- 1Department of Applied Social Sciences, Technical University of Applied Sciences Würzburg-Schweinfurt, Würzburg, Germany
- 2Department of Media Psychology, Julius Maximilians University of Würzburg, Würzburg, Germany
Introduction: Schizophrenia imposes a significant burden on global public health and is associated with pervasive stigmatization, perpetuating misconceptions of danger and incompetence. This review examines the efficacy of simulation interventions in reducing stigmas associated with schizophrenia and fostering empathy towards affected individuals.
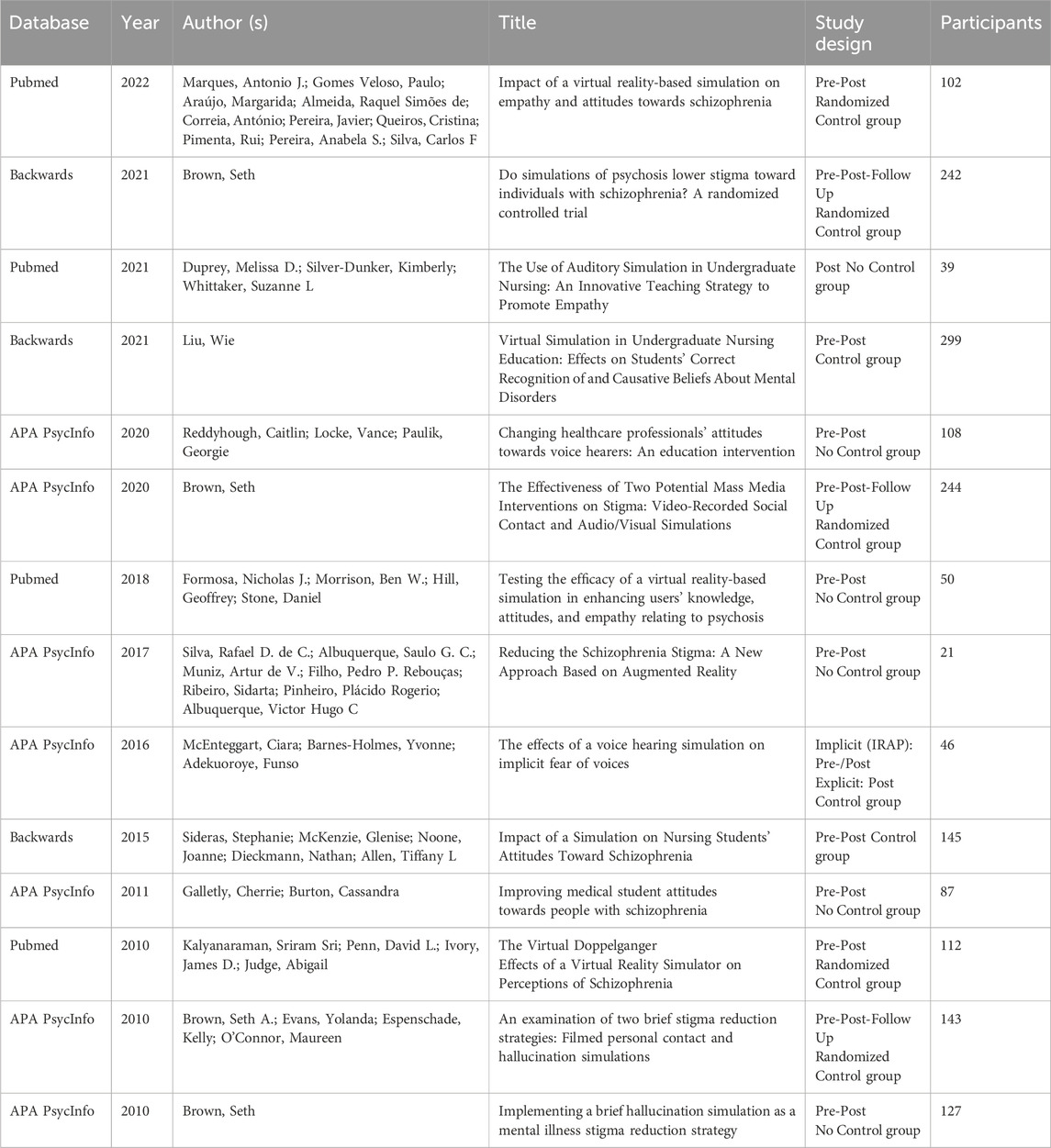
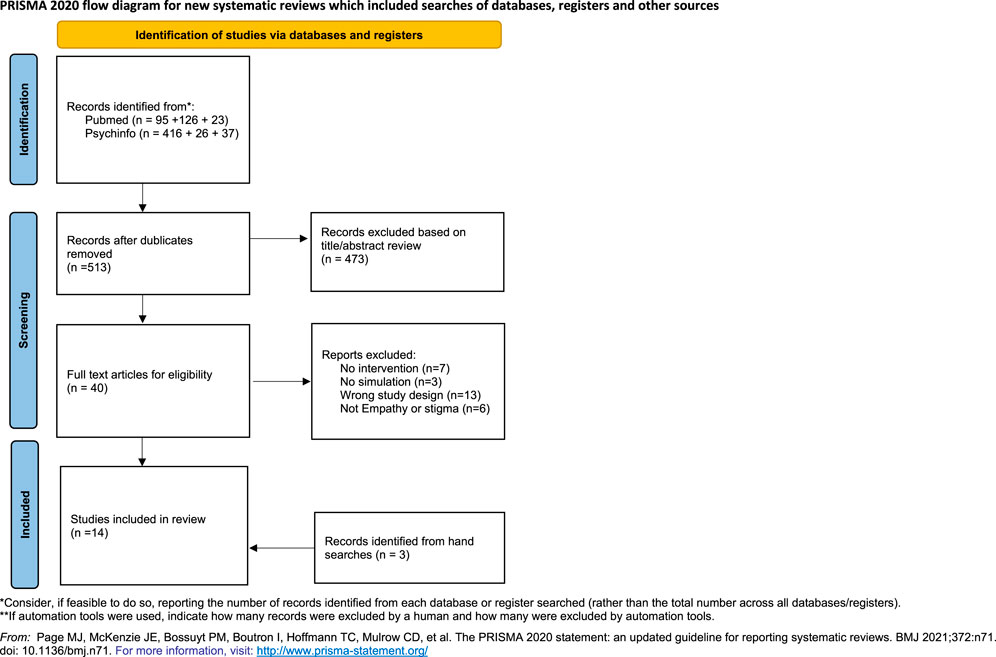
Methods: A comprehensive literature review spanning from August 2021 to September 2022 identified 14 relevant studies meeting inclusion criteria.
Results: Analysis revealed a diverse landscape of simulation-based interventions, characterized by variability in methodological rigor, intervention design, and technological modalities. While some studies demonstrated promising outcomes in stigma reduction and empathy enhancement, methodological limitations and inconsistencies underscore the need for cautious interpretation of findings. Furthermore, mixed outcomes in stigma characteristics and empathy development highlight the complexity of intervention effectiveness.
Discussion: Despite these challenges, simulation interventions, particularly when integrated with additional components, hold potential in mitigating stigmatization and promoting empathy. Future research should prioritize methodological rigor, comprehensive outcome assessment, and tailored intervention strategies to advance the field of stigma reduction in schizophrenia.
1 Introduction
Schizophrenia ranks among the 20 most prevalent causes of years lived with disabilitiy worldwide (GBD, 2021 Diseases and Injuries Collaborators, 2024). According to the World Health Organization (2022), approximately 24 million people worldwide are affected by schizophrenia. Individuals with schizophrenia face stigmatization (Vistorte et al., 2018), being perceived as particularly dangerous (Angermeyer et al., 2021; Angermeyer et al., 2013; Overton and Medina, 2008; Sheehan et al., 2017), unpredictable (Angermeyer et al., 2013), and incapable of managing their own lives (Angermeyer et al., 2013; Overton and Medina, 2008; Sheehan et al., 2017).
1.1 Definition and consequences of stigma
A stigma is defined as the connection between a personal attribute and a stereotype. It is characterised by the social devaluation of a certain attribute, which leads to extensive discrediting of the person concerned (Goffman and Huaug, 2012; Link and Phelan, 2001). Stigma is a dynamic concept influenced by societal, social, and temporal contexts (Goffman and Huaug, 2012).
Moreover, stigma includes an active element: it is accompanied by explicit or implicit discrimination, which may be evidenced, for instance, by a preference for social distance. Stigmatization procedures create a distinct separation between the stigmatized group and the non-stigmatized majority society. This establishes a binary divide between ‘we’ and ‘them’. This division illustrates a power disparity between marginalized individuals and those who impose the stigma (Link and Phelan, 2001; Rüsch et al., 2021). The stigmatization of mental illness is frequently referred to as a secondary illness and has extensive consequences for individuals impacted (Finzen, 2017).
Affected individuals not only experience stigmatization from the general public but also from healthcare professionals (Valery and Prouteau, 2020; van Dorn et al., 2005), leading to negative social and personal consequences (Baumann et al., 2003; Gaebel et al., 2004; Vistorte et al., 2018). Stigmatization not only promotes social isolation and the occurrence of other mental illnesses, but can also lead to treatment being delayed or avoided (Col et al., 2004; Gaebel et al., 2004). However, the timely initiation of treatment is essential for the therapeutic efficacy of schizophrenia (Riecher-Rössler et al., 2006).
1.2 Perspective-taking and empathy as a mechanism to reduce stigma
It is hypothesized that the initially clear separation inherent in stigma towards the stigmatized person or group can be reduced or eliminated by immersing oneself in the perspective and emotions of others (Davis et al., 1996; Yee and Bailenson, 2006). Thus, perspective-taking and empathy serve as a bridge between the two groups (Outgroup and Ingroup), potentially preventing the activation of stereotypes and excluding stigmatization as a behavioral option (Davis et al., 1996; Galinsky and Moskowitz, 2000).
Perspective-taking represents the cognitive component of empathy, allowing individuals to comprehend and assume another person’s viewpoint (Batson et al., 1997a). However, empathy goes beyond simple cognitive understanding; it encompasses an emotional aspect that enables humans to connect affectively with the experiences of others. Empathy includes both cognitive and emotional processes. The cognitive aspect pertains to mentalizing and comprehending another’s state of mind, and the affective component concerns the experience of emotions in reaction to another’s feelings, while preserving self-other difference (Batson, 2009; Blair, 2005). Empathy for an individual within the stigmatized group seems sufficient to improve stigmatizing attitudes toward the entire group (Batson et al., 2002; Batson et al., 1997b).
To comprehensively assist individuals with mental illness, psychiatric treatment should consider (self-)stigmatization and its consequences, alongside therapeutic and pharmacological interventions (Finzen, 2017; Hansson and Markström, 2014; Knaak et al., 2017; Reddyhough et al., 2021). Targeted measures by social workers, healthcare professionals, and public safety experts can contribute to dismantling stigmas against mentally ill individuals, facilitating appropriate and context-sensitive care.
1.3 Intervention approaches to reduce stigma
Studies, meta-analyses, and systematic reviews indicate the effectiveness of contact interventions and educational programs in reducing stigmatizing attitudes and the desire for social distance (Amsalem et al., 2021; Brown, 2020; Koike et al., 2018; Maunder and White, 2019; Mehta et al., 2015; Morgan et al., 2018; Rodríguez-Rivas et al., 2021; Yamaguchi et al., 2013). Whether contact occurs directly or through media seems to be less relevant, though stable long-term effects remain elusive (Mehta et al., 2015; Morgan et al., 2018).
A more recent intervention approach aims to make the lived experiences of stigmatized individuals more tangible through simulation techniques, such as experiencing homelessness (Herrera et al., 2018) or embodying an avatar with a different racial identity (Banakou et al., 2016). Studies confirm that perspective-taking and empathy development can reduce stigmatization (Batson et al., 2002; Batson et al., 1997b; Galinsky et al., 2005; Herrera et al., 2018; Koike et al., 2018; Levin et al., 2016; Tassinari et al., 2021; Yee and Bailenson, 2006).
1.4 The role of virtual reality in stigma reduction
To enhance understanding and promote perspective-taking, many studies have utilized audio or video simulations. More recently, researchers have increasingly utilized virtual reality (VR) technology to further intensify the experience and potentially improve the stability of its effects (Herrera et al., 2018).
While VR-based interventions offer a promising avenue for reducing stigma, their effects are not unequivocally positive. On one hand, VR simulations can effectively promote empathy and reduce stigmatizing attitudes by enabling individuals to experience the perspective of a stigmatized person (Banakou et al., 2016; Bertrand et al., 2018; Herrera et al., 2018; Tay et al., 2023). VR technologies intended to make perspective-taking an even more intense experience. In this context, factors such as the sense of presence, the feeling of embodiment, and the emotional intensity of the experience may determine whether stigma is reduced or reinforced (Yuen and Mak, 2021).
On the other Hand, it is noted that simulated experiences in VR can amplify the desire for social distance (Ando et al., 2011; Lee and Lin, 2017). Given that social distance is a key indicator of stigma, these findings highlight the necessity of scrutinizing the underlying mechanisms.
Research suggests that empathy, knowledge dissemination, and strong emotions such as fear and anger play a mediating role between the intervention (e.g., social contact) and the manifestation of stigmas and their components (Banakou et al., 2020; Kalyanaraman et al., 2010; Pettigrew and Tropp, 2008; White et al., 2020). Consequently, the content and visual design, regardless of the type of intervention (contact, knowledge dissemination, or simulation), appear crucial for intervention success (Rüsch and Xu, 2017; Tassinari et al., 2021). For instance, addressing the mental illness and presenting recovery options can be pivotal for intervention success (Ando et al., 2013; Baumann et al., 2003; Morgan et al., 2018; Rodríguez-Rivas et al., 2022).
Studies utilizing Virtual Reality for simulation also indicate that the adopted perspective (Outgroup vs Ingroup), the sense of presence, the feeling of embodiment, and the emotions triggered by the simulation influence whether stigmas decrease or escalate (Yuen and Mak, 2021). Consequently, researchers propose that VR simulations may yield the best results when integrated with other conventional intervention methods, such as educational programs or social contact strategies (Galletly and Burton, 2011; Kalyanaraman et al., 2010; Antonietti et al., 2001; Godat, 2007; Pan et al., 2006; Parkes et al., 2009).
The effectiveness of VR simulations appears to be contingent upon several design and user-experience factors. A high degree of presence and embodiment can enhance the impact of an intervention, while a lack of control within the simulated environment may provoke negative emotional responses such as fear or discomfort (Wan and Lam, 2019). Furthermore, although VR enables a highly controllable and manipulable intervention environment, its applicability remains limited by practical constraints. Studies indicate that VR interventions require significant technical and financial resources, and their appeal tends to be stronger among younger populations, potentially limiting their generalizability (Wan and Lam, 2019).
Due to the inconclusive results concerning the effectiveness of VR simulations in diminishing stigma, additional research is required to investigate the elements that influence their success or failure. This review offers a thorough synthesis of current research regarding the efficacy of simulation-based interventions in reducing stigma associated with individuals diagnosed with schizophrenia. Specifically, it examines the extent to which simulated hallucination contributes to stigma reduction and empathy enhancement. This review analyzes the impact of key factors—namely, the target audience, content design, and the technological modalities employed to provide hallucinations—on intervention effects. This effort aims to identify research gaps and guide the formulation of more effective intervention strategies by addressing these elements. Previous reviews have focused on general technology-based interventions, such as educational programs or media-mediated social contact. The recent review by Rodríguez-Rivas et al. (2021) examines the impact of computing technologies in alleviating stigma; however, it does not particularly focus on simulation-based methods or explore the mechanisms driving their effects. In contrast, the present review provides a more targeted analysis by concentrating exclusively on simulation-based interventions that seek to elicit perspective-taking through direct experiential engagement.
This work synthesizes research on the framework conditions, advantages, and drawbacks of various techniques, offering a comprehensive view of their potential and delineating essential concerns for future improvement. To structure the analysis, this review addresses the following research question: To what extent do simulation-based interventions, particularly virtual reality and audio or visual simulations, reduce stigma and increase empathy toward individuals with schizophrenia?
2 Methods
2.1 Registration
This systematic review was registered on OSF (https://doi.org/10.17605/OSF.IO/7NG5U) during the peer review process. Although prospective registration is preferable to enhance methodological transparency, all inclusion criteria, search strategies, and quality assessment procedures were predefined prior to study selection and data extraction. The registration was conducted to ensure long-term accessibility of the study protocol and to facilitate reproducibility.
2.2 Eligibility criteria
Eligibility criteria for the present overview were pre-established. Only quantitative studies published in English or German between January 2010 and September 2022 were included. Furthermore, only studies utilizing simulation-based intervention (e.g., VR, AR, audio/visual simulation) for stigma reduction related to schizophrenia, hallucination, or auditory experiences, or those designed to foster empathy for this specific population, were considered. No restrictions were imposed on the study population. Studies investigating participants from any background, including general public students, and healthcare professionals, were considered eligible.
2.3 Information sources and search strategy
The whole search for this review was conducted by one reviewer and spanned the period from August 2021 to September 2022. The research group acknowledges that the fact that only one person was responsible for summarizing the studies may have implications for the reliability of the synthesis process and the potential presence of biases. This constitutes a limitation of the present review.
A systematic search was conducted across the APA Psychinfo (via OVID) and Pubmed databases using various keywords. The search terms were repeatedly refined and adapted throughout the research process. A comprehensive list of search terms can be found in the Appendix. Additionally, hand searches, such as the evaluation of reference lists of key articles (e.g., previous reviews or papers) were conducted to identify further studies.
The search results were then transferred to the literature management program Citavi for comprehensive review and checking.
To enhance the comprehensiveness and validity of the search results, the AI-based literature search tool Elicit was used retrospectively as an additional validation step. This tool allowed for a post-hoc cross-check of retrieved studies to identify any overlooked relevant publications. No major discrepancies were found between the original manual search and the AI-assisted validation, supporting the robustness of the initial search strategy.
2.4 Study selection and data extraction
This review was conducted in accordance with the PRISMA guidelines (Page et al., 2021) for the selection of studies. Following the identification of relevant studies, they were managed in Citavi, with duplicates being automatically recognized and consequently excluded. Citavi was subsequently employed for the perusal of titles and abstracts, with the full texts stored and viewed within the software.
Study selection and data extraction were conducted by a single reviewer. This constitutes a limitation of the present review, as independent double-screening is recommended to reduce selection bias. To mitigate this limitation, predefined eligibility criteria were strictly applied, and ambiguous cases were discussed within the research team.
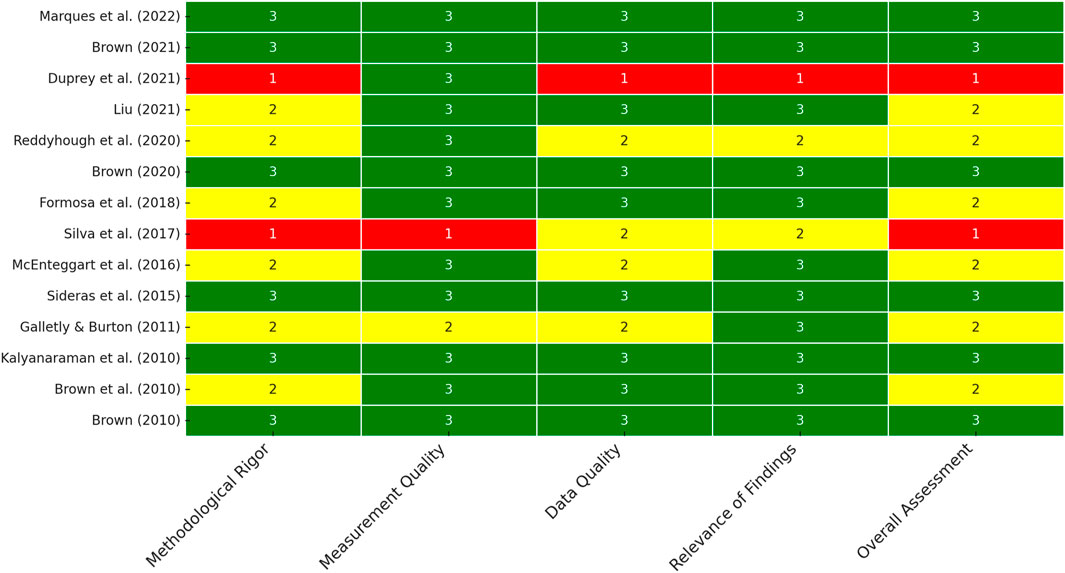
2.5 Quality assessment
The results tables (Tables 1–6) present the important information required as a basis for the quality assessment of the included studies in this review. The developed quality assessment is based on established evaluation frameworks for methodological appraisal, including the PRISMA guidelines (Page et al., 2021; Page et al., 2021), the Joanna Briggs Institute (JBI) Critical Appraisal Tools (Barker et al., 2023), the Cochrane Risk of Bias (RoB) Tool (Higgins et al., 2011), and the STROBE checklist for observational studies (Elm et al., 2007). Additionally, aspects of the COSMIN checklist (Mokkink et al., 2010) assessing the psychometric quality of measurement instruments were incorporated. By integrating these criteria, the present assessment model ensures a structured and differentiated evaluation of the methodological quality of the included studies. The quality assessment of the studies included (see Figure 1) was conducted based on four key dimensions: methodological rigor, measurement quality, data quality, and relevance of findings. Each dimension was categorized into three levels: high, medium, or low, depending on predefined criteria. The final overall assessment for each study was derived from the combined evaluation of these dimensions.
Methodological rigour was assessed based on study design, transparency of reporting and adherence to key methodological principles. Highly regarded research used a well-defined approach that included randomization, control groups and before-and-after measurements, along with clear data collection and analysis. Moderately rated studies explained their approach but had shortcomings such as lack of control groups or randomization and provided unclear or incomplete information on data collection. Low-rated studies provided few methodological details, had no control mechanisms, were based on post-intervention assessments and lacked transparency in data collection and analysis. This categorization ensures an orderly assessment of the quality of the studies.
The measurements were assessed on the basis of the validity and reliability of the instruments used. Highly rated studies used well-validated instruments with clear operationalization. Studies with average ratings sometimes used validated measurement instruments or had gaps in reliability. Poorly rated research used non-standardized or specially developed tools without explanation.
The quality of the data was assessed based on the statistical accuracy and representativeness of the sample. Highly rated studies conducted comprehensive analyses, including effect sizes and significance tests. Moderately rated studies included information on descriptive statistics but lacked detailed analyses or were based on small but interpretable samples. Poorly rated research was based on percentages, contained little statistical data or used very limited samples.
The significance of the results was determined based on the contribution of the study to research and practical application. Important studies of high quality addressed significant research gaps that have clear practical implications. Moderately rated studies provided important findings but had limited generalizability. Low-rated studies either lacked innovation or had more limited applications.
The overall assessment combines these aspects and considers advantages and disadvantages. Research with sound methodology and good measurement and data quality was rated favorably, while research with methodological weaknesses, poor data quality and limited impact was rated less favorably. This framework ensured an organized and objective assessment.
3 Results
3.1 Study characteristics
As illustrated in Figure 2, the Prisma flow diagram demonstrates that the present review encompasses a total of 14 studies.
3.2 Intervention characteristics
The current state of research on the use of simulation interventions for reducing stigmas against individuals with schizophrenia appears limited. While some randomized controlled trials with partial follow-ups have been conducted (Brown, 2010; 2020; 2021; Kalyanaraman et al., 2010; Marques et al., 2022; Sideras et al., 2015), there are also studies lacking randomization, control groups, or relying solely on post-measurements (Brown et al., 2010; Duprey et al., 2021; Formosa et al., 2018; Galletly and Burton, 2011; Liu, 2021; McEnteggart et al., 2016; Reddyhough, 2021; Silva et al., 2017). The limited number of research and occasional methodological deficiencies need cautious interpretation of the current results for their applicability to the general population.
As the majority of studies focused on healthcare professionals or trainees (such as psychologists, nurses), the current results may be insightful for this specific group. For the interpretability of the presented findings, this implies that they appear suitable for healthcare professionals, allowing inferences to be drawn regarding targeted training and continuing education opportunities for professionals in the field.
3.3 Intervention design
The duration of the interventions examined in the present studies exhibited significant variability, ranging from 3 min to 20 min for individual simulations. Combined interventions like workshops spanned from 10 min to over 4 h. Neither in the case of pure simulations nor in combined interventions could a direct influence of duration on intervention success be discerned. This indicates that longer interventions do not seem to be more beneficial or promising than shorter ones, confirming current findings (e.g., Morgan et al., 2018).
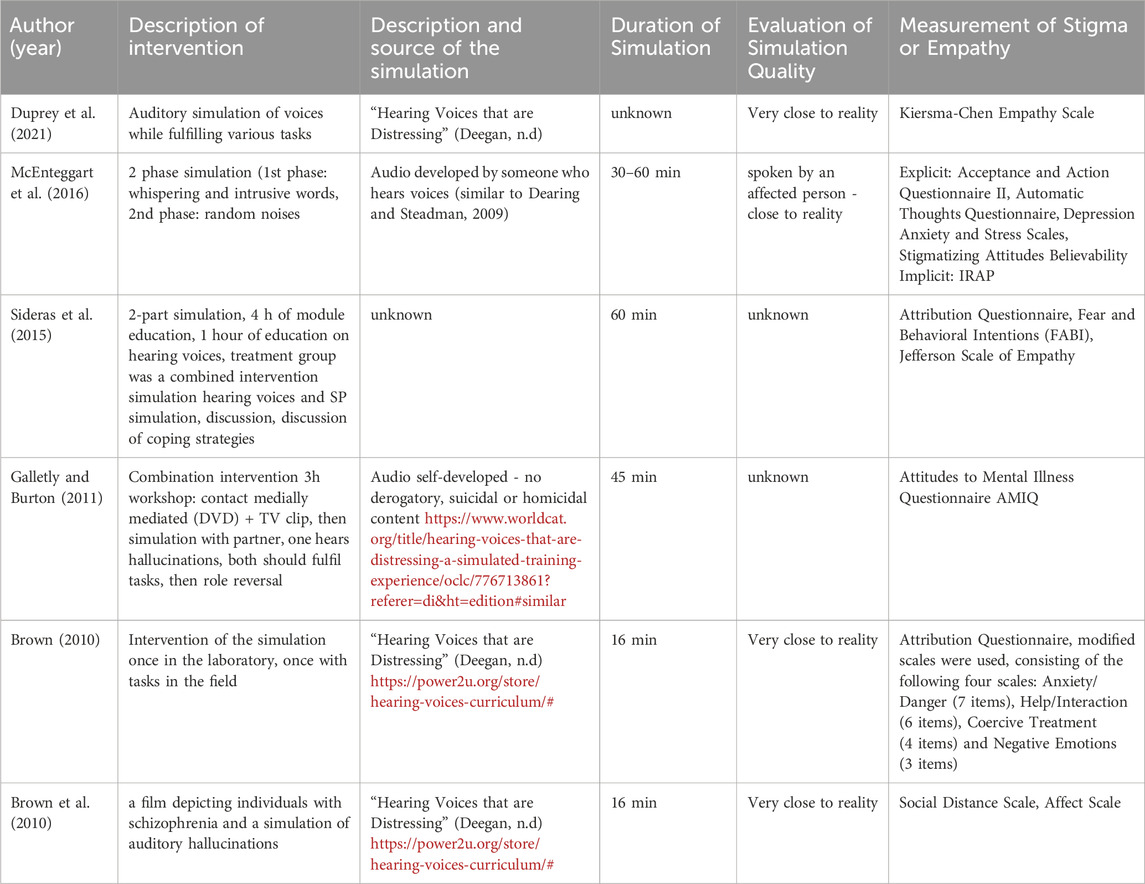
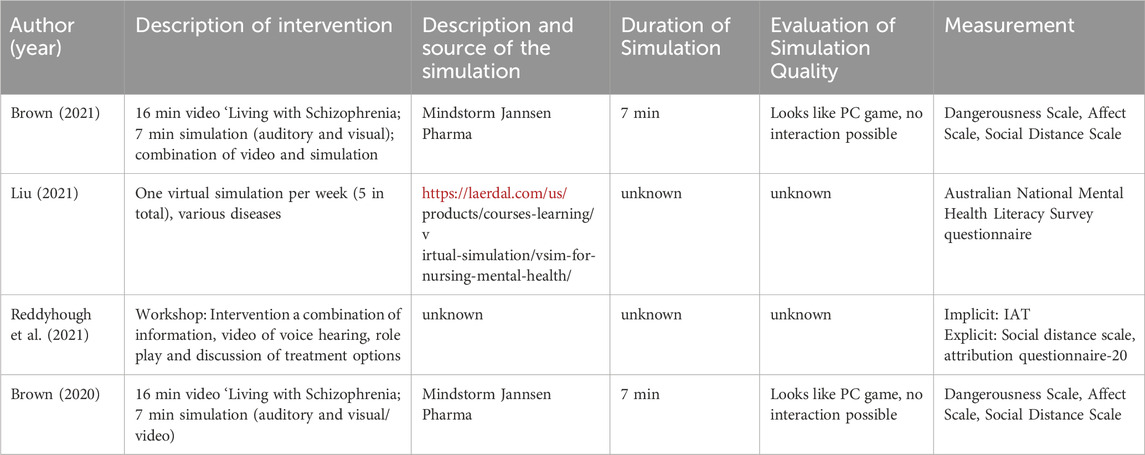
Regarding the technologies employed and, consequently, the type of simulation, there was substantial variability. Simulations were frequently presented as audio hallucinations via headphones, with a few studies also conveying visual hallucinations through video (Table 3 and 4). Occasionally, augmented reality (AR) or virtual reality (VR) applications were chosen to represent hallucinations in both visual and auditory forms (Table 2). Statements about the quality of simulations and their degree of presence were made sporadically or not at all, even though these aspects can have a significant impact on the effects. A high degree of presence may be associated with strong emotional reactions, such as fear (Diemer et al., 2015; Lombard and Ditton, 1997).
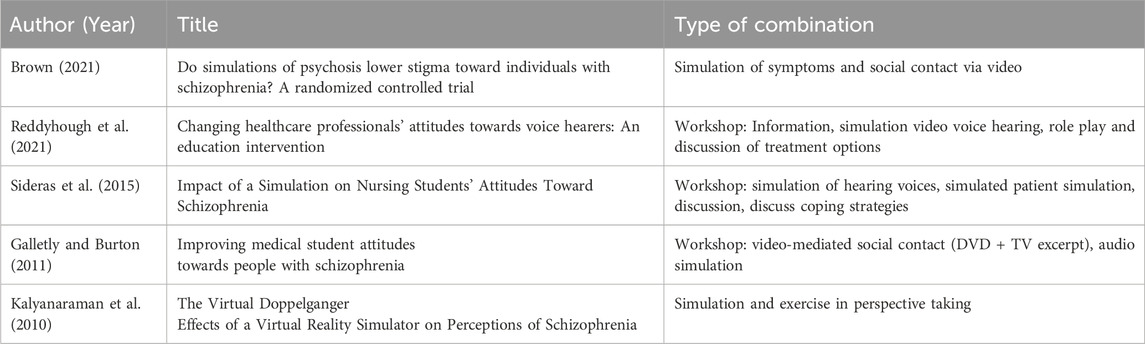
In five studies, simulation interventions were combined with additional interventions. Three investigations embedded simulation interventions in workshops that extended over several hours and included various elements (discussions, coping strategies, treatment options, information, social contact) in addition to the simulation. Combined interventions demonstrated mixed results. There positive changes in the measured stigma elements (Brown, 2021; Galletly and Burton, 2011; Kalyanaraman et al., 2010; Reddyhough, 2021; Sideras et al., 2015)), nevertheless, in certain instances or specific stigma components, no significant change was detected (Brown, 2021; Kalyanaraman et al., 2010; Reddyhough et al., 2021; Sideras et al., 2015).
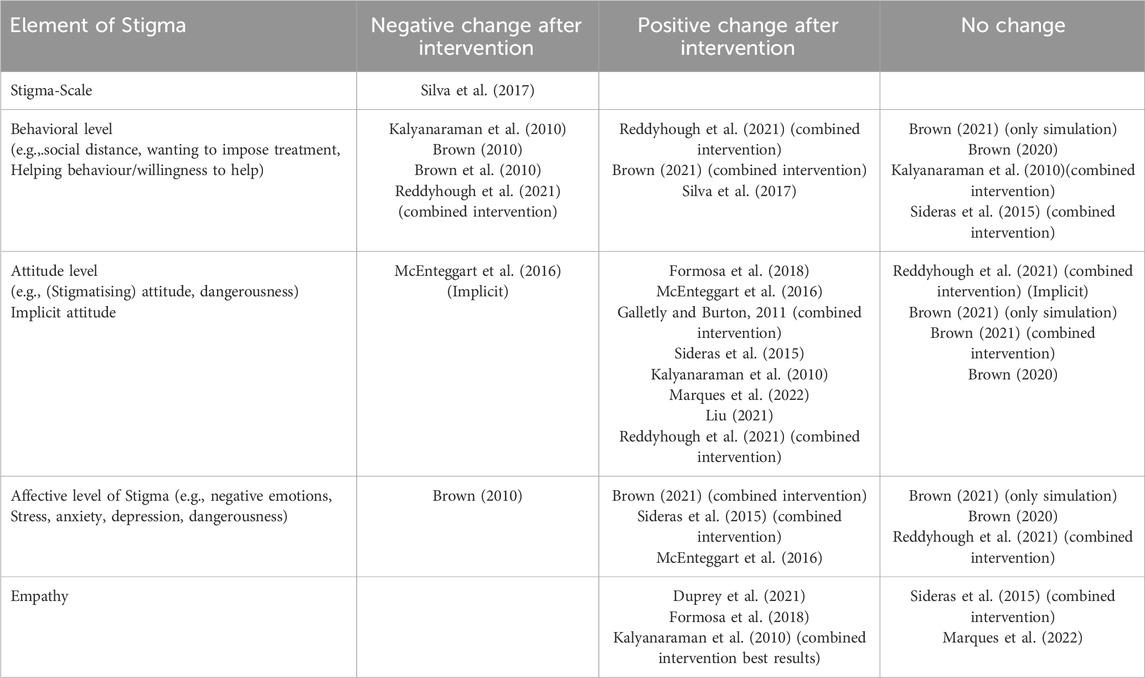
3.4 Impact on stigma characteristics
Stigma comprises multiple facets and can be assessed through features on the behavioral, attitudinal, or emotional levels. Additionally, the degree of stigmatization can be captured comprehensively through a stigma scale. Most studies focused on evaluating individual stigma characteristics. Only one study utilized an unevaluated stigma scale, thereby not concentrating on specific aspects of stigma. In this instance, a general deterioration of stigma was observed following the intervention (Silva et al., 2017).
In accordance with the categorization by Maunder and White (2019), the results are presented below with reference to the measured stigmatized characteristics.
3.5 Explicit and implicit attitudes
The stereotype that individuals with schizophrenia are dangerous was only examined in two studies. In both studies (Brown, 2020; 2021) the intervention did not show any change in the perception of danger.
Stigmatizing attitudes and attitudes towards individuals with mental illness were found to improve through simulation interventions (Formosa et al., 2018; Galletly and Burton, 2011; Kalyanaraman et al., 2010; McEnteggart et al., 2016; Sideras et al., 2015) However, an assessment of implicit attitudes by McEnteggart et al. (2016) revealed negative changes towards hearing voices after the implementation of auditory simulation. Reddyhough et al. (2021) did not observe implicit changes in their study.
3.6 Behavioral intentions and behavior
The study results regarding the desire for social distance were mixed. Simulation as a standalone intervention appeared to lead to an increase in the desire for social distance (Brown et al., 2010; Kalyanaraman et al., 2010) or remained unchanged (Brown, 2020; 2021). When the simulation was combined with another intervention, there was no change or a tendency towards a reduction in the desire for social distance, even through implicit measurements (Brown, 2021; Kalyanaraman et al., 2010; Reddyhough, 2021). The intervention’s focus on either professionals exclusively or a diverse group seems to have minimal impact on the results.
The readiness to offer assistance was investigated in merely two investigations, producing conflicting outcomes. A simulation utilizing augmented reality (AR) increased participants’ willingness to provide assistance (Silva et al., 2017). Brown (2010) reported a diminished readiness to offer aid in his study.
3.7 Affective reactions and empathy development
Both individual simulation interventions and combined interventions appeared to mitigate negative emotions towards individuals with mental illnesses (Brown, 2021; McEnteggart et al., 2016; Sideras et al., 2015). Other studies could not observe any change (Brown, 2020; Brown, 2021).
A total of five studies (Duprey et al., 2021; Formosa et al., 2018; Kalyanaraman et al., 2010; Marques et al., 2022; Sideras et al., 2015) measured empathy values of their participants before and after the intervention. In three of these works, it was demonstrated that empathy towards mentally ill individuals could be enhanced through the simulation of hallucinations. In most studies, participants were healthcare professionals in training. Kalyanaraman et al. (2010) also tested a combined intervention, yielding the most favorable results in their experimental setup. The combined intervention by Sideras et al. (2015) and the study ob Marques et al. (2022) showed no significant changes in empathy values. Overall, the simulation of hallucinations (auditory or visual) positively influenced the development of empathy.
4 Discussion
The presented review delves into the efficacy of simulation interventions aimed at reducing stigmas associated with schizophrenia, shedding light on the potential of such interventions in fostering empathy towards individuals with mental illness.
Moreover, the current study indicates that simulation strategies aimed at mitigating stigma have garnered minimal attention thus far. Historically, antistigma initiatives have mostly concentrated on the spread of knowledge and social contact, partially through the mediation of technology (e.g., Rodríguez-Rivas et al., 2021). The present analysis encompasses simulation interventions, from audio-only simulations (auditory hallucinations) to immersive technology that can deliver both visual and auditory hallucinations. Their influence in diminishing stigma is inconsistent and occasionally paradoxical. Considering the widespread stigmatizing attitudes among healthcare workers (Baumann et al., 2003; Gaebel et al., 2004; Vistorte et al., 2018) the findings herein can serve as a foundation for advancing anti-stigma campaigns and educational training programs.
The studies analysed investigated the impact of simulation interventions on individual stigma characteristics across behavioral, attitudinal, and emotional dimensions. On the behavioral level (social distance, helping behavior), results were heterogeneous and inconclusive. Explicit measurements regarding the reduction of stigmatizing attitudes and beliefs through simulations showed positive effects, although this was not corroborated by implicit attitude measurements. Implicit attitudes were scarcely measured, severely limiting their ability to provide insights into attitude changes. Explicit statements, constrained by social desirability biases, may lack reliability. Concerning other stigma elements, the potential of virtual reality simulations was evident (Banakou et al., 2016; Peck et al., 2013; Yee and Bailenson, 2006). Effects associated with the use of simulations to promote empathy showed positive trends, as shown in prior research (Chua et al., 2021; Herrera et al., 2018; Zare-Bidaki et al., 2022). Combining simulations with other interventions (knowledge dissemination, social contact) demonstrated positive trends, with the efficacy of the non-simulation intervention seemingly influencing the outcome alongside the simulation.
Regarding the intervention design, several aspects may influence the intervention’s effectiveness. The heterogeneity in intervention design, particularly concerning duration and technological modalities, complicates the interpretation of results. Previous studies have hinted at the impact of intervention duration (Ando et al., 2011). Through virtual reality, even brief simulation frequencies appear to have a positive effect on users, while excessively prolonged simulations in a virtual environment are not recommended (Archer and Finger, 2018).
The choice of technological modalities, including audio and visual simulations, augmented reality (AR), and virtual reality (VR), further contributes to the complexity of intervention design. While audio simulations via headphones were predominant, studies employing AR or VR applications offer novel avenues for immersive experiences. However, the quality of simulations and their degree of presence, though crucial determinants of intervention efficacy, were inconsistently addressed across studies. Future research should prioritize comprehensive assessments of simulation fidelity and participant immersion to elucidate their impact on intervention outcomes definitively.
Despite the potential that VR offers, research shows that the advantage of VR simulations over pure audio simulations has not yet been recognized (Martingano et al., 2021). Influencing factors and mechanisms of action should be considered. In addition to temporal considerations, the content and creative implementation of the intervention, regardless of its type, can influence the direction and strength of the effects (Banakou and Slater, 2014; Hadjipanayi and Michael-Grigoriou, 2020; Kalyanaraman et al., 2010; Norman et al., 2017; Tassinari et al., 2021). Emphasizing the role of arousal and triggered emotions could be pivotal (Diemer et al., 2015). Virtual Reality simulations, offering a high level of presence, can elicit emotions comparable to real situations, fostering empathy (Diemer et al., 2015; Lombard and Ditton, 1997).
The mechanisms of action indicate that the simulation experience, perhaps combined with a sense of loss of control and efficacy, may evoke a sensation of immersion in the virtual realm and a corresponding detachment from the actual surroundings. The absence of cognitive coping skills may induce anxiety and avoidance behaviors (Stöber and Schwarzer, 2000). In hallucination simulations specifically, the perceived absence of control might explain the contradictory results concerning various stigma attributes, the potential enhancement of empathy on the one hand, while on the other, a persistent or even heightened social distancing. A potential rationale for the inconclusive results regarding the enhancement of empathy may be that emotional empathy, rather than cognitive empathy, is predominantly fostered (Martingano et al., 2021).
However, with regards to the mechanisms of action, it should be noted that the simulation experience, possibly coupled with a sense of lack of control and efficacy, may be accompanied by the feeling of entering into the virtual world and being cut off from the real world. The absence of cognitive strategies for coping with the situation (cognitive control) may induce fear and avoidance tendencies (Stöber and Schwarzer, 2000). The perceived lack of control, specifically during hallucination simulations, could explain the conflicting results observed in various stigma characteristics–the potential for empathy development on one hand and a tendency toward increased or unaltered social distancing on the other.
The mechanisms of action suggest that the simulation experience, potentially linked to a perceived loss of control and efficacy, may induce a sensation of immersion in the virtual world, leading to a consequent disconnection from the actual surroundings. The lack of cognitive coping skills may lead to fear and avoidance behaviors (Stöber and Schwarzer, 2000). The perceived absence of control during hallucination simulations could explain the conflicting results concerning various stigma-related attributes—specifically, unchanged or heightened social distancing contrasted with the potential enhancement of empathy. One potential explanation for the inconsistent findings regarding the enhancement of empathy may be that only emotional empathy, rather than cognitive empathy, is cultivated. (Martingano et al., 2021).
Notably, the amalgamation of simulation interventions with additional components, such as workshops or discussions, yielded mixed but generally positive results in stigma reduction. Combined interventions demonstrated favorable changes in measured stigma elements (Brown, 2021; Galletly and Burton, 2011; Reddyhough et al., 2021; Sideras et al., 2015), suggesting the potential synergistic effects of multifaceted intervention approaches. However, discrepancies in outcomes highlight the need for tailored intervention strategies informed by a nuanced understanding of target populations and contextual factors.
4.1 Risk assessment
One key observation pertains to the methodological rigor of the studies reviewed. While randomized controlled trials with partial follow-ups offer robust insights into intervention effectiveness (Brown, 2010; 2020; 2021; Kalyanaraman et al., 2010; Marques et al., 2022; Sideras et al., 2015), the presence of studies lacking rigorous experimental design raises concerns regarding the generalizability of findings. The absence of control groups, randomization, and reliance on post-measurements in some studies (Formosa et al., 2018; Galletly and Burton, 2011; Liu, 2021; McEnteggart et al., 2016; Reddyhough et al., 2021; Sideras et al., 2015; Silva et al., 2017) underscores the need for methodologically sound investigations to establish the efficacy of simulation interventions conclusively.
5 Limitations
A significant drawback of this evaluation is that both study selection and data extraction were conducted by a single reviewer. This may result in selection bias, as doubles screening is typically advised (Page et al., 2021). To alleviate the danger of selection bias, the AI-driven literature search tool Elicit was used to corroborate the preliminary search findings. The implementation of stringent set inclusion criteria and the careful documenting of all exclusion decisions sought to improve openness and consistency. Future reviews should incorporate independent double-screening to strengthen the reliability of the synthesis process. Another limitation of this review is that the OSF registration occurred during the peer review process instead of prior to data collection. Prospective registration is typically advised to mitigate selective reporting bias and improve methodological transparency. All methodological procedures, including eligibility criteria, search strategy, and risk of bias assessment, were predetermined prior to the initiation of the research selection process. The registration was undertaken to document the review process retrospectively and ensure greater accessibility and reproducibility of the research approach.
6 Implications for future research
Future simulation studies might benefit from incorporating specific content that imparts a sense of control and efficacy to participants during and after the simulation. Additionally, forthcoming research endeavors should employ enhanced, more specific measurement methods. In addition to implicit measurements, the validity of stigma reduction could be bolstered by assessing actual behavioral outcomes (Norman et al., 2017).
In conclusion, the findings of this overview article highlight both the potential of simulation interventions for fostering empathy and the current research gaps and risks associated with such interventions. Through further studies and targeted refinement of simulations, this form of intervention could evolve into a cost-effective, widely deployable, and valuable tool for the ongoing education and professional development of healthcare professionals.
Future research should prioritize methodological rigor, comprehensive assessment of intervention outcomes, and tailored intervention strategies to realize the full potential of simulation interventions in combating stigma and promoting empathy in mental health contexts.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Author contributions
E-MW: Writing – original draft, Writing – review and editing. DCU: Supervision, Writing – review and editing. FS: Supervision, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The authors declare that the publication of this article was supported by the Publication Fund of the Technical University of Applied Sciences Würzburg-Schweinfurt.
Acknowledgments
We used DeepL (DeepL GmbH, 2025) and ChatGPT (OpenAI, 2024) to improve the language of the manuscript. The authors remain responsible for the content.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Amsalem, D., Yang, L. H., Jankowski, S., Lieff, S. A., Markowitz, J. C., and Dixon, L. B. (2021). Reducing stigma toward individuals with schizophrenia using a brief video: a randomized controlled trial of young adults. Schizophr. Bull. 47 (1), 7–14. doi:10.1093/schbul/sbaa114
Ando, S., Clement, S., Barley, E., Elizabeth, A., and Thornicroft, G. (2011). The simulation of hallucinations to reduce the stigma of schizophrenia: a systematic review. Schizophrenia Res. 133 (1-3), 8–16. doi:10.1016/j.schres.2011.09.011
Ando, S., Yamaguchi, S., Aoki, Y., and Thornicroft, G. (2013). Review of mental-health-related stigma in Japan. Psychiatry Clin. Neurosci. 67 (7), 471–482. doi:10.1111/pcn.12086
Angermeyer, M. C., Grausgruber, A., Hackl, E., Moosbrugger, R., and Prandner, D. (2021). Evolution of public beliefs about schizophrenia and attitudes towards those afflicted in Austria over two decades. Soc. Psychiatry Psychiatric Epidemiol. 56 (8), 1427–1435. doi:10.1007/s00127-020-01963-0
Angermeyer, M. C., Millier, A., Rémuzat, C., Refaï, T., and Toumi, M. (2013). Attitudes and beliefs of the French public about schizophrenia and major depression: results from a vignette-based population survey. BMC Psychiatry 13, 313. doi:10.1186/1471-244X-13-313
Antonietti, A., Imperio, E., Rasi, C., and Sacco, M. (2013). Virtual reality and hypermedia in learning to use a turning lathe. J. Comput. Assist. Learn. 17 (2), 142–155. doi:10.1046/j.0266-4909.2001.00167.x
Archer, D., and Finger, K. (2018). Walking in another's virtual shoes: do 360-degree video news stories generate empathy in viewers. doi:10.7916/D8669W5C
Banakou, D., Beacco, A., Neyret, S., Blasco-Oliver, M., Seinfeld, S., and Slater, M. (2020). Virtual body ownership and its consequences for implicit racial bias are dependent on social context. R. Soc. Open Sci. 7 (12), 1–18. doi:10.1098/rsos.201848
Banakou, D., Hanumanthu, P. D., and Slater, M. (2016). Virtual embodiment of white people in a black virtual body leads to a sustained reduction in their implicit racial bias. Front. Hum. Neurosci. 10, 601. doi:10.3389/fnhum.2016.00601
Banakou, D., and Slater, M. (2014). Body ownership causes illusory self-attribution of speaking and influences subsequent real speaking. Proc. Natl. Acad. Sci. U. S. A. 111 (49), 17678–17683. doi:10.1073/pnas.1414936111
Barker, T. H., Stone, J. C., Sears, K., Klugar, M., Leonardi-Bee, J., Tufanaru, C., et al. (2023). Revising the JBI quantitative critical appraisal tools to improve their applicability: an overview of methods and the development process. JBI Evid. Synth. 21 (3), 478–493. doi:10.11124/JBIES-22-00125
Batson, C. D. (2009). “These things called empathy: eight related but distinct phenomena,” in The social neuroscience of empathy. Editors J. Decety, and W. Ickes (The MIT Press), 3–16. doi:10.7551/mitpress/9780262012973.003.0002
Batson, C. D., Chang, J., Orr, R., and Rowland, J. (2002). Empathy, attitudes, and action: can feeling for a member of a stigmatized group motivate one to help the group? Personality Soc. Psychol. Bull. 28 (12), 1656–1666. doi:10.1177/014616702237647
Batson, C. D., Early, S., and Salvarani, G. (1997a). Perspective taking: imagining how another feels versus imaging how you would feel. Personality Soc. Psychol. Bull. 23 (7), 751–758. doi:10.1177/0146167297237008
Batson, C. D., Polycarpou, M. P., Harmon-Jones, E., Imhoff, H. J., Mitchener, E. C., Bednar, L. L., et al. (1997b). Empathy and attitudes: can feeling for a member of a stigmatized group improve feelings toward the group? J. Personality Soc. Psychol. 72 (1), 105–118. doi:10.1037/0022-3514.72.1.105
Baumann, A., Zaeske, H., and Gaebel, W. (2003). Das Bild psychisch Kranker imSpielfilm: Auswirkungen auf Wissen, Einstellungen und soziale Distanz am Beispiel des Films Das weiße Rauschen. Psychiatr. Prax. 30, 372–378. doi:10.1055/s-2003-43245
Bertrand, P., Guegan, J., Robieux, L., McCall, C. A., and Zenasni, F. (2018). Learning empathy through virtual reality: multiple strategies for training empathy-related abilities using body ownership illusions in embodied virtual reality. Front. Robotics AI 5, 26. doi:10.3389/frobt.2018.00026
Blair, R. J. R. (2005). Responding to the emotions of others: dissociating forms of empathy through the study of typical and psychiatric populations. Conscious. Cognition 14 (4), 698–718. doi:10.1016/j.concog.2005.06.004
Brown, S. A. (2010). Implementing a brief hallucination simulation as a mental illness stigma reduction strategy. Community Ment. Health J. 46 (5), 500–504. doi:10.1007/s10597-009-9229-0
Brown, S. A. (2020). The effectiveness of two potential mass media interventions on stigma: video-recorded social contact and audio/visual simulations. Community Ment. Health J. 56 (3), 471–477. doi:10.1007/s10597-019-00503-8
Brown, S. A. (2021). Do simulations of psychosis lower stigma toward individuals with schizophrenia? A randomized controlled trial. Psychiatry Res. Commun. 1 (1), 100001. doi:10.1016/j.psycom.2021.100001
Brown, S. A., Evans, Y., Espenschade, K., and O'Connor, M. (2010). An examination of two brief stigma reduction strategies: filmed personal contact and hallucination simulations. Community Ment. Health J. 46 (5), 494–499. doi:10.1007/s10597-010-9309-1
Chua, J. Y. X., Ang, E., Lau, S. T. L., and Shorey, S. (2021). Effectiveness of simulation-based interventions at improving empathy among healthcare students: a systematic review and meta-analysis. Nurse Educ. Today 104, 105000. doi:10.1016/j.nedt.2021.105000
Col, C. de, Seewald, G., and Meise, U. (2004). “Individuelle Bewältigung von Stigmatisierung und Diskriminierung,” in Psychiatrische rehabilitation: mit 90 tabellen. Editors W. Rössler, and C. Lauber (Springer), 861–874.
Davis, M. H., Conklin, L., Smith, A., and Luce, C. (1996). Effect of perspective taking on the cognitive representation of persons: a merging of self and other. J. Personality Soc. Psychol. 70 (4), 713–726. doi:10.1037/0022-3514.70.4.713
Dearing, K. S., and Steadman, S. (2009). Enhancing intellectual empathy: the lived experience of voice simulation. Perspect. Psychiatric Care 45 (3), 173–182. doi:10.1111/j.1744-6163.2009.00219.x
Deegan, P. E. (n.d.). “The hearing distressing voices toolkit. Available online at:https://power2u.org/store/hearing-voices-curriculum/#
DeepL, GmbH. (2025). “DeepL Translator (Version 24.4.2) [Machine translation system]. Available online at:https://www.deepl.com/translator
Diemer, J., Alpers, G. W., Peperkorn, H. M., Shiban, Y., and Mühlberger, A. (2015). The impact of perception and presence on emotional reactions: a review of research in virtual reality. Front. Psychol. 6, 26. doi:10.3389/fpsyg.2015.00026
Duprey, M. D., Silver-Dunker, K., and Whittaker, S. L. (2021). The use of auditory simulation in undergraduate nursing: an innovative teaching strategy to promote empathy. Nurs. Educ. Perspect. 42 (6), E125–E126. doi:10.1097/01.NEP.0000000000000829
Elm, E. von, Altman, D. G., Egger, M., Pocock, S. J., Gøtzsche, P. C., Vandenbroucke, J. P., et al. (2007). The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. Lancet London, Engl. 370 (9596), 1453–1457. doi:10.1016/S0140-6736(07)61602-X
Finzen, A. (2017). “Stigma and stigmatization within and beyond psychiatry,” in The stigma of mental illness - end of the story? Editors W. Gaebel, W. Roessler, and N. Sartorius (Springer International Publishing), 29–42.
Formosa, N. J., Morrison, B. W., Hill, G., and Stone, D. (2018). Testing the efficacy of a virtual reality-based simulation in enhancing users’ knowledge, attitudes, and empathy relating to psychosis. Aust. J. Psychol. 70 (1), 57–65. doi:10.1111/ajpy.12167
Gaebel, W., Baumann, A., and Zäske, H. (2004). “Gesellschaftsrelevante Ansätze zur Überwindung von Stigma und Diskriminierung,” in Psychiatrische rehabilitation: mit 90 tabellen. Editors W. Rössler, and C. Lauber (Springer), 875–886.
Galinsky, A. D., Ku, G., and Wang, C. S. (2005). Perspective-taking and self-other overlap: fostering social bonds and facilitating social coordination. Group Process. and Intergr. Relat. 8 (2), 109–124. doi:10.1177/1368430205051060
Galinsky, A. D., and Moskowitz, G. B. (2000). Perspective-taking: decreasing stereotype expression, stereotype accessibility, and in-group favoritism. J. Personality Soc. Psychol. 78 (4), 708–724. doi:10.1037//0022-3514.78.4.708
Galletly, C., and Burton, C. (2011). Improving medical student attitudes towards people with schizophrenia. Aust. N. Z. J. Psychiatry 45 (6), 473–476. doi:10.3109/00048674.2011.541419
GBD 2021 Diseases and Injuries Collaborators Santomauro, D. F., Aali, A., Abate, Y. H., Abbafati, C., Abbastabar, H., et al. (2024). Global incidence, prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990-2021: a systematic analysis for the Global Burden of Disease Study 2021. Lancet London, Engl. 403 (10440), 2133–2161. doi:10.1016/S0140-6736(24)00757-8
Goffman, E. (2012). Stigma: Über Techniken der Bewältigung beschädigter Identität. Haug, Frigga: Taschenb. Wiss. 140.
Godat, M. (2007). Virtual golden foods corporation: generic skills in a virtual crisis environment (a pilot study). Journal of Educational Multimedia and Hypermedia, 16 (1), 67–84.
Hadjipanayi, C., and Michael-Grigoriou, D. (2020). Conceptual knowledge and sensitization on Asperger's syndrome based on the constructivist approach through virtual reality. Heliyon 6 (6), e04145. doi:10.1016/j.heliyon.2020.e04145
Hansson, L., and Markström, U. (2014). The effectiveness of an anti-stigma intervention in a basic police officer training programme: a controlled study. BMC Psychiatry 14, 55. doi:10.1186/1471-244X-14-55
Herrera, F., Bailenson, J., Weisz, E., Ogle, E., and Zaki, J. (2018). Building long-term empathy: a large-scale comparison of traditional and virtual reality perspective-taking. PloS One 13 (10), e0204494. doi:10.1371/journal.pone.0204494
Higgins, J. P. T., Altman, D. G., Gøtzsche, P. C., Jüni, P., Moher, D., Oxman, A. D., et al. (2011). The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ 343, d5928. doi:10.1136/bmj.d5928
Kalyanaraman, S. S., Penn, D. L., Ivory, J. D., and Judge, A. (2010). The virtual doppelganger: effects of a virtual reality simulator on perceptions of schizophrenia. J. Nerv. Ment. Dis. 198 (6), 437–443. doi:10.1097/NMD.0b013e3181e07d66
Knaak, S., Mantler, E., and Szeto, A. (2017). Mental illness-related stigma in healthcare: barriers to access and care and evidence-based solutions. Healthc. Manag. Forum 30 (2), 111–116. doi:10.1177/0840470416679413
Koike, S., Yamaguchi, S., Ojio, Y., Ohta, K., Shimada, T., Watanabe, K., et al. (2018). A randomised controlled trial of repeated filmed social contact on reducing mental illness-related stigma in young adults. Epidemiol. Psychiatric Sci. 27 (2), 199–208. doi:10.1017/S2045796016001050
Lee, M.-F., and Lin, C.-L. E. (2017). The effects of auditory hallucination simulation on empathy, knowledge, social distance, and attitudes toward patients with mental illness among undergraduate students: a systemic review and meta-analysis. Hu li za zhi J. Nurs. 64 (5), 59–68. doi:10.6224/JN.000069
Levin, M. E., Luoma, J. B., Vilardaga, R., Lillis, J., Nobles, R., and Hayes, S. C. (2016). Examining the role of psychological inflexibility, perspective taking, and empathic concern in generalized prejudice. J. Appl. Soc. Psychol. 46 (3), 180–191. doi:10.1111/jasp.12355
Link, B. G., and Phelan, J. C. (2001). Conceptualizing stigma. Annu. Rev. Sociol. 27, 363–385. doi:10.1146/annurev.soc.27.1.363
Liu, W. (2021). Virtual simulation in undergraduate nursing education: effects on students' correct recognition of and causative beliefs about mental disorders. Comput. Inf. Nurs. Cin. 39 (11), 616–626. doi:10.1097/CIN.0000000000000745
Lombard, M., and Ditton, T. (1997). At the heart of it all: the concept of presence. J. Computer-Mediated Commun. 3 (2), 0. doi:10.1111/j.1083-6101.1997.tb00072.x
Marques, A. J., Gomes Veloso, P., Araújo, M., Almeida, R. S. de, Correia, A., Pereira, J., et al. (2022). Impact of a virtual reality-based simulation on empathy and attitudes toward schizophrenia. Front. Psychol. 13, 814984. doi:10.3389/fpsyg.2022.814984
Martingano, A. J., Hererra, F., and Konrath, S. (2021). Virtual reality improves emotional but not cognitive empathy: a meta-analysis. Technol. Mind, Behav. 2 (1). doi:10.1037/tmb0000034
Maunder, R. D., and White, F. A. (2019). Intergroup contact and mental health stigma: a comparative effectiveness meta-analysis. Clin. Psychol. Rev. 72, 101749. doi:10.1016/j.cpr.2019.101749
McEnteggart, C., Barnes-Holmes, Y., and Adekuoroye, F. (2016). The effects of a voice hearing simulation on implicit fear of voices. J. Contextual Behav. Sci. 5 (3), 154–159. doi:10.1016/j.jcbs.2016.06.003
Mehta, N., Clement, S., Marcus, E., Stona, A.-C., Bezborodovs, N., Evans-Lacko, S., et al. (2015). Evidence for effective interventions to reduce mental health-related stigma and discrimination in the medium and long term: systematic review. Br. J. Psychiatry 207 (5), 377–384. doi:10.1192/bjp.bp.114.151944
Mokkink, L. B., Terwee, C. B., Patrick, D. L., Alonso, J., Stratford, P. W., Knol, D. L., et al. (2010). The COSMIN checklist for assessing the methodological quality of studies on measurement properties of health status measurement instruments: an international Delphi study. Qual. Life Res. An Int. J. Qual. Life Aspects Treat. Care Rehabilitation 19 (4), 539–549. doi:10.1007/s11136-010-9606-8
Morgan, A. J., Reavley, N. J., Ross, A., Too, L. S., and Jorm, A. F. (2018). Interventions to reduce stigma towards people with severe mental illness: systematic review and meta-analysis. J. Psychiatric Res. 103, 120–133. doi:10.1016/j.jpsychires.2018.05.017
Norman, R. M. G., Li, Y., Sorrentino, R., Hampson, E., and Ye, Y. (2017). The differential effects of a focus on symptoms versus recovery in reducing stigma of schizophrenia. Soc. Psychiatry Psychiatric Epidemiol. 52 (11), 1385–1394. doi:10.1007/s00127-017-1429-2
OpenAI., (2024). ChatGPT (Version GPT-4-turbo) [Large language model]. Available online at:. https://chat.openai.com/
Overton, S. L., and Medina, S. L. (2008). The stigma of mental illness. J. Couns. and Dev. (86), 143–151. doi:10.1002/j.1556-6678.2008.tb00491.x
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372, n71. doi:10.1136/bmj.n71
Pan, Z., Cheok, A. D., Yang, H., Zhu, J., and Shi, J. (2006). Virtual reality and mixed reality for virtual learning environments. Computers & Graphics, 30 (1), 20–28. doi:10.1016/j.cag.2005.10.004
Parkes, R., Forrest, N., and Baillie, S. (2009). A Mixed Reality Simulator for Feline Abdominal Palpation Training in Veterinary Medicine. In Studies in Health Technology and Informatics. Medicine Meets Virtual Reality 17. Amsterdam, The Netherlands: IOS Press. doi:10.3233/978-1-58603-964-6-244
Peck, T. C., Seinfeld, S., Aglioti, S. M., and Slater, M. (2013). Putting yourself in the skin of a black avatar reduces implicit racial bias. Conscious. Cognition 22 (3), 779–787. doi:10.1016/j.concog.2013.04.016
Pettigrew, T. F., and Tropp, L. R. (2008). How does intergroup contact reduce prejudice? Meta-analytic tests of three mediators. Eur. J. Soc. Psychol. 38 (6), 922–934. doi:10.1002/ejsp.504
Reddyhough, C. (2021). Changing healthcare professionals' attitudes towards voice hearers. Available online at: https://researchrepository.murdoch.edu.au/id/eprint/62775/1/reddyhough2021.pdf.
Reddyhough, C., Locke, V., and Paulik, G. (2021). Changing healthcare professionals' attitudes towards voice hearers: an education intervention. Community Ment. Health J. 57 (5), 960–964. doi:10.1007/s10597-020-00695-4
Riecher-Rössler, A., Gschwandtner, U., Borgwardt, S., Aston, J., Pflüger, M., and Rössler, W. [W. (2006). Early detection and treatment of schizophrenia: how early. Acta Psychiatr. Scand. 113, 73–80. doi:10.1111/j.1600-0447.2005.00722.x
Rodríguez-Rivas, M. E., Cangas, A. J., Cariola, L. A., Varela, J. J., and Valdebenito, S. (2021). Innovative technology-based interventions to reduce stigma toward people with mental illness: a systematic review and meta-analysis (preprint). doi:10.2196/preprints.35099
Rodríguez-Rivas, M. E., Cangas, A. J., Cariola, L. A., Varela, J. J., and Valdebenito, S. (2022). Innovative technology-based interventions to reduce stigma toward people with mental illness: systematic review and meta-analysis. JMIR Serious Games 10 (2), e35099. doi:10.2196/35099
Rüsch, N., Heland-Graef, M., and Berg-Peer, J. (2021). Das Stigma psychischer Erkrankung: Strategien gegen Ausgrenzung und Diskriminierung: Wissenschaftsbasiertes Sachbuch (1. Auflage). Elsevier.
Rüsch, N., and Xu, Z. (2017). “Strategies to reduce mental illness stigma,” in The stigma of mental illness - end of the story? Editors W. Gaebel, W. Roessler, and N. Sartorius (Springer International Publishing), 451–468.
Sheehan, L., Nieweglowski, K., and Corrigan, P. W. (2017). “Structures and types of stigma,” in The stigma of mental illness - end of the story? Editors W. Gaebel, W. Roessler, and N. Sartorius (Springer International Publishing), 43–66.
Sideras, S., McKenzie, G., Noone, J., Dieckmann, N., and Allen, T. L. (2015). Impact of a simulation on nursing students' attitudes toward schizophrenia. Clin. Simul. Nurs. 11 (2), 134–141. doi:10.1016/j.ecns.2014.11.005
Silva, R. D. d. C., Albuquerque, S. G. C., Muniz, A. d. V., Filho, P. P. R., Ribeiro, S., Pinheiro, P. R., et al. (2017). Reducing the schizophrenia stigma: a new approach based on augmented reality. Comput. Intell. Neurosci. 2017, 1–10. doi:10.1155/2017/2721846
Stöber, J., and Schwarzer, R. (2000). “Angst,” in Emotionspsychologie: ein Handbuch. Editor J. H. Otto (Weinheim, Beltz, Psychologie-Verlags-Union), 189–198.
Tassinari, M., Aulbach, M., and Jasinskaja-Lahti, I. (2021). The use of virtual reality in studying prejudice and its reduction: a systematic review. Available online at: https://psyarxiv.com/xrac7/.
Tay, J. L., Xie, H., and Sim, K. (2023). Effectiveness of augmented and virtual reality-based interventions in improving knowledge, attitudes, empathy and stigma regarding people with mental illnesses-A scoping review. J. Personalized Med. 13 (1), 112. doi:10.3390/jpm13010112
Valery, K.-M., and Prouteau, A. (2020). Schizophrenia stigma in mental health professionals and associated factors: a systematic review. Psychiatry Res. 290, 113068. doi:10.1016/j.psychres.2020.113068
van Dorn, R. A., Swanson, J. W., Elbogen, E. B., and Swartz, M. S. (2005). A comparison of stigmatizing attitudes toward persons with schizophrenia in four stakeholder groups: perceived likelihood of violence and desire for social distance. Psychiatry 68 (2), 152–163. doi:10.1521/psyc.2005.68.2.152
Vistorte, A. O. R., Ribeiro, W. S., Jaen, D., Jorge, M. R., Evans-Lacko, S., and Mari, J. d. J. (2018). Stigmatizing attitudes of primary care professionals towards people with mental disorders: a systematic review. Int. J. Psychiatry Med. 53 (4), 317–338. doi:10.1177/0091217418778620
Wan, W. H., and Lam, A. H. Y. (2019). The Effectiveness of virtual reality-based simulation in health professions education relating to mental illness: a literature review. Health 11 (06), S. 646–660. doi:10.4236/health.2019.116054
White, F. A., Maunder, R., and Verrelli, S. (2020). Text-based E-contact: harnessing cooperative Internet interactions to bridge the social and psychological divide. Eur. Rev. Soc. Psychol. 31 (1), 76–119. doi:10.1080/10463283.2020.1753459
World Health Organization (2022). Schizophrenia. Available online at: https://www.who.int/news-room/fact-sheets/detail/schizophrenia.
Yamaguchi, S., Wu, S.-I., Biswas, M., Yate, M., Aoki, Y., Barley, E. A., et al. (2013). Effects of short-term interventions to reduce mental health-related stigma in university or college students: a systematic review. J. Nerv. Ment. Dis. 201 (6), 490–503. doi:10.1097/NMD.0b013e31829480df
Yee, N., and Bailenson, J. (2006). “Walk a mile in digital shoes: the impact of embodied perspective-taking on the reduction of negative stereotyping in immersive virtual environments,” in Proceedings of PRESENCE 2006: the 9th annual international workshop on presence. Available online at: https://stanfordvr.com/mm/2006/yee-digital-shoes.pdf.
Yuen, A. S. Y., and Mak, W. W. S. (2021). The effects of immersive virtual reality in reducing public stigma of mental illness in the university population of Hong Kong: randomized controlled trial. J. Med. Internet Res. 23 (7), e23683. doi:10.2196/23683
Zare-Bidaki, M., Ehteshampour, A., Reisaliakbarighomi, M., Mazinani, R., Khodaie Ardakani, M. R., Mirabzadeh, A., et al. (2022). Evaluating the effects of experiencing virtual reality simulation of psychosis on mental illness stigma, empathy, and knowledge in medical students. Front. Psychiatry 13, 880331. doi:10.3389/fpsyt.2022.880331
Appendix
List of search terms:
• (Stigma* OR prejudice OR stereotype OR discrimination) AND (Virtual Reality OR 360° Video OR 3D Video OR Augmented Reality OR AR OR VR OR immersive OR media) AND reduc*
• (Stigma* Or prejudice) AND reduc* AND (mental illness OR Schizophrenia) AND (Virtual reality OR Augmented Reality OR mixed Reality OR immersive
• (((Intervention and reduc* and Stigma and Schizophrenia) or hallucination) and simulation).
• ((Stigma) AND (Simulation)) AND (intervention)
• ((((Stigma or Empathy) and Schizophrenia) or Hallucination) and Simulation
• (((((Stigma) OR (Empathy)) AND (Schizophrenia))
• (((Stigma* OR Prejudice) AND (Intervention OR reduc*)) AND (Mental ill* OR Schizophrenia)) AND (Virtual Reality OR Augmented Reality OR mixed Reality OR immersive OR Simulation)
Keywords: Schizophrenia, stigma reduction, simulation-based intervention, virtual reality, empathy, psychosis simulation, intervention, experiential learning
Citation: Weiß E-M, Unz DC and Schwab F (2025) Scoping Review on the Effects of Simulation-Based Interventions on Reducing Stigma Toward People with Schizophrenia. Front. Virtual Real. 6:1404156. doi: 10.3389/frvir.2025.1404156
Received: 20 March 2024; Accepted: 07 April 2025;
Published: 01 May 2025.
Edited by:
Lei Zhang, Kennesaw State University, United StatesReviewed by:
Diego Vilela Monteiro, ESIEA University, FranceRaquel Simões de Almeida, Polytechnic of Porto, Portugal
Copyright © 2025 Weiß, Unz and Schwab. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Eva-Maria Weiß, ZXZhLW1hcmlhLndlaXNzQHRod3MuZGU=
 Eva-Maria Weiß
Eva-Maria Weiß Dagmar C. Unz
Dagmar C. Unz Frank Schwab
Frank Schwab