- 1Department of Orthopedics, Shanghai Key Laboratory of Orthopedic Implant, Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 2Department of Plastic and Reconstructive Surgery, Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
- 3Department of Nursing, Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China
Purpose: The syndesmotic screws are frequently utilized in the treatment of unstable ankle fractures. However, significant controversies persist regarding their optimal application strategies. This study aims to investigate the dynamic changes in syndesmotic reduction among patients with unstable ankle fractures following syndesmotic screw fixation and to explore the relationship between malreduction and functional outcomes.
Methods: Patients with unstable ankle fractures who underwent open reduction and internal fixation (ORIF) with syndesmotic screw fixation from January 2020 were prospectively enrolled. Syndesmotic screws were routinely removed 8–12 weeks post-fixation. All patients were followed up at five time points: immediately after internal fixation, prior to syndesmotic screw removal (8–12 weeks), and at 3, 6, and 12 months post-initial fixation. Evaluations included imaging (Computed Tomography, CT), functional outcomes [Ankle and Hindfoot Function Scoring System (AOFAS), Olerud-Molander Ankle Score (OMAS)], and pain assessment (Visual Analog Scale, VAS).
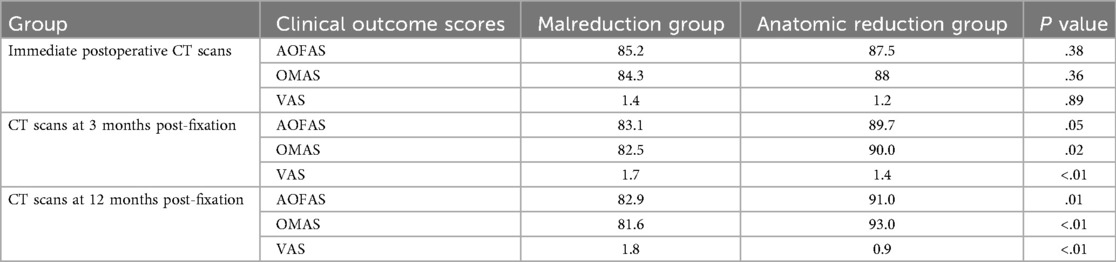
Results: From January 2020 to January 2021, a total of 26 patients were included in this study. The incidence of malreduction at the five follow-up time points was 69.2% (18/26), 61.5% (17/26), 50% (13/26), 61.5% (16/26), and 61.5% (16/26), respectively. Malreduction of the anterior tibiofibular distance and fibular rotation were the primary contributing factors. Functional outcomes were significantly worse for patients with malreduction following syndesmotic screw removal compared to those without malreduction (p < 0.05).
Conclusions: (1) Dynamic changes in syndesmotic reduction were observed at various time points within one year post-surgery. Removal of the syndesmotic screw improved syndesmotic reduction to some extent; however, re-diastasis may occur after weight-bearing. (2) Syndesmotic malreduction following screw removal was associated with poorer ankle functional outcomes.
1 Introduction
Ankle fractures are among the most prevalent fractures encountered in the emergency department, frequently accompanied by distal tibiofibular syndesmosis injury and ankle instability. According to reports, approximately 5%–10% of ankle sprain injuries and 10%–20% of ankle fractures involve distal tibiofibular syndesmosis injury, which typically requires surgical intervention (1–8). The current standard treatment involves using syndesmotic screws (SS) to stabilize the distal tibiofibular syndesmosis following open reduction and internal fixation (ORIF) for fractures (9–14). However, several aspects remain controversial, including the optimal diameter, position, and number of SS, whether and when the screw should be removed, and when weight-bearing should commence (15–21).
Malreduction of the distal tibiofibular syndesmosis is recognized as a common complication of unstable ankles, potentially leading to early ankle dysfunction and long-term traumatic arthritis (6, 22). Previous studies have explored the use of SS for reduction. Gardner et al. retrospectively evaluated 25 patients with ankle fractures and syndesmotic instability who underwent ORIF, finding that 52% exhibited evidence of syndesmotic malreduction on postoperative CT imaging. Endo et al. demonstrated that the anterior tibiofibular distance widened one year after syndesmotic screw removal (23). Nevertheless, these studies assessed syndesmotic reduction solely from an imaging perspective, without considering patient function. Consequently, they fail to provide clinically meaningful recommendations.
Currently, there remains a paucity of observations regarding continuous imaging changes in ankles following syndesmotic screw fixation, including reduction after SS placement, changes in the tibiofibular distance before and after screw removal, and short-term and long-term changes in the tibiofibular syndesmosis after weight-bearing. Additionally, further investigation into the relationship between these dynamic changes and functional outcomes is essential.
The objectives of this prospective study were as follows: (1) To observe time-dependent changes in images and functions of ankles within one year in patients undergoing SS fixation; (2) To evaluate the effect of SS removal on the tibiofibular syndesmosis; (3) To determine the rate of syndesmotic malreduction before and after SS removal; and (4) To investigate the relationship between imaging changes and functional outcomes of the ankles.
To our knowledge, this study provides the most comprehensive follow-up imaging data within one year for patients with ankle fractures involving tibiofibular syndesmosis injury who underwent ORIF. Most prior studies selected only one or two time points for follow-up (23, 24). In contrast, this study evaluated five key time points to capture the most complete dynamic trend of tibiofibular syndesmosis changes.
2 Materials and methods
2.1 Patients
This study was approved by the Ethics Committee of our hospital, and all participants provided written informed consent. Patients were prospectively recruited at our hospital between January 2020 and January 2021. This study was conducted in accordance with the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guidelines.
Inclusion criteria were as follows: patients aged 18–75 years, suffering from ankle fractures with diastasis of the tibiofibular syndesmosis or Maisonneuve fractures, and receiving ORIF with syndesmotic screw fixation within two weeks.
Exclusion criteria included open fractures, history of ankle injuries or surgeries, history of ankle osteoarthritis (Kellgren-Lawrence grade ≥2 based on x-ray), fractures accompanied by vascular or nerve injury, pathological fractures, concomitant fractures of the ipsilateral lower limb, and mental disorders precluding cooperation.
2.2 Surgical plan
All patients underwent ORIF according to AO principles. Distal fibula fractures were fixed with anatomical plates, and medial malleolus fractures were fixed with two cannulated screws (3.5 mm in diameter). Posterior malleolus fractures involving more than 25% of the articular surface were fixed with one to two cannulated screws, while those involving less than 25% were managed at the surgeon's discretion during the operation.
Following bone structure fixation, the stability of the distal tibiofibular syndesmosis was further assessed intraoperatively. The hook test was performed under C-arm fluoroscopy, and the tibiofibular distance or medial ankle joint space was measured bilaterally. A difference exceeding 2 mm indicated tibiofibular syndesmosis instability (25). Syndesmosis reduction was achieved under direct visualization. During SS insertion, the ankle was maintained in a neutral position, and the reduction clamp was used to temporarily fix the distal tibiofibular joint before screw insertion. Then, one SS (3.5 mm full-threaded cortical screw) was inserted from the fibula to the tibia. The optimal location for syndesmotic screw placement is typically 2–4 cm above the tibial plafond, parallel to the joint line, and engaging three or four cortices. For Maisonneuve injuries, the distal tibiofibular syndesmosis was stabilized using two syndesmotic screws (SS), and the deltoid ligament complex of the medial ankle was repaired with anchors. All SS were designed to penetrate three layers of the bone cortex. Patients were instructed to gradually perform non-weight-bearing functional exercises of the ankles until the SS were removed 8–12 weeks post-internal fixation (26). Following screw removal, gradual weight-bearing commenced on the injured limb (Supplementary Table S1).
2.3 Postoperative follow-up
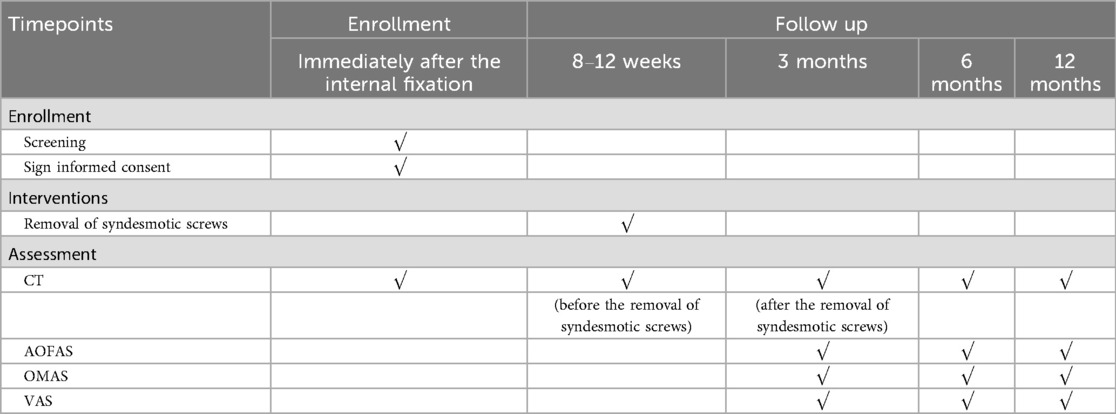
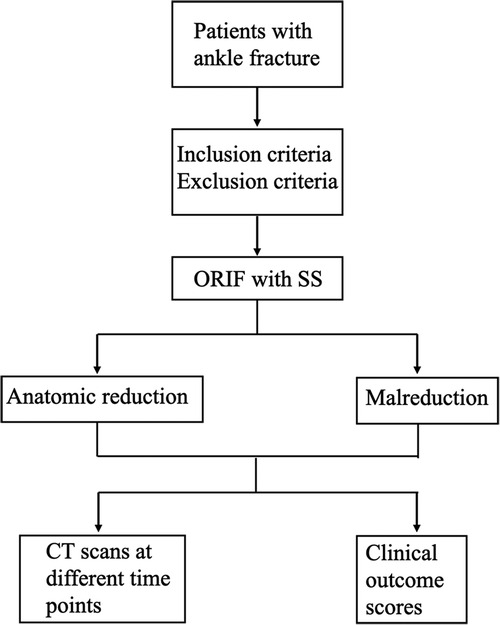
All participants underwent follow-up assessments at five specific time points (Table 1): immediately after internal fixation, prior to syndesmotic screw removal, 3 months post-internal fixation, 6 months post-internal fixation, and 12 months post-internal fixation. Conventional ankle computed tomography (CT) scans were performed at these time points, including bilateral scans at each assessment. Using the uninjured side as a control, imaging parameters of the injured side were measured to evaluate the reduction of the tibiofibular syndesmosis. During each CT examination, non-scanned body parts were shielded with lead clothing to minimize radiation exposure. Additionally, the American Orthopedic Foot and Ankle Society Score (AOFAS), Olerud-Molander Ankle Score (OMAS), and Visual Analogue Scale (VAS) were utilized to assess functional outcomes at 3, 6, and 12 months post-internal fixation (Figure 1).
2.4 Imaging measurements of the distal tibiofibular syndesmosis
In this study, a 1 mm-thick CT scan was employed. Imaging data were stored in Digital Imaging and Communications in Medicine (DICOM) format and imported into RadiAnt Viewer software (V2021.2, Medixant, Promienista 2560-288 Poznań, Poland) for analysis. All measurements were conducted at a standard axial position 10 mm above the articular surface. The following parameters were assessed (Figure 2): anterior tibiofibular distance (ATD), central tibiofibular distance (CTD), posterior tibiofibular distance (PTD), fibular translation distance (FTD), and fibular rotation angle (FRA) (27–30). Furthermore, the syndesmosis area and syndesmosis volume were also quantified (31). The syndesmosis area was defined by the boundaries of the tibiofibular joint and its anterior and posterior edges. The syndesmosis volume was calculated layer-by-layer from the syndesmosis area extending 3 cm above the ankle joint, approximated as the sum of the syndesmosis area × thickness of layers: syndesmosis volume = [A1 × T] + [A2 × T] + [A3 × T] + … + [An × T], where A represents the syndesmosis area at each layer, and T represents the thickness of each layer (1 mm in this study).
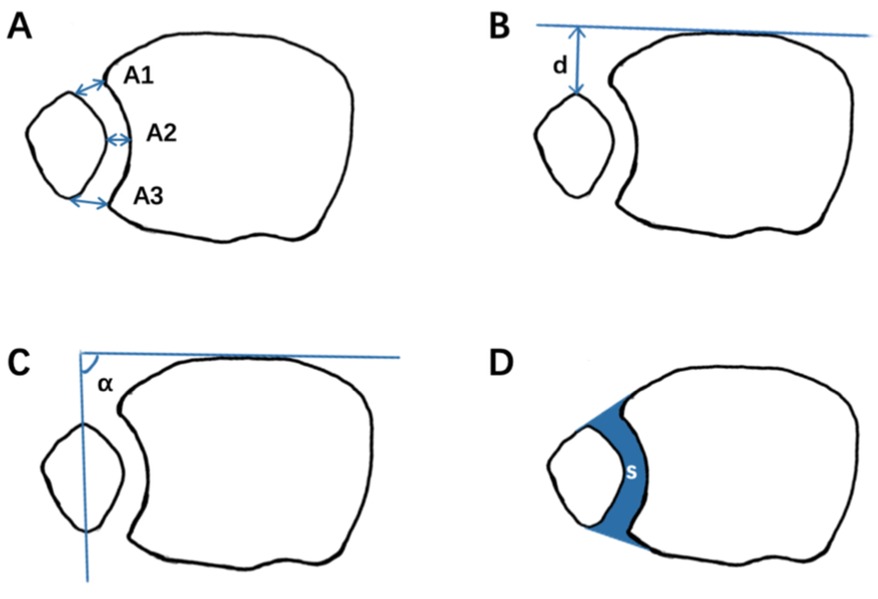
Figure 2. Measurements for evaluating syndesmotic reduction. (A) Illustration of an axial view of a normal syndesmosis proximal to the tibial plafond with measures A1 to A3. (B) Anteroposterior fibular translation. (C) Fibular rotation. (D) The sum of the syndesmosis area.
Malreduction of the tibiofibular syndesmosis was defined as meeting any of the following criteria: (1) a side-to-side difference of 2 mm or more in at least one parameter, including ATD, CTD, PTD, FTD; (2) a side-to-side difference of 5 degrees or more in FRA (23).
Participants were categorized into two groups based on CT findings at different time points: malreduction and anatomic reduction. Functional outcomes at 12 months post-internal fixation were compared between the two groups. A senior orthopedic surgeon, who was not involved in the treatment, conducted all CT measurements. To confirm measurement repeatability, assessments were repeated at 12-week intervals. The results of the two measurements were evaluated using the Intraclass Correlation Coefficient (ICC). Comparisons were made between the malreduction and anatomical reduction groups at various time points. Additionally, a comparison was conducted between the affected and healthy limbs within each patient.
2.5 Statistical analysis
All data were analyzed using Tukey's multiple comparison post-hoc test and Wilcoxon signed-rank test via the Statistical Package for the Social Sciences (SPSS, version 26.0, IBM Corporation, Chicago, IL, USA). A p-value < 0.05 was considered statistically significant.
3 Results
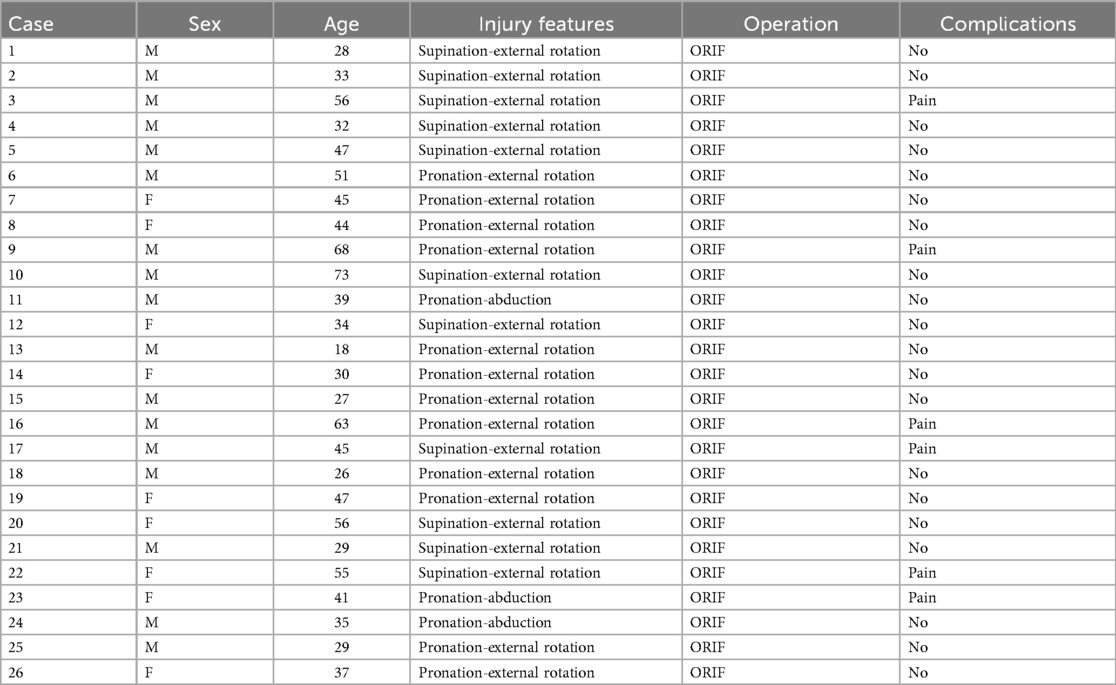
Between January 2020 and January 2021, 179 patients with ankle fractures were hospitalized for open reduction and internal fixation (ORIF). Of these, 37 patients (20.6%) met the inclusion criteria; however, four patients declined informed consent, and seven patients dropped out during the one-year follow-up period. Ultimately, 26 eligible patients (17 males and 9 females, mean age 46 years, range 18–73 years) were included in the study (Table 2). Eleven patients had 44-B fractures, and 15 patients had 44-C fractures. According to the Lauge-Hansen classification, there were 11 cases of supination-external rotation fractures, 12 cases of pronation-external rotation fractures, and 3 cases of pronation-abduction fractures. Among these, 22 patients were stabilized with one syndesmotic screw, while the remaining four (Maisonneuve injuries) required two SS (Supplementary Table S2).
3.1 Imaging measurements
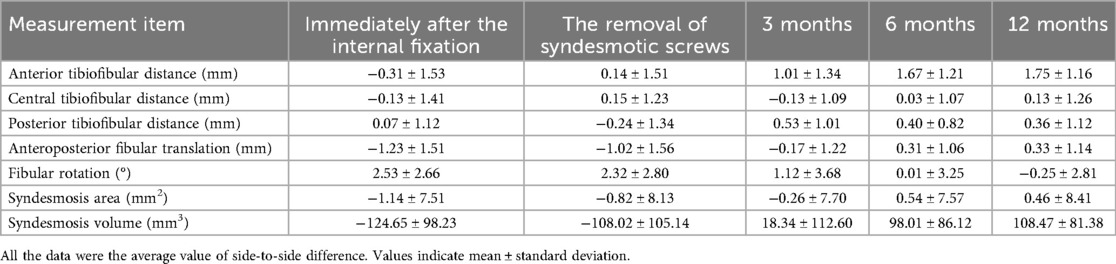
The results of imaging measurements are presented in Table 3 and Figure 3. Within one year post-internal fixation, the bilateral differences in ATD, FTD, FRA, syndesmosis area, and syndesmosis volume exhibited changes. No statistically significant differences were observed in the mean values of CTD and PTD across any time points within one year post-internal fixation. According to the definition of malreduction of the distal tibiofibular syndesmosis used in this study, the incidences of malreduction immediately after internal fixation, before removal of syndesmotic screws (SS), after removal of SS (3 months post-fixation), 6 months post-fixation, and 12 months post-fixation were 69.2% (18/26), 61.5% (17/26), 50% (13/26), 61.5% (16/26), and 61.5% (16/26), respectively. Among these, anterior tibiofibular distance malreduction and fibular rotational malreduction accounted for the majority.
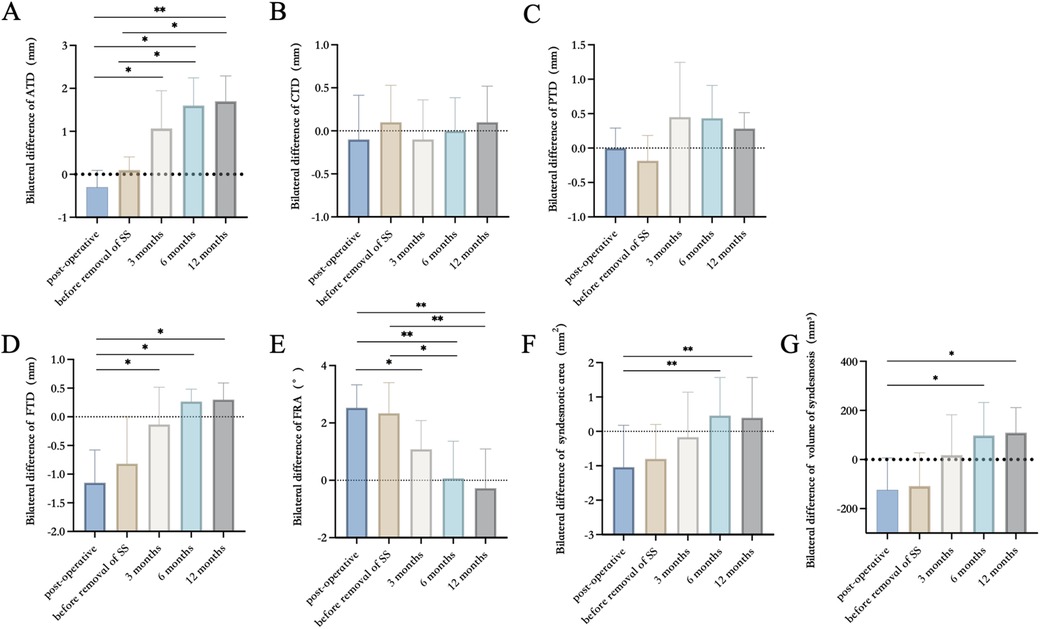
Figure 3. The results of imaging measurements in ATD, CTD, PTD, FTD, FRA, the sum of the syndesmosis area, and volume of syndesmosis. (A) Bilateral difference of ATD. (B) Bilateral difference of CTD. (C) Bilateral difference of PTD. (D) Bilateral difference of FTD. (E) Bilateral difference of FRA. (F) Bilateral difference of syndesmosis area. (G) Bilateral difference of volume of syndesmosis. Error bars present mean ± SD. *p < 0.05, **p < 0.01, and ***p < 0.001.
3.2 Functional follow-up
The median AOFAS scores at 3, 6, and 12 months following internal fixation were 53 (IQR: 28), 80 (IQR: 18), and 85 (IQR: 18), respectively. The median OMAS scores at 3, 6, and 12 month post-fixation were 37.5 (IQR: 15), 75 (IQR: 20), and 85 (IQR: 20), respectively. The average VAS scores at 3, 6, and 12 month post-fixation were 2.43, 1.63, and 1.54, respectively.
All patients were divided into two groups based on immediate postoperative CT scans of their ankles: anatomic reduction and malreduction. At the 12-month follow-up, the anatomic reduction group exhibited higher AOFAS, OMAS, and VAS scores compared to the malreduction group; however, no statistically significant differences were observed. Subsequently, according to ankle CT scans taken at 3 months and 12 months post-fixation, all patients were again categorized into anatomic reduction and malreduction groups. The results demonstrated a significant difference in functional and pain scores at 12 months post-fixation (Table 4).
4 Discussion
This study revealed that the absolute bilateral differences in anterior tibiofibular distance (ATD), fibular rotation angle (FRA), syndesmosis area, and syndesmosis volume significantly decreased after the removal of syndesmotic screws. Additionally, the fibula shifted posteriorly and rotated externally, potentially due to overcompression of the tibiofibular syndesmosis during SS implantation in some patients. Automatic reduction of the ankle occurred after SS removal. With the initiation of weight-bearing exercises, the absolute side-to-side differences in these parameters gradually increased and stabilized by six months post-fixation.
Based on these measurements, we can more accurately assess the reduction quality of the tibiofibular syndesmosis in patients. In this study, the immediate postoperative rate of syndesmotic malreduction reached 69.2%, likely attributable to overcompression of the tibiofibular syndesmosis. Following SS removal, the malreduction rate decreased. Several studies have reported syndesmotic overcompression and external rotation after fixation of ankle fractures with syndesmotic injury when using reduction forceps, particularly noticeable in elderly patients with osteoporosis (32–35). Cosgrove et al. emphasized the importance of the position of the medial clamp tine during syndesmotic reduction using forceps (36). Regauer et al. suggested that the stability of the posterior malleolus, as well as the medial and lateral collateral ankle ligaments, are critical determinants of tibiofibular reduction quality and recommended avoiding the use of reduction clamps or forceps whenever possible (37). Furthermore, surgeons' tactile feedback during SS insertion into the bone cortex also plays a subjective role in assessing potential overcompression during tibiofibular syndesmosis reduction.
Anatomic reduction of the distal tibiofibular syndesmosis is crucial for long-term functional outcomes (38–40). Numerous clinical studies have investigated postoperative changes in the tibiofibular syndesmosis, with varying results depending on time points and treatment strategies. Song et al. evaluated postoperative CT scans of bilateral ankles within two weeks of internal fixation and 30 days after SS removal (41). All SS were removed three months post-fixation. Results indicated that nine patients (36%) exhibited evidence of tibiofibular syndesmosis malreduction on initial postoperative axial CT scans. After SS removal, 8 out of 9 (89%) cases showed adequate reduction of the tibiofibular syndesmosis based on CT findings. Conversely, Kortekangas et al. utilized intraoperative CT with O-arm and postoperative CT of bilateral ankles under weight-bearing conditions at two-year follow-up to assess tibiofibular syndesmosis reduction (42). SS were not removed in any patients. Results showed that the rate of syndesmotic malreduction with SS increased from 5% (1/21)–16% (3/19) after two years. Comparatively, as reported by Endo et al., all patients had their SS removed six weeks post-fixation, and the rate of syndesmotic malreduction increased from 50% immediately post-fixation to 60% one year later (23).
In this study, patients were categorized into two groups—malreduction and anatomical reduction—based on computed tomography (CT) scans obtained three months after initial fixation following the removal of syndesmotic screws (SS). Functional outcomes at 12 months post-internal fixation were compared between the two groups. The results revealed statistically significant differences in AOFAS, OMAS, and VAS scores (p = .05, p = .02, p < .01), suggesting that malreduction of the syndesmosis after SS removal may negatively affect functional recovery.
Although ankle CT scans have been widely accepted by surgeons as a reliable method for evaluating tibiofibular syndesmosis, they are typically performed only before and after internal fixation, with limited attention given to post-removal assessment. Sagi et al. reported that patients with syndesmotic malreduction exhibited significantly worse functional outcomes at a two-year follow-up based on postoperative CT findings (40). Consequently, they recommended comparing postoperative CT scans with those of the contralateral limb to improve diagnostic accuracy. In contrast, this study emphasizes the importance of conducting CT evaluations after SS removal. Due to the stabilizing effect of the SS, some patients may maintain an anatomical reduction immediately after surgery; however, malreduction or diastasis may become apparent only after screw removal. Therefore, we recommend routine CT scanning following SS removal to enable early detection of syndesmotic abnormalities and timely intervention.
The optimal timing and necessity of SS removal remain controversial. Some studies advocate removing the screws six to eight weeks postoperatively to facilitate ligament healing and promote early weight-bearing, which has been shown to enhance functional outcomes (23). Conversely, other researchers support a more conservative approach, advising non-weight-bearing activity until 12 weeks or longer after surgery to prevent late syndesmotic diastasis, particularly in cases involving Weber C fractures. Furthermore, systematic reviews have found no significant difference in functional outcomes between routine and on-demand SS removal (43–45). Thus, it is suggested that SS removal should be considered only when patients present symptoms such as pain, mobility impairment, or infection (9, 46–48).
This study has several limitations. Although it was designed as a prospective cohort study, the sample size was relatively small due to a short enrollment period, multiple follow-up time points, and the impact of the COVID-19 pandemic. Among the 37 eligible patients enrolled in January 2020, four declined to provide informed consent (10.8%, 4/37), and seven were lost to follow-up (18.9%, 7/37). Potential reasons include the high frequency of required follow-ups (five times within one year), which many patients found burdensome after regaining normal ambulatory function within three to six months post-surgery. Additionally, the ongoing pandemic restricted patient mobility and discouraged hospital visits due to concerns about infection risk.
Another limitation pertains to the relatively short observation period. As noted by Egol et al., maximal functional recovery after ankle fracture surgery is typically achieved within one year (49). Our imaging data also indicated that syndesmotic parameters stabilized around six months post-fixation.
Future research will aim to address these limitations by including a control group comprising patients who did not undergo SS fixation and by strictly standardizing the timing of SS removal to enhance intergroup homogeneity. Moreover, gait analysis and weight-bearing CT scans will be incorporated into follow-up protocols to allow for a more comprehensive evaluation of syndesmotic integrity and functional outcomes.
5 Conclusion
1. Tibiofibular syndesmosis exhibits time-dependent changes within one year following internal fixation and SS removal. While SS removal may reduce the incidence of syndesmotic malreduction, syndesmotic diastasis may recur upon initiation of weight-bearing activities.
2. Malreduction of the tibiofibular syndesmosis following internal fixation was primarily characterized by a reduced anterior tibiofibular distance, internal rotation of the fibula, and anterior displacement of the fibula. This phenomenon may be associated with excessive compression of the tibiofibular syndesmosis by screws or improper screw insertion angles.
3. Routine postoperative CT evaluation is recommended after removal of the syndesmotic screw (SS). Furthermore, corrective intervention should be considered if malreduction is detected following screw removal.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Ethics Committee of the Shanghai Ninth People's Hospital, Shanghai JiaoTong University School of Medicine. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
XL: Investigation, Methodology, Writing – original draft, Data curation, Formal analysis, Software. PL: Investigation, Writing – original draft, Data curation, Project administration. RD: Writing – original draft. XW: Writing – original draft. QZ: Writing – original draft. SN: Writing – review & editing. XW: Conceptualization, Funding acquisition, Supervision, Writing – review & editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This research was supported by the National Key Research and Development Program of China (grant No. 2023YFB3813004), the Cross Disciplinary Research Fund of Shanghai Ninth People's Hospital, Shanghai Jiao Tong University School of Medicine (grant No. JYJC202229), and the Fundamental Research Funds for the Central Universities (grant No. YG2025QNA18).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The Reviewer SL declared a shared parent affiliation with the authors to the handling editor at the time of review.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fsurg.2025.1689228/full#supplementary-material
References
1. Dubin JC, Comeau D, McClelland RI, Dubin RA, Ferrel E. Lateral and syndesmotic ankle sprain injuries: a narrative literature review. J Chiropr Med. (2011) 10:204–19. doi: 10.1016/j.jcm.2011.02.001
2. Fort NM, Aiyer AA, Kaplan JR, Smyth NA, Kadakia AR. Management of acute injuries of the tibiofibular syndesmosis. Eur J Orthop Surg Traumatol. (2017) 27:449–59. doi: 10.1007/s00590-017-1956-2
3. Halabchi F, Hassabi M. Acute ankle sprain in athletes: clinical aspects and algorithmic approach. World J Orthop. (2020) 11:534–58. doi: 10.5312/wjo.v11.i12.534
4. Kellett JJ. The clinical features of ankle syndesmosis injuries: a general review. Clin J Sport Med. (2011) 21:524–9. doi: 10.1097/JSM.0b013e318234be7d
5. Michelson JD, Magid D, McHale K. Clinical utility of a stability-based ankle fracture classification system. J Orthop Trauma. (2007) 21:307–15. doi: 10.1097/BOT.0b013e318059aea3
6. Paez CJ, Lurie BM, Upasani VV, Pennock AT. Functional outcomes of unstable ankle fractures with and without syndesmotic fixation in the adolescent population. J Child Orthop. (2021) 15:418–25. doi: 10.1302/1863-2548.15.200250
7. Purvis GD. Displaced, unstable ankle fractures: classification, incidence, and management of a consecutive series. Clin Orthop Relat Res. (1982) 165:91–8. doi: 10.1097/00003086-198205000-00013
8. Rammelt S, Obruba P. An update on the evaluation and treatment of syndesmotic injuries. Eur J Trauma Emerg Surg. (2015) 41:601–14. doi: 10.1007/s00068-014-0466-8
9. Andersen MR, Frihagen F, Madsen JE, Figved W. High complication rate after syndesmotic screw removal. Injury. (2015) 46:2283–7. doi: 10.1016/j.injury.2015.08.021
10. de-Las-Heras Romero J, Alvarez AML, Sanchez FM, Garcia AP, Porcel PAG, Sarabia RV, et al. Management of syndesmotic injuries of the ankle. EFORT Open Rev. (2017) 2:403–9. doi: 10.1302/2058-5241.2.160084
11. Pogliacomi F, De Filippo M, Casalini D, Longhi A, Tacci F, Perotta R, et al. Acute syndesmotic injuries in ankle fractures: from diagnosis to treatment and current concepts. World J Orthop. (2021) 12:270–91. doi: 10.5312/wjo.v12.i5.270
12. Schepers T. Acute distal tibiofibular syndesmosis injury: a systematic review of suture-button versus syndesmotic screw repair. Int Orthop. (2012) 36:1199–206. doi: 10.1007/s00264-012-1500-2
13. Van Heest TJ, Lafferty PM. Injuries to the ankle syndesmosis. J Bone Joint Surg. (2014) 96:603–13. doi: 10.2106/JBJS.M.00094
14. Yu GS, Lin YB, Xiong GS, Xu HB, Liu YY. Diagnosis and treatment of ankle syndesmosis injuries with associated interosseous membrane injury: a current concept review. Int Orthop. (2019) 43:2539–47. doi: 10.1007/s00264-019-04396-w
15. Stuart K, Panchbhavi VK. The fate of syndesmotic screws. Foot Ankle Int. (2011) 32:S519–525. doi: 10.3113/FAI.2011.0519
16. Kukreti S, Faraj A, Miles JN. Does position of syndesmotic screw affect functional and radiological outcome in ankle fractures? Injury. (2005) 36:1121–4. doi: 10.1016/j.injury.2005.01.014
17. Wikerøy AK, Høiness PR, Andreassen GS, Hellund JC, Madsen JE. No difference in functional and radiographic results 8.4 years after quadricortical compared with tricortical syndesmosis fixation in ankle fractures. J Orthop Trauma. (2010) 24:17–23. doi: 10.1097/BOT.0b013e3181bedca1
18. Manjoo A, Sanders DW, Tieszer C, MacLeod MD. Functional and radiographic results of patients with syndesmotic screw fixation: implications for screw removal. J Orthop Trauma. (2010) 24:2–6. doi: 10.1097/BOT.0b013e3181a9f7a5
19. Miller AN, Paul O, Boraiah S, Parker RJ, Helfet DL, Lorich DG. Functional outcomes after syndesmotic screw fixation and removal. J Orthop Trauma. (2010) 24:12–6. doi: 10.1097/BOT.0b013e3181c6e199
20. Rogero RG, Illical EM, Corr DO, Raikin SM, Krieg JC, Tsai J. Management of ankle fractures with syndesmotic disruption: a survey of orthopaedic surgeons. Cureus. (2021) 13:e16391.34408944
21. Moon YJ, Kim DH, Lee KB. Is it necessary to remove syndesmotic screw before weight-bearing ambulation? Medicine (Baltimore). (2020) 99:e19436. doi: 10.1097/MD.0000000000019436
22. Kohake MBJ, Wiebking U, O'Loughlin PF, Krettek C, Gaulke R. Mid- to long-term outcomes after weber B-type ankle fractures with and without syndesmotic rupture. In Vivo. (2019) 33:255–61. doi: 10.21873/invivo.11469
23. Endo J, Yamaguchi S, Saito M, Morikawa T, Akagi R, Sasho T. Changes in the syndesmotic reduction after syndesmotic screw fixation for ankle malleolar fractures: one-year longitudinal evaluations using computer tomography. Injury. (2016) 47:2360–5. doi: 10.1016/j.injury.2016.07.031
24. Kimura S, Yamaguchi S, Ono Y, Watanabe S, Akagi R, Sasho T, et al. Changes in the syndesmotic reduction after syndesmotic suture-button fixation for ankle malleolar fractures: 1-year longitudinal evaluations using computed tomography. Foot Ankle Int. (2021) 42:1270–6. doi: 10.1177/10711007211008518
25. Mukhopadhyay S, Metcalfe A, Guha AR, Mohanty K, Hemmadi S, Lyons K, et al. Malreduction of syndesmosis–are we considering the anatomical variation? Injury. (2011) 42:1073–6. doi: 10.1016/j.injury.2011.03.019
26. Schepers T. To retain or remove the syndesmotic screw: a review of literature. Arch Orthop Trauma Surg. (2011) 131:879–83. doi: 10.1007/s00402-010-1225-x
27. Ebinger T, Goetz J, Dolan L, Phisitkul P. 3D model analysis of existing CT syndesmosis measurements. Iowa Orthop J. (2013) 33:40–6.24027459
28. Hamard M, Neroladaki A, Bagetakos I, Dubois-Ferrière V, Montet X, Boudabbous S. Accuracy of cone-beam computed tomography for syndesmosis injury diagnosis compared to conventional computed tomography. Foot Ankle Surg. (2020) 26:265–72. doi: 10.1016/j.fas.2019.03.006
29. Knops SP, Kohn MA, Hansen EN, Matityahu A, Marmor M. Rotational malreduction of the syndesmosis: reliability and accuracy of computed tomography measurement methods. Foot Ankle Int. (2013) 34:1403–10. doi: 10.1177/1071100713489286
30. Nault ML, Hébert-Davies J, Laflamme GY, Leduc S. CT scan assessment of the syndesmosis: a new reproducible method. J Orthop Trauma. (2013) 27:638–41. doi: 10.1097/BOT.0b013e318284785a
31. Kurokawa H, Taniguchi A, Miyamoto T, Tanaka Y. The relationship between the distal tibial fibular syndesmosis and the varus deformity in patients with varus ankle osteoarthritis. Foot Ankle Orthop. (2021) 6:24730114211041111. doi: 10.1177/24730114211041111
32. Cherney SM, Haynes JA, Spraggs-Hughes AG, McAndrew CM, Ricci WM, Gardner MJ. In vivo syndesmotic overcompression after fixation of ankle fractures with a syndesmotic injury. J Orthop Trauma. (2015) 29:414–9. doi: 10.1097/BOT.0000000000000356
33. Nimick CJ, Collman DR, Lagaay P. Fixation orientation in ankle fractures with syndesmosis injury. J Foot Ankle Surg. (2013) 52:315–8. doi: 10.1053/j.jfas.2013.02.005
34. Phisitkul P, Ebinger T, Goetz J, Vaseenon T, Marsh JL. Forceps reduction of the syndesmosis in rotational ankle fractures: a cadaveric study. J Bone Joint Surg. (2012) 94:2256–61. doi: 10.2106/JBJS.K.01726
35. Ambrose CG, Kiebzak GM, Sabonghy EP, Tabor OB, Peindl RD, Clanton TO, et al. Biomechanical testing of cadaveric specimens: importance of bone mineral density assessment. Foot Ankle Int. (2002) 23:850–5. doi: 10.1177/107110070202300913
36. Cosgrove CT, Putnam SM, Cherney SM, Ricci WM, Spraggs-Hughes A, McAndrew CM, et al. Medial clamp tine positioning affects ankle syndesmosis malreduction. J Orthop Trauma. (2017) 31:440–6. doi: 10.1097/BOT.0000000000000882
37. Regauer M, Mackay G, Nelson O, Böcker W, Ehrnthaller C. Evidence-based surgical treatment algorithm for unstable syndesmotic injuries. J Clin Med. (2022) 11:331. doi: 10.3390/jcm11020331
38. Del Balso C, Hamam AW, Chohan MBY, Tieszer C, Lawendy AR, Sanders DW. Anatomic repair vs. closed reduction of the syndesmosis. Foot Ankle Int. (2021) 42:877–85. doi: 10.1177/1071100721990008
39. Naqvi GA, Cunningham P, Lynch B, Galvin R, Awan N. Fixation of ankle syndesmotic injuries: comparison of tightrope fixation and syndesmotic screw fixation for accuracy of syndesmotic reduction. Am J Sports Med. (2012) 40:2828–35. doi: 10.1177/0363546512461480
40. Sagi HC, Shah AR, Sanders RW. The functional consequence of syndesmotic joint malreduction at a minimum 2-year follow-up. J Orthop Trauma. (2012) 26:439–43. doi: 10.1097/BOT.0b013e31822a526a
41. Song DJ, Lanzi JT, Groth AT, Drake M, Orchowski JR, Shaha SH, et al. The effect of syndesmosis screw removal on the reduction of the distal tibiofibular joint: a prospective radiographic study. Foot Ankle Int. (2014) 35:543–8. doi: 10.1177/1071100714524552
42. Kortekangas T, Savola O, Flinkkilä T, Lepojärvi S, Nortunen S, Ohtonen P, et al. A prospective randomised study comparing TightRope and syndesmotic screw fixation for accuracy and maintenance of syndesmotic reduction assessed with bilateral computed tomography. Injury. (2015) 46:1119–26. doi: 10.1016/j.injury.2015.02.004
43. van den Bekerom MP, Kloen P, Luitse JS, Raaymakers EL. Complications of distal tibiofibular syndesmotic screw stabilization: analysis of 236 patients. J Foot Ankle Surg. (2013) 52:456–9. doi: 10.1053/j.jfas.2013.03.025
44. Dingemans SA, Rammelt S, White TO, Goslings JC, Schepers T. Should syndesmotic screws be removed after surgical fixation of unstable ankle fractures? A systematic review. Bone Joint J. (2016) 98-b:1497–504. doi: 10.1302/0301-620X.98B11.BJJ-2016-0202.R1
45. Walley KC, Hofmann KJ, Velasco BT, Kwon JY. Removal of hardware after syndesmotic screw fixation: a systematic literature review. Foot Ankle Spec. (2017) 10:252–7. doi: 10.1177/1938640016685153
46. Boyle MJ, Gao R, Frampton CM, Coleman B. Removal of the syndesmotic screw after the surgical treatment of a fracture of the ankle in adult patients does not affect one-year outcomes: a randomised controlled trial. Bone Joint J. (2014) 96-b:1699–705. doi: 10.1302/0301-620X.96B12.34258
47. Davidovitch RI, Weil Y, Karia R, Forman J, Looze C, Liebergall M, et al. Intraoperative syndesmotic reduction: three-dimensional versus standard fluoroscopic imaging. J Bone Joint Surg. (2013) 95:1838–43. doi: 10.2106/JBJS.L.00382
48. Sanders FRK, Birnie MF, Dingemans SA, van den Bekerom MPJ, Parkkinen M, van Veen RN, et al. Functional outcome of routine versus on-demand removal of the syndesmotic screw: a multicentre randomized controlled trial. Bone Joint J. (2021) 103-b:1709–16. doi: 10.1302/0301-620X.103B11.BJJ-2021-0348.R2
Keywords: ankle fracture, syndesmotic fixation, computed tomography, syndesmosis, malreduction
Citation: Li X, Liu P, Duan R, Wang X, Zhu Q, Ni S and Wang X (2025) Ankle fracture with syndesmotic injury treated by screw fixation: a prospective study on clinical and radiographic outcomes. Front. Surg. 12:1689228. doi: 10.3389/fsurg.2025.1689228
Received: 20 August 2025; Accepted: 11 September 2025;
Published: 9 October 2025.
Edited by:
Mohammad Nikkhoo, Islamic Azad University, IranReviewed by:
Shengdi Lu, Shanghai Jiao Tong University, ChinaYi Zhou, Shanghai Fuyu Rehabilitation Clinic, China
Copyright: © 2025 Li, Liu, Duan, Wang, Zhu, Ni and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuangling Ni, bnNsMTAwOUAxNjMuY29t; Xiaoqing Wang, b3N0ZW9jbGFzdDIwMDZAc2p0dS5lZHUuY24=
†These authors have contributed equally to this work and share first authorship
 Xiaodong Li
Xiaodong Li Pengcheng Liu
Pengcheng Liu Ran Duan
Ran Duan Xiang Wang
Xiang Wang Qianhua Zhu1
Qianhua Zhu1 Xiaoqing Wang
Xiaoqing Wang