- 1Shanxi Bethune Hospital, Shanxi Academy of Medical Sciences, Tongji Shanxi Hospital, Third Hospital of Shanxi Medical University, Taiyuan, China
- 2Tongji Hospital, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
- 3Department of Orthopaedic Surgery, Shengjing Hospital of China Medical University, Shenyang, China
Objectives: This study compared the efficacy of teriparatide and bisphosphonates(BPs) in osteoporotic patients who underwent thoracolumbar spinal fusion through a comprehensive meta-analysis of published data from randomized controlled trials and other types of comparative studies.
Methods: Major online databases, including PubMed, EMBASE, Web of Science, and Cochrane Central, were searched for studies on the efficacy of teriparatide and BPs in patients treated with thoracolumbar spinal fusion. Studies that evaluated bone union conditions and other subjective or objective outcomes were included. The publication period ranged from database inception to June 13, 2025.
Results: Ultimately, 6 articles with 329 patients were included in this meta-analysis. Compared with BPs, teriparatide had advantages in terms of improving the bone union rate at both the 6-month and 1-year follow-ups and reducing the Oswestry Disability Index (ODI) and leg pain visual analogue scale (VAS) score at the 1-year follow-up. The screw loosening rate, VAS score for low back pain at the 1-year follow-up and ODI score at the 6-month follow-up were not clearly different between the teriparatide and BP groups.
Conclusion: In patients undergoing thoracolumbar spinal fusion, compared with BPs, teriparatide clearly promotes bone fusion and improves quality of life, with high safety. However, the small number of studies included in this meta-analysis (six) may have influenced the results in the forest plots.
1 Introduction
Spinal fusion surgery for terminal thoracic spine, lumbar spine and initial sacral spine yields similar outcomes compared to surgery for cervical vertebrae. These fusion surgeries, such as Posterior lumbar interbody fusion and transforaminal lumbar interbody fusion, are the most common surgical methods for lumbar degenerative diseases and spinal fractures (1). These surgeries can relieve nerve compression, thereby alleviating pain and neurological symptoms (2, 3). The final outcome of spinal fusion is a combination of bone formation and remodelling, resulting from both bone formation and resorption (4). However, lumbar degenerative diseases and spinal fractures are more common in older individuals (5, 6); as people age, they typically suffer from osteoporosis, another common disease (7, 8) that is characterized by an imbalance between osteoblasts and osteoclasts that results in a fragile bone microstructure and a low bone mineral density (BMD). Patients with osteoporosis who undergo spinal fusion surgery tend to experience more complications, such as fusion failure, cage subsidence and vertebral compressive fractures (VCFs) (8, 9). Therefore, the management of osteoporosis may improve the outcomes of spinal fusion surgery.
Antiosteoporosis drugs can be classified according to their functions, including those that inhibit bone resorption, such as bisphosphonates (BPs) and denosumab; those that promote bone anabolism, such as teriparatide; and those that influence both functions, such as romosozumab (10). Among these antiosteoporotic drugs, BPs, one of the earliest and most classical group of drugs, are recommended as the first-line medication by most researchers and physicians, who recommend that patients with osteoporosis receive BP treatment to control their decreasing BMD (11, 12). However, one previous meta-analysis suggested that although BPs can clearly reduce the rates of vertebral compression fracture, cage subsidence, and pedicle screw loosening after spinal fusion, they do not greatly increase the bone fusion rate (13). Compared with BPs, which inhibit the activity of osteoclasts, teriparatide can clearly induce the activity of osteoblasts and promote bone formation since it is a recombinant form of a human parathyroid hormone fragment (14), which presents similar efficacy in thoracolumbar spines (15). One previous meta-analysis documented the efficacy of teriparatide in improving the bone fusion rate after spinal fusion surgery (16). The difference in the clinical efficacy between BPs and teriparatide may be due to their different effects on bone metabolism; therefore, the corresponding literature should be summarized to obtain greater insights into these differences and aid in developing more efficient drugs. From 2018 to 2020, previous systematic and meta-analyses compared the efficacy of teriparatide and BPs in patients undergoing thoracolumbar spinal fusion (17–19); however, some of the meta-analyses included studies that compared one drug with a control group. In addition, several studies in this field have been published since the publication of the two meta-analyses. Therefore, performing an updated meta-analysis to compare these two drugs directly and provide information on evidence-based medicine to clinical doctors when making clinical decisions is necessary.
This study compared the efficacy of teriparatide and BPs in osteoporotic patients who underwent thoracolumbar spinal fusion by performing a comprehensive meta-analysis of published data from randomized controlled trials (RCTs) and other types of comparative studies.
2 Material and methods
2.1 Search strategy
Two independent researchers screened major online databases, including PubMed, EMBASE, Web of Science, and Cochrane Central, with a publication period ranging from database inception to June 13, 2025. The key terms used for searching the titles and abstracts were “interbody fusion”, “lumbar fusion”, “spinal fusion”, “thoracic vertebra”, “teriparatide”, “bisphosphonate”, “alendronate”, “clodronate”, “etidronate”, “ibandronate”, “minodronate”, “neridronate”, “olpadronate”, “pamidronate”, “risedronate”, “tiludronic acid”, and “zoledronic acid”; these terms were used in different combinations.
2.2 Eligibility criteria and study identification
Articles were included if they met the following criteria: (1) target population—osteoporosis patients who suffered from thoracolumbar spinal disease; (2) intervention—spinal interbody fusion, with one group using teriparatide and the other group using BPs; (3) outcomes—parameters evaluating BMD, the bone union rate and other subjective or objective outcomes; (4) type of study—although RCTs were desirable, other types of comparative studies were also accepted; and (5) language—English.
Using the inclusion criteria listed above, the two researchers independently read the titles and abstracts in the online databases. If they thought the article was eligible, they read the full text. Any disagreements were resolved by discussion with a third investigator.
2.3 Data extraction and risk of bias assessment
After identifying the included studies, the two researchers extracted the following information from the eligible articles: first author names, publication year, the number of patients allocated to each group, the number of male patients in each group, the mean body mass index (BMI) of each group, the mean age of each group, major diagnosis, surgery type, the intervention method used in each group, and treatment and follow-up durations. The quality of the RCTs was assessed using the Cochrane risk of bias tool (20), whereas the Newcastle–Ottawa Scale (NOS) was used to assess the quality of other types of comparative studies (21).
2.5 Statistical analysis
RevMan 5.3 software was used to conduct the statistical analyses. The odds ratio (OR) and 95% confidence interval (CI) were computed as summary statistics for the dichotomous variables, and pooled summary statistics were calculated with the use of a random effects model. The mean difference (MD) and 95% CI were computed as summary statistics for continuous variables, and pooled summary statistics were calculated with the use of a fixed effects model if the heterogeneity was not significant; otherwise, a random effects model was applied. P < 0.05 was regarded as statistically significant. Statistical heterogeneity was quantified using chi-square (χ2) and I2 tests, and heterogeneity was considered to exist based on P < 0.05 or I2 > 50%. Getdata (version 2.22) was used if the data were presented only as figures in the article instead of as detailed information.
3 Results
3.1 Literature search
After eliminating duplicate articles, 357 studies identified from the electronic databases using the search strategy listed above were included. Of these studies, 285 were from PubMed, 15 were from EMBASE, 33 were from Web of Science, and 14 were from Cochrane Central. A total of 334 studies were then excluded since they were not RCTs or comparative cohort trials (CCTs) or were not published in English. After the full texts were read, 15 studies were found to have data that could not be included in the meta-analysis. Two studies involved a mixed intervention of teriparatide and BPs. Ultimately, 6 articles were included in this meta-analysis (22–27). Figure 1 presents the process of screening and identifying eligible studies.
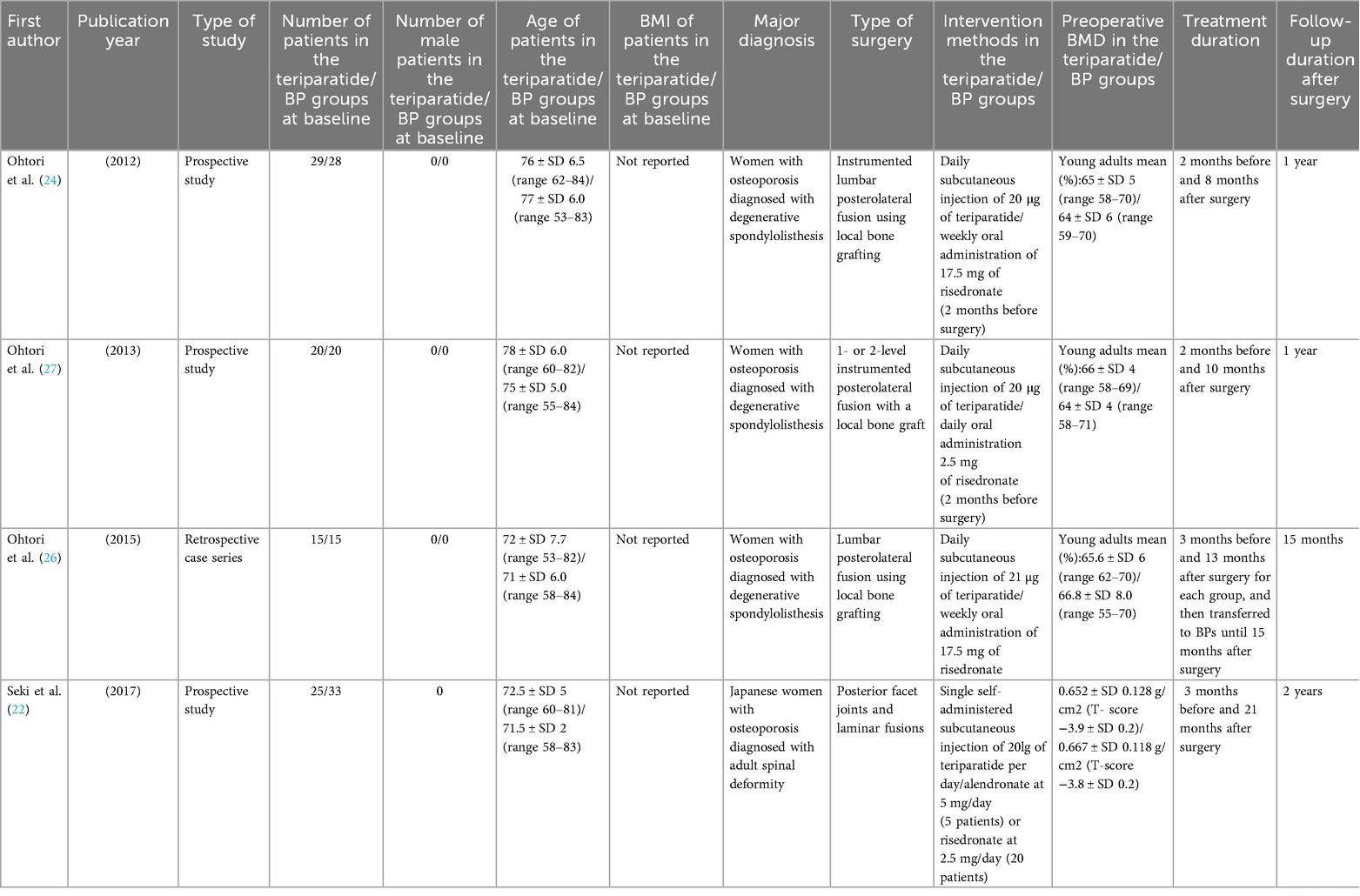
3.2 Study characteristics
The main characteristics of the 6 included studies are summarized in Table 1. Only one study was an RCT. The two studies published after 2020 were conducted in China, while the other four studies were conducted in Japan. Participants in the teriparatide group of one study were treated with teriparatide for an average of 13 months and then with BPs until 15 months after surgery; however, some parameters were evaluated 12 months after surgery; therefore, the RCT was included in this study, and a meta-analysis was conducted for the outcomes that were measured at the 12-month follow-up (26). The publication period ranged from 2012 to 2022. A total of 329 patients were analysed in this work. One study included 7 male patients, and only two studies provided detailed information on BMI. The two most recent studies used zoledronic acid, whereas the other four studies used oral BPs. The duration of the intervention ranged from 1 to 2 years.
3.3 Study quality
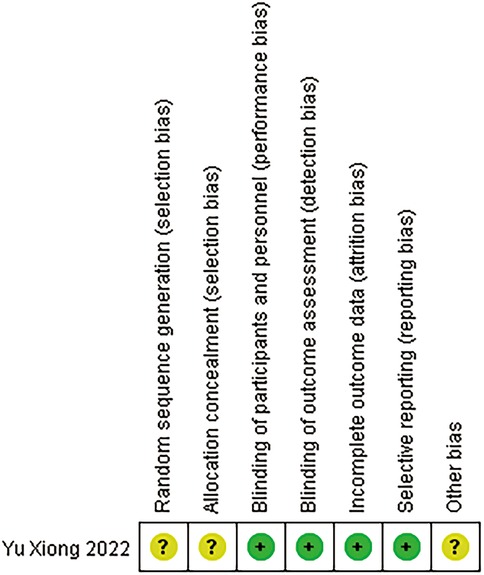
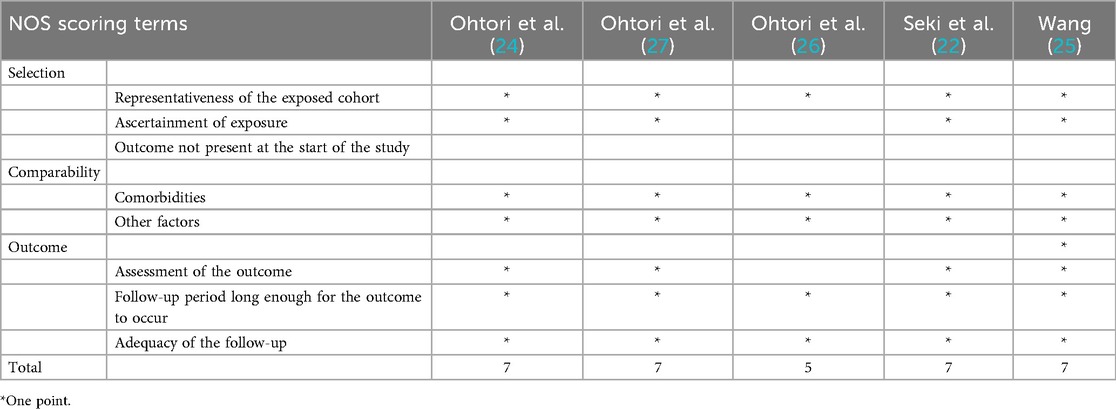
The six included studies were of relatively high quality (Figure 2). The RCT was considered to have a low risk of bias in terms of the blinding methods, the completeness of the outcome data and selective reporting. The CCTs were of good quality, with 4 of the 5 CCTs receiving a score of 7 on the NOS and the last study receiving a score of 5 (Table 2).
According to Egger et al. (28), an assessment of publication bias comparing fewer than 10 studies is not reliable. Therefore, a funnel plot was not constructed to evaluate publication bias.
3.4 Bone union condition
Figure 3 shows the results for the bone union rate evaluated by computed tomography (CT) (the number of facet joints) at the 6-month and 1-year follow-ups, the bone union rate assessed by radiology (the number of segments) at the 1-year follow-up, and the bone union period. The forest plots suggest that, compared with the BP group, the teriparatide group had an obviously shorter bone union period and a higher bone union rate at both the 6-month and 1-year follow-ups. A random-effects model was applied to generate the forest plot for bone union period, since this is a continuous variable and the associated heterogeneity was high (I2 > 50%), while the forest plots for bone union rate were obtained with a random-effects model since it was a dichotomous variable.
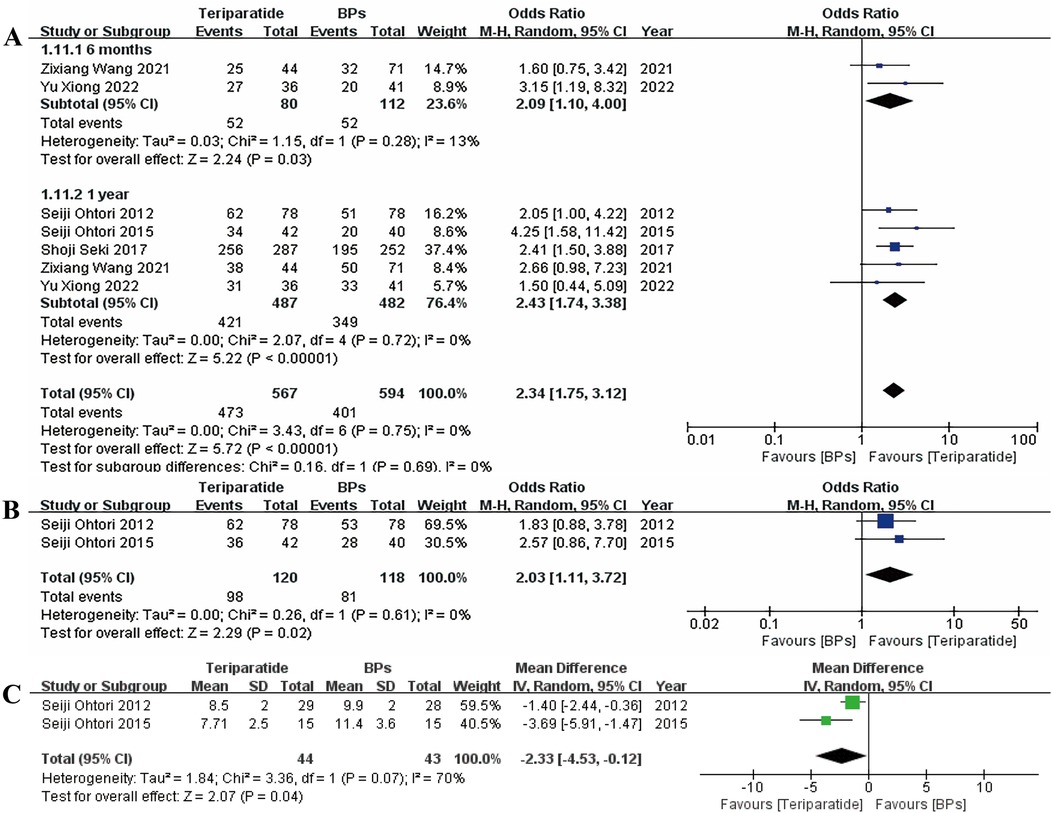
Figure 3. Forest plots of A the bone union rate evaluated by CT at the 6-month and 1-year follow-ups, B the bone union rate evaluated by radiology at the 1-year follow-up, and C the bone union period.
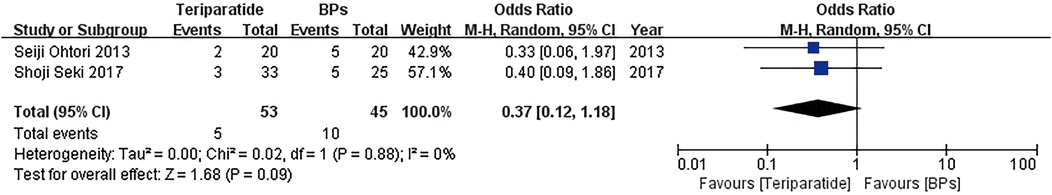
3.5 Screw loosening rate
Figure 4 presents forest plots of the screw loosening rate at the 1-year follow-up, and the results revealed no significant difference between teriparatide and BPs. The forest plot was obtained with a random-effects model since this was a dichotomous variable.
3.6 Patient-reported outcomes
Figure 5 presents the forest plots of the visual analogue scale (VAS) scores for low back pain and leg pain at the 1-year follow-up and the Oswestry Disability Index (ODI) scores at the 6-month and 1-year follow-ups, respectively; the results suggested no significant differences in the ODI score at the 6-month follow-up or the VAS score at the 1-year follow-up between the two groups. However, teriparatide could greatly lower the ODI score at the 1-year follow-up compared with BPs. A fixed-effects model was used to generate the forest plots of the VAS score and ODI since they were continuous variables and the associated heterogeneity was low (I2 < 50%).
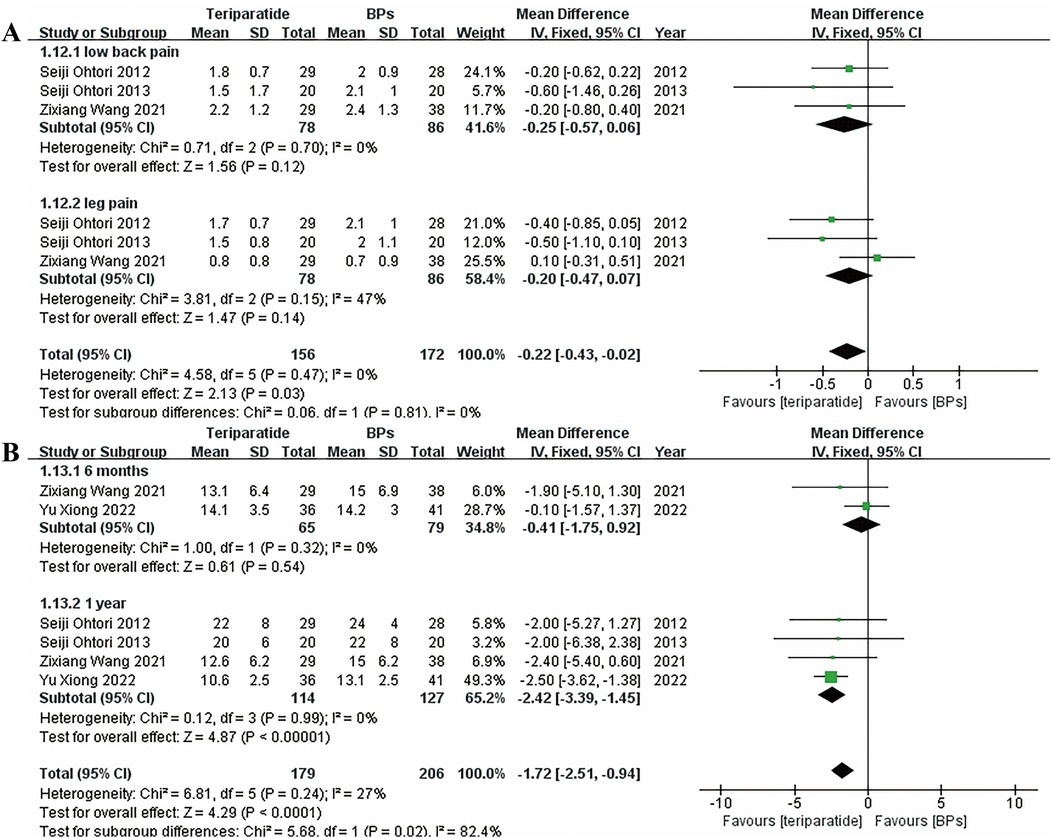
Figure 5. Forest plots of (A) the VAS score for low back pain and leg pain at the 1-year follow-up, and (B) the ODI score at the 6-month and 1-year follow-ups.
3.7 Sensitivity analysis
Although most comparisons presented low heterogeneity, the heterogeneity of the forest plot for the bone union period was high; nevertheless, sensitivity or subgroup analyses could not be conducted since only two studies were included in this comparison. In the comparison of the VAS score of leg pain, the heterogeneity was moderately high (I2 = 47%); to reduce the heterogeneity, the study conducted by Zixiang Wang et al. was omitted since, unlike the other two studies, which used risedronate, they used zoledronic acid. The results noticeably changed with the removal of this study (Figure 6), indicating that the teriparatide group had a significantly lower VAS score than the BPs group.
4 Discussion
This meta-analysis summarized previously published results regarding two major areas: fusion conditions and patients' subjective feelings. Overall, the results of the forest plots presented above suggest that, compared with BPs, teriparatide has advantages in terms of improving the bone union rate at both the 6-month and 1-year follow-ups and reducing the ODI and leg pain VAS score at the 1-year follow-up. The screw loosening rate, VAS score for low back pain at the 1-year follow-up and ODI score at the 6-month follow-up were not clearly different between the teriparatide and BP groups.
Three outcomes for bone union conditions were evaluated in the meta-analysis: the bone union period, the screw loosening rate and the bone union rate. The bone union period is a new parameter that has not been compared in previous meta-analyses. Our forest plot suggested that, compared with BPs, teriparatide clearly shortened the bone union period and therefore promoted bone union, although the heterogeneity was slightly high in the comparison. The bone union rate, as evaluated by CT and radiology, also supported this result. In addition, in a study conducted by Seiji Ohtori et al. in (24) the stability rate of the teriparatide group was higher than that of the BP group, which was similar to the results of another study conducted by Seiji Ohtori et al. in (26); however, because the follow-up period of the study in 2015 covered the BP treatment period in the teriparatide group, a meta-analysis could not be conducted. No included study reported detailed information about the risks for compression fracture, VCFs and cage subsidence, which may be advantages of BPs according to previous studies (13, 17). However, although BPs have been reported to be effective in reducing screw loosening and our results also suggest no significant difference in this parameter between teriparatide and BP treatments, the trend of our forest plot is quite obvious for the teriparatide group, which had a lower loosening rate, perhaps because the small sample size affected the results. Shoji Seki et al. also suggested better outcomes for VCFs in the teriparatide group than in the BP group, but no other included studies reported this outcome; thus, a meta-analysis was unable to be conducted. Additionally, teriparatide has been shown to exhibit similar efficacy in thoracic and lumbar spine (15). However, no previous study has demonstrated the effect of BPs on the two locations. Further studies are needed to explore these topics.
Two patient-reported outcomes were included in the meta-analysis: VAS and ODI scores. The VAS is a common tool for evaluating pain, while the ODI is used to assess self-care ability in daily life; higher scores on these two tools indicate worse outcomes (29, 30). Compared with one previous study (17), we compared these parameters at each follow-up point instead of mixing the results at different follow-up points. Although the results suggested that teriparatide could reduce the ODI and leg pain VAS score only at the 1-year follow-up, the trend of the forest plots for teriparatide was clearly a reduction in the VAS score for low back pain at the 1-year follow-up and the ODI score at the 6-month follow-up; once again, the small sample size may have affected the results. In addition, Yu Xiong et al. reported no significant difference in the ODI score at the 2-year follow-up between the teriparatide and BP groups; however, Shoji Seki et al. obtained significant differences in the ODI score at the 2-year follow-up. The different diagnosis and scoring methods, as well as the BP type may have caused this difference, and further studies are needed to explore this issue. In addition, Shoji Seki et al. reported the Scoliosis Research Society questionnaire-22 score, a parameter that also evaluates the pain domain, which also suggested better outcomes for the teriparatide group than for the BP group. A meta-analysis could not be conducted since no other included studies reported this parameter.
The two most recent included studies provided detailed information on BMD (7, 23), which can reflect the direct therapeutic efficacy of the two drugs. Both studies suggested a better BMD outcome for the teriparatide group than for the BP group. Moreover, they both suggested limited efficacy for BPs in increasing BMD after spinal fusion surgery. Nevertheless, the two studies did not assess the same location; therefore, their data could not be subjected to a meta-analysis, and the number of included patients may also be small. Wang et al. also presented a change in the expression of bone turnover markers, including P1NP and β-CTX, suggesting that the levels of these two markers were increased in the teriparatide group and decreased in the BP group; it is widely accepted that the decrease in β-CTX represents a relief in bone resorption, while the increase in P1NP is a sign of active bone anabolism (31, 32). Our results are consistent with those of previous studies, reflecting the effects of each drug. Five of the six included studies reported associated adverse effects of the two drugs, except the study conducted by Xiong et al., and none of the studies reported drug-related adverse effects in either group, which suggested the safety of the two drugs. However, in women older than 65 years, a previous study suggested a relatively greater risk of adverse effects in the BP group than in the control group (33); the number of articles regarding the adverse effects of teriparatide was low, which may suggest an advantage in the safety of teriparatide over BPs.
Compared with the previous meta-analysis, this work included more studies and compared more parameters to compare the efficacy of teriparatide and BPs in patients who underwent thoracolumbar spinal fusion and obtained different results (19). Nevertheless, limitations are unavoidable. First, the major limitation of this study is the small number of included studies, despite the inclusion of CCTs to increase the number of included trials. Furthermore, the RCT included here presented no clear difference in the forest plots when conducting sensitivity analysis, as did elimination of the study that scored a 5 on NOS. This small number of studies may have decreased the reliability of the forest plots. Additionally, meta-regression analysis and funnel plots could not be used to identify the sources of heterogeneity and bias due to the small number of studies. Moreover, the small sample size may obscure potentially scarce but serious adverse effects for the two drugs. Second, the intervention methods, surgical techniques, drugs doses and BP types differed across the included studies, which may have caused heterogeneity and impaired the reliability of the forest plots. Third, the efficacy of the two drugs could not be compared because we did not have results for direct BMD parameters. Fourth, previous studies have suggested that farnesyl pyrophosphate synthase gene polymorphisms are a key mechanism in the response to BPs, which is absent in eastern Asians (34, 35), indicating that racial differences may influence the antiosteoporotic effect; therefore, racial bias may have affected the results since only eastern Asians were included in the current study. Finally, selection and publication bias may be present since only English language articles were included.
5 Conclusions
This meta-analysis revealed that, compared with BPs, teriparatide clearly promotes bone fusion and improves the quality of life of patients who underwent thoracolumbar spinal fusion, with high safety. However, a small number of studies (six) was included in this meta-analysis, which may have influenced the results depicted in the forest plots. Further work involving larger sample sizes should be conducted to confirm the results and provide stronger evidence in this field.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Author contributions
XJ: Conceptualization, Writing – review & editing, Resources. JD: Writing – review & editing. GH: Writing – review & editing, Investigation. JW: Writing – original draft, Writing – review & editing. ZX: Resources, Writing – review & editing, Funding acquisition.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by grants from project of Health Commission of Shanxi Province (No. 2020011).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Chan CW, Peng P. Failed back surgery syndrome. Pain Med. (2011) 12:577–606. doi: 10.1111/j.1526-4637.2011.01089.x
2. Liu XY, Qiu GX, Weng XS, Yu B, Wang YP. What is the optimum fusion technique for adult spondylolisthesis-PLIF or PLF or PLIF plus PLF? A meta-analysis from 17 comparative studies. Spine (Phila Pa 1976). (2014) 39:1887–98. doi: 10.1097/BRS.0000000000000549
3. Schnake KJ, Rappert D, Storzer B, Schreyer S, Hilber F, Mehren C. [Lumbar fusion-indications and techniques]. Orthopade. (2019) 48:50–8. doi: 10.1007/s00132-018-03670-w
4. Hirsch BP, Unnanuntana A, Cunningham ME, Lane JM. The effect of therapies for osteoporosis on spine fusion: a systematic review. Spine J. (2013) 13:190–9. doi: 10.1016/j.spinee.2012.03.035
5. Boskey AL, Imbert L. Bone quality changes associated with aging and disease: a review. Ann N Y Acad Sci. (2017) 1410:93–106. doi: 10.1111/nyas.13572
6. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990–2010: a systematic analysis for the global burden of disease study 2010. Lancet. (2012) 380:2163–96. doi: 10.1016/S0140-6736(12)61729-2
7. Wang QY, Ding N, Dong YH, Wen ZX, Chen R, Liu SY, et al. Pharmacological treatment of osteoporosis in elderly people: a systematic review and meta-analysis. Gerontology. (2021) 67:639–49. doi: 10.1159/000514449
8. Hu S, Li J, Liu L, Dai R, Sheng Z, Wu XP, et al. Micro/nanostructures and mechanical properties of trabecular bone in ovariectomized rats. Int J Endocrinol. (2015) 2015:252503. doi: 10.1155/2015/252503
9. Liu P, Zhou B, Chen F, Dai Z, Kang Y. Effect of trabecular microstructure of spinous process on spinal fusion and clinical outcomes after posterior lumbar interbody fusion: bone surface/total volume as independent favorable indicator for fusion success. World Neurosurg. (2020) 136:e204–13. doi: 10.1016/j.wneu.2019.12.115
10. Yuki E, Takaaki N, Toshitaka Y, Tomonori K, Masafumi K, Okamura G, et al. Impact of baseline PINP on the BMD increase with romosozumab, teriparatide, and denosumab in treatment-naïve primary osteoporosis: a retrospective cohort study. Bone. (2025) 201. doi: 10.1016/j.bone.2025.117627
11. Kanis JA, Cooper C, Rizzoli R, Reginster JY. Executive summary of the European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Calcif Tissue Int. (2019) 104:235–8. doi: 10.1007/s00223-018-00512-x
12. Murad MH, Drake MT, Mullan RJ, Mauck KF, Stuart LM, Lane MA, et al. Clinical review. Comparative effectiveness of drug treatments to prevent fragility fractures: a systematic review and network meta-analysis. J Clin Endocrinol Metab. (2012) 97:1871–80. doi: 10.1210/jc.2011-3060
13. Mei J, Song X, Guan X, Wu D, Wang J, Liu Q. Postoperative bisphosphonate do not significantly alter the fusion rate after lumbar spinal fusion: a meta-analysis. J Orthop Surg Res. (2021) 16:284. doi: 10.1186/s13018-021-02444-z
14. Lindsay R, Krege JH, Marin F, Jin L, Stepan JJ. Teriparatide for osteoporosis: importance of the full course. Osteoporos Int. (2016) 27:2395–410. doi: 10.1007/s00198-016-3534-6
15. Mikula AL, St Jeor JD, Naylor RM, Bernatz JT, Patel NP, Fogelson JL, et al. Teriparatide treatment increases Hounsfield units in the thoracic spine, lumbar spine, Sacrum, and ilium out of proportion to the cervical spine. Clin Spine Surg. (2021) 34(7):E370–6. doi: 10.1097/BSD.0000000000001203
16. Fatima N, Massaad E, Hadzipasic M, Shankar GM, Shin JH. Assessment of the efficacy of teriparatide treatment for osteoporosis on lumbar fusion surgery outcomes: a systematic review and meta-analysis. Neurosurg Rev. (2021) 44:1357–70. doi: 10.1007/s10143-020-01359-3
17. Buerba RA, Sharma A, Ziino C, Arzeno A, Ajiboye RM. Bisphosphonate and teriparatide use in thoracolumbar spinal fusion: a systematic review and meta-analysis of comparative studies. Spine (Phila Pa 1976). (2018) 43:E1014–23. doi: 10.1097/BRS.0000000000002608
18. Cheng SH, Kuo YJ, Chen C, Kang YN. Effects of teriparatide and bisphosphonate on spinal fusion procedure: a systematic review and network meta-analysis. PLoS One. (2020) 15:e0237566. doi: 10.1371/journal.pone.0237566
19. Tsai SHL, Chien RS, Lichter K, Alharthy R, Alvi MA, Goyal A, et al. Teriparatide and bisphosphonate use in osteoporotic spinal fusion patients: a systematic review and meta-analysis. Arch Osteoporos. (2020) 15:158. doi: 10.1007/s11657-020-00738-z
20. Shuster JJ. Review: Cochrane handbook for systematic reviews for interventions, version 5.1.0, published 3/2011. In: Higgins JPT, Green S, editors. Research Synthesis Methods. Vol. 2. Hoboken, NJ: Research Synthesis Methods (2011) p. 126–30.
21. Wells G, Shea B, O’Connell D, Peterson J, Welch V. The Newcastle-Ottawa scale (NOS) for assessing the quality of case-control studies in meta-analyses. Eur J Epidemiol. (2011) 25:603–5.
22. Seki S, Hirano N, Kawaguchi Y, Nakano M, Yasuda T, Suzuki K, et al. Teriparatide versus low-dose bisphosphonates before and after surgery for adult spinal deformity in female Japanese patients with osteoporosis. Eur Spine J. (2017) 26:2121–7. doi: 10.1007/s00586-017-4959-0
23. Xiong Y, Li L, Liu P, Zhou B, Kang Y, Wang G. Effect of teriparatide versus zoledronate on posterior lumbar interbody fusion in postmenopausal women with osteoporosis. World Neurosurg. (2022) 167:e1310–6. doi: 10.1016/j.wneu.2022.09.021
24. Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Teriparatide accelerates lumbar posterolateral fusion in women with postmenopausal osteoporosis: prospective study. Spine (Phila Pa 1976). (2012) 37:E1464–8. doi: 10.1097/BRS.0b013e31826ca2a8
25. Wang Z, Zhuang C, Chen W, Li Z, Li J, Lin H, et al. The effect of daily teriparatide versus one-time annually zoledronic acid administration after transforaminal lumbar interbody fusion in osteoporotic patients. Clin Interv Aging. (2021) 16:1789–99. doi: 10.2147/CIA.S333207
26. Ohtori S, Orita S, Yamauchi K, Eguchi Y, Ochiai N, Kuniyoshi K, et al. More than 6 months of teriparatide treatment was more effective for bone union than shorter treatment following lumbar posterolateral fusion surgery. Asian Spine J. (2015) 9:573–80. doi: 10.4184/asj.2015.9.4.573
27. Ohtori S, Inoue G, Orita S, Yamauchi K, Eguchi Y, Ochiai N, et al. Comparison of teriparatide and bisphosphonate treatment to reduce pedicle screw loosening after lumbar spinal fusion surgery in postmenopausal women with osteoporosis from a bone quality perspective. Spine (Phila Pa 1976). (2013) 38:E487–92. doi: 10.1097/BRS.0b013e31828826dd
28. Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. Br Med J. (1997) 315:629–34. doi: 10.1136/bmj.315.7109.629
29. Fairbank JC, Couper J, Davies JB, O'Brien JP. The oswestry low back pain disability questionnaire. Physiotherapy. (1980) 66:271–3.6450426
30. Tesler MD, Savedra MC, Holzemer WL, Wilkie DJ, Ward JA, Paul SM. The word-graphic rating scale as a measure of children’s and adolescents’ pain intensity. Res Nurs Health. (1991) 14:361–71. doi: 10.1002/nur.4770140507
31. Eastell R, Mitlak BH, Wang Y, Hu M, Fitzpatrick LA, Black DM. Bone turnover markers to explain changes in lumbar spine BMD with abaloparatide and teriparatide: results from ACTIVE. Osteoporos Int. (2019) 30:667–73. doi: 10.1007/s00198-018-04819-1
32. Liang BC, Shi ZY, Wang B, Wu P, Kong LC, Yao JL, et al. Intravenous zoledronic acid 5 mg on bone turnover markers and bone mineral density in east China subjects with newly diagnosed osteoporosis: a 24-month clinical study. Orthop Surg. (2017) 9:103–9. doi: 10.1111/os.12307
33. Fan Q, Wang J. The efficacy and safety of bisphosphonates for osteoporosis in women older than 65 years: a meta-analysis. Curr Pharm Des. (2020) 26:4022–30. doi: 10.2174/1381612826666200423092602
34. Olmos JM, Zarrabeitia MT, Hernández JL, Sañudo C, González-Macías J, Riancho JA. Common allelic variants of the farnesyl diphosphate synthase gene influence the response of osteoporotic women to bisphosphonates. Pharmacogenomics J. (2012) 12(3):227–32. doi: 10.1038/tpj.2010.88
Keywords: teriparatide, bisphosphonate, thoracolumbar spinal fusion, meta-analysis, osteoporosis
Citation: Ji X, Duan J, He G, Wang J and Xing Z (2025) Comparing the efficacy of teriparatide and bisphosphonates in osteoporotic patients undergoing thoracolumbar spinal fusion: a meta-analysis. Front. Surg. 12:1656134. doi: 10.3389/fsurg.2025.1656134
Received: 29 June 2025; Accepted: 6 October 2025;
Published: 21 October 2025.
Edited by:
Abdellah El Maghraoui, Mohammed V University, MoroccoReviewed by:
Zenghui Zhao, First Affiliated Hospital of Chongqing Medical University, ChinaPengguo Gou, Shanxi Provincial People’s Hospital Affiliated to Shanxi Medical University, China
Copyright: © 2025 Ji, Duan, He, Wang and Xing. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Zejun Xing, MTg3MzUxMzA5NjVAMTYzLmNvbQ==
†These authors have contributed equally to this work
 Xinghua Ji1,2,†
Xinghua Ji1,2,† Junjie Wang
Junjie Wang Zejun Xing
Zejun Xing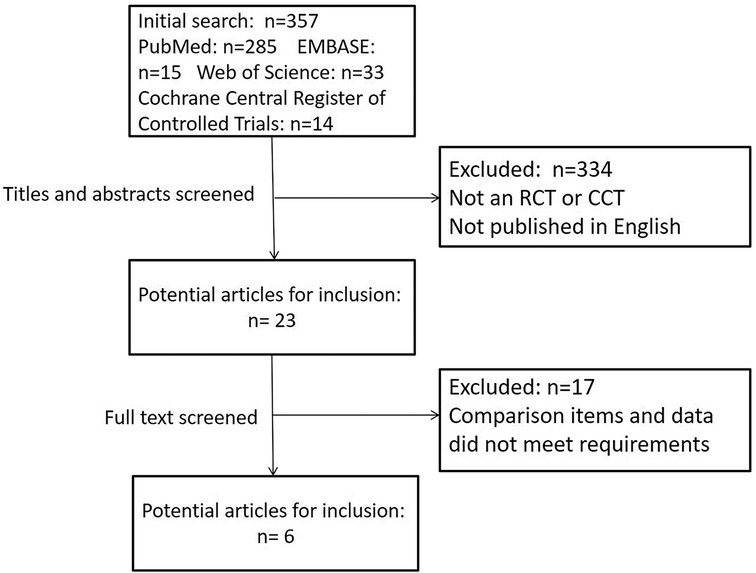
![Forest plot comparing the effects of Teriparatide versus Bisphosphonates (BPs) on low back pain and leg pain across three studies from 2012 to 2021. Mean differences with 95% confidence intervals are shown. Heterogeneity and overall effect tests are included, displaying significant results favoring Teriparatide for leg pain, with a total mean difference of -0.34 [-0.57, -0.10]. Squares represent individual study results, and diamonds illustrate pooled estimates.](https://www.frontiersin.org/files/Articles/1656134/fsurg-12-1656134-HTML/image_m/fsurg-12-1656134-g006.jpg)