- 1Department of Orthopedic Surgery, Sichuan University West China Hospital, Chengdu, China
- 2West China Hospital School of Nursing, Sichuan University, Chengdu, China
- 3Operating Room, Department of Anesthesiology, West China Hospital, Sichuan University, Chengdu, China
Background: Cervical disc herniation at the C2-3 level, resulting in cervical spondylotic myelopathy (CSM), is an uncommon clinical entity. The diagnostic and therapeutic complexity escalates when this pathology coexists with non-contiguous multilevel cervical disc degenerative disease (CDDD). Due to the segmental variability in pathological features, the clinical manifestations of such cases are highly heterogeneous, thereby necessitating a highly individualized treatment strategy. Hybrid surgery (HS), which integrates cervical disc arthroplasty (CDA) and anterior cervical discectomy and fusion (ACDF), offers a tailored approach for the management of multilevel degenerative cervical pathology. The unique anatomical features and surgical technical challenges at the C2-3 level impose significant constraints on treatment options. This article presents a case of non-contiguous three-level hybrid surgery involving CDA at C2-3 and ACDF at C4-5 and C5-6, and discusses the feasibility of this technique for upper cervical disc pathology.
Case presentation: A 62-year-old female was admitted with a 6-month history of neck and right upper limb pain, numbness, and gait instability, which had been unresponsive to conservative management. DR revealed loss of the normal cervical lordosis. CT showed no significant osteophyte formation or bony canal stenosis. MRI demonstrated a large disc extrusion at C2-3 causing spinal cord compression, and disc herniations at C4-5 and C5-6 with nerve root impingement. Based on clinical and imaging findings, a diagnosis of multilevel cervical spondylopathy (C2-3, C4-5, and C5-6 disc herniation) was established. The patient underwent anterior cervical discectomy followed by artificial disc arthroplasty (CDA) at C2-3, and anterior cervical discectomy and fusion (ACDF) at C4-5 and C5-6, successfully completing a non-contiguous three-level hybrid surgical procedure.
Results: Postoperative symptoms were significantly alleviated. At the 12-month follow-up, pain and gait disturbance had largely returned to normal. MRI confirmed adequate decompression of neural compression, DR demonstrated satisfactory range of motion (ROM) at C2-3, and CT revealed satisfactory bone healing at the fused segments.
Conclusion: CDA serves as an effective alternative for C2-3 disc pathology, achieving neural decompression while preserving segmental mobility. The HS provides a valuable surgical option for the precise treatment of non-contiguous multilevel degenerative disease.
Introduction
Hybrid surgery (HS), a combination of anterior cervical discectomy and fusion (ACDF) and cervical disc arthroplasty (CDA), is applicable for the treatment of both single-level and multi-level cervical degenerative disc disease (CDDD). Non-contiguous CDDD is a special form of multi-level CDDD. As a clinically rare pathological condition, the degeneration of the cervical discs in this disease is non-contiguous, with one or more normal discs between two or more degenerated cervical discs. The therapeutic effect of HS for the treatment of multi-level CDDD has been proven to be non-inferior to ACDF or CDA alone (1, 2). Due to the presence of uncontiguous lesions, managing the intermediate normal segments poses a challenge in the treatment of this type of cervical spondylosis, where personalized management for each disc segment level is particularly important (3). According to the results of a finite element study, HS has the biomechanical advantage in the treatment of non-contiguous CDD for potentially reducing the likelihood of loss of intervertebral disc height (IDH) of the intermediate segment (IS) between CDA and ACDF (4, 5). More importantly, CDA demonstrates significant biomechanical advantages by effectively mitigating stress concentration in intermediate and adjacent spinal segments (6).
Compared to the common degenerative changes in the lower cervical spine, C2-3 disc herniation is much rarer. The literature mentions that C2-3 pathologies are usually associated with trauma or hangman's fractures (7). Surgical options for C2-3 disc herniation include anterior decompression and fusion, posterior decompression and fixation, as well as other methods. Compared to posterior cervical surgery, C2-3 anterior surgery has advantages such as fewer complications and less postoperative axial neck pain, although the surgical approach can be challenging (8–10). Reported outcomes of C2-3 ACDF have shown satisfactory clinical results and are often recommended for unstable hangman's fractures (11, 12). Owing to the limitations of ACDF surgery, such as the loss of mobility in the operated segment and the increased risk of ASD, CDA offers more advantages by preserving mobility and avoiding stress concentration in the intermediate and adjacent segments. Additionally, the range of motion (ROM) of C2-3 segment plays a crucial role in maintaining cervical stability, making CDA a more suitable option (6, 13). Therefore, in our report, we adopted a HS approach to provide individualized treatment for each segment of non-contiguous cervical lesions, aiming to maintain cervical stability and protect the intermediate segments as much as possible.
Case presentation
Preoperative assessment
The patient is a 62-year-old woman who presented with gait instability and recurrent pain and numbness in the neck, shoulder, and right upper limb for 6 months [Visual Analogue Scale (VAS) score = 7, Japanese Orthopaedic Association score (JOA) = 10, Neck Disability Index (NDI) = 23]. The pain was characterized by a stabbing sensation radiating to the thumb, index, and middle fingers. Symptoms were exacerbated by coughing, sneezing, or physical exertion. Motor examination showed 4/5 strength in the right deltoid, biceps, and triceps muscles, with 5/5 strength in the remaining limb muscles. Hoffmann's sign was positive while Babinski's sign was negative. She underwent muscle relaxation exercises and medical treatment for over 6 months without improvement, and the pain and numbness persisted. Preoperative MRI revealed degenerative changes and extrusion of the C2-3 disc with secondary spinal canal stenosis; disc herniations at C4-5 and C5-6 caused nerve compression. CT scans ruled out cervical ossification of posterior longitudinal ligament (OPLL) (Figure 1). Additionally, lateral bending and extension dynamic x-rays successfully demonstrated good cervical spine mobility from C2 to C7. The preoperative ROM at C2-3, C4-5, and C5-6 are 6.7°, 8.8°, and 8.8°, respectively. The patient had limited neck movement and complained of neck stiffness. The bone mineral density (BMD) report indicated a T-score of −0.8. Electromyography (EMG) findings revealed neurogenic injury in the right biceps and triceps muscles. Based on the aforementioned clinical manifestations and preoperative examination results, we devised an individualized surgical strategy for the patient, taking into account the existing anterior nerve compression, discontinuous disc pathology, and the unique feature of a normal C3-4 segment. Specifically, we performed CDA at the C2-3 level and ACDF at the C4-5 and C5-6 levels.
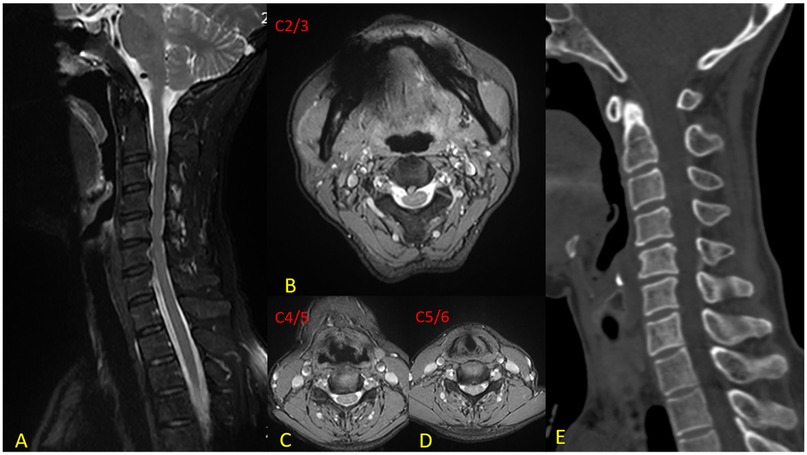
Figure 1. Preoperative imaging. (A) Sagittal MRI reveals a massive disc extrusion at C2-3 resulting in secondary spinal canal stenosis, along with disc protrusions at C4-5 and C5-6; (B) Axial T2-weighted image at C2–3 demonstrates a large right paramedian soft disc extrusion; (C) Axial view at C4–5 shows a disc protrusion causing neural compression; (D) Axial image at C5–6 illustrates disc herniation leading to neuroforaminal stenosis; (E) CT scan depicts osteophyte formation surrounding the C4–6 vertebral bodies, ruling out ossification of the posterior longitudinal ligament (OPLL).
Surgical procedure
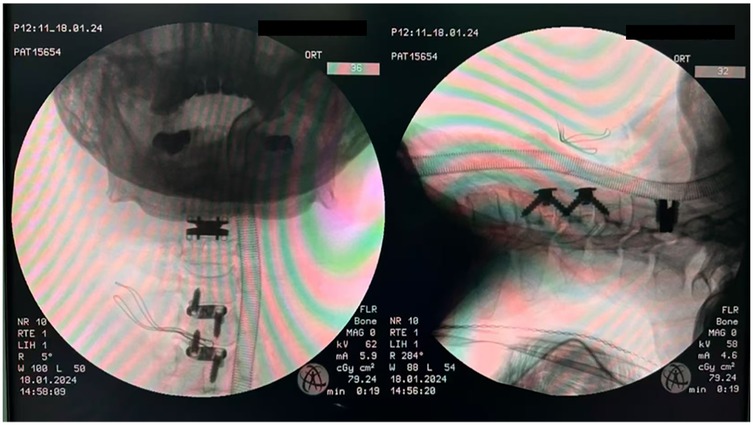
During the surgery, after general anesthesia induction and endotracheal intubation with laryngoscopic assistance, the patient was maintained in a neutral position (with mild cervical extension). A standard right anterior cervical approach and exposure were performed. A transverse incision approximately 7 cm in length was made in the anterior neck, and the approach was through the interval between the carotid sheath and the tracheoesophageal sheath. Initially, the surgeon completely resected the intervertebral disc tissue at the corresponding level. Bilateral uncovertebral joints and osteophytes were removed using a high-speed drill or Kerrison rongeurs to achieve thorough decompression until pulsation of the dural sac was visible. Secondly, for CDA, after preparing the endplates and performing an insertion trial, an appropriately sized Prestige-LP (Medtronic Sofamor Danek, Memphis, TN) was inserted along with the channels in the endplates. Thirdly, for fusion, after determining the appropriate size of the trajectory spacer, the corresponding Zero-P implant (Synthes, Oberdorf, Switzerland) filled with β-tricalcium phosphate or locally harvested bone was inserted into the prepared intervertebral space. Next, two locking screws were tightened cranially and caudally to secure the implant. Then, intraoperative C-arm fluoroscopy was used to confirm the correct placement of the implants (Figure 2). The natural structure of the intervertebral space and prevertebral tissues were preserved during the surgery. Finally, a drain was inserted before closing the incision. After the patient was fully awake, following commands, and had regular and strong spontaneous breathing with satisfactory tidal volume, the endotracheal tube was removed. The patient was closely monitored in the ICU for 24 h. In the absence of dyspnea, stridor, or decreased oxygen saturation, the patient was transferred to a general ward for further observation.
Postoperative course
The patient's hospital course was uneventful, with no occurrence of C5 palsy, hematoma, dysphagia, hoarseness, or dysphonia. Significant symptomatic relief was noted immediately after surgery (postoperative VAS score = 2), although intermittent neck, shoulder, and right upper arm pain persisted. Gait instability had largely resolved. Postoperative MRI confirmed complete decompression of neural compression and CT revealed satisfactory bone healing at the fused segments (Figure 3). At the 12-month follow-up, dynamic radiographs (including flexion–extension lateral views) demonstrated preserved ROM at each surgical level: preoperative ROM measured 6.7°, 8.8°, and 8.8° at C2-3, C4-5, and C5-6, respectively, compared to 6.0°, 9.5°, and 8.4° postoperatively. Notably, no loss of IDH was observed at the IS (C3-4), and its mobility remained unchanged (Figure 4). The patient reported only mild pain (VAS = 2), with complete resolution of preoperative gait instability and persistent discomfort in the neck and shoulder [JOA = 16, NDI = 5]. No postoperative complications were noted during the follow-up period, and cervical spine mobility was well maintained.
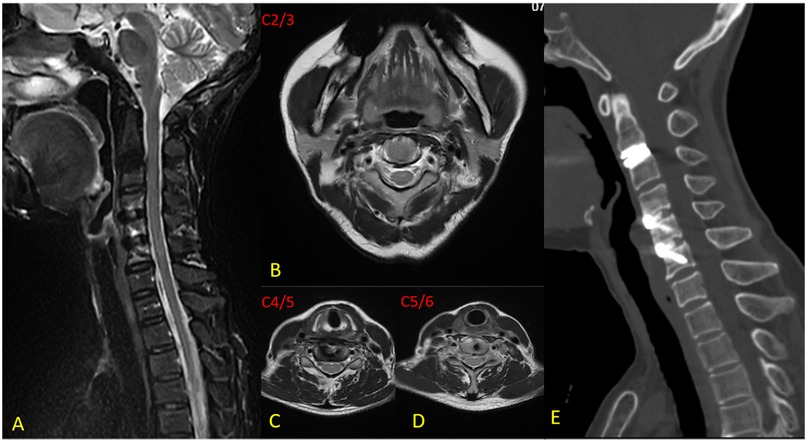
Figure 3. Imaging at 12-month follow-up. (A) Sagittal metal artifact-reduced MRI demonstrates complete resolution of neural compression at C2-3, C4-5, and C5-6 levels, with no residual occupying lesion in the spinal canal; (B) Axial view at C2-3 confirms thorough neural decompression without residual compression; (C) Axial image at C4-5 shows adequate decompression of previously compressed neural structures; (D) Axial image at C5-6 illustrates complete relief of spinal cord and nerve root compression; (E) CT scan reveals well-positioned artificial cervical disc at C2-3 and Zero-P implants at C4-5 and C5-6, with satisfactory bony fusion.
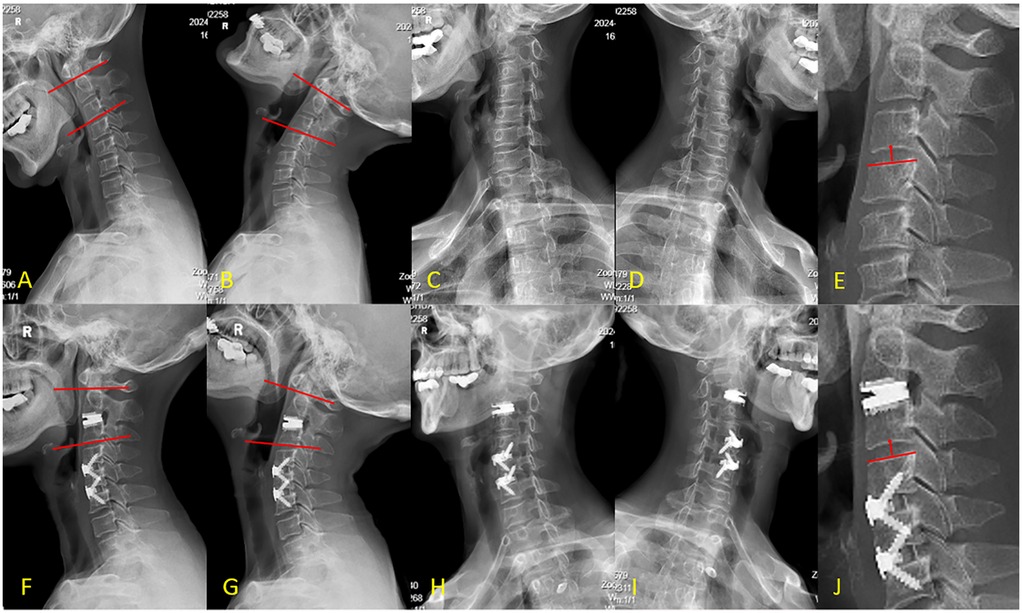
Figure 4. (A–E) Preoperative x-rays, F-J: postoperative x-rays. Image (A) and (B) shows preoperative C2-3 range of motion was 7.1°. Image (F) and (G) shows postoperative range of motion was 6.9°. Image (C) shows stenosis of the C4-5 and C5-6 intervertebral foramina. Image (H) shows complete resolution of the stenosis with the intervertebral foramina enlarged compared to preoperative status. Image (E) shows preoperative intervertebral disc height (IDH) of C3-4 is 14.1 mm, Image (J) shows postoperative IDH of 13.4 mm with no loss.
Discussion
There are multiple surgical options for the treatment of C2-3 cervical disc herniation. For upper cervical lesions, posterior surgery is a safe choice (9). However, compared to posterior cervical surgery, the anterior approach has advantages such as fewer complications and less postoperative axial neck pain (8). Anterior cervical surgery includes different surgical approaches, such as the standard right anterior cervical approach, transfacetal approach, transoral approach, anterolateral epidural approach, and submandibular approach (8, 14–17). Nevertheless, C2-3 surgery is particularly challenging due to the complex surrounding anatomy (18). The C2-3 surgical procedure is particularly challenging due to the complex surrounding anatomical structures. Specifically, the C2-3 segment is in close proximity to the medulla oblongata and upper cervical spinal cord, while also adjacent to the vertebral artery and internal carotid artery (19). These spatial constraints significantly limit the operating space, making intraoperative precise decompression and fixation extremely technically demanding. In addition, the atlas and the second cervical vertebra form the atlanto-axial joint, which constitutes the main structure for head rotation. During surgery to thoroughly decompress and relieve nerve compression, imprecise resection may disrupt spinal stability, and extensive fixation and fusion may lead to limited cervical spine mobility. Therefore, when operating in the C2-3 region, it is necessary to balance decompression and cervical stability, requiring high precision to maintain joint stability and avoid postoperative cervical instability. To date, there is no unified consensus on the treatment of C2-3 cervical disc herniation. Previous retrospective studies have shown that ACDF is a widely used surgical method for C2-3 cervical disc herniation (12). As an alternative to ACDF, this case report demonstrates that in addition to fusion, CDA can also be performed effectively and safely.
Considering the anterior neural compression, discontinuous and variable disc degeneration, and normal C3-4 segment in this case, an individualized surgical strategy was devised to achieve complete neural decompression, preserve the C3-4 disc, and maintain cervical spine mobility. Anterior surgery was preferred over posterior approaches due to its direct access to anterior neural compression and ability to restore intervertebral height and stability with implants. Given the anterior osteophytes at C4-5, significant posterior endplate sclerosis at C5-6, and substantial height discrepancy in the intervertebral space, ACDF was selected for C4-5 and C5-6 to restore height and lordosis and achieve solid fusion. For the large central disc herniation at C2-3, surgical intervention was necessary to relieve neural compression. Moreover, the absence of significant disc degeneration and spinal cord compression at the C3-4 level, along with the need to preserve the rotational stability of the atlantoaxial joint by avoiding excessive restriction of C2 vertebral motion, and to prevent stress concentration and subsequent ASD at C3-4, made CDA at C2-3 a more suitable option. Importantly, the C2-3 level had favorable bone quality, consistent intervertebral height, and no significant osteophytes or endplate sclerosis, supporting CDA as the optimal surgical strategy. Therefore, we performed a hybrid surgery combining CDA at C2-3 with ACDF at C4-5 and C5-6, achieving an individualized, non-contiguous three-level procedure.
ACDF recognized globally as the “gold standard” for anterior cervical surgery, is characterized by its broad indications, mature technique, high fusion rate, and strong stability (20). Over the past two decades, CDA has emerged as an established alternative to ACDF for the treatment of radiculopathy and myelopathy, favored by spine surgeons for its ability to maintain motion at the treated segment, potentially reduce adjacent segment degeneration, and demonstrate satisfactory long-term clinical outcomes with low surgical complication and revision rates in long-term follow-up (20, 21). As a combination of ACDF and CDA, HS encompasses the advantages of anterior cervical surgery. Depending on the location of the lesion, different combinations are selected after precise identification of indications to provide the optimal treatment strategy for different lesion levels (2). ACDF fuses and fixes adjacent vertebrae, which may lead to increased stress on adjacent segments and accelerate their degeneration. Studies have shown that compared to ACDF, HS has a smaller mechanical impact on adjacent segments and can reduce the interaction between CDA segments and ACDF segments (1, 22). This makes HS a suitable option for the treatment of non-contiguous CDDD (23).
Despite the advantages of HS in preserving cervical spine mobility and reducing the incidence of ASD, surgeons must be vigilant about potential risks such as periprosthetic bone absorption and heterotopic ossification (HO) (24). Anterior bone loss (ABL) of vertebra is a common early postoperative complication, which is usually self-limiting and occurs within the first year after surgery. Wu et al. (25) reported an incidence of ABL of 52.8% in patients who underwent CDA with the Prestige-LP prosthesis. Severe ABL can lead to adverse outcomes such as implant subsidence and displacement. Fortunately, our follow-up results did not reveal any significant bone absorption around the C2-3 CDA. Moreover, HO is another potential long-term complication of CDA. Clinical series comparing ACDF with CDA indicate that HO remains an important factor affecting the long-term success of motion-preserving implants (26). Although CDA is designed to preserve motion, severe HO can restrict segmental mobility, and in some cases, lead to complete loss of segmental motion, thereby threatening the longevity of the cervical prosthesis. It can also negatively impact surgical outcomes, causing postoperative neck pain, stiffness, and restricted mobility. Further research and longer-term follow-up are still needed to support the use of CDA at the C2-3 level.
We evaluated published English literature by searching EMBASE, PubMed, Medline, and Scopus. To date, only two cases of CDA at the C2-3 level have been reported. One such case, as described by Yang et al. (27), involved a 49-year-old female patient who successfully underwent non-contiguous two-level CDA at C2-3 and C5-6 using Prestige-LP artificial discs under nasal anesthesia intubation. During the 2-year postoperative follow-up period, this procedure achieved relatively satisfactory clinical outcomes. Another case involved Jason Ku et al. (28) performing contiguous three-level CDA from C2-5 using Mobi-C (Zimmer-Biomet) artificial discs in a 52-year-old male patient. Postoperatively, the range of motion at each surgical level was preserved, with satisfactory outcomes observed during follow-up. At present, it remains uncertain whether C2-3 level CDA can be applied to non-contiguous CDDD.
In this case report, we demonstrate the successful implementation of standard anterior cervical CDA at C2-3 despite the high technical challenges. Furthermore, the non-contiguous three level hybrid surgical approach combining C2-3 CDA with C4-5 and C5-6 ACDF achieved successful clinical outcomes in this patient. During the 12-month follow-up period after the surgery, the clinical and radiographic results of this case are good. Although CDA has not yet been universally accepted as the standard treatment for cervical disc herniation at the C2-3 level, it appears to represent a safe and feasible surgical option. For patients presenting with isolated C2-3 disc herniation who maintain normal neurological function and cervical lordosis, the strategic use of CDA to preserve segmental mobility is clinically justified and merits particular attention in the field of spinal surgery.
Conclusion
This case report demonstrates that CDA represents a viable alternative for managing degenerative disc disease at the C2-3 level, providing satisfactory clinical outcomes while preserving segmental mobility. This approach broadens the therapeutic spectrum beyond fusion-based techniques for high cervical disc pathology. Furthermore, the hybrid surgical strategy offers a tailored treatment option for non-contiguous cervical disc disease, enabling precise and level-specific surgical intervention.
Data availability statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by the Biomedical Ethics Review Committee of West China Hospital, Sichuan University. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
XZ: Data curation, Investigation, Writing – original draft, Resources. YL: Investigation, Supervision, Writing – review & editing. SC: Data curation, Writing – original draft. MY: Investigation, Writing – original draft. YD: Investigation, Visualization, Writing – review & editing. TW: Investigation, Supervision, Writing – review & editing. KH: Investigation, Writing – review & editing. BW: Conceptualization, Methodology, Supervision, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
CDDD, cervical degenerative disc disease; HS, hybrid surgery; ACDF, anterior cervical discectomy and fusion; CDA, cervical disc arthroplasty; OPLL, ossification of posterior longitudinal ligament; BMD, bone mineral density; IS, intermediate segment; ROM, range of motion; ASD, adjacent segment disease; ABL, anterior bone loss; HO, heterotopic ossification.
References
1. Michalopoulos GD, Bhandarkar AR, Jarrah R, Yolcu YU, Alvi MA, Ghaith AK, et al. Hybrid surgery: a comparison of early postoperative outcomes between anterior cervical discectomy and fusion and cervical disc arthroplasty. J Neurosurg Spine. (2022) 36(4):575–84. doi: 10.3171/2021.7.SPINE21478
2. Shin DA, Yi S, Yoon DH, Kim KN, Shin HC. Artificial disc replacement combined with fusion versus two-level fusion in cervical two-level disc disease. Spine. (2009) 34(11):1153–9. doi: 10.1097/BRS.0b013e31819c9d39
3. Wu TK, Wang BY, Cheng D, Rong X, Lou JG, Hong Y, et al. Clinical and radiographic features of hybrid surgery for the treatment of skip-level cervical degenerative disc disease: a minimum 24-month follow-up. J Clin Neurosci. (2017) 40:102–8. doi: 10.1016/j.jocn.2017.02.030
4. Sun XY, Zhang QM, Cao L, Wang JY, Huang J, Liu YQ, et al. Biomechanical effects of hybrid constructions in the treatment of noncontinuous cervical spondylopathy: a finite element analysis. J Orthop Surg Res. (2023) 18(1):57. doi: 10.1186/s13018-023-03537-7
5. Sun X, Huang J, Zhang Q, Cao L, Liu Y, Song Z, et al. Segment selection for fusion and artificial disc replacement in the hybrid surgical treatment of noncontiguous cervical spondylosis: a finite element analysis. Front Bioeng Biotechnol. (2024) 12:1345319. doi: 10.3389/fbioe.2024.1345319
6. Wong C-E, Hu H-T, Hsieh M-P, Huang K-Y. Optimization of three-level cervical hybrid surgery to prevent adjacent segment disease: a finite element study. Front Bioeng Biotechnol. (2020) 8:154. doi: 10.3389/fbioe.2020.00154
7. Deshmukh VR, Rekate HL, Sonntag VKH. High cervical disc herniation presenting with C-2 radiculopathy - case report and review of the literature. J Neurosurg. (2004) 100(3):303–6. doi: 10.3171/spi.2004.100.3.0303
8. Ge CY, Hao DJ, He BR, Mi BB. Anterior cervical discectomy and fusion versus posterior fixation and fusion of C2-3 for unstable Hangman’s fracture. J Spinal Disord Tech. (2015) 28(2):E61–6. doi: 10.1097/BSD.0000000000000150
9. Salunke P, Karthigeyan M, Sahoo SK, Prasad PK. Multiplanar realignment for unstable Hangman’s fracture with posterior C2-3 fusion: a prospective series. Clin Neurol Neurosurg. (2018) 169:133–8. doi: 10.1016/j.clineuro.2018.03.024
10. Youssef JA, Heiner AD, Montgomery JR, Tender GC, Lorio MP, Morreale JM, et al. Outcomes of posterior cervical fusion and decompression: a systematic review and meta-analysis. Spine J. (2019) 19(10):1714–29. doi: 10.1016/j.spinee.2019.04.019
11. Finn MA, MacDonald JD. C2-C3 anterior cervical fusion technical report. Clin Spine Surg. (2016) 29(10):E536–41. doi: 10.1097/BSD.0b013e318292b3ca
12. Kotil K, Sengoz A. The management in the C2-C3 disc herniations: a clinical study. Turk Neurosurg. (2011) 21(1):15–21. PMID: 21294086
13. Anderst WJ, Donaldson WF, Lee JY, Kang JD. Three-dimensional intervertebral kinematics in the healthy young adult cervical spine during dynamic functional loading. J Biomech. (2015) 48(7):1286–93. doi: 10.1016/j.jbiomech.2015.02.049
14. Singh DK, Shankar D, Singh RK, Kaif M, Yadav K. C2/3 transfacetal fixation: an underutilized technique of C2 fixation in the management of atlantoaxial dislocation - a technical note with review of literature. J Craniovert Junction Spine. (2022) 13(1):4–8. doi: 10.4103/jcvjs.jcvjs_135_21
15. Hadley MN, Spetzler RF, Sonntag VKH. The transoral approach to the superior cervical-spine - a review of 53 cases of extradural cervicomedullary compression. J Neurosurg. (1989) 71(1):16–23. doi: 10.3171/jns.1989.71.1.0016
16. Türe U, Güclü B, Naderi S. Anterolateral extradural approach for C2-C3 disc herniation:: technical case report. Neurosurg Rev. (2008) 31(1):117–21. doi: 10.1007/s10143-007-0095-3
17. Russo A, Albanese E, Quiroga M, Ulm AJ. Submandibular approach to the C2-3 disc level: microsurgical anatomy with clinical application laboratory investigation. J Neurosurg Spine. (2009) 10(4):380–9. doi: 10.3171/2008.12.SPINE08281
18. Spurgas MP, Entezami P, Thomas J, DiRisio DJ. Long segment anterior cervical discectomy and fusion, including C2 surgical pearls and review of our experience. Clin Spine Surg. (2022) 35(1):E13–8. doi: 10.1097/BSD.0000000000001245
19. Park SA, Lee JH, Nam YS, An X, Han SH, Ha KY. Topographical anatomy of the anterior cervical approach for c2-3 level. Eur Spine J. (2013) 22(7):1497–503. doi: 10.1007/s00586-013-2713-9
20. Paek S, Zelenty WD, Dodo Y, Sarin M, Shue J, Soffin EM, et al. Up to 10-year surveillance comparison of survivability in single-level cervical disc replacement versus anterior cervical discectomy and fusion in New York. J Neurosurg Spine. (2023) 39(2):206–15. doi: 10.3171/2023.3.SPINE221377
21. Singh M, Balmaceno-Criss M, Anderson G, Parhar K, Daher M, Gregorczyk J, et al. Anterior cervical discectomy and fusion versus cervical disc arthroplasty: an epidemiological review of 433,660 surgical patients from 2011 to 2021. Spine J. (2024) 24(8):1342–51. doi: 10.1016/j.spinee.2024.02.016
22. Huang KK, Wang Q, Rong X, Wu TK, Ding C, Meng Y, et al. Biomechanical effects on the prostheses and vertebrae of three-level hybrid surgery: a finite element study. Orthop Surg. (2024) 16(8):2019–29. doi: 10.1111/os.14125
23. Hey HWD, Hong CC, Long AS, Hee HT. Is hybrid surgery of the cervical spine a good balance between fusion and arthroplasty? Pilot results from a single surgeon series. Eur Spine J. (2013) 22(1):116–22. doi: 10.1007/s00586-012-2486-6
24. Tabanli A, Eren TK. Comparison of fusion, arthroplasty and hybrid surgery outcomes in patients with two-level cervical disc disease. Joint Dis Relat Surg. (2024) 35(3):596–602. doi: 10.52312/jdrs.2024.1663
25. Wu T, Liu H, Wang B, He J, Ding C, Rong X, et al. Incidence of bone loss after prestige-LP cervical disc arthroplasty: a single-center retrospective study of 396 cases. Spine J. (2020) 20(8):1219–28. doi: 10.1016/j.spinee.2020.05.102
26. Tabanli A, Akcay E, Yilmaz H, Ak C, Bologur O, Kayikci E. Comparison of the outcomes of anterior cervical discectomy and fusion and cervical disc replacement for cervical disc disease. J Coll Physicians Surg Pak. (2024) 34(5):551–5. doi: 10.29271/jcpsp.2024.05.551
27. Yang Y, Yang MY, Wu S, Hong Y, Ma LT, Wang BY, et al. Two-year follow-up results of C2/3 prestige-LP cervical disc replacement: first report. Int J Clin Exp Med. (2016) 9(4):7349–53.
Keywords: hybrid surgery (HS), cervical disc arthroplasty (CDA), anterior cervical discectomy and fusion (ACDF), C2-3, non-contiguous three-level
Citation: Zhao X, Li Y, Chen S, Yao M, Deng Y, Wu T, Huang K and Wang B (2025) Non-contiguous three-level hybrid surgery with C2-3 cervical disc arthroplasty: a case report and literature review. Front. Surg. 12:1706862. doi: 10.3389/fsurg.2025.1706862
Received: 16 September 2025; Revised: 1 November 2025;
Accepted: 12 November 2025;
Published: 2 December 2025.
Edited by:
Sidong Yang, Hebei International Joint Research Centre for Spinal Diseases, ChinaReviewed by:
Piotr Yablonskii, St-Petersburg Research Institute of Phthisiopulmonology, RussiaAlper Tabanli, Tınaztepe University, Türkiye
Copyright: © 2025 Zhao, Li, Chen, Yao, Deng, Wu, Huang and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Beiyu Wang, ZG92ZS1iYWtlckAxNjMuY29t
 Xiaoqiang Zhao
Xiaoqiang Zhao Yaling Li2,3
Yaling Li2,3 Beiyu Wang
Beiyu Wang