- Department of Neurosurgery, Mahatma Gandhi Memorial Medical College and Maharaja Yeshwantrao Hospital, Indore, Madhya Pradesh, India
Lower cranial nerve palsy is a rare condition, most commonly caused by malignant skull base lesions or internal carotid artery dissection, and only rarely resulting from trauma. We report two cases of road traffic accident victims presenting with lower cranial nerve palsy involving cranial nerves IX, X, and XI. Both patients had similar clinical complaints. The most important findings were a dislocated occipital condyle fracture and suspected associated soft tissue injury. Both were treated conservatively with a rigid cervical collar. A nasogastric tube was required for the first patient during the initial recovery period due to severe dysphagia, while the second patient tolerated oral intake and did not require enteral feeding. Both patients showed gradual improvement in symptoms during hospitalization and follow-up. These injuries, with their often subtle clinical presentation, may be easily overlooked and require prompt detection to prevent complications.
Introduction
Lower cranial nerve palsy is a rare condition, attributed to malignant skull base lesions such as multiple myeloma (1), metastasis of prostate cancer (2, 3), internal carotid dissection (4, 5), hypoglossal schwannoma (6), and Jefferson fracture (7, 8), among other causes. Symptoms can present slowly over time or suddenly (i.e., after trauma), depending on the cause, which affects the prognosis. Lower cranial nerve palsy is also associated with occipital condyle fractures (OCF) as described by Bell in 1817 (9). These injuries are rarely reported in the literature, and it is unclear whether these fractures are rare or underdiagnosed. They have been seen more frequently during the past decade, which may be due to the increased use of computed tomography (CT) and magnetic resonance imaging (MRI) scans (10, 11). These fractures are typically accompanied by other injuries of the cervical spine and are rarely seen as isolated injuries. One study found that 22% of patients with OCF had associated injuries of the cervical spine, with the majority of injuries being fractures of C1 and C2 vertebrae (12). In 1915, Collet became the first person to describe “glossolaryngoscapulopharyngeal” hemiplegia in a patient with a gunshot injury to the mastoid, which involved the four lower cranial nerves (13). Two years later, in 1917, Sicard described it as “The syndrome of the condyloposterior lacerated foramen” (14) with clinical presentations of hoarseness, difficulty swallowing (cranial nerves IX and X), and shoulder and neck weakness (cranial nerve XI), after which it came to be known as the Collet–Sicard Syndrome. We report two cases of lower cranial nerve palsy with occipital condyle fracture due to a road traffic accident (RTA). These injuries with subtle clinical symptoms may be overlooked and need prompt attention to avoid complications.
Case report
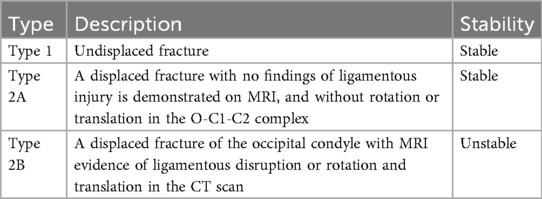
A 26-year-old woman presented to the emergency department following an RTA. At presentation, the Glasgow Coma Score (GCS) of the patient was E4V5M6, but she was clinically drowsy and easily roused with a normal bilateral pupillary response. She had no associated injury. On examination, the patient had normal motor and sensory responses in all four limbs. Local examination revealed contusions over the left mastoid region and the left lateral aspect of the neck. An non-contrast computed tomography (NCCT) brain scan was performed, which was suggestive of a fracture of the left occipital condyle with a lacerated fragment in the foramen magnum extending into the jugular foramen (Figures 1a–c). The right occipital bone was also fractured. The patient began to experience difficulty swallowing, accompanied by regurgitation of liquid from the nose. She showed signs of IX and X cranial nerve palsy. On examination, she also had left winging of the scapula, indicating XI cranial nerve palsy. MRI was advised, which showed mild pre-vertebral soft tissue thickening with no compression over any neural structure by a dislocated fragment or any ligament instability (Figure 2). She was managed conservatively and fitted with a hard cervical collar, and she remained hospitalized for 7 days. Over the 7 days, she was fed via a nasogastric tube, which was removed as her swallowing function improved. Gradually, her symptoms improved. At a follow-up examination 3 months after the injury, she had achieved complete recovery with minimal residual neck pain.
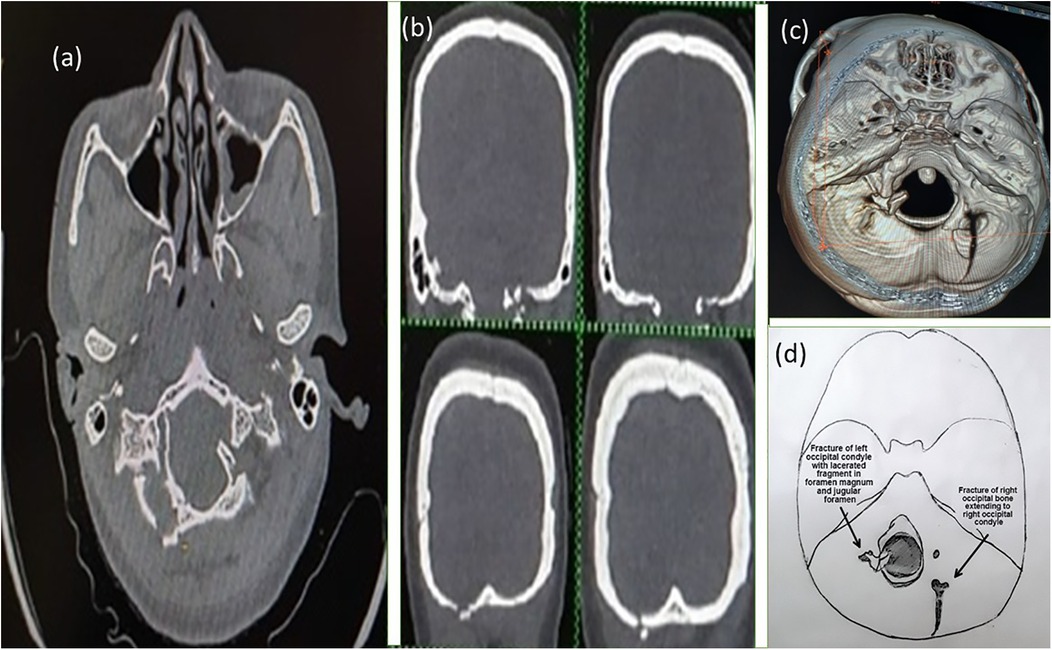
Figure 1. Axial (a) and coronal (b) section NCCT scan of the first patient with virtual reconstruction (c) and pictorial diagram (d) of the fracture (axial craniocaudal view).
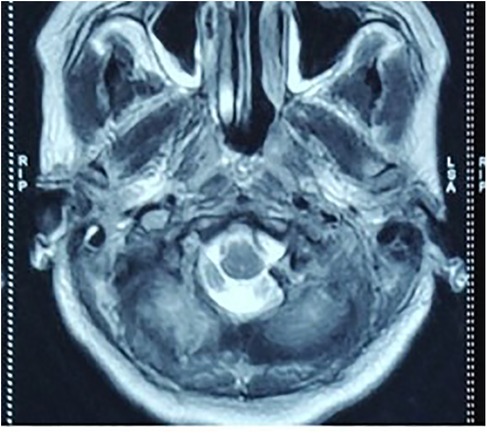
Figure 2. MRI of the first patient showing a lacerated fragment of the fractured occipital condyle in the foramen magnum without any neurovascular compression.
Another patient, a 45-year-old man, following an RTA, presented to the hospital with GCS E4V5M6, without any other injury. The following day, the patient began to notice hoarseness of voice, difficulty swallowing, and limited movement in the right shoulder. An NCCT brain scan was done, which was suggestive of a fracture of the right mastoid bone with extension to the occipital bone and a comminuted, undisplaced fracture of the right occipital condyle with a small chip in the jugular foramen (Figure 3). He was managed conservatively and fitted with a hard cervical collar for 3 months. His swallowing difficulty was mild due to which nasogastric tube feeding was not required. He showed improvement in his symptoms and remained symptom-free after 3 months.
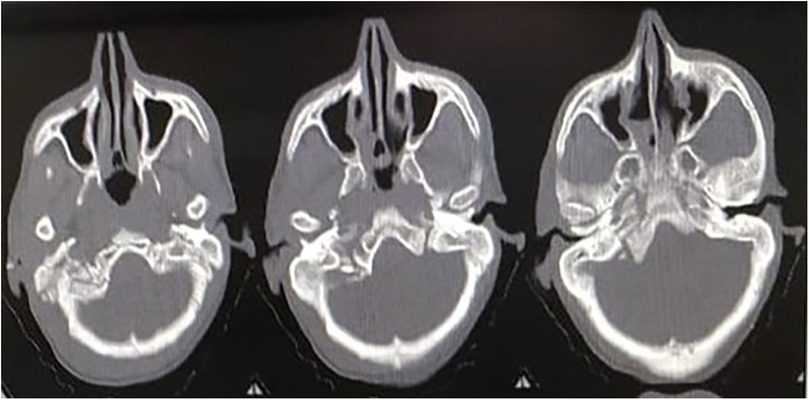
Figure 3. NCCT of the second patient showing a comminuted, undisplaced fracture of the right occipital condyle with a small chip in the jugular foramen.
At the 3-month follow-up, both patients had complete resolution of lower cranial nerve deficits. The first patient reported only minimal residual neck pain, while the second patient remained entirely asymptomatic. Both patients actively participated in their care and recovery. The first patient reported that, initially, swallowing with oral intake was difficult and stressful, making nasogastric feeding uncomfortable but necessary. She appreciated the guidance and support from the neurosurgeon and noted a gradual improvement in her swallowing as the first week progressed. By 3 months, she expressed satisfaction with her recovery and minimal residual neck discomfort.
The second patient, with milder symptoms, reported only minor difficulty with swallowing and hoarseness, which did not significantly affect daily activities. He found the cervical collar manageable and experienced no significant discomfort or limitation during the treatment period. Both patients underscored the importance of careful monitoring by and communication with the treating team, which helped them cope with the rare and complex nature of their injuries.
Discussion
The clinical symptoms shown by both patients were cranial nerve palsy of cranial nerves IX, X, and XI. Neither of the patients had weakness in any limb or dysfunction of the bowel or bladder. Occipital condyle fractures are generally caused by high-energy blunt trauma. In most cases, neurological deficits are attributed more to the severity of the head and neck injury than to the occipital condyle fracture itself. Such patients generally have polytrauma and do not survive the initial trauma (15). Both patients developed paralysis of the sternocleidomastoid and trapezius muscles and hoarseness in addition to difficulty swallowing with a deviation of the palate, indicating palsy of cranial nerves IX, X, and XI. The most important findings in our case report were a dislocated occipital condyle fracture and suspected soft tissue injury. Alar ligament thickening, stretching, or discontinuity is a useful, direct CT sign of disruption, but we cannot confidently diagnose the integrity of the alar ligaments using these criteria because of the frequent presence of minor positional asymmetry (16). Anderson and Montesano (17) published a classification guideline in 1988 based on a retrospective review of six patients who were scanned using either CT or conventional tomography. Tuli et al. modified the above guidelines in 1997 (18), determining instability according to CT and MRI scans, considering the extent of ligamentous injury and occiput-C1-C2 rotation and translation. Tuli et al. divided the classification into three types, based on dislocation, rotation, and translation of the O-C1-C2 complex and ligamentous injury verified by MRI (Table 1).
The first patient had a type 2A fracture, and the second patient had a type 1 fracture. The palsy of cranial nerves IX, X, and XI was likely already present directly after the accident, which was noticed the next day in both patients after starting the oral diet. Hanson et al. supported the hypothesis that disruption of all craniocervical ligaments is required for complete occipitoatlantal dissociation, and stabilization of a unilateral condyle avulsion fracture is maintained by an intact contralateral alar ligament and tectorial membrane (16). Both of our patients were RTA victims, consistent with prior studies identifying RTAs as the most frequent cause of cranial nerve injuries (19, 20). While Basheer et al. and Swamiyappan et al. reported facial nerve (CN VII) palsy as the most common injury, Coello et al. identified the olfactory nerve (CN I) as the most common cranial nerve involved in head injury patients; however, all three studies noted that lower cranial nerve (IX–XII) involvement was rare (19–21). In contrast, our patients developed isolated lower cranial nerve deficits (IX–XI) following occipital condyle fractures, with no involvement of the more commonly affected nerves. The likely biomechanical mechanism in our patients was a combination of axial loading and lateral bending, producing occipital condyle fractures with fracture fragments extending toward the jugular foramen. However, the exact mechanism is still unclear. This close anatomical relationship predisposes cranial nerves IX, X, and XI to stretching, avulsion, or compression. The absence of persistent compression on MRI, along with eventual complete recovery, suggests that transient nerve stretch or traction was the most plausible mechanism, consistent with prior reports of lower cranial neuropathy in occipital condyle fractures.
Immobilization with a hard collar is recommended in stable OCF without bone fragment displacement because it could migrate with head movements (22). There is no sufficient evidence showing that patients treated with a hard neck collar have a better outcome than patients who do not receive any treatment. Most studies recommend treatment of occipital condyle fractures with a hard neck collar or a halo frame for 6–12 weeks. Tuli et al. (18) recommended that undisplaced fractures without ligamentous injury (type 1) not be immobilized, but that type 2A fractures should be treated with a hard collar. Type 2B should be treated with a halo vest or by surgical fixation. There are reports of three patients (12) with potentially unstable fractures who were operated on to remove the dislocated fragment. In these cases, all patients showed improvement in cranial nerve palsy; however, it is unclear whether the surgery was responsible for the recovery of nerve function. The strength of our study lies in the detailed clinical documentation, radiological correlation, and adherence to conservative management protocols with favorable outcomes. However, limitations must be acknowledged. With only two cases, the findings cannot be generalized to all patients with occipital condyle fractures. Furthermore, while CT and MRI scans demonstrated fracture configuration and ruled out gross instability, subtle ligamentous or axonal injuries could not be confirmed, limiting the certainty of the proposed mechanisms of cranial nerve palsy. The follow-up period of 3 months, though adequate to document recovery, does not exclude the possibility of delayed instability or recurrence. Despite these limitations, our cases add to the sparse literature describing Collet–Sicard syndrome following occipital condyle fractures, particularly involving cranial nerves IX–XI, which is less frequently reported than XII nerve palsy.
Conclusion
Lower cranial nerve palsy following occipital condyle fracture is a rare but clinically important manifestation of craniocervical trauma. These two cases highlight the potential for IX, X, and XI cranial nerve involvement due to the proximity of the jugular foramen to the occipital condyle—an association less commonly reported than hypoglossal nerve involvement. Although direct compression by the dislocated fragment cannot be excluded, axonal injury from traction or nerve root avulsion is the more likely mechanism, with onset probably occurring immediately after the accident. This study contributes to the limited literature on Collet–Sicard syndrome secondary to occipital condyle fractures and underscores the importance of prompt cranial nerve examination along with targeted CT and MRI of the craniocervical junction. Early recognition enables appropriate conservative management and can lead to favorable neurological recovery.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by MGM Medical College, Indore, Madhya Pradesh. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written informed consent was obtained from the individual(s), and minor(s)' legal guardian/next of kin, for the publication of any potentially identifiable images or data included in this article.
Author contributions
SG: Writing – original draft, Writing – review & editing. RG: Formal analysis, Project administration, Writing – review & editing. ZS: Conceptualization, Writing – review & editing. AB: Data curation, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Tappin JA, Satchi G, Corless JA, Ashworth F. Multiple myeloma presenting as the Collet-Sicard syndrome. J Neurol Neurosurg Psychiatry. (1996) 60(1):14. doi: 10.1136/jnnp.60.1.14
2. Prashant R, Franks A. Collet-Sicard syndrome—a report and review. Lancet Oncol. (2003) 4(6):376–7. doi: 10.1016/s1470-2045(03)01097-0
3. Wilson H, Johnson DH. Jugular foramen syndrome as a complication of metastatic cancer of the prostate. South Med J. (1984) 77(1):92–3. doi: 10.1097/00007611-198401000-00029
4. Waespe W, Niesper J, Imhof HG, Valavanis A. Lower cranial nerve palsies due to internal carotid dissection. Stroke. (1988) 19(12):1561–4. doi: 10.1161/01.str.19.12.1561
5. Walker S, McCarron MO, Flynn PA, Watt M. Left internal carotid artery dissection presenting with headache, Collet-Sicard syndrome and sustained hypertension. Eur J Neurol. (2003) 10(6):731–2. doi: 10.1046/j.1468-1331.2003.00662.x
6. Garcia-Escrivà A, Pampliega Pérez A, Martín-Estefania C, Botella C. Síndrome de Collet-Sicard como presentación de schwannoma del nervio hipogloso [Schwannoma of the hypoglossal nerve presenting as a syndrome of Collet-Sicard]. Neurologia. (2005) 20(6):311–3.
7. Connolly B, Turner C, DeVine J, Gerlinger T. Jefferson fracture resulting in Collet-Sicard syndrome. Spine. (2000) 25(3):395–8. doi: 10.1097/00007632-200002010-00023
8. Hsu HP, Chen ST, Chen CJ, Ro LS. A case of Collet-Sicard syndrome associated with traumatic atlas fractures and congenital basilar invagination. J Neurol Neurosurg Psychiatry. (2004) 75(5):782–4. doi: 10.1136/jnnp.2003.024083
10. Blacksin MF, Lee HJ. Frequency and significance of fractures of the upper cervical spine detected by CT in patients with severe neck trauma. AJR Am J Roentgenol. (1995) 165(5):1201–4. doi: 10.2214/ajr.165.5.7572503
11. Link TM, Schuierer G, Hufendiek A, Horch C, Peters PE. Substantial head trauma: value of routine CT examination of the cervicocranium. Radiology. (1995) 196(3):741–5. doi: 10.1148/radiology.196.3.7644638
12. Alcelik I, Manik KS, Sian PS, Khoshneviszadeh SE. Occipital condylar fractures. Review of the literature and case report. J Bone Joint Surg Br. (2006) 88(5):665–9. doi: 10.1302/0301-620X.88B5.16598
13. Collet FJ. Sur un novueau syndrome paralytique pharyngolarynge par blessure de guerre (Hemiplegie glosso-laryngo-scapulo-pharyngee). Lyon Med. (1915) 124:121–9.
14. Sicard J. Syndrome de carrefour condylo-dechire posterieur (type purde paralysie laryngee assiciee). Marseille Med. (1917) 53:383.
15. Bucholz RW, Burkhead WZ, Graham W, Petty C. Occult cervical spine injuries in fatal traffic accidents. J Trauma. (1979) 19(10):768–71. doi: 10.1097/00005373-197910000-00009
16. Hanson JA, Deliganis AV, Baxter AB, Cohen WA, Linnau KF, Wilson AJ, et al. Radiologic and clinical spectrum of occipital condyle fractures: retrospective review of 107 consecutive fractures in 95 patients. AJR Am J Roentgenol. (2002) 178(5):1261–8. doi: 10.2214/ajr.178.5.1781261
17. Anderson PA, Montesano PX. Morphology and treatment of occipital condyle fractures. Spine. (1988) 13(7):731–6. doi: 10.1097/00007632-198807000-00004
18. Tuli S, Tator CH, Fehlings MG, Mackay M. Occipital condyle fractures. Neurosurgery. (1997) 41(2):368–77. doi: 10.1097/00006123-199708000-00006
19. Basheer N, Varghese JC, Kuruvilla R, Alappat JP, Mathew J. A prospective study on the incidence and outcome of cranial nerve injuries in patients with traumatic brain injuries. Indian J Neurotrauma. (2021) 18(01):45–50. doi: 10.1055/s-0041-1724141
20. Swamiyappan SS, Visvanathan K, Kumar SK, Naleer M, Vivek V, Ganesh K. Traumatic cranial nerve injuries—an institutional experience. Interdiscip Neurosurg. (2024) 36:101973. doi: 10.1016/j.inat.2024.101973
21. Coello AF, Canals AG, Gonzalez JM, Martín JJ. Cranial nerve injury after minor head trauma. J Neurosurg. (2010) 113(3):547–55. doi: 10.3171/2010.6.JNS091620
Keywords: cranial nerve palsy, head injury, lower cranial nerve, occipital condyle, trauma
Citation: Gupta S, Gupta R, Sheikh Z and Bele A (2025) Case Report: Head injury presenting as lower cranial nerve palsy. Front. Surg. 12:1613887. doi: 10.3389/fsurg.2025.1613887
Received: 17 April 2025; Accepted: 14 October 2025;
Published: 30 October 2025.
Edited by:
Manish Singh Sharma, Veteran Affairs Medical Center, United StatesReviewed by:
Luis Rafael Moscote-Salazar, Colombian Clinical Research Group in Neurocritical Care, ColombiaVisvanathan Krishnaswamy, Sri Ramachandra Institute of Higher Education and Research, India
Egemen Yildiz, Kutahya City Hospital, Türkiye
Copyright: © 2025 Gupta, Gupta, Sheikh and Bele. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shubham Gupta, YWRzaHViaEBnbWFpbC5jb20=
†Present Address: Shubham Gupta,Department of Neurosurgery, Sawai Man Singh Medical College and Hospital, Jaipur, Rajasthan, India
 Shubham Gupta
Shubham Gupta Rakesh Gupta
Rakesh Gupta Abhijeet Bele
Abhijeet Bele