- Department of Orthopedic, Liaocheng People’s Hospital, Liaocheng, Shandong, China
Background: Femoral shaft fractures in adolescents are commonly treated with either antegrade intramedullary nailing (AIN) or lateral plate (LP) fixation. This study compared the clinical outcomes of these two methods.
Methods: Adolescent patients with femoral shaft fractures were randomly assigned to either the AIN group (n = 62) or the LP group (n = 62). Surgical parameters, early recovery metrics, levels of inflammatory cytokines, pain mediators, and bone metabolism markers were assessed.
Results: The AIN group had significantly shorter incision lengths (6.8 vs. 8.5 cm, p < 0.001) and lower intraoperative blood loss (120 vs. 170 ml, p < 0.001) compared to the LP group. AIN patients began weight-bearing activities earlier (34 vs. 47 days, p < 0.01). Three months post-operation, the AIN group showed superior proximal femoral geometry and hip function, with a higher non-arthritic hip score (NAHS, 87 vs. 75, p < 0.001). One-week post-operation, the AIN group had lower serum levels of inflammatory cytokines and pain mediators, indicating a reduced inflammatory response and less postoperative pain.
Conclusions: AIN offers significant advantages over LP in treating adolescent femoral shaft fractures, including reduced surgical trauma, faster early recovery, lower inflammatory response, less postoperative pain, and enhanced bone healing.
Introduction
Femoral shaft fractures in adolescents, while relatively uncommon, represent a significant clinical challenge. In our department, these fractures accounted for 1.98% of all pediatric fractures (124 cases out of 6,268 total pediatric fractures). Despite their rarity, these injuries demand prompt and effective surgical intervention to ensure optimal healing and functional recovery (1, 2). These fractures often resulting from high-energy trauma such as sports injuries or vehicular accidents, present unique challenges due to the ongoing growth and development of the adolescent skeletal system. The primary goals in managing these fractures are to ensure proper healing, restore full function, and prevent any long-term complications that could affect the mobility and quality of patient life (3, 4). Given the complexity and potential impact of these fractures, selecting the most effective surgical treatment is critical for optimizing outcomes.
Treating displaced femoral shaft fractures typically requires surgical intervention. The choice of treatment method is influenced by factors such as the age, weight, fracture type, and socioeconomic status (5, 6). Two prevalent surgical techniques for treating adolescent femoral shaft fractures are antegrade intramedullary nailing (AIN) and locking plate (LP) fixation (3, 6, 7). AIN involves inserting a metal rod into the marrow canal of the femur, providing internal support that allows for early weight-bearing and mobilization (8). This procedure involves inserting a metal rod (nail) into the medullary canal of the bone from the proximal end, typically through the hip for femoral fractures or the knee for tibial fractures. The nail is then secured with screws at both ends to provide stabilization and promote healing. AIN offers several advantages, including minimal disruption to the fracture site, preservation of the periosteal blood supply, and early weight-bearing for patients (9, 10). It is particularly effective for diaphyseal fractures, where it provides strong internal support and allows for relatively quick recovery. LP fixation is another common method for treating fractures, especially in cases where the bone is highly comminuted or where there is a need for angular stability (11). This technique involves the application of a plate along the bone with screws that lock into the plate, creating a fixed-angle construct. Unlike traditional plating methods, locking plates do not rely on bone compression for stability, making them suitable for osteoporotic bones and fractures near joints. LP fixation provides robust stabilization, maintains the alignment of the fracture, and minimizes the risk of secondary displacement. It is often used in complex periarticular fractures and where intramedullary nailing is not feasible.
Inflammation and pain management post-surgery are crucial for recovery (12). Elevated levels of inflammatory cytokines and pain mediators could prolong recovery and negatively impact the life quality of patients. Techniques that minimize tissue disruption and reduce the inflammatory response are therefore highly desirable. Our study combined multiple assessment parameters to offer a holistic evaluation of these techniques. We examine surgical impact and early postoperative recovery, including incision length, intraoperative blood loss, and time to weight-bearing. The study also evaluates the inflammatory response and pain levels by measuring specific inflammatory cytokines [interleukin (IL)-6, IL-1β, IL-8] and pain mediators [Prostaglandin E2 (PGE2), Substance P]. Furthermore, we analyze bone metabolism through bone formation and resorption markers. By examining these diverse parameters, we seek to provide a nuanced understanding of the relative benefits and drawbacks of each technique. Through this study, we aim to contribute to the evolving body of knowledge in pediatric orthopedics, potentially leading to improved treatment strategies, reduced recovery times, and better long-term outcomes for adolescent patients with femoral shaft fractures.
Methods
Patients
The study was approved by Liaocheng People's Hospital. Written consent was waived since this is a retrospective study. This retrospective clinical study included 124 patients with adolescent femoral shaft fractures treated in our department. The patients were divided into two groups: 62 treated with AIN and 62 treated with locking plate fixation. The inclusion criteria were: age 11–16 years, body weight 49–59 kg, high-energy trauma as the cause of injury, unilateral femoral shaft fracture, postoperative follow-up of at least 1 year with complete clinical and imaging data from injury to bony union, and surgery performed within 7 days of injury. The exclusion criteria were: pathological fractures, open fractures, concurrent fractures in other parts of the limbs, associated vascular or nerve injuries in the lower limbs, and underlying conditions such as osteogenesis imperfecta or neuromuscular diseases. To minimize selection bias, our study utilized propensity score matching for patient selection. The matching criteria included age, body mass index (BMI), injury cause, and AO classification of fracture, with a caliper value of 0.05.
Surgical techniques
Adolescent intramedullary nailing (AIN)
Patients in the AIN group were treated using the Expert Adolescent Lateral Femoral Nail System provided by Synthes. Following general anesthesia or combined spinal-epidural anesthesia, patients were positioned supine on an orthopedic surgical table. After routine sterilization and draping, a longitudinal incision was made at the proximal end of the greater trochanter. Subcutaneous fat and fascia overlying the gluteus maximus were incised, and the gluteus medius muscle fibers were separated to expose the greater trochanter. Using a 20 mm distal to the lesser trochanter as a reference point and a 12° lateral deviation at the greater trochanter as the entry point, a guidewire was inserted. The medullary canal was progressively enlarged with a flexible reamer, and the intramedullary nail was inserted. Under C-arm fluoroscopic guidance, the fracture was reduced satisfactorily, and locking screws and an end cap were inserted using a targeting arm. The surgical field was irrigated, and the wound was closed in layers. Postoperative management included routine anti-infection treatment and early quadriceps muscle contraction training without weight-bearing, progressing to gradual weight-bearing at 6–8 weeks.
Locking plate fixation
In the locking plate group, a 6–8 cm longitudinal incision centered over the fracture site was made. The fascia lata was incised, exposing the vastus lateralis muscle. The lateral intermuscular septum was identified, and dissection continued along the plane between the vastus lateralis and the septum to expose the femoral shaft. After clearing hematoma and soft tissue from the fracture site, reduction was achieved with the aid of a reduction device. A locking plate was then implanted, ensuring the distal end was at least 20 mm from the distal femoral epiphysis. Screws were inserted through small incisions at both ends of the plate. Satisfactory reduction was confirmed under C-arm fluoroscopy, the surgical field was irrigated, and the wound was closed in layers. Postoperative care included dressing changes every 2 days. From the second postoperative day, patients began non-weight-bearing functional exercises, including early hip and knee joint movements and later non-weight-bearing walking exercises.
Measurement and analysis
Proximal femoral geometry
Bilateral proximal femoral geometric parameters were measured on anteroposterior radiographs at the final follow-up using imaging software. Two experienced residents performed the measurements, focusing on the maximum diameters of the femoral neck and femoral head.
Non-arthritic hip score (NAHS)
Hip function was assessed using the Non-Arthritic Hip Score (NAHS), which is suitable for young patients without hip arthritis. A score of 100 indicates normal hip function, with lower scores indicating worse hip function.
Collection of venous blood
Fasting venous blood samples were collected from the pediatric patients before surgery and 1 week postoperatively. Serum was separated and stored at −80°C for further analysis.
Inflammatory markers
Postoperative inflammation and pain were assessed by analyzing serum levels of inflammatory cytokines and pain mediators 1 week postoperatively. The extent of the inflammatory response was correlated with the degree of surgical trauma. The concentrations of inflammatory cytokines and pain mediators in serum were measured using enzyme-linked immunosorbent assay (ELISA) kits according to the manufacturers' instructions. The following kits were used: Human IL-6 ELISA Kit (Cat# EH0201), Human IL-1β ELISA Kit (Cat# EH0185), Human IL-8 ELISA Kit (Cat# EH0205), Human PGE2 ELISA Kit (Cat# EH4233)—all purchased from Wuhan Fine Biotechnology Co., Ltd (Wuhan, China). Pain mediator P was detected using an ELISA kit (Cat# E-EL-0067) purchased from Elabscience Biotechnology Co., Ltd (Wuhan, China).
Bone metabolism indicators
Bone formation and resorption were evaluated 1 month postoperatively by measuring serum levels of bone alkaline phosphatase (BALP), bone gamma-carboxyglutamate protein (BGP), and beta-crosslaps (β-CTX) using ELISA kits according to the manufacturers' instructions. The following kits were used: Human BALP ELISA Kit (Cat# EH2691), Human OC/BGP ELISA Kit (Cat# EH3468), Human β-CTx ELISA Kit (Cat# EH3989). All kits were purchased from Wuhan Fine Biotech Co., Ltd. These indicators were analyzed to understand the balance of bone metabolism and its impact on fracture healing.
Both groups underwent early functional exercise, and all patients completed follow-up ranging from 19 to 48 months. At the final follow-up, all fractures had achieved bony union without significant limitations in hip or knee joint mobility. Radiographic evaluations revealed no complications such as femoral head necrosis or hip valgus deformity.
Statistical analysis
Data were expressed as n (percentage, %) or mean ± standard deviation (SD). The normality of the data before analysis was examined using Anderson–Darling test. The comparisons of data between the two groups were done by unpaired t test with Welch's correction, Chi-square test or Fisher's exact test. The significant statistical difference was determined when p values were less than 0.05.
Results
The demographic and clinical characteristics of the participants
The demographic and clinical characteristics of adolescents with femoral shaft fractures treated with either AIN or LP were summarized in Table 1. Propensity score matching was employed to minimize selection bias, using age, BMI, injury cause, and AO classification of fracture as matching criteria, with a caliper value of 0.05. The process of the subject selection was shown in Supplementary Figure S1. The comparison revealed no significant differences between the two groups in terms of age (AIN: 13.75 ± 1.24 years, LP: 13.69 ± 1.38 years, p = 0.582), BMI (AIN: 23.35 ± 0.49 kg/m2, LP: 23.16 ± 0.57 kg/m2, p = 0.184), gender distribution (boys: AIN 61.3%, LP 53.2%; girls: AIN 38.7%, LP 46.8%; p = 0.468), injury cause (accident: AIN 32.3%, LP 40.3%; fall injury: AIN 46.8%, LP 45.2%; sports injury: AIN 20.9%, LP 14.5%; p = 0.522), and AO classification of the fracture (A: AIN 61.3%, LP 58.2%; B: AIN 24.2%, LP 20.9%; C: AIN 14.5%, LP 20.9%; p = 0.630).
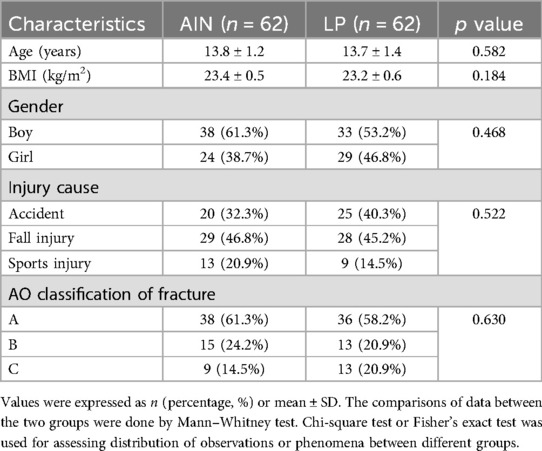
Table 1. Demographic and clinical characteristics of femoral shaft fractures adolescent received the treatment of adolescent intramedullary nail (AIN) or locking plate (LP).
Surgical impact and early postoperative recovery
Figure 1 illustrated the progression of fracture healing and the stability of fixation methods in adolescents treated with either an AIN or a LP over time. The typical x-ray images of a 13-year-old boy with a left femoral shaft fracture treated with AIN are shown at different stages: pre-operation, post-operation, 1-month post-operation, 3 months post-operation, and at the last follow-up (Figure 1A). The corresponding x-ray images for a 14-year-old boy with a left femoral shaft fracture treated with LP are also shown at these stages (Figure 1B). The images in both panels highlight the sequential healing process and the effectiveness of the respective treatment methods in maintaining fracture alignment and promoting bone healing.
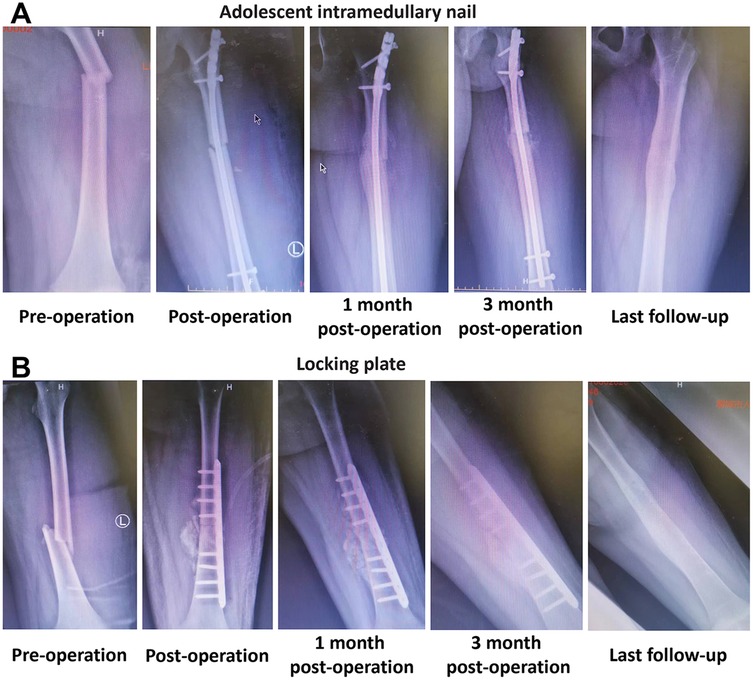
Figure 1. Typical cases of femoral shaft fractures adolescent received the treatment of adolescent intramedullary nail (AIN) or locking plate (LP). (A) X-ray images of a 13 years old boy with left femoral shaft fracture received the treatment of AIN at different times. (B) X-ray images of a 14 years old boy with left femoral shaft fracture received the treatment of LP at different times.
The comparisons between the AIN and LP groups revealed significant differences in several surgical and early postoperative parameters (Figure 2). The incision length was significantly shorter in the AIN group (p < 0.001), with a mean incision length of 6.8 cm compared to 8.5 cm in the LP group (Figure 2A). Intraoperative blood loss was also notably lower in the AIN group, averaging 120 ml compared to 170 ml in the LP group (p < 0.001, Figure 2B). Additionally, the time to walking with load post-operation was significantly shorter for the AIN group, with patients beginning weight-bearing activities at an average of 34 days post-surgery compared to 47 days in the LP group (p < 0.01, Figure 2C). These findings indicate that the AIN procedure is less invasive and facilitates earlier mobilization compared to the LP method.
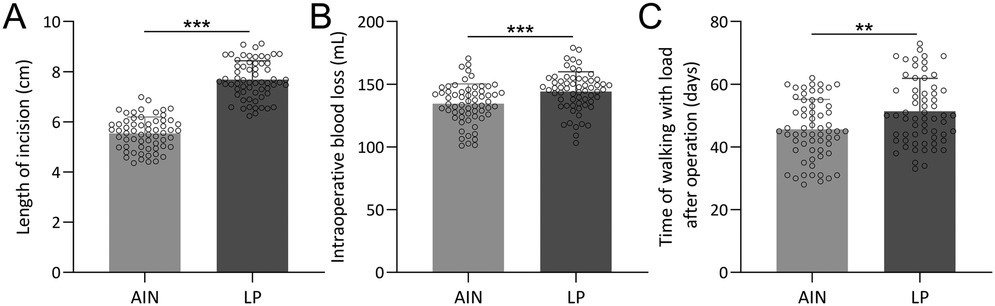
Figure 2. Comparisons of length of incision (A), intraoperative blood loss (B) and time of walking with load after operation (C) between femoral shaft fractures adolescent received the treatment of adolescent intramedullary nail (AIN) or locking plate (LP). n = 62 for each group. Data were shown with mean ± SD. **p < 0.01, ***p < 0.001 from Unpaired t test with Welch's correction.
Proximal femoral geometry and hip function
At 3 months post-operation, significant differences were observed in the widest diameter of the femoral head and the NAHS between the two groups (Figure 3). The AIN group exhibited a larger widest diameter of the femoral head and neck (p < 0.05, Figures 3A,B) and higher NAHS (p < 0.001, Figure 3C), suggesting better early postoperative hip function and geometry. Specifically, the mean NAHS was 87 in the AIN group vs. 75 in the LP group. However, by the last follow-up, these differences were no longer significant, with both groups showing comparable outcomes in the widest diameter of the femoral neck and head, as well as in the NAHS (Figures 3D–F). This convergence indicates that while both treatment methods ultimately lead to satisfactory long-term recovery, the AIN group achieves faster initial improvements in hip function and femoral geometry.
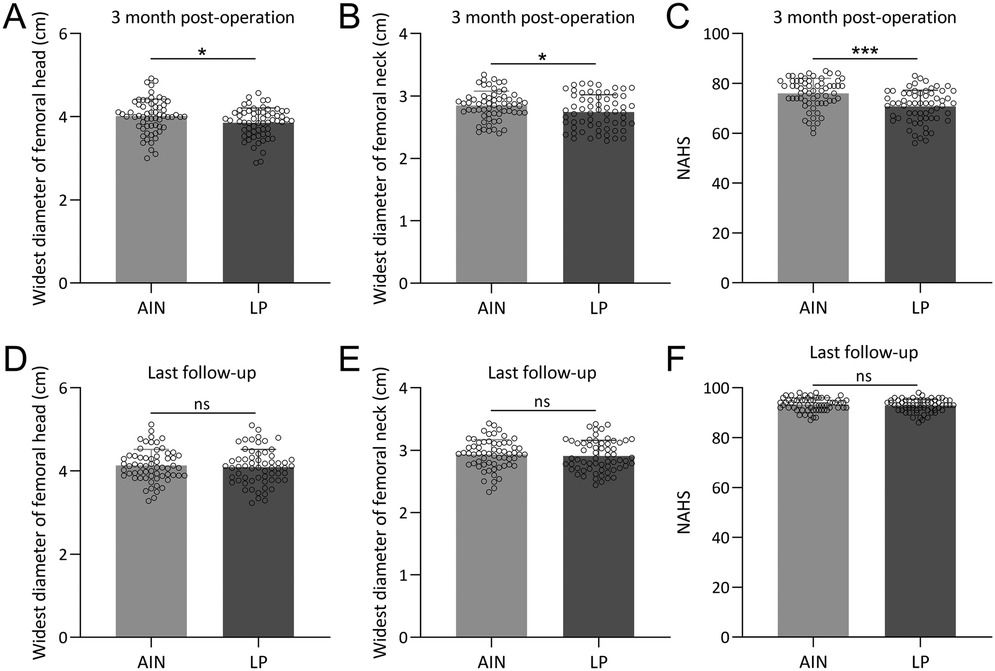
Figure 3. Comparisons of widest diameter of femoral head (A), widest diameter of femoral head (B), NAHS (C) between the two groups at the time of 3 months post-operation and also at the time of last follow-up (D–F). n = 62 for each group. Data were shown with mean ± SD. *p < 0.05, **p < 0.01, ***p < 0.001 from Unpaired t test with Welch's correction.
Intramedullary nailing reduces inflammation and pain in adolescent femoral fractures
We next compared the levels of serum inflammatory cytokines and pain mediators between the AIN and LP groups 1-week post-operation. To establish baseline comparability, the serum levels of these inflammatory markers and pain mediators pre-operation were assessed and the data confirm that there were no significant differences between the groups before surgery (Supplementary Figures S2A–E).
However, there were significant differences in the levels of inflammatory markers and pain mediators between the two groups. Specifically, the LP group had higher serum concentrations of IL-6 (Figure 4A), IL-1β (Figure 4B), IL-8 (Figure 4C), PGE2 (Figure 4D), and pain mediator P (Figure 4E) compared to the AIN group. These results indicate that the AIN method is associated with a lower inflammatory response and reduced pain levels 1-week after surgery, suggesting it is less traumatic and more effective in minimizing postoperative pain.
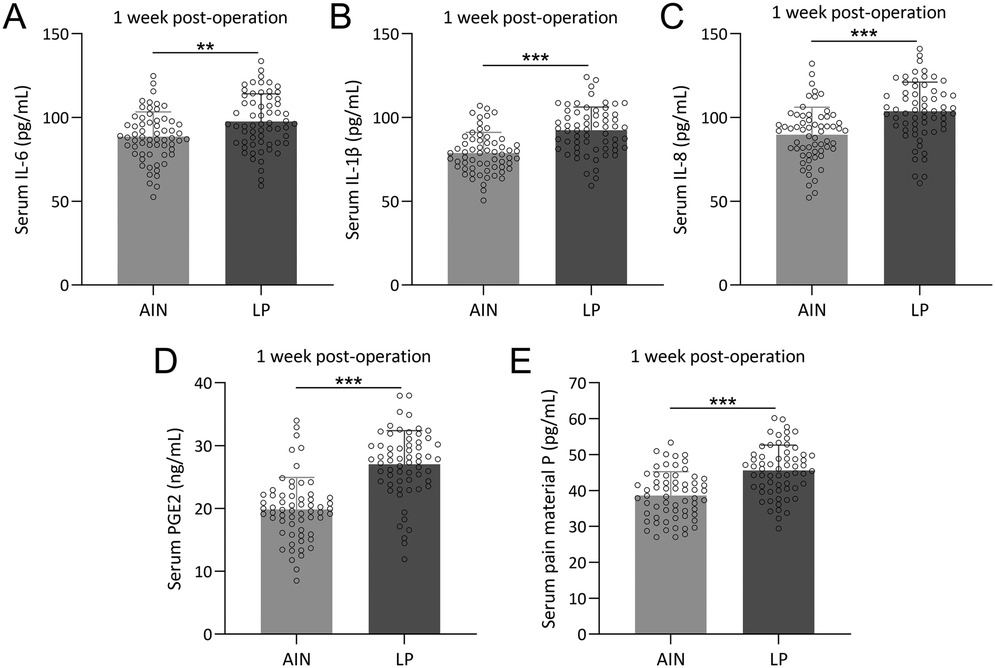
Figure 4. Comparisons of serum IL-6 (A), IL-1β (B), IL-8 (C), PGE2 (D) and pain material P (E) between the two groups at the time of 1 week post-operation. n = 62 for each group. Data were shown with mean ± SD. **p < 0.01, ***p < 0.001 from Unpaired t test with Welch's correction.
Enhanced bone formation and reduced resorption in AIN
To compare the levels of bone formation and resorption markers between the AIN and LP groups 1-month post-operation, we assessed the bone metabolism indicators between the two groups. There were no significant differences in serum levels of BALP, BGP, and β-CTX between the groups before surgery (Supplementary Figures S3A–C). Interestingly, 1-month after operation, the AIN group showed higher levels of bone formation markers BALP (Figure 5A) and BGP (Figure 5B), and lower levels of the bone resorption marker β-CTX (Figure 5C) compared to the LP group. These findings suggest that the AIN treatment promotes better bone formation and less bone resorption 1 month after surgery, which correlates with faster fracture healing observed in the AIN group.
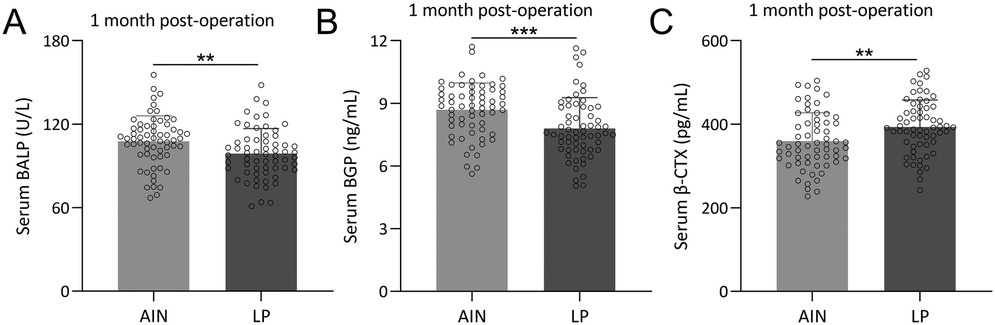
Figure 5. Comparisons of serum BALP (A), BGP (B) and β-CTX (C) between the two groups at the time of 1-month post-operation. n = 62 for each group. Data were shown with mean ± SD. **p < 0.01, ***p < 0.001 from Unpaired t test with Welch's correction.
Discussion
This study compared the clinical outcomes of AIN and LP fixation in the treatment of femoral shaft fractures of adolescents. Our results highlighted significant differences in surgical impact, early postoperative recovery, inflammatory response, pain levels, and bone metabolism markers, providing valuable insights into the relative efficacy and safety of these treatment modalities.
Surgical impact and early postoperative recovery
Our findings indicated that AIN was less invasive than LP, as evidenced by significantly shorter incision lengths and lower intraoperative blood loss. Specifically, the mean incision length in the AIN group was 6.8 cm, compared to 8.5 cm in the LP group, and the average blood loss was 120 vs. 170 ml, respectively. These differences suggest that the AIN procedure minimizes tissue damage and bleeding, leading to a more favorable surgical profile. Additionally, patients in the AIN group began weight-bearing activities on average 34 days post-surgery, significantly earlier than the 47 days observed in the LP group. Early mobilization is crucial for reducing the risk of postoperative complications such as deep vein thrombosis and muscle atrophy, and it contributes to overall better recovery outcomes (13–15). Similar trends were reported that minimally invasive approaches in femoral fracture repair were associated with reduced soft tissue disruption and faster rehabilitation (16).
Proximal femoral geometry and hip function
The AIN group exhibited superior early postoperative hip function and proximal femoral geometry compared to the LP group at 3 months post-operation. The widest diameters of the femoral head and neck were significantly larger in the AIN group, and the NAHS was higher, with a mean score of 87 compared to 75 in the LP group. These metrics suggest that AIN better preserves the anatomical integrity of the femur and supports hip function during the initial recovery phase. However, by the last follow-up, the differences in proximal femoral geometry and NAHS between the two groups were no longer significant, indicating that both treatment methods achieve similar long-term recovery outcomes. This convergence implies that while AIN offers faster initial improvements, both methods are effective in restoring function and anatomy over time.
A previous study that retrospectively analyzed the functional outcomes of LP vs. AIN for extra-articular distal femoral fractures noted a faster, albeit not statistically significant, union rate for AIN compared to LP (17). Our results similarly indicated that AIN generally leads to quicker fracture healing, supporting its advantage in facilitating faster recovery. Additionally, a meta-analysis of 20 studies involving 1,384 patients with proximal humeral fractures found that intramedullary nails were superior to LP in terms of shorter incision length, less peri-operative bleeding, reduced operation time, and faster fracture healing (18). These findings are consistent with our observations. Another study reported that AIN resulted in significantly lower shoulder pain and higher median Constant and ASES scores compared to LP, with fewer complications and revision surgeries (19). Collectively, these studies reinforce that while both AIN and LP are effective in achieving long-term clinical outcomes, AIN offers distinct advantages in the early postoperative period and in reducing complications.
Furthermore, similar patterns have been observed in femoral neck fracture treatments, where minimally invasive intramedullary fixation techniques were associated with improved short-term hip function and preservation of proximal femoral alignment (20). Moreover, biomechanical analyses have demonstrated that intramedullary implants distribute load more efficiently along the femoral axis compared to lateral plates, which may explain the superior early outcomes observed in our study. For instance, a biomechanical comparison using synthetic bone models found that proximal femoral intramedullary nails sustained approximately 1.78-fold greater axial load before failure than locking proximal anatomic femoral plates, highlighting their superior load-sharing capacity under axial compression (21). Additionally, finite element analysis studies have shown that intramedullary nails bear higher von Mises stresses and transmit loads centrally through the bone's mechanical axis, reducing stress concentration in the implant—a biomechanical advantage that correlates with improved early fracture stabilization (22).
Intramedullary nailing reduces inflammation and pain
Intramedullary nailing can trigger a “second hit” effect on a patient physiology, which includes several inflammatory and physiological responses (23–25). This second hit is caused by increased pressures within the intramedullary canal, intravasation of fat particles, activation of coagulation, marrow embolization to the lungs or brain, and overheating of the endosteum. Femoral reaming is associated with increased blood loss from the fractured extremity.
Various biomarkers have been studied to understand the cumulative effects of these factors during AIN (26). Key biomarkers such as IL-6, IL-8, IL-10, and TNF-α have been identified. IL-6, in particular, is a significant marker of the early post-traumatic immune response and is elevated in both reamed and unreamed nailing. Studies have shown that the type of surgical procedure, initial trauma severity, specific injury combinations, and timing of surgical intervention are critical factors influencing the inflammatory response (27). The period between 48 h and the 5th day post-trauma is identified as suboptimal for major surgeries due to the heightened risk of systemic inflammatory response syndromeand complications (26, 28). Effective resuscitation and careful timing of surgical interventions are crucial to mitigating the second hit's impact. Here, we found that 1-week after operation, the LP group had significantly higher serum levels of inflammatory cytokines IL-6, IL-1β, and IL-8, as well as pain mediators PGE2 and pain mediator P, compared to the AIN group. These elevated levels indicate a higher inflammatory response and greater pain in the LP group, suggesting that the AIN method is less traumatic and more effective in minimizing postoperative pain. Reduced inflammation and pain are associated with faster recovery and improved patient comfort, underscoring the advantages of AIN in postoperative management (29).
Enhanced bone formation and reduced resorption in AIN
BALP and BGP were used as bone formation markers, and β-CTX was employed as a bone resorption marker. BALP promotes bone mineralization (30), while BGP regulates bone matrix crystallization and reflects recent osteoblast activity (31, 32). β-CTX, released during increased osteoclast activity, is the gold standard for assessing bone resorption (33). Bone metabolism markers provide insight into the biological processes underlying fracture healing. One-month post-operation, the AIN group demonstrated higher levels of bone formation markers BALP and BGP and lower levels of the bone resorption marker β-CTX compared to the LP group. These findings suggest that AIN promotes better bone formation and less bone resorption, correlating with faster and more robust fracture healing. Enhanced bone formation is crucial for the stabilization and consolidation of fractures, while reduced bone resorption minimizes the risk of delayed union or nonunion. The absence of significant differences in these markers pre-operation further supports the postoperative benefits observed with AIN.
Our study comparing AIN and LP fixation for adolescent femoral shaft fractures revealed significant advantages of AIN in terms of surgical impact, early recovery, and bone metabolism. These findings align with broader research in pediatric orthopedics. Chin See et al. demonstrated the efficacy of rigid intramedullary nailing in children with metabolic bone diseases, supporting its application beyond typical cases (34). Another study explored bioabsorbable intramedullary nails for pediatric forearm fractures, highlighting potential benefits in eliminating secondary surgeries but also noting technique-dependent complications (35). For overweight pediatric patients with narrow medullary canals, Tang et al. proposed combining elastic stable intramedullary nails with temporary external fixators as an alternative to locking compression plates, showing improved outcomes in operation time, blood loss, and union rates (36). Collectively, these studies, including our own, underscore the importance of tailoring fixation methods to patient-specific factors such as age, weight, bone quality, and fracture characteristics. While AIN demonstrates clear advantages in our adolescent cohort, the evolving landscape of pediatric orthopedic fixation techniques suggests a nuanced approach is necessary. Future research should focus on refining selection criteria for various fixation methods, optimizing techniques to minimize complications, and conducting long-term follow-up studies to ensure sustained positive outcomes across diverse patient populations.
Conclusion
In conclusion, AIN offers significant advantages over LP in the treatment of adolescent femoral shaft fractures, including reduced surgical trauma, faster early recovery, lower inflammatory response, less postoperative pain, and enhanced bone healing. These benefits make AIN a more favorable option for managing these types of fractures, particularly in the early postoperative period. While both treatment methods ultimately achieve satisfactory long-term outcomes, the faster initial recovery associated with AIN provides a compelling case for its use in clinical practice.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Department of Orthopedic, Liaocheng People's Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
JH: Validation, Writing – review & editing, Data curation, Writing – original draft. YB: Writing – original draft, Validation, Data curation, Resources, Supervision, Writing – review & editing, Funding acquisition.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2025.1614146/full#supplementary-material
Abbreviations
AIN, antegrade intramedullary nailing; BALP, bone alkaline phosphatase; BGP, bone gamma-carboxyglutamate protein; BMI, body mass index; IL, interleukin; LP, lateral plate; NAHS, non-arthritic hip score; PEG2, prostaglandin E2; SD, standard deviation; β-CTX, beta-crosslaps.
References
1. Madhuri V, Dutt V, Gahukamble AD, Tharyan P. Interventions for treating femoral shaft fractures in children and adolescents. Cochrane Database Syst Rev. (2014) 2014(7):CD009076. doi: 10.1002/14651858.CD009076.pub2
2. John R, Sharma S, Raj GN, Singh J, Varsha C, Arjun RHH, et al. Current concepts in paediatric femoral shaft fractures. Open Orthop J. (2017) 11:353–68. doi: 10.2174/1874325001711010353
3. Gupte D, Axelrod D, Worthy T, Woolnough T, Selznick A, Johal H. Management of femoral shaft fractures: the significance of traction or operative position. Cureus. (2023) 15(1):e33776. doi: 10.7759/cureus.33776
4. Denisiuk M, Afsari A. Femoral shaft fractures. In: StatPearls. Treasure Island (FL): StatPearls Publishing (2024).
5. Fischer H, Maleitzke T, Eder C, Ahmad S, Stockle U, Braun KF. Management of proximal femur fractures in the elderly: current concepts and treatment options. Eur J Med Res. (2021) 26(1):86. doi: 10.1186/s40001-021-00556-0
6. Liau GZQ, Lin HY, Wang Y, Nistala KRY, Cheong CK, Hui JHP. Pediatric femoral shaft fracture: an age-based treatment algorithm. Indian J Orthop. (2021) 55(1):55–67. doi: 10.1007/s43465-020-00281-6
7. Gaid M, Jeer P. Cost analysis of managing paediatric femoral shaft fractures: flexible intramedullary nailing versus non-operative management. Acta Orthop Belg. (2006) 72(2):170–5.16768260
8. Ricci WM, Gallagher B, Haidukewych GJ. Intramedullary nailing of femoral shaft fractures: current concepts. J Am Acad Orthop Surg. (2009) 17(5):296–305. doi: 10.5435/00124635-200905000-00004
9. Kumar D, Ghosh A, Jindal K, Berwal P, Sharma S, Dhillon M. Antegrade vs retrograde intramedullary nailing in humerus shaft fractures: a systematic review and meta-analysis. J Orthop. (2022) 34:391–7. doi: 10.1016/j.jor.2022.10.003
10. Shin WC, Jang JH, Jung SJ, Moon NH. Advantages and limitations of intramedullary nailing for the surgical treatment of ipsilateral intertrochanteric and femoral shaft fractures: a retrospective comparative study based on propensity score matching. Eur J Trauma Emerg Surg. (2022) 48(3):1779–86. doi: 10.1007/s00068-020-01469-z
11. Foruria AM. Plate fixation of proximal humerus fractures: how to get it right and future directions for improvement. Curr Rev Musculoskelet Med. (2023) 16(10):457–69. doi: 10.1007/s12178-023-09853-z
12. Elsevier H, Cannada LK. Management of pain associated with fractures. Curr Osteoporos Rep. (2020) 18(3):130–7. doi: 10.1007/s11914-020-00578-3
13. Tazreean R, Nelson G, Twomey R. Early mobilization in enhanced recovery after surgery pathways: current evidence and recent advancements. J Comp Eff Res. (2021) 11(2):121–9. doi: 10.2217/cer-2021-0258
14. Choi YS, Kim TW, Chang MJ, Kang SB, Chang CB. Enhanced recovery after surgery for major orthopedic surgery: a narrative review. Knee Surg Relat Res. (2022) 34(1):8. doi: 10.1186/s43019-022-00137-3
15. Mithany RH, Daniel N, Shahid MH, Aslam S, Abdelmaseeh M, Gerges F, et al. Revolutionizing surgical care: the power of enhanced recovery after surgery (ERAS). Cureus. (2023) 15(11):e48795. doi: 10.7759/cureus.48795
16. Nourian A, Dhaliwal S, Vangala S, Vezeridis PS. Midshaft fractures of the clavicle: a meta-analysis comparing surgical fixation using anteroinferior plating versus superior plating. J Orthop Trauma. (2017) 31(9):461–7. doi: 10.1097/BOT.0000000000000936
17. Ocalan E, Ustun CC, Aktuglu K. Locking plate fixation versus antegrade intramedullary nailing for the treatment of extra-articular distal femoral fractures. Injury. (2019) 50(Suppl 3):55–62. doi: 10.1016/j.injury.2019.07.008
18. Li M, Wang Y, Zhang Y, Yang M, Zhang P, Jiang B. Intramedullary nail versus locking plate for treatment of proximal humeral fractures: a meta-analysis based on 1384 individuals. J Int Med Res. (2018) 46(11):4363–76. doi: 10.1177/0300060518781666
19. Boyer P, Couffignal C, Bahman M, Mylle G, Rousseau MA, Dukan R. Displaced three and four part proximal humeral fractures: prospective controlled randomized open-label two-arm study comparing intramedullary nailing and locking plate. Int Orthop. (2021) 45(11):2917–26. doi: 10.1007/s00264-021-05217-9
20. Lalueza-Andreu P, Martinez-Garcia A, Checa-Betegon P, Garcia-Coiradas J, Valle-Cruz JA, Marco-Martinez F. Surgical treatment of non-displaced subcapital hip fracture: femoral neck system vs. cannulated screws. Comparative study. Rev Esp Cir Ortop Traumatol. (2024). doi: 10.1016/j.recot.2024.09.008
21. Ozkan K, Turkmen I, Sahin A, Yildiz Y, Erturk S, Soylemez MS. A biomechanical comparison of proximal femoral nails and locking proximal anatomic femoral plates in femoral fracture fixation: a study on synthetic bones. Indian J Orthop. (2015) 49(3):347–51. doi: 10.4103/0019-5413.156220
22. Charles-Harris M, Lacroix D, Proubasta I, Planell JA. Intramedullary nails vs osteosynthesis plates for femoral fracture stabilization: a finite element analysis. J Appl Biomater Biomech. (2005) 3(3):157–67.20799221
23. Giannoudis P, Snowden S, Matthews S, Smye S, Smith R. Friction burns within the tibia during reaming: are they affected by the use of a tourniquet? J Bone Joint Surg Br. (2002) 84(4):492–6. doi: 10.1302/0301-620X.84B4.0840492
24. Lasanianos NG, Kanakaris NK, Dimitriou R, Pape HC, Giannoudis PV. Second hit phenomenon: existing evidence of clinical implications. Injury. (2011) 42(7):617–29. doi: 10.1016/j.injury.2011.02.011
25. Van Griensven M. Cytokines as biomarkers in polytraumatized patients. Unfallchirurg. (2014) 117:699–702. doi: 10.1007/s00113-013-2543-6
26. Kanakaris NK, Anthony C, Papasotiriou A, Giannoudis PV. Inflammatory response after nailing. Injury. (2017) 48(Suppl 1):S10–4. doi: 10.1016/j.injury.2017.04.017
27. Arias JI, Aller MA, Arias J. Surgical inflammation: a pathophysiological rainbow. J Transl Med. (2009) 7:19. doi: 10.1186/1479-5876-7-19
28. Pape HC, van Griensven M, Rice J, Gansslen A, Hildebrand F, Zech S, et al. Major secondary surgery in blunt trauma patients and perioperative cytokine liberation: determination of the clinical relevance of biochemical markers. J Trauma. (2001) 50(6):989–1000. doi: 10.1097/00005373-200106000-00004
29. ElHawary H, Baradaran A, Abi-Rafeh J, Vorstenbosch J, Xu L, Efanov JI. Bone healing and inflammation: principles of fracture and repair. Semin Plast Surg. (2021) 35(3):198–203. doi: 10.1055/s-0041-1732334
30. Halling Linder C, Ek-Rylander B, Krumpel M, Norgård M, Narisawa S, Millán JL, et al. Bone alkaline phosphatase and tartrate-resistant acid phosphatase: potential co-regulators of bone mineralization. Calcif Tissue Int. (2017) 101(1):92–101. doi: 10.1007/s00223-017-0259-2
31. Catherwood BD, Marcus R, Madvig P, Cheung AK. Determinants of bone gamma-carboxyglutamic acid-containing protein in plasma of healthy aging subjects. Bone. (1985) 6(1):9–13. doi: 10.1016/8756-3282(85)90400-4
32. Zoch ML, Clemens TL, Riddle RC. New insights into the biology of osteocalcin. Bone. (2016) 82:42–9. doi: 10.1016/j.bone.2015.05.046
33. Chubb SAP, Vasikaran SD. Measurement and clinical utility of betaCTX in serum and plasma. Adv Clin Chem. (2017) 81:97–134. doi: 10.1016/bs.acc.2017.01.003
34. Chin See CK, Al-Naser S, Nicolaou N, Giles SN, Fernandes JA. Rigid intramedullary nailing of lower limb segments in children and adolescents with metabolic bone disease. J Pediatr Orthop B. (2025) 34(3):264–70. doi: 10.1097/BPB.0000000000001215
35. Jozsa G, Kassai T, Varga M, David AL, Toth Z, Molnar T, et al. Considerations and challenges of resorbable intramedullary nailing in pediatric forearm fractures. Children. (2025) 12(5):606. doi: 10.3390/children12050606
36. Tang X, Liang J, Zhang B, Rai S, Hu Q, Zou Y, et al. An alternative choice for overweight pediatric patient with femoral shaft fracture when rigid nail is contraindicated due to narrow intramedullary canal: elastic stable intramedullary nail plus temporary external fixator. J Orthop Sci. (2025). doi: 10.1016/j.jos.2025.01.002
Keywords: adolescent femoral shaft fractures, antegrade intramedullary nailing, bone healing, inflammation, lateral plate fixation
Citation: Huang J and Bian Y (2025) Comparative analysis of adolescent intramedullary nailing and locking plate fixation for femoral shaft fractures. Front. Surg. 12:1614146. doi: 10.3389/fsurg.2025.1614146
Received: 28 April 2025; Accepted: 26 June 2025;
Published: 17 July 2025.
Edited by:
Georgia Damoraki, National and Kapodistrian University of Athens, GreeceReviewed by:
Marcos Edgar Herkenhoff, Santa Catarina State University, BrazilGawel Solowski, Bingöl University, Türkiye
Spyros Foutadakis, Biomedical Research Foundation of the Academy of Athens (BRFAA), Greece
Copyright: © 2025 Huang and Bian. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Yiqun Bian, ZXRoYW5kckAxNjMuY29t
 Jian Huang
Jian Huang Yiqun Bian
Yiqun Bian