- 1Department of Surgery, Bellinzona e Valli Regional Hospital, EOC, Bellinzona, Switzerland
- 2Faculty of Biomedical Sciences, Università Della Svizzera Italiana, Lugano, Switzerland
Background: The use of robotic surgery for combined abdominal wall hernias, including multiquadrant hernias, is underexplored in the literature. While the prevalence of simultaneous hernias is not well documented, they represent a frequent clinical challenge.
Aims: This study aimed to evaluate the feasibility of a robotic approach for treating simultaneous epigastric, umbilical, incisional, and inguinal hernias.
Materials and Methods: We retrospectively reviewed a prospectively maintained dataset of abdominal wall hernias to identify patients treated for combined hernias (i.e., incisional/umbilical/epigastric and inguinal). Patients were divided into two groups based on the robotic docking technique, and the data were analyzed.
Results: From January 2020 to December 2024, 30 patients underwent robotic combined hernia repair. Ninety percent were male, with a median age of 64.0 years (56.3–73.3). Most patients (56.7%) had an ASA score of 2. Single docking was feasible for 9 of 30 patients with midline hernias with median diameter of 2.0 cm (1.6–3.0) combined with an unilateral inguinal hernia. Double docking was necessary for 70% of patients with wider midline hernia defect with median diameter of 3.0 cm (2.0–5.0) or bilateral inguinal hernias. No intraoperative complications or conversions were reported. The median operative time was 158.0 min (141.0–160.0) for the single docking and 238.0 min (178.0–268.8) for the double docking and the median hospital stay was 2.0 days (2.0–2.0) for the single docking and 3.0 days (2.0–3.0) for the double docking. The morbidity rate was 11.1% for the single docking and 23.8% for the double docking, only one reintervention was needed in the double docking group. Most of the complications in both groups were seromas or hematomas, managed conservatively. At a median follow-up of 15.6 months (6.6–30.4), no recurrences were observed.
Conclusions: Robotic combined hernia repair is a safe and effective minimally invasive option. Single docking offers advantages but is limited to patients with midline defects combined with unilateral inguinal hernias. For midline defects combined with bilateral inguinal hernias, double docking is generally required.
Introduction
The surgical treatment of combined abdominal wall hernias, such as multisite hernias, remains underexplored, particularly with the use of robotic surgery. The multiquadrant robotic approach is gaining interest due to its ability to address multiple abdominal regions with a minimally invasive technique (1). However, this approach of reconstruction in simultaneous repair of epigastric, umbilical, incisional and inguinal hernias remains underdescribed in the literature (2, 3).
Abdominal wall hernias are common, affecting 4% of adults over 45 years old and 1.7% of the general population (4). Inguinal hernias account for over 75% of cases, while incisional hernias occur in 12.8% 2 years after a midline incision (5). Umbilical hernias are common and may be present in up to 25% of the population (6, 7). The incidence of combined hernias, involving multiple types in a single patient, remains poorly understood.
Currently, there are no large series or clear guidelines in the literature regarding the treatment of multisite combined hernias. The choice of surgical approach—open or laparoscopic—largely depends on the individual surgeon's experience, as evidence comparing thetechniques for this specific condition is lacking.
The evolution of hernia repair techniques has enabled a tailored approach for each patient. Surgeons can now address multiple defects, even in different anatomical sites, within a single surgical session. This strategy aims to reduce overall recovery time while ensuring effective repair.
This study aims to analyze the benefits of robotic surgery in the multiquadrant approach for the simultaneous repair of epigastric, umbilical, incisional, and inguinal mono and bilateral hernias, focusing on perioperative outcomes providing technical details to simplify combined robotic hernia repair.
Material and methods
At our institution, which is a specialized referral center for minimally invasive abdominal wall surgery, we retrospectively searched from a prospectively maintained and audited database patients who underwent robotic-assisted surgery for multisite hernias (https://www.herniamed.de). The search was carried out from January 2020 to December 2024. We excluded patients operated with laparoscopy or open surgery and those not agreeing to participate to the study. Both primary and recurrent hernias were included. The primary endpoint was to assess safety and feasibility of the multisite hernia treatment as new concept of care for combined abdominal wall hernias.
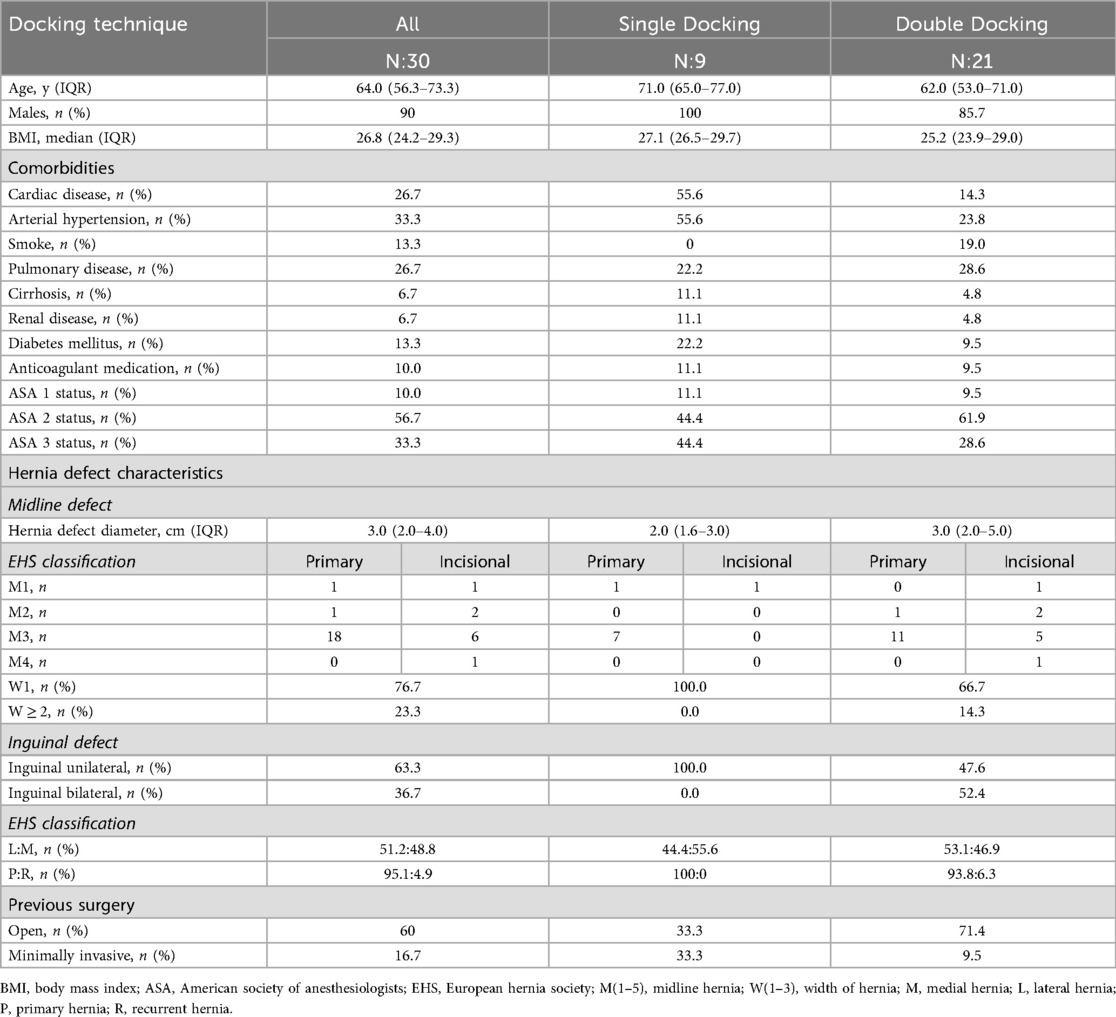
We retrieved data on age, sex, height, weight, body mass index (BMI), presence of comorbidities (cardiac disease, arterial hypertension, smoking status, pulmonary disease, cirrhosis, renal disease, diabetes mellitus, anticoagulant medication), American Society of Anesthesia (ASA) score, previous abdominal surgery, type of surgical approach [i.e., extended totally extraperitoneal repair (eTEP) lateral or sovrapubic approach; extended transabdominal preperitoneal repair (eTAPP); single docking and double docking], type of hernia, hernia defect size and other hernia characteristics (location, primary, recurrent) according to EHS classification (8), type, dimension and number of implanted mesh, time of surgery, intraoperative complications and postoperative complications according to the Clavien-Dindo classification (9) and hospital length of stay (LOS). The follow-up included a clinical assessment 30 days after surgery and subsequently annually for up to five years post the hernia operation.
All operations were performed with the da Vinci Xi® platform. The surgical technique rTAPP for inguinal hernia and the eTEP approach for midline primary or incisional defects were already described in previous publications of our research group (10–13). In case of unilateral inguinal hernia combined with a midline primary or incisional hernia with small defect size (<4 cm) the lateral single docking technique was used, instead for the bilateral inguinal hernias and wider midline hernia defects the double docking technique was adopted.
The dissection plane is primarily preperitoneal whenever feasible, particularly for small to medium-sized primary defects. In contrast, a retromuscular approach is preferred for larger and incisional hernias. Each procedure is carefully tailored according to the defect characteristics, their anatomical location, and the combination of multiple defects. Furthermore, patient-specific factors such as prior surgical history, age, quality of life, and activity level play a critical role in surgical planning. Due to the complexity often associated with multiple hernias, advanced imaging studies are frequently recommended to enable precise preoperative assessment and optimal operative strategy.
The study was approved by the local ethic committee (Comitato Etico Cantonale Ticino, 2019–01132 CE 3495), and informed consent was obtained from included patients. This research was conducted in accordance with current international regulations. Strengthening the reporting of observational studies in epidemiology (STROBE) guidelines were followed (14).
Statistical analysis
Descriptive statistics were presented as absolute frequencies for categorical variables and median with interquartile range (IQR) for continuous variables. All analyses were performed using MedCalc Statistical Software version 19.5.3 (MedCalc Software Ltd, Ostend, Belgium; https://www.medcalc.org; 2020).
Results
During the study period, 30 patients who underwent multisite combined hernia repair were retrieved. Median age was 64.0 years (56.3–73.3), 27 patients were male (90%), median BMI was 26.8 kg/m2 (24.2–29.3) and most patients (56.7%) were classified ASA II.
The three most frequent comorbidities were arterial hypertension (33.3%), cardiac (26.7%) and pulmonary diseases (26.7%). Other comorbidities included diabetes mellitus (13.3%), smoking (13.3%), cirrhosis (6.7%) and renal disease (6.7%).
Concerning the hernia defect characteristics, the epigastric, umbilical and incisional hernias were grouped in W1 and W2–3 and in M1–5, according to the EHS Classification (8). The inguinal hernias were divided into unilateral and bilateral and, according to the EHS Classification, in lateral vs. medial and primary vs. recurrent hernias (15). The majority of hernias were primary defects in both groups, to be accurate, 66.7% of midline hernias and 95.1% of inguinal hernias. Specifically, 88.9% of midline hernias in the single docking and 57.1% in the double docking, 100% of inguinal hernias in the single docking and 93.8% in the double docking were primary defects. The midline hernia defects were divided in epigastric, umbilical and incisional hernias. The epigastric hernia covered in the single docking and in the double docking 11.1% and 9.5% respectively; umbilical hernias 77.8% and 47.6% respectively and incisional hernias 11.1% and 42.9% respectively. Hernia defect diameter of midline hernias was calculated.
Single docking was feasible for 9 of 30 patients with W1 midline hernias with median defect diameter of 2.0 cm (1.6–3.0) combined with an unilateral inguinal hernia. All epigastric (11.1%), umbilical (77.8%) and incisional (11.1%) hernias were W1 in the single docking and the majority were M3. The inguinal hernias in the single docking were all unilateral and primary hernias, of which 55.5% were medial hernias.
Double docking was necessary for 70% of patients with wider (W1–3) midline hernia defect, mean defect diameter of 3.0 cm (2.0–5.0) or bilateral inguinal hernias. The epigastric (9.5%), umbilical (47.6%) and incisional (42.9%) hernias in the double docking were mostly W1 (66.7%) and M3 (76.2%). The inguinal hernias in the double docking were mostly bilateral (52.4%), primary (93.8%) and lateral (53.1%) hernias.
We analyzed if patients underwent previous surgeries and the type of surgeries they experienced, 33.3% of patients in the single docking and 71.4% of patients in the double docking underwent open surgery and 33.3% in the single docking and 9.5% in the double docking experienced minimally invasive surgery. All details about patients demographics and preoperative parameters are reported in Table 1.
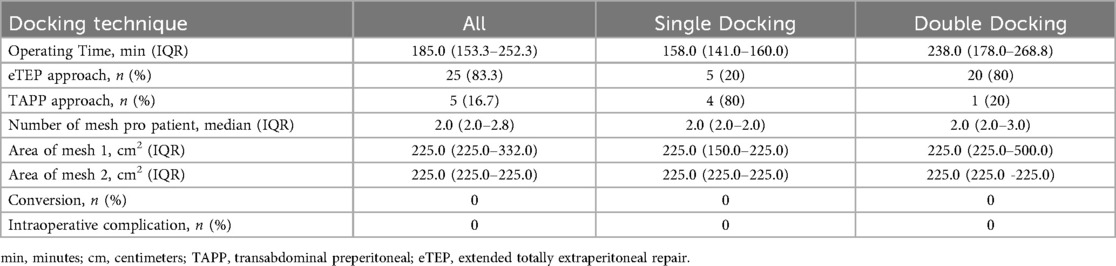
Regarding the intraoperative results, no complications or conversions were reported. When analyzing the surgical technique, the eTEP approach was predominantly used, accounting for 25 cases (83.3%). Among these, 20 cases (80%) belonged to the double docking group. In contrast, the TAPP approach was performed in 5 cases (16.7%), with 4 cases (80%) allocated to the single docking group.
The median operative time was 158.0 min (141.0–160.0) for the single docking and 238.0 min (178.0–268.8) for the double docking. The median number of mesh used for each patient was 2.0 (2.0–2.0) in the single docking and 2.0 (2.0–3.0) in the double docking. The median area of the mesh number 1 was 225.0 cm2 (150.0–225.0) and of mesh number 2 was 225.0 cm2 (225.0–225.0) in the single docking, in the double docking the median area of mesh number 1 was 225.0 cm2 (225.0–500.0) and of mesh number 2 was 225.0 cm2 (225.0–225.0). Intraoperative parameters are summarized in Table 2.
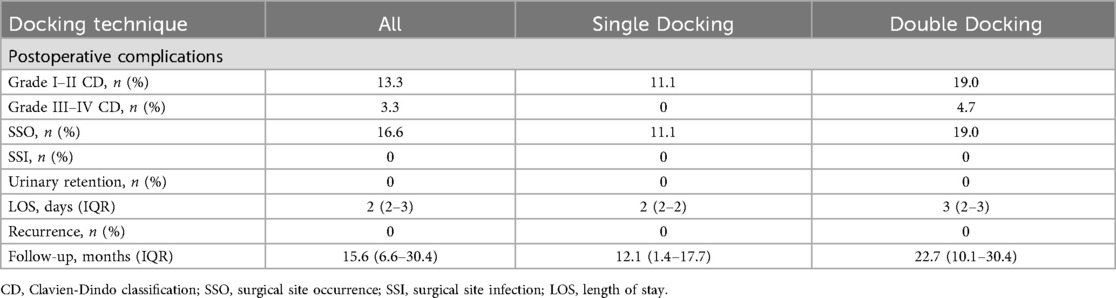
The morbidity rate was 11.1% for the single docking, all of which were classified Grade I-II according the Clavien-Dindo Classification and 23.8% for the double docking, only with one reintervention needed to treat a bleeding due to a preperitoneal hematoma in the double docking group, which was classified CD Grade ≥ IIIb. All except one of the complications in both groups were surgical site occurrences, 11.1% in the single docking and 19.0% in the double docking, managed conservatively. One patient had postoperative ileus CD Grade II. No surgical site infections occurred. As for urinary retention, no case was reported in neither of the groups. The median hospital stay was 2 days (2–2) for the single docking and 3 days (2–3) for the double docking.
After surgery patients were followed up at one month and then after one year. In all our series, at a median follow-up of 15.6 months (6.6–30.4), 12.1 months (1.4–17.7) for the single docking and 22.7 months (10.1–30.4) for the double docking, no recurrences were observed. Postoperative parameters and follow up details are described in Table 3.
Discussion
In our experience, robotic multisite hernia repair can be a safe and effective minimally invasive option.
Despite the existing skepticism concerning its usefulness, robotic surgery is gaining interest as an alternative approach for hernia repair. Indeed, some arguments in favor of robots, such as the feasibility of suturing instead of tacking to fix the mesh or the better surgeon ergonomics, appear undebatable (16).
The robotic approach in the simultaneous repair of multiquadrant hernias remains underexplored in the literature. In a recent case series, Anoldo et al. described their dual docking technique for repair of simultaneous inguinal and umbilical hernia (2). So far, more authors have dealt with the multiquadrant robotic approach in the treatment of colorectal cancer (17–20). Thanks to its robotic arms technology and integrated table motion, the da Vinci Xi system (Intuitive Surgical, Sunnyvale, CA) empowers the surgeon to carry on multiquadrant procedures. Our study shows encouraging results in terms of feasibility and safety of the robotic approach in the simultaneous treatment of epigastric, umbilical, incisional and inguinal hernias.
From a technical point of view, we found that single docking is particularly feasible in small umbilical or incisional hernias combined with a unilateral inguinal hernia, while double docking is necessary for wider W1–3 midline defect, whether primary or incisional and in case of combination with bilateral inguinal hernias. A relevant difference was observed in the distribution of surgical approaches between the two groups, with the eTEP technique predominantly adopted in the double docking group and the TAPP approach more frequently used in the single docking group. This divergence may reflect underlying differences in case complexity or surgeon preference. However, the interpretation of this finding should be approached with caution due to the limited sample size.
Switching from single to double docking has a certain relevance: as advantages of the single docking technique, a short operative time and a reduced number of trocar accesses are to mention. Arguably, the latter might be associated with lesser postoperative pain, reduced SSO risk and better cosmetic results. Of course, the operative time is mainly affected by the type and number of hernias. In our series, both docking techniques showed the multiquadrant approach to be feasible and safe, with no reported intraoperative complications and/or conversions, only minor post-operative complications and no recurrences at a median follow up time of 15.6 months.
As the benefit assessment of an intervention should be related to the patient (21), we should evaluate the robotic multisite hernia repair compared with a defined alternative treatment. Despite the lack of control group, if we assume that combined abdominal wall hernias are commonly treated through multiple procedures and repeated hospital admissions, we can see the multiquadrant robotic approach as a potentially added value to the patient. In addition, minimizing the number of hospitalization should have benefits in terms of healthcare costs.
This study has many limitations. Besides the above-mentioned lack of control group, it is based on a single surgical group's experience and a small sample size. Last but not least, our results are the consequence of a 10-year-long robotic experience using standardized procedures. A proper learning curve should be taken into account when considering starting with robotic abdominal wall surgery.
Based on our results, we can conclude that patients with simultaneous abdominal wall hernias can safely undergo minimally invasive surgery using a robotic platform, achieving favorable intra- and post-operative outcomes. These outcomes include low postoperative morbidity, such as a short hospital stay, minimal to no surgical site complications or infections, and no intraoperative conversions or post-operative recurrences.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Comitato Etico Cantonale Ticino, 2019-01132 CE 3495. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
EDC: Data curation, Investigation, Validation, Writing – original draft, Writing – review & editing. FM: Data curation, Formal analysis, Methodology, Writing – review & editing. SS: Conceptualization, Validation, Writing – review & editing. DL: Validation, Writing – review & editing, Investigation, Supervision, Visualization, Writing – original draft. FG: Supervision, Validation, Writing – review & editing. FI: Writing – review & editing. RP: Conceptualization, Project administration, Writing – review & editing. JT: Conceptualization, Project administration, Supervision, Validation, Writing – original draft, Writing – review & editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Abbreviations
ASA, American society of anesthesia; eTEP, extended totally extraperitoneal repair; eTAPP, extended transabdominal preperitoneal repair; rTAPP, robotic rransabdominal preperitoneal repair; BMI, body mass index; EHS, European hernia society; CD, Clavien-Dindo classification; LOS, hospital length of stay; IQR, interquartile range; W (1–3), width of hernia; M (1–5), midline hernia; SSO, surgical site occurrences.
References
1. Bianchi G, Gavriilidis P, Martinez-Perez A, de'Angelis GL, Uzzan M, Sobhani I, et al. Robotic multiquadrant colorectal procedures: a single-center experience and a systematic review of the literature. Front Surg. (2022) 9:991704. doi: 10.3389/fsurg.2022.991704
2. Anoldo P, Manigrasso M, D'Amore A, Musella M, De Palma GD, Milone M. Dual docking technique for robotic repair of simultaneous inguinal and umbilical hernia: a preliminary single center experience. Int J Med Robot. (2023) 20:e2586. doi: 10.1002/rcs.2586
3. Kudsi OY, Kaoukabani G, Bou-Ayash N, Gokcal F. Robotic ventral hernia repair and concomitant procedures: mid-term outcomes and risk factors associated with postoperative complications. Surg Laparosc Endosc Percutan Tech. (2023) 33(1):27–30. doi: 10.1097/SLE.0000000000001140
4. Jenkins JT, O'Dwyer PJ. Inguinal hernias. Br Med J. (2008) 336(7638):269–72. doi: 10.1136/bmj.39450.428275.AD
5. Bosanquet DC, Ansell J, Abdelrahman T, Cornish J, Harries R, Stimpson A, et al. Systematic review and meta-regression of factors affecting midline incisional hernia rates: analysis of 14,618 patients. PLoS One. (2015) 10(9):e0138745. doi: 10.1371/journal.pone.0138745
6. Burcharth J, Pedersen MS, Pommergaard HC, Bisgaard T, Pedersen CB, Rosenberg J. The prevalence of umbilical and epigastric hernia repair: a nationwide epidemiologic study. Hernia. (2015) 19(5):815–9. doi: 10.1007/s10029-015-1376-3
7. Bedewi MA, El-Sharkawy MS, Al Boukai AA, Al-Nakshabandi N. Prevalence of adult paraumbilical hernia. assessment by high-resolution sonography: a hospital-based study. Hernia. (2012) 16(1):59–62. doi: 10.1007/s10029-011-0863-4
8. Muysoms FE, Miserez M, Berrevoet F, Campanelli G, Champault GG, Chelala E, et al. Classification of primary and incisional abdominal wall hernias. Hernia. (2009) 13(4):407–14. doi: 10.1007/s10029-009-0518-x
9. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. (2004) 240(2):205–13. doi: 10.1097/01.sla.0000133083.54934.ae
10. Pini R, Di Giuseppe M, Toti JMA, Mongelli F, Marcantonio M, Spampatti S, et al. Robot-assisted treatment of epigastric hernias with a suprapubic approach. Surg Laparosc Endosc Percutan Tech. (2021) 31(5):584–7. doi: 10.1097/SLE.0000000000000941
11. Proietti F, La Regina D, Pini R, Di Giuseppe M, Cianfarani A, Mongelli F. Learning curve of robotic-assisted transabdominal preperitoneal repair (rtapp) for inguinal hernias. Surg Endosc. (2021) 35(12):6643–9. doi: 10.1007/s00464-020-08165-4
12. Spampatti S, La Regina D, Pini R, Mongelli F, Gaffuri P, Porcellini I, et al. Three-Point mesh fixation in robot-assisted transabdominal preperitoneal (R-tapp) repair of 208 inguinal hernias: preliminary results of a single-center consecutive series. Langenbecks Arch Surg. (2022) 407(6):2555–61. 35581394
13. Pini R, Mongelli F, Iaquinandi F, Gaffuri P, Previsdomini M, Cianfarani A, et al. Switching from robotic-assisted extended transabdominal preperitoneal (etapp) to totally extraperitoneal (etep) hernia repair for umbilical and epigastric hernias. Sci Rep. (2024) 14(1):1800. doi: 10.1038/s41598-024-52165-6
14. Vandenbroucke JP, von Elm E, Altman DG, Gøtzsche PC, Mulrow CD, Pocock SJ, et al. Strengthening the reporting of observational studies in epidemiology (strobe): explanation and elaboration. PLoS Med. (2007) 4(10):e297. doi: 10.1371/journal.pmed.0040297
15. Miserez M, Alexandre JH, Campanelli G, Corcione F, Cuccurullo D, Pascual MH, et al. The European hernia society groin hernia classification: simple and easy to remember. Hernia. (2007) 11(2):113–6. doi: 10.1007/s10029-007-0198-3
16. Prabhu AS, Carbonell A, Hope W, Warren J, Higgins R, Jacob B, et al. Robotic inguinal vs transabdominal laparoscopic inguinal hernia repair: the rival randomized clinical trial. JAMA Surg. (2020) 155(5):380–7. 32186683
17. Hollandsworth HM, Stringfield S, Klepper K, Zhao B, Abbadessa B, Lopez NE, et al. Multiquadrant surgery in the robotic era: a technical description and outcomes for Da Vinci Xi robotic subtotal colectomy and total proctocolectomy. Surg Endosc. (2020) 34(11):5153–9. doi: 10.1007/s00464-020-07633-1
18. Protyniak B, Jorden J, Farmer R. Multiquadrant robotic colorectal surgery: the Da Vinci Xi vs Si comparison. J Robot Surg. (2018) 12(1):67–74. doi: 10.1007/s11701-017-0689-x
19. Scotton G, Contardo T, Zerbinati A, Tosato SM, Orsini C, Morpurgo E. From laparoscopic right colectomy with extracorporeal anastomosis to robot-assisted intracorporeal anastomosis to totally robotic right colectomy for cancer: the evolution of robotic multiquadrant abdominal surgery. J Laparoendosc Adv Surg Tech A. (2018) 28(10):1216–22. 30117748
20. Xian SH, Tan HJ, Marino MV, Thiruchelvam N, Heng AK. Review of robotic simultaneous resection of colorectal cancer with synchronous liver metastases using Da Vinci Xi: technical considerations and outcomes. Chirurgia (Bucur). (2023) 118(1):20–6. doi: 10.21614/chirurgia.2831
21. Institute for quality and efficiency in health care. General Methods [Internet] Version 4.2. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG) (2015). https://www.ncbi.nlm.nih.gov/books/NBK332872/
Keywords: multisite hernia, multiquadrant hernia, combined hernias, robotics abdominal wall surgery, docking technique
Citation: Diaz Casanova EC, Mongelli F, Spampatti S, La Regina D, Garofalo F, Iaquinandi F, Pini R and Toti JMA (2025) Multisite hernia treatment: the robotic approach makes it feasible. Front. Surg. 12:1711703. doi: 10.3389/fsurg.2025.1711703
Received: 23 September 2025; Accepted: 16 October 2025;
Published: 5 November 2025.
Edited by:
Alec Engledow, Barts Health NHS Trust, United KingdomReviewed by:
Duray Şeker, Dışkapı Yildirim Training and Research Hospital, TürkiyeVincenzo Nicastro, Niguarda Ca' Granda Hospital, Italy
Copyright: © 2025 Diaz Casanova, Mongelli, Spampatti, La Regina, Garofalo, Iaquinandi, Pini and Toti. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Johannes Maria Alberto Toti, am9oYW5uZXN0b3RpQGdtYWlsLmNvbQ==
†These authors have contributed equally to this work and share first authorship
 Eva Carmen Diaz Casanova1,†
Eva Carmen Diaz Casanova1,† Francesco Mongelli
Francesco Mongelli Davide La Regina
Davide La Regina Fabiano Iaquinandi
Fabiano Iaquinandi Johannes Maria Alberto Toti
Johannes Maria Alberto Toti