- 1Department of Orthopedic, Qilu Hospital Dezhou Hospital of Shandong University Dezhou Hospital, Dezhou, Shandong, China
- 2Department of Endocrinology, Qilu Hospital Dezhou Hospital of Shandong University Dezhou Hospital, Dezhou, Shandong, China
- 3Health Management Center, Qilu Hospital Dezhou Hospital of Shandong University Dezhou Hospital, Dezhou, Shandong, China
Introduction: Proximal humeral fractures are common in elderly patients with osteoporosis. Complex three- or four-part fractures often require surgical intervention. Philos locking plates and Multiloc intramedullary nails are widely used, but their comparative effectiveness in osteoporotic elderly patients remains uncertain.
Methods: A retrospective study was performed on 90 elderly patients (aged 70–95 years) with Neer three- or four-part proximal humeral fractures treated between January 2021 and December 2023. Patients received either Philos plate fixation (n = 50) or Multiloc intramedullary nail fixation (n = 40). Clinical data included incision length, operative time, blood loss, complications, and functional outcomes. Pain was assessed via VAS, and shoulder function via Constant-Murley scores at 1 week, 1 month, and 12 months postoperatively.
Results: Both groups achieved fracture healing and functional improvement. Compared to the Philos group, the Multiloc group had shorter incisions, less blood loss, and shorter operative time (all P < 0.05). VAS scores were lower and Constant-Murley scores higher in the Multiloc group at all time points (P < 0.05). Complication rates were lower in the Multiloc group (10% vs. 20%).
Discussion: Both techniques are effective, but Multiloc intramedullary nail fixation offers superior early outcomes and fewer complications. It may be preferable for elderly patients with osteoporotic proximal humeral fractures when proper surgical technique is ensured.
1 Introduction
Proximal humeral fractures are a common type of fracture, accounting for approximately 3%–5% of all fractures (1). Typically caused by external forces, they present with shoulder swelling, pain, and limited mobility, impairing limb function and affecting daily activities (2–3). Conservative treatment is effective for minimally displaced proximal humeral fractures; however, unstable or significantly displaced fractures often require surgical intervention to achieve anatomical reduction, stable fixation, and early mobilization (4, 5). In older patients with osteoporosis, complex proximal humeral fractures involve multiple displacement sites and pose clinically severe injuries. These fractures necessitate timely surgical intervention to restore local anatomy and accelerate fracture healing (6, 7). Philos plate and Multiloc intramedullary nail fixation are commonly used surgical methods for treating proximal humeral fractures, each with distinct characteristics. However, the optimal surgical technique for managing osteoporotic complex fractures remains debated (8–10). This study retrospectively compared the clinical efficacy of Philos plate and Multiloc intramedullary nail fixation in older patients with osteoporotic complex proximal humeral fractures, providing a reference for surgical management.
2 Materials and methods
2.1 Inclusion and exclusion criteria
Patients with radiographic and CT confirmation of a fresh, significantly displaced proximal humeral fractures, classified as Neer three- or four-part fractures, were eligible for inclusion. Preoperative CT scans were routinely performed to evaluate fracture complexity, humeral head position, medial metaphyseal support, and bone loss beneath the humeral head, thereby guiding surgical decision-making. Additional criteria included the absence of significant symptoms of nerve injury, an age range of 70–95 years, treatment with either Philos plate or Multiloc intramedullary nail fixation, and the availability of complete clinical follow-up data.
Exclusion criteria encompassed a history of restricted shoulder joint mobility, the presence of preoperative acute or chronic infections, and severe comorbid internal diseases. Patients with psychiatric disorders and incomplete follow-up data were also excluded.
2.2 Study setting and ethical approval
This retrospective study was conducted at the Department of Orthopedic, Qilu Hospital Dezhou Hospital of Shandong University, Dezhou, China. Patients treated between January 2021 and December 2023 were reviewed. The study protocol was reviewed and approved by the Ethics Committee of Qilu Hospital Dezhou Hospital of Shandong University (2025070). Written informed consent was obtained from all participants prior to data collection and analysis.
2.3 Surgical methods
Both groups underwent surgery under general anesthesia combined with a brachial plexus block. The patients were positioned in a beach chair position, with a soft cushion placed behind the surgical shoulder to ensure sufficient passive flexion and extension of the affected limb during the procedure.
2.3.1 Philos plate group
The deltopectoral approach was employed for the Philos plate group. The cephalic vein was exposed and protected, with the pectoralis major retracted medially and the deltoid laterally to assess the fracture site and evaluate the integrity of the rotator cuff. Hematomas and embedded soft tissues surrounding the fracture were cleared. Fracture reduction is achieved through traction of the forearm, bone leverage, or Kirschner wire assistance. Once satisfactory reduction was confirmed under fluoroscopy, temporary fixation was secured with Kirschner wires. The Philos locking plate was positioned approximately 0.5 cm below the greater tuberosity and 1 cm posterior to the bicipital groove. Distal locking screws were inserted, and the positioning of the screws, plate, and fracture reduction were verified under fluoroscopy. In the presence of rotator cuff damage, it was reinforced intraoperatively using nonabsorbable sutures through the locking holes of the plate. The wound was irrigated with saline, closed in layers, and covered with sterile gauze.
2.3.2 Multiloc intramedullary nail group
In the Multiloc group, a longitudinal incision of approximately 3–5 cm was made along the anterolateral acromion. A layer-by-layer dissection of the skin, subcutaneous tissue, and deltoid muscle was performed while protecting the rotator cuff and neurovascular bundles. Exposure to the greater tuberosity of the humerus allowed for the reduction of the fracture ends, which was temporarily fixed using Kirschner wires under fluoroscopic guidance. A guidewire was inserted through the greater tuberosity into the medullary canal, followed by sequential reaming under C-arm fluoroscopy. A Multiloc intramedullary nail of suitable length was inserted into the distal end of the fracture. The position of the nail was confirmed via intraoperative fluoroscopy, after which proximal and distal locking screws were inserted using a targeting device. The multiplanar angles of the locking screws were adjusted to ensure reliable fixation of both the humeral head and distal fracture end. After confirming satisfactory alignment and secure fixation, the surgical site was thoroughly irrigated. The deltoid muscle, subcutaneous tissue, and skin were closed in layers, and the incision was covered with a sterile dressing.
2.4 Postoperative management
All patients had their affected limbs suspended and immobilized for 6 weeks postoperatively. On the second day post-surgery, patients commenced active and passive functional exercises targeting the elbow, wrist, and finger joints of the affected limb. Shoulder shrugging, pendulum exercises, active/passive forward flexion, and elevation of the affected shoulder were also incorporated. The intensity of the exercises was tailored to maintain mild discomfort, with a visual analog scale (VAS) score of 2–3.
In the PHILOS plate group, excessive shoulder movements—such as abduction, external rotation, and extension—were restricted during the initial 6 weeks postoperatively. Following this period, the forearm sling was removed, and patients began active and passive range-of-motion exercises in all directions. At 12 weeks, progressive resistance and weight-bearing exercises were initiated as tolerated. In contrast, patients in the Multiloc intramedullary nail group were typically permitted—and actively encouraged—to initiate active-assisted and passive shoulder mobilization at an earlier stage. This early rehabilitation strategy was tailored according to the intraoperative assessment of fixation stability and the patient's postoperative comfort, leveraging the superior biomechanical support provided by the intramedullary construct. Particular attention was given to patients with diabetes or other comorbidities associated with a higher risk of joint stiffness. These individuals were closely monitored and received early, supervised physiotherapy to minimize the risk of adhesive capsulitis and to preserve shoulder mobility throughout the recovery period.
2.5 Follow-up and evaluation indicators
The surgical incision length, operative time, intraoperative blood loss, postoperative complications, and fracture healing status were recorded and compared between the two groups. Postoperative pain was assessed using the VAS at one week, one month, and 12 months post-surgery. Shoulder joint function was evaluated using the Constant-Murley score.
2.6 Statistical methods
Data in this study were analyzed using IBM SPSS Statistics version 25.0. The Shapiro–Wilk test was applied to assess the normality of the data distribution, while the Levene test was used to evaluate the homogeneity of variance.
For data conforming to a normal distribution and homogenous variance, results are expressed as mean ± standard deviation (X ± S). For non-normally distributed data, results are presented as median (interquartile range) [M (Q1, Q3)]. Continuous variables were compared between the two groups using an independent sample T-test, and the χ2 test was employed for comparisons of categorical variables. For comparisons of repeated measures within the same group at different time points, the F-test was applied. A P-value of <0.05 was considered statistically significant.
3 Results
3.1 General clinical data
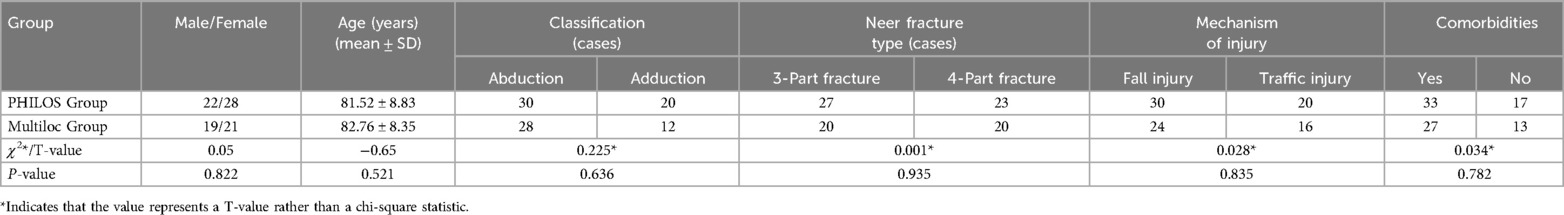
A total of 90 patients with complex proximal humeral fractures treated between January 2021 and December 2023 were included based on the inclusion and exclusion criteria. Patients were categorized into two groups according to the surgical method: the Philos plate (n = 50) and Multiloc intramedullary nail groups (n = 40). No significant differences existed in baseline characteristics, including sex, age, fracture classification, fracture type, mechanism of injury, and comorbidities between the two groups (P > 0.05), indicating comparability (Table 1). This study protocol was approved by the Ethics Committee of our institution, and informed consent was obtained from all enrolled patients.
3.2 Comparison of surgical metrics
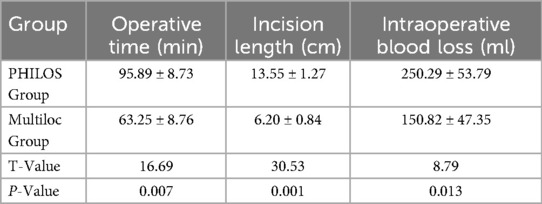
The Multiloc intramedullary nail group exhibited a significantly shorter surgical incision length compared to the PHILOS plate group (6.0 ± 0.8 cm vs. 13.5 ± 1.2 cm, P < 0.05). Intraoperative blood loss was also significantly lower in the Multiloc group than in the PHILOS group (150 ± 40 ml vs. 250 ± 50 ml, P < 0.05). Furthermore, the operative time in the Multiloc group was significantly shorter than that in the PHILOS group (63.25 ± 8.76 min vs. 95.89 ± 8.73 min, P < 0.05), as demonstrated in Table 2.
3.3 Comparison of VAS scores at different time points
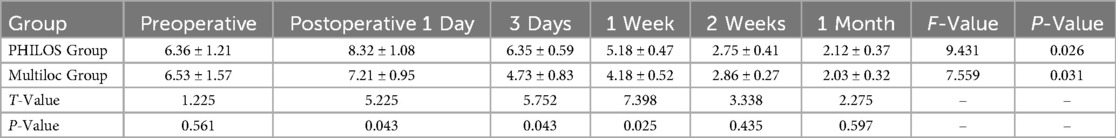
Postoperative VAS scores decreased over time in both groups with no significant differences between them. However, at one day, three days, and one week postoperatively, the PHILOS plate group exhibited significantly higher VAS scores than the Multiloc group (P < 0.05). No significant differences were observed between the two groups at two weeks and one month postoperatively (P > 0.05) (Table 3).
3.4 Comparison of constant-murley shoulder function scores
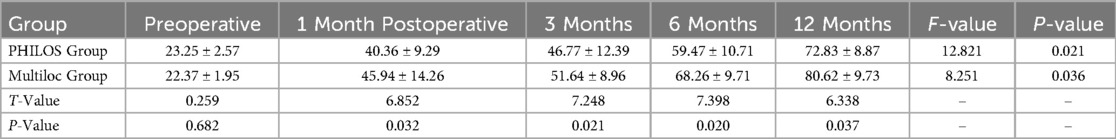
Constant-Murley shoulder function scores demonstrated a significant improvement over time in both groups (P < 0.05). No significant differences existed in preoperative scores between the two groups (P > 0.05). However, at 1, 3, 6, and 12 months postoperatively, the MultiLoc group demonstrated significantly higher shoulder function scores than the PHILOS group (P < 0.05), as shown in Table 4.
3.5 Comparison of postoperative complications
The incidence of postoperative complications was significantly higher in the PHILOS plate group than in the Multiloc group. In the PHILOS group, complications occurred in 20% of cases, including three screw cut-outs, three humeral head varus necroses, and two humeral head malunion. Conversely, the MultiLoc group had a 10% complication rate, with two cases of locking screws loosening and two peri-implant fractures. The difference between the two groups was statistically significant (χ2 = 7.231, P = 0.025).
3.6 Radiographic evaluation indicators
Radiographic assessment at follow-up showed that all patients achieved clinical and radiographic union within the observation period. The mean time to fracture union was 14.2 ± 2.1 weeks in the Multiloc group and 16.8 ± 2.6 weeks in the PHILOS group (P < 0.05). The fracture union rate at 3 months postoperatively was 92.5% (37/40) in the Multiloc group and 84.0% (42/50) in the PHILOS group. The remaining cases achieved union by the 6-month follow-up. No cases of nonunion were observed in either group during the 12-month follow-up period.
4 Discussion
This retrospective study analyzed and compared the efficacy and safety of Philos plate fixation and Multiloc intramedullary nail fixation for treating complex osteoporotic proximal humeral fractures in plder patients. While both methods effectively facilitated fracture healing and restored shoulder function, they differed significantly in postoperative functional recovery, intraoperative characteristics, and complication rates.
The Philos plate, a locking plate with multiple screw holes and an angular locking design, provides excellent biomechanical stability. Compared with traditional plates, it reduces soft tissue irritation and periosteal stripping, thereby preserving the vascular supply to the proximal humerus, thus making it particularly effective in managing osteoporotic fractures (11–13). However, findings from this study indicated that the Philos plate group experienced greater intraoperative blood loss, longer operative times, and higher postoperative VAS scores compared to the Multiloc group, suggesting a potentially significant impact on surrounding soft tissues and vascular supply. Additionally, the Philos plate group exhibited a higher incidence of postoperative complications, including screw cutout and humeral head necrosis, likely related to challenges in screw positioning and achieving precise intraoperative fracture reduction (14, 15). One potential factor contributing to the higher complication rate in the PHILOS group was the lack of intramedullary augmentation beneath the humeral head. In elderly patients with osteoporosis, structural support using autologous iliac crest bone grafts or synthetic bone substitutes may help to prevent humeral head collapse, necrosis, and hardware cut-out. However, in our practice, such augmentation was not routinely performed due to the increased surgical time, invasiveness, and donor site complications associated with bone graft harvesting. The decision to forgo augmentation was made based on intraoperative assessment of fracture stability and bone integrity. Nonetheless, this may represent a limitation in our treatment strategy, and future studies should further explore the role of intramedullary augmentation in optimizing outcomes for elderly patients undergoing plate fixation. To mitigate these risks, surgeons must accurately assess fracture fragments alignment during anatomical reduction and optimize screw length and orientation to prevent postoperative cut-out or loosening (16–18), which are more likely to occur with inexperienced surgeons. Recommendations include the use of precise fluoroscopic guidance to confirm the position and angle of each screw during surgery. Additionally, minimizing soft tissue dissection around the fracture site is essential to preserve humeral head vascularity. Furthermore, implementing individualized rehabilitation plans postoperatively is required (19–21).
Reverse shoulder arthroplasty (RSA) is recognized as an effective treatment option for elderly patients with complex proximal humeral fractures, particularly in cases involving irreparable rotator cuff tears or severe comminution. However, it was not employed in the present cohort. All patients included in this study had either an intact or reparable rotator cuff and adequate proximal humeral bone stock, making them suitable candidates for internal fixation. Furthermore, RSA is associated with higher costs, an increased risk of prosthesis-related complications, and prolonged rehabilitation, especially in resource-limited healthcare settings. At our institution, motion-preserving and joint-conserving surgical techniques are preferred as the first-line approach when stable fixation is feasible. Nevertheless, RSA remains a valuable alternative in selected patients and should be considered when internal fixation is unlikely to yield satisfactory outcomes.
MultiLoc intramedullary nail fixation is a minimally invasive technique offering high stability. Its unique multiplanar locking design enhances humeral head fixation and reduces the risk of fracture redisplacement (22–24). In this study, the Multiloc group demonstrated shorter incision lengths, lower intraoperative blood loss, and superior postoperative shoulder function than the Philos group. These findings suggest that the Multiloc method better preserves surrounding soft tissues and vascular supply, facilitating early postoperative recovery. Furthermore, the Multiloc group had fewer postoperative complications, highlighting its superiority in treating older patients with osteoporosis. The success of Multiloc intramedullary nail fixation depends on the precise selection of the entry point and the reaming technique. Postoperative complications such as proximal humeral refracture may result from inadequate mastery of reaming techniques (25, 26). To optimize surgical outcomes, ensuring precise fluoroscopic guidance during reaming is critical to prevent deviation from the fracture site, carefully position locking screws for stable multiplanar support that minimizes fracture fragment displacement, and to emphasize pain-free rehabilitation postoperatively, while avoiding early weight-bearing to prevent fixation failure (27, 28).
This study also revealed that the surgical method significantly influences early shoulder function recovery. The minimally invasive nature of Multiloc intramedullary nail fixation minimizes damage to the rotator cuff and surrounding soft tissues, thereby promoting superior postoperative recovery of shoulder function. Conversely, although Philos plate fixation offers excellent biomechanical stability in certain cases, the extensive soft tissue dissection required may increase postoperative pain and complications, thereby hindering early functional recovery, particularly in older patients with osteoporosis (29, 30). The Constant-Murley scores in this study demonstrated a significantly better functional recovery in the Multiloc group compared to the PHILOS group at 1, 3, 6, and 12 months postoperatively. This may be attributed to the minimally invasive nature of intramedullary nailing, which reduces soft tissue disruption and preserves rotator cuff integrity. Early initiation of functional exercises, facilitated by the biomechanical stability of the Multiloc construct, may have further contributed to improved shoulder mobility and strength in the early and mid-term phases of recovery. In contrast, although the PHILOS plate provides strong angular stability, the relatively extensive soft tissue exposure and the subacromial impingement potential may delay early mobilization and cause postoperative stiffness, which can negatively affect functional outcomes. These findings are consistent with previous studies reporting faster and more complete functional recovery in patients treated with intramedullary nails, especially in osteoporotic elderly populations.
In addition to functional outcomes, fracture healing was also evaluated and compared between the two groups. The Multiloc group exhibited a significantly shorter mean time to radiographic union (14.2 ± 2.1 weeks) than the PHILOS group (16.8 ± 2.6 weeks), with higher union rates observed at the 3-month follow-up (92.5% vs. 84.0%). This difference may reflect the biological and mechanical advantages of intramedullary fixation, which maintains alignment with minimal periosteal disruption and preserves the fracture hematoma—factors known to facilitate bone healing. Conversely, the longer healing time in the PHILOS group may be partially attributed to the more invasive surgical approach, which requires extensive soft tissue dissection and may impair local vascularity. Although all fractures eventually achieved union in both groups, the faster healing observed with the Multiloc nail could allow for earlier functional recovery and reduced complication risk, particularly in elderly osteoporotic patients who are more susceptible to delayed union.
Shoulder stiffness is a recognized complication following prolonged immobilization, particularly in elderly patients with diabetes. In our protocol, despite sling immobilization for six weeks, early initiation of passive and active-assisted ROM exercises helped minimize this risk. Patients with diabetes received individualized physiotherapy and close follow-up to detect and manage early signs of frozen shoulder. As a result, the incidence of clinically significant postoperative stiffness was low and did not differ substantially between groups. Nonetheless, future protocols may consider shortening sling duration or incorporating earlier aggressive mobilization in select high-risk individuals.
This study is limited by its small sample size and retrospective, single-center design, which may introduce selection bias. Additionally, variations in the surgeon expertise and patient adherence to postoperative rehabilitation protocol may have influenced the outcomes. Future studies should involve larger, multicenter, prospective, and randomized controlled trials to validate these findings and explore the efficacy of alternative surgical methods for treating complex proximal humeral fractures in elderly patients.
Multiloc intramedullary nail fixation demonstrated certain advantages in managing complex osteoporotic fractures in older patients, particularly in terms of functional recovery and complication reduction. In clinical practice, selecting the appropriate surgical method should be based on a comprehensive evaluation of individual patient characteristics and fracture type to achieve optimal treatment outcomes.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
QL: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Writing – original draft, Writing – review & editing. ZC: Conceptualization, Data curation, Formal analysis, Methodology, Project administration, Resources, Software, Writing – review & editing. JL: Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – review & editing. ZL: Methodology, Project administration, Resources, Software, Validation, Visualization, Writing – review & editing. WZ: Conceptualization, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors extend their heartfelt gratitude to all the patients who participated in this study and to their families for their support. We sincerely thank the surgical and nursing teams at Qilu Hospital, Dezhou Hospital of Shandong University, for their dedication and professionalism in patient care and data collection. Special thanks go to the Department of Anesthesiology for their meticulous intraoperative monitoring and management, ensuring the safety of patients with hypertension during the study.We are also grateful to the Institutional Review Board of Qilu Hospital, Dezhou Hospital of Shandong University for approving this study and providing guidance on ethical considerations.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Palvanen M, Kannus P, Niemi S, Parkkari J. Update in the epidemiology of proximal humeral fractures. Clin Orthop Relat Res. (2006) 442:87–92. doi: 10.1097/01.blo.0000194672.79634.78
2. Iglesias-Rodríguez S, Domínguez-Prado DM, García-Reza A, Fernández-Fernández D, Pérez-Alfonso E, García-Piñeiro J, et al. Epidemiology of proximal humerus fractures. J Orthop Surg Res. (2021) 16(1):402. doi: 10.1186/s13018-021-02551-x
3. Relvas Silva M, Linhares D, Leite MJ, Nunes B, Torres J, Neves N, et al. Proximal humerus fractures: epidemiology and trends in surgical management of hospital-admitted patients in Portugal. JSES Int. (2022) 6(3):380–4. doi: 10.1016/j.jseint.2021.12.003
4. Hohmann E, Keough N, Glatt V, Tetsworth K. Surgical treatment is not superior to nonoperative treatment for displaced proximal humerus fractures: a systematic review and meta-analysis. J Shoulder Elbow Surg. (2023) 32(5):1105–20. doi: 10.1016/j.jse.2023.01.002
5. Nho Shane J, Brophy Robert H, Barker Joseph U, Cornell Charles N, MacGillivray John D. Management of proximal humeral fractures based on current literature. JBJS. (2007) 89(suppl_3):44–58. doi: 10.2106/JBJS.G.00648
6. Greenberg A, Rosinsky PJ, Gafni N, Kosashvili Y, Kaban A. Proximal humeral nail for treatment of 3- and 4-part proximal humerus fractures in the elderly population: effective and safe in experienced hands. Eur J Orthop Surg Traumatol. (2021) 31(4):769–77. doi: 10.1007/s00590-020-02832-x
7. Setaro N, Rotini M, Luciani P, Facco G, Gigante A. Surgical management of 2- or 3-part proximal humeral fractures: comparison of plate, nail and K-wires. Musculoskelet Surg. (2022) 106(2):163–7. doi: 10.1007/s12306-020-00686-4
8. Spross C, Platz A, Rufibach K, Lattmann T, Forberger J, Dietrich M. The PHILOS plate for proximal humeral fractures—risk factors for complications at one year. J Trauma Acute Care Surg. (2012) 72(3):783–92. doi: 10.1097/TA.0b013e31822c1b5b
9. Geiger EV, Maier M, Kelm A, Wutzler S, Seebach C, Marzi I. Functional outcome and complications following PHILOS plate fixation in proximal humeral fractures. Acta Orthop Traumatol Turc. (2010) 44(1):1–6. doi: 10.3944/AOTT.2010.2270
10. Jia Z, Li C, Lin J, Liu Q, Li G, Hu X. Clinical effect of using MultiLoc® nails to treat four-part proximal humeral fractures. J Int Med Res. (2020) 48(12):1220778764. doi: 10.1177/0300060520979212
11. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. (1987) 214:160–4.
12. Ethiraj P, Venkataraman S, S J K, Shanthappa A H, Agarawal S. Does proximal humerus inter locking system (PHILOS) plating provide a good functional outcome in proximal humerus fractures? Cureus. (2022) 14(6):e26474. doi: 10.7759/cureus.26474
13. George PK, Dasgupta B, Bhaladhare SM, Reddy B, Jain A, Jogani AD. Functional outcome and complications in management of proximal humerus fractures operated with proximal humerus locking plate. Malays Orthop J. (2021) 15(2):47–54. doi: 10.5704/MOJ.2107.008
14. Oldrini LM, Feltri P, Albanese J, Marbach F, Filardo G, Candrian C. PHILOS Synthesis for proximal humerus fractures has high complications and reintervention rates: a systematic review and meta-analysis. Life. (2022) 12(2):311. doi: 10.3390/life12020311
15. Spross C, Platz A, Erschbamer M, Lattmann T, Dietrich M. Surgical treatment of neer group VI proximal humeral fractures: retrospective comparison of PHILOS® and hemiarthroplasty. Clin Orthop Relat Res. (2012) 470:2035–42. doi: 10.1007/s11999-011-2207-1
16. Mahmoodian A, Yavari P, Fadaei B, Eslami S, Boroujeni MS, Mohammadsharifi G. Outcomes of patients with humerus fracture under treatment with PHILOS plate. Int J Burns Trauma. (2021) 11(1):75.33824789
17. Barlow JD, Sanchez-Sotelo J, Torchia M. Proximal humerus fractures in the elderly can be reliably fixed with a “hybrid” locked-plating technique. Clin Orthop Relat Res. (2011) 469(12):3281–91. doi: 10.1007/s11999-011-1894-y
18. Gönç U, Atabek M, Teker K, Tanrıöver A. Minimally invasive plate osteosynthesis with PHILOS plate for proximal humerus fractures. Acta Orthop Traumatol Turc. (2017) 51(1):17–22. doi: 10.1016/j.aott.2016.10.003
19. Jannelli E, Castelli A, Ferranti CE, Annunziata S, Maccario G, Ivone A, et al. Fractures in patients with COVID-19 infection: early prognosis and management. A case series of 20 patients in a single institution in lombardy, northern Italy. J Orthop Trauma. (2020) 34(10):e389–97. doi: 10.1097/BOT.0000000000001905
20. Salaja BT, Staunton P, Hickey P, Ryan J, Madden SF, Condon F. Unveiling factors influencing mortality in Irish hip fracture patients: a comprehensive five-year analysis. J Arthroplasty. (2025) 40(4):923–8. doi: 10.1016/j.arth.2024.10.012
21. Tanaka S, Osawa Y, Takegami Y, Okui N, Yamauchi KI, Aoki Y, et al. Changes of hip fracture in older patients before and after the COVID-19 pandemic: a retrospective multicentre study in Japan. BMC Musculoskelet Disord. (2024) 25(1):1006. doi: 10.1186/s12891-024-08050-4
22. Chen W, Zhang Z, Zhu C, Song Z, Liu Z. Straight intramedullary MultiLoc nails for displaced proximal humeral fractures: health status, radiographic results, clinical outcome, and complications. BMC Musculoskelet Disord. (2024) 25(1):531. doi: 10.1186/s12891-024-07656-y
23. Katthagen JC, Schwarze M, Bauer L, Meyer-Kobbe J, Voigt C, Hurschler C, et al. Is there any advantage in placing an additional calcar screw in locked nailing of proximal humeral fractures? Orthop Traumat Surg Res. (2015) 101(4):431–5. doi: 10.1016/j.otsr.2015.01.018
24. Martinez-Catalan N, Boileau P. The role of intramedullary nailing for proximal humerus fractures: what works and what does not. Curr Rev Musculoskelet Med. (2023) 16(2):85–94. doi: 10.1007/s12178-022-09816-w
25. Mocini F, Cazzato G, Masci G, Malerba G, Liuzza F, Maccauro G. Clinical and radiographic outcomes after antegrade intramedullary nail fixation of humeral fractures. Injury. (2020) 51:S34–8. doi: 10.1016/j.injury.2020.04.043
26. Kloub M, Holub K, Urban J, Látal P, Peml M, Křivohlávek M. Intramedullary nailing of displaced four-part fractures of the proximal humerus. Injury. (2019) 50(11):1978–85. doi: 10.1016/j.injury.2019.06.029
27. Wu L, Jiang Y, Cao X, Meng X. Efficacies and complications of internal fixations with PHILOS plate and intramedullary multiloc® nails in the surgical treatment of proximal humerus fractures. Am J Transl Res. (2021) 13(10):11786.34786107
28. Lopiz Y, Garríguez-Pérez D, Martínez-Illán M, García-Fernández C, Marco F. Third-generation intramedullary nailing for displaced proximal humeral fractures in the elderly: quality of life, clinical results, and complications. Arch Orthop Trauma Surg. (2022) 142(2):227–38. doi: 10.1007/s00402-020-03678-y
29. Doshi C, Sharma GM, Naik LG, Badgire KS, Qureshi F. Treatment of proximal humerus fractures using PHILOS plate. J Clin Diagn Res. (2017) 11(7):RC10–3. doi: 10.7860/JCDR/2017/26782.10304
Keywords: proximal humerus fracture, PHILOS plate, MultiLoc nail, osteoporosis, functional recovery, fluoroscopy
Citation: Liu Q, Cao Z, Liu J, Liu Z and Zhang W (2025) Comparison of the efficacy of Philos plate and Multiloc intramedullary nail in the treatment of complex proximal humeral fractures with osteoporosis in the elderly. Front. Surg. 12:1606898. doi: 10.3389/fsurg.2025.1606898
Received: 6 April 2025; Accepted: 2 June 2025;
Published: 18 June 2025.
Edited by:
Eugenio Jannelli, IRCCS Policlinico San Matteo Foundation, ItalyReviewed by:
Giuseppe Della Rotonda, pineta grande hospital, ItalyRadu-Dan Necula, Universitatea Transilvania din Brașov, Romania
Copyright: © 2025 Liu, Cao, Liu, Liu and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wenbo Zhang, ZHpzcm15eXp3YkAxNjMuY29t
 Qian Liu
Qian Liu Zongbing Cao
Zongbing Cao Jing Liu2
Jing Liu2