- 1Department of Ultrasonic, Ningbo Yinzhou No.2 Hospital, Ningbo, Zhejiang, China
- 2Department of Infection, Ningbo Yinzhou No.2 Hospital, Ningbo, Zhejiang, China
Bone cement leakage is a relatively common complication following percutaneous vertebroplasty (PVP); however, cement migration to the heart via the venous system is rare, causing severe chest pain and dyspnea. This case reports an 80-year-old male who presented to the Department of Infectious Diseases with mild fever, 2 months after undergoing PVP for a compression fracture of the third lumbar vertebra. A chest computed tomography initially misidentified the lesion as a pacemaker lead within the right ventricle. However, echocardiography revealed that the distal bone cement was embedded in the myocardium of the right ventricular apex, leading to the diagnosis of bone cement leakage. Thereafter, the patient underwent an open-chest procedure with direct cardiac visualization for cement removal in the cardiac surgery department.
1 Introduction
Percutaneous vertebroplasty (PVP) is a widely used minimally invasive procedure for managing vertebral compression fractures. It involves injecting bone cement into the compressed vertebra to restore structural integrity and alleviate pain (1). As its use has expanded, reports of complications have increased, most notably bone cement leakage (2). The typical pathway for cement migration into the right ventricle is through the perivertebral venous system, which connects the vertebral venous plexus to the inferior vena cava and, ultimately, to the right atrium and ventricle (3). In severe cases, this can lead to intracardiac and pulmonary artery embolism, posing potentially life-threatening risks. Although cardiac perforation due to bone cement leakage is a recognized complication, several patients with intracardiac cement remain asymptomatic, often diagnosed incidentally, indicating that the potential risk remains underestimated (4). In this case, bone cement leakage was identified in the right ventricle via echocardiography 2 months after PVP. On computed tomography (CT), it was strikingly similar to a pacemaker lead. Due to its distinct shape and relatively stable position, the leaked cement did not cause further cardiac perforation or significant symptoms.
2 Case description
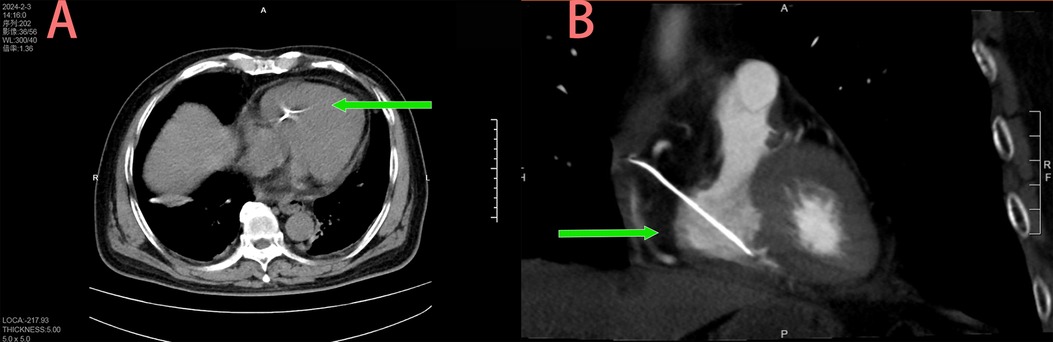
An 80-year-old male was admitted to the Department of Infectious Diseases with a 1-day history of fever and no cardiac symptoms. The patient had no history of hypertension, diabetes mellitus, renal dysfunction, hyperlipidemia, blood transfusion, trauma, smoking, alcohol consumption, or hereditary diseases. A chest CT, performed to investigate suspected respiratory tract infection, revealed a structure resembling a pacemaker lead within the right heart (Figures 1A,B). Electrocardiography showed sinus rhythm, while laboratory tests revealed that cardiac troponin I levels were within the normal limits. In addition, inflammatory markers were abnormally elevated. Transthoracic echocardiography identified an elongated, hyperechoic, rigid foreign body spanning the right ventricle and atrium (Figure 2A). The object exhibited no mobility relative to the heart and had its distal end embedded in the myocardium of the right ventricular apex; hence, no motion or free end was observed. Mild tricuspid regurgitation and pericardial effusion were observed. In the short-axis view of the great arteries, the foreign body extended into the right ventricular outflow tract (Figure 2B). The echocardiographic findings were initially misinterpreted as a pacemaker lead in the right ventricle. The patient was initially diagnosed with a fever of unknown infectious origin. Therefore, initial treatment consisted of intravenous ceftriaxone (2.0 g once daily) for anti-infective therapy in the Department of Infection. After 2 days of treatment, the fever resolved, and inflammatory markers decreased, indicating the effectiveness of the anti-infective therapy. However, further inquiry revealed that the patient had undergone PVP for osteoporotic compression fracture of the third lumbar vertebra 2 months earlier. A multidisciplinary team composed of doctors from the Departments of Infectious Diseases, Ultrasound, and Radiology, confirmed that the patient had no history of pacemaker implantation. Based on the echocardiographic and CT images, intracardiac bone cement leakage was diagnosed. After thorough discussion of the risks associated with the intracardiac foreign body, the patient consented to surgical intervention in the Department of Cardiac Surgery.
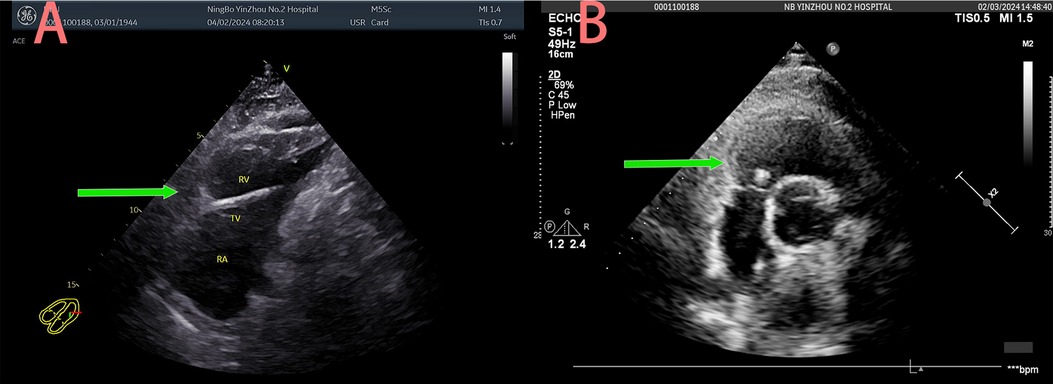
Figure 2. Right ventricle and atrium of hyperechoic foreign body (A) right ventricular outflow tract of hyperechoic foreign body (B).
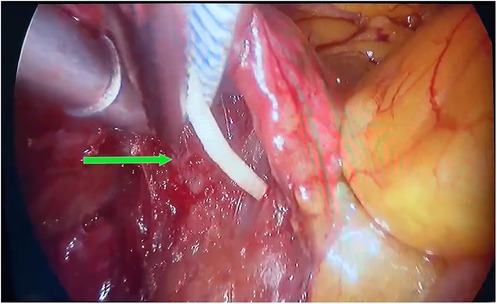
To prevent further severe complications, the cardiac surgeon proceeded with surgical excision. A 5-cm incision was made at the fourth intercostal space of the right anterolateral chest wall, along with a 1-cm endoscopic port at the sixth intercostal space of the right midaxillary line. Upon opening the pericardium superior to the right phrenic nerve, a rigid, rod-shaped white protrusion of bone cement was observed in the right atrium (Figure 3 and Supplementary Video S1). Cardiac surgeons initially attempted en bloc removal of the bone cement using vascular forceps through a minimally invasive approach. Unfortunately, the cement fragmented during the extraction attempts. Subsequently, cardiopulmonary bypass was initiated with induced cardiac arrest, followed by right atriotomy under direct visualization. The tricuspid valve was fully exposed and opened, revealing bone cement located on the right ventricular surface at the junction with the anterior diaphragm, which was subsequently removed (Supplementary Figure S1). Although the procedure proceeded smoothly, the patient's intraoperative blood loss was approximately 1,000 ml. Considering the patient's venerable age and to minimize postoperative complications, he was transferred to the ICU for 2 days of observation and discharged on postoperative day 12 for routine follow-up.
3 Discussion
This case involved an 80-year-old male who presented with mild fever and was diagnosed with bone cement leakage into the right ventricle. PVP is a widely used, minimally invasive procedure for treating osteoporotic vertebral compression fractures in the elderly. It primarily involves injecting polymethylmethacrylate into the vertebrae to stabilize the bone and alleviate pain. Bone cement leakage, affecting 30%–65% of patients with osteoporotic vertebral collapse after surgery, is a relatively common complication of PVP (5). While symptoms of leakage vary, severe complications such as pulmonary embolism and cardiac perforation can be fatal (6). Ziad et al. reported that intracardiac bone-cement embolism is a rare complication of PVP or kyphoplasty (7). The bone cement typically enters the right ventricle through the perivertebral venous system, which connects the vertebral venous plexus to the inferior vena cava and ultimately reaches the right atrium and ventricle (3, 8). The incidence of severe complications from bone cement leakage ranges from 2% to 11.5%, emphasizing the importance of early detection and management for patient prognosis (5). Common symptoms of intracardiac embolism are chest pain and dyspnea, which can manifest days, months, or even years after surgery (9). In this case, the patient presented with low-grade fever 2 months after PVP without significant chest pain or dyspnea, offering a rare and unique diagnostic perspective.
In a retrospective study, Zhang et al. performed a polynomial logistic analysis to identify risk factors contributing to segmental venous (S-type) leakage, including sex, cement dispersion type, presence of basal vertebral foramen or fissures, fracture severity, and posterior wall invasion (10). In this study, an 80-year-old male patient presented with a moderate wedge compression fracture of the L3 vertebra and underwent PVP via a bilateral transpedicular approach. The bone cement demonstrated a diffuse distribution pattern, meeting the high-risk criteria defined by Zhang et al. (10). However, these predisposing factors were not adequately identified by the initial clinical team during the perioperative period. This case highlights the critical importance of early identification of patients with high-risk profiles to prevent potential complications. Currently, bone cement leakage is primarily diagnosed through imaging, with CT considered the gold standard (5). In this case, echocardiography combined with CT imaging enabled accurate diagnosis and guided subsequent surgical treatment. Echocardiography offers real-time visualization of bone cement mobility, assessment of cardiac valve structure and function, and facilitates timely repeat examinations. In patients with limited mobility, echocardiography can be performed at the bedside, which is an advantage.
On echocardiography, leaked bone cement may appear as a hyperechoic structure, which may resemble a pacemaker lead, potentially leading to misdiagnosis. The misdiagnosis primarily stemmed from the overlapping echocardiographic characteristics of the two entities, both appearing as hyperechoic linear foreign bodies with similar morphologic features on two-dimensional imaging, potentially obscured by thrombus-induced acoustic interference. This diagnostic challenge was exacerbated by inadequate multiplanar dynamic tracking due to operator inexperience, particularly the failure to systematically assess the fixation of the foreign body to the myocardium using standardized views such as the apical four-chamber and subcostal long-axis projections. Additionally, limited clinical reasoning led to the omission of critical integration of surgical history and multimodality imaging, including cardiac CT angiography. The rarity of the condition and limited clinical awareness among practitioners further compounded the diagnostic dilemma. Key echocardiographic differentiators between intracardiac bone cement emboli and pacemaker leads include anatomic location, imaging characteristics, and pathophysiological features. Bone cement emboli typically lodge deep within the myocardium of the right ventricular inflow tract or free wall, presenting as hyperechoic signals with irregular surfaces and characteristic comet-tail artifacts, with fixed proximal ends that show slight undulation due to blood flow (11). In contrast, pacemaker leads are typically anchored at the apical or septal regions, characterized by smooth spiral configurations, synchronized motion with the cardiac cycle, and intact endothelial coverage (12). Suboptimal echocardiographic resolution and limited clinical experience may increase the likelihood of misinterpretation, thereby delaying accurate diagnosis. Several studies support surgical removal as the preferred treatment for symptomatic intracardiac embolism, given the risks associated with conservative management, including perforation, pericardial tamponade, severe valvular dysfunction, and sudden death (5, 13, 14). This case aims to raise awareness among clinicians about the potential complications of PVP, thereby facilitating early diagnosis, treatment, and prevention of severe outcomes. Overall, while cardiac complications resulting from bone cement leakage are relatively rare, their potential risks should not be underestimated. Echocardiography serves as an effective diagnostic tool, enabling the early detection of bone cement leakage and assessment of its effect on the cardiac function.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of Ningbo Yinzhou No.2 Hospital Registration No. 2025-003. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
DK: Writing – original draft, Investigation, Conceptualization, Writing – review & editing. XX: Resources, Writing – original draft, Methodology, Supervision. YJ: Supervision, Visualization, Writing – review & editing. YZ: Writing – review & editing, Conceptualization, Supervision, Investigation.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The study was supported by the Medical Health Science and Technology Project of Zhejiang Province (grant no. 2024KY1608).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2025.1608784/full#supplementary-material
Supplementary Figure S1 | Fragmented bone cement specimen retrieved during surgery.
References
1. Hou JG, Zhang N, Chen GD. Factors affecting cement leakage in percutaneous vertebroplasty: a retrospective cohort study of 309 patients. Eur Rev Med Pharmacol Sci. (2023) 27(9):3877–86. doi: 10.26355/eurrev_202305_32293
2. Rose LD, Bateman G, Ahmed A. Clinical significance of cement leakage in kyphoplasty and vertebroplasty: a systematic review. Eur Spine J. (2024) 33(4):1484–9. doi: 10.1007/s00586-023-08026-3
3. Groen RJ, du Toit DF, Phillips FM, Hoogland PV, Kuizenga K, Coppes MH, et al. Anatomical and pathological considerations in percutaneous vertebroplasty and kyphoplasty: a reappraisal of the vertebral venous system. Spine. (2004) 29(13):1465–71. doi: 10.1097/01.BRS.0000128758.64381.75
4. Schoechlin S, Schröfel H, Czerny M, Siepe M, Ahlgrim C, Zeller T, et al. Massive cardiopulmonary cement embolism with cardiac perforation after vertebroplasty: a case series. Eur Heart J Case Rep. (2022) 6(9):ytac385. doi: 10.1093/ehjcr/ytac385
5. Zhan Y, Jiang J, Liao H, Tan H, Yang K. Risk factors for cement leakage after vertebroplasty or kyphoplasty: a meta-analysis of published evidence. World Neurosurg. (2017) 101:633–42. doi: 10.1016/j.wneu.2017.01.124
6. Deng K, Yu JL, Feng YJ, Huang K, Wu GF. Case report: inspiration from a rare fatal heart perforation after percutaneous vertebroplasty. Front Surg. (2023) 10:1227056. doi: 10.3389/fsurg.2023.1227056
7. Audat ZA, Alfawareh MD, Darwish FT, Alomari AA. Intracardiac leakage of cement during kyphoplasty and vertebroplasty: a case report. Am J Case Rep. (2016) 17:326–30. doi: 10.12659/AJCR.897719
8. Duijvelshoff R, Anthonissen NFM, Morshuis WJ, Van Garsse L. Intracardiac cement embolism resulting in tricuspid regurgitation. Eur J Cardiothorac Surg. (2019) 55(2):366–8. doi: 10.1093/ejcts/ezy233
9. Fadili Hassani S, Cormier E, Shotar E, Drir M, Spano JP, Morardet L, et al. Intracardiac cement embolism during percutaneous vertebroplasty: incidence, risk factors and clinical management. Eur Radiol. (2019) 29(2):663–73. doi: 10.1007/s00330-018-5647-0
10. Zhang K, She J, Zhu Y, Wang W, Li E, Ma D. Risk factors of postoperative bone cement leakage on osteoporotic vertebral compression fracture: a retrospective study. J Orthop Surg Res. (2021) 16(1):183. doi: 10.1186/s13018-021-02337-1
11. Huang C. Life-threatening intracardiac cement embolisms after percutaneous kyphoplasty: a case report and literature review. J Int Med Res. (2022) 50(5):3000605221102088. doi: 10.1177/03000605221102088
12. Almomani A, Siddiqui K, Ahmad M. Echocardiography in patients with complications related to pacemakers and cardiac defibrillators. Echocardiography. (2014) 31(3):388–99. doi: 10.1111/echo.12483
13. Pan HY, Wu TY, Chen HY, Wu JY, Liao MT. Intracardiac cement embolism: images and endovascular treatment. Circ Cardiovasc Imaging. (2021) 14(4):e011849. doi: 10.1161/CIRCIMAGING.120.011849
Keywords: percutaneous vertebroplasty, bone cement leakage, echocardiography, computed tomography, case report
Citation: Kong D, Xie X, Jin Y and Zhang Y (2025) Case Report: Bone cement leakage in the right heart: a rare case of misinterpreted echocardiographic findings. Front. Surg. 12:1608784. doi: 10.3389/fsurg.2025.1608784
Received: 9 April 2025; Accepted: 20 June 2025;
Published: 4 July 2025.
Edited by:
Osvaldo Mazza, Bambino Gesù Children's Hospital (IRCCS), ItalyReviewed by:
Han Wu, Jilin University, ChinaBhanu Maturi, University of Alabama at Birmingham, United States
Copyright: © 2025 Kong, Xie, Jin and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yong Jin, eW9uZ2ppbjE5OTNAMTYzLmNvbQ==; Yizhen Zhang, emhhbmd5aXpoZW5zbWlsZUAxNjMuY29t
†These authors have contributed equally to this work and share first authorship
 Dongji Kong1,†
Dongji Kong1,† Yong Jin
Yong Jin