- Department of Hepatobiliary and Pancreas Surgery, The First Affiliated Hospital of Xi'an JiaoTong University, Xian, China
Objective: To collect and analyse the hospital complication status of hospitalised patients with pancreatic disease in a tertiary hospital in western China and to explore the influencing factors, providing a foundation for further research.
Methods: A retrospective study design was adopted. Electronic medical records of pancreatic surgery patients hospitalised at the First Affiliated Hospital of Xi'an JiaoTong University from March 1, 2024, to July 31, 2024, were retrospectively reviewed. Data on demographic characteristics, NRS2002 scores, diagnoses, laboratory results, surgical methods, and complications were collected. SPSS software was used for univariate and multivariate analyses.
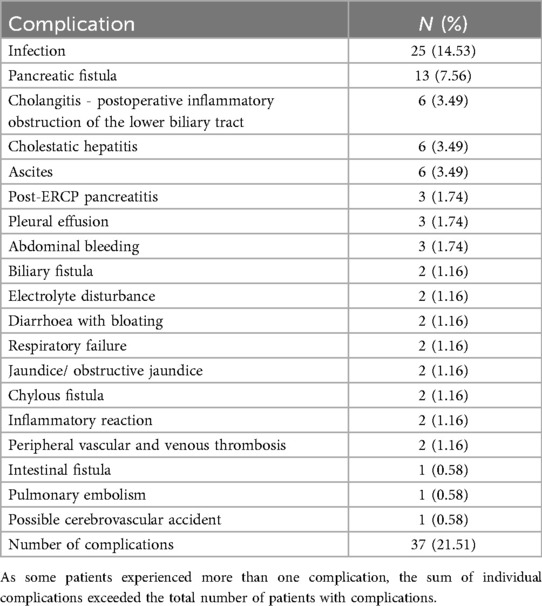
Results: In total, 172 patients, with a mean age of 60.21 ± 10.94 years, were included. Hospital complications occurred in 21.51% of pancreatic disease patients. The three most common complications were infection (14.53%), pancreatic fistula (7.56%), and cholangitis (3.49%). Univariate analysis revealed that disease diagnosis category (χ² = 8.342, P = 0.015), postoperative red blood cell (RBC) count (t = −2.552, P = 0.012), and postoperative haemoglobin concentration (Hb, g/L) (t = −2.393, P = 0.018) were risk factors for complications. Multivariate analysis confirmed that a high NRS2002 score was an independent risk factor (OR = 4.20; 95% CI: 1.017–17.368; P = 0.047).
Conclusion: The hospital complication rate in pancreatic disease patients was 21.51%, with infection, pancreatic fistula, and cholangitis being the most common complications. Low postoperative RBC counts, low postoperative Hb concentrations, and high preoperative NRS2002 scores were significant risk factors. These findings underscore the potential clinical importance of integrated perioperative nutritional support and anaemia management in improving surgical outcomes for pancreatic tumour patients, warranting further investigations in larger prospective studies.
1 Introduction
Pancreatic neoplasms are highly malignant and have shown a slowly increasing incidence since 2000. Global cancer statistics indicate that approximately 490,000 individuals were diagnosed with pancreatic neoplasms in 2020, with 460,000 deaths worldwide (1). In China, the National Cancer Center estimated 76,030 new cases and 68,222 deaths in 2024 (2).
Managing pancreatic disease typically involves comprehensive treatment centred on surgical resection (3). Surgery remains the cornerstone of curative treatment; however, postoperative complications frequently occur, adversely affecting patient recovery, survival, and health care costs. Approximately 50% of hospitalised pancreatic disease patients experience hospital complications (4). A study by Weinberg et al. revealed that the median (IQR) hospital cost in US dollars was 31.6% greater for patients who experienced complications than for those who experienced no complications [40,717.8 (27,358.0–59,834.3) vs. 30,946.9 (23,910.8–46,828.1)] (5).
While previous studies have identified various risk factors, there is a paucity of data comprehensively evaluating the role of dynamic perioperative laboratory values (e.g., immediate postoperative haemoglobin levels) alongside validated nutritional screening tools (such as NRS2002) in specific regional populations, such as those in western China.
A precise understanding of these modifiable risk factors is crucial for developing targeted preventive strategies. Therefore, this study investigated postoperative complication status and influencing factors in pancreatic disease patients at a tertiary hospital in western China.
2 Materials and methods
2.1 Study design
The study adopted a retrospective study design.
2.2 Study population
Electronic medical records of hospitalised patients in the Department of Pancreatic Surgery at the First Affiliated Hospital of Xi'an JiaoTong University from March 1, 2024, to July 31, 2024, were retrospectively reviewed. Inclusion criteria: Adult patients aged ≥18 years. Exclusion criteria: Patients who voluntarily discharged or transferred during hospitalisation or those whose electronic records were incomplete.
2.3 Sample size calculation
A convenience sampling method was employed to review all eligible electronic medical records during the study period.
2.4 Data collection
The following data were collected: (1) Demographic characteristics: sex, age, weight, and height. (2) NRS2002 scores and diagnoses (pancreatic neoplasms, periampullary tumour, cholangiocarcinoma). (3) Preoperative laboratory results: White blood cell count (WBC, 109/L), red blood cell count (RBC, 1012/L), haemoglobin concentration (Hb, g/L), platelet count (109/L), neutrophil percentage (%), AST concentration (U/L), ALT concentration (U/L), ALP concentration (U/L), total bilirubin concentration (μmol/L), direct bilirubin concentration (μmol/L), total protein concentration (g/L), and albumin concentration (g/L). Postoperative laboratory results: WBC count, RBC count, Hb concentration, platelet count, neutrophil percentage, AST concentration, ALT concentration, ALP concentration, total bilirubin concentration, direct bilirubin concentration, total protein concentration, and albumin concentration. (4) Surgical methods: Pancreatoduodenectomy, distal pancreatectomy, endoscopic procedures, biopsy (other), or no surgery. (5) Complication status.
2.5 Data quality control
Two researchers independently extracted data from the electronic medical records. After data collection, discrepancies were resolved by cross-checking and reverifying against the original records. A third researcher addressed missing values and outliers by reexamining the electronic records. Although the data analysis has a cross-sectional component in assessing the incidence of complications during a specific period, the fundamental design for data collection was retrospective.
2.6 Statistical analysis
Data were double-entered using EpiData 3.1 to construct a database. Inconsistent entries were corrected by referencing original records, followed by logical error checks. Statistical analyses were performed with SPSS 23.0: Categorical data are expressed as percentages and were analysed using chi-square tests. Continuous data are expressed as the means ± standard deviations and were analysed using t tests, ANOVA, or SNK-q tests.
Multivariate analysis was performed using binary logistic regression to identify independent factors associated with postoperative complications (coded as Yes = 1, No = 0). We employed a forced entry approach, including all the variables collected for the study in the final model, regardless of their significance in the univariate analysis. This conservative strategy was chosen to ensure a comprehensive assessment and to minimise the risk of overlooking potential predictors. Prior to model fitting, multicollinearity among all the independent variables was assessed using the variance inflation factor (VIF). All the VIF values were less than 5, indicating no substantial multicollinearity, thus justifying their simultaneous inclusion in the model. The results are expressed as adjusted odds ratios (ORs) with 95% confidence intervals (CIs).
Categorical variables (e.g., sex, disease diagnosis, surgical procedure) were handled using dummy coding in the multivariate logistic regression model. For each categorical variable, a reference group was specified to facilitate the interpretation of odds ratios. A complete list of variable categories and their corresponding reference groups is provided in the footnotes of Table 3.
All the statistical tests were two-sided, with a significance level of α = 0.05.
3 Results
3.1 Baseline characteristics of included subjects
A total of 199 electronic medical records were reviewed. After 27 patients whose records were incomplete were excluded, 172 patients were included, yielding an effective sample size of 172 patients. Among them, 101 were men and 71 were women, with ages ranging from 26 to 82 years and a mean age of 60.21 ± 10.94 years (Table 2).
3.2 Hospital complications in pancreatic disease patients
Among the 172 patients, 37 (21.51%) experienced postoperative complications. The most common complication was infection (25 cases, 14.53%), followed by pancreatic fistula (13 cases, 7.56%) and cholangitis (6 cases, 3.49%). The complete spectrum of complications is detailed in Table 1.
A total of 15 patients did not undergo surgery. One of these nonsurgical patients experienced severe complications, including sepsis, septic shock, and biliary tract infection, culminating in respiratory failure. The remaining 14 nonsurgical patients did not experience any documented in-hospital complications during the study period.
3.3 Univariate analysis of factors influencing hospital complications in pancreatic disease patients
Using chi-square tests, t tests, and ANOVA, independent variables (study factors) were compared with the dependent variable (occurrence of hospital complications) to identify differences across study factors. The results demonstrated that disease diagnosis category (χ² = 8.342, P = 0.015), postoperative red blood cell (RBC) count (t = −2.552, P = 0.012), and postoperative haemoglobin concentration (Hb, g/L) (t = −2.393, P = 0.018) significantly influenced the occurrence of complications (P < 0.05) (Table 2).
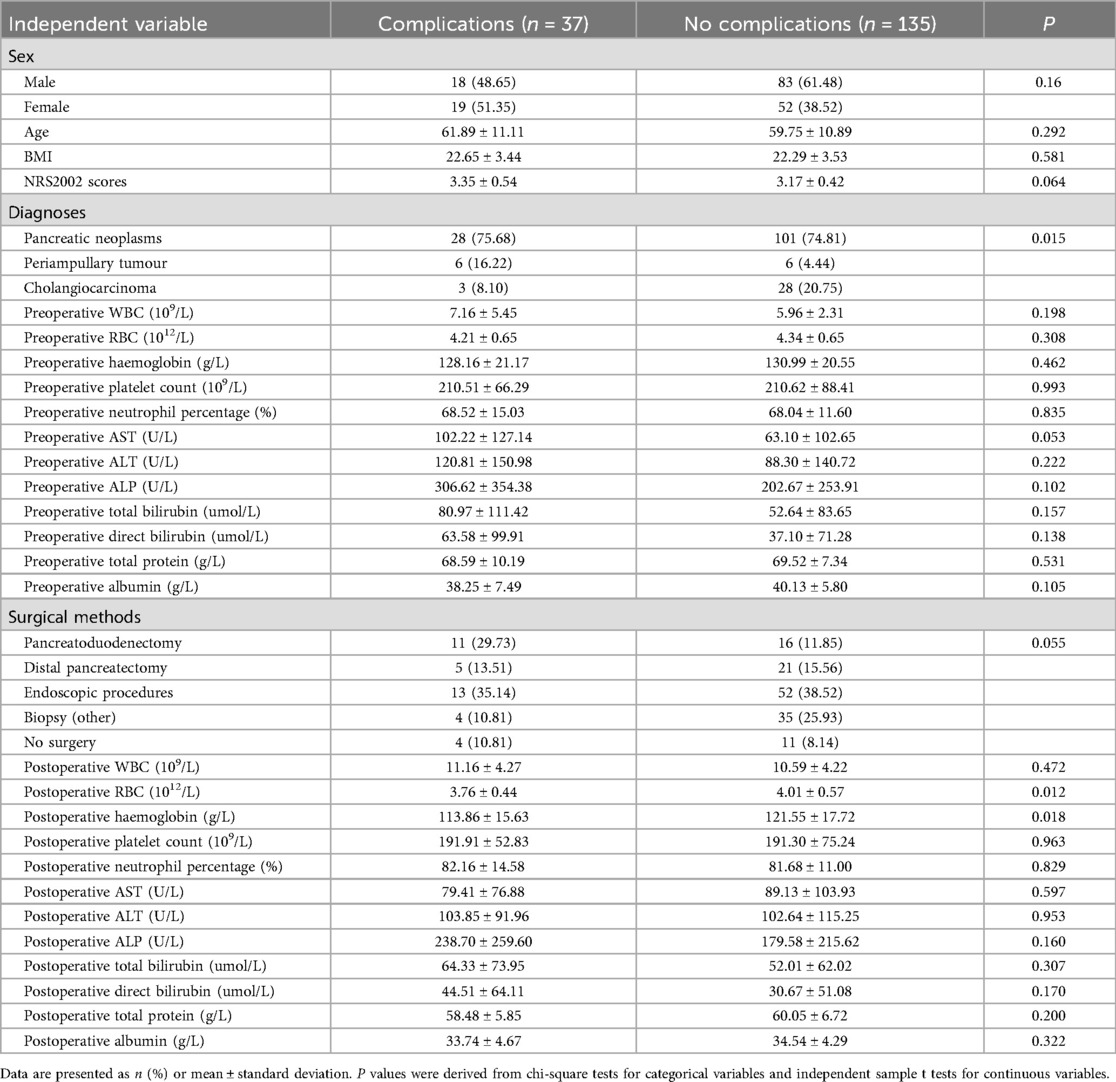
Table 2. Univariate analysis of factors influencing hospital complications in pancreatic disease patients.
3.4 Multivariate analysis of factors influencing hospital complications in pancreatic disease patients
Through stepwise regression analysis, independent variables (study factors) were analysed against the dependent variable (occurrence of hospital complications in patients with pancreatic disease). The results indicated that the NRS2002 score significantly influenced the occurrence of hospital complications (OR = 4.20; 95% CI: 1.017–17.368; P = 0.047) (Table 3).
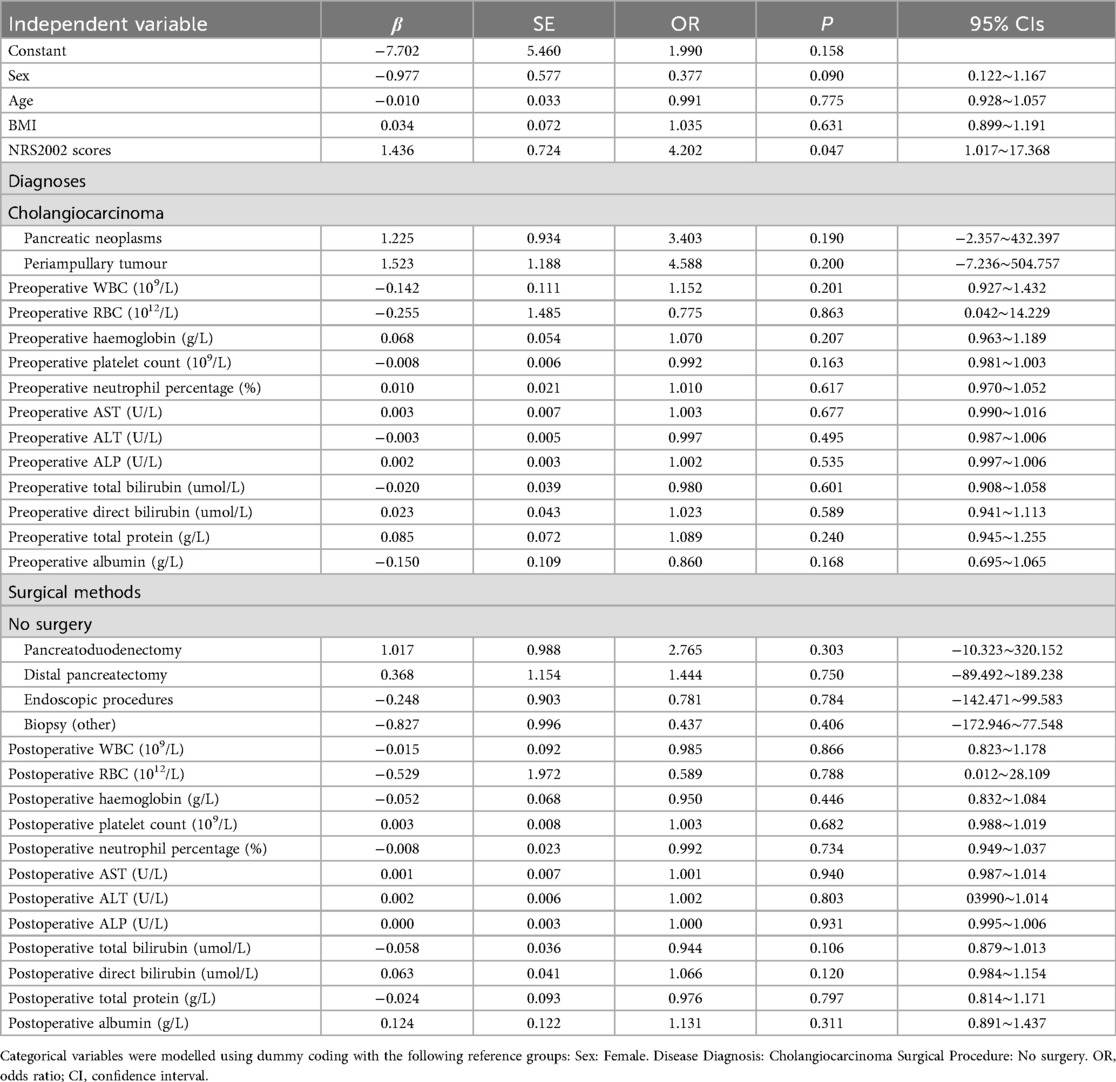
Table 3. Multivariate analysis of factors influencing hospital complications in pancreatic disease patients.
4 Discussion
4.1 Postoperative complication profile in pancreatic disease patients
This study revealed a postoperative complication rate of 21.51% in pancreatic disease patients, which was lower than the 72.6% reported by Weinberg et al. (5). for patients undergoing distal pancreatectomy (DP). Labib et al. (6) reported infection and/or major complication rates of 11% and 16%, respectively, in 348 patients following distal pancreatectomy with splenectomy. These discrepancies may arise from differences in surgical methods, treatment protocols, or follow-up duration, as this study focused solely on complications during hospitalisation and did not track postdischarge outcomes.
The most frequent complications in this study were infection (14.53%), pancreatic fistula (7.56%), and cholangitis (3.49%). In contrast, Weinberg et al. (5). reported that endocrine derangement (25.8%), postoperative systemic inflammatory response syndrome (22.6%), and postoperative pancreatic fistula (20.9%) were the most common complications. Notably, the incidence of postoperative pancreatic fistula aligns with our findings (7).
4.2 Factors influencing hospital complications in pancreatic disease patients
In the univariate analysis of factors influencing hospital complications, low postoperative red blood cell (RBC) counts (P = 0.012) and low postoperative haemoglobin (Hb) levels (P = 0.018) were identified as significant risk factors. The potential mechanisms linking reduced RBC and Hb levels to complications include the following: (1) Increased infection risk: Anaemia compromises tissue oxygenation and weakens immune cell function, increasing the incidence of postoperative pneumonia, intra-abdominal infections, and other infectious complications. Studies indicate that patients with low Hb levels face a fivefold greater risk of hospital complications and increased susceptibility to infections (8, 9). (2) Delayed recovery: Low Hb levels are associated with delayed intestinal function recovery, potentially prolonging hospitalisation (10). Nakamura et al. (8). confirmed that preoperative anaemia exacerbates hospital complications in elderly patients.
According to the multivariate analysis, high NRS2002 scores (P = 0.047) are an independent predictor of complications. Lee et al. (11). reported that preoperative malnutrition, assessed via serum albumin levels and body mass index (BMI), was correlated with poor short-term outcomes in pancreatic head cancer patients who underwent radical pancreatoduodenectomy (PD), with a significantly greater major complication rate in the malnutrition group (36.7% vs. 21.8%, P = 0.032). Zhang et al. (12). reported that protein-energy malnutrition is associated with increased mortality, prolonged hospital stays, higher costs, and systemic complications in pancreatic cancer patients undergoing open PD. Gillis et al. (13). highlighted that enhanced nutritional rehabilitation reduces hospital stays by 2 days and decreases complication rates in colorectal surgery patients. Similarly, Martin et al. (14). emphasised the clinical value of preoperative immunonutrition for reducing complications and length of stay (LOS) and improving postoperative nutritional indices (e.g., the NRI and serum albumin concentration) in patients with advanced pancreatic disease. Xu et al. (15). further showed that preoperative nutritional support reduces the incidence of postoperative pancreatic fistula in high-risk patients according to the NRS2002. Conversely, preoperative frailty has also been validated as a predictor of complications in pancreatic cancer patients (16).
Owing to the limited sample size within each specific surgical procedure category (e.g., only 27 pancreatoduodenectomies), a formal subgroup analysis to identify procedure-specific risk factors was not feasible. Future larger studies are needed to explore this aspect.
4.3 Limitations
(1) Sample size limitations: While numerous influencing factors were explored, the relatively small sample size restricts the generalisability of the findings. Future studies with larger cohorts are needed to validate these associations. (2) Limited follow-up: This study focused solely on complications during hospitalisation. Postdischarge complications were not investigated, potentially leading to an underestimation of the true complication burden. (3) The limitations of this work are its single-centre and retrospective design. Consequently, our results require validation in larger, prospective, multicentre studies. Subsequent research should aim to definitively establish whether interventions targeting these risk factors can lead to improved clinical outcomes.
5 Conclusions
The postoperative complication rate in pancreatic disease patients was 21.51%, with infection (14.53%), pancreatic fistula (7.56%), and cholangitis (3.49%) being the most common complications. Low postoperative RBC counts, low postoperative haemoglobin levels, and high preoperative NRS2002 scores were significant risk factors. Future large-scale, multicentre studies are warranted to validate these findings and refine clinical strategies.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the institutional review board of the Department of Hepatobiliary and Pancreas Surgery, The First Affiliated Hospital, Xi’an Jiaotong University. The studies were conducted in accordance with the local legislation and institutional requirements. The ethics committee/institutional review board waived the requirement of written informed consent for participation from the participants or the participants legal guardians/next of kin.
Author contributions
MZ: Conceptualization, Project administration, Writing – original draft. NL: Data curation, Investigation, Writing – original draft. WT: Data curation, Investigation, Writing – original draft. QX: Formal analysis, Supervision, Writing – review & editing. KW: Supervision, Writing – review & editing. ZW: Formal analysis, Supervision, Writing – review & editing. HL: Conceptualization, Project administration, Writing – original draft.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
1. Ilic I, Ilic M. International patterns in incidence and mortality trends of pancreatic cancer in the last three decades: a joinpoint regression analysis. World J Gastroenterol. (2022) 28(32):4698–4715. doi: 10.3748/wjg.v28.i32.4698
2. Wu Y, He S, Cao M, et al. Comparative analysis of cancer statistics in China and the United States in 2024. Chin Med J (Engl). (2024) 137(24):3093–3100. doi: 10.1097/CM9.0000000000003442
3. Mizrahi JD, Surana R, Valle JW, et al. Pancreatic cancer. Lancet. (2020) 395(10242):2008–2020. doi: 10.1016/S0140-6736(20)30974-0
4. Garcia-Ochoa C, McArthur E, Skaro A, et al. Pre-operative stenting and complications following pancreatoduodenectomy for pancreatic cancer: an analysis of the ACS-NSQIP registry. Surg Endosc. (2021) 35(12):6604–6611. doi: 10.1007/s00464-020-08160-9
5. Weinberg L, Ratnasekara V, Tran AT, et al. The association of postoperative complications and hospital costs following distal pancreatectomy. Front Surg. (2022) 9:890518. doi: 10.3389/fsurg.2022.890518
6. Labib JY, Lovasik BP, Lad N, et al. Implications of leukocytosis following distal pancreatectomy splenectomy (DPS) and association with postoperative complications. J Surg Oncol. (2022) 126(6):1012–1020. doi: 10.1002/jso.26988
7. de Oliveira SNA, Silva O, Duarte BN, et al. Suture versus stapler in distal pancreatectomy and its impact on postoperative pancreatic fistula. Sci Rep. (2025) 15(1):6052. doi: 10.1038/s41598-025-90617-9
8. Nakamura N, Kaida D, Tomita Y, et al. Risk factors for overall complications and remote infection after gastrectomy in elderly gastric cancer patients. In Vivo. (2021) 35(5):2917–2921. doi: 10.21873/invivo.12582
9. Kirkizlar TA, Kirkizlar O, Demirci U, et al. Incidence and predisposing factors of infection in patients treated with hypomethylating agents. Leuk Res. (2023) 127:107043. doi: 10.1016/j.leukres.2023.107043
10. Pecorelli N, Guarneri G, Quattromani R, et al. The impact of preoperative anemia on pancreatic resection outcomes. HPB (Oxford). (2022) 24(5):717–726. doi: 10.1016/j.hpb.2021.09.022
11. Lee B, Han HS, Yoon YS, et al. Impact of preoperative malnutrition, based on albumin level and body mass index, on operative outcomes in patients with pancreatic head cancer. J Hepatobiliary Pancreat Sci. (2021) 28(12):1069–1075. doi: 10.1002/jhbp.858
12. Zhang YX, Yang YF, Han P, et al. Protein-energy malnutrition worsens hospitalization outcomes of patients with pancreatic cancer undergoing open pancreaticoduodenectomy. Updates Surg. (2022) 74(5):1627–1636. doi: 10.1007/s13304-022-01293-7
13. Gillis C, Buhler K, Bresee L, et al. Effects of nutritional prehabilitation, with and without exercise, on outcomes of patients who undergo colorectal surgery: a systematic review and meta-analysis. Gastroenterology. (2018) 155(2):391–410. doi: 10.1053/j.gastro.2018.05.012
14. Martin RN, Agle S, Schlegel M, et al. Efficacy of preoperative immunonutrition in locally advanced pancreatic cancer undergoing irreversible electroporation (IRE). Eur J Surg Oncol. (2017) 43(4):772–779. doi: 10.1016/j.ejso.2017.01.002
15. Xu JY, Tian XD, Song JH, et al. Preoperative nutrition support may reduce the prevalence of postoperative pancreatic Fistula after open pancreaticoduodenectomy in patients with high nutritional risk determined by NRS2002. Biomed Res Int. (2021) 2021:6691966. doi: 10.1155/2021/6691966
Keywords: hospitalisation, pancreatic fistula, pancreatic disease, nutritional status, hospital complications, pancreatoduodenectomy, pancreatectomy
Citation: Zhang M, Li N, Tian W, Xiao Q, Wei K, Wang Z and Lu H (2025) High-risk factors for postoperative complications in patients with pancreatic disease: a single-center experience. Front. Surg. 12:1689107. doi: 10.3389/fsurg.2025.1689107
Received: 3 September 2025; Accepted: 5 November 2025;
Published: 19 November 2025.
Edited by:
Ravi Kumar Sharma, Chandigarh University, IndiaReviewed by:
Yusheng Shi, Shanghai Jiao Tong University, ChinaArchana Machireddy, Oregon Health and Science University, United States
Copyright: © 2025 Zhang, Li, Tian, Xiao, Wei, Wang and Lu. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Huapeng Lu, bHVodWFwZW5nQHhqdHVmaC5lZHUuY24=
 Man Zhang
Man Zhang Ning Li
Ning Li Kongyuan Wei
Kongyuan Wei Huapeng Lu
Huapeng Lu