- 1Spine Surgery, Peking University People’s Hospital, Beijing, China
- 2Department of Orthopedic Surgery, 363 Hospital, Chengdu, Sichuan, China
- 3Orthopedics Department, Huailai County Hospital, Zhangjiakou, Hebei, China
Background: High-density pedicle screws provide satisfactory correction in adolescent idiopathic scoliosis (AIS) but add to the operative time, blood loss, and cost; low-density constructs may mitigate these burdens and achieve similar correction results. Studies use inconsistent density cutoffs (most often <1.6 screws/level) and report conflicting results; therefore, we performed a systematic review and meta-analysis to clarify the clinical, radiographic, and economic impact of low screw density in patients with AIS.
Methods: A systematic review and meta-analysis were conducted following PRISMA guidelines. The PubMed, Web of Science, and Embase databases were searched until December 2024 for comparative studies. The outcomes analyzed included surgical and safety parameters (blood loss, operative time, revision rates, and complications), radiographic outcomes (Cobb angle, correction rate, and thoracic kyphosis), and implant costs. Statistical analyses were performed using RevMan 5.4, with fixed- or random-effects models applied on the basis of heterogeneity (I² threshold < 50%).
Results: Twenty-one studies comprising 1,762 patients met the inclusion criteria. Low-density screws were superior in reducing blood loss [mean difference (MD) = −88.06, P = 0.01] and operative time (MD = −22.27, P = 0.02), with no significant difference in revision rates (P = 0.78) or complications (P = 0.64). No differences were observed between the groups in the final Cobb angle (P = 0.4), Cobb correction rate (P = 0.21), or thoracic kyphosis (P = 0.43). The per-level implant cost was lower (standard mean difference = −1.32, P < 0.00001) in the low-density group.
Conclusion: Compared with high-density screws, low-density pedicle screws provide comparable radiographic and safety outcomes while reducing the operative time, blood loss, and cost. These findings support the use of low-density constructs in AIS surgery, although the variability in study designs and screw density definitions warrants further research. Future multicenter randomized controlled trials are needed to refine the optimal screw density strategies for treating AIS.
Systematic Review Registration: https://www.crd.york.ac.uk/PROSPERO/view/CRD420251088403, PROSPERO CRD420251088403.
1 Introduction
Adolescent idiopathic scoliosis (AIS) is a complex three-dimensional spinal deformity (1, 2). Studies have reported that compared with other instruments, pedicle-screw constructs provide enhanced three-dimensional deformity correction, achieve satisfactory three-column fixation, and minimize neurological complications (3–6). Although pedicle-screw constructs provide strong fixation and correction, excessive instrumentation may sacrifice more motion segments than necessary. Optimizing the fusion level and screw density may help limit the fused area and preserve adjacent segment mobility. Moreover, the high cost of AIS surgery is closely related to the use of pedicle screws, which account for a significant proportion of hospital expenses (7, 8). The use of fewer pedicle screws has been shown to reduce hospital costs and decrease the risk of neurological complications (9–11).
Given the cost of pedicle screws, reducing the number of screws improves surgical efficiency and potentially reduces the costs associated with spinal instrumentation. Compared with high-density constructs, low-density pedicle-screw constructions result in shorter operative times and less blood loss (12, 13). The reported cutoffs for low-density screws range from 1.0 to 1.6 screws/level, whereas those for high-density screws range from 1.3 to 2.0 screws/level, creating overlap between categories. Gotfryd and Avanzi (14) reported that there was no significant difference in radiographic corrective outcomes between patients with a density > 1.6 and those with a density < 1.2 (14). Chang et al. (15) reported similar radiographic outcomes between a density of 1.9 and a density of 1.1 (15). However, Ketenci et al. (16) reported that a density of 2 was superior to a density of 1.14 in terms of radiographic outcomes (16). A comprehensive review comparing the efficacy and safety of low- vs. high-density pedicle screws is still lacking.
The aim of this study is to evaluate the efficacy and safety of low-density and high-density pedicle screws in adolescent scoliosis patients by performing a systematic review and meta-analysis of published studies.
2 Methods
Our methodology and reporting of this systematic review followed PRISMA guidelines (17). Systematic review protocol is registered in PROSPERO (CRD420251088403).
2.1 Search strategy
To collect comprehensive published studies, we used the search terms ((pedicle screw density) OR (consecutive pedicle screw) OR (interval pedicle screw)) AND (adolescent idiopathic scoliosis) in PubMed, Web of Science, and Embase, covering the period from the inception of each database to December 2024. Two authors also screened reference lists for additional studies.
2.2 Inclusion criteria
Eligibility criteria were established a priori with the population, intervention, comparison, outcome, study design (PICOS) framework. We included studies—randomized controlled trials (RCTs) and prospective or retrospective cohort studies—that examined surgical treatment of AIS across all Lenke classifications. Eligible studies compared low-density pedicle-screw constructs (<1.6 screws per fused level) with high-density constructs (>1.6 screws per level). We excluded studies on congenital, degenerative, neuromuscular, or neurofibromatosis-associated scoliosis, as well as single-case reports and technical notes. Studies were included if they reported at least one prespecified outcome: intraoperative blood loss, operative time, revision rate, cost per fused level, complication rate, major curve magnitude, thoracic kyphosis, or major curve correction rate—defined as (preoperative Cobb angle − postoperative Cobb angle)/preoperative Cobb angle × 100%. Two reviewers independently screened titles and abstracts retrieved from the search and then assessed the full texts of potentially relevant articles; any disagreements were resolved through discussion and consensus.
2.3 Study selection
Two reviewers independently conducted the study selection in EndNote 20 (Clarivate Analytics, Philadelphia, PA, USA), a reference-management platform that automates duplicate removal and facilitates screening. The screening proceeded in three sequential stages—titles, abstracts, and full texts (18). Any disagreements that arose at any stage were resolved through discussion with the corresponding author until consensus was achieved.
2.4 Risk of bias
For observational studies, two authors independently assessed risk on the basis of the Newcastle–Ottawa scale (NOS) (19). For RCTs, both authors used the Cochrane recommended criteria (20). Following the PRISMA and Cochrane Collaboration criteria, two authors independently assessed the risk of bias in the RCTs in the following areas: (1) random sequence generation, (2) allocation concealment, (3) blinding of participants and personnel, (4) blinding of outcome assessment, (5) incomplete outcome data, (6) selective reporting, and (7) other biases.
2.5 Statistical analysis
The authors performed the analysis with RevMan 5.4 software (The Cochrane Collaboration, Copenhagen, Denmark). The software assessed heterogeneity via the χ2 test and inconsistency index statistics (I2). When significant heterogeneity emerged (I2 > 50%), the analysis adopted a random-effects model. Conversely, in cases of homogeneity (I2 ≤ 50%), a fixed-effects model was used. For effect analysis, the mean difference (MD) and odds ratio (OR) served as the statistical measures for continuous and binary variables, respectively, each accompanied by a 95% confidence interval (CI). In the included studies, the cost of the currency was different. Therefore, in the cost analysis, the standard mean difference (SMD) and 95% CI were applied for analysis.
3 Results
3.1 Summary of the included studies
After screening 1,072 studies, 21 studies (12, 14–16, 21–37) including 1,762 patients were eligible for meta-analysis. The selection process is shown in Figure 1. A total of 884 patients were in the low-density group, 91 were in the medium-density group, and 787 were in the high-density group. Three studies were RCTs (14, 26, 37), and the other 18 were retrospective studies.
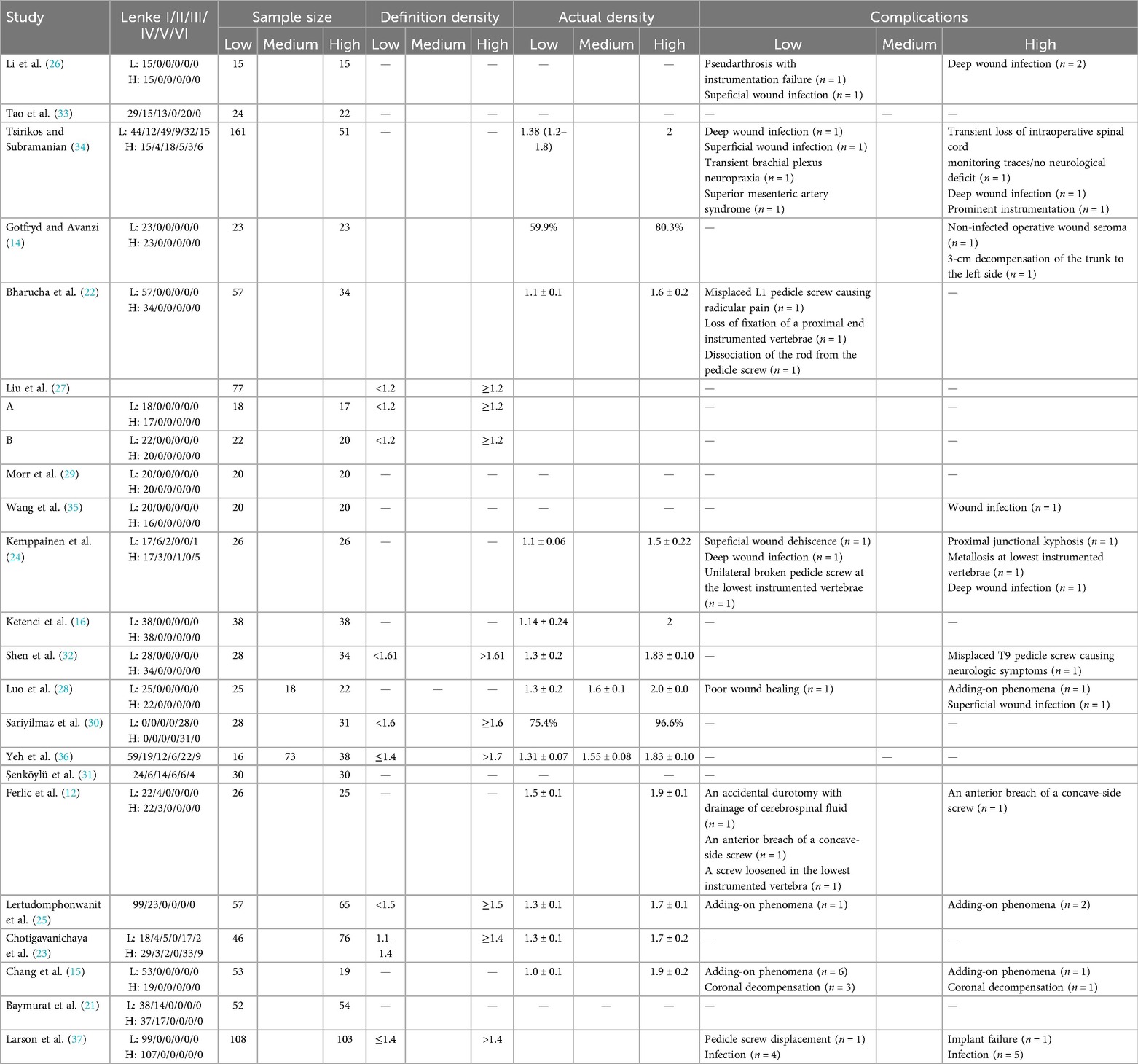
The included studies used different thresholds for defining pedicle-screw density. Low density was generally set at ≤1.0–1.6 screws per fused level (with most papers clustering ∼1.2–1.4 screws/level), whereas high density was defined as >1.4 up to ≥2.0 screws/level. Some studies also introduced an intermediate “medium-density” category. Although the cutoffs varied, this meta-analysis retained the original definitions of each study when classifying cases into low- and high-density groups. The characteristics of the included studies are given in Table 1.
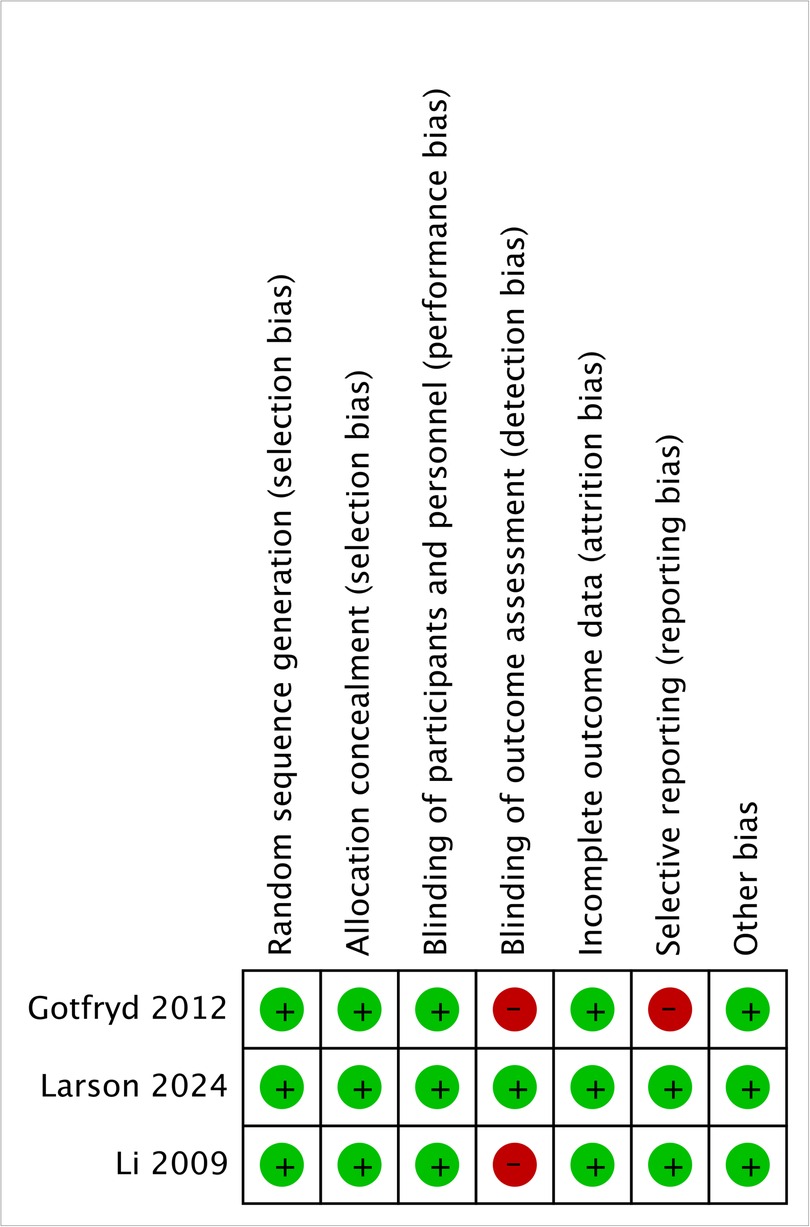
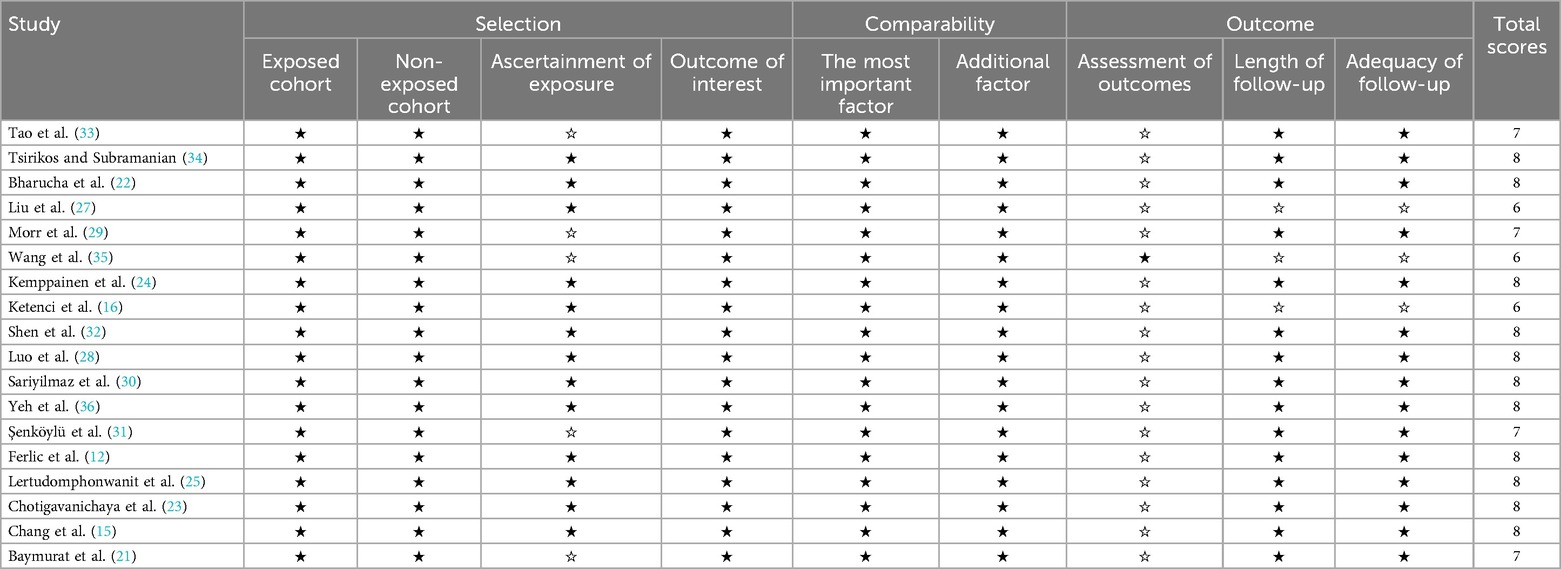
Figure 2 shows that the three included RCTs were evaluated at a low risk of bias for random sequence generation, allocation concealment, performance bias, attrition bias, and other domains; only outcome-assessor blinding and selective reporting displayed isolated high-risk ratings, so their overall methodological quality remained moderate to high. Table 2 shows that, among the 18 cohort studies, 11 earned eight NOS stars, 4 earned seven, and 3 earned six, with none rated ≤5; most point deductions stemmed from follow-up adequacy. Taken together, the available literature provided moderate-to high-quality evidence to support the conclusions of the review, despite some limitations in terms of blinding and follow-up.
3.2 Surgical and safety parameters
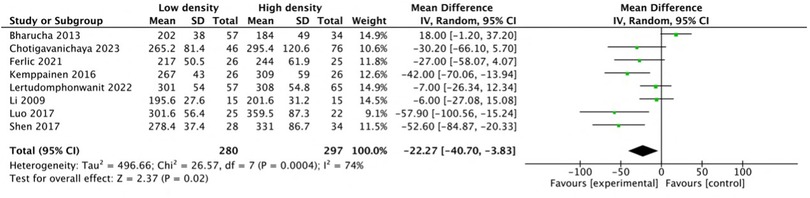
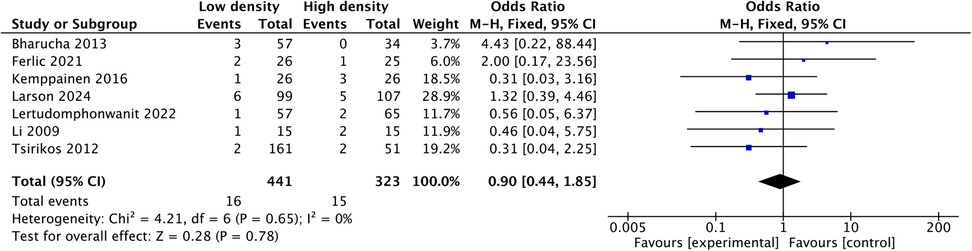
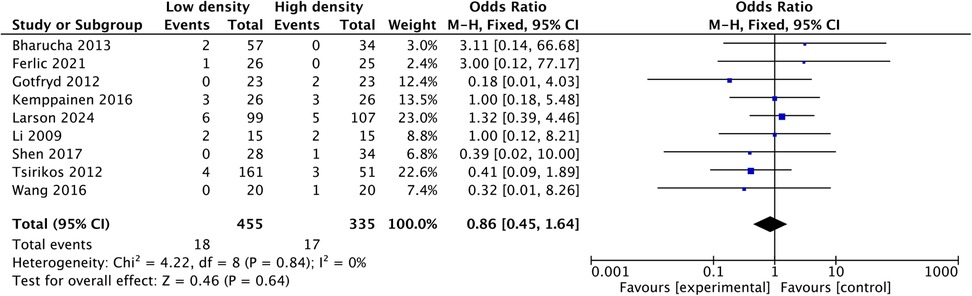
Pooled analysis of seven studies (21, 23–26, 28, 32) revealed that the mean intraoperative blood loss in the low-density group was reduced by 88.06 mL (MD: −88.06; 95% CI: −158.5 to −17.6; P = 0.01; I2 = 33%), as shown in Figure 3. Three studies (24, 28, 32) reported shorter operative times in the low-density group, and five studies (12, 22, 23, 25, 26) reported similar operative times between the two groups. Pooled analysis of eight studies revealed that the operative time decreased by 22.27 min (MD: −22.27, 95% CI: −40.7 to −3.83, P = 0.02; heterogeneity Chi2 = 26.57, df = 7, P = 0.0004, I2 = 74%) in the low-density group, as shown in Figure 4. These gains in surgical efficiency were not offset by increased risk. A pooled analysis of seven studies (12, 22, 24–26, 34, 37) reported similar revision rates (P = 0.78), as shown in Figure 5. The pooled analysis of nine studies (12, 14, 22, 24, 26, 32, 34, 35, 37) revealed similar complication events (P = 0.64), as shown in Figure 6.
3.3 Deformity correction
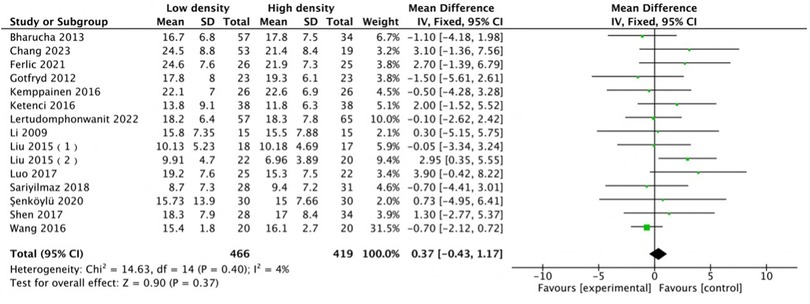
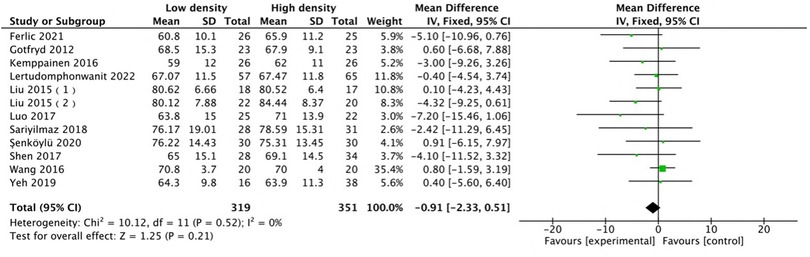
The radiographic results indicated that the two groups were comparable in terms of deformity correction. Among all the included studies, 14 studies (12, 14–16, 22, 24–28, 30–32, 35) with 15 comparison groups were pooled for major Cobb analysis, and the results indicated no difference (MD: 0.37, 95% CI: −0.43 to 1.17, P = 0.37; heterogeneity Chi2 = 14.63, df = 14, P = 0.4, I2 = 4%), as shown in Figure 7. A pooled analysis of the studies (12, 14, 24, 25, 27, 28, 30–32, 35–37) revealed no difference in major curve correction (MD: −0.91, 95% CI: −2.33 to 0.51, P = 0.21; heterogeneity Chi2 = 10.21, df = 11, P = 0.52, I2 = 0%), as shown in Figure 8. With respect to thoracic kyphosis, Liu et al. (27) reported less thoracic kyphosis at the final follow-up in the low-density group. Lertudomphonwanit et al. (25) reported greater thoracic kyphosis. Other studies (12, 14, 16, 22, 24–28, 32, 35) reported no difference between the two groups. Pooled analysis revealed no difference (MD: −1.01, 95% CI: −3.49 to 1.48, P = 0.43; heterogeneity Chi2 = 48.08, df = 11, P < 0.00001, I2 = 77%), as shown in Figure 9.
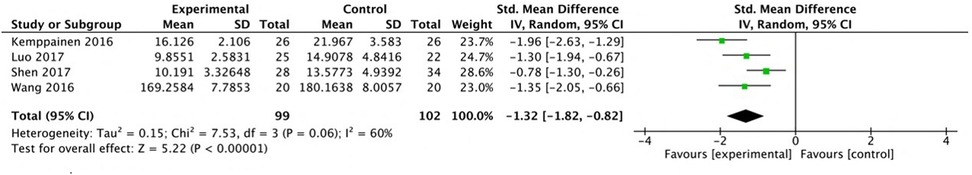
3.4 Implant cost per level
Four studies (24, 28, 32, 38) reported a lower cost per level in the low-density group, and pooled analysis revealed a lower cost (SMD: −1.32, 95% CI: −1.82 to −0.82, P < 0.00001; heterogeneity Chi2 = 7.53, df = 3, P = 0.06, I2 = 60%) in the low-density group, as shown in Figure 10.
4 Discussion
Pedicle-screw constructs have become the standard instrumentation in the treatment of AIS. Because of the three-column anchorage of pedicle screws, more corrective forces can be applied, thus allowing three-dimensional correction of the curve. Despite advancements in pedicle screw techniques and the use of neuromonitoring, surgeons continue to encounter challenges such as neurologic complications, high intraoperative blood loss, and elevated implant costs when high-density screw constructs are used (39–42).
The pedicle screw density is defined as the number of pedicle screws per level of spinal fusion. If low-density constructs prove as efficacious as high-density constructs in correcting the spinal curvature, they could improve surgical efficiency while also significantly reducing implantation costs. Previous studies have not been consistent in their results on the corrective ability of high-density vs. low-density pedicle-screw constructs in AIS (14, 32, 35). Therefore, in this study, we systematically reviewed the literature and performed a meta-analysis to compare low- and high-density screw constructs.
The studies analyzed included AIS patients with mixed Lenke curve types. For completeness, we pooled data from all eligible studies, and the heterogeneity of the outcomes was acceptable. This suggests that the study results were comparable across the included papers.
In clinical studies, low density was superior in reducing blood loss and operative time. These improvements were an expected result of placing fewer screws. Although the differences in blood loss and operative time were statistically significant, their clinical significance needs further evaluation. The pooled analysis revealed that the low-density group had an average blood loss reduction of 88.06 mL, which corresponds to approximately 9.7% of the average intraoperative blood loss in the high-density group. This relative reduction, while modest in absolute terms, may be clinically meaningful in certain populations, such as those with comorbidities or increased bleeding risk. Similarly, the average reduction in operative time in the low-density group was 22.27 min, accounting for approximately 5.6% of the mean operative time in the high-density group. Although not large, a shorter surgical duration may help reduce anesthetic exposure and surgical team fatigue, potentially improving safety in elderly or high-risk patients. There was no difference between the two methods in terms of complications. Although the use of more pedicle screws could theoretically increase the risk of screw-related damage or prolong surgery, in the included studies, the surgeries were performed by experienced surgeons (minimizing any learning curve issues) (43). There was no difference in complications such as nerve damage or pedicle screw misplacement. The current study did not evaluate whether surgeon expertise influenced the results. This may represent a potential confounding factor, as operative experience can significantly impact complication rates, surgical precision, and operative efficiency.
Given the advantages of low-density screws in terms of a shorter operative time and less bleeding, the current controversy over low-density screws vs. high-density screws focuses on the ability of low-density screws to achieve comparable correction capacity and maintain long-term results. In this study, a meta-analysis of the radiographic parameters reported in the included studies was performed to obtain more plausible results in the form of an expanded sample size. There was no difference between low-density and high-density screws in terms of the final Cobb angle, Cobb angle correction, or final follow-up of thoracic kyphosis. In scoliosis surgery, screws provide the point at which the implanted rods are anchored. Studies have shown that the quality of the screw anchorage points is more important than the quantity (44). The stability of the screw as an anchoring point is critical. A strong anchorage point can more effectively carry and distribute the corrective forces applied to the spine. Even with many anchorage points, if these are not stable enough, it will be difficult to effectively correct scoliosis or maintain correction. Properly placed screws not only are more tightly integrated into the spine but also reduce the risk of bone damage and implant loosening (45, 46). Importantly, even a small number of screws, when properly placed, can achieve good orthopedic results. During scoliosis correction, a balanced distribution of forces is more crucial than the magnitude of any single force. High-quality anchorage points distribute corrective forces more efficiently, reducing the stress on any single segment (38, 44, 47).
Although implant density is an important factor in optimizing the outcomes and cost-effectiveness of surgery for AIS, it should not be considered in isolation. The extent of spinal fusion—particularly the upper instrumented vertebra (UIV) and lower instrumented vertebra (LIV)—plays a critical role in balancing deformity correction with postoperative mobility. Recent biomechanical studies have demonstrated that, compared with simply increasing the number of screws, the positioning of anchor points, construct configuration, and screw quality have a more significant impact on the load distribution and construct stability (48, 49). Computer-based biomechanical studies have also shown that individualized correction strategies and preoperative objectives influence radiographic outcomes more than implant density alone does (50). However, in this systematic review, most included studies did not consistently report UIV and LIV selections or stratify results on the basis of the fusion range, which represents a limitation. Therefore, future studies should comprehensively consider fusion level selection, construction strategies, and implant density to optimize both correction outcomes and functional preservation in AIS surgery.
The high cost of AIS surgery is closely related to the use of expensive pedicle screws, which account for a significant proportion of hospital expenses (8, 51). The use of fewer pedicle screws has been shown to reduce hospital costs and decrease the risk of neurological complications. Consistent with our findings, multiple studies reported lower costs with low-density constructs, and our meta-analysis confirmed this trend. Larson et al. (52) examined the NIS database for AIS cases in the US and reported that switching from high-density to low-density screw patterns would reduce total national costs by an estimated $11–$20 million annually (52).
The limitations of this study were as follows: (1) Most of the studies included were retrospective studies, and only two were high-quality RCTs. In addition, the sample size in two RCTs was limited (30 and 46 total patients). The bias introduced was unavoidable. (2) A major limitation of the study was the lack of uniform definitions for low- and high-density screw constructs across the included studies. This inconsistency may have introduced clinical heterogeneity, potentially masking subtle differences in correction capacity or complication profiles. While overall statistical heterogeneity was acceptable, future studies should adopt standardized density thresholds or explore the dose-dependent effects of screw number to clarify optimal construct strategies. (3) The included studies exhibited variability in curve classification and deformity severity. Although the meta-analysis demonstrated acceptable and comparable heterogeneity, the lack of uniformity in baseline characteristics limited the precision of pooled estimates. Future research should aim for more standardized study designs with consistent definitions of curve type and severity. (4) Sufficient data on detailed curve characteristics were lacking. In cases of severe deformity—such as curves exceeding 90°, significant rotation, or high stiffness—implants with greater mechanical stability may be needed to achieve effective correction and long-term integrity. Moreover, the selection of the UIV and LIV is crucial, as it directly affects not only the corrective capacity and construct stability but also the risk of junctional complications. However, most of the included studies did not provide detailed information on curve length, rigidity, or specific UIV/LIV selection strategies, which limited further analysis of the interaction between screw density and fusion-level configuration. This limitation highlights the need for future research to better define the relationships among curve characteristics, the fusion range, and the implant strategy to optimize individualized surgical planning in patients with AIS. (5) Follow-up periods varied across different articles. Three studies had a follow-up period of 1 year, which was not long enough. The remaining studies had follow-up periods of at least 2 years, but there are still differences among them.
5 Conclusion
Compared with high-density screws, low-density pedicle screws reduced the operative time and blood loss in patients who had undergone AIS surgery. Importantly, this low-density approach did not increase complication or revision rates. Low-density pedicle screws achieved similar Cobb angles and Cobb angle corrections and maintain thoracic kyphosis comparable to that of high-density screws at the final follow-up. The cost per level was lower for low-density pedicle screws.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, and further inquiries can be directed to the corresponding author.
Author contributions
BZ: Writing – review & editing, Investigation, Data curation, Writing – original draft. QZ: Writing – review & editing, Writing – original draft, Methodology. XL: Methodology, Writing – original draft, Writing – review & editing, Validation. KM: Data curation, Writing – review & editing. ZQ: Investigation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Kadoury S, Labelle H. Classification of three-dimensional thoracic deformities in adolescent idiopathic scoliosis from a multivariate analysis. Eur Spine J. (2012) 21:40–9. doi: 10.1007/s00586-011-2004-2
2. Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet. (2008) 371(9623):1527–37. doi: 10.1016/s0140-6736(08)60658-3
3. Barr SJ, Schuette AM, Emans JB. Lumbar pedicle screws versus hooks: results in double major curves in adolescent idiopathic scoliosis. Spine. (1997) 22(12):1369–79. doi: 10.1097/00007632-199706150-00016
4. Suk S-I, Kim J-H, Kim S-S, Lim D-J. Pedicle screw instrumentation in adolescent idiopathic scoliosis (AIS). Eur Spine J. (2012) 21(1):13–22. doi: 10.1007/s00586-011-1986-0
5. Lehman RA Jr, Lenke LG, Keeler KA, Kim YJ, Buchowski JM, Cheh G, et al. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine. (2008) 33(14):1598–604. doi: 10.1097/BRS.0b013e318178872a
6. Crawford AH, Lykissas MG, Gao X, Eismann E, Anadio J. All-pedicle screw versus hybrid instrumentation in adolescent idiopathic scoliosis surgery: a comparative radiographical study with a minimum 2-year follow-up. Spine. (2013) 38(14):1199–208. doi: 10.1097/BRS.0b013e31828ce597
7. Raudenbush BL, Gurd DP, Goodwin RC, Kuivila TE, Ballock RT. Cost analysis of adolescent idiopathic scoliosis surgery: early discharge decreases hospital costs much less than intraoperative variables under the control of the surgeon. J Spine Surg. (2017) 3(1):50–7. doi: 10.21037/jss.2017.03.11
8. Bozzio AE, Hu X, Lieberman IH. Cost and clinical outcome of adolescent idiopathic scoliosis surgeries-experience from a nonprofit community hospital. Int J Spine Surg. (2019) 13(5):474–8. doi: 10.14444/6063
9. Roach JW, Mehlman CT, Sanders JO. Does the outcome of adolescent idiopathic scoliosis surgery justify the rising cost of the procedures? J Pediatr Orthop. (2011) 31(1):S77–80. doi: 10.1097/BPO.0b013e3181f73bfd
10. Martin CT, Pugely AJ, Gao Y, Mendoza-Lattes SA, Ilgenfritz RM, Callaghan JJ, et al. Increasing hospital charges for adolescent idiopathic scoliosis in the United States. Spine. (2014) 39(20):1676–82. doi: 10.1097/brs.0000000000000501
11. Kamerlink JR, Quirno M, Auerbach JD, Milby AH, Windsor L, Dean L, et al. Hospital cost analysis of adolescent idiopathic scoliosis correction surgery in 125 consecutive cases. J Bone Joint Surg Am. (2010) 92(5):1097–104. doi: 10.2106/jbjs.I.00879
12. Ferlic PW, Hauser L, Götzen M, Lindtner RA, Fischler S, Krismer M. Correction of adolescent idiopathic scoliosis using a convex pedicle screw technique with low implant density. Bone Joint J. (2021) 103(3):536–41. doi: 10.1302/0301-620X.103B3.BJJ-2020-0760.R1
13. Kilinc BE, Tran DP, Johnston C. Comparison of implant density in the management of Lenke 1B and 1C adolescent idiopathic scoliosis. Acta Ortop Bras. (2019) 27(1):33–7. doi: 10.1590/1413-785220192701189400
14. Gotfryd AO, Avanzi O. Randomized clinical study on surgical techniques with different pedicle screw densities in the treatment of adolescent idiopathic scoliosis types Lenke 1A and 1B. Spine Deform. (2013) 1:272–9. doi: 10.1016/j.jspd.2013.05.004
15. Chang SY, Kim JH, Mok S, Chang B-S, Lee C-K, Kim H. The use of high-density pedicle screw construct with direct vertebral derotation of the lowest instrumented vertebra in selective thoracic fusion for adolescent idiopathic scoliosis: comparison of two surgical strategies. Asian Spine J. (2023) 17(2):338–46. doi: 10.31616/asj.2022.0111
16. Ketenci IE, Yanik HS, Demiroz S, Ulusoy A, Erdem S. Three-dimensional correction in patients with Lenke 1 adolescent idiopathic scoliosis comparison of consecutive versus interval pedicle screw instrumentation. Spine. (2016) 41(2):134–8. doi: 10.1097/BRS.0000000000001182
17. Higgins JPT, Altman DG, Gotzsche PC, Juni P, Moher D, Oxman AD, et al. The Cochrane collaboration’s tool for assessing risk of bias in randomised trials. Br Med J. (2011) 343:d5928. doi: 10.1136/bmj.d5928
18. Bramer WM, Milic J, Mast F. Reviewing retrieved references for inclusion in systematic reviews using EndNote. J Med Libr Assoc. (2017) 105(1):84–7. doi: 10.5195/jmla.2017.111
19. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol. (2010) 25(9):603–5. doi: 10.1007/s10654-010-9491-z
20. Lundh A, Gøtzsche PC. Recommendations by Cochrane Review groups for assessment of the risk of bias in studies. BMC Med Res Methodol. (2008) 8:1–9. doi: 10.1186/1471-2288-8-22
21. Baymurat AC, Yapar A, Kilicaslan OF, Tokgoz MA, Selcuk H, Yas S, et al. Intermittent pedicle screw application provides better kyphosis restoration in adolescent idiopathic scoliosis for Lenke type 1 and type 2 curves. Eur Spine J. (2023) 32(6):2213–20. doi: 10.1007/s00586-023-07669-6
22. Bharucha NJ, Lonner BS, Auerbach JD, Kean KE, Trobisch PD. Low-density versus high-density thoracic pedicle screw constructs in adolescent idiopathic scoliosis: do more screws lead to a better outcome?. Spine J. (2013) 13(4):375–81. doi: 10.1016/j.spinee.2012.05.029
23. Chotigavanichaya C, Adulkasem N, Pisutbenya J, Ruangchainikom M, Luksanapruksa P, Wilartratsami S, et al. Comparative effectiveness of different pedicle screw density patterns in spinal deformity correction of small and flexible operative adolescent idiopathic scoliosis: inverse probability of treatment weighting analysis. Eur Spine J. (2023) 32(6):2203–12. doi: 10.1007/s00586-023-07615-6
24. Kemppainen JW, Morscher MA, Gothard MD, Adamczyk MJ, Ritzman TF. Evaluation of limited screw density pedicle screw constructs in posterior fusions for adolescent idiopathic scoliosis. Spine Deform. (2016) 4(1):33–9. doi: 10.1016/j.jspd.2015.07.010
25. Lertudomphonwanit T, Berry CA, Jain VV, Sturm PF. Does implant density impact three-dimensional deformity correction in adolescent idiopathic scoliosis with Lenke 1 and 2 curves treated by posterior spinal fusion without Ponte osteotomies? Asian Spine J. (2021) 16(3):375–85. doi: 10.31616/asj.2020.0398
26. Li M, Shen Y, Fang X, Ni J, Gu S, Zhu X, et al. Coronal and sagittal plane correction in patients with Lenke 1 adolescent idiopathic scoliosis: a comparison of consecutive versus interval pedicle screw placement. J Spinal Disord Tech. (2009) 22(4):251–6. doi: 10.1097/BSD.0b013e3181884940
27. Liu H, Li Z, Li S, Zhang K, Yang H, Wang J, et al. Main thoracic curve adolescent idiopathic scoliosis: association of higher rod stiffness and concave-side pedicle screw density with improvement in sagittal thoracic kyphosis restoration. J Neurosurg Spine. (2015) 22(3):259–66. doi: 10.3171/2014.10.SPINE1496
28. Luo M, Shen M, Wang W, Xia L. Comparison of consecutive, interval, and skipped pedicle screw techniques in moderate Lenke type 1 adolescent idiopathic scoliosis. World Neurosurg. (2017) 98:563–70. doi: 10.1016/j.wneu.2016.11.064
29. Morr S, Carrer A, Alvarez-García de Quesada LI, Rodriguez-Olaverri JC. Skipped versus consecutive pedicle screw constructs for correction of Lenke 1 curves. Eur Spine J. (2015) 24(7):1473–80. doi: 10.1007/s00586-015-3769-5
30. Sariyilmaz K, Ozkunt O, Karademir G, Gemalmaz HC, Dikici F, Domanic U. Does pedicle screw density matter in Lenke type 5 adolescent idiopathic scoliosis? Medicine. (2018) 97(2):e9581. doi: 10.1097/md.0000000000009581
31. Şenköylü A, Çetinkaya M, Daldal İ, Eren A, Aktaş E. The implant density does not change the correction rate of the main and the accompanying curves: a comparison between consecutive and intermittent pedicle screw constructs. Acta Orthop Traumatol Turc. (2020) 54(3):293. doi: 10.5152/j.aott.2020.03.16
32. Shen M, Jiang H, Luo M, Wang W, Li N, Wang L, et al. Comparison of low density and high density pedicle screw instrumentation in Lenke 1 adolescent idiopathic scoliosis. BMC Musculoskelet Disord. (2017) 18(1):336. doi: 10.1186/s12891-017-1695-x
33. Tao F, Zhao Y, Wu Y, Xie Y, Li M, Lu Y, et al. The effect of differing spinal fusion instrumentation on the occurrence of postoperative crankshaft phenomenon in adolescent idiopathic scoliosis. J Spinal Disord Tech. (2010) 23(8):e75–80. doi: 10.1097/BSD.0b013e3181d38f63
34. Tsirikos A, Subramanian A. Posterior spinal arthrodesis for adolescent idiopathic scoliosis using pedicle screw instrumentation: does a bilateral or unilateral screw technique affect surgical outcome? J Bone Joint Surg Br. (2012) 94(12):1670–7. doi: 10.1302/0301-620X.94B12.29403
35. Wang F, Xu X-M, Lu Y, Wei X-Z, Zhu X-D, Li M. Comparative analysis of interval, skipped, and key-vertebral pedicle screw strategies for correction in patients with Lenke type 1 adolescent idiopathic scoliosis. Medicine (Baltimore). (2016) 95(10):e3021. doi: 10.1097/MD.0000000000003021
36. Yeh Y-C, Niu C-C, Chen L-H, Chen W-J, Lai P-L. The correlations between the anchor density and the curve correction of adolescent idiopathic scoliosis surgery. BMC Musculoskelet Disord. (2019) 20(1):1–10. doi: 10.1186/s12891-019-2844-1
37. Larson AN, Polly DW, Sponseller PD, Kelly MP, Richards BS, Garg S, et al. The effect of implant density on adolescent idiopathic scoliosis fusion: results of the minimize implants maximize outcomes randomized clinical trial. J Bone Joint Surg Am. (2024) 106(3):180–9. doi: 10.2106/jbjs.23.00178
38. Wang X, Aubin C-E, Crandall D, Parent S, Labelle H. Biomechanical analysis of 4 types of pedicle screws for scoliotic spine instrumentation. Spine. (2012) 37(14):E823–35. doi: 10.1097/BRS.0b013e31824b7154
39. Mulpuri K, Perdios A, Reilly CW. Evidence-based medicine analysis of all pedicle screw constructs in adolescent idiopathic scoliosis. Spine. (2007) 32(19):S109–14. doi: 10.1097/BRS.0b013e318134eaa3
40. Yilmaz G, Borkhuu B, Dhawale AA, Oto M, Littleton AG, Mason DE, et al. Comparative analysis of hook, hybrid, and pedicle screw instrumentation in the posterior treatment of adolescent idiopathic scoliosis. J Pediatr Orthop. (2012) 32(5):490–9. doi: 10.1097/BPO.0b013e318250c629
41. Mendiratta A, Emerson RG. Neurophysiologic intraoperative monitoring of scoliosis surgery. J Clin Neurophysiol. (2009) 26(2):62–9. doi: 10.1097/WNP.0b013e31819f9049
42. Pastorelli F, Di Silvestre M, Plasmati R, Michelucci R, Greggi T, Morigi A, et al. The prevention of neural complications in the surgical treatment of scoliosis: the role of the neurophysiological intraoperative monitoring. Eur Spine J. (2011) 20:105–14. doi: 10.1007/s00586-011-1756-z
43. Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine. (2010) 35(11):E465–70. doi: 10.1097/BRS.0b013e3181d1021a
44. Wang X, Aubin CE, Robitaille I, Labelle H. Biomechanical comparison of alternative densities of pedicle screws for the treatment of adolescent idiopathic scoliosis. Eur Spine J. (2012) 21(6):1082–90. doi: 10.1007/s00586-011-2089-7
45. Wang X, Larson AN, Polly DW Jr., Aubin CE. Biomechanical computational study of pedicle screw position and density in adolescent idiopathic scoliosis instrumentation. Spine. (2023) 48(20):1436–45. doi: 10.1097/brs.0000000000004742
46. Wang X, Larson AN, Crandall DG, Parent S, Labelle H, Ledonio CGT, et al. Biomechanical effect of pedicle screw distribution in AIS instrumentation using a segmental translation technique: computer modeling and simulation. Scoliosis Spinal Disord. (2017) 12(1):13. doi: 10.1186/s13013-017-0120-4
47. Chen J, Yang C, Ran B, Wang Y, Wang C, Zhu X, et al. Correction of Lenke 5 adolescent idiopathic scoliosis using pedicle screw instrumentation: does implant density influence the correction? Spine. (2013) 38(15):E946–51. doi: 10.1097/BRS.0b013e318297bfd4
48. La Barbera L, Larson AN, Aubin CE. How do spine instrumentation parameters influence the 3D correction of thoracic adolescent idiopathic scoliosis? A patient-specific biomechanical study. Clin Biomech. (2021) 84:105346. doi: 10.1016/j.clinbiomech.2021.105346
49. La Barbera L, Larson AN, Rawlinson J, Aubin CE. In silico patient-specific optimization of correction strategies for thoracic adolescent idiopathic scoliosis. Clin Biomech. (2021) 81:105200. doi: 10.1016/j.clinbiomech.2020.105200
50. La Barbera L, Larson AN, Aubin CE. Correction objectives have higher impact than screw pattern and density on the optimal 3D correction of thoracic AIS: a biomechanical study. Spine Deform. (2021) 9(3):655–64. doi: 10.1007/s43390-020-00275-2
51. Jaquith BP, Chase A, Flinn P, Sawyer JR, Warner WC, Freeman BL, et al. Screws versus hooks: implant cost and deformity correction in adolescent idiopathic scoliosis. J Child Orthop. (2012) 6(2):137–43. doi: 10.1007/s11832-012-0400-8
Keywords: adolescent idiopathic scoliosis, screw density, high density, low density, deformity
Citation: Zheng B, Zhou Q, Liu X, Ma K and Qiang Z (2025) Low-density pedicle screw in adolescent idiopathic scoliosis: a systematic review and meta-analysis of 1,762 patients. Front. Surg. 12:1607323. doi: 10.3389/fsurg.2025.1607323
Received: 7 April 2025; Accepted: 10 July 2025;
Published: 30 July 2025.
Edited by:
Luca Ambrosio, Campus Bio-Medico University, ItalyReviewed by:
Luigi La Barbera, Polytechnic University of Milan, ItalyTao Li, Shandong Provincial Hospital, China
Copyright: © 2025 Zheng, Zhou, Liu, Ma and Qiang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zhe Qiang, cWlhbmd6aGVfc3BpbmVAc2luYS5jb20=
 Bin Zheng
Bin Zheng Qiang Zhou2
Qiang Zhou2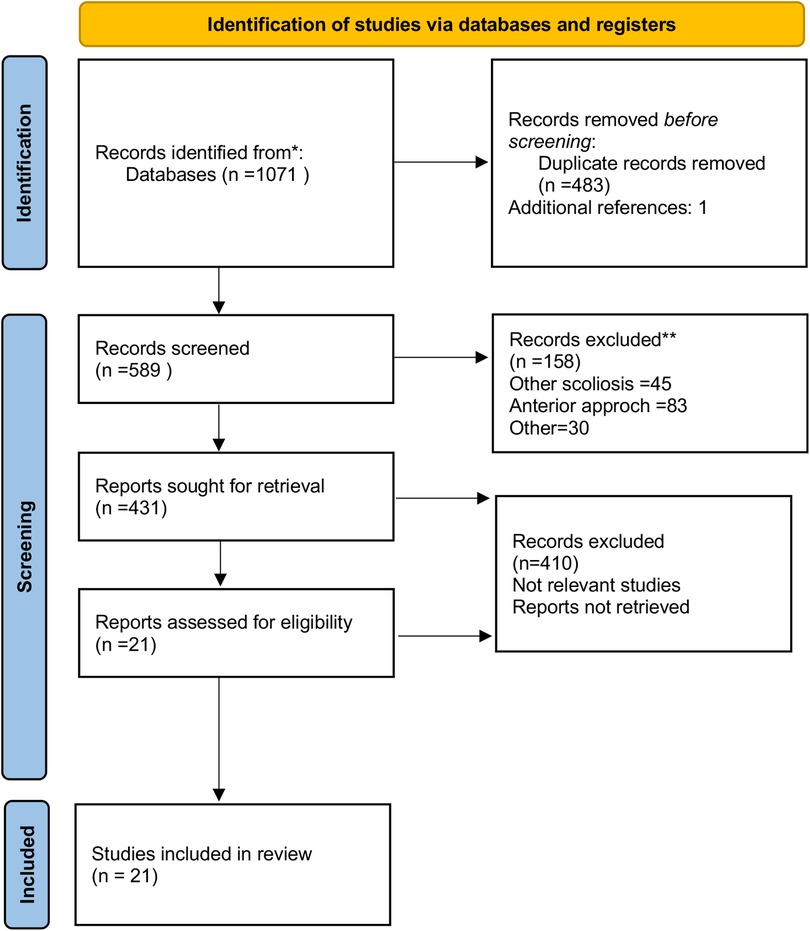
![Forest plot depicting mean differences between low and high density groups across seven studies, with a total effect estimate of -88.06 [95% CI: -158.50, -17.63]. The overall test shows statistical significance with Z = 2.45, p = 0.01. Each study's result is marked by a square with horizontal lines representing confidence intervals, and a diamond indicates the total pooled effect. Heterogeneity is noted with I² = 33%.](https://www.frontiersin.org/files/Articles/1607323/fsurg-12-1607323-HTML/image_m/fsurg-12-1607323-g003.jpg)
![Forest plot showing a meta-analysis of studies comparing low and high-density treatments. Each study lists mean, standard deviation, total, and weight. The mean difference with 95% confidence intervals is shown on the right. The overall pooled mean difference is \\(-1.01\\) [\\(-3.49\\), \\(1.48\\)] with heterogeneity \\(I^2 = 77\\%\\). The diamond at the bottom represents the overall effect size, suggesting no significant difference between groups.](https://www.frontiersin.org/files/Articles/1607323/fsurg-12-1607323-HTML/image_m/fsurg-12-1607323-g009.jpg)