- 1Department of Hepatobiliary and Pancreatic Surgery, University Medical Center at Ho Chi Minh City, Ho Chi Minh City, Vietnam
- 2Department of Surgery, Faculty of Medicine, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
- 3Faculty of Human Medicine, Benha University, Benha, Egypt
- 4Online Research Club, Nagasaki, Japan
- 5Queen Alexandra Hospital, Portsmouth, United Kingdom
- 6Al Mokattam Insurance Hospital, Cairo, Egypt
- 7Faculty of Medicine, Alzaiem Alazhari University, Khartoum, Sudan
- 8Pediatric Surgery Department, University of Medicine and Pharmacy at Ho Chi Minh City, Ho Chi Minh City, Vietnam
- 9Russell H. Morgan Department of Radiology and Radiological Science, Johns Hopkins University School of Medicine, Baltimore, MD, United States
- 10Invasive Cardiology Nam Can Tho University, Can Tho, Vietnam
- 11Institute of Research and Development, Duy Tan University, Da Nang, Vietnam
- 12School of Medicine and Pharmacy, Duy Tan University, Da Nang, Vietnam
- 13School of Tropical Medicine and Global Health (TMGH), Nagasaki University, Nagasaki, Japan
Training in surgery and approval of new techniques in low- and middle-income countries (LMICs), usually depends on informal apprenticeship systems, that is often lacking standardization, structured mentorship and produce inconsistent patient outcomes. These challenges are particularly severe in rural areas, where training opportunities and healthcare infrastructure are limited. Recently, artificial intelligence (AI) has emerged as a reliable solution, providing applicable, Quantitative methods for skill development, competency evaluation and regulatory supervision. AI-powered tools, such as virtual reality (VR) simulations and tele-mentoring platforms, provide independent skill assessments and expand access to high-quality surgical education. However, implementing AI in LMICs faces some challenges, including inadequate resources, financial constraints and ethical issues related to data security and Equitable algorithms. This review compares usual surgical training and approval processes in LMICs and evaluates the promising role of AI to fill existing gaps and compares both approaches in terms of applicability, cost-effectiveness and impact on patient outcomes.
1 Introduction
Implementing new surgical techniques, in Low and Middle -Income Countries (LMICs), often follows informal, apprenticeship-style pathways. Training usually runs through bedside observation, short-term workshops, or mentorship from visiting specialists. These approaches lack standardized curricula and objective assessment tools. This system can lead to wide variability in surgical competency among surgeons and patient outcomes, especially in rural areas where access to mentorship and infrastructure is limited (1). Despite the absence of strong, evidence-based validation, the successful application of a novel technique by a single experienced surgeon can be sufficient to gain institutional or even ministry-level approval for broader use (2). Recently, artificial intelligence (AI) has begun to reshape rules for surgical education in LMICs. AI-powered tools, particularly those using computer vision and machine learning, offer data-driven solutions for skill acquisition and performance assessment. These technologies can analyze surgical videos and kinematic data, to distinguish between expert and limited performance, providing standardized and reliable assessments (3, 4). AI platforms also enable personalized feedback and remote simulation-based learning, allowing trainees to practice and improve skills outside traditional settings (5). These new technologies are impactful in LMICs, where training opportunities are sparse and surgical capacity building is a critical need (1).
This review explores the traditional processes by which new surgical techniques are learned and approved in LMICs, examines how AI addresses existing limitations and compares these pathways to highlight their effects on surgical quality, information access and patient safety.
2 Traditional training and approval in LMICs
2.1 Learning new techniques
The junior surgeons observe and assist their seniors in the operating room, then gradually practice. Mentorship system is still the base for surgical education, However, the shortage of experienced mentors, especially for advanced operations like laparoscopy or endoscopy, minimizes opportunities, especially in rural areas. The development of new surgical skills in LMICs is constrained by limited access to formal training programs, which are often concentrated in urban centers of high-income countries (HICs). Some surgeons pursue international fellowships in HICs, but high costs, visa restrictions and limited availability make this option feasible for only a few. Short-term workshops and cadaver labs provide concentrated exposure to new techniques, yet their sporadic nature and high costs limit scalability. Industry-sponsored training, often tied to proprietary technologies like laparoscopic systems, offers another avenue, but these programs prioritize commercial interests and lack standardization. These fragmented approaches result in inconsistent skill acquisition, leading to variable patient outcomes and potential risks to patient safety (6, 7).
2.2 Gaining approval without prior experience
Approval systems in Many LMICs, lack standardized criteria to assess surgeon clinical qualifications, relying instead on Preliminary evaluations by senior colleagues or hospital committees. Approving of new surgical techniques in LMICs is often informal and ethically complex. In some cases, surgeons perform a small number of demonstration cases under supervision, but access to experienced assessors is limited. Ministries of Health may grant approvals based on limited evidence, such as case reports or international guidelines, which may not account for local patient demographics or resource constraints. Certificate-based credentialing, where completion of a workshop or simulated-skills course suffices for operative privileges, is common but often lacks objective proof of proficiency. These regulatory gaps raise concerns about patient safety, as inexperienced surgeons may undertake complex procedures without adequate preparation, potentially compromising informed consent and clinical outcomes (8–10).
3 AI-Enhanced training and regulatory frameworks
3.1 AI in surgical training
Due to the lack of professional surgical mentorship in LMICs, there has been development of alternative solutions such AI platforms such as Touch Surgery which utilises virtual or augmented reality. Among several AI benefits include identifying errors, tracking performance, real-time objective feedback and steps for improvements. This enhances personalised surgical training tailored to the learner's current skill level leading to faster and efficient advancement. Furthermore, learners can receive real-time remote supervision from seniors or experts through digital technologies such as tele-mentoring.
All this have reduced barriers such as geographical location and unavailable experienced expert support. The result culminating into high-quality surgical education with less expenses on infrastructural constraints or inadequate in-person mentors (11, 12).
3.2 AI in credentialing and approval
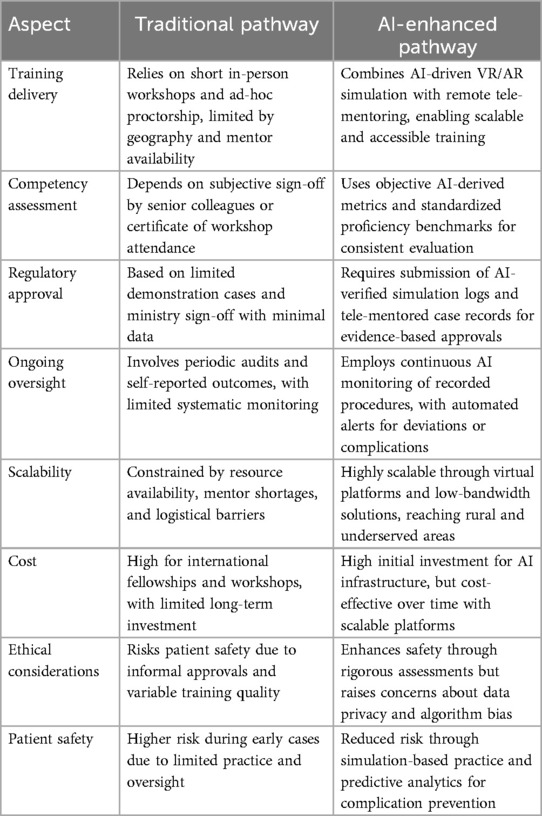
Surgical proficiency among Surgical residents can be assessed with the Objective Structured Assessment of Technical Skills (OSATS). Machine learning models, trained on surgical videos, analyze performance metrics like speed, precision and error rates, providing standardized assessments that overcome the subjectivity of traditional evaluations. These advancements streamline approvals and enhance patient safety by ensuring only competent surgeons perform new techniques. Through analysis of simulation and real-operation data, predictive metrics identifies surgeons' capability for independent practice, providing assessors with unbiazed decision. For example, after credentialing, AI systems enable continuous quality monitoring by reviewing recorded procedures to detect technique drift or rising complication rates, triggering targeted remedial training or privilege reassessment. Some regulators are exploring automated certification systems, where AI-verified training logs detailing simulated cases, competency scores and error trends are submitted as part of credentialing packages. AI enhances the objectivity and rigor of credentialing and regulatory processes (13–15), Table 1 shows comparison between traditional and AI enhanced pathways.
3.3 Challenges of AI adoption in LMICs
LMICs are burdened with several mitigating factors to implement AI in surgical training or care. Among many include poor internet access, unstable electricity and technical support. Furthermore, the overall cost in hardware, software license and system updates demand enormous initial investments and can be achieved through innovative funding models such as public-private collaborations or international grants. There also exists the challenge of data or information governance involving how surgical videos and performance metrics are handles under patient privacy laws, and the complexities involving data ownership ambiguities.
Lastly, some regulators and professionals push back the implementation of AI platforms particularly because of familiarity with conventional methods. There have also been some concerns about the accuracy and transparency of AI's decision-making process (16–18).
This expanded comparison illustrates how AI shifts surgical training and approval from resource-intensive, subjective processes to scalable, data-driven systems, improving equity, safety and regulatory rigor.
4 Future directions and recommendations
The future of surgical training within LMICs lies between the mix of hybrid educational models that balances traditional in-person and AI driven simulation platforms. This would allow dual needs for scalability and practical experience acquisition (19, 20). To ensure a sustainable future for AI integration in LMICs surgical training, it is important that stakeholders such as educators, private sectors and policy makers work in partnership to provide and fund affordable, locally sensitive context AI platforms within their region (21, 22). International collaborations and integration into existing healthcare education budgets, with cost-benefit perspective can overcome the financial constraints particularly taking into consideration the long-term investment.
AI incorporation into surgical training in LMICs would require enhances in information governance systems that aligns with ethical standards and objective validation (23, 24).
4.1 Standardization of AI-based surgical training
Because of limited resources in LMICs, healthcare centers can vary in their needs even within the same country. So, we recommend the development of centralized guidelines, shared evaluation metrics and partnerships with regional medical councils. And these guidelines should be accredited by higher healthcare authorities like ministries of health in these countries. Which will ensure training equivalency across centers. These strategies will help to standardize the surgical skills acquired within the all centers.
4.2 Data privacy and bias in AI models
Data privacy is a major concern when talking about AI models, particularly in LMICs where there are inconsistent data standards, unclear policies, fragmented data architectures, financial constraints and confidentiality breaches (25). As a response to the growing use of AI in healthcare, several universities are working on developing a secure access to AI model to protect sensitive data. For example, Johns Hopkins University has created Hopkins AI (26) which provides access to several AI models including OpenAI, Meta and Claude while protecting sensitive patient data from being leaked. Several methods can be used to anonymize data used in AI models like, replacing protected health information (PHI) with codes and avoiding the use of any identifiers on AI models. Adherence to local protective laws and regulations will be very helpful in protecting data privacy when using AI models as well. Bias in AI models poses a major threat to the fairness and effectiveness of AI-driven surgical training. These systems are only as good as the data they learn from. When AI is trained predominantly on data from high-income countries, it may fail to accurately assess skills or predict outcomes in low-resource settings. This can result in unfair evaluations, misclassification of surgeon competence and inappropriate training recommendations. Bias can stem from unbalanced datasets, lack of contextual diversity or developer assumptions. To reduce bias, AI models must be trained on inclusive, representative datasets and undergo validation across diverse geographic, cultural and clinical environments. Testing multiple models and comparing results to guidelines and literature is also crucial in avoiding bias produced by AI models.
Finally, launching pilot programs in a range of urban and rural LMIC settings is essential. These efforts should systematically evaluate how AI integration influences skill development, surgical outcomes and regulatory preparedness, generating the evidence base required for broader implementation and policy integration (27, 28).
5 Conclusion
In LMICs, surgical training and credentialing traditionally rely on informal, mentor-based systems with limited oversight and variable outcomes. This system, while accessible, often compromises patient safety and lacks standardized competency assessment. The integration of artificial intelligence offers a transformative shift, providing scalable, objective and data-driven solutions for training, evaluation and regulatory processes. AI-driven platforms enhance access to high-quality education through simulation and tele-mentoring while enabling continuous monitoring and evidence-based credentialing. Despite infrastructural and ethical challenges, hybrid models combining AI and conventional mentorship may present the most viable path forward. To ensure effective adoption, investment in digital infrastructure, governance frameworks and capacity building is essential. Ultimately, AI holds significant potential to elevate surgical standards, improve equity in care and support safer, more accountable surgical practices across resource-limited settings.
Author contributions
LD: Writing – original draft, Writing – review & editing. HM: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review & editing. DT: Writing – original draft, Writing – review & editing. SA-A: Writing – review & editing, Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization. MT: Conceptualization, Data curation, Formal analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review & editing, Writing – original draft. HH: Writing – review & editing. DK: Writing – review & editing. AG: Writing – review & editing. PT: Writing – original draft. NH: Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Awuah WA, Tan JK, Bharadwaj HR, Aderinto N, Ferreira T, Patel H, et al. Surgical mentorship in low-resource environments: opportunities and challenges, a perspective. Health Sci Rep. (2024) 7(8):e2258. doi: 10.1002/hsr2.2258
2. Konda NN, Lewis TL, Furness HN, Miller GW, Metcalfe AJ, Ellard DR, et al. Surgeon views regarding the adoption of a novel surgical innovation into clinical practice: systematic review. BJS open. (2024) 8(1):zrad141. doi: 10.1093/bjsopen/zrad141
3. Yanik E, Intes X, Kruger U, Yan P, Diller D, Van Voorst B, et al. Deep neural networks for the assessment of surgical skills: a systematic review. J Def Model Simul. (2022) 19(2):159–71. doi: 10.1177/15485129211034586
4. Yoonhee Ryder C, Mott NM, Gross CL, Anidi C, Shigut L, Bidwell SS, et al. Using artificial intelligence to gauge competency on a novel laparoscopic training system. J Surg Educ. (2024) 81(2):267–74. doi: 10.1016/j.jsurg.2023.10.007
5. Ma R, Kiyasseh D, Laca JA, Kocielnik R, Wong EY, Chu TN, et al. Artificial intelligence-based video feedback to improve novice performance on robotic suturing skills: a pilot study. J Endourol. (2023) 38(8):884–91. doi: 10.1089/end.2023.0328
6. Wilkinson E, Aruparayil N, Gnanaraj J, Brown J, Jayne D. Barriers to training in laparoscopic surgery in low- and middle-income countries: a systematic review. Trop Doct. (2021) 51(3):408–14. doi: 10.1177/0049475521998186
7. Yankunze Y, Mwachiro MM, Lando JO, Bachheta N, Mangaoang D, Bekele A, et al. Laparoscopy experience in east, central, and Southern Africa: insights from operative case volume analysis. Surg Endosc. (2024) 38(8):4415–21. doi: 10.1007/s00464-024-10960-2
8. Blazeby JM, Cousins S, Pullyblank A. Safety and transparency in surgical innovation. Br J Hosp Med. (2022) 83(4):1–3. doi: 10.12968/hmed.2022.0073
9. Niyitegeka J, Patel R. Should implementation of new health technology in low- and middle-income countries follow the same guidelines as multinational drug trials? Bull R Coll Surg Engl. (2020) 102(4):138–40. doi: 10.1308/rcsbull.2020.117
10. Strong VE, Forde KA, MacFadyen BV, Mellinger JD, Crookes PF, Sillin LF, et al. Ethical considerations regarding the implementation of new technologies and techniques in surgery. Surg Endosc. (2014) 28:2272–6. doi: 10.1007/s00464-014-3644-1
11. Varas J, Coronel BV, Villagrán I, Escalona G, Hernandez R, Schuit G, et al. Innovations in surgical training: exploring the role of artificial intelligence and large language models (LLM). Rev Col Bras Cir. (2023) 50:e20233605. doi: 10.1590/0100-6991e-20233605-en
12. Bing EG, Brown ML, Cuevas A, Sullivan R, Parham GP. User experience with low-cost virtual reality cancer surgery simulation in an African setting. JCO Glob Oncol. (2021) 7:435–42. doi: 10.1200/GO.20.00510
13. Wu J, Hines OJ. Using artificial intelligence to assess surgeon skill. JAMA Surg. (2023) 158(8):e231140. doi: 10.1001/jamasurg.2023.1140
14. Grüter AAJ, Van Lieshout AS, van Oostendorp SE, Henckens SPG, Ket JCF, Gisbertz SS, et al. Video-based tools for surgical quality assessment of technical skills in laparoscopic procedures: a systematic review. Surg Endosc. (2023) 37(6):4279–97. doi: 10.1007/s00464-023-10076-z
15. Boal MWE, Anastasiou D, Tesfai F, Ghamrawi W, Mazomenos E, Curtis N, et al. Evaluation of objective tools and artificial intelligence in robotic surgery technical skills assessment: a systematic review. Br J Surg. (2024) 111(1):3–11. doi: 10.1093/bjs/znad331
16. Kewalramani D, Loftus TJ, Mayol J, Narayan M. Artificial intelligence in surgery: a global balancing act. Br J Surg. (2024) 111(3):znae062. doi: 10.1093/bjs/znae062
17. Guo J, Li B. The application of medical artificial intelligence technology in rural areas of developing countries. Health Equity. (2018) 2(1):174–81. doi: 10.1089/heq.2018.0037
18. Wang D, Wang L, Zhang Z, Wang D, Zhu H, Gao Y, et al. “Brilliant AI Doctor” in rural China: tensions and challenges in AI-powered CDSS deployment. (2021). doi: 10.48550/arXiv.2101.01524
19. Yahanda AT, Joseph K, Bui T, Greenberg JK, Ray WZ, Ogunlade JI, et al. Current applications and future implications of artificial intelligence in spine surgery and research: a narrative review and commentary. Global Spine J. (2025) 15(2):1445–54. doi: 10.1177/21925682241290752
20. Min Z, Lai J. Innovating robot-assisted surgery through large vision models. Nat Rev Electr Eng. (2025) 2:350–63. doi: 10.1038/s44287-025-00166-6
21. Hong L, Luo M, Wang R, Lu P, Lu W, Lu L, et al. Big data in health care: applications and challenges. Data Inf Manag. (2019) 2(3):175–97. doi: 10.2478/dim-2018-0014
22. Jaleel A, Aziz R, Farid G, Bashir MZ. The impact of ChatGPT on academic integrity in medical education: a developing nation perspective. Front Educ. (2025) 10:2–7. doi: 10.3389/feduc.2025.1554444
23. Banerjee P, Hati M, Dorage R, Singh S, Jadhav V. She, the algorithm, and the invisible hand: re- imagining economic paradigms in the age of feminist AI. Int J Multidiscip Res. (2025) 7:7–15. doi: 10.36948/ijfmr.2025.v07i03.45549
24. Ifeanyichukwu A, Vaswani V, Ekmekci PE. Exploring artificial intelligence-based distribution planning and scheduling systems’ effectiveness in ensuring equitable vaccine distribution in low-and middle-income countries—witness seminar approach. Discov Artif Intell. (2025) 5(1):3–15. doi: 10.1007/s44163-025-00298-6
25. Kaushik A, Barcellona C, Mandyam NK, Tan SY, Tromp J. Challenges and opportunities for data sharing related to artificial intelligence tools in health care in low- and middle-income countries: systematic review and case study from Thailand. J Med Internet Res. (2025) 27:e58338. doi: 10.2196/58338
27. Muralidharan V, Ng MY, AlSalamah S, Pujari S, Kalra K, Singh R, et al. Global initiative on AI for health (GI-AI4H): strategic priorities advancing governance across the united nations. NPJ Digit Med. (2025) 8(1):219. doi: 10.1038/s41746-025-01618-x
Keywords: surgery, artificial intelligence, LMIC (low and middle income countries), healthcare, residency accreditation
Citation: Duy Tran LC, Metwalli H, Tien Le D, Amo-Afful S, Todry Gerges MS, Hassan Ahmed HH, Kim Quyen DT, Gamil Gad A, Tran P and Huy NT (2025) Learning new surgical techniques in low and middle income countries, approval processes, and the impact of artificial intelligence. Front. Surg. 12:1647899. doi: 10.3389/fsurg.2025.1647899
Received: 16 June 2025; Accepted: 14 July 2025;
Published: 8 August 2025.
Edited by:
Dhruva Ghosh, Christian Medical College, IndiaReviewed by:
Edwin Stephen, Sultan Qaboos University Hospital, OmanCopyright: © 2025 Duy Tran, Metwalli, Tien Le, Amo-Afful, Todry Gerges, Hassan Ahmed, Kim Quyen, Gamil Gad, Tran and Huy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nguyen Tien Huy, bmd1eWVudGllbmh1eTRAZHV5dGFuLmVkdS52bg==; Long Cong Duy Tran, dHJhbmNvbmdkdXlsb25nQGdtYWlsLmNvbQ==; bG9uZy50Y2RAdW1jLmVkdS52bg==
†These authors have contributed equally to this work
‡ORCID:
Long Cong Duy Tran
orcid.org/0000-0002-3994-4864
Helal Metwalli
orcid.org/0009-0001-9103-1034
Dat Tien Le
orcid.org/0000-0002-5623-9737
Hajer Hatim Hassan Ahmed
orcid.org/0000-0002-9211-2186
Dinh Thi Kim Quyen
orcid.org/0000-0001-7028-2881
Abdelrahman Gamil Gad
orcid.org/0000-0002-4461-3517
Phillip Tran
orcid.org/0000-0003-3329-2276
Nguyen Tien Huy
orcid.org/0000-0002-9543-9440
 Long Cong Duy Tran1,2*†,‡
Long Cong Duy Tran1,2*†,‡ Dat Tien Le
Dat Tien Le Samuel Amo-Afful
Samuel Amo-Afful Abdelrahman Gamil Gad
Abdelrahman Gamil Gad Nguyen Tien Huy
Nguyen Tien Huy