- Exponent, Human Factors, Menlo Park, CA, United States
Virtual Reality (VR) technologies allow children to experience a multitude of environments and interactions; however, little is known regarding the extent to which moderate and sustained VR use impacts aspects of children’s physical and cognitive functioning. In the present research, we examine the extent to which 60-min VR play sessions over the course of 4 days impact 10- to 12-year-olds’ visual functioning (e.g., acuity, stereoacuity), visuomotor coordination (e.g., hand-eye coordination), postural stability, inhibitory control, and subjective visual and musculoskeletal discomfort (e.g., symptoms of visually-induced motion sickness). Measures of visual, physical, and cognitive functioning were administered before any VR use (day 1), after 4 days of daily VR use (day 4), and after a break from VR use (day 5). Results from this 5-day study demonstrate that moderate and daily VR usage did not negatively affect children’s visual, physical, and cognitive functioning. Overall, the present study provides novel insights into the growing body of evidence regarding the health and safety considerations surrounding VR use by children.
Introduction
Advances in virtual reality (VR) technology have allowed for the capability to create immersive, virtual experiences. This is accomplished by presenting the user with real-time, dynamic sensory input through the complex integration of hardware, computer software, and the user themselves. These advances have led to applications in various fields such as education, clinical treatment, entertainment, and gaming. A report released by Common Sense Media, a 501(c) (3) non-profit organization whose mission is to provide insights into the extent to which various media and technology is suitable for children, indicated that young people are increasingly engaging in VR technologies (Reed and Joseff, 2022). In a follow up publication by Common Sense Media, Rideout et al., 2021 reported that 17% of U.S. children aged 8–18 years live in households with VR headsets, and 22% of 8- to 12-year-olds and 27% of 13- to 18-year-olds have tried VR technologies. Given the increased availability and application of VR technology across domains, researchers have sought to understand potential health and safety effects on users, including youth (Bailey and Bailenson, 2017; Kaimara et al., 2022).
Developmental theorists have long emphasized the role of the environment as a driving factor in child development across the physical, cognitive, and psychosocial domains (Bronfrenbrenner, 1981; Piaget, 1954; Vygotsky, 1978). Recently, experts have indicated the relative importance of the “techno-subsystem,” thereby emphasizing the role technology plays in children’s developmental outcomes (Johnson and Puplampu, 2008). Children’s increasing engagement with VR technology raises questions regarding the extent to which, if at all, VR use may impact youths’ development and functioning. Based on previous research, VR use and content may influence cognitive and physical factors including visual functioning (e.g., acuity, stereoacuity), visuomotor coordination (e.g., hand-eye coordination), balance and vestibular functioning (e.g., postural stability), executive functioning (e.g., inhibitory control), and subjective visual and musculoskeletal discomfort (e.g., symptoms of visually-induced motion sickness or VIMS; Bailey and Bailenson, 2017; LaViola, 2000; Rushton and Riddell, 1999). Below, we summarize existing research regarding the impact of VR use on children’s visual, physical, and cognitive functioning.
Visual functioning
There are many metrics used to characterize vision from both a research and clinical standpoint. One of the most characterized aspects of the visual system is individuals’ ability to resolve fine spatial details, known as visual acuity. This is traditionally measured via a Snellen Eye Chart and a near-point card viewed at far and near distances for far and near acuity measurements, respectively (Snellen, 1862; de Jong, 2024). In addition to fine acuity, the visual system relies on the two eyes working together to estimate different focal distances and visually integrate depth information. Accommodation describes the eye’s ability to adjust focus for near and far stimuli by changing the shape of the lens, which is crucial for maintaining clear spatial vision at different distances. Vergence refers to the movement of both eyes in opposite directions to maintain binocular vision when shifting focus between near and distant objects. Accommodation facility and vergence facility measure how quickly and accurately the eye can perform these adjustments. Accommodation facility assesses the speed and precision with which the eye can shift focus between near and far objects, while vergence facility evaluates the efficiency of eye movements in maintaining proper alignment for clear, single vision during changes in gaze. Convergence more specifically describes when the eyes both move inward (or nasally). An example of a convergence eye movement might include how both eyes move when driving to change focus from the road (far) to then focusing on the dashboard (near). Phoria is a latent deviation of the eyes that occurs when binocular vision is disrupted, revealing the natural tendency of the eyes to drift inward, outward, upward, or downward (Kim et al., 2010; Ripps et al., 1962). These tendencies reflect the balance between the eye’s focusing ability (accommodation) and its alignment (convergence). The accommodative convergence (AC/A) ratio measures how much the eyes converge in response to a change in accommodation, indicating how eye alignment adjusts as the lens focuses on different distances. Conversely, the convergence accommodation (CA/C) ratio measures how much accommodation occurs as a result of a change in eye convergence, reflecting how the lens reshapes when the eyes move towards or away from a target (Bruce et al., 1995). These metrics are used to quantify the interaction between eye alignment and focusing effort (Bruce et al., 1995). When the visual system coordinates accommodation and vergence movements, it becomes capable of perceiving depth cues. Due to the slight horizontal separation between the eyes, each eye views an object from a slightly different angle, resulting in binocular disparity. The visual system utilizes these subtle differences in perspective to enable stereovision, allowing us to perceive the depth and three-dimensional structure of objects. Changes in each of these metrics within the context of VR can provide insights into how effectively an individual’s visual system adapts to a new visual environment.
One previous study investigated changes in visual and oculomotor functioning in 5- to 16-year-old children who viewed virtual imagery in a head-mounted device (HMD) or high-definition television (HDTV) for 30 min or 80 min (Kozulin et al., 2009). Similar visual/ocular measures were assessed at baseline, immediately after device use, and 10-min after device use. The study found that near and far visual acuity decreased significantly between baseline and immediately after 30-min of HMD use, with the decrease in near visual acuity remaining significant at 10 min post use. Furthermore, immediately after 30 min of HMD use, accommodation CA/C ratio was significantly higher and stereoacuity was significantly lower compared to baseline, suggesting increased difficulty in accommodation. However, this change was no longer significant at 10-min after device use. Near point convergence, describing the smallest distance from the center of the face to where subjects could focus both eyes on a target, decreased and was the only measure that differed significantly between baseline and 10 min post device use. After 80 min of HMD use, while there were reported changes in eye alignment, there was significant variance noted across subjects and the authors concluded that HMD use had a relatively small effect on the visual system and that such impacts were no different than those imparted from HDTV use.
Additional research has similarly found the impact of VR use on visual functioning to be minimal. In a study with 4- to 10-year-olds conducted by Tychsen and Foeller, 2020, there were no significant changes in measures of visual acuity, binocular eye alignment, or stereoacuity before and after VR use. In that study, children used a VR headset for two consecutive 30-min play sessions, and assessments were administered at baseline (before use), after the first session (post 30 min of use), and at the end of the second session (post 60 cumulative minutes of use). In another study where 10- to 12-year-olds used a VR headset for 30 min per day for five consecutive days, Rauschenberger and Barakat (2020) observed no significant changes in visual acuity, phoria, or stereoacuity across the study period. In that study, assessments were completed on day 1 prior to VR use, immediately after daily VR use on day 5, and after 24 h after VR use on day 6. The authors noted that accommodative facility improved between baseline and day 5.
Visuomotor coordination
The study by Rauschenberger and Barakat (2020) also evaluated changes in visuomotor coordination, specifically hand-eye coordination, using a near-depth and a far-depth perception task. The near-depth perception task, referred to as the skewer-straw task, required participants to place wooden skewers into randomly angled upright straws, while the far-depth perception task required participants to walk to visually identified near or far targets while blindfolded. Results showed that there were no adverse effects of daily VR use on these measures (Rauschenberger and Barakat, 2020).
Balance and vestibular functioning
To our knowledge, only two studies have examined balance and vestibular functioning in children after VR use (Rauschenberger and Barakat, 2020; Tychsen and Foeller, 2020). One study of 4- to 10-year-olds found no changes in postural stability between baseline and after 60 min of VR use (Tychsen and Foeller, 2020). Another study of 10-to-12-year-olds demonstrated that total sway was higher after five consecutive days of VR use; however, the authors noted that values were generally low compared to previous studies and suggestive of a lack of overt or practically significant impairment (Rauschenberger and Barakat, 2020).
Cognitive functioning
Notably, in the existing literature on the impact of VR on children, there is less known about the potential effects on children’s cognitive functioning, particularly in relation to executive function. Executive function refers to a set of skills or cognitive capacities that enable individuals to regulate other cognitive abilities and behaviors. Inhibitory control is a core component of executive function that refers to the ability to consciously suppress or regulate automatic, impulsive, or habitual responses. To date, no research has examined the extent to which VR use impacts children’s inhibitory control, although some have raised the notion that the way children experience immersive VR environments may relate to executive function because the salient sensory feedback in immersive VR may challenge children’s behavioral and emotional regulation (Bailey and Bailenson, 2017). However, given there is evidence of a positive association between 2D gaming and some domains of executive functioning in youth (e.g., Eng et al., 2023; Granic et al., 2014), engagement in VR gaming may also provide similar cognitive benefits. Moreover, recent work has demonstrated also that VR games provide opportunities for reducing symptoms of inattention, disorganization, and/or hyperactivity/impulsivity in children (Weerdmeester et al., 2016).
Subjective discomfort
Researchers have also investigated the extent to which VR use leads to physical discomfort. In their study with 5- to 16-year-olds, Kozulin and colleagues (2009) found that immediately after using an HMD for 30 min, symptoms related to “feeling tired,” “feeling sleepy,” “difficulty concentrating,” and “sore/aching eyes” increased from baseline measurements, but these symptoms were reduced after 10 min. Immediately after 80 min of HMD use, symptoms related to “feeling tired,” “feeling bored,” “feeling sleepy,” and “tired eyes” increased relative to baseline as well. Additionally, subjective discomfort symptoms did not differ between HMD and HDTV conditions, suggesting that HMD viewing may be as comfortable as HDTV viewing.
Similarly, in the study of 4- to-10-year-olds by Tychsen and Foeller, 2020, scores on self-reported assessments of discomfort showed an increase in general discomfort, head-neck discomfort, fatigue, and visually induced motion sickness (measured using a child-friendly version of the Simulator Sickness Questionnaire or SSQ) post-VR use relative to measurements obtained prior to any VR use. However, the authors concluded that it is doubtful that these observed increases in SSQ scores equate to meaningful physical effects given that the majority (94%) of study participants did not terminate the session and most expressed disappointment when the VR gaming session concluded (Tychsen and Foeller, 2020).
Other studies have also explored discomfort after moderate and sustained VR use. For example, in the study by Rauschenberger and Barakat (2020), the authors reported that 10- to 12-year-olds’ subjective discomfort was significantly higher on day 1 relative to day 6 (after five consecutive days of daily VR use); however, the authors note the discomfort was overall low relative to other research, suggesting that such effects were relatively minimal. In sum, the available scientific evidence suggests that both brief (i.e., single VR session lasting up to 80 min) and repeated (i.e., daily 30-min VR sessions across a 5-day period) VR use introduces some subjective discomfort among children; however, the impact appears to be mild. Any visual discomfort following HMD use by children and adolescents may be similar to visual discomfort experienced after using technological devices ubiquitous to modern life, such as 2D virtual displays (Kozulin et al., 2009).
Current study
As reviewed above, few studies have examined the impacts of VR use on children’s functioning. To date, the available scientific evidence suggests that changes in postural stability, vision, hand eye coordination, visually induced motion sickness and discomfort associated with children’s VR use may be relatively mild and clinically nonsignificant. While promising, recent developments and changes in VR technologies warrant a re-examination of the potential impacts of VR usage on children across various domains of visual, physical, and cognitive functioning. Moreover, as noted above, no research has investigated the extent to which, if at all, VR use impacts children’s inhibitory control.
Using the latest VR technology available and appropriate for children between the ages of 10 and 12 years old, the current study aims to expand existing knowledge and investigate the effects of daily VR use on children’s visual functioning, balance and vestibular functioning, visuomotor coordination, inhibitory control, and subjective discomfort. In the current study, children aged 10–12 years engaged in 60 min of VR play across four consecutive days and completed a battery of assessments at three timepoints: before VR gaming (baseline), immediately after VR gaming (post VR), and up to 24 h after VR gaming (no VR). We focused on the ages 10–12 years for its developmental importance and because this age is the youngest age group for which VR use is appropriate per manufacturer guidelines (Meta, 2024a). Specifically, the 10- to- 12-year-old age group represents a developmentally significant cohort where ongoing maturation of visual, motor, and cognitive systems may intersect uniquely with the demands of VR technology. Studying this population not only aligns with safety guidelines but also addresses critical questions about how immersive environments may interact with developmental trajectories during a sensitive period of growth and increasing technological engagement.
Based on findings from previous studies (e.g., Rauschenberger and Barakat, 2020; Tychsen and Foeller, 2020), we expect not to find any clinically significant changes in children’s visual functioning, balance and vestibular functioning, and VIMS (as measured by the SSQ). Additionally, we expect to replicate clinically nonsignificant findings by Rauschenberger and Barakat (2020) related to visuomotor coordination. Lastly, we predict that VR use will not have negative effects on children’s musculoskeletal discomfort or inhibitory control. While research on inhibitory control and VR use is limited, current recommendations limit screen time for children aged 8–14 years to one to 2 hours per day (National Center for Chronic Disease Prevention and Health Promotion, 2016a); since VR use in the present study will not exceed this recommendation, we do not expect negative effects of VR use children’s inhibitory control.
It should be noted that, although we do not expect negative effects of VR use on children’s health and safety, the present study affords an opportunity to contribute relevant insights into a growing body of literature on children’s VR use and wellbeing (e.g., Sobel, 2019; Bailey and Bailenson, 2017). Additionally, new VR technology (i.e., hardware and software) raises questions regarding the extent to which findings from previous research that employed older or different HMDs may be generalizable to new VR technology. Thus, findings from the present study may provide additional and converging evidence for the lack of negative health and safety effects of VR use on children’s development, thereby contributing to the growth of established scientific consensus on this topic. As children’s VR use increases, both at home and in educational settings, understanding the potential impacts, if any, is critical (Rideout et al., 2021).
The present study advances prior research by addressing several key limitations in existing literature. Unlike earlier studies that relied on outdated head-mounted displays, this study employs updated VR technology appropriate for children aged 10 years and above. Additionally, this is the first study to incorporate a direct assessment of executive functioning, specifically inhibitory control, providing novel insights into cognitive domains previously unexamined in VR safety research involving youth. These methodological advancements position the current research to contribute a modern, comprehensive evaluation of VR’s short-term effects on developing children.
Materials and methods
Participants and eligibility criteria
The study sample was comprised of 32 males and 18 females. The greater percentage of males in the sample may reflect the gender bias in gaming engagement documented in the literature (e.g., Fromme, 2003). The fifty participants in this study were 10 years old (40%), 11 years old (36%), and 12 years old (24%) children. The mean age was 10.84 (SD = 0.79). 72% of the sample was Black/African American, 12% were Hispanic/Latino, 8% were Caucasian, and 4% were mixed race. Prior to study participation, participants read and signed an assent form, and their accompanying parent or legal guardian signed a consent form on their behalf. All study procedures were approved by an Institutional Review Board.
The target sample size of 50 participants was determined based on several considerations, including alignment with prior research in pediatric VR studies, the statistical power required to detect meaningful effects, and practical constraints associated with conducting comprehensive, multi-day assessments in a controlled environment.
Eligible participants were naïve VR users, defined as having no history of regular VR use and no more than 1 hour of VR use in the last 90 days preceding study participation. Additional inclusion criteria were as follows: normal or corrected-to-normal vision; interpupillary distance (IPD) between 57.5 and 70 mm (based on the minimum and maximum mechanical lens spacing in the VR headset with a slightly lower bound due to accommodation, Meta, n. d.); stereoacuity of 400 s of arc or better (i.e., upper limit of the standard animal Randot stereo test used for children, Hahn et al., 2010); no history of strabismus, amblyopia, or correction for eye misalignment; no current use of heart, anxiety, or depression medications.
Visual acuity and stereoacuity were assessed onsite by a licensed optometrist prior to participation. To ensure that participants had normal or corrected-to-normal vision, a Nidek ARK-530A autorefractor was used to assess if the spherical equivalent was within −0.5 to +1.0 diopters (D). If the spherical equivalent refractive error was narrowly outside this margin, a Reichert phoropter was used to determine prescription correction; participants qualified if the spherical equivalent was within −0.5 to +1.0 D. If a participant wore glasses, the optometrist assessed whether the participant’s current prescription was within −0.5 to +1.0 D of the presently required correction to achieve 20/20 vision. Stereoacuity was measured by the Randot Stereotest. Eye alignment was assessed by cover-uncover and alternate-cover testing as the child viewed an accommodative target at arm’s length.
Study design
The study design consisted of a 5-day study during which participants spent 1 hour using a VR device for four consecutive days; there was no VR usage on day 5. To accommodate participant availability and scheduling, participants were enrolled in either Block 1 or Block 2 of the design. Participants in Block 1 completed the study on weekdays, Monday through Friday, with approximately 24 h between study sessions, whereas participants in Block 2 completed the study from Tuesday through Saturday, with approximately 24 h between study sessions on days 1–3 and approximately 12–19 h between study sessions on days 4 and 5. Block design was analyzed as a potential confounding factor in the current study (see Data Analysis).
All participants completed a battery of assessments at three time points: on day 1 before any VR use, day 4 immediately after VR use, and day 5 after a 12-to-24-h break from VR use. The length of time that elapsed between day 4 and day 5 assessments determined the length of the break from VR use, which in turn depended on scheduling and participant availability. The battery of assessments comprised a series of tasks to measure visual/ocular functioning, postural balance, depth perception, hand-eye coordination, inhibitory control, and subjective comfort. All measures in the battery are described in detail below.
The VR device used in the present study was a Meta Quest 3. Ten games were preloaded into the VR devices, including Bait, Bonfire, Color Space, Curious Tale of the Stolen Pets, First Contact- Nature Treks, Ocean Right, Star Chart, Tilt Brush, Titans of Space, and Wonderglade. In the first study session, participants were instructed to engage in all games available on their VR device at least once, otherwise participants were free to choose which content they wanted to play throughout the study sessions. Participants were instructed to remain seated during VR gameplay and were monitored at all times by a study moderator. In addition, participants were instructed to take a 10-min break after 30 min of VR usage. During this 10-min break, participants completed a series of guided neck stretches and were restricted from viewing any displays (e.g., cell phone).
Measures
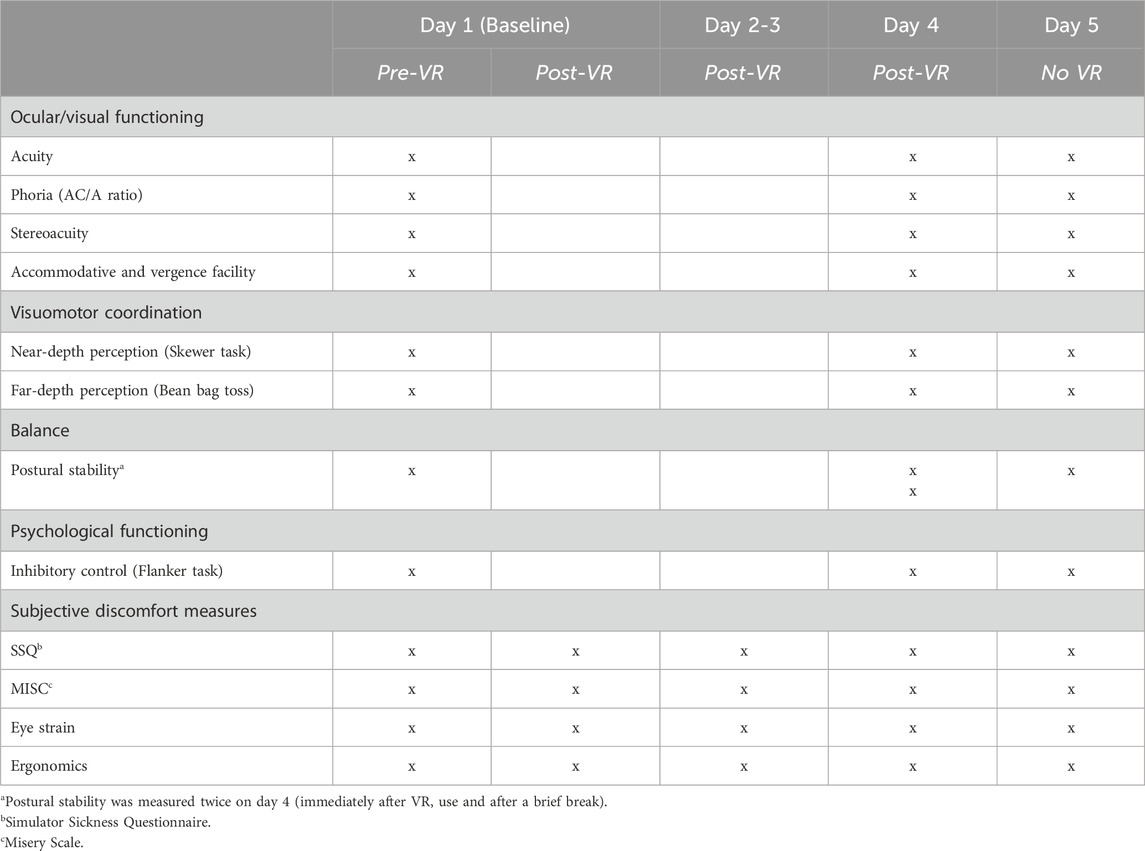
The measures utilized in this study were selected to comprehensively assess domains where VR use may plausibly impact children’s physical health, cognitive functioning, and subjective wellbeing. These domains were identified based on existing literature, known physiological responses to immersive technologies, developmental considerations, and gaps in prior research on pediatric VR use. The battery of measures utilized in the present study, and how/when they were administered, are summarized in Table 1.
Visual functioning
VR headsets present unique visual demands due to prolonged near-field viewing, fixed focal distances, and stereoscopic imagery, which may challenge the normal coordination between accommodation and vergence. Given that children’s visual systems are still maturing during late childhood, we prioritized a range of ophthalmological assessments—such as acuity, stereoacuity, phoria (AC/A ratio), accommodative facility, and vergence facility—to detect subtle disruptions in focus, depth perception, and binocular vision. These measures have been studied in previous work (e.g., Kozulin et al., 2009; Rauschenberger and Barakat, 2020; Tychsen and Foeller, 2020) due to theoretical concerns regarding visual fatigue and strain following VR use among youth.
Acuity, phoria (AC/A ratio), stereoacuity, accommodative facility, and vergence facility were assessed on site by a licensed optometrist. Near and far-field visual acuity was measured without the participant’s prescription (if applicable). Far-field acuity was assessed using a Snellen Eye Chart at a distance of 10 feet in front of the participant. Near-Field acuity was measured using a Jaeger near-point reading card, placed 40 cm in front of the participant. Visual acuity was evaluated monocularly for both eyes.
Stereoacuity was assessed using a Stereo Optical stereovision test (Stereo Optical Inc, Chicago, Illinois, United States). Wearing polarized glasses, participants viewed a three-dimensional image of a butterfly and were asked to “pinch the wings” of the butterfly depicted in the image to verify stereoacuity. Participants then viewed a display of nine sets of four concentric-circle targets. One target in each set “pops out” from the page. The disparity of the targets varied from 800 (most easy to perceive) to 40 (most difficult to perceive) seconds of arc. Participants were asked to identify the target in each of the nine displays. Only subjects with a stereoacuity of at least 400 s of arc were eligible to participate in this study.
Phoria (AC/A ratio) was measured using the alternating cover test with prism neutralization. During this procedure, the examiner covers one eye of the participant and neutralizes any deviation in the uncovered eye using a prism bar. Measurements were taken at both near (47 cm) and far (clinical infinity) distances. AC/A ratio was calculated using the heterophoria method.
Accommodative facility is measured by having participants read 2-point-font letters through a pair of +2/-2 flippers and only respond once each letter was clear. The number of flips from +2D to -2D was recorded for a period of 30 s and then multiplied by two to yield the standard per-minute rate.
Vergence facility was measured with 12D base-out and 3D base-in, whereby participants were instructed to report alphanumeric characters presented at near distance in a 2-point font as soon as they successfully fuse the initial double images into a single image. The number of flips was recorded for a period of 30 s and then multiplied by two to yield the standard per-minute rate.
Visual/ocular assessments were administered at three time points: on day 1 (before VR use), day 4 (after four consecutive days of VR use), and day 5 (after a break from VR use).
Postural balance and vestibular functioning
Immersive VR environments may create sensory conflicts between visual input and vestibular or proprioceptive feedback, potentially leading to temporary impairments in balance or spatial orientation. As children are still refining postural control during this developmental stage, measuring postural sway under various sensory conditions (e.g., eyes open/closed, stable/unstable surfaces) was critical to assess whether VR exposure might transiently disrupt balance or vestibular integration. These metrics are particularly relevant given concerns about motion-induced instability and fall risk after VR sessions.
Postural stability was recorded using an Otometric ICS Balance Platform (Whitney and Wrisley, 2004). A participant’s postural stability was measured in four separate conditions with their eyes either open or closed and either standing with or without a cushion placed on top of the balance platform. Thus, four conditions were: eyes open/no cushion, eyes closed/no cushion, eyes open/cushion, and eyes closed/cushion, and were completed in that order at each time point. During each measurement, participants were instructed to fixate on an “X” on the wall (eyes open condition only), stand as still as possible, with their arms crossed over their chest, while their postural stability was measured for 20 s. Participants repeated this task once in each of the four conditions. Anterior-posterior sway, lateral sway, and total sway area were the metrics of interest for analysis. Anterior-posterior sway provided a measure of variability in a participant’s stance along the front-back axis; lateral sway provided a measure of variability in a participant’s stance along the left-right axis; and total sway provided a measure of the two-dimensional area of space that was covered by deviations in a participant’s center of gravity. Output values from the balance platform software were analyzed.
Postural stability was assessed at four time points: on day 1 prior to VR use (baseline), twice on day 4 (immediately following VR use and approximately 20 min after VR use), and on day 5 (after a break from VR use). The measurement was administered twice on day 4 to determine if any imbalance detected immediately after VR use might normalize after a slight delay.
Visuomotor coordination
VR environments may alter depth cues and spatial representations, which could impact real-world hand-eye coordination and spatial judgment a following VR use. To evaluate this, we included tasks targeting both near-depth perception and far-depth spatial accuracy. These functional assessments were selected to determine whether repeated VR exposure affects children’s ability to coordinate visual input with motor responses—skills essential for daily activities and safe navigation of physical environments.
Three-dimensional spatial representation and hand-eye coordination were assessed using two measures: the skewer-straw task for near-depth perception and the beanbag task for far-depth perception (Loomis et al., 1992). In the skewer-straw task, participants inserted 25 skewers into 30 randomly oriented straws, one at a time, and the total time to complete the task was recorded. Performance in this task relied on dexterity, stereoacuity, and hand-eye coordination. Participants completed a ‘practice round’ prior to the test. The apparatus was rotated 90° after the practice round, to prevent improvements in performance that were due to spatial memory. It should be noted that we included a practice round owing to previous research which suggests that participants undergo an acclimation period when initially performing repeated near-depth perception tasks (Long, 2003).
The beanbag toss was used to measure spatial representation and hand-eye coordination in the absence of visual feedback. That is, participants are blindfolded during this task. In the bean bag toss task, participants were instructed to throw a small beanbag at two targets—a “near” target positioned 15 feet in front of the participant and a “far” target positioned 30 feet in front of the participant. The participant stood at one end of a black rug measuring 35-feet in length and threw the beanbag from a marked tossing line, alternating throws between the near and far targets. The targets were identified by a white cross positioned at the specified locations (15 and 30 feet) along the black rug surface. Participants had 8 throws for each target, for a total of 16 throws completed at each time measurement. Participants were blindfolded during throws but encouraged to view the target between throws to establish target distance before blindfolding again. To avoid providing participants with visual feedback on their performance, participants were not allowed to look at the location where the bean bag landed after each throw. To accommodate this, the experimenter used a piece of black Velcro to mark the location of the beanbag on the black rug after each throw and while the participant was still blind folded. The experimenter measured the vertical distance between the location of the beanbag and the location of the intended target. The outcome measurement in this task was the average vertical distance (in inches) between the beanbag location and the intended target (average across 8 trials per target).
These tasks were administered at three time points: on day 1 (before VR use), day 4 (after four consecutive days of VR use), and day 5 (after a break from VR use).
Executive functioning
Executive functions, particularly visual/attentional inhibitory control, are critical cognitive processes that continue to develop throughout adolescence. While concerns exist that highly stimulating VR environments could challenge self-regulation or attentional control (Bailey and Bailenson, 2017), no prior studies have directly assessed VR’s impact on inhibitory control in children. This variable was included to address this research gap and to explore whether moderate VR use influences behavioral regulation, impulse control, or attentional focus.
The Flanker Inhibitory Control and Attention task was used to assess attentional and visual inhibitory control. We used the version of the Flanker task created for the National Institute of Health (NIH) Toolbox Cognition Battery. The Flanker task tests the ability to inhibit visual attention to irrelevant task dimensions. Participants are required to indicate the left-right orientation of a centrally presented stimulus while inhibiting attention to the potentially incongruent stimuli that surround it. On each trial, a central directional target (arrows on fish for ages 8 and older) is flanked by similar stimuli on the left and right. The task is to indicate the direction of the central stimulus. On congruent trials, the flankers (i.e., distractors) face the same direction as the target. On incongruent trials, they face the opposite direction.
A scoring algorithm integrates accuracy and reaction time and yields four scores: computed score, age-adjustment standard score, change sensitive score, and a national age-adjusted percentile score. Higher scores indicate better attentional and visual inhibitory control. There are 30 trials and the average time to complete the task is 3 min (NIH Toolbox, 2024).
The Flanker task was administered at three time points: on day 1 (before VR use), day 4 (after four consecutive days of VR use), and day 5 (after a break from VR use).
Subjective discomfort measures
Simulator sickness, visual fatigue, and musculoskeletal discomfort are among the most frequently assessed side effects of VR use across age groups (Rauschenberger and Barakat, 2020; Tychsen and Foeller, 2020). Children may be particularly susceptible to these effects due to ongoing sensory and physical development. Therefore, validated self-report measures were incorporated to capture participants’ subjective experiences. The selected measures ensure that even subclinical symptoms, which may not manifest in functional impairments but could affect user wellbeing, are systematically evaluated.
Subjective discomfort was assessed using the Simulator Sickness Questionnaire (SSQ; Kennedy et al., 1993), which comprises three subscales: nausea, oculomotor discomfort, and disorientation. The SSQ contains 16 items, including eye strain, fatigue, sweating, etc., and participants indicate the extent to which participants are currently experiencing each symptom on a scale of 0 (“None”) to 3 (“Severe”). These numeric responses are summed and weighted separately for each of the subscales.
Eye strain was additionally assessed via a single question, “How annoyed are you with eye strain? Example symptoms include tired or heavy eyes, soreness.” Participants responded on 5-point scale: (1) “Not an issue at all; ” (2) “Noticeable, but not annoying; ” (3) “Noticeable, and slightly annoying; ” 4) “Noticeable, and moderately annoying; ” (5) “Noticeable, and very annoying.”
Subjective misery was assessed with the so-called Misery Scale (MISC; Bos et al., 2005; Bos, 2015), which is a one-item assessment where participants are asked, “Are you experiencing any uneasiness, dizziness, or nausea?” and provide a response on an 11-point discomfort rating scale that ranges from 0 (“No problems”) to 10 (“Vomiting”), with the midpoint on the scale indicating feelings of nausea.
Lastly, for specific body parts, including face, head, neck, hands, arms, and shoulders, participants were asked if they felt any tiredness or soreness (binary yes/no response). For any part that a participant indicated feeling tiredness or soreness, a follow-up question probed the participant to indicate the level tiredness/soreness they felt in that body part using a 5-point Likert scale from 1 (“Little bit sore or tired”) to 5 (“Most sore or tired”), with each response option modified to include Wong-Baker faces for simplification (Garra et al., 2010; 2013).
These self-report assessments were administered at three time points: on day 1 (before VR use), day 4 (after four consecutive days of VR use), and day 5 (after a break from VR use).
Data Analysis
We examined baseline measurements for differences across the three age groups represented in the study sample. Moreover, given the participant block design and associated variability in the length of time that elapsed between participants’ day 4 and day 5 measurements, we examined day 5 measurements for any differences as a function of block. If means on any outcome of interest varied as a function of age or block, age and/or block were included as covariate(s) in all subsequent analyses. All data were analyzed using repeated measures analysis of variance (ANOVA) that compared the baseline measurements (day 1) to the measurements taken immediately after VR use on day 4, and after a break from VR use on day 5. If ANOVA indicated differences in mean scores across each time point, post-hoc t-tests with Bonferroni adjustment were conducted to compare means between days. All analyses were conducted in Python. Specifically, ANOVAs were carried out using the pingouin library in Python, which computes Mauchly’s test of sphericity to determine whether the p-values need correction and calculates Greenhouse-Geisser corrected p-values.
Results
There were no statistically significant differences in any of the baseline measurements as a function of age. Likewise, there were no statistically significant differences in any of the day 5 measurements as a function of participant block. Based on these initial analyses, no covariates were included in the main analyses. The results of the main analyses are summarized in detail below. In each figure presented, the error bars represent standard error of the mean.
Visual functioning
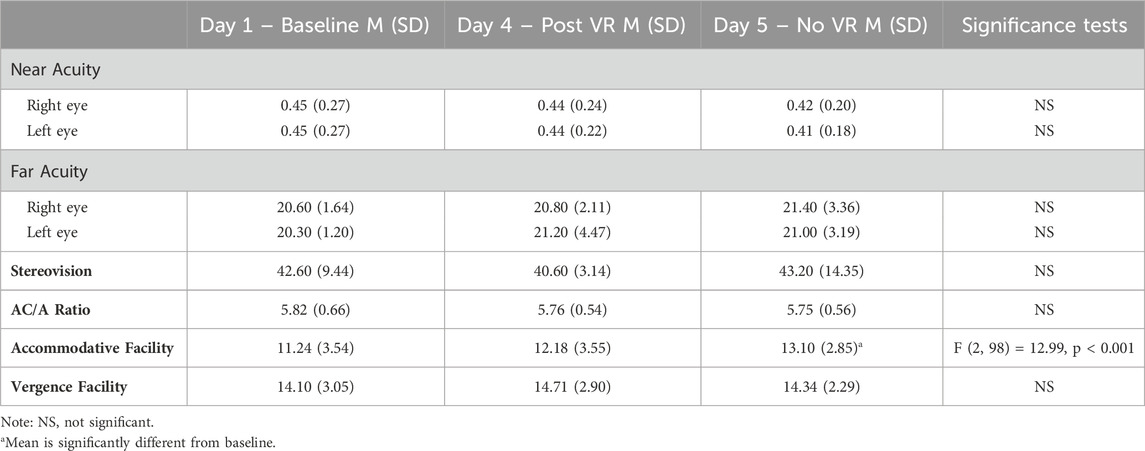
Table 2 provides descriptive statistics and ANOVA results for each of the ophthalmological outcomes. There were no significant differences in any of the ophthalmological measurements, except for accommodative facility, across the three measurement time points: day 1 (baseline), day 4 (post VR use), and day 5 (after break from VR use). Accommodative facility values differed significantly across time points, F (2, 98) = 12.99, p < 0.001. There was a slight increase in recorded accommodative facility values across measurements (see Figure 1). This difference was not significant between day 1 (baseline) and day 4 (post VR use), t (49) = −2.27, p = 0.083. Accommodative facility values were significantly higher on day 5 (after break from VR use) compared to baseline, t (49) = −5.46, p < 0.0001. The mean accommodative facility value for the sample was 13.10 on day 5 compared to 11.24 at baseline.
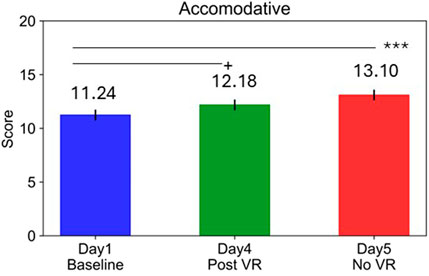
Figure 1. Differences in mean accommodative facility across time measurements. Note: +p < 0.10; ***p < 0.001; error bars represent standard error of the mean.
Balance and vestibular functioning
There was no indication of systematic or pervasive changes in postural stability metrics across time, as illustrated in Figures 2A–C. Of the 36 planned comparisons that were made—i.e., three time point comparisons (baseline compared to the three post measurements) for each combination of three balance metrics in four conditions—only two of the comparisons were found to be statistically significant. Specifically, there were significant differences in average total sway area between baseline and post-tests during the eyes open/no cushion condition only, F (3, 144) = 5.50, p < 0.01 (see Figure 2A). Total sway was higher at the first post-VR measurement on day 4 compared to baseline, t (48) = −3.03, p < 0.05, indicating an increase in postural instability. However, this change in total sway was not significant at the second post-VR measurement, t (48) = −2.54, p = 0.087. Total sway was also significantly higher on day 5 compared to baseline, t (48) = −3.45, p < 0.01. There were no changes across the study period in lateral sway (see Figure 2B) or anterior-posterior sway (see Figure 2C).
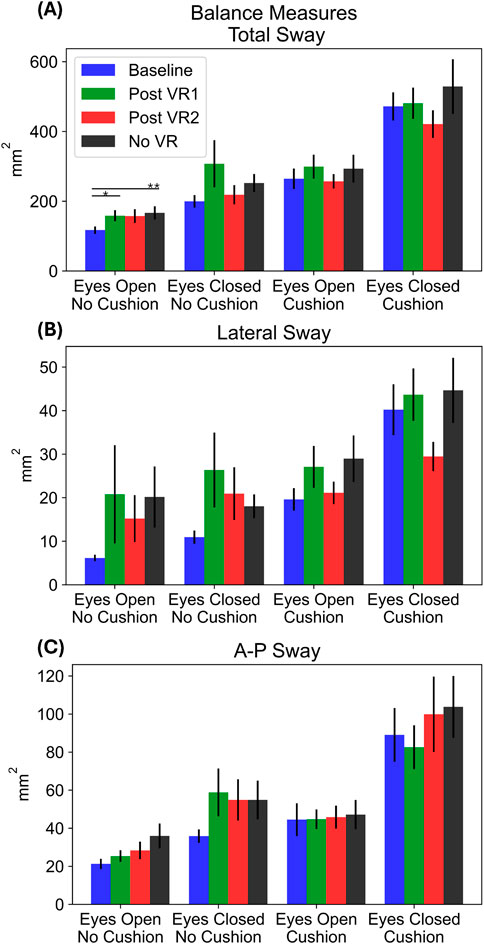
Figure 2. Three measures of postural balance (A) total sway area (B) lateral sway, and (C) anterior-posterior sway), across four different conditions, averaged across participants for each time measurement. Two post measures (Post VR 1 and Post VR 2) were taken 20 min apart on day 4 to evaluate whether any potential effects dissipated by the second post VR measurement. Note: A-P = Anterior-Posterior; *p < 0.05; **p < 0.01; error bars represent standard error of the mean.
Visuomotor coordination
In the skewer straw task, there were no significant differences in average completion times across study days, F (2, 98) = 0.36, p > 0.05 (see Figure 3). In the bean bag toss, there were no significant differences in average distances from the near target across study days, F (2, 98) = 1.10, p > 0.05. However, there were significant differences in the average distance from the far target across days, F (2, 98) = 6.14, p < 0.01. Post-hoc tests revealed significant increases in distance from the far target on day 4 compared to baseline, t (49) = −3.06, p < 0.05, as well as on day 5 compared to baseline, t (49) = −2.59, p < 0.05. Results from the beanbag toss are illustrated in Figures 4A,B.
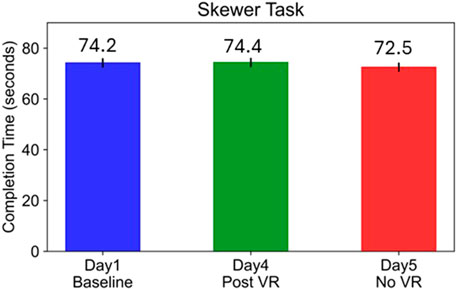
Figure 3. Mean completion time in the Skewer Straw Task across time measurements. Note: Error bars represent standard error of the mean.
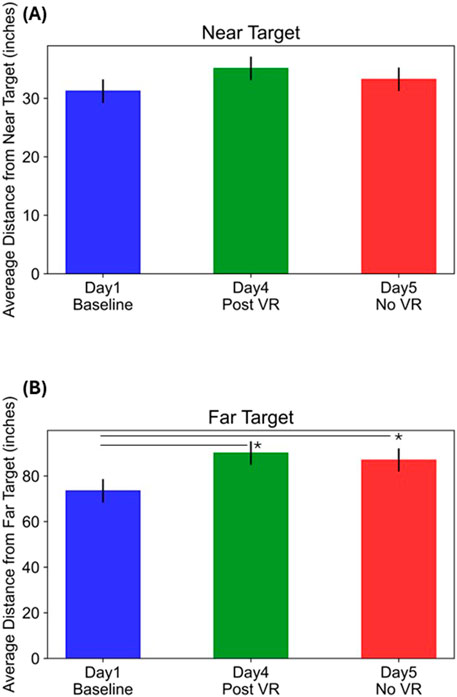
Figure 4. Average distance from near (A) and far (B) targets across time measurements. *p < 0.05; Error bars represent standard error of the mean.
Executive functioning
The NIH Toolbox provides four metrics to characterize performance in the Flanker task for attentional and visual inhibitory control including a computed score, an age-adjusted standard score, a change sensitive score, and a national age-adjusted percentile (see Figures 5A–D). Mean scores, including computed scores, change sensitive scores, and age-adjusted standard scores, were significantly higher at post measurements (day 4 and day 5) compared to baseline, all p’s < 0.05. These results suggest the participants’ task performance generally improved with time. The national age-adjusted percentile was marginally higher on day 5 compared to baseline (see Figure 5D).
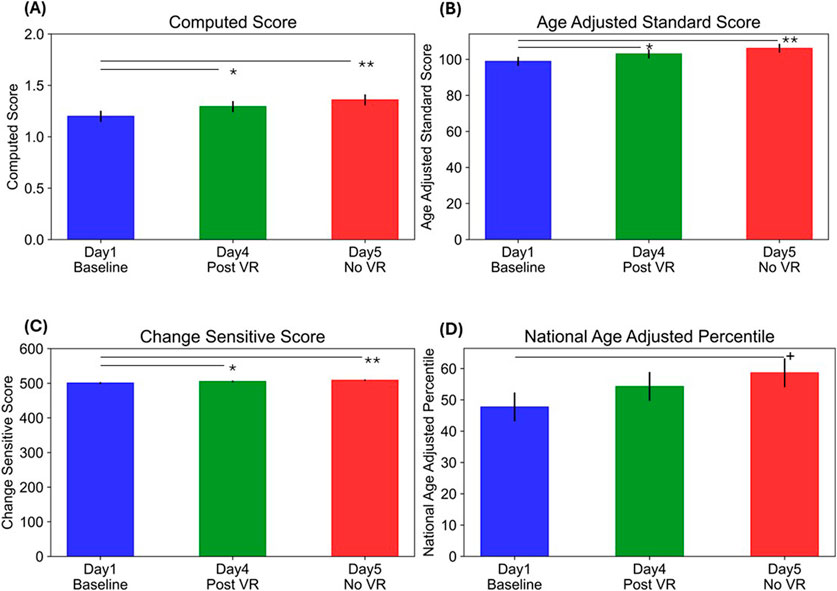
Figure 5. Mean (A) Computer Score (B) Age Adjusted Standard Score (C) Change Sensitive Score, and (D) National Age Adjusted Percentile, on the Flanker Inhibitory Control Task across time measurements. Note: *p < 0.05; **p < 0.01; +p < 0.10; error bars represent standard error of the mean.
Subjective comfort outcomes
Figure 6A illustrates the mean scores across time measurements for self-reported SSQ, eye strain, and misery. The scores for the three subscales of the SSQ—nausea, oculomotor discomfort, and disorientation—decreased numerically from day 1 (baseline) to day 4 (post VR use) and day 5 (after break from VR use), but such change did not reach statistically significance (all p’s > 0.05). A total SSQ score was also calculated and there were no differences in total mean scores across the study period, p > 0.05.
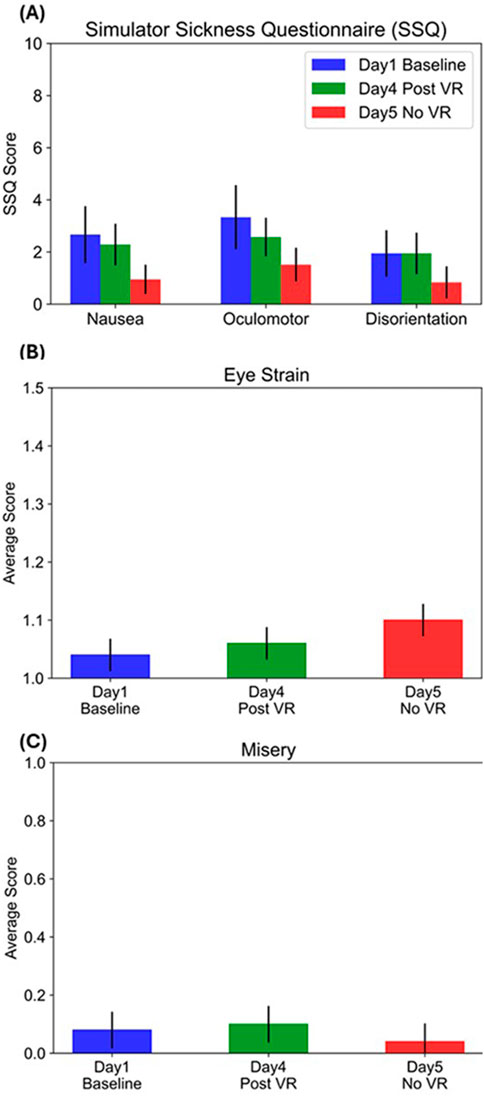
Figure 6. Mean self-report discomfort scores based on (A) simulator sickness questionnaire (SSQ) (B) eye strain scale, and (C) misery scale at each time measurement. Note: Error bars represent standard error of the mean. The maximum possible scores for each measure or subscale is as follows—Nausea: 200.24; Oculomotor: 159.18; Disorientation: 292.32; Eye Strain: 10; Misery: 5.
There was a numerical increase in self-reported eye strain from baseline to day 4 and day 5, but this increase was not statistically significant (p > 0.05; see Figure 6B). The maximum score possible in the eye strain measure is 5 and the highest score reported in the current sample was 3 (“noticeable, and slightly annoying”), reported by a single child. Likewise, there was a numerical increase in self-reported misery from baseline to day 4, and a decrease by day 5, but such changes were not statistically significant (p > 0.05; see Figure 6C).
Table 3 shows the number of participant endorsements for any soreness or tiredness in various body parts at each time measurement. The count of endorsements represented in each column is not mutually exclusive. A total of 11 unique participants reported soreness/tiredness in at least one body part during the study period. On day 1, two unique participants reported soreness/tiredness on the head, arms, and shoulders. On day 4, ten unique participants reported soreness/tiredness in different body parts except the head. On day 5, there were no participants who reported any bodily soreness/tiredness.
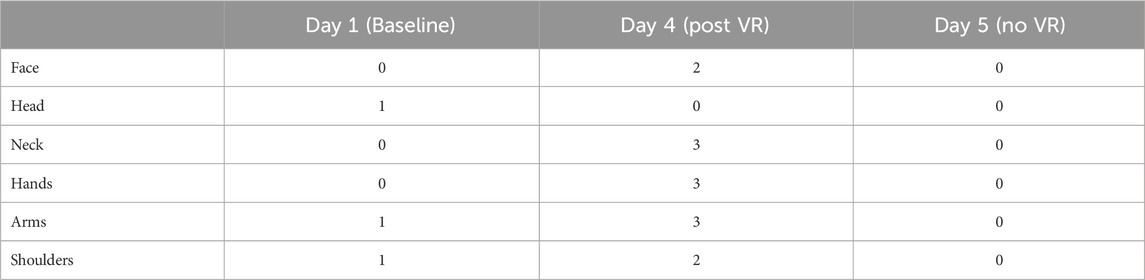
Table 3. Number of endorsements of soreness/tiredness in different body parts at each time measurements. On day 1, two unique participants endorsed any soreness/tiredness; on day 4, ten unique participants endorsed any soreness/tiredness.
Discussion
The present study examined the effects of moderate and repeated use of VR, operationalized as 60 min of daily VR immersion for four consecutive days, on children ages 10 through 12 years. Results from a battery of measures designed to detect the potential presence of adverse effects on vision, postural stability, hand-eye coordination, subjective discomfort, and attentional and visual inhibitory control suggest that health or safety consequences are unlikely to occur from moderate use of VR in 10-to-12-year-old children.
Beyond replicating prior findings related to visual, postural, and motor outcomes, this study introduces several methodological innovations that expand the field’s understanding of pediatric VR use. The use of next-generation VR hardware allows for more relevant assessments of contemporary VR experiences, addressing concerns about the generalizability of findings from studies using older technology. The inclusion of executive function measures—specifically inhibitory control of the visual system—broadens the scope of VR safety research to encompass cognitive self-regulation, a critical developmental domain previously overlooked. Additionally, the multi-day exposure design, reflective of reasonable at-home VR engagement, offers a more realistic evaluation of cumulative short-term effects compared to single-session paradigms. These contributions collectively ensure that the present study not only confirms but also extends prior work, providing an updated, evidence-based guidance on VR use in children.
Visual functioning
Consistent with previous work demonstrating that changes in visual functioning as a result of VR use are clinically nonsignificant (Rauschenberger and Barakat, 2020; Tychsen and Foeller, 2020), we expected that ophthalmological outcomes (acuity, phoria, stereoacuity, accommodative facility, vergence facility, and near- and far-field visual acuity) would not differ as a function of VR use across time points (i.e., between day 1 at baseline, day 4 post VR use, and day 5 after break from VR use). ANOVA results for each of the ophthalmological outcomes provided support for our hypotheses, with the exception of accommodative facility, which were significantly higher on day 5 after a break from VR use compared to day 1 baseline.
Despite the statistically significant difference in accommodation facility between day 1 and day 5, the scale of these changes is within a normative range (22.6 ± 221.7 cpm, Kȩdzia et al., 1999; Zellers et al., 1984). Further, recent research has shown that accommodation facility for this age group can vary greatly on an hourly basis (varying within 3 diopters from morning to afternoon in children between 10 and 19 years old, Park et al., 2019), something that does not occur to the same degree in adults. In addition, Rauschenberger and Barakat (2020) reported similar, but clinically insignificant improvements in performance.
It should be noted that our results, and those reported by Rauschenberger and Barakat (2020) and Tychsen and Foeller, 2020, are inconsistent with results reported by Kozulin and colleagues (2009). Kozulin and colleagues (2009) observed reductions in 5- to 16-year-olds near visual acuity after they engaged in 30- or 80-min HMD viewing sessions–a finding the authors note warranted additional research. It is possible that these differences emerged owing to differences in HMD screen resolution across studies. Kozulin and colleagues (2009) report that the HMD used in their study had a resolution of 320x240 pixels, which the authors suggest is a Snellen equivalent of 6/11, whereas the resolution of the device used in the present study is 2064 × 2,208 per eye (Meta, 2024b). Thus, it is possible that higher resolution screens are less likely to lead to decreases in near visual acuity; however, more research is needed to support this claim. Taken together, the results of the present study contribute to providing converging evidence for the clinically nonsignificant impact of VR use on 10- to 12-year-olds visual functioning.
Balance and vestibular functioning
Based on prior research indicating that VR use does not significantly impact children’s postural stability (Rauschenberger and Barakat, 2020; Tychsen and Foeller, 2020), we predicted that participants’ postural stability would not differ as a function of VR use across time points. Postural stability was measured in four conditions (listed in order of lowest to highest expected difficulty): eyes open/no cushion, eyes closed/no cushion, eyes open/cushion, and eyes closed/cushion and measurements were produced for anterior-posterior sway, lateral sway, and total sway area. Results indicated that total sway area was higher in the eyes open/no cushion condition immediately after VR use on day 4 relative to baseline. However, this increase in total sway normalized or resolved after a 20-min delay, suggesting no prolonged effects of VR use on postural stability. The increase in total sway observed on day 5 (after a break from VR use), compared to baseline, is unexpected. We speculate that it may be related to the balance measurement being the first assessment completed when children returned to the study on day 5. Children may have arrived at the study site excited, having associated the space with VR play. Such excitatory state would be expected to affect balance performance. Interestingly, the average total sway area during the eyes open/no cushion condition was numerically similar to values reported by Rauschenberger and Barakat (2020). Overall, the results in the present study provide support for our hypotheses and build on findings from Rauschenberger and Barakat (2020) and Tychsen and Foeller, 2020 in demonstrating that VR use does not impose meaningful impacts on children’s postural stability and risks to children’s balance functioning immediately following after VR use are negligible.
Visuomotor coordination
Rauschenberger and Barakat (2020) found that children’s spatial representation abilities and hand-eye coordination did not differ as a function of VR use; however, it should be noted that the HMDs used by Rauschenberger and Barakat (2020) differed in terms of both hardware and software from those used in the current study. Based on these findings, we predicted that children in the present study would demonstrate spatial representation abilities and hand-eye coordination behavior that was not adversely impacted by VR use while remaining attentive to the goal of discovering any differential findings, should they occur, owing to hardware and software differences. In the task that assessed children’s near-depth perception, no significant differences emerged, thereby corroborating the results found by Rauschenberger and Barakat (2020) and suggesting that there exists some stability in near-depth perception impacts across varying HMDs. In the task that assessed children’s far-depth perception, ANOVA and post-hoc t-test results revealed that children tended to throw bean bags such that they landed further from the target on day 4 (post VR use) and day 5 (after a break from VR use) relative to baseline. On the one hand, these results may suggest that children’s spatial representation abilities, and more specifically, their ability to engage in distance depth judgments were distorted by cumulative VR use. However, previous research suggests that tasks used to assess distance depth judgments may be subject to artifacts related to task repetition. For example, Rauschenberger and Barakat (2020) also found that participants tended to have higher distance judgments for both near and far targets after a 24-h break from daily VR use.
Executive functioning
Chen et al. (2023) suggest that prolonged screen time may adversely impact children’s neuropsychological development, which may then in turn impact children’s attenional and visual inhibitory control functioning. However, given that VR use durations in the present study aligned with recommendations current recommendations for screen time limits of one to 2 hours per day for children aged 8–14 years (National Center for Chronic Disease Prevention and Health Promotion, 2016b), we hypothesized that VR use in the present study would not adversely impact children’s attentional and visual inhibitory control behaviors. The results showed that computed scores, change sensitive scores, and age-adjusted standard scores were significantly higher at day 4 and day 5 relative to day 1 baseline measurements. No other results were statistically significant. The monotonic increases in participants’ scores (See Figure 5) and the lack of significant differences between day 4 post VR and day 5 without VR scores are suggestive of practice effects. The present study is the first to explore the notion that VR use may impact children’s attentional and visual inhibitory control. Overall, our results indicate that moderate and sustained VR use (i.e., 60-min VR sessions over a period of 4 days) do not deplete children’s ability to suppress or regulate habitual or impulsive responses.
Subjective discomfort
In line with previous research by Rauschenberger and Barakat (2020) and Tychsen and Foeller, 2020, we hypothesized that VR use would not lead to clinically significant changes in VIMS, visual discomfort, or musculoskeletal discomfort. Results derived from VIMS metrics, the SSQ and MISC, provide evidence in support of our hypothesis such that no statistically significant differences in self-reported discomfort emerged cross the study period. Participants’ reports of subjective eye strain also provided support for our hypotheses in that subjective eye strain did not differ significantly across time points. Across the course of the study, 22% of participants endorsed soreness or tiredness on one or more body part; however, the magnitude of such soreness remained relatively low. Furthermore, no participants wished to end the VR session early. Overall, the results from the present study demonstrate a lack of significant findings related to VIMS and subjective eye strain paired with numerical assessments of low incidence of participant musculoskeletal discomfort and study termination (i.e., participant drop out). Our findings demonstrate that moderate and sustained use is unlikely to lead to clinically significant impacts on children’s comfort.
Strengths, considerations, and future directions
The present research is the first to suggest that repeated VR use over four consecutive days does not adversely impact 10- to 12-year-olds attentional and visual inhibitory control. Additionally, this work contributes further insights to a growing body of scientific research on the potential effects of VR on children’s vision, postural stability, depth perception and hand-eye coordination, and subjective discomfort. Notably, our results mostly corroborate previous findings, with the exception of discrepancies related to far-depth perception, reported by Rauschenberger and Barakat (2020) and Tychsen and Foeller, 2020.
It should be noted that some features of the present study impose limitations regarding the generalizability of the results. Specifically, the present study was conducted within a controlled laboratory setting and VR play was limited to 60 min per day for 4 days, with a 10-min break halfway through each play session. Given that children who live in a household with access to a VR headset may engage in VR gameplay for longer periods of time, in terms of session length, number of sessions per day, and/or number of consecutive days that VR is used, generalizing the results of the present study to such use cases should be done with caution. It is possible that longer, more frequent VR use may yield a different pattern of results. Additionally, the VR games utilized in the present study were stationary and only required passive involvement from the player. Engagement with other types of games may offer different physical and/or cognitive benefits and challenges for children, and thus may yield a different pattern of results. The results of this study should not be generalized across all VR content types, especially those requiring more vigorous or physically demanding interaction. While the assessments were conducted up to 24 h after the final VR session, the study did not evaluate potential long-term effects or cumulative impacts beyond this point. Moreover, although validated tools were used, some measures (e.g., subject discomfort scales, postural sway metrics) may not capture nuanced or transient changes, especially if children underreport symptoms due to excitement or novelty effects associated with VR gameplay. Since participants were limited to VR-naïve users that fit within a specific interpupillary distance and vision criteria, the results of the current study cannot be generalized to other pediatric populations such as children with prior VR experience or those with pre-existing visual or neurological conditions. To address these limitations, future research should explore long-term VR use, incorporate a wider range of VR content, and assess variable naturalistic usage patterns.
Two findings from the present study provide viable avenues for future research. Our findings regarding increased near target distance judgment when participants completed the far-depth perception task are incongruent with previous research by Rauschenberger and Barakat (2020) and raise questions regarding the extent to which the task elicited a study artifact (i.e., repetition effect) or children’s far-depth perception is impacted by sustained VR use when judging the distance of near targets. More research is needed to clarify these results. The second finding that invites future research is regarding children’s attentional visual inhibitory control. In the present study, we investigated one of several aspects of executive functioning. Although the results in the present study do not demonstrate any negative effects of VR use on children’s ability to appropriately attend to task relevant stimuli and exhibit inhibitory control, our results do not necessarily speak to the extent to which, if at all, other aspects of executive function may be affected. Given previous research demonstrating positive associations between exergaming and executive functioning skills, additional research is needed to explore the potential effects of VR use on different constructs of executive functioning (Best and Miller, 2010).
Conclusion
The present study contributes novel insights into the growing body of evidence regarding the physical and cognitive impacts of VR use on children, and to a growing body of literature demonstrating that repeated VR use is unlikely to have clinically meaningful effects on children’s vision, postural stability, three-dimensional spatial representation and hand-eye coordination, and subjective comfort. Moreover, the present study is the first to investigate the effects of VR use on children’s attentional and visual inhibitory control and to suggest that, similarly, VR use does not negatively impact this important aspect of executive functioning. The current study results indicate that 10- to 12-year-olds’ moderate VR use may be relatively low risk, having no adverse effects on some aspects of physical and cognitive functioning and wellbeing.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by Exponent Institutional Review Board. The studies were conducted in accordance with the local legislation and institutional requirements. Written informed consent for participation in this study was provided by the participants' legal guardians/next of kin. Written assent was also provided by each minor/child participant.
Author contributions
KS: Formal Analysis, Project administration, Supervision, Writing – original draft, Writing – review and editing. NB: Writing – original draft, Writing – review and editing. AMC: Formal Analysis, Writing – original draft, Writing – review and editing. OI: Formal Analysis, Validation, Writing – review and editing. RLK: Funding acquisition, Methodology, Supervision, Writing – review and editing, Conceptualization.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. The current study was sponsored by Meta Platforms, Inc. The funder was not involved in the study design, collection, analysis, or interpretation of data, the writing of this article, or the decision to submit for publication.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Bailey, J. O., and Bailenson, J. N. (2017). “Immersive virtual reality and the developing child,” in Cognitive development in digital contexts. Editors F. C. Blumberg, and P. J. Brooks (Academic Press), 181–200. doi:10.1016/B978-0-12-809481-5.00009-2
Best, J. R., and Miller, P. H. (2010). A developmental perspective on executive function. Child. Dev. 81, 1641–1660. doi:10.1111/j.1467-8624.2010.01499.x
Bos, J. E. (2015). Less sickness with more motion and/or mental distraction. J. Vestib. Res. 25, 23–33. doi:10.3233/ves-150541
Bos, J. E., MacKinnon, S. N., and Patterson, A. (2005). Motion sickness symptoms in a ship motion simulator: effects of inside, outside, and no view. Aviat. Space, Environ. Med. 76, 1111–1118.
Bronfrenbrenner, U. (1981). The ecology of human development: experiments by nature and design. Harvard University Press.
Bruce, A. S., Atchison, D. A., and Bhoola, H. (1995). Accommodation-convergence relationships and age. Investigative Ophthalmol. and Vis. Sci. 36, 406–413.
Chen, Y. Y., Yim, H., and Lee, T. H. (2023). Negative impact of daily screen use on inhibitory control network in preadolescence: a two-year follow-up study. Dev. Cogn. Neurosci. 60, 101218. doi:10.1016/j.dcn.2023.101218
de Jong, P. T. (2024). A history of visual acuity testing and optotypes. Eye 38, 13–24. doi:10.1038/s41433-022-02180-6
Garra, G., Singer, A. J., Domingo, A., and Thode, Jr. H. C. (2013). The Wong-Baker pain FACES scale measures pain, not fear. Pediatr. Emerg. care 29, 17–20. doi:10.1097/pec.0b013e31827b2299
Garra, G., Singer, A. J., Taira, B. R., Chohan, J., Cardoz, H., Chisena, E., et al. (2010). Validation of the Wong-Baker FACES pain rating scale in pediatric emergency department patients. Acad. Emerg. Med. 17, 50–54. doi:10.1111/j.1553-2712.2009.00620.x
Granic, I., Lobel, A., and Engels, R. C. M. E. (2014). The benefits of playing video games. Am. Psychol. 69, 66–78. doi:10.1037/a0034857
Hahn, E., Comstock, D., Durling, S., MacCarron, J., Mulla, S., James, P., et al. (2010). Monocular clues in seven stereotests. Dalhous. Med. J. 37, 4–13. doi:10.15273/dmj.vol37no1.3861
Johnson, G. M., and Puplampu, K. P. (2008). Internet use during childhood and the ecological techno-subsystem. Can. J. Learn. Technol. 34. doi:10.21432/t2cp4t
Kaimara, P., Oikonomou, A., and Deliyannis, I. (2022). Could virtual reality applications pose real risks to children and adolescents? A systematic review of ethical issues and concerns. Virtual Real. 26, 697–735. doi:10.1007/s10055-021-00563-w
Kȩdzia, B., Pieczyrak, D., Tondel, G., and Maples, W. C. (1999). Factors affecting the clinical testing of accommodative facility. Ophthalmic Physiological Opt. 19, 12–21. doi:10.1046/j.1475-1313.1999.00396.x
Kennedy, R. S., Lane, N. E., Berbaum, K. S., and Lilienthal, M. G. (1993). Simulator sickness questionnaire: an enhanced method for quantifying simulator sickness. Int. J. Aviat. Psychol. 3, 203–220. doi:10.1207/s15327108ijap0303_3
Kim, E. H., Granger-Donetti, B., Vicci, V. R., and Alvarez, T. L. (2010). The relationship between phoria and the ratio of convergence peak velocity to divergence peak velocity. Investigative Ophthalmol. and Vis. Sci. 51, 4017–4027. doi:10.1167/iovs.09-4560
Kozulin, P., Ames, S. L., and McBrien, N. A. (2009). Effects of a head-mounted display on the oculomotor system of children. Optometry Vis. Sci. 86, 845–856. doi:10.1097/OPX.0b013e3181adff42
LaViola, J. J. (2000). A discussion of cybersickness in virtual environments. ACM SIGCHI Bull. 32, 47–56. doi:10.1145/333329.333344
Long, J. (2003). “Two practical tasks for assessing depth perception at near distance comparison of performance under monocular and binocular conditions,” in 39th annual conference of the ergonomics society of Australia Inc, brisbane, Australia, 24-26 november 2003. Narrabundah, ACT: hfesa.
Loomis, J. M., Da Silva, J. A., Fujita, N., and Fukusima, S. S. (1992). Visual space perception and visually directed action. J. Exp. Psychol. Hum. Percept. Perform. 18, 906–921. doi:10.1037//0096-1523.18.4.906
Meta (2024a). Meta Quest safety information for parents and pre-teens. Available online at: https://www.meta.com/quest/parent-info/ (Accessed on June 12, 2024).
Meta (2024b). Sign up for Meta quest 3 release: new mixed reality VR headset. Available online at: https://www.meta.com/quest/quest-3/ (Accessed on March 12, 2024).
National Center for Chronic Disease Prevention and Health Promotion (U.S.) (2016a). Screen time vs. lean time: age group 11-14. Available online at: https://stacks.cdc.gov/view/cdc/47583 (Accessed on July 12, 2024).
National Center for Chronic Disease Prevention and Health Promotion (U.S.) (2016b). Screen time vs. lean time: age group 8-10. Available online at: https://stacks.cdc.gov/view/cdc/47584 (Accessed on March 12, 2024).
NIH Toolbox (2024). V3 administration manual. Available online at: https://nihtoolbox.org/ (Accessed on March 12, 2024).
Park, S. M., Moon, B. Y., Kim, S. Y., and Yu, D. S. (2019). Diurnal variations of amplitude of accommodation in different age groups. Plos one 14, e0225754. doi:10.1371/journal.pone.0225754
Piaget, J. (1954). The construction of reality in the child. New York: Basic Books. doi:10.1037/11168-000
Rauschenberger, R., and Barakat, B. (2020). “Health and safety of VR use by children in an educational use case,” in Proceedings - 2020 IEEE conference on virtual reality and 3D user interfaces, VR 2020, 878–884. doi:10.1109/VR46266.2020.1581276262586
Reed, N., and Joseff, K. (2022). Kids and the metaverse: what parents, policymakers, and companies need to know. Available online at: https://www.commonsensemedia.org/sites/default/files/featured-content/files/metaverse-white-paper.pdf (Accessed March 12, 2024).
Rideout, V., Peebles, A., Mann, S., and Robb, M. B. (2021). The Common Sense census: medica use by tweens and teens. San Francisco, CA: Common Sense. Available online at: https://www.commonsensemedia.org/sites/default/files/research/report/8-18-census-integrated-report-final-web_0.pdf (Accessed on March 12, 2024).
Ripps, H., Chin, N. B., Siegel, I. M., and Breinin, G. M. (1962). The effect of pupil size on accommodation, convergence, and the AC/A ratio. Investigative Ophthalmol. and Vis. Sci. 1, 127–135.
Rushton, S. K., and Riddell, P. M. (1999). Developing visual systems and exposure to virtual reality and stereo displays: some concerns and speculations about the demands on accommodation and vergence. Appl. Ergon. 30, 69–78. doi:10.1016/S0003-6870(98)00044-1
Sobel, K. (2019). “Immersive media and child development: synthesis of a cross-sectoral meeting on virtual, augmented, and mixed reality and young children,” in The joan ganz cooney center at sesame workshop. New York.
Tychsen, L., and Foeller, P. (2020). Effects of immersive virtual reality headset viewing on young children: visuomotor function, postural stability, and motion sickness. Am. J. Ophthalmol. 209, 151–159. doi:10.1016/j.ajo.2019.07.020
Vygotsky, L. S. (1978). Mind in society: development of higher psychological processes. Cambridge: Harvard University Press.
Weerdmeester, J., Cima, M., Granic, I., Hashemian, Y., and Gotsis, M. (2016). A feasibility study on the effectiveness of a full-body videogame intervention for decreasing attention deficit hyperactivity disorder symptoms. Games health J. 5, 258–269. doi:10.1089/g4h.2015.0103
Whitney, S. L., and Wrisley, D. M. (2004). The influence of footwear on timed balance scores of the modified clinical test of sensory interaction and balance. Archives Phys. Med. Rehabilitation 85, 439–443. doi:10.1016/j.apmr.2003.05.005
Keywords: children, health, safety, visual functioning, inhibitory control, postural balance, depth perception, virtual reality
Citation: Silva K, Breeland N, Clark AM, Öztekin I and Kelly RL (2025) Effects of virtual reality use in children aged 10 to 12 years. Front. Virtual Real. 6:1547198. doi: 10.3389/frvir.2025.1547198
Received: 17 December 2024; Accepted: 08 May 2025;
Published: 02 July 2025.
Edited by:
Manuela Chessa, University of Genoa, ItalyReviewed by:
Dimitrios Stamovlasis, Aristotle University of Thessaloniki, GreeceLamiaa Mostafa, Arab Academy for Science, Technology and Maritime Transport (AASTMT), Egypt
Onorina Botezat, Bucharest Academy of Economic Studies, Romania
Copyright © 2025 Silva, Breeland, Clark, Öztekin and Kelly. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Karol Silva, a3NpbHZhQGV4cG9uZW50LmNvbQ==
 Karol Silva
Karol Silva Nichole Breeland
Nichole Breeland Ashley M. Clark
Ashley M. Clark Ilke Öztekin
Ilke Öztekin Rachel L. Kelly
Rachel L. Kelly