- 1Department of Obstetrics, Shijiazhuang Obstetrics and Gynecology Hospital, Shijiazhuang, Hebei, China
- 2Department of Neonatal Surgery, Hebei Children’s Hospital, Shijiazhuang, Hebei, China
Objective: This study aims to evaluate the predictive value of neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) independently and in combination for surgical site infection (SSI) after emergency cesarean section (CS).
Method: This retrospective case-control study was conducted at the Maternity Medical Centre in China, a large tertiary teaching medical centre, between January 2019 and February 2022. A total of 627 patients with emergency CS were enrolled, and cases (post-SSI) and controls (without post-SSI) were matched 1:2. Various demographic, clinical and obstetric characteristics were collected. Laboratory values were measured on preoperative and postoperative days 1, 3. Univariate and multivariate logistic regression analyses were conducted to identify the influencing factors. The predictive values of NLR and PLR independently and in combination for SSI were evaluated using receiver operating characteristics (ROC) analysis.
Result: In the univariate analysis, the BMI before delivery, preoperative NLR and PLR, and postoperative day 1 NLR and PLR et al. were significantly different between the two groups (P < 0.05). In multivariate analysis, BMI before delivery > 28.89 kg/m2, preoperative NLR > 9.89 and PLR > 177.99 appeared to be independent predictors of SSI after emergency CS. Combined indices of BMI before delivery, NLR and PLR were significantly more predictive of SSI after emergency CS than independent indices (AUC 0.85, P < 0.001, 95% CI 0.757–0.912, sensitivity 79.1%, and specificity 88.5%).
Conlusion: The combined index of BMI before delivery, preoperative NLR and PLR may be a simple, sensitive, inexpensive, versatile, and rapid test for predicting SSI after emergency CS. Of course, further prospective research and external verification will be more scientific and also our future work focus.
1 Introduction
Cesarean section (CS) is one of the most common obstetric procedures worldwide, and the number of CS has increased over the past decade (1). Compared with vaginal delivery, CS is associated with a 5–20 times higher risk of postpartum infections, ranging from endometritis to urinary tract and wound infections (2). Surgical site infection (SSI) following CS is a common complication and a major cause of morbidity and mortality, affecting the recovery process and increasing both hospitalisation and medical costs (3, 4). The incidence of SSI after CS varies between 3% and 30% (5, 6). For this reason, it is important to predict and prevent the development of SSI after CS as early as possible. Several observational studies have reported that emergent CS, multiple gestation, volume of blood loss, operative technique, duration of surgery, and maternal obesity are common risk factors for SSI (7–10). The risk of SSI after emergency CS was approximately 20% higher than that after elective surgery (7).
It is know that neutrophils, monocytes, and platelets have important roles in normal wound healing. There has been increasing evidence that the hematological indicators neutrophil-to-lymphocyte ratio (NLR) and platelet-to-lymphocyte ratio (PLR) may be used as markers of systemic inflammation, reflecting inflammatory status and activity in a variety of diseases such as infectious diseases, metabolic syndrome, lung diseases, malignant tumours and cardiovascular diseases (11–15). Furthermore, some other studies have preliminarily shown that NLR and PLR may play an increasingly important role in obstetrics and may be effective markers for predicting postpartum infection, early abortion, threatened abortion, pre-eclampsia and hyperemesis gravidarum (11, 12, 16–18).
In recently studies, the role of NLR and PLR in predicting SSI after CS was examined, and NLR was found as a potential marker (19). Additionally, the PLR has been reported to be an independent predictor of reduced survival and has a negative prognostic value in gynaecological diseases and hepatobiliary malignancies (20). Previous studies have tentatively confirmed the independent predictive value of NLR and PLR after CS infection (16). However, the independent predictive value and combined predictive value of NLR and PLR for SSI after emergency CS remains unclear. Therefore, the aim of this study was to evaluate the predictive value of NLR and PLR in SSI after emergency CS, independently and in combination, to aid in their early prediction.
2 Materials and methods
2.1 Study design and participants
This retrospective case-control study was conducted at the Shijiazhuang Obstetrics and Gynecology Hospital in Hebei, China, between January 2019 and February 2022. Our hospital is one of the largest maternity hospitals in Hebei Province with approximately 30,000 deliveries per year. This study was approved by the Institutional Review Board of Shijiazhuang Obstetrics and Gynecology Hospital (approval number 20230040). Informed consent was waived by the same ethics committee that approved the study.
Six hundred and twenty-seven pregnant women who underwent emergency CS and were followed up at our institution at one month with a maternal postnatal examination were considered eligible for the study. Cases were defined as patients undergoing emergency CS who experienced an SSI within 30 days of the procedure; controls were patients undergoing emergency CS who did not experience an SSI within 30 days of the procedure. Cases (with SSI) were matched to controls (without SSI) on a 1:2 basis.
Inclusion criteria were as follows: (1) adult patients aged ≥ 22y; (2) patients who underwent energency CS between January 2019 and February 2022; (3) patients in the case group with a positive wound swab indicating infection within 30 days of surgery; (4) patients in the control group without a postive wound swab; (5) patients in the control and case groups were of similar age and received CS on the same day. The following groups were excluded from the study: (1) patients undergoing elective CS; (2) patients with chronic systemic diseases that may alter the preoperative complete blood count, such as systemic lupus erythematosus, nephropathy, renal or hepatic dysfunction, rheumatoid arthritis; (3) pregnancies with known chromosomal abnormalities, congenital malformations, eclampsia, or hypertensive disorders; (4) patients with missing data, known maternal infection, recent use of corticosteroids, various hematological conditions, tuberculosis or malignant tumour disease; (5) patients who died either before or on the same day as the blood test were excluded from the analysis.
SSI was defined as an infection occurring within 30 days of a postoperative procedure involving the skin, subcutaneous tissue, soft tissue, or any other part of the body (21). The diagnostic criteria for SSI were in assordance with relevant guidelines (22): (1) patients with body temperature higher than 38℃; (2) the percentage of neutrophils was higher than 70%, and the white blood cell count was less than 4.0 × 109/L or higher than 10.0 × 109/L; (3) the pathogenic bacteria were cultured in incision secretions.
2.2 Data collection of variables
Data were extracted from Hospital In-Patient Enquiry database (HIPE) for the period 2019–2022. The HIPE database is a computerized system designed to capture the administrative, demographic and clinical data on all inpatient discharges in the Shijiazhuang Obstetrics and Gynecology Hospital. The medical records including maternal age, place of residence, body mass index (BMI) before delivery, parity, previous cesareans section, gestational weeks, diabetes, operative time, type of anesthesia, and blood loss. BMI was calculated from pre-pregnancy weight and height. In addition, complete blood count (CBC) results routinely obtained on day 1 and 3 postoperatively were included. The following blood count variables were analyzed: hemoglobin (HGB), red blood cells (RBC), white blood cells (WBC), albumin (ALB), C-reactive protein (CRP), neutrophils, lymphocytes, platelets. The NLR and PLR were calculated by dividing the total neutrophil count and the total platelet count by the total lymphocyte count, respectively.
It is worth noting that all blood samples were collected by drawing 5 ml of blood from the antecubital vein without the use of anticoagulants by professionally trained phlebotomists. To control for circadian rhythms, all samples were routinely collected during the same time period (6:00 am to 8:00 am) on the preoperative day and on days 1 and 3 postoperatively. The samples were transported to the biochemistry laboratory within one hour for testing, which was performed in our hospital's hematology laboratory using the same Beckman Coulter Gen-S automated analyzer (Brea, CA, United States) for all samples.
2.3 Surgical procedures
All emergency CS were performed by consultants and senior obstetric residents. At our institution, prophylactic antibiotics are routinely administered for emergency CS. Prophylactic antibiotics were administered with a single dose of 1 g cefazoline 30–60 min before starting the skin incision. As standard for all emergency CSs, the anesthetist administers general or local anesthesia, depending on the patient. During surgery, both the abdomen and vagina were sterilized with 10% povidone-iodine disinfectant immediately after spinal anaesthesia. After delivery, the abdominal fascia was closed with 0 monofilament continuous sutures. After the incision sites were washed with saline, a 4–0 monofilament dermostitch suture was performed. There were no reported cases of subcutaneous drains among the samples analyzed. After surgery, the incision sites were covered with sterile dressings, which were removed on postoperative day 3.
2.4 Statistical analysis
Data were analyzed using SPSS 21.0 (IBM, Armonk, NY). Continuous variables with a normal distribution are presented as mean ± SD (standard deviation). The Shapiro–Wilk test was used to assess the normality of continuous variables. For nonnormally distributed continuouus variables, the Mann–Whitney U-test was used. Categorical variables are presented as counts and percentages, using chi-squared or Fisher's exact test when appropriate. Besides, univariate and multivariate logisitcs regression analyses was utilized to identify identify influencing factors for SSI after emergency CS. Variables with significant differences (P < 0.05) were entered into a multiple logistic regression model to assess whether there was an independent association between hematological indices and ISS of emergency CS. In all cases, a significance threshold of P < 0.05 was used.
3 Results
3.1 Patient characteristics
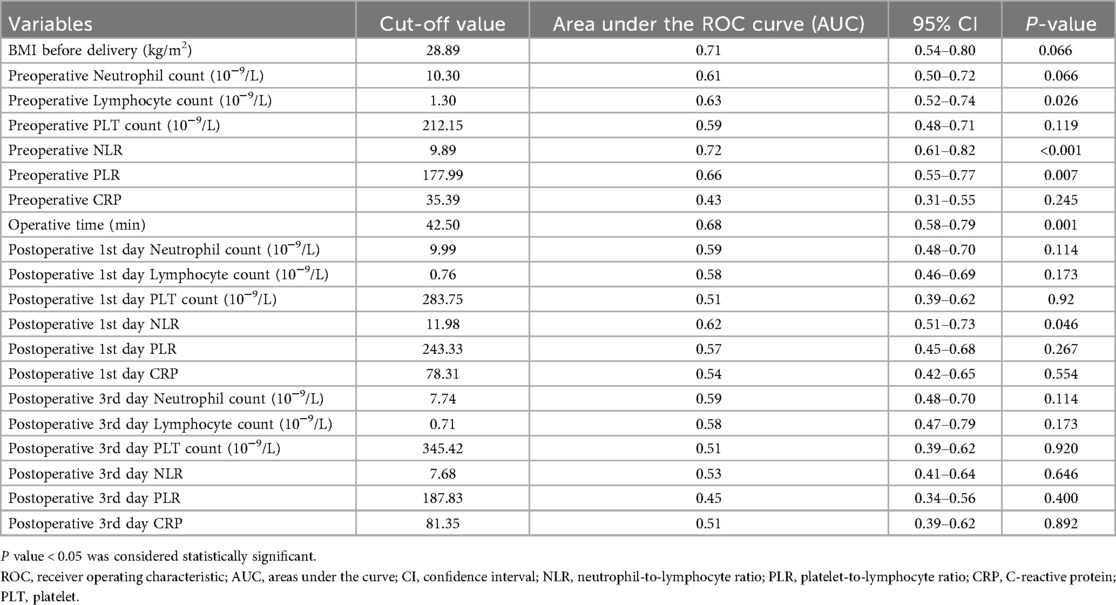
During a 3-year study, a total of 627 pregnant women who underwent emergency CS surgery were included in the study (mean age 27.6 ± 3.2 years). There were 209 patients diagnosed with postoperative SSI (group 1) and 418 patients without postoperative SSI (group 2). The BMI before delivery, operative time and preoperative and postoperative day 1 and 3 neutrophil count, lymphocyte count, PLT count, NLR, PLR, CRP were determined by ROC curve analysis (Table 1).
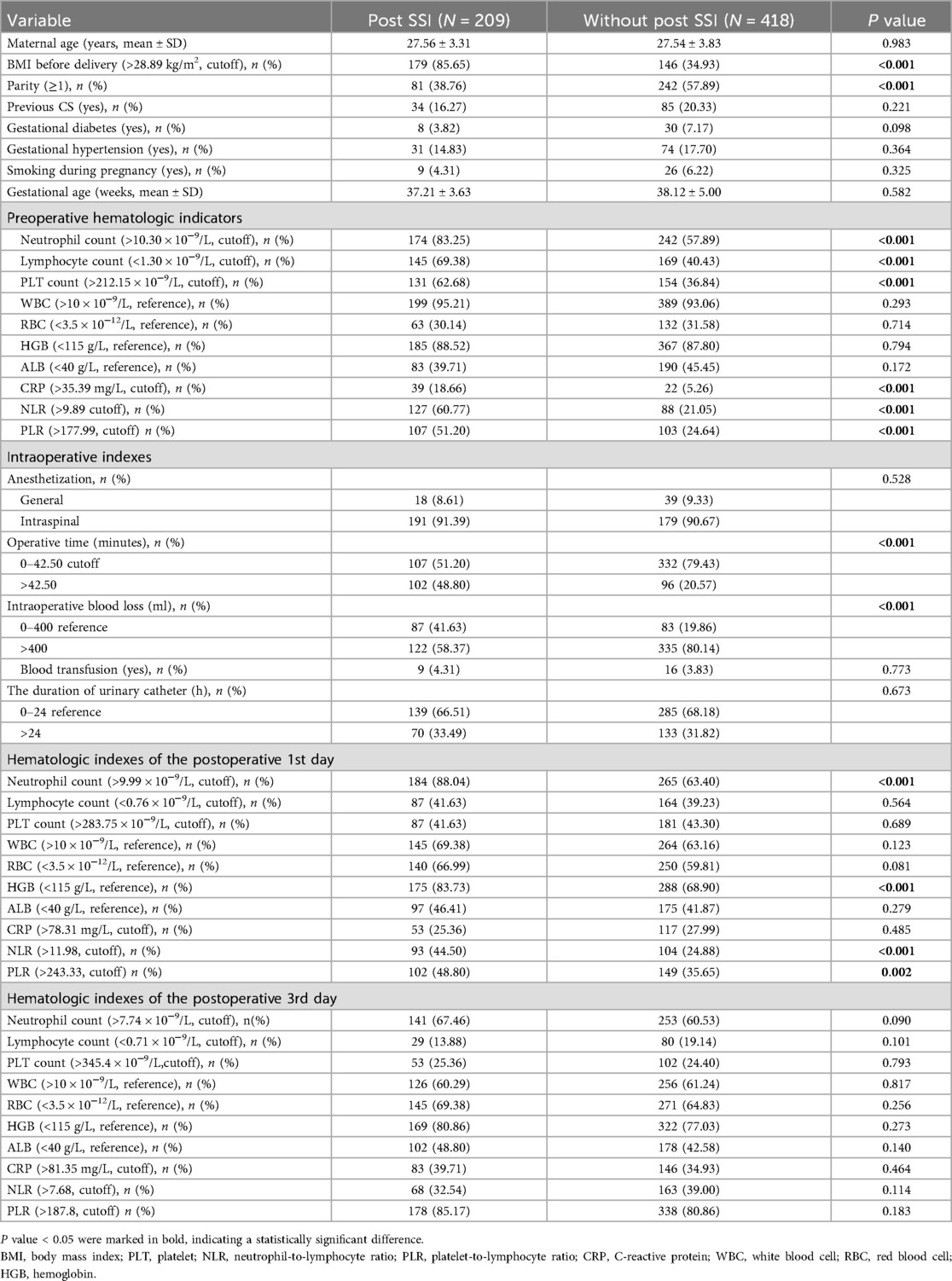
In the univariate analysis, the BMI before delivery, parity, preoperative neutrophil count > 10.30 × 10−9/L, lymphocyte count < 1.30 × 10−9/L, PLT count > 212.15 × 10−9/L, NLR > 9.89 × 10−9/L, PLR > 177.99 × 10−9/L, CRP > 35.39 mg/L, operative time > 42.50 min, intraoperative blood loss > 400 ml, 1st day postoperative neutrophil count > 9.99 × 10−9/L, HGB < 115 g/L, NLR > 11.98 (P < 0.001), and 1st day postoperative PLR >243.33 (P = 0.002) of patients in group 1 were significantly different from those in group 2 (Table 2). The multivariate logistic regression analysis model included the significant associated factors shown in Table 1. The final multivariate analysis results indicated that preoperative NLR > 9.89 (OR 4.39, 95% CI 1.79–12.57, P = 0.001), preoperative PLR > 177.99 (OR 3.55, 95% CI 0.81–15.53, P = 0.033), BMI before delivery > 28.89 kg/m2 (OR 8.65, 95% CI 3.24–14.36, P = 0.048) were independent risk factors for SSI after emergency CS (Table 3).
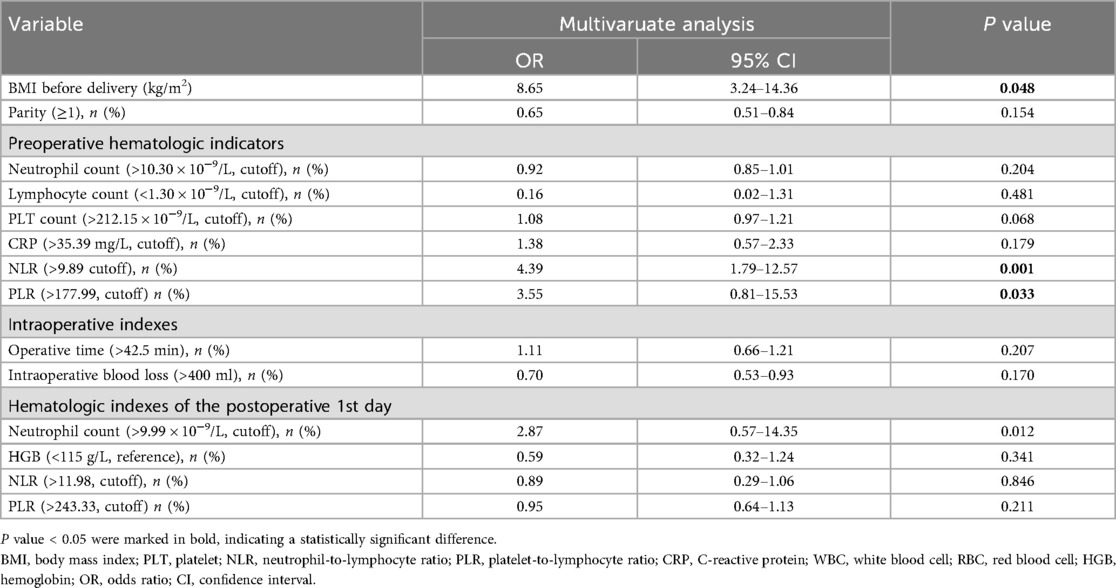
Table 3. Mutivariable logistic regression analyses of variables associated with SSI after emergency CS.
3.2 Indepentent indices
In this study, BMI before delivery > 28.89 kg/m2, peroperative NLR > 9.89 and PLR > 177.99 were significantly increased in the postoperative SSI group compared to the no SSI group (P < 0.001). ROC curve analysis was performed independently for the prediction of SSI in emergency CS. For BMI before delivery > 28.89 kg/m2, AUC was 0.714, sensitivity was 0.817, and specificity was 0.649%. For peroperative NLR > 9.89, AUC was 0.718, sensitivity was 0.605 and specificity was 0.789. For PLR > 177.99, AUC was 0.658, sensitivity was 0.612 and specificity was 0.754 (Figure 1).
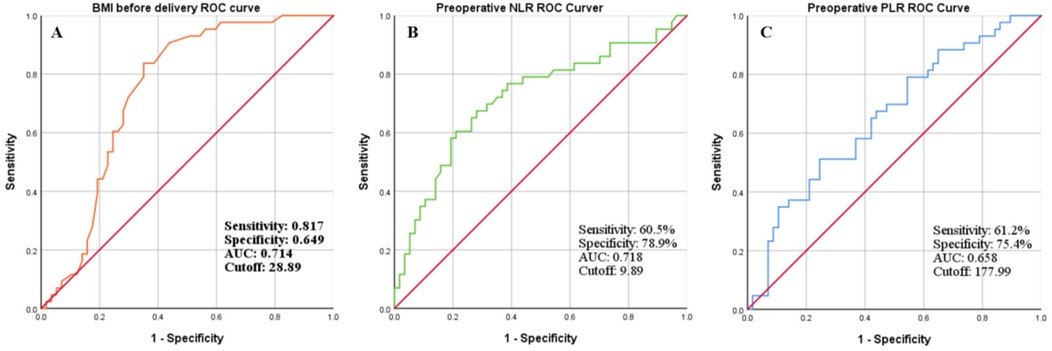
Figure 1. ROC curve analysis was performed to determine the cut-off value of (A) BMI before delivery; (B) preoperative NLR; and (C) preoperative PLR and to calculate the sensitivity, specificity and AUC for independently predicting SSI after emergency CS.
3.3 Combined indices
According to the combined predictive probabilities by logistic regression analysis, ROC curves were used to evaluate the predictive values of the combination of BMI before delivery > 28.89 kg/m2, preoperative NLR > 9.89 and PLR > 177.99 in the SSI group compared with with no SSI. For BMI before delivery > 28.89 kg/m2 combined with preoperative NLR > 9.89, the AUC was 0.804, the sensitivity was 0.719 and the specificity was 0.743. For BMI before delivery > 28.89 kg/m2 combined with preoperative PLR > 177.99, AUC was 0.761, sensitivity was 0.667, specificity was 0.816. For preoperative NLR > 9.89 combined with PLR > 177.99, AUC was 0.729, sensitivity was 0.789, specificity was 0.605. For BMI before delivery > 28.89 kg/m2 combined with preoperative NLR > 9.89 and PLR > 177.99, the AUC was 0.854, sensitivity was 0.791, specificity was 88.47, better than individually independent or pariwise combined index of BMI before delivery, preoperative NLR and PLR (Figure 2).
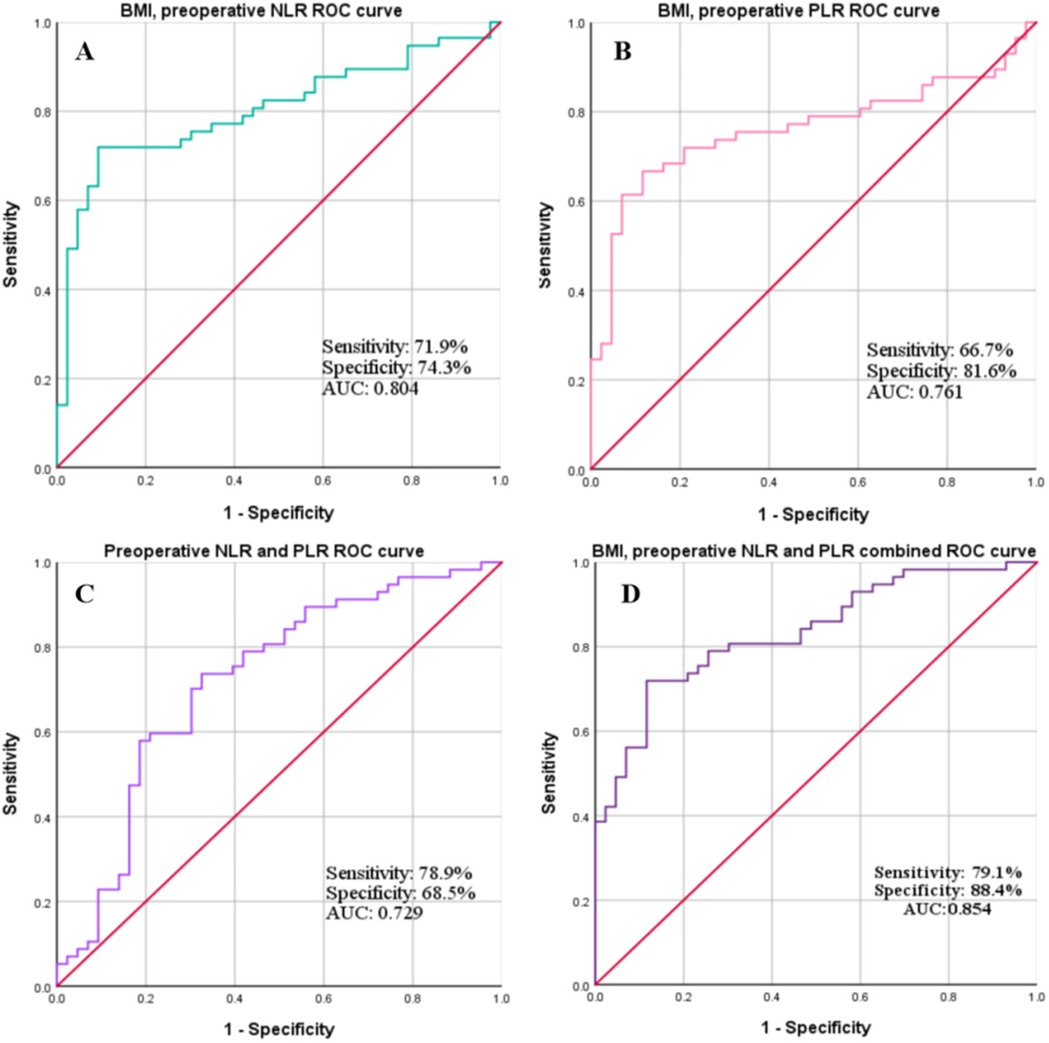
Figure 2. ROC curve analysis was performed to calculate the sensitivity, specificity and AUC for predicting SSI after emergency CS using a combination of 2 or more indics (A), BMI before delivery combined with preoperative NLR; (B), BMI before delivery combined with preoperative PLR; (C), preoperative NLR combined with preoperative PLR; (D), BMI before delivery combined with preoperative NLR and PLR.
4 Discussion
In recent years, many studies have found that NLR and PLR may be associated with the further development of infection after CS (16, 23). To our knowledge, this is the first study to use the simple, inexpensive laboratory indicators in combination to predict postoperative SSI in patients with emergency CS. In our study, the results of multiple logistic regression analysis showed that preoperative NLR > 9.89 (OR 4.39, 95% CI 1.79–12.57, P = 0.001), preoperative PLR > 177.99 (OR 3.55, 95% CI 0.81–15.53, P = 0.033), BMI before delivery > 28.89 kg/m2 (OR 8.65, 95% CI 3.24–14.36, P = 0.048) were independent predictors of SSI after emergency CS. In addition, the combined predictive value of preoperative BMI, NLR and PLR (AUC was 0.854, sensitivity was 0.791, specificity was 0.884) was significantly better than that of independent or pariwise combined indices.
Emergency CS is a common procedure worldwide, and with increasing rates of CS, the occurrence of SSI following emergency CS is a major clinical and public health concern (7, 9). Much international literature has identified several risk factors that predispose an individual to develop SSI following CS in general, including obesity and increased BMI, increased age, existing comorbidities, prolonged operative time, intraoperative blood loss and the complexity of an emergency CS (8, 24, 25). In our study, BMI > 28.89 kg/m2 is a significant risk factor for developing SSI after emergency CS, which is consistent with previous research demonstrating a negative impact on the risk of postoperative infection (24). Previous studies have shown that impaired immune response, larger wound area and poor perfusion of prophylactic antibiotics in obese individuals may account for this increased risk. Another possible explanation is that BMI plays a role in emergency CS due to the potential dysfunction that excess adipose tissue can cause to the immune system and a decrease in periorperative tissue oxygenation (26). Therefore, increased monitoring and control of antenatal BMI in this group may effectively mitigate the potential development of postoperative SSI.
Especially in the past 20 years, the relationship between these hematologic markers and many diseases has been examined. SSI is a clinical condition in which healing is impaired as a result of an infection, blood cells will have an important effect on the development of SSI, both in terms of inflammation and wound healing (27). However, the number of studies examining the relationship between preoperative and postoperative inflammatory hematologic markers and SSI is limited. Some studies have shown that NLR and PLR were the most commonly used inflammatory markers among CBC parameters and were reliable markers of systemic inflammation and may reflect both pro- and anti-inflammatory states (12, 15). These markers have been studied as novel predictors of several diseases, including cardiovascular disease, sepsis, irritable bowel syndrome, inflammatory bowel disease, rheumatic diseases, pulmonary diseases, malignancy, and others (12, 28, 29). In obstetrics, some scholars still have dispute over the predictive value of NLR and PLR for SSI after CS. Some scholars believe that NLR and PLR may not be effective and useful parameters to predict SSI after CS (30). However, a larger number of scholars believe that NLR and PLR are independent markers of postpartum infection, pre-eclampsia, preterm labour in pregnant women and many other gynecological conditions (18, 23). Rotem et al. (16). showed that both NLR and PLR during the first 24 postoperative hours may have a predictive value in the early detection of post-CS infection. However, the number of studies on the combination of NLR and PLR to predict SSI after emergency CS is limited.
SSI is one of the most common infections in CS, which is mostly superficial and usually occurs 4–7 days after surgery (29). Early prediction of SSI after emergency CS is a major challenge to control the disease and improve surgical outcomes. Currently, no combination screening test for the prediction of postoperative SSI has gained widespread acceptance in clinical practice. It is of utmost importance to find simple predictive parameters before the development of classic clinical signs and symptoms of SSI after emergency CS (31, 32). To reduce the rate of postoperative SSI, our medical center has adopted routine measures such as perioperative antibiotic use, chlorhexidine skin preparation, same level of surgery, same surgical strategy and no sutures. In our study, multivariate logistic regression analysis showed that preoperative NLR > 9.89, preoperative PLR > 177.99 and BMI > 28.89 kg/m2 were independent risk factors for SSI after emergency CS. However, ROC curve analysis shows that the predictive value of the three indices independently (BMI, AUC was 0.714, sensitivity was 0.817 and specificity was 0.649; NLR, AUC was 0.718, sensitivity was 0.605 and specificity was 0.789; PLR, AUC was 0.658, sensitivity 0.612, specificity was 0.754) and pairwise combination (BMI combined with NLR, AUC was 0.804, sensitivity was 0.719 and specificity was 0.743; BMI combined with PLR, AUC was 0.761, sensitivity was 0.667, specificity was 0.816; NLR combined with PLR, AUC was 0.729, sensitivity was 0.789, specificity was 0.605) is significantly lower than the predictive value of the three indices combined (BMI combined with NLR and PLR, AUC was 0.854, sensitivity was 0.791, specificity was 0.885). Therefore, we believe that our findings have clinical implications; patients with BMI before delivery > 28.89 kg/m2, preoperative NLR > 9.89 and preoperative PLR > 177.99 may benefit from closer monitoring. Early detection and treatment of postoperative infections may also have economic implications.
Our study has several limitations. First, this is a retrospective and single-center study, which has its inherent flaws. Second, this study could not investigate the detailed pathogenesis of elevated NLR and PLR levels in emergency CS patients with SSI. Additionally, other laboratory test results of certain clinical and inflammatory markers, such as interleukin (IL)-6, IL-10, erythrocyte sedimentation rate, and TNF-α, were not included in the analysis because they were not measured in all patients. Finally, due to the short hospital stay of CS patients in our center, only whole blood samples were taken before surgery and 1, 3 days after surgery were used for analysis. Therefore, the results of this study should be verified in further prospective and multicenter studies.
5 Conclusions
In conclusion, the results of the present study have demonstrated that patients with emergency CS with BMI > 28.89 kg/m2, NLR > 9.89 and PLR > 177.99 should receive targeted intervention and close monitoring to prevent SSI. The combined index of BMI, preoperative NLR and PLR is a simple, sensitive, inexpensive, versatile and rapid test for predicting SSI in patients undergoing emergency CS. Controlling BMI, reducing preoperative NLR and PLR is beneficial for the prevention of SSI. In addition, further studies are warranted to elucidate the risk factors for SSI after CS to provide evidence for the management of CS.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Institutional Review Board of Shijiazhuang Obstetrics and Gynecology Hospital. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XY: Funding acquisition, Investigation, Methodology, Writing – original draft. WY: Data curation, Formal analysis, Writing – review & editing. QH: Data curation, Methodology, Resources, Visualization, Writing – review & editing. XZ: Formal analysis, Software, Validation, Writing – review & editing. QL: Conceptualization, Formal analysis, Resources, Writing – review & editing. HL: Supervision, Validation, Visualization, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This study was funded by the Shijiazhuang Science and Technology Research and Development Programme Project (20242126).
Acknowledgments
We would to express our thanks to Shijiazhuang Obstetrics and Gynecology Hospital, research and technology interchange for all the contributions in conducting this study and we also would like to extend our deepest gratitude to governmental for providing permission to conduct this study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Huang HP, Zhao WJ, Pu J, He F. Prophylactic negative pressure wound therapy for surgical site infection in obese women undergoing cesarean section: an evidence synthesis with trial sequential analysis. J Matern Fetal Neonatal Med. (2021) 34:2498–505. doi: 10.1080/14767058.2019.1668924
2. Igwemadu GT, Eleje GU, Eno EE, Akunaeziri UA, Afolabi FA, Alao AI, et al. Single-dose versus multiple-dose antibiotics prophylaxis for preventing caesarean section postpartum infections: a randomized controlled trial. Womens Health. (2022) 18:17455057221101071. doi: 10.1177/17455057221101071
3. Farret TCF, Dallé J, da Silva Monteiro V, Riche CVW, Antonello VS. Risk factors for surgical site infection following cesarean section in a Brazilian Women’s hospital: a case-control study. Braz J Infect Dis. (2015) 19:113–7. doi: 10.1016/j.bjid.2014.09.009
4. Getaneh T, Negesse A, Dessie G. Prevalence of surgical site infection and its associated factors after cesarean section in Ethiopia: systematic review and meta-analysis. BMC Pregnancy Childbirth. (2020) 20:311. doi: 10.1186/s12884-020-03005-8
5. Shiferaw WS, Aynalem YA, Akalu TY, Petrucka PM. Surgical site infection and its associated factors in Ethiopia: a systematic review and meta-analysis. BMC Surg. (2020) 20:107. doi: 10.1186/s12893-020-00764-1
6. Li L, Cui H. The risk factors and care measures of surgical site infection after cesarean section in China: a retrospective analysis. BMC Surg. (2021) 21:248. doi: 10.1186/s12893-021-01154-x
7. Saeed KB, Corcoran P, Greene RA. Incisional surgical site infection following cesarean section: a national retrospective cohort study. Eur J Obstet Gynecol Reprod Biol. (2019) 240:256–60. doi: 10.1016/j.ejogrb.2019.07.020
8. Saeed KB, Corcoran P, O'Riordan M, Greene RA. Risk factors for surgical site infection after cesarean delivery: a case-control study. Am J Infect Control. (2021) 47:164–9. doi: 10.1016/j.ajic.2018.07.023
9. Ousey K, Blackburn J, Stephenson J, Southern T. Incidence and risk factors for surgical site infection following emergency cesarean section: a retrospective case-control study. Adv Skin Wound Care. (2021) 34:482–7. doi: 10.1097/01.ASW.0000767368.20398.14
10. Salim R, Braverman M, Teitler N, Berkovic I, Suliman A, Shalev E. Risk factors for infection following cesarean delivery: an interventional study. J Matern Fetal Neonatal Med. (2012) 25:2708–12. doi: 10.3109/14767058.2012.705394
11. Aslan MM, Yeler MT, Bıyık İ, Yuvacı HU, Cevrioğlu AS, Özden S. Hematological parameters to predict the severity of hyperemesis gravidarum and ketonuria. Rev Bras Ginecol Obstet. (2022) 44:458–66. doi: 10.1055/s-0042-1743101
12. Bai YY, Xi Y, Yin BB, Zhang JH, Chen F, Zhu B. Reference intervals of systemic immune-inflammation index, neutrophil-to-lymphocyte ratio, lymphocyte-to-monocyte ratio, and platelet-to-lymphocyte ratio during normal pregnancy in China. Eur Rev Med Pharmacol Sci. (2023) 27:1033–44. doi: 10.26355/eurrev_202302_31199
13. Haybar H, Pezeshki SMS, Saki N. Evaluation of complete blood count parameters in cardiovascular diseases: an early indicator of prognosis? Exp Mol Pathol. (2019) 110:104267. doi: 10.1016/j.yexmp.2019.104267
14. Huang Z, Fu Z, Huang W, Huang K. Prognostic value of neutrophil-to-lymphocyte ratio in sepsis: a meta-analysis. Am J Emerg Med. (2020) 38(3):641–7. doi: 10.1016/j.ajem.2019.10.023
15. Langley BO, Guedry SE, Goldenberg JZ, Hanes DA, Beardsley JA, Ryan JJ. Inflammatory bowel disease and neutrophil-lymphocyte ratio: a systematic scoping review. J Clin Med. (2021) 10:4219. doi: 10.3390/jcm10184219
16. Rotem R, Erenberg M, Rottenstreich M, Segal D, Yohay Z, Idan I, et al. Early prediction of post cesarean section infection using simple hematological biomarkers: a case control study. Eur J Obstet Gynecol Reprod Biol. (2020) 245:84–8. doi: 10.1016/j.ejogrb.2019.12.009
17. Cui HX, Chen C, Jung YM, Guo ZY, Dong CY, LEE SM, et al. Neutrophil-to-lymphocyte ratio (NLR) as a predictive index for liver and coagulation dysfunction in preeclampsia patients. BMC Pregnancy Childbirth. (2023) 23(1):4. doi: 10.1186/s12884-022-05335-1
18. Gezer C, Ekin A, Ertas IE, Ozeren M, Solmaz U, Mat E, et al. High first-trimester neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios are indicators for early diagnosis of preeclampsia. Ginekol Pol. (2016) 87:431–5. doi: 10.5603/GP.2016.0021
19. Forget P, Dinant V, De Kock M. Is the neutrophil-to-lymphocyte ratio more correlated than C-reactive protein with postoperative complications after major abdominal surgery? PeerJ. (2015) 3:e713. doi: 10.7717/peerj.713
20. Wang D, Yang JX, Cao DY, Wan XR, Feng FZ, Huang HF, et al. Preoperative neutrophil-lymphocyte and platelet-lymphocyte ratios as independent predictors of cervical stromal involvement in surgically treated endometrioid adenocarcinoma. Onco Targets Ther. (2013) 6:211–6. doi: 10.2147/OTT.S41711
21. Alfouzan W, Al Fadhli M, Abdo N, Alali W, Dhar R. Surgical site infection following cesarean section in a general hospital in Kuwait: trends and risk factors. Epidemiol Infect. (2019) 147:e287. doi: 10.1017/S0950268819001675
22. Ban KA, Minei JP, Laronga C, Harbrecht BG, Jensen EH, Fry DE, et al. American college of surgeons and surgical infection society: surgical site infection guidelines, 2016 update. J Am Coll Surg. (2017) 224:59–74. doi: 10.1016/j.jamcollsurg.2016.10.029
23. Morisaki N, Piedvache A, Nagata C, Michikawa T, Morokuma S, Kato K, et al. Maternal blood count parameters of chronic inflammation by gestational age and their associations with risk of preterm delivery in the Japan environment and Children’s study. Sci Rep. (2021) 11:15522. doi: 10.1038/s41598-021-93101-2
24. Ohr SO, Ball J, Teber E, Ferguson JK, Petherbridge R, Giles M. Effectiveness of HealthTracker for post-caesarean section surgical site infection surveillance: an intervention study. Nurs Health Sci. (2024) 26(1):e13108. doi: 10.1111/nhs.13108
25. Wloch C, Wilson J, Lamagni T, Harrington P, Charlett A, Sheridan E. Risk factors for surgical site infection following caesarean section in England: results from a multicentre cohort study. BJOG. (2012) 119:1324–33. doi: 10.1111/j.1471-0528.2012.03452.x
26. Kabon B, Nagele A, Reddy D, Eagon C, Fleshman JW, Sessler DI, et al. Obesity decreases perioperative tissue oxygenation. Anesthesiology. (2004) 100:274–80. doi: 10.1097/00000542-200402000-00015
27. Baum CL, Arpey CJ. Normal cutaneous wound healing: clinical correlation with cellular and molecular events. Dermatol Surg. (2005) 31:674–86. doi: 10.1097/00042728-200506000-00011
28. Gasparyan AY, Ayvazyan L, Mukanova U, Yessirkepov M, Kitas GD. The platelet-to-lymphocyte ratio as an inflammatory marker in rheumatic diseases. Ann Lab Med. (2019) 39:345–57. doi: 10.3343/alm.2019.39.4.345
29. Güçlü M, Ağan AF. Relationship of peripheral blood neutrophil to lymphocyte ratio and irritable bowel syndrome. Turk J Med Sc. (2017) 47:1067–71. doi: 10.3906/sag-1509-44
30. Aktoz F, Tercan C, Cigdem B, Vurgun E. Preoperative and postoperative complete blood cell counts and prediction of surgical site infection after cesarean delivery: a retrospective case-control study. Wound Manag Prev. (2022) 68:19–23. doi: 10.25270/wmp.2022.9.1923
31. Kawakita T, Landy HJ. Surgical site infections after cesarean delivery: epidemiology, prevention and treatment. Matern Health Neonatol Perinatol. (2017) 3:12. doi: 10.1186/s40748-017-0051-3
Keywords: emergency cesarean section, surgical site infection, neutrophil-to-lymphocyte, platelet-to-lymphocyte, predictive value
Citation: Yang X, Yang W, He Q, Zhou X, Liu Q and Li H (2025) Combined predictive values of neutrophil-lymphocyte ratio and platelet-lymphocyte ratio for surgical site infection after emergency cesarean section: a retrospective case-control study. Front. Surg. 12:1670583. doi: 10.3389/fsurg.2025.1670583
Received: 21 July 2025; Accepted: 28 August 2025;
Published: 16 September 2025.
Edited by:
Anna Franca Cavaliere, Agostino Gemelli University Polyclinic (IRCCS), ItalyReviewed by:
Federica Perelli, Azienda Ospedaliera Universitaria Meyer IRCCS—Firenze, ItalyFatih Aktoz, Hacettepe University, Türkiye
Copyright: © 2025 Yang, Yang, He, Zhou, Liu and Li. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Xuemei Yang, bGp5YWl5eG1fMjAwNEAxNjMuY29t
 Xuemei Yang
Xuemei Yang Weina Yang1
Weina Yang1