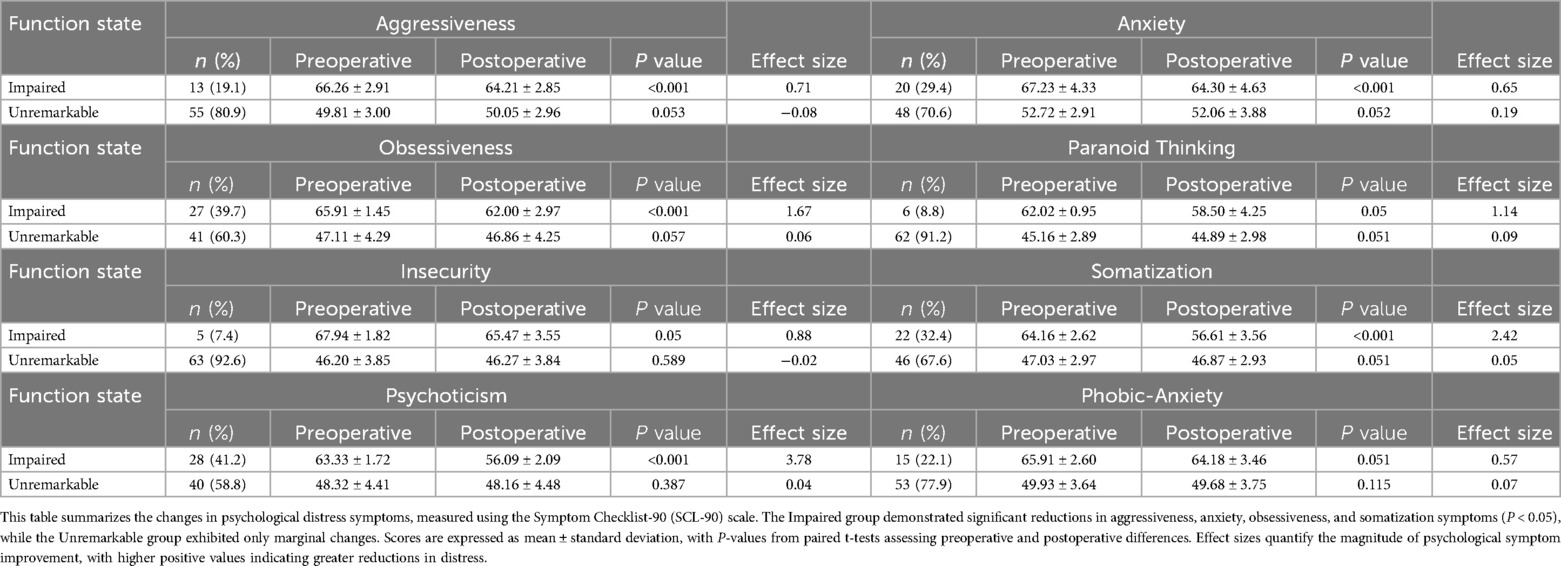
Table 4. Postoperative improvements in psychological outcomes in Chinese patients with moyamoya disease, evaluated by the SCL-90 scale.
3.4 Postoperative improvements in depression
After revascularization, participants experienced marked reductions in depressive symptoms, as assessed by the BDI-II and the depression component of the SCL-90 scale. Among the 29.4% of patients (n = 20) classified as impaired preoperatively, BDI-II scores significantly decreased from 19.45 ± 3.03 to 12.01 ± 3.59 postoperatively (P < 0.001). In contrast, no significant change was observed in the 70.6% of patients (n = 48) classified as unremarkable (P = 0.051). Similarly, the depression item of the SCL-90 improved in 32.4% of impaired patients (n = 22), with scores decreasing from 64.60 ± 2.67 to 59.86 ± 3.27 postoperatively (P < 0.001). No significant changes were noted in the 67.6% of patients (n = 46) with unremarkable preoperative scores (P = 0.494). These results indicate that revascularization significantly reduces depressive symptoms in patients with preoperative impairments. Detailed results are presented in Table 5.
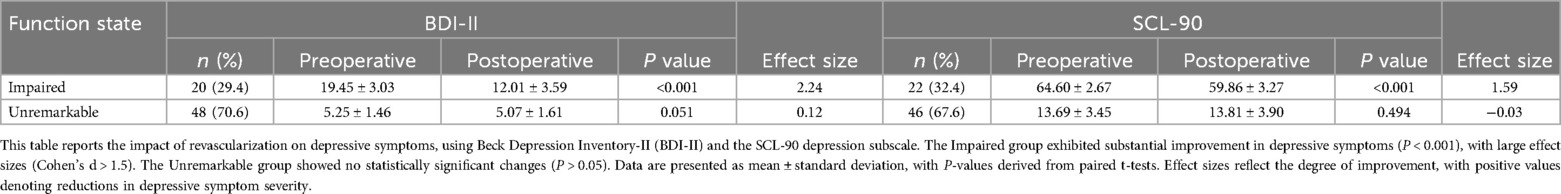
Table 5. Postoperative improvements in depressive symptoms in Chinese patients with moyamoya disease, evaluated by the BDI-II and SCL-90 scales.
3.5 Postoperative improvements in executive function
In this study, executive function was evaluated in Chinese patients with moyamoya disease before and after revascularization using the Trail Making Test A (TMTA), Trail Making Test B (TMTB), Chapuis Maze (CM) score, and Digit D2 (D2) score. Among patients classified as impaired preoperatively, TMTA scores improved significantly in 45.6% of patients, with values rising from −3.08 ± 1.11 to −1.10 ± 1.21 postoperatively (P < 0.001). Similarly, TMTB scores improved in 47.1% of impaired patients, increasing from −2.31 ± 0.67 to −0.38 ± 0.72 (P < 0.001). Chapuis Maze performance showed a modest, non-significant improvement in 44.1% of impaired patients, with scores increasing from 6.19 ± 3.10 to 6.54 ± 3.19 (P = 0.094). In contrast, significant gains were observed in the Digit D2 scores, with 42.6% of impaired patients improving from 81.44 ± 2.06 to 86.54 ± 3.06 postoperatively (P < 0.001). Patients classified as unremarkable preoperatively did not experience notable changes postoperatively, as reflected by non-significant differences in scores for TMTA (P = 0.597), TMTB (P = 0.7), CM (P = 0.641), and D2 (P = 0.068). Detailed information is presented in Table 6.
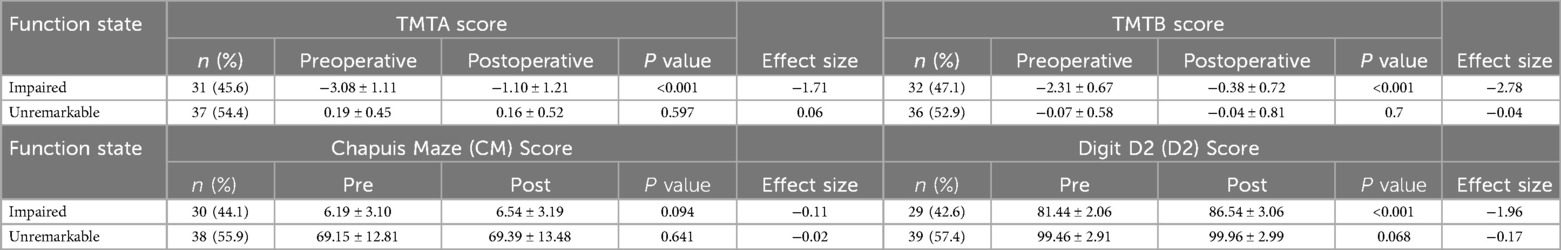
Table 6. Postoperative improvements in executive function in Chinese patients with moyamoya disease, evaluated by TMTA, TMTB, chapuis maze, and digit D2.
4 Discussion
Moyamoya disease (MMD) is a chronic cerebrovascular disorder that predominantly affects East Asian populations, including Chinese individuals, leading to significant risks of stroke, cognitive impairment, and diminished HRQOL (19, 20). While revascularization surgery has been established as an effective intervention to restore cerebral perfusion and reduce ischemic events, its impact on neuropsychological recovery and HRQOL remains variable. This study aimed to evaluate the psychological outcomes and HRQOL in Chinese patients with MMD following revascularization surgery. The findings demonstrate significant improvements across multiple domains, particularly in those patients who exhibited preoperative impairments in executive function, psychological well-being, and HRQOL.
The results indicated substantial improvements in physical functioning, general health, and emotional role functioning among patients with preoperative impairments. Specifically, 27.9% of patients exhibited enhanced physical functioning, and 47.1% showed improved general health, consistent with findings from previous studies that have linked improved cerebral perfusion with better physical outcomes post-revascularization (7, 21). The improvements in physical pain and role function also align with research suggesting that revascularization alleviates the physical burden of recurrent ischemic events (22, 23). However, unlike studies reporting mixed results in mental health domains, this study found significant gains in psychological well-being, emotional role functioning, and vitality. This discrepancy may be attributed to differences in cultural perceptions of health and the specific neuropsychological interventions provided in the Chinese healthcare context, which emphasize both physical recovery and emotional support (24, 25). Interestingly, patients classified as “unremarkable” preoperatively did not show significant changes postoperatively, reinforcing the hypothesis that surgical interventions primarily benefit those with pre-existing deficits. This outcome is consistent with the literature suggesting that cognitive recovery is most pronounced in patients who exhibit measurable impairments prior to revascularization (10, 26).
Moreover, the improvements in psychological outcomes, particularly reductions in anxiety, obsessiveness, aggressiveness, and somatization, suggest that revascularization has a profound impact on emotional regulation in MMD patients. This may be partly explained by the restoration of cerebral blood flow to areas of the brain responsible for emotional control, such as the prefrontal cortex and amygdala (27, 28). The observed decrease in depression symptoms, as reflected in both the BDI-II and SCL-90, is noteworthy. Depression is a common comorbidity in MMD, often exacerbated by chronic hypoperfusion (29, 30). The reduction in depressive symptoms in 29.4% of patients is consistent with research highlighting the psychological benefits of revascularization in cerebrovascular disorders (31). These findings support the notion that improving cerebral perfusion can have a cascading effect on psychological health, reducing the emotional distress that often accompanies chronic illness. Nevertheless, the limited improvements in phobic-anxiety and insecurity scores indicate that not all psychological symptoms are equally responsive to surgical intervention. This suggests the need for adjunctive therapies, such as cognitive-behavioral therapy (CBT), to address persistent anxiety and insecurity (32, 33).
The significant postoperative improvements in executive function, as measured by the Trail Making Test (TMT) and Digit D2 tests, underscore the cognitive benefits of revascularization in MMD patients. Executive dysfunction in MMD is thought to result from chronic cerebral hypoperfusion, particularly in frontal lobe regions (23, 34). The observed improvements in TMTA and TMTB scores in 45.6% and 47.1% of impaired patients, respectively, suggest that revascularization can restore higher-order cognitive processes such as attention, task-switching, and problem-solving. These findings are consistent with studies that have shown similar improvements in cognitive function following revascularization, particularly in younger patients or those undergoing early intervention (15, 35–37). However, the lack of significant change in the Chapuis Maze (CM) test highlights a potential limitation in the extent of cognitive recovery. Spatial navigation deficits, which are often linked to hippocampal damage, may not fully resolve despite improved blood flow, as the hippocampus is highly susceptible to ischemic injury (38–40). This underscores the importance of neuroprotective strategies to preserve cognitive function during the chronic phases of MMD.
This study is the first to systematically investigate the psychological outcomes and HRQOL changes in Chinese patients with MMD following revascularization surgery, addressing a significant gap in the current literature. By applying stringent inclusion and exclusion criteria, this study excluded patients with significant psychiatric comorbidities and advanced cognitive impairments, ensuring the homogeneity of the study sample and enhancing the validity and reliability of the findings. Additionally, the use of multiple validated psychological and cognitive assessment tools, such as the SCL-90, BDI-II, SF-36, and Trail Making Test (TMT), allowed for a comprehensive evaluation of changes in patients' psychological and cognitive functions, ensuring a more accurate understanding of the impact of surgery on their quality of life and mental health.
5 Limitations
However, this study has several limitations. This retrospective study relies on past records, introducing selection bias as only patients who underwent surgery were included, likely those with severe symptoms or better adherence. This limits generalizability, especially to milder cases or non-surgical patients. To mitigate bias, we defined clear inclusion/exclusion criteria and controlled for confounders where possible. However, prospective cohorts or RCTs are needed for stronger causal inference. As a single-center study, institutional/regional factors may further impact external validity. Future multi-center studies could improve generalizability. Additionally, the one-year follow-up may not capture long-term cognitive and psychological outcomes, necessitating further studies to assess whether improvements are sustained or if cognitive decline recurs.
This study employs the SCL-90 and BDI-II to assess psychological distress in Chinese Moyamoya patients, but cultural differences in emotional expression may affect their accuracy. While Western populations primarily report emotional symptoms like sadness, Chinese individuals often express distress through somatic complaints (e.g., fatigue, dizziness), potentially leading to underreporting of depression. Though validated in Chinese populations, these tools may not fully capture culturally specific distress patterns—for instance, lower cognitive-affective scores but higher somatic symptom reports. To improve cultural sensitivity, future studies should consider China-specific scales (e.g., SDS), qualitative interviews, or structured clinical assessments. While SCL-90 and BDI-II remain valid, their cultural adaptability is a limitation, warranting further refinement for Chinese patients.
6 Conclusion
In summary, this study demonstrates that revascularization surgery leads to significant improvements in HRQOL, psychological well-being, and executive function in Chinese patients with MMD, particularly among those with preoperative impairments. These findings provide strong evidence for the broader therapeutic benefits of revascularization beyond stroke prevention, highlighting its potential to alleviate the cognitive and emotional burden of MMD. Further research is needed to explore the long-term sustainability of these benefits and the potential role of adjunctive therapies in optimizing patient outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The study was approved by the Ethics Committee of the Nanjing Drum Tower Hospital Affiliated to Nanjing University Medical School. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants' legal guardians/next of kin because Written informed consent was waived due to the retrospective nature of this study.
Author contributions
HL: Formal analysis, Validation, Writing – original draft. PY: Formal analysis, Validation, Writing – original draft. TX: Investigation, Validation, Writing – review & editing. ChJ: Investigation, Validation, Writing – review & editing. CuJ: Conceptualization, Funding acquisition, Methodology, Resources, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the Key projects of nursing scientific research in 2024 in Nanjing Drum Tower Hospital affiliated to Nanjing University School of Medicine (No. 2024-B722).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
MMD, moyamoya disease; TIA, transient ischemic attacks; HRQOL, health-related quality of life.
References
1. Berry JA, Cortez V, Toor H, Saini H, Siddiqi J. Moyamoya: an update and review. Cureus. (2020) 12:e10994. doi: 10.7759/cureus.10994
2. Fox BM, Dorschel KB, Lawton MT, Wanebo JE. Pathophysiology of vascular stenosis and remodeling in moyamoya disease. Front Neurol. (2021) 12:661578. doi: 10.3389/fneur.2021.661578
3. Zhang H, Zheng L, Feng L. Epidemiology, diagnosis and treatment of moyamoya disease. Exp Ther Med. (2019) 17:977–1984. doi: 10.3892/etm.2019.7198
4. Kim JS. Moyamoya disease: epidemiology, clinical features, and diagnosis. J Stroke. (2016) 18:2–11. doi: 10.5853/jos.2015.01627
5. Lei Y, Chen X, Su JB, Zhang X, Yang H, Gao XJ, et al. Recognition of cognitive impairment in adult moyamoya disease: a classifier based on high-order resting-state functional connectivity network. Front Neural Circuits. (2020) 14:603208. doi: 10.3389/fncir.2020.603208
6. Weinberg DG, Rahme RJ, Aoun SG, Batjer HH, Bendok BR. Moyamoya disease: functional and neurocognitive outcomes in the pediatric and adult populations. Neurosurg Focus. (2011) 30:E21. doi: 10.3171/2011.3.FOCUS1150
7. Guzman R, Lee M, Achrol A, Bell-Stephens T, Kelly M, Do HM, et al. Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J Neurosurg. (2009) 111:927–35. doi: 10.3171/2009.4.JNS081649
8. Yuan X, Yu H, Sun Z, Wu J, Gao L, Chong Z, et al. Evaluation of surgical revascularization procedure outcomes for adult Moyamoya disease: a computed tomography perfusion-based study. Insights Imaging. (2023) 14:18. doi: 10.1186/s13244-023-01519-1
9. Haas P, Kittelberger BB, Hurth H, Wang S, Tellermann J, Tatagiba M, et al. Health-related quality of life and neuropsychological outcome after EC-IC bypass revascularization in adult patients with moyamoya disease. Neurosurgery. (2024). doi: 10.1227/neu.0000000000002813
10. Uchida S, Kubo Y, Oomori D, Yabuki M, Kitakami K, Fujiwara S, et al. Long-term cognitive changes after revascularization surgery in adult patients with ischemic moyamoya disease. Cerebrovasc Dis Extra. (2021) 11:145–54. doi: 10.1159/000521028
11. Shen XX, Zhang HD, Fu HG, Xu JL, Zhang HT, Hou L, et al. Association of cognitive function and hypoperfusion in moyamoya disease patients without stroke. J Cereb Blood Flow Metab. (2023) 43:542–51. doi: 10.1177/0271678X221140349
12. Kim T, Oh CW, Bang JS, Kim JE, Cho WS. Moyamoya disease: treatment and outcomes. Stroke. (2016) 18:21–30. doi: 10.5853/jos.2015.01739
13. Oh W-O, Yeom I, Lim S-H, Kim DS, Shim KW. The moyamoya health behavior scale for adolescent patients: measurement tool development and psychometric evaluation. Int J Environ Res Public Health. (2021) 18:4064. doi: 10.3390/ijerph18084064
14. Zhang W, Pan Z, Zhu Y, Lv D, Zhang H, Li S, et al. Illness uncertainty, resilience, and perceived social support among patients with moyamoya disease: a cross-sectional study. Front Psychiatry. (2024) 15:1405594. doi: 10.3389/fpsyt.2024.1405594
15. El Naamani K, Chen CJ, Jabre R, Saad H, Grossberg JA, Dmytriw AA, et al. Direct versus indirect revascularization for moyamoya: a large multicenter study. J Neurol Neurosurg Psychiatry. (2024) 95:256–63. doi: 10.1136/jnnp-2022-329176
16. Fujimura M, Tominaga T, Kuroda S, Takahashi JC, Endo H, Ogasawara K, et al. 2021 Japanese guidelines for the management of moyamoya disease: guidelines from the research committee on moyamoya disease and Japan stroke society. Neurol Med Chir. (2022) 62:165–70. doi: 10.2176/jns-nmc.2021-0382
17. Haas P, Fudali M, Wang SS, Hurth H, Hauser TK, Ernemann U, et al. Quality of life impairment in adult moyamoya patients-preoperative neuropsychological assessment and correlation to MRI and H(2)(15)O PET findings. Neurosurg Rev. (2022) 45:1533–41. doi: 10.1007/s10143-021-01660-9
18. Roder C, Haas P, Fudali M, Milian M, Ernemann U, Meyer PT, et al. Neuropsychological impairment in adults with moyamoya angiopathy: preoperative assessment and correlation to MRI and H(2)(15)O PET. Neurosurg Rev. (2020) 43:1615–22. doi: 10.1007/s10143-019-01192-3
19. Sun Y, Zhou G, Feng J, Chen L, Liu G, Wang J, et al. Incidence and prevalence of moyamoya disease in urban China: a nationwide retrospective cohort study. Stroke Vasc Neurol. (2021) 6:615–23. doi: 10.1136/svn-2021-000909
20. Kappel AD, Feroze AH, Torio E, Sukumaran M, Du R. Management of moyamoya disease: a review of current and future therapeutic strategies. J Neurosurg. (2024) 141:975–82. doi: 10.3171/2024.1.JNS221977
21. Zhang K, Ren W, Sun YX, Wang XJ, Li CY, Wang ZL, et al. Angiographic characteristics of cerebral perfusion and hemodynamics of the bridging artery after surgical treatment of unilateral Moyamoya disease. Front Neurosci. (2022) 16:922482. doi: 10.3389/fnins.2022.922482
22. Teo M, Abhinav K, Bell-Stephens TE, Madhugiri VS, Sussman ES, Azad TD, et al. Short- and long-term outcomes of moyamoya patients post-revascularization. J Neurosurg. (2023) 138:1374–84. doi: 10.3171/2022.8.JNS22336
23. Nakamizo A, Kikkawa Y, Hiwatashi A, Matsushima T, Sasaki T. Executive function and diffusion in frontal white matter of adults with moyamoya disease. J Stroke Cerebrovasc Dis. (2014) 23:457–61. doi: 10.1016/j.jstrokecerebrovasdis.2013.03.022
24. Sit HF, Ling R, Lam AIF, Chen W, Latkin CA, Hall BJ. The cultural adaptation of step-by-step: an intervention to address depression among Chinese young adults. Front Psychiatry. (2020) 11:650. doi: 10.3389/fpsyt.2020.00650
25. Guo Z, Zeng S, Ling K, Chen S, Yao T, Li H, et al. Experiences and needs of older patients with stroke in China involved in rehabilitation decision-making: a qualitative study. BMC Med Inform Decis Mak. (2024) 24(1):330. doi: 10.1186/s12911-024-02735-5
26. Kronenburg A, Van Den Berg E, Van Schooneveld MM, Braun KPJ, Calviere L, van der Zwan A, et al. Cognitive functions in children and adults with moyamoya vasculopathy: a systematic review and meta-analysis. J Stroke. (2018) 20:332–41. doi: 10.5853/jos.2018.01550
27. Wei J, Zhong P, Qin L, Tan T, Yan Z. Chemicogenetic restoration of the prefrontal Cortex to amygdala pathway ameliorates stress-induced deficits. Cereb Cortex. (2018) 28:1980–90. doi: 10.1093/cercor/bhx104
28. Banks SJ, Eddy KT, Angstadt M, Nathan PJ, Phan KL. Amygdala–frontal connectivity during emotion regulation. Soc Cogn Affect Neurosci. (2007) 2:303–12. doi: 10.1093/scan/nsm029
29. Oakley CI, Lanzino G, Klaas JP. Neuropsychiatric symptoms of moyamoya disease: considerations for the clinician. Neuropsychiatr Dis Treat. (2024) 20:663–9. doi: 10.2147/NDT.S440975
30. Mansuri Z, Patel K, Trivedi C, Desai S, Patel S, Desai R, et al. Burden of psychiatric disorders in Moyamoya disease: a national inpatient perspective from 2007 to 2014. Prim Care Companion CNS Disord. (2022) 24:21m03157. doi: 10.4088/PCC.21m03157
31. Gallego Moyano FD, Janssen HC, Venkatraghavan L, Mikulis DJ, Andrade Barazarte H, Radovanovic I, et al. The impact of revascularization surgery on headaches in association with cerebrovascular reactivity in patients with moyamoya angiopathy. Brain Sci. (2024) 14:967. doi: 10.3390/brainsci14100967
32. Carpenter JK, Andrews LA, Witcraft SM, Powers MB, Smits JAJ, Hofmann SG. Cognitive behavioral therapy for anxiety and related disorders: a meta-analysis of randomized placebo-controlled trials. Depress Anxiety. (2018) 35:502–14. doi: 10.1002/da.22728
33. Scott AJ, Bisby MA, Heriseanu AI, Salameh Y, Karin E, Fogliati R, et al. Cognitive behavioral therapies for depression and anxiety in people with chronic disease: a systematic review and meta-analysis. Clin Psychol Rev. (2023) 106:102353. doi: 10.1016/j.cpr.2023.102353
34. Kang CG, Chun MH, Kang JA, Do KH, Choi SJ. Neurocognitive dysfunction according to hypoperfusion territory in patients with Moyamoya disease. Ann Rehabil Med. (2017) 41:1–8. doi: 10.5535/arm.2017.41.1.1
35. Tsiakiri A, Christidi F, Tsiptsios D, Vlotinou P, Kitmeridou S, Bebeletsi P, et al. Processing speed and attentional shift/mental flexibility in patients with stroke: a comprehensive review on the trail making test in stroke studies. Neurol Int. (2024) 16:210–25. doi: 10.3390/neurolint16010014
36. Mitchell DL, Shlobin NA, Lopresti MA, Scoville JP, Winterhalter E, Lam S. Post-surgical cognitive outcomes of Moyamoya disease: a systematic review. World Neurosurg. (2023) 178:181–190.e1. doi: 10.1016/j.wneu.2023.07.099
37. Shim KW, Park EK, Kim JS, Kim DS. Cognitive outcome of pediatric Moyamoya disease. J Korean Neurosurg Soc. (2015) 57:440–4. doi: 10.3340/jkns.2015.57.6.440
38. Goodroe SC, Starnes J, Brown TI. The Complex nature of hippocampal-striatal interactions in spatial navigation. Front Hum Neurosci. (2018) 12:250. doi: 10.3389/fnhum.2018.00250
39. Guderian S, Dzieciol AM, Gadian DG, Jentschke S, Doeller CF, Burgess N, et al. Hippocampal volume reduction in humans predicts impaired allocentric spatial memory in virtual-reality navigation. J Neurosci. (2015) 35:14123–31. doi: 10.1523/JNEUROSCI.0801-15.2015
Keywords: editing moyamoya disease, revascularization, psychological outcomes, health-related quality of life, executive function
Citation: Liang H, Yuan P, Xu T, Jin C and Ji C (2025) Psychological outcomes and health-related quality of life changes in Chinese patients with moyamoya disease after revascularization. Front. Surg. 12:1573992. doi: 10.3389/fsurg.2025.1573992
Received: 10 February 2025; Accepted: 31 March 2025;
Published: 11 April 2025.
Edited by:
Shihao He, Peking Union Medical College Hospital (CAMS), ChinaReviewed by:
Yifan Xu, The Affiliated Hospital of Qingdao University, ChinaAnqi Li, Capital Medical University, China
Copyright: © 2025 Liang, Yuan, Xu, Jin and Ji. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Cuiling Ji, b3JzY2p1NDc5QDE2My5jb20=
 Haijuan Liang
Haijuan Liang Cuiling Ji
Cuiling Ji