- 1Hebei North University, Zhangjiakou, Hebei, China
- 2Department of Orthopedics, Hebei General Hospital, Shijiazhuang, Hebei, China
Oblique lumbar interbody fusion (OLIF) is a minimally invasive technique for the treatment of degenerative diseases of the lumbar spine, and the left operative window is always used to avoid the inferior vena cava (IVC). However, in cases with anatomical variations—particularly vascular anomalies, which most significantly impact surgical approaches—the right retroperitoneal approach may serve as a preferable alternative. This case report describes a 59-year-old man with lumbar instability and a rare left-sided IVC who underwent OLIF via a right approach. Preoperative imaging of this patient showed an isolated left IVC. The procedure was performed through a right-sided surgical corridor bounded medially by the abdominal aorta(AA) and laterally by the right psoas major muscle. The approach was supplemented with lateral screw-rod instrumentation to maintain stability. The patient's neurological function improved significantly after surgery, and the surgical approach proved to be feasible while maintaining biomechanical stability while avoiding vascular risk. This case highlights the importance of vascular evaluation before OLIF. Especially for the rare left-sided IVC, OLIF via right approach can effectively improve safety.
Introduction
The choice of surgical approach for each spinal fusion technique is governed by unique anatomical considerations. In the lumbar region, the abdominal aorta (AA) and inferior vena cava (IVC) run anterolaterally along the vertebral column, positioned left-anterior and right-anterior to the vertebral bodies, respectively. The bilateral psoas muscles originate from the lateral aspects of the lumbar vertebrae and their transverse processes. A natural anatomical corridor exists between the psoas muscle and the AA, which the oblique lumbar interbody fusion (OLIF) technique utilizes, accessing the target intervertebral disc through a left abdominal incision while navigating this avascular plane. OLIF represents a minimally invasive fusion technique that utilizes an oblique lateral approach. Compared to posterior approaches, this technique preserves the lamina, paraspinal muscles, and facet joints, consequently reducing approach-related complications (1). These advantages have established OLIF as a preferred surgical option for degenerative lumbar pathologies. Previous studies have demonstrated significant postoperative improvements in thecal sac cross-sectional area, foraminal dimensions, and neurological function following OLIF procedures (2).
However, the retroperitoneal surgical channel passes by major blood vessels, which carries a potential risk of vascular-related complications that can result in catastrophic iatrogenic injury. And the incidence of vascular-related complications was reported as about 0.37% (3). Therefore, it is necessary to select an appropriate operative window to effectively prevent the occurrence of vascular-related complications (4, 5). The IVC is more susceptible to intraoperative injury due to its thin wall and low elasticity. The IVC originates at the L4-L5 vertebral level through the confluence of the left and right common iliac veins (CIV), located anterolateral to the right side of the spinal column. From this junction, it ascends cephalad along the right anterolateral aspect of the vertebral bodies, maintaining a consistent parallel course with the AA throughout its thoracic trajectory. Due to its thin-walled structure and low elasticity, the IVC demonstrates particular vulnerability to intraoperative injury. Therefore, the conventional left-sided OLIF approach exploits the natural retroperitoneal plane between the abdominal aorta (medially) and psoas major (laterally). This strategic selection reduces the risk of injuring the thin-walled IVC. Notably, anatomical studies have identified left-sided IVC variants in 0.2%−0.5% of asymptomatic individuals (6, 7). For these patients, a right abdominal approach offers superior anatomical compatibility (8).
This case report describes a successful OLIF performed via a right retroperitoneal approach in a patient with degenerative lumbar disease and left-sided IVC anomaly. It should be emphasized that the left and right retroperitoneal approaches are not anatomical mirror images. Significant variations exist in the lumbar venous plexus distribution, sympathetic nerve relationships, and relative spatial positioning between vascular structures and the spine. Despite the anatomical differences compared to the standard left-sided approach, the procedure achieved favorable clinical outcomes while effectively preventing vascular injury. Key to this case were: (1) detailed preoperative vascular evaluation and (2) strategic utilization of the right surgical window, which collectively enabled safe OLIF execution despite the vascular anomaly.
Case presentation
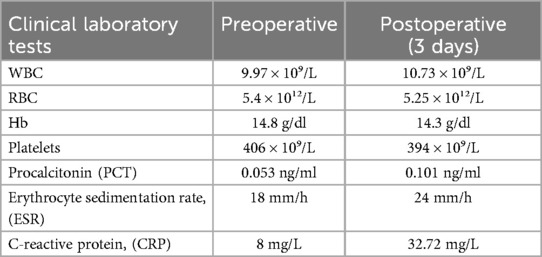
A 59-year-old male patient presented with progressively worsening low back pain and bilateral lower limb pain and numbness despite one year of unsuccessful conservative therapy and pain management. The condition worsened over the next few months, and he developed neurological claudication (Figure 1). The visual analog scale (VAS) score for low back pain was 7 points, and the VAS score for lower extremity pain was 5 points, with an Oswestry Disability Index (ODI) of 58.
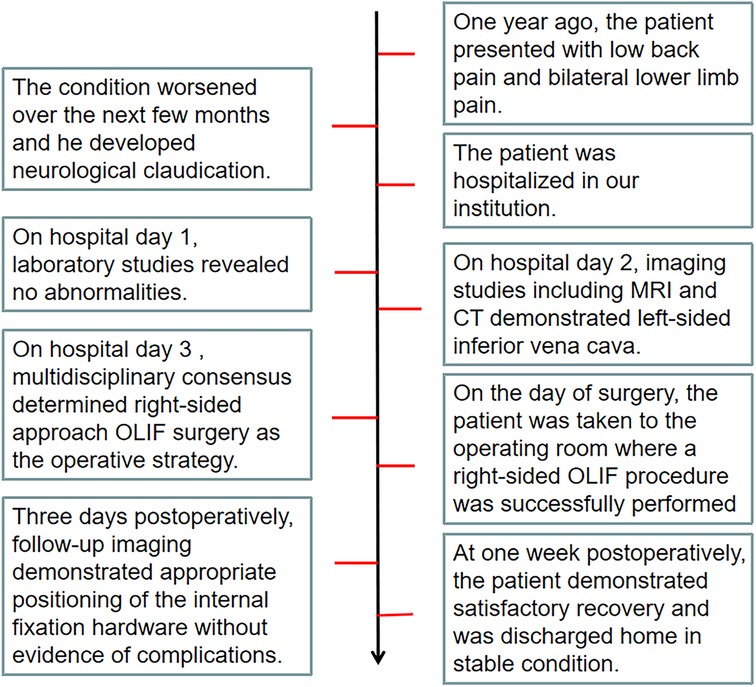
Figure 1. The diagram illustrates the entire process of the patient from the onset of the disease, through diagnosis and treatment, to full recovery.
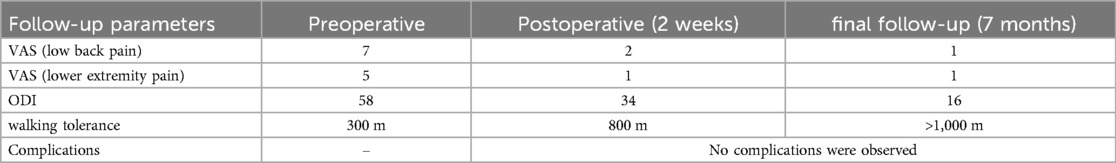
On physical examination, lumbar spine flexion and extension were limited, pain was caused by tapping and light pressure, the foraminal compression test was positive, and the bilateral straight leg elevation test was positive by 50°. The complete blood count (CBC) test showed a WBC count of 9.97 × 10⁹/L, an RBC count of 5.4 × 10¹²/L, hemoglobin of 14.8 g/dl, and a platelet count of 406 × 10⁹/L. Hepatorenal function tests indicated a total protein of 68.9 g/L, albumin of 32.8 g/L, total bilirubin of 7.3 μmol/L, AST of 11.1 U/L, ALT of 12.01 U/L, urea of 6.3 mmol/L, serum creatinine (Cr) of 67.0 μmol/L, and a GFR of 99.98 ml/min. Bone mineral density and metabolism were evaluated, revealing a 25-hydroxyvitamin D level of 11.24 ng/ml. Bone mineral density was assessed using dual-energy x-ray absorptiometry (DXA). The lowest value of the spine was 0.846 g/cm². The lowest value of the ulnar radius was 0.650 g/cm². The lowest value of the hip joint was 0.546 g/cm². It belongs to osteoporosis. Urine analysis and coagulation five showed no significant abnormalities.
Magnetic resonance imaging (MRI) (Figures 2A,B) showed a herniated disc at the L4-L5 level, resulting in an abnormally narrow spinal canal. Unlike the common case, the MRI of the patient's lumbar spine revealed that the IVC was located on the left side of the AA. The L4-L5 intervertebral disc space was unstable with an angle variation of 11° on the hyperextension lateral radiographs and the flexion lateral radiographs (Figures 2C,D). We confirmed that the patient had a left-sided IVC by CT venography. The imaging (Figure 2E) demonstrated that the IVC, formed by the union of the left and right CIV, arises superior and to the left of the aorta. At the level of approximately the L1-2 intervertebral space, where the left and right renal veins converge, it sequentially crosses the midline of the spine and the AA, eventually coursing along the left side of the AA. This is consistent with the left-sided IVC described in the literature (9).
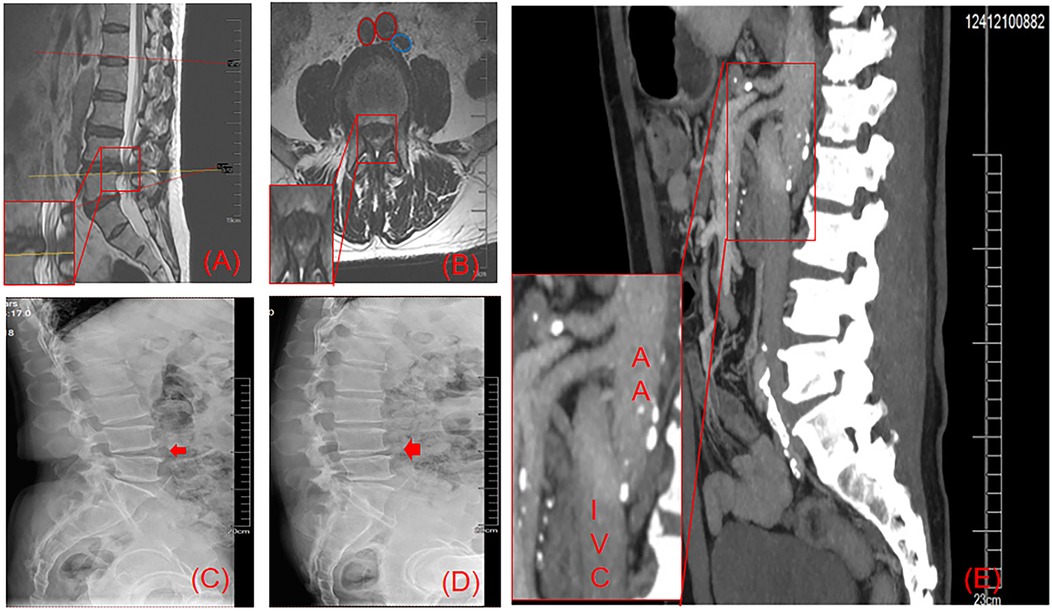
Figure 2. As shown in the magnified sagittal (A) and axial (B) T2-weighted MRI views, a massive L4-5 disc herniation with significant spinal canal stenosis and neural compression is observed. Figure B demonstrates the left-sided IVC (blue circle) and the bifurcated AA (red circle) at the L4-5 level. Comparative dynamic radiographs (C): hyperextension; (D) hyperflexion) reveal 11° of angular change between the L4-5 endplates. (E) (IVC venography) confirms the IVC's left-anterior course along the spine, crossing ventral to the aorta at the L1 inferior endplate.
Diagnosis
1.Grade I L4-L5 spondylolisthesis (anterior displacement of L4 vertebral body relative to L5, Meyerding classification); 2. L4-L5 lumbar spinal stenosis secondary to:Central disc protrusion
Surgical plan
For this lumbar fusion case, we recommend the oblique lumbar interbody fusion (OLIF) procedure with lateral fixation to optimally balance the patient's clinical needs with minimally invasive objectives.
Surgical procedure
After successful anesthesia, the patient was placed in the left lateral decubitus position. Standard chest and iliac supports were applied, with additional bolsters placed between the legs (padded with blankets) and a protective donut-shaped pad under the dependent fibular head (Figure 3). The operating table was flexed at the lumbar bridge to level the surgical-side flank with the thorax and pelvis, thereby increasing the distance between the left costal margin and iliac crest to optimize surgical access. Under fluoroscopic guidance, the anterior superior iliac spine (ASIS) and iliac crest were identified and marked, followed by localization and marking of the target L4-5 intervertebral disc space.
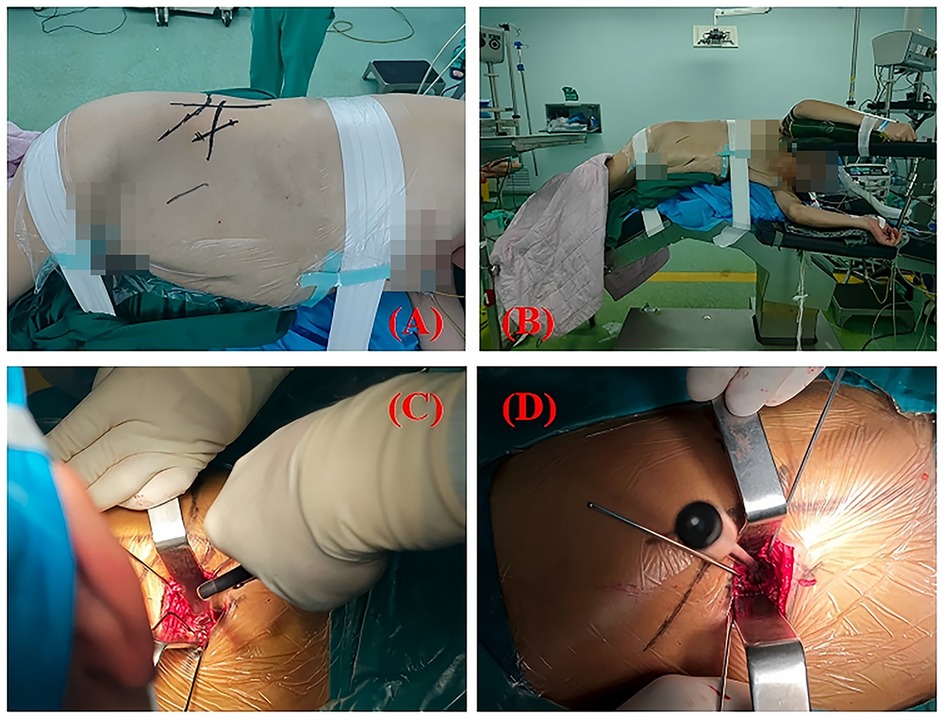
Figure 3. (A,B) demonstrates the standardized OLIF positioning, with the patient in left lateral decubitus and hips elevated. Skin markings are visible for surgical planning. (C) demonstrates the surgeon performing discectomy using a pituitary rongeur, while (D) shows the trial cage being inserted into the intervertebral space.
A 6 cm oblique incision was made in the right anterolateral abdomen, extending posterosuperiorly to anteroinferiorly. The incision was carried through the layers of the anterior abdominal wall to enter the peritoneal cavity. Subsequently, the posterior abdominal wall was approached to expose the retroperitoneal structures. The transversalis fascia was not incised but instead bluntly dissected with finger dissection, sweeping the fascia and retroperitoneal fat anteriorly to naturally guide the approach toward the psoas muscle region. The psoas muscle was identified through blunt dissection of the anterolateral attachments to the intervertebral disc space.Simultaneously, the palpable pulsation of the abdominal aorta was identified. After locating the pulse, deeper finger dissection allowed identification of the non-pulsatile IVC, which presented as a soft tissue structure overlying the anterior disc space. Upon direct visualization through the incision, the IVC appeared deep blue with an approximate diameter of 2.5 cm, positioned anterior and slightly leftward relative to the spine. The oblique working corridor was established through simultaneous anterior mobilization of the peritoneal and vascular structures, coupled with posterior retraction of the psoas muscle. After adequate exposure of the target intervertebral disc, discectomy, cartilaginous endplate removal, and interbody cage implantation were performed. Given the oblique trajectory of OLIF, precise directional control is critical—deviation toward the spinal canal risks inadequate disc space penetration and potential neural injury. The retroperitoneal space was accessed via blunt dissection. After clearing superficial annular tissue, the annulus fibrosus was incised, followed by discectomy and intervertebral space preparation. Under fluoroscopic guidance, the disc space was appropriately distracted, and a properly sized interbody cage was implanted orthogonally. Supplemental lateral screw fixation was then performed (Figure 4). During retractor removal, meticulous hemostasis was verified to ensure no active bleeding remained. All residual bone graft material was meticulously cleared from the psoas muscle surface. The surgical site was copiously irrigated, followed by layered wound closure with placement of a closed suction drain.
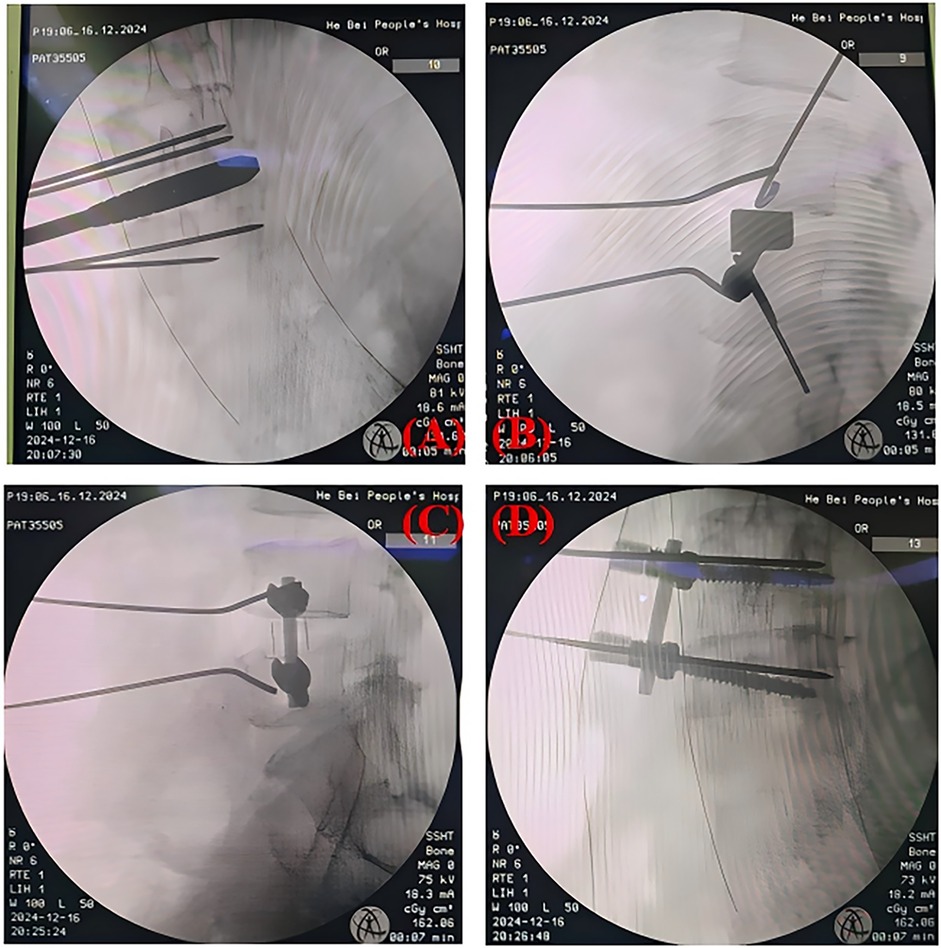
Figure 4. (A,B) show intraoperative fluoroscopic views after trial cage placement, while (C,D) display the final construct with implanted instrumentation.
Postoperative outcomes
The total operative time was 104 minutes, with an estimated blood loss of approximately 15 ml (Table 1). The position and size of the implant were confirmed by re-examination of the radiographs on the 3rd postoperative day (Figure 5). With the lower back pain VAS score decreasing from 7 to 2 and the lower limb pain VAS score decreasing from 5 to 1, the patient's pain was significantly relieved. Meanwhile, the patient's continuous walking distance gradually increased. No surgical complications were observed during the perioperative period (Table 2).
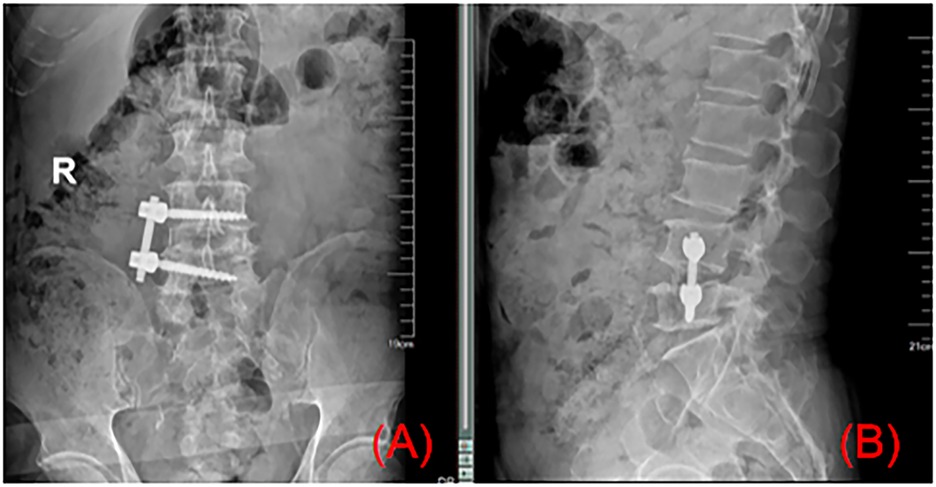
Figure 5. Postoperative radiographs (A,B) confirmed optimal positioning of the lateral screw-rod construct and interbody cage, consistent with intraoperative fluoroscopic findings.
Ostoperative telephone surveys were completed at 2 weeks and 7 months to evaluate recovery status.
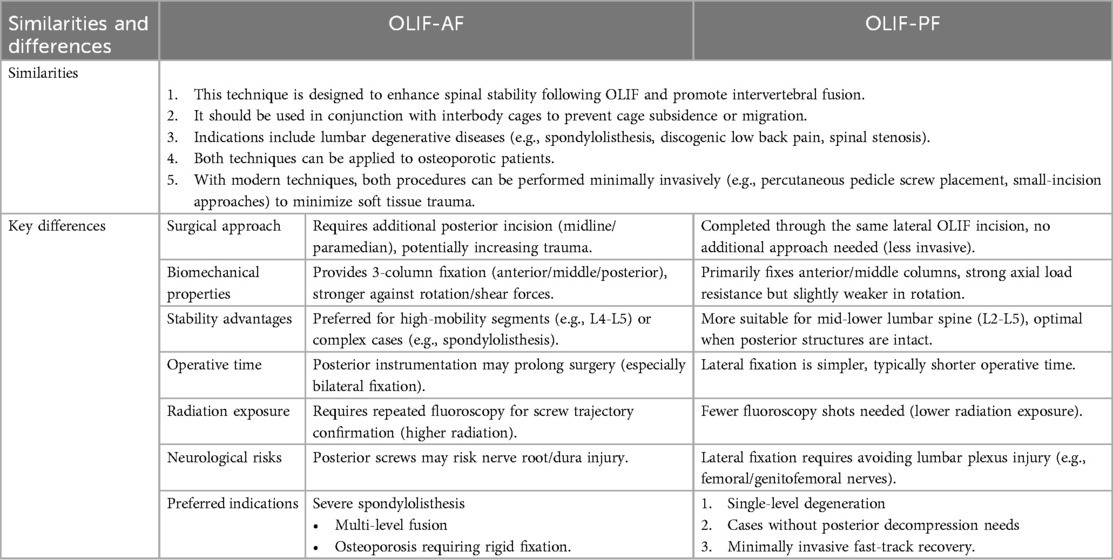
Discussion
In 2012, Silvestre et al. first reported the OLIF (10). This procedure accesses the target intervertebral disc through an oblique anterior abdominal incision. In the general population, the IVC is located anterior and to the right of the spine, so the surgical window is consistently chosen between the left edge of the AA and the right edge of the left psoas muscle. Molinares et al. (11) described the surgical window at the L2-S1 intervertebral discs through the dissection and measurement of 20 fresh-frozen cadaveric torso specimens. Through quantitative evaluation of the surgical window. Tao et al. (4) concluded that the positioning of major retroperitoneal vessels, particularly the IVC, is a significant potential factor contributing to variations in the surgical window. This is because intraoperative injury to the IVC can lead to catastrophic vascular complications. However, the above studies have not elaborated on the situation when anatomical variations in the IVC occur. Among the various anatomical variations described by Dilli et al. (12), both the left-sided IVC and the duplicated IVC are considered to influence the surgical approach (9, 13). Therefore, we report this case of OLIF performed via a right anterolateral approach, combined with the case reports from Berry (14) and Liu et al. (15), to provide references for the right-sided approach.For patients with scoliosis, prior lumbar surgery or significant abdominal scarring, a right-sided approach may be necessary.
This patient was treated with lateral screw-rod internal fixation. OLIF can be used alone without internal fixation (OLIF-SA), combined with lateral screw-rod internal fixation (OLIF-AF), and posterior percutaneous pedicle screw internal fixation (OLIF-PF) to obtain more stable support (16). OLIF-SA carries potential risks of complications due to its questionable biomechanical stability (17). The other two internal fixation methods differ in terms of perioperative complications and fusion rates. OLIF-AF has fewer complications because it does not require intraoperative repositioning or additional incisions. Compared to lateral fixation, OLIF-PF is widely used to enhance fusion rates (18, 19). Studies have shown that as the degree of osteoporosis increases, the range of motion in flexion-extension, lateral bending, and rotation decreases across all internal fixation methods (20). Compared with OLIF-PF, OLIF-AF has a larger range of flexion, extension, and rotation, and no significant difference in lateral bending range. Some advantages of OLIF-AF are well demonstrated in this case (Table 3). However, the long-term therapeutic outcomes must be evaluated through long-term follow-up data.
Patient-friendly version
Preoperative 3D imaging clearly demonstrated anomalous left-sided vascular anatomy, contraindicating the conventional approach. Although right-sided access represented a less common surgical strategy, it provided safer vascular avoidance. While minor incision-related tightness persists, the dramatic improvement in pain-related quality of life validates this approach.
At one-week follow-up, recovery met all expected milestones: ambulation was pain-limited only by surgical site discomfort, wounds healed without erythema or drainage, and oral analgesics provided adequate symptom control. The discharge protocol included detailed activity restrictions, red flag education, and scheduled 4-week postoperative evaluation.
Conclusions
A left-sided IVC is uncommon but holds significant clinical importance. When the anatomical characteristics of IVC variants remain indeterminate, preoperative IVC venography becomes essential. This imaging modality provides definitive vascular mapping to guide safe surgical corridor selection, particularly for OLIF approaches in anatomically complex cases. Meanwhile, overcoming the muscle memory formed during the conventional left abdominal approach presents some challenges for surgeons. For this patient, the surgery via the right abdominal approach was successful. However, we are still following up to assess the long-term therapeutic outcomes.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
YM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. SG: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. FM: Conceptualization, Data curation, Funding acquisition, Investigation, Methodology, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. WL: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Project administration, Resources, Software, Visualization, Writing – original draft, Writing – review & editing. YN: Conceptualization, Formal analysis, Funding acquisition, Investigation, Software, Validation, Visualization, Writing – original draft, Writing – review & editing. JW: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Li R, Li X, Zhou H, Jiang W. Development and application of oblique lumbar interbody fusion. Orthop Surg. (2020) 12(2):355–65. doi: 10.1111/os.12625
2. Mobbs RJ, Phan K, Malham G, Seex K, Rao PJ. Lumbar interbody fusion: techniques, indications and comparison of interbody fusion options including PLIF, TLIF, MI-TLIF, OLIF/ATP, LLIF and ALIF. J Spine Surg. (2015) 1(1):2–18. doi: 10.3978/j.issn.2414-469X.2015.10.05
3. Mehren C, Mayer HM, Zandanell C, Siepe CJ, Korge A. The oblique anterolateral approach to the lumbar spine provides access to the lumbar spine with few early complications. Clin Orthop Relat Res. (2016) 474(9):2020–7. doi: 10.1007/s11999-016-4883-3
4. Tao Y, Huang C, Li F, Chen Q. Magnetic resonance imaging study of oblique corridor and trajectory to L1-L5 intervertebral disks in lateral position. World Neurosurg. (2020) 134:e616–23. doi: 10.1016/j.wneu.2019.10.147
5. Woods KR, Billys JB, Hynes RA. Technical description of oblique lateral interbody fusion at L1-L5 (OLIF25) and at L5-S1 (OLIF51) and evaluation of complication and fusion rates. Spine J. (2017) 17(4):545–53. doi: 10.1016/j.spinee.2016.10.026
6. Bass JE, Redwine MD, Kramer LA, Huynh PT, Harris JH Jr. Spectrum of congenital anomalies of the inferior vena cava: cross-sectional imaging findings. Radiographics. (2000) 20(3):639–52. doi: 10.1148/radiographics.20.3.g00ma09639
7. Hirsch DM Jr, Chan KF. Bilateral inferior vena cava. JAMA. (1963) 185:729–30. doi: 10.1001/jama.1963.03060090061024
8. Glotzer OS, Rieth G, Kistler A, Hnath J, Gifford E, Darling RC. Use of the right retroperitoneum as an alternative approach to the abdominal aorta. J Vasc Surg. (2023) 78(1):71–6. doi: 10.1016/j.jvs.2023.02.013
9. Li SJ, Lee J, Hall J, Sutherland TR. The inferior vena cava: anatomical variants and acquired pathologies. Insights Imaging. (2021) 12(1):123. doi: 10.1186/s13244-021-01066-7
10. Silvestre C, Mac-Thiong JM, Hilmi R, Roussouly P. Complications and morbidities of Mini-open anterior retroperitoneal lumbar interbody fusion: oblique lumbar interbody fusion in 179 patients. Asian Spine J. (2012) 6(2):89–97. doi: 10.4184/asj.2012.6.2.89
11. Molinares DM, Davis TT, Fung DA. Retroperitoneal oblique corridor to the L2-S1 intervertebral discs: an MRI study. J Neurosurg Spine. (2016) 24(2):248–55. doi: 10.3171/2015.3.SPINE13976
12. Dilli A, Coşar Ayaz FS, Karacan K, Zengin K, Ayaz ÜY, Karabacak OR, et al. Evaluation of renal anomalies, inferior vena cava variations, and left renalvein variations by lumbar magnetic resonance imaging in 3000 patients. Turk J Med Sci. (2017) 47(6):1866–73. doi: 10.3906/sag-1611-23
13. Sheth S, Fishman EK. Imaging of the inferior vena cava with MDCT. Am J Roentgenol. (2007) 189(5):1243–51. doi: 10.2214/AJR.07.2133
14. Berry CA. Oblique lumbar interbody fusion in patient with persistent left-sided inferior vena cava: case report and review of literature. World Neurosurg. (2019) 132:58–62. doi: 10.1016/j.wneu.2019.08.176
15. Liu C, Zhai J, Yuan Q, Zhang Y, Xu H. A patient with left-sided inferior vena cava who received oblique lumbar interbody fusion surgery: a case report. J Med Case Rep. (2020) 14(1):21. doi: 10.1186/s13256-020-2342-y
16. Zhang XY, Wang K, Wang YT, Zhang WK, Wu H. Efficacy of oblique lumbar interbody fusion combined with different internal fixation methods in the treatment of degenerative lumbar diseases. Zhonghua yi xue za zhi. (2023) 103(7):520–5. doi: 10.3760/cma.j.cn112137-20221123-02478
17. Wu MT, Chung TT, Chen SC, Kao TJ, Song WS. Oblique lateral interbody fusion in heterogenous lumbar diseases: anterolateral screw fixation vs. Posterior percutaneous pedicle screw fixation - A single center experience. Front Surg. (2022) 9:989372. doi: 10.3389/fsurg.2022.989372
18. Abe K, Orita S, Mannoji C, Motegi H, Aramomi M, Ishikawa T, et al. Perioperative complications in 155 patients who underwent oblique lateral interbody fusion surgery: perspectives and indications from a retrospective, multicenter survey. Spine. (2017) 42(1):55–62. doi: 10.1097/BRS.0000000000001650
19. Li HD, Zhong L, Min JK, Fang XQ, Jiang LS. Oblique lateral interbody fusion combined with lateral plate fixation for the treatment of degenerative diseases of the lumbar spine: a retrospective study. Medicine (Baltimore). (2022) 101(7):e28784. doi: 10.1097/MD.0000000000028784
Keywords: oblique lumbar interbody fusion, left-sided inferior vena cava, vascular anomaly, lateral screw-rod fixation, lumbar degenerative disease
Citation: Meng Y, Gao S, Meng F, Li W, Niu Y and Wei J (2025) Oblique lumbar interbody fusion—address to an anatomical challenge: a case report. Front. Surg. 12:1621533. doi: 10.3389/fsurg.2025.1621533
Received: 8 May 2025; Accepted: 31 July 2025;
Published: 20 August 2025.
Edited by:
Osvaldo Mazza, Bambino Gesù Children's Hospital (IRCCS), ItalyReviewed by:
Suyash Singh, All India Institute of Medical Sciences, IndiaLiviu Moldovan, George Emil Palade University of Medicine, Pharmacy, Sciences and Technology of Târgu Mureş, Romania
Copyright: © 2025 Meng, Gao, Meng, Li, Niu and Wei. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jingchao Wei, NjE4NjEwNTlAcXEuY29t
 Yuxin Meng
Yuxin Meng Shangju Gao2
Shangju Gao2 Wenyi Li
Wenyi Li