- Department of Dermatology, Huangshi Central Hospital, Affiliated Hospital of Hubei Polytechnic University, Huangshi, Hubei, China
Background: Basal cell carcinoma (BCC) commonly affects facial skin, with surgical excision being the usual treatment. However, surgery often leads to complications and slow healing, impacting quality of life. Recently, ultra-pulsed CO₂ laser has emerged as a minimally invasive option with good cosmetic results, but its effectiveness and patient satisfaction compared to surgery are still uncertain.
Objective: This study aims to compare the clinical outcomes and patient satisfaction between ultra-pulsed CO₂ laser treatment and surgical excision for patients with facial BCC.
Methods: A retrospective analysis was conducted on 100 patients with facial BCC treated at our dermatology department from January 2021 to January 2024.Among them, 50 patients received ultra-pulsed CO₂ laser treatment, while 50 underwent traditional surgical excision. We compared the tumor excision rates, incidence of postoperative complications, healing times, and patient satisfaction (assessed through a questionnaire) between the two groups.
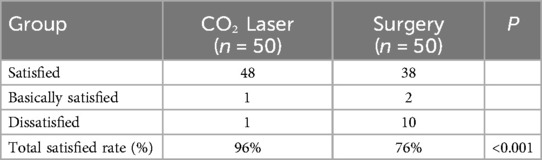
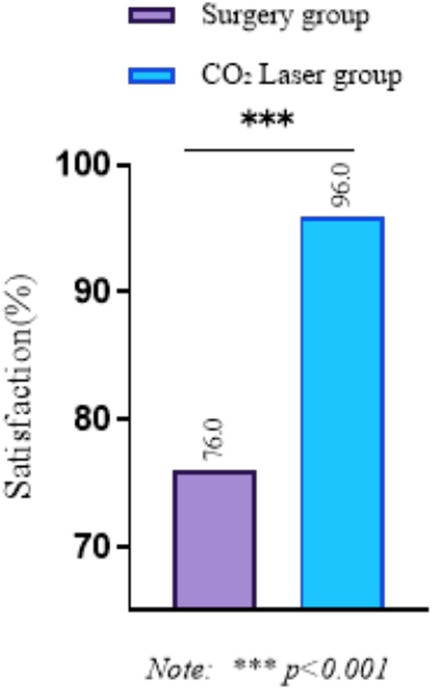
Results: The clinical effective rate in the ultra-pulsed CO₂ laser group was 94.0%, compared to 90.0% in the surgical excision group, with no statistically significant difference between the two groups (p > 0.05).Postoperative complications in the CO₂ laser group were primarily mild burns and inflammatory erythema, all of which resolved spontaneously within 1–2 days without treatment, with no serious adverse reactions reported. Recurrence rates were 4.00% (laser) vs. 16.00% (surgery), the difference between the two groups was statistically significant (p < 0.05). Regarding pain scores, there was no significant difference in preoperative pain scores between the groups; however, the CO₂ laser group reported significantly lower pain scores at 1, 3 days and 7days postoperatively (P < 0.001). Furthermore, patient satisfaction was significantly higher in the CO₂ laser group compared to the surgical group (96.0% vs. 76.0%, P < 0.001).
Conclusion: In summary, both ultra-pulsed CO₂ laser treatment and surgical excision exhibit similar clinical efficacy in the management of facial basal cell carcinoma. Nonetheless, ultra-pulsed CO₂ laser treatment offers notable benefits regarding postoperative complication rates, pain scores, and patient satisfaction. Consequently, ultra-pulsed CO₂ laser treatment may be regarded as an effective and patient-friendly alternative for the treatment of facial basal cell carcinoma.
Introduction
Basal cell carcinoma (BCC) is one of the most common skin malignancies, particularly prevalent in facial regions (1). BCC arises from the atypical proliferation of cells within the basal layer of the epidermis. Owing to its indolent growth and minimal metastatic potential, it is frequently categorized as a relatively benign neoplasm (2). However, with the aging global population and increased ultraviolet exposure, the incidence of BCC has been rising annually, significantly impacting patients' quality of life (3). This is particularly applicable to lesions situated in prominent areas, such as the face, where they not only impact aesthetic appearance but may also contribute to psychological distress and social anxiety (4).
Surgical excision has traditionally been considered the primary approach for treating BCC (5). By directly removing the tumor along with surrounding tissue, surgical excision effectively eliminates tumor cells and reduces the risk of recurrence (6). However, this procedure is frequently linked to a greater risk of postoperative issues, such as infections, excessive bleeding, pain, and the formation of scars (7). These complications can extend the recovery period and adversely affect patients' mental health and social interactions (8). Moreover, the extended healing time post-surgery further increases the burden on patients.
Recent advancements in laser technology have sparked significant interest in ultra-pulsed CO₂ laser treatment, primarily due to its minimally invasive properties and excellent cosmetic results (9). This technique employs a high-energy laser beam to precisely excise tumor tissue while minimizing damage to surrounding healthy tissue, thereby reducing the risk of postoperative complications and accelerating the healing process (10). When compared to traditional surgical excision, ultra-pulsed CO₂ laser treatment presents several advantages, including reduced trauma, quicker recovery times, and enhanced aesthetic outcomes—factors that are leading to its growing acceptance among patients and healthcare providers alike (11).
While various studies have investigated the use of laser therapy for treating skin tumors, there is still a notable gap in comparative research focusing on clinical outcomes and patient satisfaction between ultra-pulsed CO₂ laser treatment and traditional surgical excision for BCC. This study seeks to systematically assess the clinical effectiveness and patient satisfaction associated with ultra-pulsed CO₂ laser treatment compared to surgical excision in individuals with facial BCC. The results aim to deliver more precise and trustworthy evidence for clinical practice, assisting physicians in creating more informed and effective treatment strategies for their patients.
Methods
General information
This study conducted a retrospective analysis of 100 patients with facial BCC who received treatment in the dermatology department of our hospital from March 2021 to October 2024. All patients were diagnosed through pathology and had no significant comorbidities. Participants were categorized into two groups based on their treatment approach: the ultra-pulsed CO₂ laser treatment group, which included 50 patients, and the surgical excision group, also comprising 50 patients. Group allocation was determined by clinical decision-making considering tumor characteristics and patient preference, ensuring no significant differences in baseline data.
Specifically, several factors influenced the group assignment:
• Tumor site: For tumors located in cosmetically sensitive areas (such as the nasal tip, eyelid margin, and lip), where preserving facial appearance is of high priority, patients were more likely to be assigned to the ultra-pulsed CO₂ laser treatment group after full communication with physicians. In contrast, tumors in non-cosmetically critical areas (such as the forehead, cheek with abundant soft tissue) were more inclined to be treated with surgical excision.
• Patient preference: Some patients expressed strong willingness to avoid surgical scars or preferred a less invasive treatment, thus choosing ultra-pulsed CO₂ laser treatment; others preferred a more radical treatment method and opted for surgical excision.
• Tumor characteristics: Although all tumors had a diameter of 2.0 cm or less, for those with a relatively shallow invasion depth (assessed by preoperative ultrasound), ultra-pulsed CO₂ laser treatment was more often recommended, while surgical excision was preferred for tumors with a slightly deeper invasion.
Inclusion and exclusion criteria
Inclusion criteria were as follows:
1. Confirmation of basal cell carcinoma through skin biopsy and histological examination (12);
2. Patients had not received any other treatments such as radiotherapy or chemotherapy;
3. Tumor diameter was 2.0 cm or less;
4. Availability of complete clinical data.
Exclusion criteria included:
1. History of photosensitivity;
2. Presence of severe systemic diseases;
3. Currently undergoing radiotherapy or chemotherapy;
4. Pregnant or breastfeeding women.
Ethical approval
This study was reviewed and approved by the Ethics Committee of Huangshi Central Hospital. A formal waiver of informed consent for study participation was granted by the committee due to the retrospective nature of the research, which involved analysis of de-identified clinical data routinely collected during standard care. All patient information was processed with strict confidentiality measures to protect privacy, in accordance with the Declaration of Helsinki and local ethical guidelines. As no identifiable personal data or images were included in the manuscript, additional consent for publication was not required.
Treatment methods
Ultra-pulsed CO₂ Laser Treatment (13): Patients received ultra-pulsed CO₂ laser treatment under local anesthesia. The specific steps are as follows: the lesion area was routinely disinfected, and local infiltration anesthesia (2% lidocaine) was administered. A CO₂ laser treatment machine was used to ablate the diseased tissue. The laser was set with a wavelength of 10.6 μm, pulse duration of 100–300 μs, and fluence of 50–100 J/cm2. Initially, the tumor was vaporized from the epidermis gradually deeper into the lesion. At a distance of 0.5 cm from the lesion edge, coagulation vaporization was performed around the lesion until reaching the dermal papilla layer. Upon observing the dermal papilla granules, vaporization was continued inward along the dermis, surrounding the tumor until complete removal of the lesion. If bleeding occurred during vaporization, coagulation hemostasis was performed first, followed by vaporization. The 635 nm semiconductor laser treatment device was manufactured by Wuhan Lingyun Optoelectronic Technology Co., Ltd., model FD-400-B; the CO₂ laser treatment machine was produced by Xiaogan Sunshine Shenqi Medical Technology Co., Ltd., model YG-40A.
Surgical Excision: Patients in the surgical group underwent traditional surgical excision under local anesthesia. The specific steps are as follows: local anesthesia was administered using 2% lidocaine, and a diamond-shaped excision was performed at a distance of 5 mm from the tumor edge, removing the basal cell carcinoma and an additional 5 mm of surrounding skin. The subcutaneous tissue was incised sequentially until reaching the fat layer. After excising the tumor and surrounding tissue, the wound was irrigated with saline, and the area was sutured after confirming that the lesion had been completely excised.
Observational indicators
Basic patient information was collected, including age, sex, tumor size, and location.
1. Clinical Efficacy Rate (14): All patients were followed up one year after treatment to assess the morphology, color, and area of the lesions and to evaluate efficacy. Complete response was defined as the disappearance of the lesion, with only pigmentation or depigmentation remaining, and no original pathological changes on histological examination; partial response was defined as a reduction of 50% or more in the lesion size; no response was defined as a reduction of less than 50% or no change. The total efficacy rate was the sum of complete and partial responses.
2. Complication Incidence: The incidence of complications occurring within 30 days postoperatively was recorded for both groups, including infection, bleeding, and scar formation.
3. Postoperative Recurrence Rate: All patients were followed up for one year after treatment. Recurrence was defined as the appearance of new lesions at the site of the previously disappeared lesion.
4. Postoperative Pain Assessment (15): Pain was assessed using the Visual Analog Scale (VAS), where 0 indicated no pain, 1–3 indicated mild pain, 4–6 indicated moderate pain, 7–9 indicated severe pain, and 10 indicated unbearable pain. Pain assessments were conducted preoperatively and on postoperative days 1, 3, and 7.
5. Patient Satisfaction: Assessed at 3-month follow-up, Patient satisfaction was evaluated at the 3-month postoperative follow-up using a study-specific questionnaire. The satisfaction questionnaire was developed based on clinical aesthetic concerns of facial BCC patients, including 3 core items: scar visibility, impact on facial appearance, and overall acceptability. It was categorized as follows: satisfied if only a linear scar remained and the patient felt it did not affect aesthetics; generally satisfied if the scar was more noticeable and mildly affected aesthetics; dissatisfied if a large scar remained and significantly affected aesthetics.
Statistical analysis
Statistical analyses were performed using IBM SPSS Statistics version 26.0 (IBM Corp., Armonk, NY, USA). Continuous data were expressed as mean ± standard deviation (SD) and analyzed using independent samples t-tests or paired t-tests, as appropriate. Categorical variables were presented as counts (percentages). For comparisons of proportions between two independent groups, Pearson's chi-square test was used when all expected frequencies were ≥5; otherwise, Fisher's exact test was applied. A two-sided p < 0.05 was considered statistically significant.
Results
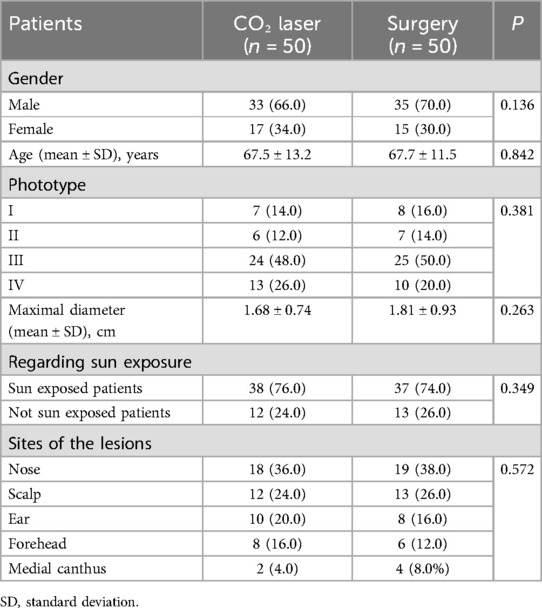
Comparison of baseline data between groups
In the CO₂ laser group of 50 patients, 66.0% (33 cases) were male and 34.0% (17 cases) were female, with an average age of 67.5 ± 13.2 years. In the surgical group, 70.0% (35 cases) were male and 30.0% (15 cases) were female, with an average age of 67.7 ± 11.5 years. The maximum diameter of the lesions in the CO₂ laser group was 1.68 ± 0.74 cm, while in the surgical group it was 1.81 ± 0.93 cm. In the CO₂ laser group, 76.0% (38 cases) were patients with sun exposure, compared to 74.0% (37 cases) in the surgical group. Statistical analysis showed no significant differences in baseline data between the two groups (P > 0.05), indicating comparability, as shown in Table 1.
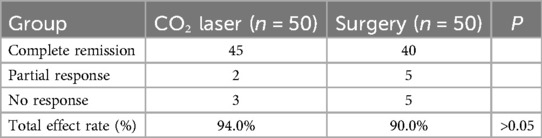
Overall clinical efficacy rate
One year after treatment, the overall clinical efficacy was compared between the two groups. In the CO₂ laser group, out of 50 patients, 45 achieved complete response and 2 achieved partial response, resulting in an overall efficacy rate of 94.0% (47/50). In the surgical group, out of 50 patients, 40 achieved complete response and 5 achieved partial response, leading to an overall efficacy rate of 90.0% (45/50). The difference in overall efficacy rates between the two groups was not statistically significant (P > 0.05), as detailed in Table 2.
Incidence of complications
After treatment, all patients in the CO₂ laser group experienced mild burns and inflammatory erythema, which resolved spontaneously within 1–2 days without serious adverse reactions. In the surgical group, 2 cases developed significant scar formation that affected the patients' appearance.
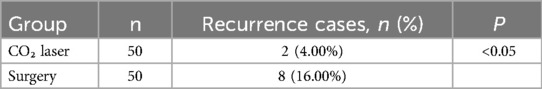
Postoperative recurrence rate
In the CO₂ laser group, there was 2 cases of recurrence, resulting in a recurrence rate of 4.00%. In the surgical group, there were 8 cases of recurrence, leading to a recurrence rate of 16.00%. The difference in overall recurrence rates between the CO₂ laser group and surgical group was statistically significant (P < 0.05), as illustrated in Table 3.
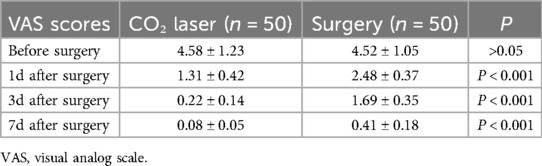
Comparison of VAS scores between groups
The preoperative pain score in the CO₂ laser group was 4.58 ± 1.23, compared to 4.52 ± 1.05 in the surgical group, with no statistically significant difference (P > 0.05). The postoperative pain scores on day 1 (1.31 ± 0.42) and day 3 (0.22 ± 0.14) were both lower than those in the control group (2.48 ± 0.37 and 1.69 ± 0.35, respectively), with statistically significant differences (P < 0.001), By day 7, pain scores in both groups were low (CO₂ laser: 0.08 ± 0.05; Surgical: 0.41 ± 0.18), but the difference remained statistically significant (P < 0.001) as shown in Table 4.
Comparison of surgical satisfaction between groups
The surgical satisfaction rate in the CO₂ laser group was 96.0% (48/50), significantly higher than the surgical group's satisfaction rate of 76.0% (38/50). The difference was statistically significant (P < 0.001), as presented in Table 5 and Figure 1.
Discussion
BCC is a common clinical skin tumor with an increasing incidence rate each year. The lesions are often superficial and grow slowly, with a low mortality rate (16). However, BCC exhibits characteristics of general malignant tumors, such as infiltration, invasion, and metastasis, which can lead to delays in treatment and serious adverse effects on patients' health (17). Currently, traditional surgery remains the primary method for treating BCC in clinical practice, but it often results in larger wounds and a higher likelihood of scarring.
This study compared the clinical effectiveness and patient satisfaction of ultra-pulsed CO₂ laser treatment vs. surgical excision for facial BCC. The results indicated no significant differences in baseline data between the two groups, ensuring the comparability and reliability of the study. In terms of overall clinical efficacy, both groups demonstrated high treatment effectiveness, with the CO₂ laser group achieving 94.0% and the surgical group achieving 90.0%. The difference in efficacy rates was not statistically significant (P > 0.05), suggesting that ultra-pulsed CO₂ laser treatment and surgical excision have comparable clinical effects in treating BCC (18).
The analysis revealed notable differences between the two groups in terms of complication rates, postoperative recurrence, pain scores, and overall satisfaction. In the CO₂ laser treatment group, postoperative complications were mainly minor, such as mild burns and inflammatory erythema, which typically resolved on their own within one to two days, without any serious side effects. In contrast, the surgical excision group reported two cases of significant scar formation that impacted aesthetics. Furthermore, the recurrence rate after surgery was considerably lower in the CO₂ laser group compared to the surgical group (4.00% vs. 16.00%, P < 0.05).
In terms of pain management, although preoperative pain scores were comparable between the two groups, the CO₂ laser treatment group demonstrated significantly lower pain scores on postoperative days 1, 3, and 7, highlighting the advantage of laser therapy in controlling postoperative discomfort. Additionally, patient satisfaction was markedly higher in the CO₂ laser group (96.0% vs. 76.0%, P < 0.001), reinforcing the benefits of this treatment option for BCC. These findings are consistent with previous studies that demonstrate the advantages of ultra-pulsed CO₂ laser treatment, including its minimally invasive nature, quicker recovery times, and improved cosmetic outcomes, alongside a reduced rate of complications (19–22). Additionally, other studies have noted the advantages of laser treatment in reducing postoperative pain and enhancing patient satisfaction (23–25). The outcomes confirm the study's conclusions, highlighting the effectiveness and benefits of ultra-pulsed CO₂ laser treatment for BCC.
Limitations
While this study has yielded valuable insights, it does have several limitations. First, being a single-center, retrospective analysis with a relatively small sample size. Notably, the non-randomized assignment based on clinical factors, especially patient preference and cosmetic location, introduces substantial potential for selection bias, particularly concerning outcomes like patient satisfaction and potentially recurrence. Second, the clinical outcomes were only assessed one year post-treatment, lacking long-term follow-up on recurrence rates, which limits the ability to evaluate the lasting effects of both treatment options. Additionally, the study did not analyze or optimize specific parameters of the laser treatment, which could impact the accuracy and reproducibility of the results. The satisfaction instrument, though clinically grounded, requires formal validation in future studies. Although we extended pain assessment to postoperative day 7, more frequent measurements during the first 72 h might have revealed nuanced pain patterns. Future studies could incorporate daily assessments during acute recovery. Future research should focus on increasing the sample size, extending the follow-up period, and refining the parameters of laser treatment to provide a more thorough evaluation of the clinical outcomes associated with ultra-pulsed CO₂ laser therapy for BCC.
Conclusion
In summary, both ultra-pulsed CO₂ laser treatment and surgical excision exhibit similar clinical efficacy in the management of facial BCC. Nevertheless, ultra-pulsed CO₂ laser treatment offers distinct benefits concerning the incidence of complications, postoperative recurrence rates, pain scores, and patient satisfaction. Consequently, ultra-pulsed CO₂ laser treatment may be regarded as an effective and patient-friendly alternative for the treatment of facial BCC. Future research should aim to further investigate and refine the specific parameters of laser treatment to improve therapeutic outcomes and enhance patient satisfaction.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Ethics Committee of Huangshi Central Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation was not required from the participants or the participants' legal guardians/next of kin in accordance with the national legislation and institutional requirements.
Author contributions
A-CC: Methodology, Data curation, Conceptualization, Writing – original draft, Visualization. CZ: Writing – original draft, Data curation, Methodology, Conceptualization, Visualization. Q-CJ: Project administration, Supervision, Writing – review & editing. PZ: Supervision, Writing – review & editing, Project administration.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Uhlman K, Bonert M, Yuen K, Farrokhyar F, Thoma A. Margin status of basal cell carcinoma: what can be done better? J Plast Reconstr Aesthet Surg. (2024) 97:156–62. doi: 10.1016/j.bjps.2024.07.063
2. Miyazaki S, Hoashi T, Tone Y, Park A, Otani S, Kanda N, et al. Narrow histopathological margins are acceptable in surgical resection of basal cell carcinoma in Japanese: a single-center retrospective study. J Nippon Med Sch. (2024) 91(3):296–306. doi: 10.1272/jnms.JNMS.2024_91-308
3. Krekel J, Dippel E, Löser CR. Full-thickness skin grafts - Better than their reputation: aesthetic defect coverage for cartilage defects after basal cell carcinoma of the ear. J Dtsch Dermatol Ges. (2024) 22(7):1036–8. doi: 10.1111/ddg.15401
4. Robinson BP, Nanni GM. Utilizing fractional lasers and tirbanibulin ointment to treat squamous and basal cell carcinomas. Arch Dermatol Res. (2024) 316(10):683. doi: 10.1007/s00403-024-03423-0
5. Solanes-Vilanova F, Chiers K, Gil-Lianes J, Hellebuyck T. Clinical features, surgical management and outcome of squamous and basal cell carcinoma in squamates and chelonians. Vet Dermatol. (2024) 35(6):626–40. doi: 10.1111/vde.13282
6. Kiely JR, Patel AJK. A retrospective study of 694 basal cell carcinoma excisions to quantify deep margin documentation and clearance compared to histological type and surgical margin. J Plast Reconstr Aesthet Surg. (2019) 72(11):1805–12. doi: 10.1016/j.bjps.2019.06.002
7. Wu MJ, Chen YC, Cui XL, Yang Q, Xue QL. Tislelizumab for squamous lung cancer combined with basal cell carcinoma of the skin: a case report. Medicine (Baltimore). (2023) 102(19):e33788. doi: 10.1097/MD.0000000000033788
8. Gürsel Ürün Y, Can N, Bağış M, Sarıkaya Solak S, Ürün M. Adequacy of surgical margins, re-excision, and evaluation of factors associated with recurrence: a retrospective study of 769 basal cell carcinomas. An Bras Dermatol. (2023) 98(4):449–59. doi: 10.1016/j.abd.2022.07.005
9. Leszczynski R, da Silva CA, Pinto A, Kuczynski U, da Silva EM. Laser therapy for treating hypertrophic and keloid scars. Cochrane Database Syst Rev. (2022) 9(9):Cd011642. doi: 10.1002/14651858.CD011642.pub2
10. Tran BQ, Tran TNA, Doan EVL, Nguyen TTP, Nguyen HT. Simultaneous versus sequential fractional CO(2) laser and subcision combination for management of post-acne atrophic scars: a split-face comparative study. J Cosmet Dermatol. (2024) 23(10):3210–21. doi: 10.1111/jocd.16395
11. Xu Y, Deng Y. Ablative fractional CO₂ laser for facial atrophic acne scars. Facial Plastic Surgery: FPS. (2018) 34(2):205–19. doi: 10.1055/s-0037-1606096
12. Lang BM, Balermpas P, Bauer A, Blum A, Dirschka T, Follmann M, et al. S2k guideline basal cell carcinoma of the skin (update 2023). J Dtsch Dermatol Ges. (2024) 22(12):1697–714. doi: 10.1111/ddg.15566
13. Kwon HH, Yang SH, Lee J, Park BC, Park KY, Jung JY, et al. Combination treatment with human adipose tissue stem cell-derived exosomes and fractional CO₂ laser for acne scars: a 12-week prospective, double-blind, randomized, split-face study. Acta Derm-Venereol. (2020) 100(18):adv00310. doi: 10.2340/00015555-3666
14. Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. (2009) 45(2):228–47. doi: 10.1016/j.ejca.2008.10.026
15. Budrovac D, Radoš I, Hnatešen D, Haršanji Drenjancevic I, Tot OK, Katic F, et al. Effectiveness of epidural steroid injection depending on discoradicular contact: a prospective randomized trial. Int J Environ Res Public Health. (2023) 20(4):3672. doi: 10.3390/ijerph20043672
16. Ürün YG, Ürün M, Danisman MS. Dermoscopic characteristics of cutaneous lupus erythematosus according to subtype, lesion location, lesion duration, and CLASI score. Dermatol Pract Concept. (2024) 14(1):e2024040. doi: 10.5826/dpc.1401a40
17. Bichakjian CK, Olencki T, Aasi SZ, Alam M, Andersen JS, Berg D, et al. Basal cell skin cancer, version 1.2016, NCCN clinical practice guidelines in oncology. J Natl Compr Canc Netw. (2016) 14(5):574–97. doi: 10.6004/jnccn.2016.0065
18. Iyer S, Bowes L, Kricorian G, Friedli A, Fitzpatrick RE. Treatment of basal cell carcinoma with the pulsed carbon dioxide laser: a retrospective analysis. Dermatologic. (2004) 30(9):1214–8. doi: 10.1111/j.1524-4725.2004.30378.x
19. Kavoussi H, Ebrahimi A. Treatment and cosmetic outcome of superpulsed CO₂ laser for basal cell carcinoma. Acta Dermatovenerol Alp Pannonica Adriat. (2013) 22(3):57–61.24089133
20. Shokrollahi K, Javed M, Aeuyung K, Ghattaura A, Whitaker IS, O'Leary B, et al. Combined carbon dioxide laser with photodynamic therapy for nodular and superficial basal cell carcinoma. Ann Plast Surg. (2014) 73(5):552–8. doi: 10.1097/SAP.0b013e3182773ed2
21. Whitaker IS, Shokrollahi K, James W, Mishra A, Lohana P, Murison MC. Combined CO(2) laser with photodynamic therapy for the treatment of nodular basal cell carcinomas. Ann Plast Surg. (2007) 59(5):484–8. doi: 10.1097/SAP.0b013e3180338536
22. Wei MZ, Luo QN, Huang JY, Yan WJ, Li X. The clinical features and surgical treatment of facial basal cell carcinoma. Lin Chuang Er Bi Yan Hou Tou Jing Wai Ke Za Zhi. (2018) 32(4):279–81. doi: 10.13201/j.issn.1001-1781.2018.04.008
23. Ebrahimi A, Rezaei M, Kavoussi R, Eidizadeh M, Madani SH, Kavoussi H. Ultra-pulsed CO₂ laser with intraoperative pathologic assessment for treatment of periorbital basal cell carcinoma involving eyelash line. Dermatol Res Pract. (2014) 2014:931657. doi: 10.1155/2014/931657
24. Campolmi P, Brazzini B, Urso C, Ghersetich I, Mavilia L, Hercogova J, et al. Ultra-pulsed CO₂ laser treatment of basal cell carcinoma with intraoperatory histopathologic and cytologic examination. Dermatol Surg. (2002) 28(10):909–11; discussion 912. doi: 10.1046/j.1524-4725.2002.02076.x
Keywords: ultra-pulsed CO₂ laser treatment, basal cell carcinoma, surgical excision, clinical outcomes, patient satisfaction
Citation: Chen A-C, Zheng C, Jian Q-C and Zhang P (2025) Comparison of clinical effects and patient satisfaction between ultra-pulsed CO₂ laser treatment and surgical excision in patients with facial basal cell carcinoma. Front. Surg. 12:1628257. doi: 10.3389/fsurg.2025.1628257
Received: 14 May 2025; Accepted: 15 July 2025;
Published: 14 August 2025.
Edited by:
Mario Faenza, University of Campania Luigi Vanvitelli, ItalyReviewed by:
Maria Catorze, Hospital de Egas Moniz, PortugalZhangyu Bu, Hangzhou First People's Hospital, China
Martin Iurilli, University of Trieste, Italy
Copyright: © 2025 Chen, Zheng, Jian and Zhang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Qi-Chao Jian, amlhbjI3QDE2My5jb20=; Peng Zhang, NDE3MTA4NTc4QHFxLmNvbQ==
†These authors have contributed equally to this work
 An-Chen Chen†
An-Chen Chen† Qi-Chao Jian
Qi-Chao Jian