- 1Department of Neurosurgery, Sahlgrenska University Hospital, Gothenburg, Sweden
- 2Department of Translational Medicine—Hand Surgery, Lund University Sweden, Lund, Sweden
- 3Department of Molecular Medicine and Surgery, Karolinska Institutet, Stockholm, Sweden
Objectives: To assess the existence of international, scientifically validated methods for manual surgical skills training and assessment. The aim was to create a descriptive chronological summary of the existing evidence and conclusions in the included articles.
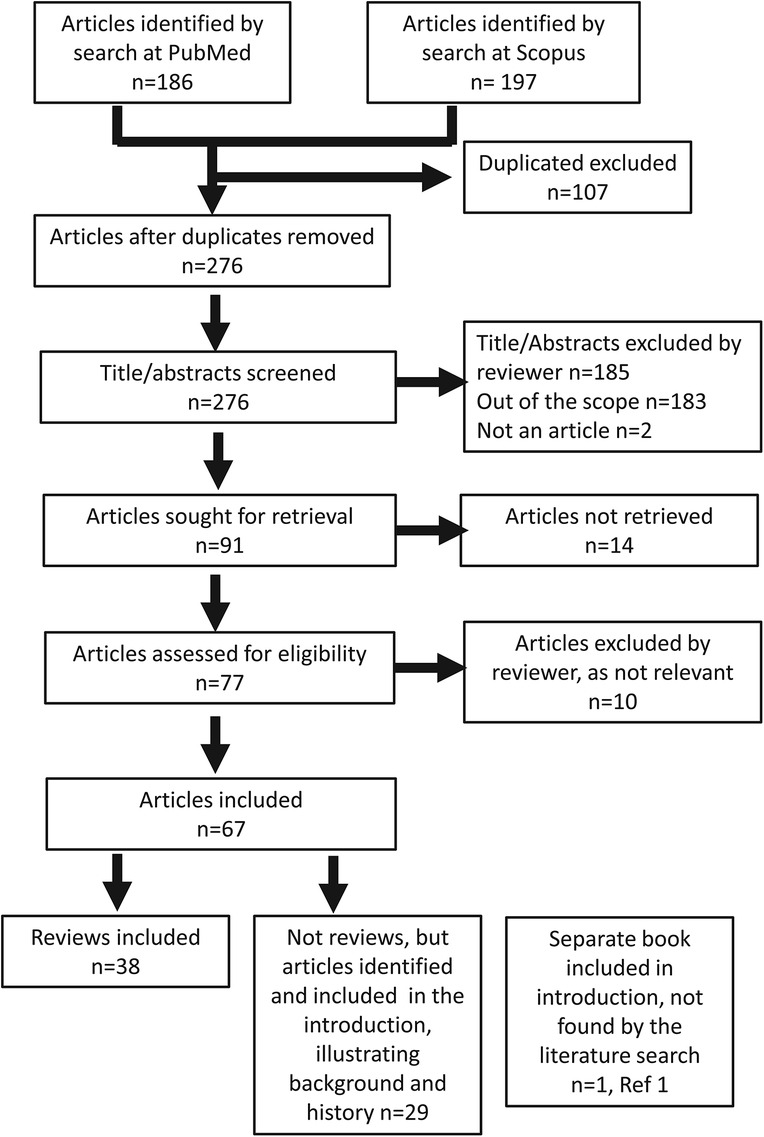
Methods: PubMed and Scopus were searched twice for reviews published between 1997 and October 2023 and between 1997 and January 2024. The search terms used were “review,” “surgical training,” “surgical skills,” “assessment,” and “evaluation” in combinations. In all, 38 reviews were included (systematic and non-systematic). In addition, 30 non-reviews were selected for the introduction and the historical background. Publications on non-technical skills were excluded.
Results: Great efforts have been invested by committees and working groups to define methods for surgical training and assessment. However, the work was found to be scattered, without attempts to be overarching and internationally valuable, and few training methods were strictly scientifically validated. Many reviews were limited to (1) one surgical procedure, (2) to one surgical specialty, (3) to one surgical method such as endoscopic procedures or “robotics,” or (4) to a limited geographical area.
Conclusions: Scientifically validated, generally applicable methods for surgical training and assessment could not be found. Further research is needed to find simple, equal, and overarching methods to allow valid and reliable comparisons of manual surgical competencies across borders, in financially strained healthcare where resources for adequate training and evaluation of skills may not be available. Financial aspects can be included in future studies, to correlate costs for training with costs for avoidable surgical complications.
Introduction
This study aimed to investigate whether there are published, rigorously scientifically validated methods for surgical education and assessment that are evidence-based and that can be applied generally across countries and all types of surgery. We presumed that a certain level of basic education is required before specialization.
Human anatomy is essentially the same, regardless of country, culture, religion, and socioeconomic status. For this reason, the surgical profession should be equal and comparable between countries and continents. This topic includes the associated questions of surgical training and assessment, surgical errors, and patient safety, as well as acknowledging that surgeons are humans making mistakes (1). Anyone of us might end up on an operation table tomorrow. The question of surgical safety is regarded as closely related to the UN Declaration of Human Rights ratified on 16 September 1949, which in this context affirms that each individual has the right to be operated on by a properly trained surgeon when a surgical procedure is required. There is scientific evidence that surgical treatment includes risks for errors, injuries, and deaths (1–4), but it is believed that validated statistics on healthcare injuries are scarce and seldom systematically divided into surgical or non-surgical (5). In a 2023 scoping review on surgical informed consent (6), surgical risk factors and outcomes were discussed, excluding the impact of the surgical intervention itself.
For the last 30 years, there have been an increasing number of publications on “surgical training” and “assessment of surgical skills,” but many of these studies lack consistency and often contain a mix of other competencies—such as diagnostics, judgment of indication for surgical interventions, mentoring, work-based assessment, and other non-technical skills such as leadership, teamwork, and work–life balance (7–22). Virtual reality training, other forms of simulation, and tools for surgical training have been widely described, most often in endoscopic surgery (23–31), while studies on simulation of open surgery, for example, cadaver training, are rare (32, 33). Complicating factors, such as the use of rapidly developing technical surgical equipment, have raised the issue of manual skills, training, and certification processes even in other scientific domains such as educational and technical sciences as well as human factors (34–37). A 2008 report on “deliberate practice” (34) from educational sciences gained substantial interest (7), as it showed that it would take 10 years or 10,000 h of deliberate practice for someone to demonstrate manual expertise. Not only the method of training but also the structure and transfer of the practice from the training situation to the OR were regarded as equally important by the author and mentioned in some of the included reviews (38–42).
A large number of surgical associations and different working groups (Table 1) have paid immense efforts to find solutions for surgical training methods (Table 2) that rarely seem to be subsequently validated in scientific studies.
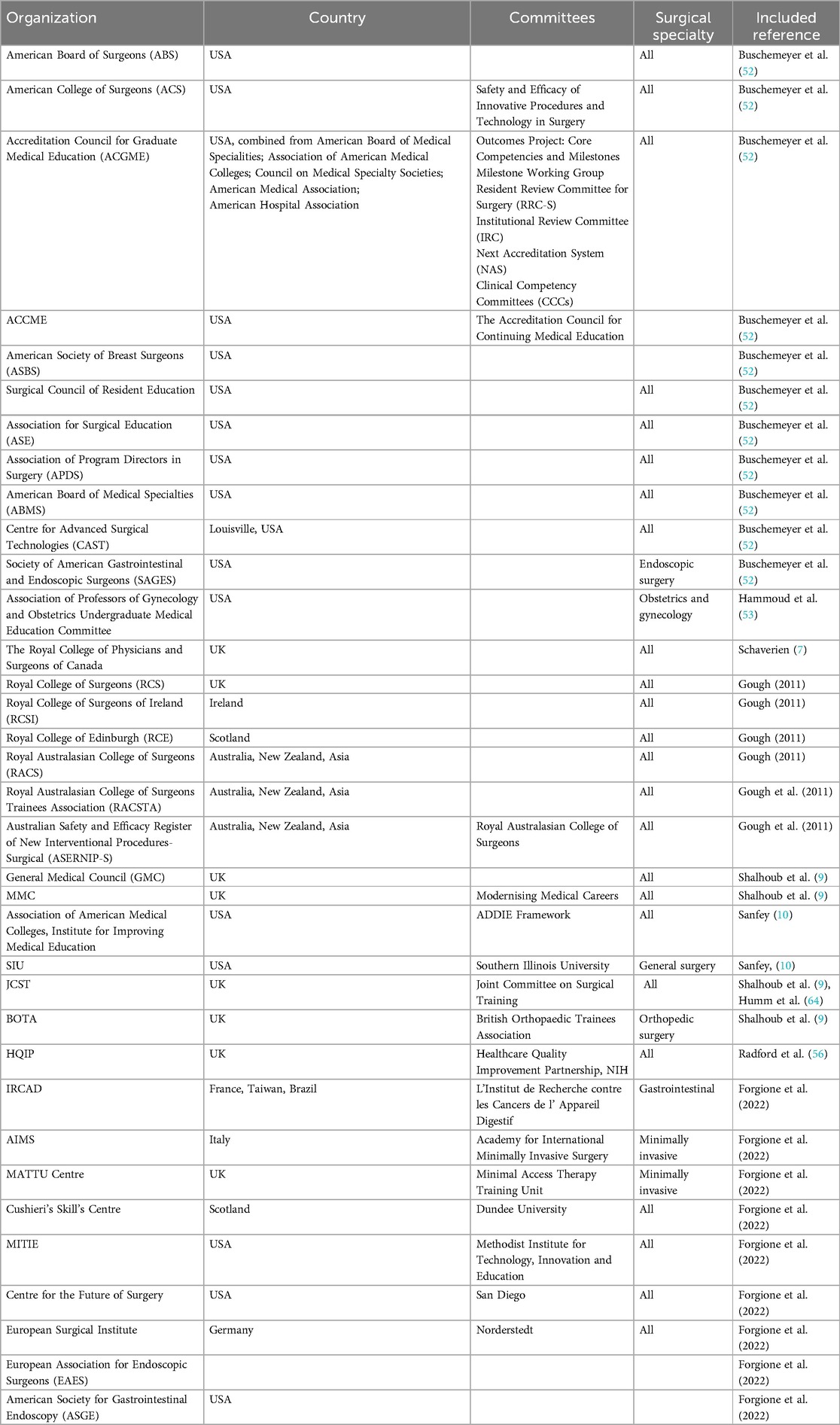
Table 1. Examples of surgical organizations, working groups, and societies working with surgical training methods mentioned in the included reviews.
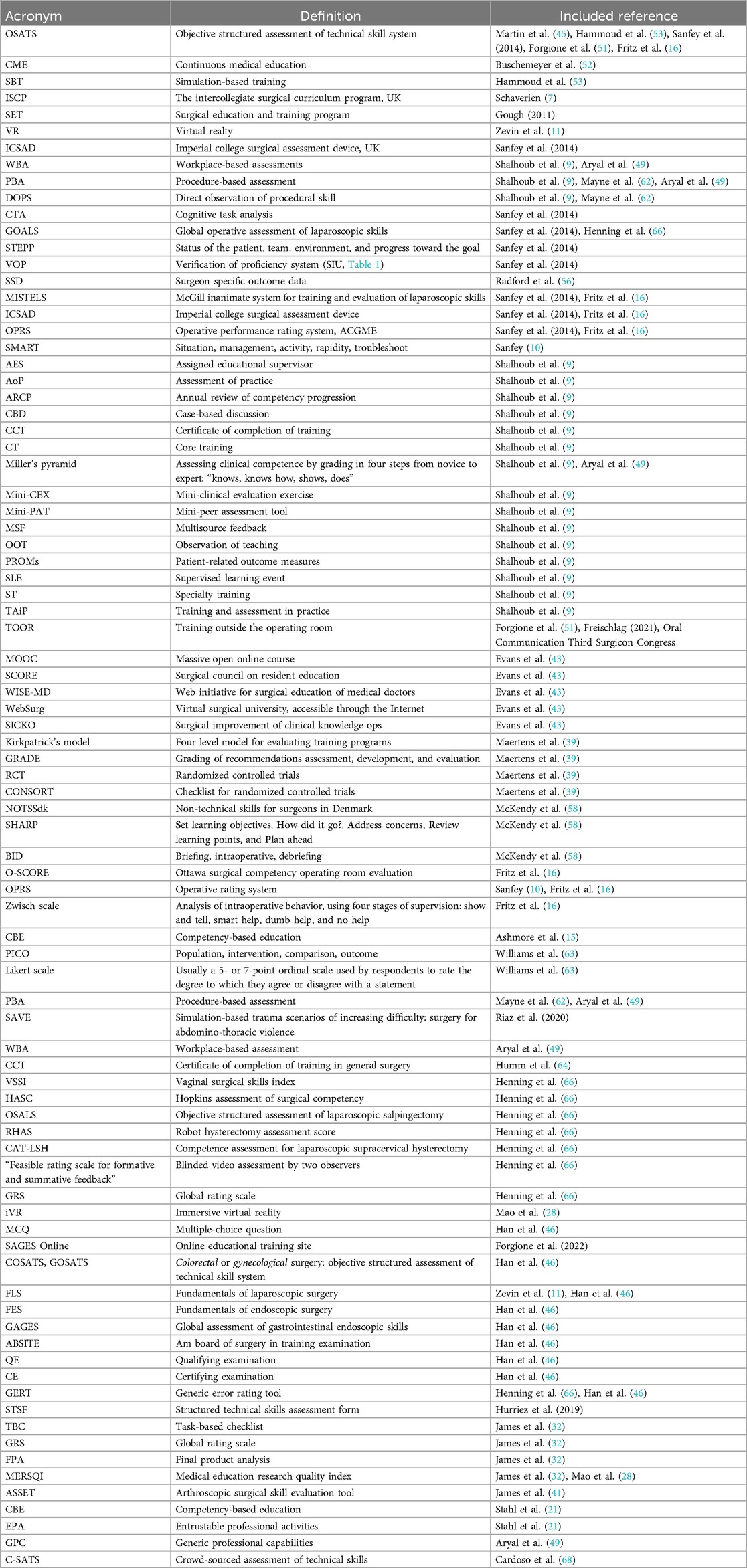
Table 2. Examples of acronyms or names for surgical training and assessment methodologies found in the included reviews.
From technical sciences (37), a study of the complexity of telemedicine and human factors tried to propose new ways of thinking forward in the conclusion: “According to numerous reviews and policy documents, system dynamics and complexity should be considered during the design and evaluation of technological change in health care,” and “this analysis serves as an example of how a complex clinical implementation context can be analysed and represented in a granular yet structured manner while also showing the interactions among the system elements.” In a 2016 study on general surgery in the USA (43), it was stated that “Simulation, VR, robotics, telemedicine, and gaming are no longer the future of surgical education, but represent the standard by which competence will be developed and measured.” In an interdisciplinary dissertation from the educational sciences and orthopedic surgery in 2022 (44), it was stated that “there is a lack of consensus among surgical educators or research into the required core skills and evaluation of their performance.” In this work, the Delphi method was used “to provide baseline data for future studies to reach a meaningful consensus to designing effective surgical training and evaluation of core surgical techniques.”
Examples of studies showing scientifically validated surgical training and assessment methods are available, such as the Objective Structured Assessment of Technical Skills (OSATS) system (45) since 1997, methods described in VR training in laparoscopic cholecystectomies in 2002 (24), and the proficiency-based progression training curriculum for an isolated endoscopic surgical procedure in 2015 (13) (arthroscopic Bankart surgery). In the latter, methods for objective measurements of manual skills were described, comparing the video of a performed surgical procedure to a standard video of the same surgical procedure. The standard video was fragmented into a number of mandatory elements to perform a correct arthroscopic Bankart procedure, and from the actual real-life video, the number of fulfilled elements was counted, in this way presenting a way to measure the surgical result. In a 2021 study on general surgery in the USA (46), “the need for standardized surgical training in this era of evidence-based medicine” was emphasized, mainly referring to mandatory multiple-choice questionnaires as an assessment method. However, it was also stated that written examination elements of board certifications did not correlate to the readiness to practice surgery, and assessment methods such as COSATS and GOSATS (Table 2) were validated but “not to be implemented as a requirement for board certification due to the costs and efforts needed to execute such assessments of surgical skills.” The question was raised “whether it is more appropriate to relegate assessment of technical competence to standardized examinations such as these or to the judgment of program directors who have access to more extensive, longitudinal evaluations of trainee performance in this domain.” A hypothesis of a generally applicable structure, with a stepwise training staircase model, was presented in 2017 (47, 48) (Figure 1), where it was presumed that surgical associations for one selected specialty might agree on the content of Level 1, Level 2, Level 3, etc., even between different countries. It was suggested that no time limit should be included for the acquirement of skills, but instead the passing of a defined clinical examination of some type to be allowed to move from one level to the next, as the time of the learning curve might vary between individuals. It was concluded that such a hypothesis of a staircase structure needs to be tested by high-quality scientific research such as randomized controlled trials (RCTs) to be supported or rejected.
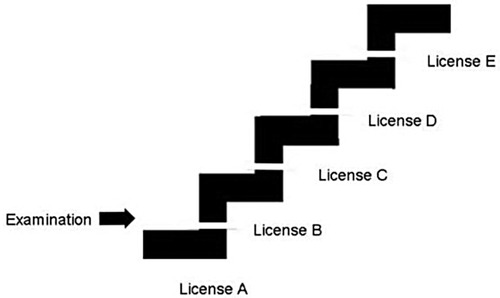
Figure 1. The surgical staircase model with interruptions at each level symbolizing practical examinations (47).
More recent work suggests the use of “work-base assessment” as a standardized tool for evaluation of surgical skills (49). A 2023 scoping review on surgical outcomes excluded the very surgical intervention as a factor influencing surgical outcomes (50). In our review, focus is paid only to the aspects of manual surgical skills, and non-technical skills are excluded. Our focus is only on training in surgical skills and assessment methods of such skills, both for beginners and mature surgeons learning new surgical techniques or instruments.
Methods
In order to find any available information on scientifically validated, internationally accepted, and generally applicable methods for training and assessment of surgical skills, regardless of surgical specialty, a literature search was made only for scientific reviews by one professional librarian and two reviewers in October 2023. The same search was remade in January 2024. PubMed and Scopus were searched for relevant reviews published from 1997 to October 2023 and then from 1997 to January 2024. The search terms used were review, surgical training, surgical skills, assessment, and evaluation using boolean operators as and and or. Both searches were limited to titles only.
Identifying relevant studies
The literature search resulted in 383 articles. After removing 107 duplicates, 276 articles were screened by title and abstract, of which 185 articles were excluded, including those out of the scope (183) or not being actual articles (2). A total of 91 articles were sought for retrieval in open-access articles, and 14 were not retrieved. In addition, 77 articles were accessed for eligibility, and 10 were excluded by the reviewers as they were not relevant. After full-text screening, a total of 38 reviews were included. In addition, 29 non-review articles were included in the introduction to illustrate the background of the topic (Figure 2). One additional book was included in the reference list, used in the introduction.
Results
Summarizing the included reviews
Of the included 38 reviews, 14 were found to be generally applicable, while 16 reviews were limited to one specific surgical procedure, to one diagnosis such as “kidney cancer,” to a special area such as “robotics” or “laparoscopy,” to one surgical specialty such as “urology,” or to a specified geographical region. However, conclusions were strikingly similar, often stating that the actual study was limited and further research would be needed to draw general conclusions. Only two of the reviews mentioned the international aspect of surgical training and assessment (8, 51).
Collating and reporting the results
The search outcome is given as a descriptive chronological overview of the reviews and their conclusions, to illustrate the history, development, scientific quality, the number of involved factors, and the status of the topic.
Results of the search
In a 2005 study on general surgery (52), it was stated that “surgery necessarily entails patient morbidity and mortality” and that “the rapid technological development is changing the surgical profession.” The challenge of defining the processes of accreditation, certification, credentialing, and privileging was pointed out, and the suggested definitions are “blurred, blended, occasionally misrepresented and misunderstood.” It was also emphasized that laparotomy and laparoscopy “now should be learned in the same amount of time” as open surgery used to be learned as the exclusive approach. Training after residency was found to lack uniform structure, organization, detailed guidelines, and nationally recognized criteria. Animal laboratories and mechanical simulators were described as excellent ways of training outside the operating room (TOOR) to simulate surgery and shorten the learning curve, but such training was seen as labor-intensive and expensive. In an attempt to standardize surgical training, a Centre for Advanced Surgical Technologies (CAST) was created at the University of Louisville, where approximately 20 predefined surgical procedures in general surgery were systematically trained in a rotation program during 5 years in residency. One conclusion was: “The surgical community is the most knowledgeable and appropriate group to issue training guidelines.”
A committee from obstetrics and gynecology (53) stated in 2008 that simulation-based surgical training was used with limited evidence-based data to support the validity and reliability. When discussing low- and high-fidelity simulators, it was concluded that: “…a more robust assessment program for surgical skills potentially can be achieved with a combination of OSATS, performance assessments from virtual reality simulators, and global rating scales from observation of a trainee operating on a real patient.”
In the UK in 2011, the general value of cadaver workshops (54) was “held in high regard and felt they help to improve operative skills” but showed that validated data on real-life skill's transfer from cadaver workshops to the operating room are missing in the literature and emphasized the need for further scientific studies.
Hand surgeons emphasized in 2011 the need for formalized programs for surgical mentorship (38) and stated that the surgical environment is unique and defined by several distinct characteristics that set it apart from other professional settings in health care: “the expectations combined with the stress associated with the operating room, present a challenging learning environment for surgical trainees of all disciplines.”
International aspects of the use of the Internet and modern communication technology in surgical training were considered in obstetrics and gynecology from Sweden and Spain in 2012 (8). Telementoring, teleproctoring, and robotic telesurgery were judged to have great potential, and it was concluded that: “The integration between surgery and telecommunications could constitute one of the major achievements of modern medicine, and its safe integration into clinical practice should be a priority for modern surgeons.”
In plastic surgery, a review focused on traditional mentorship and supervising of residents in the OR (26). The authors concluded the traditional method of medical learning “see one, do one, teach one” was still applicable but extended the method by stating: “…in this era of outcome and evidence-based medicine, medical learning should be to see many, learn from the outcome, do many with supervision and learn from the outcome, and finally teach many with supervision and learn from the outcome” and continued: “However, the method can be built upon various learning principles, committed mentors, and advanced technology such as medical simulators. Residents must be encouraged and given the opportunities to learn and improve upon their surgical skills by mentors who continue to improve upon their skills as well. This can all be done in an environment that keeps patient safety at the forefront.”
A 2014 report from the Direction of Education of the American College of Surgeons (10), after a 3-month visit to Ireland where the Royal College of Surgeons in Ireland has long been actively developing surgical training methodologies (55), emphasized the importance of “remediation,” and discussed a methodology where the first corrective measure following an error was “to discuss over a cup of coffee,” and combined the assessment of technical and non-technical operative skills. One final conclusion was: “Trainee performance should be evaluated in a rigorous, reliable and meaningful way to ensure that graduates have the skills necessary for safe, independent practice” without defining how to do this.
A 2014 review on general surgery in Canada and the UK (11) examined evidence supporting the use of simulation in surgical education and concluded that “The effectiveness of surgical simulators has been demonstrated in randomized controlled trials. The evidence from those trials has been summarized in systematic reviews and meta-analysis. Simulation has also been used in selected high-stakes examinations. Unfortunately, despite all of this progress, simulation-enhanced training is still not a standard or a mandatory component of all surgical training. Evidence of improved clinical outcomes and cost-effectiveness of surgical simulation will be required to make simulation-enhanced education a mandatory component of surgical training, retraining, certification, and re-certification. With such evidence in hand, surgeon educators will finally have the leverage necessary to advocate for simulation-enhanced training with hospital administration, government officials, surgical credentialing bodies, and, most importantly, patients.”
Surgeon-specific outcome data (SSD) from different surgical specialties in the UK (56) was first reported in 2014, where it was pointed out that “…disregarding the lack of governmental instructions on how to perform surgical training and assessment this is regarded as a significant advancement in health service transparency.” Factors influencing statistics such as outcomes of life-saving procedures with poor initial prognosis were not specifically discussed.
An evaluation of the effectiveness of different forms of e-learning in 2016 (39), stated that: “Despite significant heterogeneity amongst platforms, e-learning is at least as effective as other methods of training,” having included 87 out of 4,704 articles meeting the quality requirements using the GRADE standards and the CONSORT checklist (Table 2) for RCTs to evaluate limitations in study quality and potential risk of bias. A total of 7,871 surgeons included in the 87 studies had been using some type of e-learning. Only two RCTs demonstrated a transfer of skill to the clinical environment, and there was no evidence to show improvement in patient outcomes. They also discussed the importance of using e-learning within a larger context, combining factors as follows: “focused feedback, immediate and ample opportunities for repetition, focused practice, and emphasis on difficult aspects and areas of weakness.”
An interdisciplinary group of experts in (1) computer engineering, (2) informatics, (3) biomedical, industrial and human factors engineering, and (4) surgery (57) evaluated factors of distraction in the operating room 2016 and concluded that: “Operating room protocols should ensure that distractions from intermittent auditory and mental distractions are significantly reduced. In addition, surgical residents would benefit from training for intermittent auditory and mental distractions in order to develop automaticity and high-skills performance during distractions, particularly during more difficult surgical tasks. It is unclear as to whether training should be done in the presence of distractions or distractions should only be used for post-training testing of levels of automaticity.” Assessment of “surgical performance” was measured in different ways in the included studies, e.g., time to completion of a task, number of errors without defining “error,” and increase in movements (influencing the time to completion). They concluded that: “Due to the lack of consistency between performance measures, missing experimental or results data, or variance in experimental design, aggregated findings (i.e., a meta-analysis) could not be performed.”
A 2017 review on general surgery from an international perspective originating from Italy and Saudi Arabia (51) included aspects of patient safety during surgical training. Virtual surgical simulators were seen as the solution for both training and assessment, but “at the moment, we cannot recommend a single superior model for surgical training and assessment.”
A systematic review of general surgery and minimally invasive surgery in Canada 2017 (58), focused on perioperative teaching and feedback, searching the terms: “teaching, feedback, guidance, or debriefing” in the perioperative period and concluded that: “There is a need for improved quality and quantity of structured feedback.” Four of the 26 included studies reported examples of deliberate implementation of teaching or feedback strategies in the OR. One conclusion was: “In subsequent cases, the feedback group demonstrated a significant improvement in time to complete the procedure, errors, and economy of movement compared to the group that did not receive feedback.”
A systematic review of surgical training on reperfused human cadavers (40) was presented from Belgium in 2018 where different techniques of reperfusion and ways of embalming were used in the included studies, and the authors concluded that: “Various reperfused human cadaver models exist, enabling practice of mainly vascular procedures. Preservation method determines the level of simulation fidelity. Thorough evaluation of these models as surgical training tools and transfer effectiveness is still lacking.”
A review of surgical simulation training in sub-Saharan Africa (SSA) in 2018 (59) reported: “An estimated 5 billion people worldwide lack access to any surgical care, whilst surgical conditions account for 11%–30% of the global burden of disease. Maximizing the effectiveness of surgical training is imperative to improve access to safe and essential surgical care on a global scale.”…and continued: “Few studies reported any outcome data. Compared to the volume of surgical training initiatives that are known to take place in SSA, there is very limited good quality published evidence for the use of simulation training in this context.”
In pediatric surgery (60), it was reported in 2019 that simulation courses increased proficiency in technical skills and were useful in preparing general surgeons for work in emergency situations. However, the exposure to real-life operative trauma management was judged as a remaining issue. It was concluded that: “Literature suggests that the quality of surgical care correlates with surgical experience” while the term “experience” was not defined.
A 2019 review on orthopedics, trauma, hand, and reconstructive surgery in Germany (16) including international aspects of evidence in surgical training stated that surgical curricula contained major differences even between the countries within the European Union. No studies analyzing the educational programs in different countries were found, and there is no evidence indicating which educational system is superior. The topic assessment was pinpointed: “There is also little evidence to distinguish the good from the average surgeon or the junior surgeons’ progress, during his residency training. Although some evaluation tools are already available, the lack of resources of most teaching hospitals often results in not using these tools as long it is not mandatory by a governmental program” and continued: “Most countries provide a curriculum for surgical education, but the programs differ in their structure and time points of assessment. For example, the United Kingdom and the Republic of Ireland use structured educational programs with repeating assessments for human factors, technical skills and medical knowledge using multiple-choice questionnaires—but practical tests are not performed, so the surgical procedural quality is not part of the certification.” It was expressed that no comparability studies between residents of different hospitals were performed. The authors advocated the use of validated scores such as the Ottawa Surgical Competency Operating Room Evaluation (O-SCORE), the Operative Rating System (OPRS), or the Zwisch scale (Table 2). In addition, it was stated that few published studies focused on the simulation of open surgery and that some studies showed: “Bench model training skills are transferable to the human model (cadaveric), but that yet no study analysed the further transfer of manual skills to the operating room.”
In a 2019 study on orthopedic surgery in the UK (32), the current status of cadaveric simulation for surgical training was analyzed, concluding: “There is an abundance of relatively low-quality evidence showing that cadaveric simulation induces short-term skill acquisition as measured by objective means. There is currently a lack of evidence of skill retention, and of transfer of skills following training into the live operating theatre.”
The incorporation of surgical training in international healthcare missions and its effect on the global burden of surgical disease was reported from general surgery in the USA in 2019 (61) by a systematic review. In an “ethical checklist” with 16 organizational factors, one question on “knowledge/skill translation” was included, coming from the field of neurosurgery. It was stated that: “The impact of international missions on the professional development of surgeons in training cannot be understated” and that “several studies have presented …improved surgical skills,” but the question about how such skills were measured was not discussed. The importance of “case volumes” was mentioned, not taking any question of surgical outcome or quality into account.
The terms simulation, VR, XR, augmented reality, and mixed reality as well as haptic techniques and computing graphics were explored in ENT surgery in 2020 (18). It was stated that: “High-fidelity simulation centres require a significant upfront investment, and that the operation of these centres requires an extensive team of expert staff and incurs large running costs. Cadaveric simulation has extremely high running costs and ethical implications using human cadavers. Both of these educational tools require the learner to attend a course on a specific date and generally run through the scenario just once. These courses or educational activities, to be maximally effective, may need to be repeated, thus incurring repeated similar costs.” VR training was mentioned to have an advantage of “repeatability, reliability and online access compared to such labs and to cadaveric dissection and temporal bone laboratories for ENT surgery, and that a virtual reality simulator is relatively inexpensive, requires little space and, depending on the educational model, no supervision.”
From medical and dental training centers in Northern Ireland (62), it was concluded in 2020 that: “Procedure-Based Assessment (PBA)” and “Direct Observation of Practical Skills (DOPS) assessments are educationally useful tools in postgraduate surgical training. Further research is required to determine the number of assessments required to ensure adequate reliability.”
In a 2020 study on trauma surgery in Pakistan (20), it was concluded that: “Current training in most surgical residency programs, locally and globally, is suboptimal” and “The decrease in volume of trauma cases results in variable and/ or inadequate exposure and hands-on experience of the surgical trainees in operative management of trauma” and stated that: “We have identified the deficiencies in the trauma-related training and education in postgraduate surgical education.” A set of components was recommended in the trauma surgery curriculum such as “video review with debriefing,” “simulated trauma resuscitation,” “computer-based programs and games,” and “simulation-based trauma scenarios of increasing difficulty such as surgery for abdomino-thoracic violence (SAVE),” and it was furthermore stated that: “The estimated increase in the burden of the trauma-related injuries in coming years warrants a multifactorial concerted effort to equip our surgeons with the essentials of knowledge and skills required to adequately manage trauma cases thus reducing resultant mortality and morbidity.” No suggestions of systematic or scheduled use of simulation systems or stepwise examinations of surgical skills were described in the review.
A 2020 review on the use of augmented reality (AR) training, covering the full range of surgical disciplines in the UK (63), reported the outcomes to be measured in many different ways, such as “Competency, operational/procedural duration, user opinion recorded through a Likert scale questionnaire (Table 2) and postoperative complication rate.” Only two of the included studies were set in a real clinical environment. AR training increased the scores for competency, surgical opinion, and postoperative complication rate compared with traditional training, while operative duration increased using AR. The term population, intervention, comparison, and outcome (PICO) was also used to report outcomes. It was concluded that: “Due to the lack of any common protocol, there was an almost infinite variability in trial design.” No suggestion of a systematic use of AR in surgical training programs was made.
A systematic review on surgical training on donated cadavers in the UK (41) stated that: “Out of 51 studies, 22 assessed the impact of the cadaveric training intervention using only subjective measures, 5 measured impact by change in learner knowledge, and 23 used objective tools to assess change in learner behaviour after training.” Only one study assessed patient outcomes and demonstrated the transfer of skill from the simulated environment to the workplace. Of the included studies, 67% had weak methodology (MERSQI score <10.7). It was concluded that: “There is an abundance of relatively low-quality evidence showing that cadaveric simulation induces short-term skill acquisition as measured by objective means. There is currently a lack of evidence of skill retention, and of transfer of skills following training into the live operating theatre.”
In a systematic review from Germany and Greece (42), 18 RCTs focusing on the very transfer of skills from simulation-based training in different laparoscopic procedures to skills in the operating room 2020 it was concluded that: “Simulation provides a safe, effective, and ethical way for residents to acquire surgical skills before entering the operating room.”
The terms “work-based assessments (WBA), procedure-based assessment (PBA), clinical evaluation exercise, formative assessment, case-based discussion, and direct observation of procedural skills” were analyzed in a 2021 review of general surgery in the UK (49), where it was concluded that: “In Miller's pyramid (Table 2), a framework for assessing clinical skills and performance, WBAs are ranked at the highest level for assessing doctors in action.”
In a profound review from Canada in 2021 (28), a comparison was made between VR training and traditional training, concluding: “Trainees demonstrated improvement of surgical skills through VR simulation, especially in comparison to non-VR, traditional training. Immersive VR trainees demonstrated faster procedural completion times, greater task completion scores, and improved accuracy of surgical device implantation when compared to control in multiple RCTs.” Their conclusion was: “Further work should be done to compare the efficacy of VR with lower fidelity simulators, and clarify its role in the context of large-scale, comprehensive surgical residency programs. This nascent technology has the potential to remodel our contemporary views of surgical training and serves as a compelling supplement to cadaveric and real patient training.”
A critical evaluation of key issues in laparoscopic general surgical training and digital technology and surgical skills assessment was made in the UK and Ireland in 2021 (64), concluding a more streamlined and efficient training system supporting cognitive, technical, and non-technical skills can be achieved due to the technical development. Standardizing and automating assessments were supposed to improve surgical outcomes. Digital strategies appear to benefit surgeons, surgical teams, and patients alike. Asking for more available data, it was suggested it could lead to standardized, regulated systems that can support surgical teams in providing safer surgical care.
Innovations in urological surgical training for the 5 last years were summarized in the USA in 2021 (65), and the structured surgical video review showed improved surgical skills not only for trainees but also for qualified surgeons. Despite the advances, it was concluded that there are still unfulfilled needs for a standardized surgical training program covering both technical and non-technical skills.
A scoping review from Gynecology in Denmark 2021 (66) searched for standardized assessment tools for gynecology surgical training, as consensus was considered to be missing on which surgical assessment tool to use. Assessment methods from 544 articles were categorized, and eight tools were identified for measuring technical skills during gynecologic surgery; however, all of these depended on the user context, with varying validity frameworks. Their conclusions were: “There is a need for larger, randomized studies to evaluate their validity before they are enrolled in gynaecological curricula or used for summative assessment” and that “the review can serve as a guide for surgical educators who want to apply a scale or a specific tool in surgical assessment.”
Concerning ophthalmologic robot surgery in Canada and the Netherlands (67), the role of industrial partners in surgical training and assessment was mentioned in 2021: “There is a lag in the development of a comprehensive training and credentialing system for robotic eye surgery, and certification of robotic skills proficiency relies heavily on industry leadership.” In addition, the idea of stepwise structured learning was recommended “in a stepwise, competency-based manner from didactic learning, to simulation exercises, to finally operative experiences,” and further: “We have developed an assessment tool based on validated global rating scales for surgical skills that may be used to monitor the progress of trainees. Finally, we propose a graduating model for granting privileges to robotic surgeons.”
A group of plastic surgeons in Italy, Germany, and the USA concluded in 2022 (44): “To date, there are no standardized or ideal simulation models for local skin flap teaching,” and “most of the described models have been assessed only in small cohort numbers, and therefore larger candidate sizes and standardized methods for assessment are required.”
Simulation-based training in cardiac surgery was reviewed by colleagues in the UK and the Netherlands in 2023 (30), and they stated that: “The results of the included studies suggest that validity assessment is scarce within the field, being carried out for only 4 of the models. Nonetheless, all studies reported improvement in trainees’ confidence, clinical knowledge and surgical skills (including accuracy, speed, dexterity) of trainees both at senior and junior levels. The direct clinical impact included initiation of minimally invasive programmes and improved board exam pass rates, and creating positive behavioural changes to minimize further cardiovascular risk” meaning that reasoning about “patient safety” was connected to the question of training methods.
In a major international review on surgical simulation in 2023 (68), the question about treating the subject of surgical training strictly scientifically, as any other method in healthcare, stated that: “Few previous studies compared learners who received structured simulation training to a group of trainees who did not receive any simulation training in single-centre randomized control research.” The use of videos was emphasized, the cost of setting up a simulation lab was estimated to range from $100,000 to $300,000, and it was stated that: “a good method of simulation training is using virtual reality simulators with haptics and simulated patients. The availability of these facilities is limited, though, and a typical session might include an exercise involving stacking sugar cubes and box trainers. The degree of expertise or competency is one area that needs clarification as medical education transitions to a competency-based paradigm.” [The last conclusion about the need for competency-based training was also the general conclusion of the First Surgicon Congress in 2011 (48)].
From the Netherlands, the use of different digital tools in surgical training in different surgical specialties was reviewed (31) in relation to dry and wet labs, including digital box trainers, (immersive) virtual reality (VR) trainers, robot surgery trainers, coaching and feedback, serious games, and the role of such tools in complete surgical curricula was discussed. The conclusion stated that: “While the efficacy of digital tools in enhancing technical surgical skills is evident—especially for VR-trainers—there is a lack of evidence regarding non-technical skills, and need to improve methodological robustness of research on new (digital) tools before they are implemented in curricula.”
In an extensive but highly specialized international review (69) on the use of Artificial Intelligence in the surgical training and treatment of kidney cancer from Italy, Egypt, Belgium, Portugal, Spain, Russia, Germany, the USA, and the UK, the possibilities of international collaboration were clearly demonstrated. They concluded that: “Potential AI applications in kidney cancer surgical training include analysing surgical workflow, annotating instruments, identifying tissues, and 3D reconstruction. AI is capable of appraising surgical skills, including the identification of procedural steps and instrument tracking. While AI and augmented reality (AR) enhance training, challenges persist in real-time tracking and registration. The utilization of AI-driven 3D reconstruction proves beneficial for intraoperative guidance and preoperative preparation. Artificial intelligence (AI) shows potential for advancing surgical training by providing unbiased evaluations, personalized feedback, and enhanced learning processes. Yet challenges such as consistent metric measurement, ethical concerns, and data privacy must be addressed. The integration of AI into kidney cancer surgical training offers solutions to training difficulties and a boost to surgical education. However, to fully harness its potential, additional studies are imperative.”
Discussion
General aspects
We searched the literature for generally applicable evidence-based methods for surgical training and assessment. That is, scientifically validated, internationally accepted methods for training and assessment of surgical skills, in review articles. Few attempts to harmonize surgical training methods and competence levels internationally were found. Despite all efforts found, paid by different working groups and institutions, the suggested solutions seem to be scattered and inconsistent. However, the resemblance of the conclusions in the included reviews was striking, generally stating that “data is missing” and “more research is needed.” The formal responsibility for technical surgical training and certification, credentialing, and privileging is shown to be randomly divided between local, regional, or national interest groups and surgical societies. In each country, each surgical specialty is thus bearing the burden of creating applicable methods for training and assessment, a sustainable training structure, and the transfer of technical surgical skills from models into the OR. As a consequence, surgical skills are not comparable within countries and even less between countries, with one exception referring to a review dealing with artificial intelligence used in surgery for kidney cancer.
Decision-making in a divided medical profession
Viewing the need for structured and validated surgical skills training, this can be seen as a part of continuous medical education (CME). Decision-makers might come from non-surgical specialties, explaining why surgical topics are not often specifically addressed. Medical doctors might be divided into two separate groups: one group that treats disease or injuries by medication and another group that treats disease or injuries by manual work. When discussing CME, this distinction is seldom made, not taking the need for continuous surgical skills training into account separately. This view of two principally different groups of medical doctors could also be applied to nurses and other medical staff. Our views on manual training are thus also applicable to all kinds of staff performing manual medical procedures, which extrapolates the practical training issue to an even higher degree.
New surgical methods and the use of new surgical equipment could also be regarded as any new medical treatment and compared with the introduction of new pharmaceuticals. The surgical methods should thus be equally subjected to high-quality evaluation in prospective, randomized, and controlled (Phase 1, 2, and 3) studies collecting reliable data before new technical devices and new surgical methods are accepted for general use.
Future research leadership and external observers
As more data are needed, a new form of a combined competency might be useful, such as a new title, e.g., “University professor in surgical teaching/learning,” combining knowledge in surgery and learning sciences, to develop a high-quality scientific research path in this field. The majority of authors of the included reviews and underlying articles were surgeons themselves, originally trained in different ways and who in addition might be critically regarded as scientifically biased if the studies were performed in their own surgical department or hospital. The topic could benefit from applying normal and strictly scientific principles such as RCTs, using external unbiased observers to evaluate results. Broader views and interdisciplinary studies might also be valuable, integrating data from the medical, educational, technical, financial, and ethical domains, such as human factors adopting new technical equipment and adapting technical equipment to human (surgeons) needs.
Likewise, the introduction of a mandatory “head training officer” at each surgical department might also be helpful, including scheduled working time dedicated to the leadership for practical manual training activities. Logically, surgeons should have a defined amount of their working time dedicated to manual skills training, due to our opinion.
Future training methods and documentation
Training by simulation was generally found to be valuable by increasing manual skills in a broad sense. However, the term simulation was used to refer to many different levels of surgery-like situations, from suturing in fabrics to high-fidelity computerized simulation equipment for selected elective surgical procedures. Most of the studies dealt with endoscopic surgical procedures and coupled computerized simulation. Studies of training and assessment of skills in open surgery seem to present special challenges, as the simulation of open surgery is technically demanding most often meaning resource-intensive training by dissection or training on animals under general anesthesia or on donated human cadavers. In the not-too-distant future, video documentation of surgical procedures might replace traditional written descriptions in medical records. This might be required from health care authorities, insurance companies, and the patients themselves. The AI technology will soon be able to interpret and score surgical videos. Some Swedish orthopedic surgeons already give a CD to the patients when they are discharged from the hospital with a video of their actual ACL replacement surgery.
Structure, assessment, and transfer
The structure of the training should not be neglected, meaning that skills should be acquired stepwise, and stepwise assessed, suggesting any form of practical examinations until we have evidence-based methods for assessment. In Figure 1, each level is marked with a white line, representing the practical examination of the achieved skills. Regarding assessment methods in the included reviews, they showed to be even less well-defined compared with training methods, and the term “competence” was sometimes used without any definition. Only a few reviews mentioned the term transfer of manual skills, meaning the use of acquired skills on models transferred to the real performance in the OR.
Costs
Time and resources dedicated to surgical training and assessment might be hard to find in financially strained healthcare. To motivate the expenses, cost–benefit analyses could be used comparing costs for training with costs for surgical errors and complications and their long-term effects, such as prolonged morbidity, prolonged sick leave, reduced or impaired working capacity, or death. We believe such data are mostly unavailable, and a future way to collect such data is an international understanding of the importance of systematically and objectively registering avoidable surgical complications using the International Code of Diagnoses 10 (ICD 10) Codes T 81.0–T81.9. This will need a global paradigm shift within the surgical community by using the mentality of “no personal blame.” Surgeons are humans, and we all make errors at times. By avoidable errors, we mean that high-risk surgical efforts in life-saving procedures in high-risk patients should be excluded from such statistics.
Surgeons and the surgical industry
A final but core factor was mentioned in one of the included reviews: the educational role of industrial suppliers of surgical equipment. Surgeons and the surgical industry are forever intertwined, and training and certification are sometimes arranged by industrial partners; however, each supplier is only offering training on their own products. As far as we know, there are no defined crossing lines within the operating room where the responsibility for the use of technical equipment is held by the hospital direction—or by the certifying supplier. We argue that the different roles of industrial suppliers and hospitals, in introducing new surgical equipment, should be defined by clear and simple rules.
Conclusions
We tried to analyze the state of the art in surgical training and assessment, by searching review articles on scientifically validated, internationally accepted, and generally applicable methods. Our overall conclusion was that such general and validated methods still are missing and that most authors with few exceptions did not suggest any generally applicable solutions, but concluded that there is a profound need for further research on this topic. Most of the reviews were limited to one surgical procedure, one surgical specialty, or one geographical area. Manual training outside the operating room seemed generally to increase surgical skills in the OR.
To move forward from this kind of standstill, we take the permission to suggest the surgical staircase model to be used as a general basic template for the creation of new hypotheses for further prospective scientific research. More studies performed using the same template would allow a more uniform collection of data and distantly more uniform and internationally comparable surgical skills.
Defining the steps of increasing skill difficulty seems like an easy task, if a common understanding within each surgical specialty could be worked out. As an example in orthopedic surgery, minor hand and foot procedures and hip fracture surgery might be included in Step 1—or whatever collaborating orthopedic societies might choose. Practical examinations should be mandatory to allow the proceeding from Step 1 to Step 2, which might speed up the process and produce mature surgeons in less time—as another hypothesis that also needs to be confirmed or rejected. This kind of system might slowly be accepted even internationally for each specialty, collaborating “across borders and boards.” In some cases, all given steps would not be necessary to complete, for example, a specialized orthopedic spine surgeon might just need competencies A, B, C, F, and H.
Future scientific research in this field would also benefit from combining surgical competency with competencies from teaching and learning sciences. A separation of the topic could then be useful, into training methods, training structures, assessment methods, and transfer of skills from the training situation to the operating room.
A distant common goal is thus to create (1) international standards for each surgical specialty, including (2) increasing steps of difficulty and (3) stepwise examinations using available assessment methods. (4) External unbiased observers might be useful in evaluating surgical results.
Costs for surgical skills training could be studied compared with costs for avoidable surgical errors and their long-term effects, to motivate the investment of dedicated working time to skills training. This would need a (5) systematical and objective registration of avoidable surgical complications using the International Code of Diagnoses 10 (ICD 10) Codes T 81.0–T81.9. In turn, this will need a higher understanding of the “no-blame” principle. (6) Finally, defining the roles of the educational responsibility between educating hospitals and the surgical device industry would be beneficial, by drawing medical legal liability borderlines for surgical skills training and certification.
To date, no administrative body would be able to create, inform, and control internationally equal surgical skills by regulations and certification schemes, even if validated data were available. Instead, we believe in an easily accessible collection of validated data and a continuous extraction of practical recommendations drawn from this database. Such work might be performed by any neutral, non-profit, and scientifically based non-governmental organization (NGO). The given recommendations would be free to follow for any surgical department, slowly creating a uniform way of surgical training and assessment in the surgical community, even internationally, over time.
Author contributions
MB: Writing – original draft, Writing – review & editing. LD: Writing – review & editing. MK: Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was funded by Vetenskapsrådet (Swedish Research Council).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Institute of Medicine (US) Committee on Quality of Health Care in America. In: Kohn LT, Corrigan JM, Donaldson MS, editors. To Err Is Human: Building a Safer Health System. Washington, DC: National Academies Press (US) (2000). p. 1–312.
2. Thompson AM, Stonebridge PA. Building a framework for trust: critical event analysis of deaths in surgical care. Br Med J. (2005) 330:1139. doi: 10.1136/bmj.330.7500.1139
3. Nepogodiev D, Martin J, Biccard B, Makupe A, Bhangu A. Global burden of postoperative death. Lancet. (2019) 393(10170):401. doi: 10.1016/S0140-6736(18)33139-8
4. O'Flynn E, Bekele A, Tierney S, Borgstein E. Making all deaths after surgery count. Lancet. (2019) 393(10191):2588. doi: 10.1016/s0140-6736(19)31113-4
5. George C, Lindén T. Socialstyrelsen: När var Tionde Skadas I Vården Krävs Handling. Swedish: Dagens Samhälle (2020).
6. Melucci AD, Erlick MR, Loria A, Russell MM, Temple LK, Poles GC. Surgical informed consent: a scoping review of physician-facing decision support tools. Ann Surg Open. (2023) 4(1):e259. doi: 10.1097/AS9.0000000000000259
7. Schaverien MV. Development of expertise in surgical training. J Surg Educ. (2010) 67(1):37–43. doi: 10.1016/j.jsurg.2009.11.002
8. Gambadauro P, Torrejón R. The “tele” factor in surgery today and tomorrow: implications for surgical training and education. Surg Today. (2013) 43(2):115–22. doi: 10.1007/s00595-012-0267-9
9. Shalhoub J, Vesey AT, Fitzgerald JE. What evidence is there for the use of workplace-based assessment in surgical training? J Surg Educ. (2014) 71(6):906–15. doi: 10.1016/j.jsurg.2014.03.013
10. Sanfey H. Assessment of surgical training. Surgeon. (2014) 12(6):350–6. doi: 10.1016/j.surge.2014.07.001
11. Zevin B, Aggarwal R, Grantcharov TP. Surgical simulation in 2013: why is it still not the standard in surgical training? J Am Coll Surg. (2014) 218(2):294–301. doi: 10.1016/j.jamcollsurg.2013.09.016
12. Sinclair P, Fitzgerald JE, McDermott FD, Derbyshire L, Shalhoub J. Mentoring during surgical training: consensus recommendations for mentoring programmes from the association of surgeons in training. Int J Surg. (2014) 12(Suppl 3):S5–8. doi: 10.1016/j.ijsu.2014.08.395
13. Angelo RL, Ryu RK, Pedowitz RA, Beach W, Burns J, Dodds J, et al. A proficiency-based progression training curriculum coupled with a model simulator results in the acquisition of a superior arthroscopic Bankart skill set. Arthroscopy. (2015) 31(10):1854–71. doi: 10.1016/j.arthro.2015.07.001
14. Rashid P, Narra M, Woo H. Mentoring in surgical training. ANZ J Surg. (2015) 85(4):225–9. doi: 10.1111/ans.13004
15. Ashmore DL. Strategic thinking to improve surgical training in the United Kingdom. Cureus. (2019) 11(5):e4683. doi: 10.7759/cureus.4683
16. Fritz T, Stachel N, Braun BJ. Evidence in surgical training - a review. Innov Surg Sci. (2019) 4(1):7–13. doi: 10.1515/iss-2018-0026
17. Hurreiz H. The evolution of surgical training in the UK. Adv Med Educ Pract. (2019) 10:163–8. doi: 10.2147/AMEP.S189298
18. Abbas JR, Kenth JJ, Bruce IA. The role of virtual reality in the changing landscape of surgical training. J Laryngol Otol. (2020) 134(10):863–6. doi: 10.1017/S0022215120002078
19. Allum W. Improving surgical training. Surgery. (2020) 38(10):596–600. doi: 10.1016/j.mpsur.2020.07.015
20. Riaz Q, Saqib SU, Siddiqui NA. Changing face of trauma and surgical training in a developing country: a literature review. J Pak Med Assoc. (2020) 70(Suppl 1):S89–s94.
21. Stahl CC, Minter RM. New models of surgical training. Adv Surg. (2020) 54:285–99. doi: 10.1016/j.yasu.2020.05.006
22. Khan MR, Begum S. Apprenticeship to simulation - the metamorphosis of surgical training. J Pak Med Assoc. (2021) 71(Suppl 1):S72–s76.
23. Torkington J, Smith SG, Rees BI, Darzi A. The role of simulation in surgical training. Ann R Coll Surg Engl. (2000) 82(2):88–94.10743423
24. Seymour NE, Gallagher AG, Roman SA, O'Brien MK, Bansal VK, Andersen DK, et al. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg. (2002) 236(4):458–63. doi: 10.1097/00000658-200210000-00008
25. Seymour NE. Virtual reality in general surgical training. European Surgery - Acta Chirurgica Austriaca. (2005) 37(5):298–303. doi: 10.1007/s10353-005-0184-x
26. Kotsis SV, Chung KC. Application of the “see one, do one, teach one” concept in surgical training. Plast Reconstr Surg. (2013) 131(5):1194–201. doi: 10.1097/PRS.0b013e318287a0b3
27. Piromchai P, Avery A, Laopaiboon M, Kennedy G, O'Leary S. Virtual reality training for improving the skills needed for performing surgery of the ear, nose or throat. Cochrane Database Syst Rev. (2015) 2015(9):CD010198. doi: 10.1002/14651858.CD010198.pub2
28. Mao RQ, Lan L, Kay J, Lohre R, Ayeni OR, Goel DP. Immersive virtual reality for surgical training: a systematic review. J Surg Res. (2021) 268:40–58. doi: 10.1016/j.jss.2021.06.045
30. Arjomandi Rad A, Hajzamani D, Sardari Nia P. Simulation-based training in cardiac surgery: a systematic review. Interdiscip Cardiovasc Thorac Surg. (2023) 37(2):ivad079. doi: 10.1093/icvts/ivad079
31. Feenstra TM, van der Storm SL, Barsom EZ, Bonjer JH, Nieveen van Dijkum EJM, Schijven MP. Which, how, and what? Using digital tools to train surgical skills; a systematic review and meta-analysis. Surg Open Sci. (2023) 16:100–10. doi: 10.1016/j.sopen.2023.10.002
32. James HK, Chapman AW, Pattison GTR, Griffin DR, Fisher JD. Systematic review of the current status of cadaveric simulation for surgical training. Br J Surg. (2019) 106(13):1726–34. doi: 10.1002/bjs.11325
33. Selcuk İ, Tatar I, Huri E. Cadaveric anatomy and dissection in surgical training. Turk J Obstet Gynecol. (2019) 16(1):72–5. doi: 10.4274/tjod.galenos.2018.15931
34. Eriksson KA. Deliberate practice and acquisition of expert performance: a general overview. Acad Emerg Med. (2008) 15(11):988–94. doi: 10.1111/j.1553-2712.2008.00227.x
35. Carpenter BT, Sundaram CP. Training the next generation of surgeons in robotic surgery. Robot Surg. (2017) 4:39–44. doi: 10.2147/RSRR.S70552
36. Louie PK, McCarthy MH, Albert TJ, Kim HJ. Reaching for peak performance during surgical training: the value in assessment tools and critical performance measures. J Am Acad Orthop Surg. (2020) 28(17):e744–51. doi: 10.5435/JAAOS-D-20-00172
37. Aminoff H, Meijer S. Modeling the implementation context of a telemedicine service: work domain analysis in a surgical setting JMIR Form Res. (2021) 6(5):e26505. doi: 10.2196/26505
38. Entezami P, Franzblau LE, Chung KC. Mentorship in surgical training: a systematic review. Hand (N Y). (2012) 7(1):30–6. doi: 10.1007/s11552-011-9379-8
39. Maertens H, Madani A, Landry T, Vermassen F, Van Herzeele I, Aggarwal R. Systematic review of e-learning for surgical training. Br J Surg. (2016) 103(11):1428–37. doi: 10.1002/bjs.10236
40. Willaert W, Tozzi F, Van Herzeele I, D'Herde K, Pattyn P. Systematic review of surgical training on reperfused human cadavers. Acta Chir Belg. (2018) 118(3):141–51. doi: 10.1080/00015458.2017.1407099
41. James HK, Chapman AW, Pattison GTR, Fisher JD, Griffin DR. Analysis of tools used in assessing technical skills and operative competence in trauma and orthopaedic surgical training: a systematic review. JBJS Rev. (2020) 8(6):e1900167. doi: 10.2106/JBJS.RVW.19.00167
42. Spiliotis AE, Spiliotis PM, Palios IM. Transferability of simulation-based training in laparoscopic surgeries: a systematic review. Minim Invasive Surg. (2020) 2020:5879485. doi: 10.1155/2020/5879485
43. Evans CH, Schenarts KD. Evolving educational techniques in surgical training. Surg Clin North Am. (2016) 96(1):71–88. doi: 10.1016/j.suc.2015.09.005
44. Hadjikyriacou E, Goldsmith T, Bowerman FI, Dobbs TD, Whitaker IS. Simulation models for learning local skin flap design and execution: a systematic review of the literature. Front Surg. (2022) 9:918912. doi: 10.3389/fsurg.2022.918912
45. Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. (1997) 84(2):273–8. doi: 10.1046/j.1365-2168.1997.02502.x
46. Han A, French J, Lipman J. Value of standardized testing in surgical training. Surg Clin North Am. (2021) 101(4):679–91. doi: 10.1016/j.suc.2021.05.013
47. Berg M. Surgical training, global surgery, and a generally applicable training model. Am Coll Surg. (2017) 102:54–7. https://surgicon.org/wp-content/uploads/2021/03/ACS-Bulletin-Vol-102-Nr-9_Original-Sept-2017.pdf
48. The Surgicon Project, NGO. Available at: www.surgicon.org (Accessed October 21, 2023).
49. Aryal K, Hamed M, Currow C. The usefulness of work-based assessments in higher surgical training: a systematic review. Int J Surg. (2021) 94:106127. doi: 10.1016/j.ijsu.2021.106127
50. DeMaio M. Dissertation, A Delphi Method Study: Exploring and Identifying Foundation Skills for Surgeons to Transform Surgical Education. USA: Drexel University School of Education (2023).
51. Forgione A, Guraya SY. The cutting-edge training modalities and educational platforms for accredited surgical training: a systematic review. J Res Med Sci. (2017) 22:51. doi: 10.4103/jrms.JRMS_809_16
52. Buschemeyer WC 3rd, Cunningham DK, Edwards MJ. Surgical training and implementation of emerging surgical technologies. Am J Surg. (2005) 190(2):166–72. doi: 10.1016/j.amjsurg.2005.05.005
53. Hammoud MM, Nuthalapaty FS, Goepfert AR, Casey PM, Emmons S, Espey EL. To the point: medical education review of the role of simulators in surgical training. Am J Obstet Gynecol. (2008) 199(4):338–43. doi: 10.1016/j.ajog.2008.05.002
54. Gilbody J, Prasthofer AW, Ho K, Costa ML. The use and effectiveness of cadaveric workshops in higher surgical training: a systematic review. Ann R Coll Surg Engl. (2011) 93(5):347–52. doi: 10.1308/147870811X582954
55. Royal College of Surgeons in Ireland. Available at: www.rcsi.org (Accessed October 14, 2023).
56. Radford PD, Derbyshire LF, Shalhoub J, Fitzgerald JEF. Publication of surgeon specific outcome data: a review of implementation, controversies and the potential impact on surgical training. Int J Surg. (2015) 13:211–6. doi: 10.1016/j.ijsu.2014.11.049
57. Mentis HM, Chellali A, Manser K, Cao CG, Schwaitzberg SD. A systematic review of the effect of distraction on surgeon performance: directions for operating room policy and surgical training. Surg Endosc. (2016) 30(5):1713–24. doi: 10.1007/s00464-015-4443-z
58. McKendy KM, Watanabe Y, Lee L, Bilgic E, Enani G, Feldman LS. Perioperative feedback in surgical training: a systematic review. Am J Surg. (2017) 214(1):117–26. doi: 10.1016/j.amjsurg.2016.12.014
59. Campain NJ, Kailavasan M, Chalwe M, Gobeze AA, Teferi G, Lane R, et al. An evaluation of the role of simulation training for teaching surgical skills in Sub-Saharan Africa. World J Surg. (2018) 42(4):923–9. doi: 10.1007/s00268-017-4261-7
60. Coventry CA, Holland AJA, Read DJ, Ivers RQ. Australasian general surgical training and emergency medical teams: a review. ANZ J Surg. (2019) 89(7-8):815–20. doi: 10.1111/ans.15158
61. Washington K. Affecting the global burden of surgical disease: incorporating surgical training into international missions: a systematic review. J Pak Med Assoc. (2019) 69(Suppl 1):S51–57.
62. Mayne A, Wilson L, Kennedy N. The usefulness of procedure-based assessments in postgraduate surgical training within the intercollegiate surgical curriculum programme; A scoping review. J Surg Educ. (2020) 77(5):1227–35. doi: 10.1016/j.jsurg.2020.03.005
63. Williams MA, McVeigh J, Handa AI, Lee R. Augmented reality in surgical training: a systematic review. Postgrad Med J. (2020) 96(1139):537–42. doi: 10.1136/postgradmedj-2020-137600
64. Humm G, Harries RL, Stoyanov D, Lovat LB. Supporting laparoscopic general surgery training with digital technology: the United Kingdom and Ireland paradigm. BMC Surg. (2021) 21(1):123. doi: 10.1186/s12893-021-01123-4
65. Ma R, Reddy S, Vanstrum EB, Hung AJ. Innovations in urologic surgical training. Curr Urol Rep. (2021) 22(4):26. doi: 10.1007/s11934-021-01043-z
66. Henning LI, Sørensen JL, Hybscmann J, Strandbygaard J. Tools for measuring technical skills during gynaecologic surgery: a scoping review. BMC Med Educ. (2021) 21(1):402. doi: 10.1186/s12909-021-02790-w
67. He B, de Smet MD, Sodhi M, Etminan M, Maberley D. A review of robotic surgical training: establishing a curriculum and credentialing process in ophthalmology. Eye. (2021) 35(12):3192–201. doi: 10.1038/s41433-021-01599-7
68. Cardoso SA, Suyambu J, Iqbal J, Cortes Jaimes DC, Amin A, Sikto JT, et al. Exploring the role of simulation training in improving surgical skills among residents: a narrative review. Cureus. (2023) 15(9):e44654. doi: 10.7759/cureus.44654
Keywords: surgical training, review of reviews, surgical skills, assessment of surgical skills, evidence-based training and assessment methods
Citation: Berg M, Dahlin LB and Kjellman M (2025) Overview of surgical training and assessment of surgical skills: a narrative review. Front. Surg. 12:1605495. doi: 10.3389/fsurg.2025.1605495
Received: 3 April 2025; Accepted: 2 June 2025;
Published: 25 June 2025.
Edited by:
Marina Yiasemidou, University of York, United KingdomReviewed by:
Manuela Mastronardi, University of Trieste, ItalyAlec Engledow, Barts Health NHS Trust, United Kingdom
Andrei Chitul, Barts Health NHS Trust, United Kingdom
Copyright: © 2025 Berg, Dahlin and Kjellman. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Margareta Berg, bWJlcmdAYnJlZGJhbmQyLmNvbQ==
 Margareta Berg
Margareta Berg Lars B. Dahlin
Lars B. Dahlin Magnus Kjellman
Magnus Kjellman