- 1Department of Otolaryngology, The 971st Hospital of Chinese People’s Liberation Army, Qingdao, China
- 2Department of Ward of eye, Otolaryngology and Stomatology, The 971st Hospital of Chinese People’s Liberation Army, Qingdao, China
- 3Department of Otolaryngology, Qingdao Municipal Hospital, Qingdao, China
Objective: To construct a nomogram prediction model based on the risk factors of complications after augmentation rhinoplasty with autogenous granular costal cartilage through closed approach, and to explore its clinical application value.
Methods: From June 2022 to June 2024, 214 patients in our hospital were selected and divided into training set (n = 150) and verification set (n = 64) according to the ratio of 7:3. In the training set, the risk factors of postoperative complications were analyzed by multivariate Logistic regression, and then the nomogram prediction model was constructed. The prediction efficiency of the model is evaluated by drawing ROC curve and calibration curve, and verified in the verification set. The decision curve analysis (DCA) was used to evaluate the clinical application value of the model.
Results: Complications occurred in 31 cases (20.67%) in the training group and 13 cases (20.31%) in the verification group. There was no significant difference in the incidence and clinical characteristics between the two groups (P > 0.05). In the training set, older age, history of chronic diseases (chronic rhinitis), long operation time, large amount of bleeding during operation and thin skin on the back of nose were independent risk factors for complications (P < 0.05), and a nomogram prediction model was established accordingly. The model has good calibration and fitting degree in training set and verification set (C-index index is 0.857 and 0.848, average absolute error is 0.126 and 0.090, and χ2 of Hosmer-Lemeshow test is 7.137, P = 0.521 and χ2 = 5.923, P = 0.655). The ROC curve shows that the AUC of the training set and the validation set model for predicting postoperative complications are 0.851(95% CI: 0.764–0.937) and 0.855(95% CI: 0.675–1.000), and the sensitivity and specificity are 0.880, 0.725, 0.833 and 0.692, respectively.
Conclusion: The nomogram prediction model based on risk factors is helpful for early prediction of complications after augmentation rhinoplasty, providing guidance for clinical decision-making, helping to reduce the risk of complications and improving the surgical effect and patient satisfaction.
1 Introduction
The nose occupies a core position in facial aesthetics, and its shape has a far-reaching impact on the overall coordination of appearance. With the improvement of people's living standard and the change of aesthetic concept, the demand for rhinoplasty is increasing as an effective means to improve the shape of the nose (1). With its unique advantages, such as using its own tissue to avoid rejection, and the relatively hidden wound is conducive to recovery, the closed approach autologous granular costal cartilage augmentation rhinoplasty has been widely used in clinical practice (2). However, any operation is accompanied by certain risks, and the closed approach autologous granular costal cartilage augmentation rhinoplasty is no exception. Postoperative complications may occur, such as infection, cartilage displacement or absorption, skin redness, incision dehiscence and so on. These complications may not only make patients suffer additional physical pain and affect the recovery of nasal appearance, but also lead to psychological burden and reduce the quality of life in severe cases (3). At the same time, the occurrence of complications may also increase the medical cost and the potential risk of doctor–patient disputes. At present, the research on the postoperative complications of this operation is relatively scarce, and the related influencing factors are not completely clear. This makes it difficult for clinicians to accurately assess the surgical risk of each patient before surgery, to take effective preventive measures against potential risks during surgery, and to formulate personalized nursing plans after surgery to reduce the probability of complications (4). Therefore, it is an important problem to explore the influencing factors of postoperative complications and build a scientific and effective prediction model. As a visual forecasting tool, nomogram can integrate multiple influencing factors and predict the probability of events in an intuitive and understandable graphic way, which has been successfully applied to the risk prediction of many diseases in the medical field. It is expected to provide a convenient and efficient risk assessment method for clinicians by introducing it into the study of complications after augmentation rhinoplasty with autogenous granular costal cartilage through closed approach (5). Through the comprehensive analysis of patients' individual situation, the risk of complications can be accurately predicted, to guide doctors to formulate more reasonable surgical plans, optimize perioperative management, realize personalized medical care, minimize the risk of complications, improve the success rate of surgery, and protect patients' physical and mental health.
2 Materials and methods
2.1 Study population
Retrospective collection of clinical data from 214 patients who underwent closed approach autologous rib cartilage rhinoplasty in our plastic and cosmetic surgery department from June 2022 to June 2024. Inclusion criteria: 1. age between 18 and 50 years old, 2. first time receiving closed approach autologous granular rib cartilage rhinoplasty, 3. complete clinical data. Exclusion criteria: 1. concurrent severe dysfunction of important organs such as heart, liver, and kidney, 2. suffering from hematological disorders or abnormal coagulation function, 3. there are acute and chronic infectious diseases in the nose, 4. having mental illness or cognitive impairment, unable to cooperate with postoperative follow-up. The patients were divided into a training set (n = 150) and a validation set (n = 64) at a ratio of 7:3 using the random number table method. This study was approved by the hospital's ethics committee, and all patients signed informed consent forms.
2.2 Surgical methods
All surgeries are performed by the same experienced team of plastic surgeons. The patient is placed in a supine position, and after successful general anesthesia, a 2–3 cm incision is made on the surface of the 6th and 7th rib cartilage on the right side. The skin, subcutaneous tissue, and rib cartilage membrane are sequentially cut open, and an appropriate amount of rib cartilage is obtained by blunt dissection. Carefully trim the cut rib cartilage into particles of appropriate size and place them in physiological saline solution for later use. Make an incision at the base of the nasal columella or the inner edge of the nostril, carefully separate the fascial cavity of the nasal dorsum, evenly fill the prepared autologous granular rib cartilage in the nasal dorsum and nasal tip areas, adjust the shape to satisfaction, and then suture the incision layer by layer. Postoperative routine placement of drainage strips and pressure bandaging. During the dissection process, special attention is paid to avoiding damage to the intercostal nerves and the nerve branches innervating the serratus anterior muscle. The intramuscular nerve distribution of the serratus anterior muscle, as detailed by Yi et al. (6), provides critical anatomical guidance for this procedure—accurate knowledge of these neural pathways helps minimize iatrogenic nerve injury, thereby reducing the risk of donor-site complications such as chronic chest wall pain.
2.3 Definition of postoperative complications
Postoperative complications in closed approach autologous granular rib cartilage rhinoplasty were categorized and defined as follows: 1. early postoperative complications: infection (cellulitis or abscess formation confirmed clinically), hematoma/seroma (localized blood/fluid collection requiring intervention), skin redness/swelling (persistent inflammation >2 weeks), incision dehiscence (wound separation needing resuturing) and prolonged pain/hypersensitivity (>1 month). 2. Graft-related complications: cartilage resorption [quantified by 3D volumetric analysis as mild (<20%), moderate (20%–50%), or severe (>50%)], displacement/malposition (radiographic/clinical evidence of graft shifting), visibility/irregularities (palpable/visible contour issues), overcorrection/undercorrection (aesthetic imbalance) and fracture/fragmentation. 3. Donor-site complications: chest wall deformity, chronic pain, and pneumothorax. 4. Functional/aesthetic concerns: nasal obstruction, asymmetry, skin necrosis, and hypertrophic scarring. 5. Systemic complications: deep vein thrombosis (DVT), pulmonary embolism (PE) and anaphylaxis. Patients who experienced any of the above complications were included in the complication group. Otherwise, they were classified as the no-complication group.
2.4 Data collection
Collect detailed general information of patients, including age, gender, height, weight, smoking history, alcohol consumption history, chronic medical history (chronic rhinitis/rhinitis); Surgical related information, such as surgery time, intraoperative blood loss, cartilage granule filling amount, rib cartilage extraction amount; Preoperative nasal basic conditions (including nasal dorsal skin thickness, nasal facial angle, nasal frontal angle, nasal labial angle, nasal columella upper lip angle, nasal tip protrusion); Postoperative nursing compliance is classified into good compliance and poor compliance based on a comprehensive evaluation of the patient's nursing cooperation during the postoperative follow-up process. All patients were followed up regularly after surgery, with a total follow-up period of 6 months. The follow-up schedule was as follows: once a week within 1 month after surgery, once every 2 weeks from 1 to 3 months after surgery, and once a month from 3 to 6 months after surgery. During the follow-up period, all complications were recorded, including early complications (occurring within 1 month after surgery) and late complications (occurring from 1 month to 6 months after surgery, such as delayed cartilage resorption, and displacement).
2.5 Statistical analysis
Data were analyzed using SPSS 26.0 and R 4.2.3. Continuous variables were reported as mean ± standard deviation (SD) (if normally distributed, assessed by Shapiro–Wilk test) or median (interquartile range, Q1, Q3) (for non-normally distributed data), with between-group comparisons using independent t-tests or Mann–Whitney U tests, respectively. Categorical variables were compared via chi-square tests or Fisher's exact tests, and count data were expressed as the number of cases (percentage). Multivariate Logistic regression analysis was used to screen the risk factors of complications, and the difference was statistically significant (P < 0.05), and variance inflation factors (VIF) were calculated to exclude multicollinearity (VIF threshold <5). The final predictors were incorporated into a nomogram developed using the R “rms” package. Model performance was rigorously evaluated through multiple approaches: discrimination was assessed via the area under the receiver operating characteristic (ROC) curve (AUC) with 95% confidence intervals derived from 1,000 bootstrap samples, along with sensitivity, specificity, and predictive values; calibration was examined using bootstrap-corrected calibration curves, Brier scores, Hosmer-Lemeshow goodness-of-fit test (P > 0.05 indicating good calibration), and calibration slope analysis; potential overfitting was addressed through optimism-adjusted performance metrics using bootstrap internal validation; and clinical utility was determined via decision curve analysis (DCA). All statistical tests were two-sided, with a significance level set at α = 0.05.
3 Results
3.1 Baseline characteristics in training set and validation set
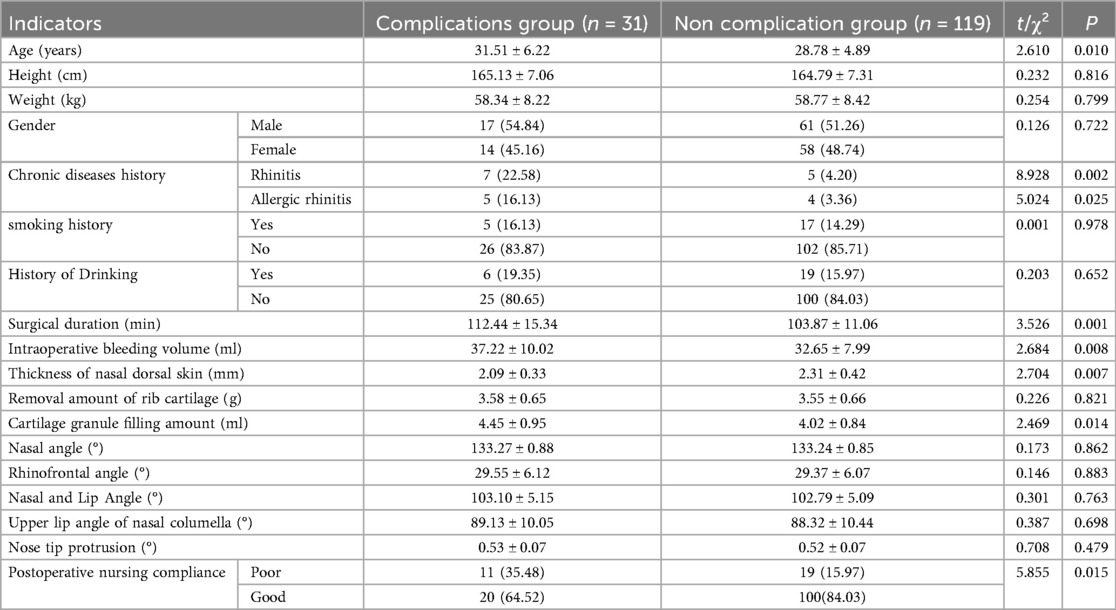
A total of 214 patients were included in the study. There were 31 cases (20.67%) of complications in the training set and 13 cases (20.31%) in the validation set. There was no statistically significant difference in the incidence of complications and clinical characteristics between the training set and the validation set (all P > 0.05) (Table 1).
3.2 Univariate analysis in the training set
In the training set, the results of univariate analysis showed that age, chronic medical history (chronic rhinitis), chronic medical history (allergic rhinitis), surgery time, intraoperative blood volume, thickness of nasal dorsal skin, cartilage granule filling amount and postoperative nursing compliance were associated with the occurrence of complications (all P < 0.05) (Table 2).
3.3 Multivariate logistic regression analysis in the training set
Multivariate logistic regression analysis was conducted with the occurrence of complications as the dependent variable, and factors with P < 0.05 in univariate analysis as independent variable. The results showed that age, chronic medical history (chronic rhinitis), long surgical time, excessive intraoperative bleeding, thin skin thickness on the nasal back, high cartilage granule filling volume and poor postoperative nursing compliance were independent risk factors for complications in patients undergoing closed approach autologous rib cartilage rhinoplasty (all P < 0.05) (Table 3). The tolerance of each variable in the regression model was >0.1, VIF was <10, conditional index was <30, and the variance ratio of multiple covariates under the same eigenvalue was >50%. Therefore, there was no collinearity among the covariates.
3.4 Construction of nomogram prediction model for postoperative complications
Based on the independent risk factors identified by multivariate logistic regression analysis, a nomogram prediction model of complications after closed approach autogenous costal cartilage augmentation rhinoplasty was constructed, and the independent risk factors in the model were assigned, and the total score of predicting complications was calculated, which was reflected by the probability of predicting complications. A higher total score indicates a greater predicted risk of postoperative complications (Figure 1).
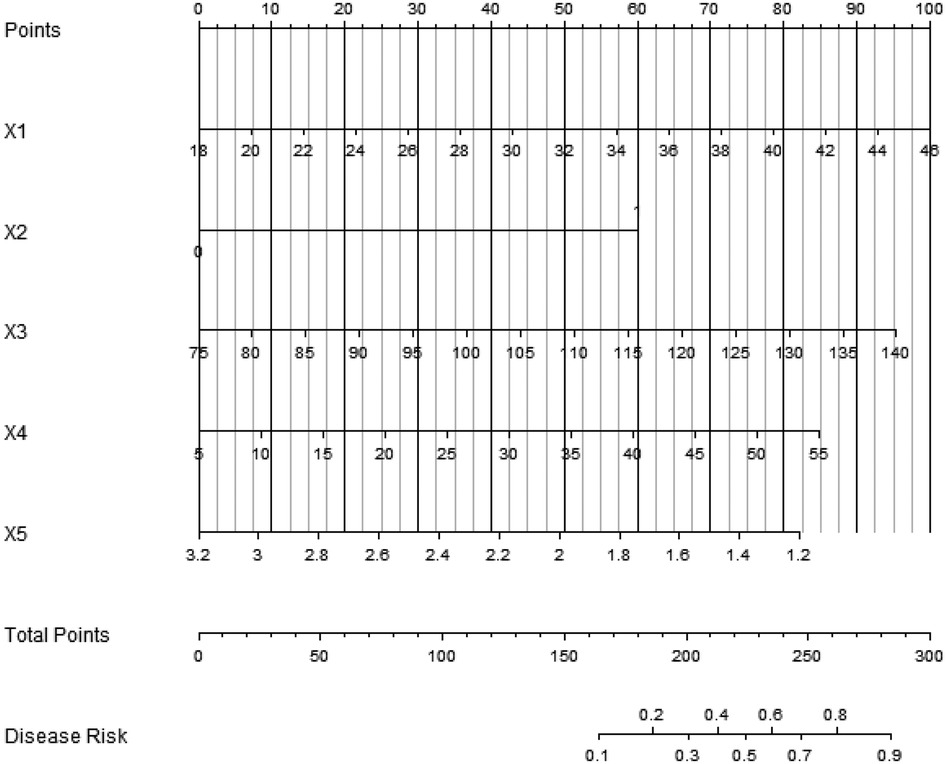
Figure 1. Nomogram prediction model of postoperative complications [X1: Age, X2: chronic medical history (chronic rhinitis), X3: surgical time, X4: intraoperative bleeding volume, X5: thickness of nasal dorsal skin].
3.5 Evaluation and validation of nomogram prediction model
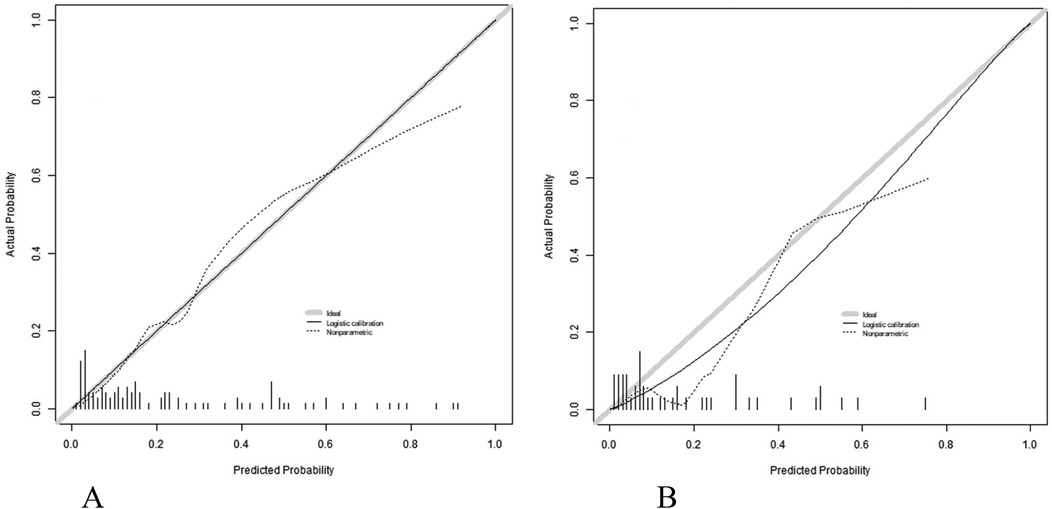
Nomogram model has good calibration and fitting degree in training set and validation set (C-index index is 0.857 and 0.848 respectively, the average absolute error of fitting degree between predicted value and real value is 0.126 and 0.090 respectively, and the results of Hosmer-Lemeshow test are χ2 = 7.137, P = 0.521 and χ2 = 5.923, P = 0.655 respectively (Figure 2). ROC curve shows that the AUC of Nomogram model in training set and validation set for predicting the complications after closed approach autogenous costal cartilage augmentation rhinoplasty is 0.851(95% CI: 0.764–0.937) and 0.855(95% CI: 0.675–1.000), respectively, and the sensitivity and specificity are 0.880, 0.725 and 0.833 (Figure 3).
3.6 Decision curve analysis of nomogram line prediction model
The decision curve analysis shows that when the threshold probability is about 0.10–0.90, the nomogram model constructed in this study has more clinical benefits than the decision that all patients have complications or all patients have no complications before operation (Figure 4).
4 Discussion
In this study, the risk factors of complications after closed approach autologous granular costal cartilage augmentation rhinoplasty were deeply analyzed, and a nomogram prediction model was successfully established. Through the research, it is found that older age, history of chronic diseases (chronic rhinitis, allergic rhinitis), long operation time, large amount of bleeding during operation, thin skin on the back of nose, large amount of cartilage particles and poor postoperative nursing compliance are independent risk factors for complications of patients undergoing this operation.
Age is one of the important factors affecting postoperative complications. With the increase of age, the physiological functions of human body gradually decline, the function of immune system declines and the ability of tissue repair weakens. In rhinoplasty, the wound healing speed of older patients is relatively slow and their anti-infection ability is reduced, which makes the risk of complications such as infection increase significantly (7). At the same time, the skin elasticity will deteriorate with age, which makes it difficult to fix and support the filled cartilage particles, and increases the possibility of cartilage displacement and absorption (8). Having a history of chronic diseases, especially chronic rhinitis, has a noticeable influence on the occurrence of complications after rhinoplasty. Chronic rhinitis will lead to chronic inflammation of nasal mucosa, impaired barrier function of mucosa and decreased resistance. When performing rhinoplasty, the surgical area relates to the nasal cavity, and inflammation is easy to spread to the surgical site, causing complications such as infection (9). In addition, frequent actions such as blowing your nose and sneezing in patients with rhinitis may affect the stability of the nose after operation, interfere with the normal healing of wounds, and further increase the incidence of complications (10). Long operation time is another key risk factor for postoperative complications. The prolonged operation time means that the operation will cause more trauma to the tissue and the operation area will be exposed to the air for a longer time, which greatly increases the chance of bacterial infection. Long-term operation may also damage the blood supply of local tissues and affect the repair and healing process of postoperative tissues. For example, during a long period of surgery, local tissues may be disordered in cell metabolism due to ischemia and hypoxia, which will affect the survival and growth of cartilage, thus causing complications such as cartilage absorption and displacement (11). The amount of intraoperative bleeding is also closely related to the occurrence of postoperative complications. Massive bleeding during operation may lead to the formation of local hematoma, which not only provides a good culture medium for the growth of bacteria, but also increases the risk of infection, and may also oppress surrounding tissues and affect local blood circulation. Blood circulation disorder will affect the nutrient supply of cartilage, lead to cartilage absorption and necrosis, and then affect the surgical effect. In addition, massive blood loss may also cause stress reaction of patients, affect immune system function, and indirectly increase the risk of complications (12, 13). Related research shows that the incidence of postoperative complications increases significantly when the amount of intraoperative bleeding exceeds a certain threshold. The thin skin thickness of nasal dorsum is an important anatomical factor affecting the effect and complications of rhinoplasty. The skin on the back of the nose is too thin to provide sufficient tissue coverage and protection for the filled cartilage particles (14, 15). In the process of postoperative recovery, thinner skin is more susceptible to external forces, leading to the displacement of cartilage particles (16, 17). At the same time, thin skin will reduce blood supply, which is not conducive to wound healing, and increase the risk of complications such as skin redness and ulceration (18, 19).
The nomogram prediction model constructed in this study shows good calibration and fitting degree in both training set and verification set, and the C-index index is 0.857 and 0.848, respectively, which shows that the model has good distinguishing ability and can well distinguish patients with and without complications. The area under ROC curve (AUC) is 0.851 in the training set and 0.855 in the verification set, which indicates that the model has high prediction efficiency. The analysis of decision curve shows that the nomogram model has obvious clinical benefits in predicting postoperative complications within a certain threshold probability range, and can provide valuable reference for clinical decision-making (20, 21). However, this study also has some limitations. This study only carried out internal verification, and did not carry out external verification. This is mainly because external verification needs to collect many case data from other medical institutions, and it faces many difficulties in actual operation, such as the differences in surgical operation norms and patient management modes of different medical institutions, and the difficulty in ensuring the accuracy and completeness of data collection. In addition, this study is a single-center study, and the representativeness of the sample may be limited. Follow-up research should actively carry out multi-center, large-sample research and external verification, to further verify and improve the nomogram prediction model and improve the accuracy and universality of the model (22). Thirdly, while we recorded detailed patient characteristics, the sample size precluded meaningful subgroup analyses that might have identified nuanced risk factors. Future multicenter studies with larger cohorts should incorporate predefined stratification by surgical history, systemic conditions, and technical variables to validate and extend our findings. Such investigations would help establish personalized risk prediction models for broader clinical application. Fourthly, the small severe complication cohort precluded meaningful severity-stratified analyses without compromising statistical power. While this binary approach ensures model robustness, future multicenter studies should prioritize larger samples to enable graded complication analyses (mild/moderate/severe) and refine risk stratification. In addition, all surgical indications in this series were purely aesthetic, with preoperative otolaryngologic examination confirming normal nasal function in all patients. While this provides a homogeneous population for analyzing aesthetic complication factors, the findings may not generalize to functional or reconstructive cases—an important direction for future study.
To address the limitation of lacking external validation, we plan to implement multi-center external validation study in the next 1–2 years. The specific roadmap includes: 1. collaborating with 3–5 tertiary hospitals with rich experience in rhinoplasty to ensure the generalizability of the model across different clinical settings; 2. establishing unified inclusion and exclusion criteria consistent with this study to minimize selection bias; 3. collecting a target sample size of at least 200 cases from collaborating centers, with detailed recording of variables included in the nomogram (age, chronic rhinitis history, surgical duration, intraoperative blood loss, nasal dorsal skin thickness) and postoperative complications; 4. validating the model using consistent statistical metrics (C-index, AUC, calibration curve, Hosmer-Lemeshow test) to evaluate its discrimination and calibration in external populations; 5. adjusting the model parameters if necessary based on external validation results to optimize its adaptability to diverse clinical scenarios. This multi-center external validation aims to confirm the model's generalizability and prepare it for clinical use. By including diverse hospitals (e.g., from northern, eastern, and southern China) with varying patient demographics, surgical practices, and care protocols, we ensure robustness across different settings. Subgroup analyses by institution type and region will further reduce bias, strengthening the model's real-world applicability.
To sum up, this study analyzed the clinical data of 214 patients who underwent closed approach autogenous costal cartilage augmentation rhinoplasty, and determined that older age, history of chronic diseases (chronic rhinitis), long operation time, large amount of blood loss during operation and thin skin thickness on the back of nose were independent risk factors for postoperative complications. The nomogram prediction model based on these risk factors shows good calibration and discrimination in both training set and verification set, and has high prediction efficiency, which can provide a convenient and effective tool for clinicians to predict postoperative complications. This model is helpful for clinicians to make individualized risk assessment of patients before operation, and make reasonable surgical plan and perioperative nursing plan according to the specific situation of patients, to minimize the risk of complications and improve the surgical effect and patient satisfaction. Although there are some limitations in this study, it lays a foundation for the follow-up research. In the future, it is necessary to carry out multi-center and large-sample research and external verification, further improve the nomogram prediction model, make it play a greater role in clinical practice, and bring better treatment results to most patients.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Ethics Committee of the 971st Hospital of Chinese People's Liberation Army (Approval No. 202125). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YJ: Formal analysis, Writing – original draft, Data curation, Conceptualization, Visualization, Writing – review & editing. CZ: Software, Writing – review & editing, Investigation, Writing – original draft. JW: Methodology, Investigation, Writing – review & editing. XS: Investigation, Formal analysis, Writing – review & editing, Methodology. WC: Software, Writing – review & editing, Methodology, Supervision.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Seah TE, Ilankovan V. Rhinoplasty as an adjunct to orthognathic surgery: a review. Oral Maxillofac Surg Clin North Am. (2023) 35(1):115–26. doi: 10.1016/j.coms.2022.06.008
2. Yan D, Li S-H, Zhang A-L, Xiao Y, Huang Z-C. A clinical study of platelet-rich fibrin combined with autologous high-density fat transplantation in augmentation rhinoplasty. Ear Nose Throat J. (2023) 102(9):598–604. doi: 10.1177/01455613211016902
3. Chen H, Wang X, Deng Y. Complications associated with autologous costal cartilage used in rhinoplasty: an updated meta-analysis. Aesthetic Plast Surg. (2023) 47(1):304–12. doi: 10.1007/s00266-022-03075-3
4. Fu X, Yin C, Liang Y, Zhou R, Wang D, Wang C. Hybrid autologous costal cartilage grafting for augmentation rhinoplasty in Asian patients. J Craniofac Surg. (2023) 34(4):1320–4. doi: 10.1097/SCS.0000000000009281
5. Kauke-Navarro M, Knoedler L, Knoedler S, Deniz C, Stucki L, Safi A-F. Balancing beauty and science: a review of facial implant materials in craniofacial surgery. Front Surg. (2024) 11:1348140. doi: 10.3389/fsurg.2024.1348140
6. Yi KH, Lee JH, Kim HJ. Intramuscular nerve distribution of the Serratus anterior muscle: implications for Botulinum neurotoxin injection in myofascial pain syndrome. Toxins (Basel). (2022) 14(4):271. doi: 10.3390/toxins14040271
7. Joshi K, Hohman MH, Seiger E. SMAS Plication Facelift. [Updated 2023 Mar 01]. In: StatPearls [Internet]. Treasure Island, FL: StatPearls Publishing (2025).
8. Knoedler S, Knoedler L, Wu M, Haug V, Broer PN, Kauke-Navarro M, et al. Incidence and risk factors of postoperative complications after rhinoplasty: a multi-institutional ACS-NSQIP analysis. J Craniofac Surg. (2023) 34(6):1722–6. doi: 10.1097/SCS.0000000000009553
9. Chen Y, Hu J, Xing J, Li Y, Xu Y, Li N, et al. Complications following thread rhinoplasty. J Cosmet Dermatol. (2022) 21(10):4722–6. doi: 10.1111/jocd.15041
10. Cai Y, Goldberg AN, Chang JL. The nose and nasal breathing in sleep apnea. Otolaryngol Clin North Am. (2020) 53(3):385–95. doi: 10.1016/j.otc.2020.02.002
11. Chiang CA, Tan PC, Zhou SB. A reinforced framework construction technique using unilateral auricular cartilage in Asian rhinoplasty to prevent long-term nasal tip drooping. J Plast Reconstr Aesthet Surg. (2023) 85:134–42. doi: 10.1016/j.bjps.2023.07.001
12. Song Z, Dong W, Fan F. Complications of diced cartilage wrapped in blood products in rhinoplasty: a meta-analysis. J Craniofac Surg. (2023) 34(2):503–10. doi: 10.1097/SCS.0000000000008960
13. Avci H. The effect of different dose regimens of tranexamic acid in reducing blood loss in rhinoplasty: a prospective randomized controlled study. J Craniofac Surg. (2021) 32(5):e442–4. doi: 10.1097/SCS.0000000000007247
14. Cabbarzade C. Skin tensioning concept in rhinoplasty using a semifixed support mechanism. J Craniofac Surg. (2023) 34(1):e28–32. doi: 10.1097/SCS.0000000000008894
15. Kook WS, Ryu DH, Baek W, Kook HM, Jang YY, Lew DH. Prevention and resolution of silicone implant-related problems in secondary rhinoplasty using a cross-linked human acellular dermal matrix. Plast Reconstr Surg. (2023) 152(1):45–54. doi: 10.1097/PRS.0000000000010205
16. Daoud RM, Alelyani AA, Bakhamees BH, Almutairi RF, AlSufyani N, Ayoub AY, et al. Thin skin in rhinoplasty: considerations for camouflaging dorsal nasal irregularities. Cureus. (2024) 16(8):e66595. doi: 10.7759/cureus.66595
17. Lozada KN, Locketz GD, Becker DG. Supracrural ligament graft in rhinoplasty. Facial Plast Surg. (2021) 37(1):98–101. doi: 10.1055/s-0040-1714666
18. Erdur ZB, Öktem F, Inci E, Yener HM, Üstündağ A. Effect of nasal soft-tissue envelope thickness on postoperative healing process following rhinoplasty. J Craniofac Surg. (2021) 32(6):2193–7. doi: 10.1097/SCS.0000000000007697
19. In SM, An HG, Kim J-Y, Lee K-I. Columellar wound immediately after open rhinoseptoplasty treated with application of DuoDERM extra thin. J Craniofac Surg. (2021) 32(1):e98–9. doi: 10.1097/SCS.0000000000006782
20. Wang X, Dong W, Wang H, You J, Zheng R, Xu Y, et al. Predicting risk of infection after rhinoplasty with autogenous costal cartilage: a cohort study. Aesthetic Plast Surg. (2022) 46(4):1797–805. doi: 10.1007/s00266-021-02704-7
21. Wang X, Dong W, Han R, Zheng R, Xu Y, Fan F. Development of a nomogram for severe costal cartilage calcification: a cohort study. Ann Palliat Med. (2022) 11(8):2668–75. doi: 10.21037/apm-21-3114
Keywords: closed path, autologous granular rib cartilage, rhinoplasty, complication, nomogram
Citation: Ju Y, Wang J, Shi X, Chi W and Zhan C (2025) Analysis of influencing factors on postoperative complications of closed approach autologous granular rib cartilage rhinoplasty and construction and verification of nomogram. Front. Surg. 12:1599790. doi: 10.3389/fsurg.2025.1599790
Received: 25 March 2025; Accepted: 29 August 2025;
Published: 15 September 2025.
Edited by:
Giovanni Papa, University of Trieste, ItalyReviewed by:
Davide De Cicco, Istituto Stomatologico Italiano, ItalyMarcello Molle, University of Campania Luigi Vanvitelli, Italy
Kyu-Ho Yi, You&I Clinic, Republic of Korea
Copyright: © 2025 Ju, Wang, Shi, Chi and Zhan. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Chenguang Zhan, a3lyaWVheW91MTFAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Ye Ju
Ye Ju Jinlei Wang2,†
Jinlei Wang2,†