- 1GET Lab, Department of Multimedia and Graphic Arts, Cyprus University of Technology, Limassol, Cyprus
- 2Physiotherapy Unit, Neurology Clinics, The Cyprus Institute of Neurology and Genetics, Nicosia, Cyprus
- 3Interactive Media, Arts and Humanities Division, New York University Abu Dhabi, Abu Dhabi, United Arab Emirates
Introduction: Integrating social interaction into stroke rehabilitation is recommended but often underutilized due to limited resources. Virtual Reality (VR) offers a way to introduce social facilitation via virtual agents in rehabilitation training. Understanding how chronic stroke survivors respond to virtual agents can inform physiotherapy practice with innovative digital tools.
Methods: This study presents five case studies of chronic stroke survivors (2 female, 3 male) with motor impairments, all with paresis of the dominant right upper limb. Participants engaged in a VR-based upper limb exergame under two conditions: playing alone and playing alongside with a virtual agent, acting as a second-player, controlled by a rule-based algorithm. Rehabilitation progress, task performance, and engagement were examined across training sessions.
Results: Participants who completed all sessions showed consistently higher engagement when playing with a virtual agent compared to playing alone. At the same time, the presence of the virtual co-player had no observable effect on game performance.
Discussion: These findings suggest that incorporating a virtual agent can enhance task engagement and promote perseverance in VR-based stroke rehabilitation. The results are discussed in the context of current VR rehabilitation practices, and implications for clinical practice and future research are outlined.
1 Introduction
Stroke is one of the leading causes of death worldwide (World Health Organization, 2016), and survivors often suffer from severe motoric and cognitive impairments (Stone et al., 2019; Herpich and Rincon, 2020). Rehabilitation therapy can mitigate the functional decline resulting from neuronal damage (Anwer et al., 2022) by promoting neuroplasticity, the ability of the brain to regain lost functionality following an injury (Puderbaugh and Emmady, 2023; Deutsch and McCoy, 2017). In essence, rehabilitation training can be seen as a process of (re)learning motor functions (Warraich and Kleim, 2010). However, stroke rehabilitation training is a process that takes significant time and effort. Alankus et al. (2010) found that only 31% of the survivors who receive stroke rehabilitation training remain compliant with their physiotherapists’ instructions. Chronic stroke survivors often require additional incentives beyond the premise of recovery to stay committed to their rehabilitation training. Such incentives often include virtual reality (VR), as it can incorporate gamification elements into the rehabilitation process (Elor et al., 2021; Lew et al., 2021), facilitate telerehabilitation (Rojo et al., 2022), and provide real-time feedback regarding rehabilitation progress (Bellomo et al., 2020; Rong et al., 2021).
1.1 Exergaming
Gamified VR applications that cater to rehabilitation goals are often considered as “exergames” in literature. Evidence-based studies suggest that integrating VR-based interactive exergaming interventions with conventional rehabilitation programs can improve upper limb function in stroke survivors, aiding in activities of daily living (Mekbib et al., 2020). However, the effectiveness of these interventions in isolation remains an area of ongoing research (AlMousa et al., 2017). Numerous questions regarding the efficacy of exergames remain unanswered, and our understanding of the potential of VR exergames in rehabilitation is currently rudimentary, primarily focusing on promoting cortical learning, neuronal modulation, and neuroplasticity (Khan et al., 2023). Whereas existing studies on rehabilitation exergames rarely describe the psychological considerations behind the design of exergames (Levac, 2024; Hadjipanayi et al., 2024), game design principles emphasize the significance of psychological and psychosocial components elicited by VR games in sustaining rehabilitation efforts. Key aspects include modulating the perceived level of challenge and fostering spontaneous motivation through gameplay, both of which can be paramount for perseverance in achieving rehabilitation goals (Elor et al., 2018; Dimbwadyo-Terrer et al., 2016).
1.2 Social interactivity in VR applications for rehabilitation
Social interaction is one of the key factors contributing to perseverance in stroke rehabilitation in both physical settings (Neibling et al., 2021) and in VR (Duckworth et al., 2023). The authors in Duckworth et al. (2023) suggested that if virtual technologies are to be used in home settings for enabling telerehabilitation, the transfer of real-world social interaction to VR is as important as the applications themselves. However, VR settings for rehabilitation are currently lacking the conditions for cultivating social interaction (Høeg et al., 2023a; Alex et al., 2021). Social interactivity constraints in VR applications for rehabilitation include unsupported computer networking and poor interactivity features between users who share the same virtual environment. Nevertheless, the significance of incorporating social interaction into VR rehabilitation has long been acknowledged by stakeholders (Flores et al., 2008), and when resources permit, efforts are often made to integrate social interaction in VR experiences. In the following paragraphs we delineate social interactivity approaches for VR stroke rehabilitation applications that include a multiplayer component.
While the literature on competitiveness within the exergame rehabilitation context is limited, instances where competitiveness positively influences rehabilitation outcomes have been documented. An example is the study described in House et al., (2016) where interventions were based on an exergaming tournament involving stroke survivors. However, it is crucial to note that the tournament was built on a team-versus-team dynamic, making it challenging to attribute the positive rehabilitation outcomes solely to either competitiveness or teamwork. Conversely, the authors in Lewis et al. (2011) suggested that survivors preferred competing against other individuals rather than their own past scores (i.e., a “ghost” of their past selves) in exergame interventions. They observed that merely competing against personal high score might be insufficient to maintain interest. The memory cards game adapted as a multiplayer VR exergame in Ballester et al. (2012) was designed to require players to reach out for the cards with their impaired hand and perform wrist movements to flip them around. The winner was determined by the player who discovered all the matching pairs first, placing competitiveness on active memory rather than motoric ability. Following the intervention, players in the multiplayer mode exhibited wider elbow flexion and extension movements, as well as better mood, compared to those in the single-player mode. Similarly, the authors in Triandafilou et al. (2018) observed a positive impact on exercise motivation and the willingness of stroke survivors to engage in multiplayer VR stroke telerehabilitation exergames which incorporated elements of both competitiveness and cooperation. The authors attributed this positive outcome to the emergence of socialization during player interaction. Additionally, prolonged in-game socialization appeared to alleviate depression symptoms in some survivors (Burdea et al., 2020; Thielbar et al., 2020). Evidently, incorporating a multiplayer component into the exergame system can add enjoyment and incentivize engagement with the exergaming intervention.
Nevertheless, the impact of in-game social interaction, whether through cooperative or competitive gameplay, can vary significantly among stroke survivors. For example, a clear connection between social exergaming and the alleviation of depressive symptoms remains unclear (Burdea et al., 2022), particularly since depression often discourages stroke survivors from participating in social exergaming activities (House et al., 2016). Additionally, whether a stroke survivor chooses to engage in competitive or cooperative multiplayer gameplay, or even to reject social exergaming altogether, depends on individual personality and occasional preference (Novak et al., 2014). Regardless, there is a state of mind (i.e., flow), which is especially important in the field of rehabilitation, as being in the flow state is optimal for a stroke survivor to maximize enjoyment and subsequently high-quality practice (Jung et al., 2020). This state of mind allows the maintenance of a deep concentration and activity engagement for periods longer than average and occurs when the challenges of the activity align with individual skill level (Jung et al., 2020; Csikszentmihalyi, 2014). The theory of flow also focuses on the aspect of “psychic entropy,” a term that describes a disorder in an individual’s consciousness when faced with information that misaligns with the individual’s goals. As psychic entropy is associated with feelings of stress and pain, the psychic entropy of rehabilitation patients is higher than that of healthy individuals. Therefore, researchers propose that games directed towards stroke survivors should avoid information overload through visuals, sound, or game mechanics for the flow state to occur (Charles et al., 2020).
In line with the concept of psychic entropy, chronic stroke survivors who experience functional loss and are susceptible to negative emotions when their perceived limitations are exposed (such as during a challenging competitive exergame) often undergo a process of identity reevaluation (Charles et al., 2020). Consequently, confrontations of psychomotor skills among chronic stroke survivors through competitive gameplay can be delicate, potentially leading to self-esteem damage. In another study (Liang et al., 2023), elderly participants were exposed to three exergaming experimental conditions for upper-limb rehabilitation training, along with a non-gaming control condition. The three exergame conditions included training either individually, against another patient, or with help from another patient. Participants were initially most motivated to train under the competitive condition (against another patient). However, their interest in competitive play quickly diminished, and participants became reluctant to play the exergame again. On the other hand, the cooperative condition (with help from another patient) engaged participants for a longer duration, thus establishing cooperative gameplay as most beneficial. This outcome is supported by the self-determination theory (Syed and Kamal, 2021), whereby connectivity is recognized as a fundamental physiological need. Fulfilling this need may result in higher autonomous motivation to engage in therapeutic interventions. Connectivity in this regard is characterized as a “non-judgmental interaction” within the context of a therapeutic alliance (Allegue et al., 2021; Allegue et al., 2022). This means that for connectivity to be successfully established, it is crucial to avoid undermining one’s sense of competence in their abilities during exergame-initiated social interactions. Cooperation, nonetheless, may not be the most suitable approach for rehabilitation exercises, as it inherently encompasses elements of competition that expose and compare participants’ skills and capabilities (Høeg et al., 2023b). Rehabilitation patients who perceive their task-specific capabilities as inferior to those of their collaborators may experience reduced task performance and enjoyment (Barak Ventura et al., 2019). In cooperative game modes, there is also the risk of social loafing, which refers to a decrease in individual effort towards achieving a common goal in group settings (Nichols, 2014).
1.3 Social facilitation and VR
Researchers from the behavioral and neuroscience domains concur that human motor behavior has been significantly influenced by social interaction throughout history (Mnif et al., 2022). Specifically, observing others’ performed actions a) influences one’s ability to perform similar actions in synchrony, b) can lead to the tendency of performing the same action even without the intention to do so, and c) can shape judgments of the observed actions’ intentions, which depend on the observer’s current motor system state (Mnif et al., 2022; Sebanz and Knoblich, 2009). Behaviorist theories of social facilitation and inhibition stress that the mere presence of peers in the environment can unconsciously enhance performance on simple, familiar tasks but hinders performance on complex, unfamiliar tasks (Zajonc and Sales, 1966). Strauss (Strauss, 2002), who focuses on the effect of social facilitation on motor tasks, concludes that social facilitation favors motor tasks that require stamina, power, and speed. This effect stems from several factors, including the affective state and the social evaluation effect - also known as evaluation apprehension (i.e., the concern of not meeting standards or goals in the eyes of others) (Schmitt et al., 1986; Guerin and Innes, 1984).
For over a century, developments in behaviorist and neuroscientific models of social interaction have progressed to a standstill. This was mainly due to the realization that studying social interactions outside the laboratory is the most promising step forward (Hari and Kujala, 2009). However, this approach poses privacy and other ethical concerns. An alternative is replicating realistic social environments in a controlled laboratory setting, albeit difficult in its execution. Advancements in VR technology mitigate these challenges by improving human 3D models and functionality, making it easier to replicate plausible social interactions. Research into virtual humans as proxies for human co-presence in VR has recently gained traction, driven by advances in artificial intelligence and growing interest in the metaverse (Kim and Jo, 2022). Evidence suggests that, irrespective of the VR user’s awareness of the virtual human’s properties, they subconsciously perceive the presence of the virtual human as akin to that of a real-life human, a phenomenon commonly referred to in the literature as co-presence (Li et al., 2024; Kyrlitsias and Michael-Grigoriou, 2022; Oh et al., 2018). VR co-presence can occur whether the virtual person being observed is the avatar embodiment of a real human or a human-like representation of a non-player character (NPC). Furthermore, co-presence operates on two levels: the perception of others within the environment and the perception of others as in-group members, sharing a mutual perception (Bulu, 2012; Slater et al., 2000). In another study (Sterna et al., 2024), the illusion of co-presence with virtual agents was found to align with theories of social facilitation and inhibition observed in real life scenarios. In the context of rehabilitation, this suggests that the illusion of social co-presence in VR negates the need for real-life human actors to serve as social facilitators during therapeutic intervention, thus saving time, costs, and effort.
Although many questions about VR co-presence and its potential implications for rehabilitation remain unanswered, introducing social interaction elements into exergaming rehabilitation offers promising prospects for enhancing rehabilitation perseverance, aligning with social facilitation theories. However, active social facilitation (i.e., coaction) is different from competitiveness or cooperation, as it emphasizes the aspect of co-presence with others performing the same task and its impact on individual performance (Zajonc, 1965). The authors in Lau et al. (2019) suggest that mere co-presence may not significantly improve performance in exergame rehabilitation unless accompanied by an incentive for interaction, such as incorporating competitive aspects into the psychosocial dimension of the therapeutic intervention.
Given this context, it is crucial to leverage VR technology to advance stroke rehabilitation, with a particular focus on the psychological wellbeing of chronic stroke survivors. To this end, we used an immersive VR application (Najm et al., 2020) that simulates an exergame designed for forearm supination and pronation training exercises commonly used in traditional rehabilitation. The virtual environment included a full-body avatar, controlled by the user from a first-person perspective, and a virtual agent controlled by the game system. The virtual agent’s performance is dynamically adapted, taking into account the user’s game performance.
To the best of our knowledge, there are currently no studies that isolate social facilitation from cooperation or competitiveness in the context of stroke rehabilitation using VR. Building on the VR exergame (Najm et al., 2020) for forearm supination and pronation exercise, our study aims to explore whether active social facilitation affects stroke survivors’ performance (measured by degrees of supination/pronation maneuvers) and engagement (assessed through momentary self-evaluation) during therapy, specifically by examining the impact of a virtual agent’s co-presence. This was accomplished without the use of in-game clues or rewards promoting either competition or cooperation. Our findings may shed light on the significance of social facilitation in stroke rehabilitation, suggesting that elements of cooperation and competitiveness in VR exergames could potentially disrupt the rehabilitation process.
2 Materials and methods
2.1 The VR exergame and setup
The VR exergame used in this study is described in detail in (Najm et al., 2020). For completeness, we provide an overview of the elements of the VR application that are relevant to our study. The exergame is a car racing game set in a virtual environment where participants find themselves in a room, embodied in a gender-matched virtual body from a first-person perspective, with a racing platform featuring two cars at the starting line, ready to race (Figure 1A). The main in-game objective is for the participant to propel the car on their side to the finish line by moving the impaired limb according to the rehabilitation exercise (supination/pronation). The greater the degree of hand rotation, the more the cars are charged. Participants’ arm movements are tracked in real-time using the Xsens wireless motion tracker attached to the affected wrist (Najm et al., 2020). In Najm et al.'s (Najm et al., 2020) VR application, the patient can play the game either in a solitary setting or in a two-payer setting, that is alongside with a virtual player agent (Figure 1B). Two pairs of virtual agents were used, each gender-matched with the participant. One agent was set to consistently outperform the participant, while the other was set to underperform. To clearly distinguish virtual agents as separate individuals, distinct avatars were used, ensuring their physical appearances matched as closely as possible. At the end of each round, the cars race, with the charge level of each car determining the strength of its engine boost.
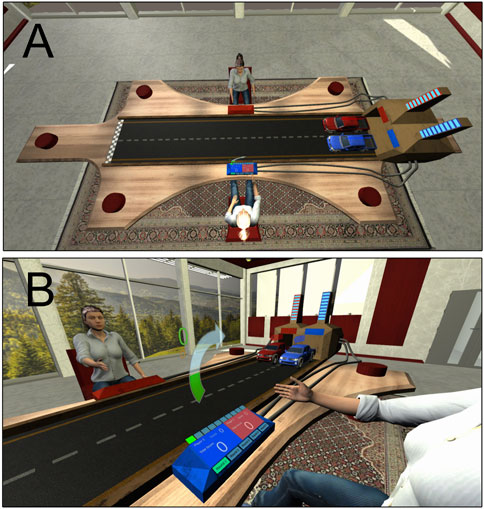
Figure 1. The virtual environment of the immersive VR exergame application (A) Bird’s eye view of the user’s avatar (blue car) and the virtual agent (red car); (B) Third person perspective of the exergame in action. The curved arrow guides the direction of the wrist rotation.
Participants’ scores are displayed on a console in front of them at all times. To prevent fostering unhealthy competition and influencing motivation through game-related feedback, no information about the winner or loser was provided (i.e., no in-game rewards). To tackle the issue of participants losing motivation, researchers have recommended using fixed or highly controllable win-loss ratios that the player remains unaware of Ibarra Zannatha et al. (2013).
The VR application used for this study integrates this feature (Najm et al., 2020). This is achieved by using participants’ real-time performance data (i.e., degrees of wrist rotation) and adjusting the virtual player’s agent’s movement based on this data through an algorithm, which incorporated a randomness in the agent’s score. Introducing this randomness was intended to create the impression that the virtual agents behaved more like humans and less like computer systems with consistent scoring patterns (e.g., above or below the participant’s current score). This randomness is programmed to range from +1 to +20° during the trials in which agents are overperforming and from −1 to −20° during the trials in which the agents are underperforming, with the baseline of this range being the corresponding performed degrees of the participant. Feasible game scores for each supination/pronation trial were bound within the range of 0–90°.
The VR application allows the research facilitator/therapist to regulate the win-loss ratio before each game session, in order to avoid having the users experience frustrating sequences of failures or monotonous streaks of successes, both of which can lead to a quick loss of interest (Levac, 2024). The win-loss ratio is one of the preset settings for each agent that can be defined through the user interface of the VR application, before the beginning of each game. In the presented study, the custom appointed overperforming and underperforming agents are set by the research facilitator to achieve a higher and lower score than the participant respectively, in three out of five rounds minimum.
2.2 Participants
The present study adopts an idiographic approach, in which data is collected and analyzed from a carefully selected group of chronic stroke survivor cases (Blampied, 2016). The study utilized purposive sampling, a method that involves the expert judgement of a physiotherapist to determine whether cases should be selected based on their relevance to the objectives of the study (Mohd and Abu Bakar, 2014). Single subject designs are commonly employed in stroke rehabilitation studies due to the substantial individual variations observed after stroke. The challenge arises from the difficulty in achieving a representative distribution of a large sample of chronic stroke survivors into groups that correspond to these variations (Slijper et al., 2014).
The physiotherapist expert identified five chronic stroke survivors (two females and three males) eligible for the VR intervention based on their medical history and a set of eligibility criteria. Specifically, the eligibility criteria included chronic stroke survivors who: i) were between 18 and 70 years of age, ii) had a restricted range of motion (supination/pronation) on the affected upper limb (Modified Ashworth Scale (MAS) (Meseguer-Henarejos et al., 2018) score:1–2), iii) were capable of maintaining and controlling a sitting position for at least 1 hour iv) had a sufficient mental and cognitive capacity for the VR task as determined by the Mini Mental State Examination (MMSE) with a score >23 (Folstein et al., 1975), v) had a history of one stroke event, vi) had no comorbidity with neurodegenerative or psychiatric conditions (e.g., multiple sclerosis, major depressive disorder, schizophrenia, etc.), vii) had no history of epilepsy or electroencephalographically documented seizures, viii) had no hearing impairments (i.e., deafness) or visual deficits (e.g., blindness, diplopia, glaucoma, blurred vision) affecting the use of VR, ix) had spasticity on upper limb but no more than a score of 2 (a marked increase in muscle tone throughout most of the range of motion, but affected part(s) are still easily moved) according to the MAS (Meseguer-Henarejos et al., 2018), x) had no motor coordination malfunction, and xi) had no aphasia as confirmed by individual medical files. The five participants agreed to the terms of the study, signed a consent form, and were assigned a unique identification number.
2.3 Research design
Motor rehabilitation typically extends over several months, making repeated measures over long periods beneficial. This approach is necessary because parameters relevant to this research, such as motricity measures, can vary over time. Additionally, the study was designed as an exploratory multiple-case study, incorporating both qualitative and quantitative data. This data was collected in parallel, analyzed separately, and then combined to provide comprehensive insights through triangulation.
In the control condition (treatment A0) participants engaged in gameplay in a solitary setting without a virtual agent present. In the two-player setting of the VR exergame, the two experimental conditions (treatments A1 and A2) involved a virtual player agent, who could be seen in the virtual environment sitting across from the participant during gameplay while co-acting. The virtual player agent A1 was set to consistently outperform the user’s (participant’s) total game session performance while the virtual player agent A2 was set to consistently underperform the user’s total game session performance. To avoid monotonous failures or successes within each session that could exacerbate user frustration or loss of interest as previously explained, the performance of each agent varied during gameplay. In the A1 treatment, in the majority of game rounds (that is in at least three out of five) the virtual agent outperforms the user, while in A2, in the majority of game rounds, the virtual agent underperforms compared to the user. Participants and virtual agents take turns playing the game, with the agent having a delay of 0.4 s before reacting, following the participant’s turn.
Participants experienced all three treatments (A0, A1, A2) during each visit in a counterbalanced order. The order was randomized using the ABC alternating treatment design (ATD) (Graham et al., 2012). This approach ensures that the sequence of the different treatments does not affect the performance results (e.g., influence of initial warm-up or late-session fatigue) (Solmi et al., 2014). Table 1 shows the order of treatment for each participant. Each case study lasted 6 weeks, with each participant visiting the physiotherapy unit twice a week.
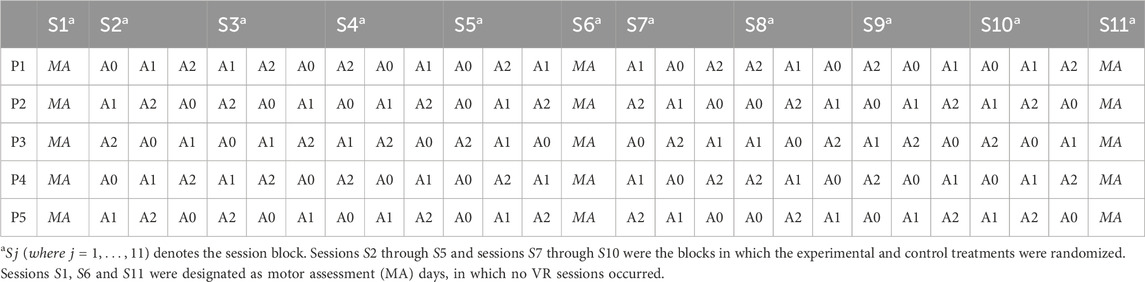
Table 1. The experimental design. Line-up of alternating treatments (A0-no agent, agent A1, agent A2) and motor assessments (MA) per participant
Additional information about the current setup and experimental design is provided in the Supplementary Video file (Multimedia Supplementary Appendix A).
2.4 Procedures
Participants visited the physiotherapy unit twice a week, where they took part in three game sessions per visit (Table 1). These game sessions were integrated into their regular physiotherapy schedule.
During the first session (S1), each participant underwent motor assessments (MA) (see Measures), conducted by an expert physiotherapist from the Physiotherapy Unit. During the second session (S2), participants, assisted by a healthcare professional if needed, sat comfortably in a chair. They were given information on the VR equipment and received instructions on how to play the game. They were informed of the potential risk of mild nausea or dizziness from using VR, and they were reminded of their right to withdraw at any time for any reason. The motion tracking sensor was then attached to the wrist of the impaired arm, and the VR headset was fitted on the participant’s head. The equipment was calibrated for each participant accordingly. Once inside the VR environment for the first time, participants were guided through a brief tutorial that introduced the tabletop car racing platform and explained the functionality of the scoring console and floating arrows that directed wrist rotation direction.
After addressing all questions, participants were randomly exposed to one of the three treatments (A0 - no agent, agent A1, or agent A2). Each treatment was comprised of 5 game rounds. Each game round lasted approximately 2 min depending on the level of wrist impairment for each participant. During each game round participants performed 10 repetitive movements (1 supination and 1 pronation in alternation, repeated 5 times). For each of the three treatments participants performed in total 25 supination and 25 pronation maneuvers of the impaired hand while playing. This resulted in a total of 150 supination/pronation maneuvers across conditions, equivalent to the amount typically performed in their weekly physiotherapy session.
A short 5-min break followed each treatment. After the break, participants were exposed to the remaining treatments. This approximately 10-min procedure was repeated until all three treatments were completed. At the end of all treatments, the experimenter helped the participant to remove the equipment and, after scheduling the next session, the participant left.
On the remaining session days, except for S6 and S11, the participants followed the same routine (Table 1). During S6, a reassessment of motor functions was conducted, similar to the one performed during S1. On the final session day (S11), the participant underwent a final motor assessment and completed a final short questionnaire.
2.5 Response variables/measurements
A series of measurements were administered to participants at various time points throughout the treatment to assess psychometric factors such as competitiveness, experience with the VR system, and task engagement, as well as game performance and overall motor functionality. These assessments were based on data collected through the system during treatment as well as pre- and post-treatment subjective questionnaires, some of which were completed by the physiotherapist. Detailed information on these measurements and the response variables are provided below.
2.5.1 Game performance
A game performance score was continuously being registered by the system during gameplay, which corresponded to the total degrees of movement in the impaired upper limb during supination and pronation maneuvers. The wrist joint was kept stable, and the elbow joint was flexed at 90°, supported on the desk. Participants could perform up to 90 degrees of movement for each supination and pronation, with one point scored for each degree of movement. The degrees of movement were shown to participants in real-time using a curved arrow gauge, which guided the wrist rotation direction and filled up when the user performed the wrist maneuver indicated by the arrow (Figure 1B). If the hand was misplaced or a wrong movement was performed, the alarm rang, notifying participants to reset their forearm position. No penalties were applied in this case and all scoring points earned during gameplay were retained. The game scoring output file recorded the scores for each of the 10 repetitive maneuvers that made up a game round, as well as their total sum (see Procedures). The overall score for each treatment (A0 - no Agent, agent A1, or agent A2) on a given session day, was extracted after data collection. The final overall score for each participant ranged from 0 to 4,500 points for each treatment.
2.5.2 Fugl-Meyer motor assessment
The Fugl-Meyer Assessment for the upper limb (FMA-UE) (Duncan et al.; Fugl-Meyer et al., 1975) was used by the physiotherapist to assess motor function progress at baseline (S1), mid-treatment (S6), and post-treatment (S11). The FMA-UE is a stroke-specific, performance-based impairment index designed to assess motor functioning, balance, sensation, range of motion and joint pain. It uses a 3-point ordinal scale for each item (0 = no performance, 1 = partial performance, 2 = full performance) with 66 being the maximum total score for the upper limb. Higher values indicate better motor performance.
2.5.3 Modified Ashworth Scale motor assessment
The MAS (Meseguer-Henarejos et al., 2018) has been used pre-, mid-, and post-treatment to measure the resistance experienced during passive range of motion (Gregson et al., 1999). The assessment involves passively extending the participant’s limb with the therapist’s help from a fully flexed to a fully extended position, assessing the resistance felt during movement. The MAS is a 5-point scale, where a score of 0 indicates no increase in muscle tone (i.e., the muscles move normally without any resistance), and a score of 4 represents limb rigidity in flexion or extension (i.e., the highest level, where the limb cannot be moved in flexion or extension). Higher values indicate worse motor performance.
2.5.4 The range of motion motor assessment
The Range of Motion (ROM) assessment was used to measure the flexibility and mobility of the impaired elbow and wrist joints Lea and Gerhardt (1995). It assesses the degree to which a joint can move through its normal, full motion, both actively (by the individual) and passively (with assistance from the therapist). The ROM method involves using a goniometer to measure the angle between the bones at a joint. The individual is placed in a relaxed position with their arm stationary. The therapist aligns the goniometer’s arms with the bones and moves the joint through its range of motion, recording the degrees of motion. The values obtained during the ROM assessment are compared to normal, established values for each joint. ROM values can be full or normal ROM, decreased ROM (if the joint does not reach the normal value), or increased ROM (if the joint exceeds normal values). Higher values indicate better motor performance.
2.5.5 Task engagement and Post-VR experience
During the short break at the end of each treatment, participants completed two short questionnaires assessing their level of task engagement and the sense of presence within the virtual environment. Task engagement was assessed using the short survey for Measuring the Momentary Account of the Individual’s Experiences (Shernoff et al., 2014) – questionnaire Set 1 (interest, enjoyment, concentration) and Set 2 (immersion, challenge, skills). Participants rated their agreement with statements related to these parameters (such as “To what extent did you find the task enjoyable?”) on 5-point Likert (1 = not at all to 5 = very much). The questionnaire scores are averaged to obtain a total score, where higher scores generally indicate more positive experiences or higher levels of engagement.
The VR experience was assessed using validated subscales of VR presence, specifically focusing on place illusion (PI) and plausibility of virtual humans (PoVH) (Steed et al., 2018). Items on these scales include statements such as “To what extent were there times during the experience when the [situation] was the reality for you” for PI and “How much did you behave as if the virtual people were real?” for measuring PoVH. Participants rated their agreement with statements related to these parameters on a 7-point Likert scale (1 = not at all or least agreement to 7 = very much or most agreement). The set of questions is provided as Supplementary Material (Multimedia Supplementary Appendix B). The PoVH questionnaire was administered only for treatments A1 and A2, but not in A0 where participants were in a solitary setting.
2.5.6 Competitiveness index scale
At the end of the final motor assessment session (S11), participants completed an additional questionnaire featuring the revised version of the Competitiveness Index scale (CI-R) (Houston et al., 2002). The CI-R assesses the personality trait of competitiveness, which could potentially influence game performance. Although the game did not explicitly convey competitive elements, such as declaring winner or a loser, the arrangement of players sitting across one another and facing each other might be perceived as competitive. This setup was intended to allow participants to observe the agent’s hand maneuvers and feel observed by the virtual agent, thereby introducing social facilitation and stimulating Mirror Neurons System (MNS) activation. The CI-R is scored by summing the responses to 14 items with five reverse-scored items. Total scores can range from 14 to 70. We used the CI-R scoring for comparing competitiveness between participants. There was an additional ad hoc questionnaire, which targeted participants’ personal view on car racing, relevant to the theme of the presented exergame. Specifically, the participants were inquired about the degree of finding car racing i) exciting, ii) purposeless, and iii) stressful on a 5-point Likert scale (1 = not at all to 5 = very much) - with questions 2 and 3 being reverse-scored. The sets of questions described are provided as Supplementary Material (Multimedia Supplementary Appendix C).
2.5.7 Observational data
Participants were encouraged to express out loud any thought relevant to the intervention. Behavioral observations reflecting the participant’s explicit reactions towards the agent were recorded additionally by either the research facilitator or professional physiotherapist and later transcribed into digital format by the research facilitator.
2.6 Technology
Participants were fitted with an Oculus Rift (CV1) head-mounted display. This has PenTile OLED 2,160 × 1,200 displays (1,080 × 1,200 per eye) running at 90 Hz. It has integrated 3D audio headphones and weighs 470 g. To control participants’ upper body movements (hand tracking), they were fitted with an Xsens Wireless Motion Tracker (MTw) on their impaired right dominant hand (Movella, 2025).
2.7 Data analysis
Game performance data were compiled from the VR application’s text log files, organized and cleaned into spreadsheets to extract individual participant information including overall usage duration of the exergame, number of game sessions completed, and game performance. Data from questionnaires and motor assessments were manually transcoded into the same format. The final analysis was done using STATA 13 (StataCorp LLC, 1994). Game performance and task engagement across treatment sessions were utilized to generate ATD graphs. Other self-report variables measured immediately after each treatment (e.g., PI and PoVH) were found to be consistent across all participants during the pre-analysis stage and they were analyzed as constant psychometric measures alongside CI-R and the ad hoc questionnaire. Subsequently, we performed simple linear regression (ANOVA) on all cases with sufficient data, employing an alpha level of 0.05.
3 Results
Table 2 presents an overview of participants’ data and psychometric measures. Firstly, all 5 participants were found to have a medium to low level of competitiveness based on the CI-R questionnaire and a mostly neutral attitude towards car racing based on the ad hoc questionnaire.
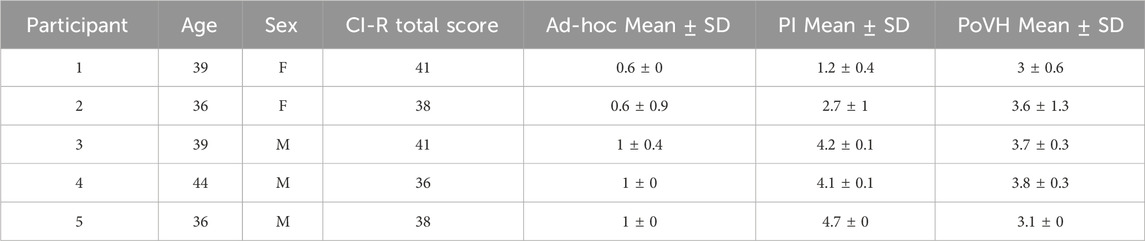
Table 2. Participants’ data and psychometric measures for competitiveness, attitudes towards racing, and post-VR experience.
Regarding the VR experience (PI) and attitude towards the virtual agent (PoVH), the analysis showed that participants’ questionnaire scores remained constant throughout the various sessions and the treatments (see Supplementary Material). Hence those were averaged, and a single score was retained per participant. The results (Table 2) indicate that, overall, participants had average levels of place illusion and acted indifferently towards the performance of the virtual agents, in the treatments where the agents consistently overperformed (A1) or underperformed (A2) compared to them.
Similarly, for game performance and task engagement, the results showed that treatments A1 and A2 did not differ across sessions (see Supplementary Material). Therefore, A1 and A2 were averaged to form a single experimental treatment (A), representing the presence of a virtual agent in the virtual environment. In our analyses, preliminary paired comparisons (ANOVA and visual inspection of the ATD graphs) revealed no statistically significant or practically meaningful differences in either game performance or task engagement between the over-performing (A1) and under-performing (A2) agent conditions. Consequently, we consolidated A1 and A2 into a single “agent” condition (A) to focus the analysis on the core contrast of virtual co-action versus solitary play (A0) and to maximize statistical power within our small-N, single-case design. Maintaining A1 and A2 as separate conditions would have necessitated redundant comparisons, increasing the risk of Type I error due to multiple testing on a very small sample. The present approach ensures that our findings represent the impact of a co-present virtual agent on patient engagement and perseverance, without obscuring any genuine subgroup effects. For the remainder of the results’ section, and for each participant case, treatment A is compared to the baseline treatment (A0) to assess the effects of social facilitation in the form of co-action mediated by the presence of a virtual player agent overtime, independent of the agents’ performance outcome.
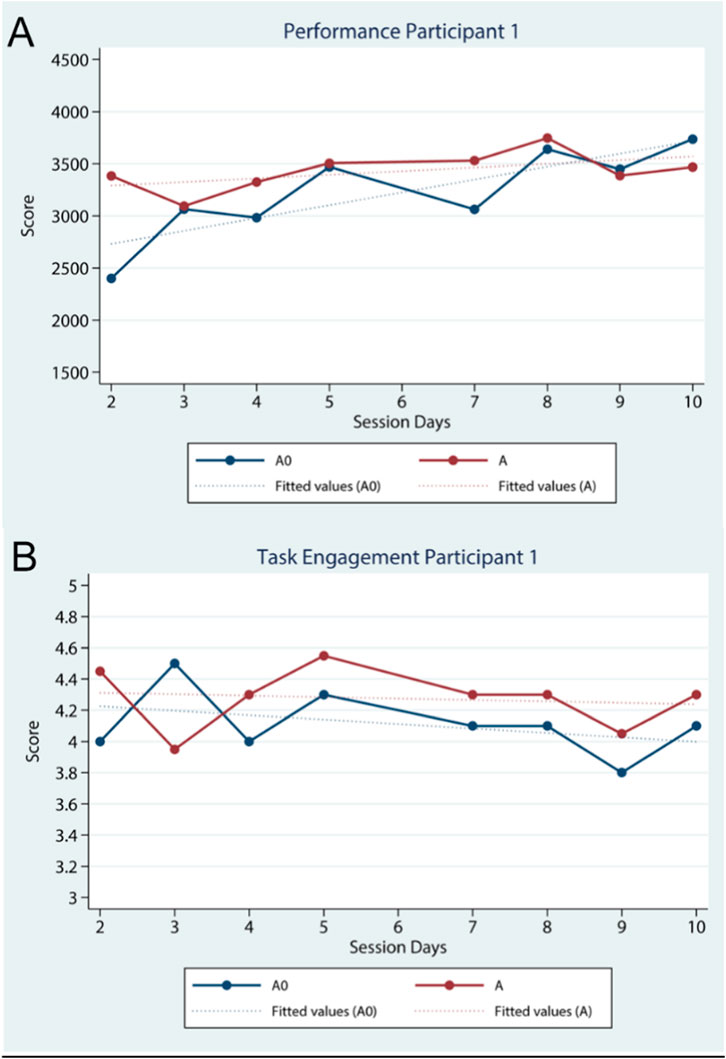
3.1 Participant 1
Participant 1 is a female 39 years of age and unfamiliar with VR technology. She adhered to the weekly schedule for the first half of the study and missed one appointment for the latter half. Nevertheless, she successfully completed all 11 sessions. The ad hoc questionnaire reveals that she has a negative view towards car racing (Table 2). She reported having extremely low levels of PI and moderate to low levels of PoVH throughout the study (Table 2). The results suggest that her game performance, as measured by overall scores, gradually improved with treatment A0, in contrast to treatment A, which had no significant impact on game performance throughout the study (Figure 2A). The linear regression model reveals a significant and highly positive relationship between session days and the participant’s game performance, but only under treatment A0, R2 = 0.68, F (1,6) = 12.96, p < 0.01. Regarding task engagement, treatment A consistently sustained her engagement at a higher level compared to treatment A0 from S3 onwards (Figure 2B). Although the linear regression model does not draw accurate predictions about the relationship between session days and her task engagement in either condition, the qualitative observations support these findings: during session 9, Participant 1 spontaneously told the facilitator that watching the virtual agent’s maneuvers was beneficial for her. This verbal feedback triangulates with her engagement data–she felt the co-player helped keep her engaged–even though her highest performance gains occurred in the solo condition. In summary, for Participant 1 the presence of a virtual co-actor boosted her engagement (as she herself noted), but did not translate to higher game scores in that condition.
In terms of rehabilitation outcomes, Participant 1 demonstrated clear improvement in her affected upper limb functionality over the course of the intervention. Her FMA-UE score increased from 23 at baseline (S1) to 28 at mid-intervention (S6), reaching 36 by the final session (S11), indicating substantial motor recovery (Table 3). Consistently, the range of motion (ROM) in her affected elbow and wrist improved in both passive and active movements (Table 3). Notably, the passive and active ROM gains mirror her high engagement with the exercises. A slight increase in muscle tone (MAS score) was recorded for the examined muscle groups (Table 3), which could be a side effect of improved activation. Overall, her committed participation and the qualitative feedback that the virtual agent helped her likely contributed to her sustained engagement and, in turn, her functional gains.
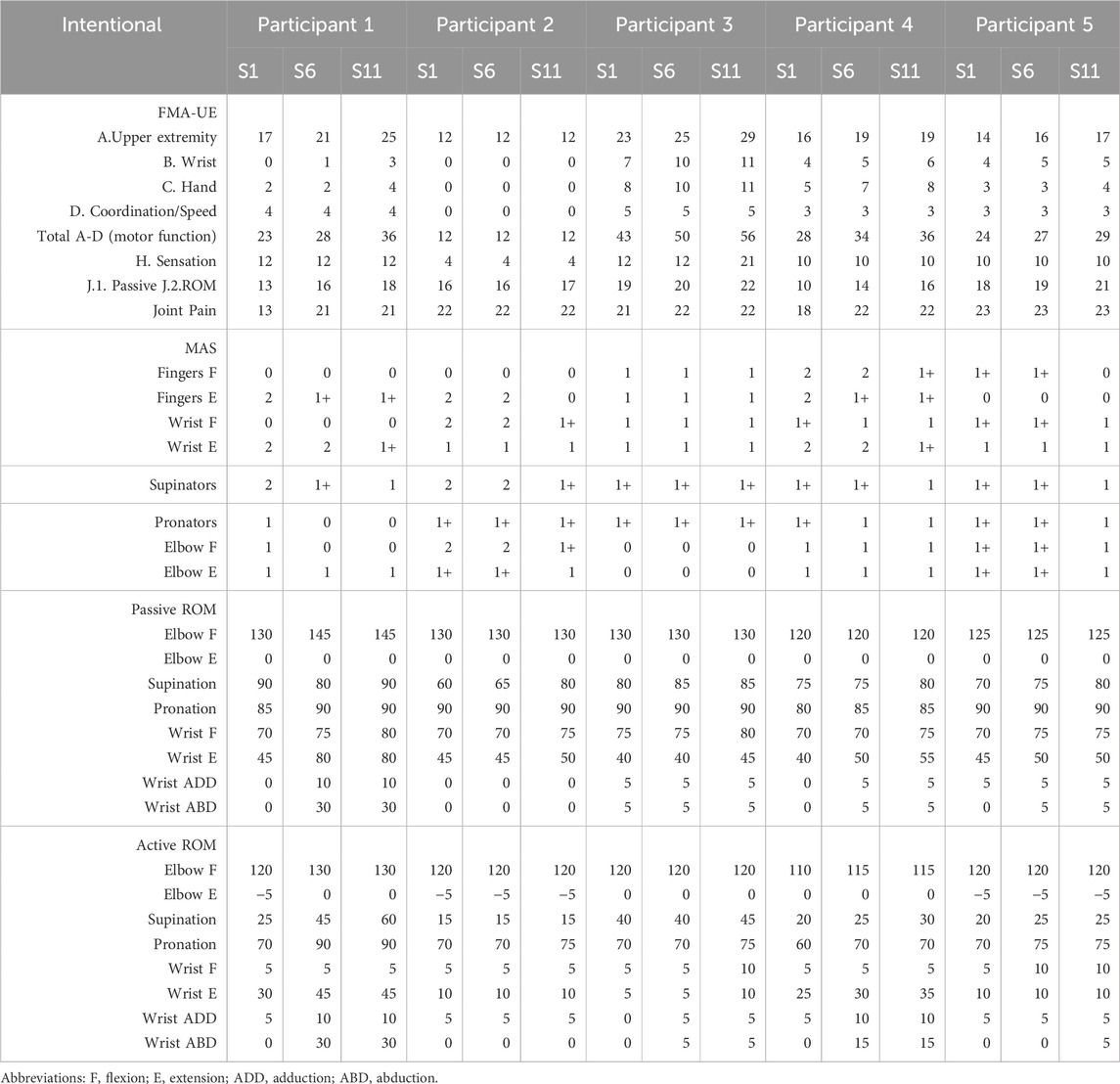
Table 3. Overview of the motor assessment results FMA-UE, MAS, and passive and active ROM at S1 (pre-), S6 (mid-), and S11 (post-intervention) for each participant.
3.2 Participant 2
Participant 2 is a 36-year-old female who was unfamiliar with VR technology. She initially kept to the weekly schedule but struggled to maintain consistency as the study progressed. Due to personal factors, she missed her 10th session (S10) and did not complete it thereafter, effectively withdrawing before the final assessment. In hindsight, the research facilitator determined that Participant 2’s game performance data should be excluded from the quantitative analysis, as she required substantial assistance from the physiotherapist during gameplay. This reliance on external help compromised the validity of her performance scores, leaving those data incomplete. To maintain analytical rigor, these compromised performance metrics were omitted from our statistical results. However, her qualitative feedback and observational notes were retained and are fully reported here, since she was exceptionally expressive and her comments provided valuable insight into her experience.
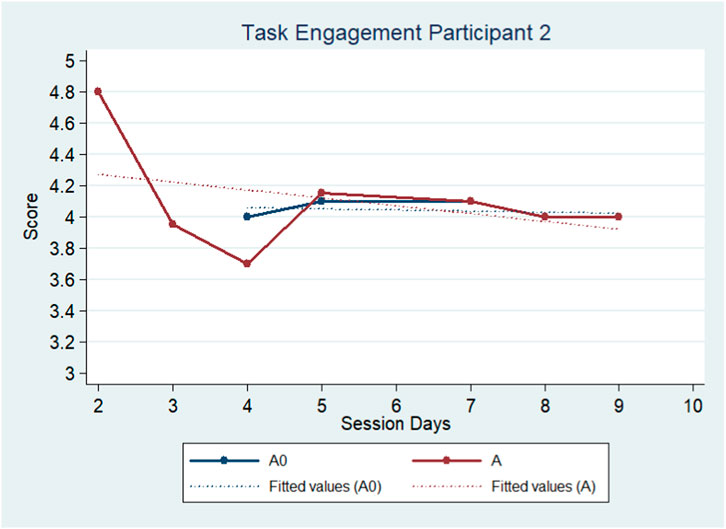
Despite her dropout, Participant 2 remained an interesting case due to this expressiveness compared to all other participants. Her ad hoc questionnaire responses indicated a neutral-to-negative view of car racing (Table 2). Early on, she appeared friendly and even enthusiastic about the virtual agents; however, observational data revealed a notable shift in her demeanor over time. By session 4, she expressed frustration to the facilitator about the repetitive questionnaires and the lack of variety in game modes, suggesting boredom and waning motivation. This coincided with a decline in her adherence and engagement. In fact, as the sessions went on, her interactions toward the virtual co-players became increasingly negative–at one point in session 7 she was heard cussing at the high-performing virtual agent when she felt pressured to adjust her pacing to the agent’s. These behaviors were reflected in her quantitative engagement data: her task engagement scores showed an overall downward trend across sessions (Figure 3). Unlike the other participants, the presence of a virtual agent did not consistently enhance her engagement; instead, she became less engaged over time, likely due to mounting frustration. By session 9, however, Participant 2 offered a mixed perspective. She told the facilitator that observing the virtual agents’ maneuvers had been helpful to her (similar to Participant 1’s remark), indicating that she did recognize some benefit in watching the co-player. She also mentioned wishing she could use her personal Functional Electrical Stimulation (FES) device during the VR training–a request that could not be accommodated due to the study protocol. These comments suggest that while she grew irritated with certain aspects of the study, she still valued the guidance provided by the virtual agent. Quantitatively, no formal regression analysis was performed on her engagement or performance trends due to the missing data from her dropout.
It’s important to note that her game performance scores were excluded from analysis because she required substantial physical assistance from the physiotherapist to complete the game tasks, which artificially inflated her scores. In summary, Participant 2’s case illustrates a contrast between qualitative and quantitative data: her increasing boredom and frustration (qualitative observations) corresponded with dropping engagement levels and eventual non-completion (quantitative outcomes), underscoring how negative perceptions can undermine rehabilitation participation. Yet paradoxically, she verbally acknowledged some positive influence of the virtual co-player, highlighting a complex interplay between her subjective experience and performance.
Consequently, Participant 2 showed no significant improvement in clinical motor outcomes over the study period. Her total FMA-UE motor score remained essentially unchanged (Table 3), reflecting a lack of functional gain in her affected arm. This lack of progress aligns with her inconsistent participation and the need for external assistance during exercises. The ROM assessments recorded only a slight increase in passive wrist/elbow movement and virtually no change in active ROM (Table 3), indicating minimal improvement in flexibility or voluntary control, perhaps due to insufficient therapeutic exercise. Additionally, her muscle tone tended to increase (MAS). The qualitative observations help explain these outcomes: her boredom with the task and eventual dropout meant she did not fully engage in the rehabilitation exercises, resulting in little to no physical improvement. Participant 2’s experience suggests that without sustained engagement (and with mounting frustration), the benefits of the VR intervention on motor function could not be realized in her case.
3.3 Participant 3
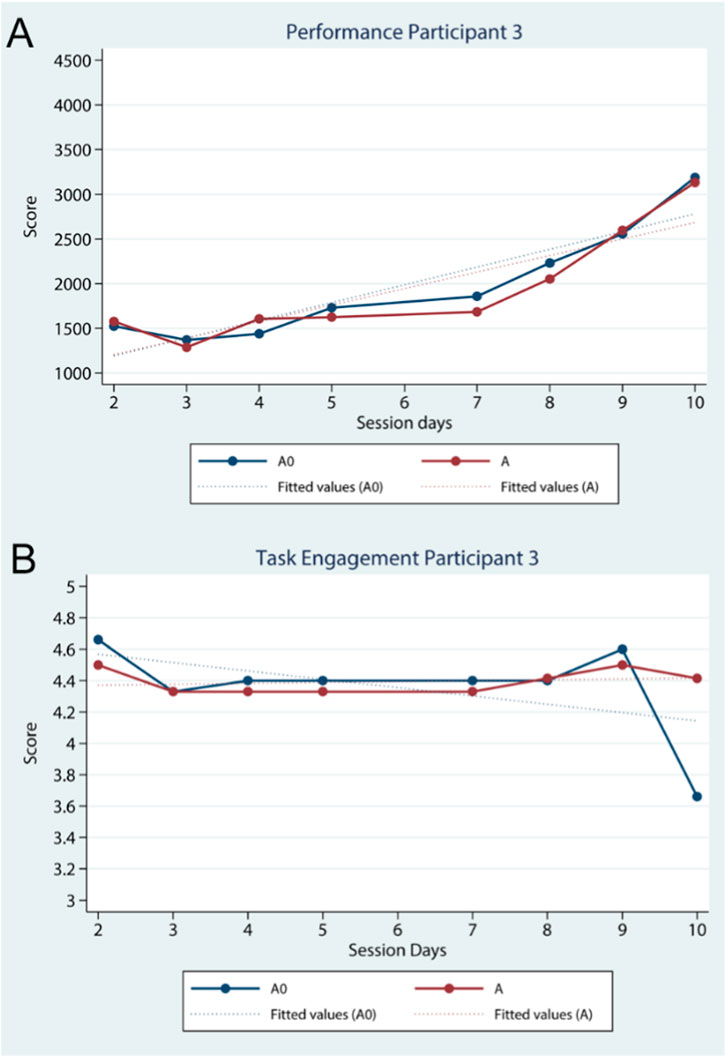
Participant 3 is a male 39 years of age and unfamiliar with VR technology. Throughout the study, he adhered to the weekly schedule. He reported a neutral-to-positive attitude toward the car-racing game theme (Table 2), which may have set a favorable tone for his engagement. Quantitatively, both his game performance and task engagement were high and steady throughout the intervention. Initially, his game scores were low in both the no-agent (A0) and agent (A) conditions, but he demonstrated a steady improvement in performance in both conditions over time (Figure 4A). By the later sessions, his scores had increased considerably, and importantly, the improvement trend was nearly identical whether or not a virtual co-player was present. Simple linear regression confirmed a significant positive relationship between session number and performance for both conditions (for A0: R2 = 0.84, F (1,6) = 32.90, p < 0.01; for A: R2 = 0.76, F (1,6) = 19.08, p < 0.01). In terms of engagement, Participant 3 started the study with a high level of task engagement in both conditions and maintained this high engagement throughout (Figure 4B). Aside from a notable dip during his final solo session (S10 in A0, where his engagement momentarily dropped), his engagement ratings for both conditions remained consistently high and closely aligned. The regression analysis did not find a strong time-related trend for engagement (likely because his engagement was near-ceiling from the start), which qualitatively suggests he was intrinsically motivated. Observationally, he remained focused on the tasks, following instructions without notable distraction. His steady improvements in performance and consistently high engagement imply a strong personal drive and comfort with the training scenario.
Regarding upper limb motor function, Participant 3 achieved measurable improvements over the intervention period. His FMA-UE score rose from 43 at baseline to 50 at mid-study and further to 56 by the end (Table 3), indicating significant recovery progress given his relatively higher starting function. Correspondingly, his wrist’s ROM increased modestly in both passive and active measurements for wrist joints (Table 3), reflecting improved flexibility and control. The MAS showed no change in muscle tone for the examined muscle groups (Table 3).
3.4 Participant 4
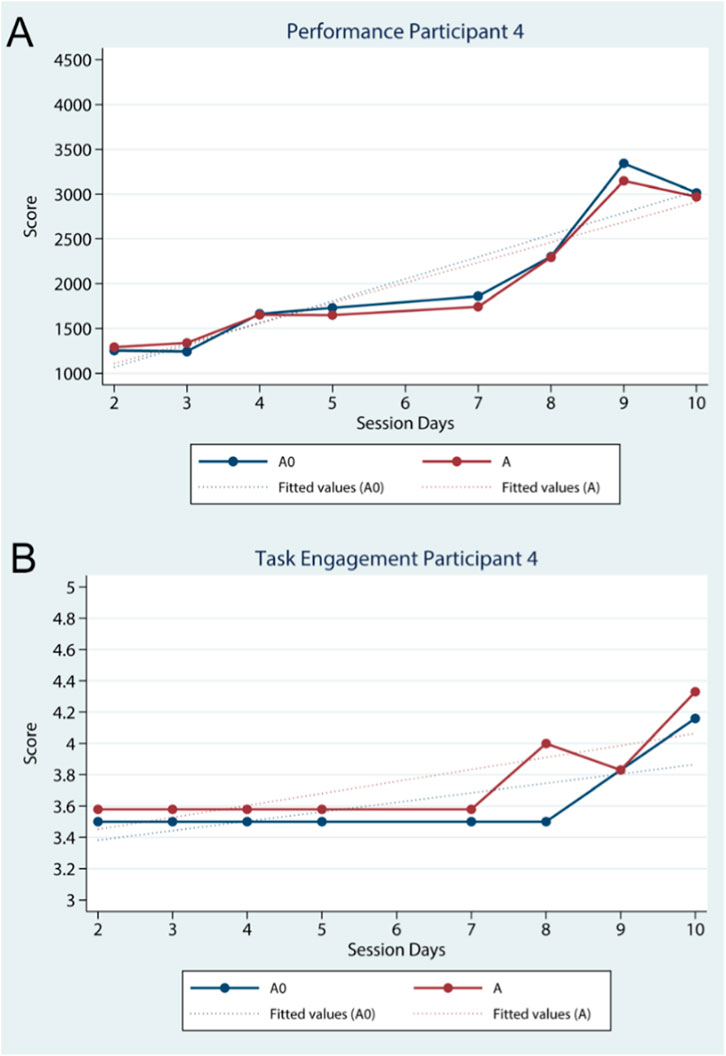
Participant 4 is a 44-year-old male with no prior VR experience. He completed all the training sessions on schedule. He reported a neutral attitude toward car racing in the ad hoc questionnaire (Table 2) and was the least competitive participant (based on CI-R scores). At the start of the program, Participant 4’s game performance was very low (initial session scores below 1,500 points per game). However, over time he showed a marked improvement in performance, and this improvement was consistently seen in both A0 and A conditions (Figure 5A). By the later sessions, his scores in both conditions had climbed substantially, indicating that he was learning and improving at the game regardless of the presence of a co-player. The linear regression model reflects this pattern: there was a highly significant positive correlation between session number and performance for both A0 (R2 = 0.85, F (1,6) = 35.58, p < 0.01) and A (R2 = 0.85, F (1,6) = 33.44, p < 0.01.), highlighting robust practice effects in his case. Similarly, in terms of task engagement, Participant 4 started off with relatively low engagement in both conditions, likely mirroring his initial difficulties with the game. Notably, around the midpoint of the intervention, his engagement levels began to rise (Figure 5B). After session four or 5, as he became more familiar with the task, his engagement increased in both conditions–and by the end of the training, his engagement in the agent-present condition (A) was higher than in the no-agent condition (A0). The linear regression confirmed a significant upward trend in engagement over time for both conditions (A0: R2 = 0.52, F (1,6) = 6.51, p = 0.04; A: R2 = 0.64, F (1,6) = 10.63, p = 0.02), consistent with his observed growing involvement. Qualitatively, Participant 4 did not provide explicit verbal feedback during the training as he generally followed the protocol quietly.
With respect to clinical motor outcomes, Participant 4 made observable gains in his affected limb. His total FMA-UE score improved from 28 at baseline to 34 by mid-intervention and to 36 in the final evaluation (Table 3), indicating an enhancement in motor function. In line with these improvements, the ROM at his wrist increased on both passive and active measures (Table 3), suggesting improved flexibility and active control. He did exhibit a slight increase in muscle tone in the wrist and finger flexors (MAS), but this was minor.
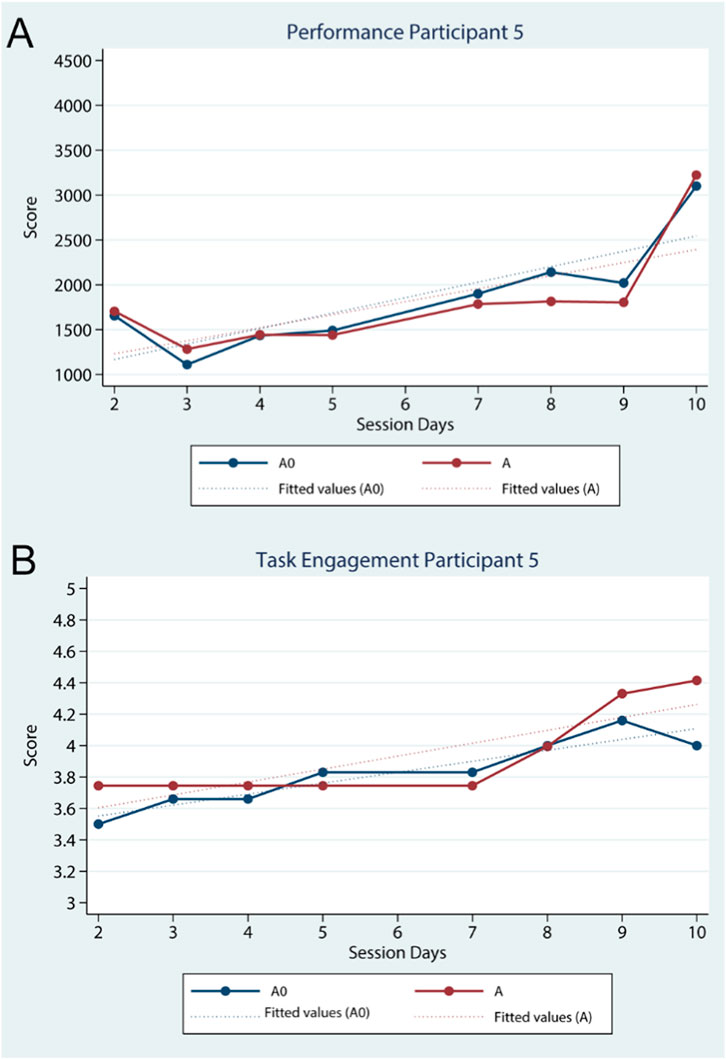
3.5 Participant 5
Participant 5 is a male 36 years of age and unfamiliar with VR technology. Throughout the study, he adhered to the weekly schedule. The ad hoc questionnaire revealed that he held a neutral perspective towards car racing (Table 2). Quantitatively, his game performance was low at the outset but steadily increased over time in both treatments A0 and A (Figure 6A). The linear regression model confirmed a significant positive relationship between session number and performance for A, R2 = 0.49, F (1,6) = 5.89, p = 0.05, and a significant positive relationship for treatment A0, R2 = 0.69, F (1,6) = 13.54, p = 0.01. Likewise, task engagement improved throughout the study, with treatment A demonstrating the most notable increase by the final session (Figure 6B). Additionally, the linear regression model predicted a highly significant positive relationship between session days and task engagement for both treatment A0, R2 = 0.87, F (1,6) = 41.41, p < 0.01, and treatment A, R2 = 0.71, F (1,6) = 14.80, p < 0.01.
Regarding upper limb motor assessment, Participant 5 demonstrated modest but consistent motor improvements in upper limb functionality. The FMA-UE results suggested that the total upper limb motor functionality score steadily increased from 24 at S1 to 27 during S6 and 29 at S11 (Table 3), reflecting better coordination and strength in his affected arm. The MAS scale showed only a slight increase in wrist and finger tone. Correspondingly, the ROM assessments indicated a general modest increase in both the passive and active wrist ROM (Table 3).
4 Discussion
In these five case studies, we explored the impact of virtual agents as social facilitators on the exercise quality of chronic stroke survivors using immersive VR. Specifically, we examined their effects on game performance and task engagement. As (Koster, 2004) argues, the enjoyment we derive from playing games (‘fun’ factor) can often be traced to the learning of patterns that our brain absorbs during gameplay. In this respect, every game perceived as enjoyable is also educational and social interactions during gameplay–similar to those in real life–can enhance the learning process. Building on this idea, both rehabilitation training and games can support motor learning, with social elements further enhancing it depending on the context and individual differences. The intervention we presented demonstrated the impact of virtual agents on chronic stroke survivors’ game performance and task engagement after using the application across eight session days over a 6-week period. Notably, improvements in the participants’ supination and pronation maneuvering were observed, both with and without the co-presence of the virtual peer.
The presence of a virtual agent appeared to increase attentiveness to the exercise, as seen in task engagement outcomes. Engagement improved for all participants except Participant 2, whose data were insufficient for valid assessment. Notably, Participant 1 showed clear differences in engagement between the no-agent (A0) and agent (A) conditions, despite reporting low perceived plausibility of virtual humans in the environment. For Participant 1, task engagement through social facilitation was higher compared to the baseline treatment without a virtual agent, but there was no significant correlation with time. Participant 3 exhibited a less distinct relationship between task engagement and time. Task engagement in the no-agent (A0) and agent (A) treatments was nearly equivalent throughout the intervention, except for the final session day, where there was a sharp decline in engagement during the no-agent treatment (A0). For participants 4 and 5, task engagement through social facilitation appeared unrelated to time and was negligible compared to baseline treatment until the fourth session. After that, the virtual agents positively influenced task engagement, leading to an increase that surpassed baseline levels. These observations are in line with the work of Belletier et al. (2019), which highlights that social co-presence can positively affect attentional mechanisms in familiar tasks and may play a crucial role in neuronal modulation. Regarding game performance, the introduction of a virtual agent in the rehabilitation training had a minimal impact on participants, which also aligns with past research (Emmerich and Masuch, 2018).
Overall, the personality of all participants was found to have a moderate level of competitiveness, which may explain why no significant differences were observed between the treatment with the overperforming virtual agent (A1) and the treatment with the underperforming virtual agent (A2). We hypothesize that participants either rejected competition due to stress or felt their physical limitations preventing them from matching their effort to the perceived challenge of surpassing each virtual agent’s score. Nevertheless, their moderate to low level of competitiveness suggests that they were more likely to choose to reject competition. Participant 1 was the only one who demonstrated competitive tendencies based on her performance scores. However, by the end of the intervention period, her effort allocation shifted, with more effort invested in the no-agent solitary treatment rather than those involving the agent. Other researchers (Muller and Butera, 2007) suggest that the presence of co-acting peers can create a potential self-evaluation threat, leading to evaluation apprehension. They propose this as a possible explanation for changes in attention that lead to social facilitation or inhibition. In line with this argument, we suggest that the participants’ avoidance of competition in this study was a response to the self-evaluation threat, as they sought to mitigate competition-related anxiety. This seems even more plausible considering that avoiding competition can alleviate cognitive load. Specifically, choosing a non-competitive stance towards the agent eliminates the cognitively taxing impulse to constantly compare game scores. Therefore, we infer that the observed avoidance of competition likely resulted from a self-evaluation threat combined with participants’ state of psychic entropy.
It is important to note that rehabilitation exergame interventions may not be suitable for all chronic stroke survivors due to individual personality traits. For example, participant 2 appeared to become easily bored with repetitive tasks and following instructions. She was also sensitive to others’ behavior in the physical space and among the least competitive participants. These characteristics suggest that alternative rehabilitation approaches, which allow for greater autonomy, might be more appropriate for such cases (Charles et al., 2020).
In rehabilitation exergames, we suggest that virtual agents should complement other engagement drivers, such as in-game rewards and intrinsic motivation. Participants’ limited interest in the agents’ performance may reflect a lack of lusory attitude, common in rehab contexts. With no in-game incentives and given Participant 3’s consistently high engagement and moderate increases in Participants 4 and 5, we infer their motivation was primarily intrinsic, driven by personal rehabilitation goals.
The insights of the present study extend social facilitation theory into the domain of digital health, suggesting that human-like coaction can be emulated in immersive VR to encourage patients to persevere during monotonous rehabilitation exercises. Importantly, our results have direct practical implications for stroke rehabilitation. For stroke survivors, the inclusion of a virtual co-actor in therapy can make training more enjoyable and motivating, potentially improving adherence to long-term exercise programs by reducing feelings of isolation and boredom. For physiotherapists and rehabilitation designers, this approach offers a scalable, low-resource means of incorporating beneficial social interaction into therapy–a single clinician or system can deploy virtual partners to multiple patients without needing additional human trainers, thereby bringing the motivational advantages of group or partner training into individual rehabilitation sessions. In sum, by showing that a co-present virtual agent can foster greater engagement and perseverance without the downsides of competitive pressure, this work contributes to the scientific understanding of VR social facilitation and provides actionable guidance for future rehabilitation program design. Integrating virtual agents to simulate human-like coaction emerges as a promising strategy to enhance patient motivation and adherence, ultimately informing next-generation rehabilitation interventions that leverage social presence to improve outcomes.
4.1 Limitations
The primary limitation of these 5 case studies is that they heavily relied on self-report measures with the exception of the game performance scores, which revealed no significant changes over time, other than the expected outcome of showing a gradual overall improvement for most participants. While self-reports are useful for collecting a large amount of data within the time constraints imposed by the study interventions, they depend on the participants’ introspective ability and are prone to bias. Furthermore, the number of observations was limited by the participants’ workload and availability. Although the data provided valuable insights, they were mostly quantitative. Participants exhibited fewer explicit reactions towards the virtual agents than anticipated, based on prior pilot trials. Notably, behavioral data came exclusively from female participants in the form of game-relevant statements. In retrospect, the observed reactions were insufficient to offer a comprehensive understanding of participants’ internal processes, which could have been better explored through data triangulation to shed more light on their relationship with the virtual agents and interaction with the VR application. Moving forward, in future studies we plan to incorporate less quantitative measures to reduce participant workload and prioritize qualitative instruments, such as behavior-based interviews.
Furthermore, there may have been confounding variables that influenced both task engagement and game performance, such as occasional noise from passersby in the facility. Although the physiotherapy unit designated a special room for the study, the room served as a multipurpose space for staff, and relocating was not an option due to patient accessibility and equipment installation challenges. Another important confounding factor is that participants were allowed to receive additional rehabilitation training outside of the confines of this study, abiding by ethical research conduct, which could have affected the physiotherapy measurements.
The small sample size (N = 5) significantly restricts the generalizability of the findings. Such a limited cohort was a deliberate choice given the exploratory, idiographic approach of this research; in rehabilitation science, small-N single-case designs or case series are a well-established and appropriate approach, particularly in stroke recovery studies examining novel interventions or facing recruitment challenges. Indeed, comparable VR-based rehabilitation studies have been conducted with similarly small samples (Lobo et al., 2017) – for example, a recent immersive VR training case series in chronic stroke included only five participants (Marks et al., 2025) – underlining that our methodology aligns with common practice in the field.
A minor limitation was the necessity to use two agents with different appearances in each pair, as the exergame lacked a suitable game mechanic that helps participants distinguish between the overperforming and underperforming agents during game sessions. While using the same (gender-matched) virtual agent for both A1 and A2 conditions would have been more robust from a research design perspective, our analysis showed that A1 and A2 yielded similar results. Consequently, the two conditions were combined, allowing us to rule out agent appearance as a potential confounding factor in this setup. Nevertheless, future studies should consider this limitation.
4.2 Comparison with prior work
The role of virtual agents as social facilitators in rehabilitation warrants further investigation, as it offers promising insights into maintaining the attentiveness of chronic stroke survivors during rehabilitation. It is important to note that social facilitation in healthy cohorts has been extensively studied over the past century (Brown et al., 2020). However, research on the impact of social facilitation and cognitive impairment on the executive attention of individuals with neurological disorders is limited. This gap is even more pronounced in studies addressing social facilitation in the context of rehabilitation exergaming, where researchers tend to focus on its effects on performance. For instance, Emmerich and Masuch (2018) found no significant relationship between social facilitation and game performance, a result that aligns with the findings of the present study. Therefore, we propose that social facilitation in VR exergaming should be re-examined from the perspective of its impact on executive functioning, rather than solely on motor performance (such as game scoring in the present study). VR technology, after all, has the potential to capture neurobehavioral responses to controlled stimuli and enhance the precision of neuropsychological assessments (Dahdah et al., 2017).
Furthermore, future studies on the gamification of rehabilitation should place greater emphasis on the impact of autonomy, individual preferences, and the sense of purpose in rehabilitation applications. All participants in this study had a generally neutral view of car racing, with the exception of Participant 1. After completing the study, she (Participant 1) suggested that the exergame could have been more thematically diverse to better engage female chronic stroke survivors like herself. Participant 2 echoed a similar sentiment during the second treatment session, asking if the game mode could be changed to something other than car racing. No noteworthy sentiments relevant to the intervention were noted among male participants. It appears that catering to personal preferences and instilling a sense of purposefulness in the individual through gameplay could have been more effective in predicting task engagement than relying on social facilitation. This is supported by participant 3, who reported enjoying the car racing theme the most among participants and also reported having the highest level of task engagement. Similarly, the study by Barak Ventura et al. (2019) identified the alignment of task nature and content with the personal preferences of (tele)rehabilitation patients as a potential factor influencing both task engagement and enjoyment. Evidence suggests that chronic stroke survivors’ mirror neurons show increased activation and demonstrate a greater capacity to reconnect synapses when observing activities in which they were actively engaging with before the stroke (Demarin and MOROVIĆ, 2014). It appears that personalizing gameplay and fostering a sense of purpose may be more effective in predicting task engagement than relying solely on social facilitation.
On a separate note, studies on VR stroke rehabilitation favor social interaction through the use of human-controlled avatars over computer-generated simulations. As mentioned in the introduction, this preference is understandable given the limitations in the behavioral realism of avatars, which affect social co-presence in VR. For instance, one study found that social co-presence is most convincingly achieved when communication from virtual agents is mediated through body language rather than verbalization (Kim and Jo, 2022). In general, the fidelity of simulation is a crucial factor in fostering social co-presence in VR, which, in turn, can enhance user performance (Strojny et al., 2020). To our knowledge, the use of virtual agents in VR rehabilitation, particularly as virtual physiotherapists, remains limited, as shown in the systematic review by Crowe et al. (2024) Nonetheless, key factors such as perceived realism and social co-presence elicited by virtual therapists are often neglected. Future studies should explore the psychosocial aspects of computer-generated human representations in VR, especially those that simulate physiotherapists, or other rehabilitation facilitators.
5 Conclusion
In conclusion, chronic stroke survivors with motor impairments experience greater benefits when engaging in an upper limb rehabilitation exergame alongside another player, even if the other player is virtual, compared to playing alone. This improvement is evident in terms of perseverance in reaching their rehabilitation goals, as supported by both psychological and physiological factors. From a psychological perspective, social facilitation suggests that the presence of co-acting peers can enhance attention to familiar tasks. From a physiological perspective, most participants exhibited mild improvement in the functionality of their upper limb. While the exergame intervention was effective in aiding rehabilitation progress, the imitation of physical performance by the virtual agents did not directly impact participants’ progress, except for strengthening perseverance. The generalizability of these findings is impeded by the idiographic approach of the study. Future research should further investigate the role of social co-presence in VR rehabilitation and its potential in maintaining perseverance in patients, especially focusing on executive functions.
Data availability statement
The datasets presented in this article are not readily available because all collected data, including non-identified, will remain secured for 2 years after the completion of the study and then will be destroyed as it is required by the research protocol approved by the Cyprus National Bioethics Committee (ΕΕΒΚ/ΕΠ/2019/108). Requests to access the datasets should be directed to Despina Michael-Grigoriou, ZGVzcGluYS5ncmlnb3Jpb3VAY3V0LmFjLmN5.
Ethics statement
The studies involving humans were approved by the Cyprus National Bioethics Committee (ΕΕΒΚ/ΕΠ/2019/108). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
CH: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Software, Validation, Visualization, Writing – original draft, Writing – review and editing. DS: Conceptualization, Investigation, Resources, Writing – review and editing. CK: Conceptualization, Investigation, Methodology, Software, Visualization, Writing – review and editing. DB: Data curation, Formal Analysis, Methodology, Project administration, Supervision, Validation, Visualization, Writing – review and editing. DM-G: Conceptualization, Data curation, Funding acquisition, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work has been funded through the scholarship of academic excellence granted to CH for his doctoral studies and the research and other activities budget ED-DESPINA MICHAIL-300155-310200-3319 granted to DMG by the Cyprus University of Technology. DB was supported by the Tamkeen NYU Abu Dhabi Funding Agency (#76 71220 ADHPG VP211). The APC fee is covered by the Cyprus University of Technology Open Access Author Fund.
Acknowledgments
Our special thanks to GET Lab researchers, Ali Najm for the clarifications provided and support on the technical aspects of the VR application and his help in preparation of some visual material, and Maria Christofi for her support in the preparation of the paperwork for the ethics committee. We also extend our gratitude to the Cyprus Institute of Neurology and Genetics for their collaboration in providing their space to run the study and their help in the participants’ recruitment.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/frvir.2025.1581240/full#supplementary-material
References
Alankus, G., Lazar, A., May, M., and Kelleher, C. (2010). “Towards customizable games for stroke rehabilitation,” in CHI 2010: Therapy and Rehabilitation, Atlanta, GA, April 10–15, 2010, 2113–2122.
Alex, M., Wünsche, B. C., and Lottridge, D. (2021). Virtual reality art-making for stroke rehabilitation: field study and technology probe. Int. J. Hum. Comput. Stud. 145, 102481. doi:10.1016/j.ijhcs.2020.102481
Allegue, D. R., Kairy, D., Higgins, J., Archambault, P. S., Michaud, F., Miller, W. C., et al. (2021). A personalized home-based rehabilitation program using exergames combined with a telerehabilitation app in a chronic stroke survivor: mixed methods case study. JMIR Serious Games 9 (3), e26153. doi:10.2196/26153
Allegue, D. R., Sweet, S. N., Higgins, J., Archambault, P. S., Michaud, F., Miller, W. C., et al. (2022). Lessons learned from clinicians and stroke survivors about using telerehabilitation combined with exergames: multiple case study. JMIR Rehabil. Assist. 9 (3), e31305. doi:10.2196/31305
AlMousa, M., Al-Khalifa, H. S., and AlSobayel, H. (2017). Requirements elicitation and prototyping of a fully immersive virtual reality gaming system for upper limb stroke rehabilitation in Saudi Arabia. Mob. Inf. Syst. 2017, 1–12. doi:10.1155/2017/7507940
Anwer, S., Waris, A., Gilani, S. O., Iqbal, J., Shaikh, N., Pujari, A. N., et al. (2022). Rehabilitation of upper limb motor impairment in stroke: a narrative review on the prevalence, risk factors, and economic statistics of stroke and state of the art therapies. Healthcare (Basel) 10 (2), 190. doi:10.3390/healthcare10020190
Ballester, B. R., i Badia, S. B., and Verschure, P. F. M. J. (2012). Including social interaction in stroke VR-based motor rehabilitation enhances performance: a pilot study. Presence 21 (4), 490–501. doi:10.1162/PRES_a_00129
Barak Ventura, R., Nakayama, S., Raghavan, P., Nov, O., and Porfiri, M. (2019). The role of social interactions in motor performance: feasibility study toward enhanced motivation in telerehabilitation. J. Med. Internet Res. 21 (5), e12708. doi:10.2196/12708
Belletier, C., Normand, A., and Huguet, P. (2019). Social-Facilitation-and-Impairment effects: from motivation to cognition and the social brain. Curr. Dir. Psychol. Sci. 28 (3), 260–265. doi:10.1177/0963721419829699
Bellomo, R. G., Paolucci, T., Saggino, A., Pezzi, L., Bramanti, A., Cimino, V., et al. (2020). The wereha project for an innovative home-based exercise training in chronic stroke patients: a clinical study. J. Cent. Nerv. Syst. Dis. 12, 117957352097986. doi:10.1177/1179573520979866
Blampied, N. M. (2016). Analyzing therapeutic change using modified brinley plots. History, Construction, and Interpretation. Available online at: www.elsevier.com/locate/bt (Accessed May 27, 2025).
Brown, A. J., and Harkins, S. G. (2020). “Chapter 9 - social facilitation and social loafing: opposite sides of the same coin,” in Individual motivation within groups. Editor S. J. Karau (Academic Press), 297–330. Available online at: https://www.sciencedirect.com/science/article/pii/B9780128498675000094 (Accessed May 27, 2025).
Bulu, S. T. (2012). Place presence, social presence, co-presence, and satisfaction in virtual worlds. Comput. Educ. 58 (1), 154–161. doi:10.1016/j.compedu.2011.08.024
Burdea, G., Kim, N., Polistico, K., Kadaru, A., Grampurohit, N., Hundal, J., et al. (2022). Robotic table and serious games for integrative rehabilitation in the early poststroke phase: two case reports. JMIR Rehabil. Assist. Technol. 9 (2), e26990. doi:10.2196/26990
Burdea, G. C., Grampurohit, N., Kim, N., Polistico, K., Kadaru, A., Pollack, S., et al. (2020). Feasibility of integrative games and novel therapeutic game controller for telerehabilitation of individuals chronic post-stroke living in the community. Top. Stroke Rehabil. 27 (5), 321–336. doi:10.1080/10749357.2019.1701178
Charles, D., Holmes, D., Charles, T., and McDonough, S. (2020). Virtual reality design for stroke rehabilitation. Biomed. Vis. 6, 53–87. doi:10.1007/978-3-030-37639-0_4
Crowe, S. E., Yousefi, M., Shahri, B., Piumsomboon, T., and Hoermann, S. (2024). Interactions with virtual therapists during motor rehabilitation in immersive virtual environments: a systematic review. Front. Virtual Real 5. doi:10.3389/frvir.2024.1284696
Dahdah, M. N., Bennett, M., Prajapati, P., Parsons, T. D., Sullivan, E., and Driver, S. (2017). Application of virtual environments in a multi-disciplinary day neurorehabilitation program to improve executive functioning using the Stroop task. NeuroRehabilitation 41 (4), 721–734. doi:10.3233/nre-172183
Demarin, V., and Morović, S. (2014). Neuroplasticity. Period. Biol. 116 (2), 209–211. Available online at: https://hrcak.srce.hr/126369 (Accessed May 27, 2025).
Deutsch, J., and McCoy, S. W. (2017). Virtual reality and serious games in neurorehabilitation of children and adults: prevention, plasticity and participation. Pediatr. Phys. Ther. 29, S23–S36. doi:10.1097/pep.0000000000000387
Dimbwadyo-Terrer, I., Gil-Agudo, A., Segura-Fragoso, A., De Los Reyes-Guzmán, A., Trincado-Alonso, F., Piazza, S., et al. (2016). Effectiveness of the virtual reality system Toyra on upper limb function in people with tetraplegia: a pilot randomized clinical trial. Biomed. Res. Int. 2016, 1–12. doi:10.1155/2016/6397828
Duckworth, J., Mumford, N., Bayliss, J. D., and Wilson, P. H. (2023). “A framework for designing tabletop games in group-based motor rehabilitation,” in Virtual Reality Games for Rehabilitation. Virtual Reality Technologies for Health and Clinical Applications. Editors: E., Brooks, and D. J., Brown. (New York, NY: Springer). doi:10.1007/978-1-0716-3371-7_2
Duncan, P. W., Goldstein, L. B., Horner, R. D., Landsman, P. B., Samsa, G. P., and Matchar, D. B. (1994). Similar motor recovery of upper and lower extremities after stroke. Stroke 25 (6), 1181–1188. doi:10.1161/01.str.25.6.1181
Elor, A., Powell, M., Mahmoodi, E., Teodorescu, M., and Kurniawan, S. (2021). Gaming beyond the novelty effect of immersive virtual reality for physical rehabilitation. IEEE Trans. Games 14 (1), 107–115. doi:10.1109/tg.2021.3069445
Elor, A., Teodorescu, M., and Kurniawan, S. (2018). Project star catcher: a novel immersive virtual reality experience for upper limb rehabilitation. ACM Trans. Accessible Comput. (TACCESS). 11 (4), 1–25. doi:10.1145/3265755
Emmerich, K., and Masuch, M. (2018). “Watch me play: does social facilitation apply to digital games?,” in Conference on human factors in computing systems - proceedings (Association for Computing Machinery).
Flores, E., Tobon, G., Cavallaro, E., Cavallaro, F. I., Perry, J. C., and Keller, T. (2008). “Improving patient motivation in game development for motor deficit rehabilitation,” in Proceedings of the 2008 international conference on advances in computer entertainment technology, 381–384. doi:10.1145/1501750.1501839
Folstein, M. F., Folstein, S. E., and Mchugh, P. R. (1975). “Mini-mental state”. J. Gsychiaf. Res. Pergamon Press 12, 189–198. doi:10.1016/0022-3956(75)90026-6
Fugl-Meyer, A. R., Jääskö, L., Leyman, I., Olsson, S., and Steglind, S. (1975). The post-stroke hemiplegic patient. 1. a method for evaluation of physical performance. Scand. J. Rehabil. Med. 7 (1), 13–31. doi:10.2340/1650197771331
Graham, J. E., Karmarkar, A. M., and Ottenbacher, K. J. (2012). Small sample research designs for evidence-based rehabilitation: issues and methods. Archives Phys. Med. Rehabilitation 93, S111–S116. doi:10.1016/j.apmr.2011.12.017
Gregson, J. M., Leathley, M., Moore, A. P., Sharma, A. K., Smith, T. L., and Watkins, C. L. (1999). Reliability of the tone assessment scale and the modified Ashworth scale as clinical tools for assessing poststroke spasticity. Arch. Phys. Med. Rehabil. 80, 1013–1016. doi:10.1016/s0003-9993(99)90053-9
Guerin, B., and Innes, J. M. (1984). Explanations of social facilitation: a review. Vol. 3, Current Psychology. Springer-Verlag, 32–52.
Hadjipanayi, C., Banakou, D., and Michael-Grigoriou, D. (2024). Virtual reality exergames for enhancing engagement in stroke rehabilitation: a narrative review. Heliyon 10, e37581. doi:10.1016/j.heliyon.2024.e37581
Hari, R., and Kujala, M. V. (2009). Brain basis of human social interaction: from concepts to brain imaging. Physiol. Rev. 89, 453–479. doi:10.1152/physrev.00041.2007
Herpich, F., and Rincon, F. (2020). Management of acute ischemic stroke. Crit. Care Med. 48, 1654–1663. doi:10.1097/ccm.0000000000004597
Høeg, E. R., Andersen, N. B., Malmkjær, N., Vaaben, A. H., and Uth, J. (2023a). Hospitalized older adults’ experiences of virtual reality-based group exercise therapy with cycle ergometers: an early feasibility study. Comput. Hum. Behav. Rep. 11, 100301. doi:10.1016/j.chbr.2023.100301
Høeg, E. R., Bruun-Pedersen, J. R., Cheary, S., Andersen, L. K., Paisa, R., Serafin, S., et al. (2023b). Buddy biking: a user study on social collaboration in a virtual reality exergame for rehabilitation. Virtual Real. doi:10.1007/s10055-021-00544-z
House, G., Burdea, G., Polistico, K., Grampurohit, N., Roll, D., Damiani, F., et al. (2016). A rehabilitation first—tournament between teams of nursing home residents with chronic stroke. Games Health J. 5 (1), 75–83. doi:10.1089/g4h.2015.0072
Houston, J., Harris, P., Mcintttze, S., and Francis, D. (2002). Revising the competitiveness index using factor analysis. Psychol. Rep. 90. 31. doi:10.2466/pr0.90.1.31-34
Ibarra Zannatha, J. M., Tamayo, A. J. M., Sánchez, Á. D. G., Delgado, J. E. L., Cheu, L. E. R., and Arévalo, W. A. S. (2013). Development of a system based on 3D vision, interactive virtual environments, ergonometric signals and a humanoid for stroke rehabilitation. Comput. Methods Programs Biomed. 112 (2), 239–249. doi:10.1016/j.cmpb.2013.04.021
Jung, H. T., Park, T., Mahyar, N., Park, S., Ryu, T., Kim, Y., et al. (2020). Rehabilitation games in real-world clinical settings: practices, challenges, and opportunities. ACM Trans. Computer-Human Interact. (TOCHI). 27 (6), 1–43. doi:10.1145/3418197
Khan, A., Podlasek, A., and Somaa, F. (2023). “Virtual reality in post-stroke neurorehabilitation–a systematic review and meta-analysis. Vol. 30,” in Topics in stroke rehabilitation. United Kingdom: Taylor and Francis Ltd., 53–72.
Kim, D., and Jo, D. (2022). Effects on Co-presence of a virtual human: a comparison of display and interaction types. Electron. Switz. 11 (3), 367. doi:10.3390/electronics11030367
Kyrlitsias, C., and Michael-Grigoriou, D. (2022). Social interaction with agents and avatars in immersive virtual environments: a survey. Front. Virtual Real. 2, 786665. doi:10.3389/frvir.2021.786665
Lau, A., Schwarz, J., and Stoll, O. (2019). Influence of social facilitation on learning development using a Wii BalanceboardTM. Ger. J. Exerc. Sport Res. 49 (1), 97–102. doi:10.1007/s12662-018-0562-8
Lea, R. D., and Gerhardt, J. J. (1995). Range-of-motion measurements. JBJS 77 (5), 784–798. doi:10.2106/00004623-199505000-00017
Levac, D. E. (2024). Individual and contextual factors influencing children’s effort in pediatric rehabilitation interventions. Dev. Med. Child Neurol. 66, 23–31. doi:10.1111/dmcn.15609
Lew, K. L., Sim, K. S., Tan, S. C., and Abas, F. S. (2021). Virtual reality post stroke upper limb assessment using unreal engine 4. Eng. Lett. 29 (4). doi:10.1007/978-3-030-63119-2_22
Lewis, G. N., Woods, C., Rosie, J. A., and Mcpherson, K. M. (2011). Virtual reality games for rehabilitation of people with stroke: perspectives from the users. Disabil. Rehabil. Assist. Technol. 6 (5), 453–463. doi:10.3109/17483107.2011.574310
Li, X., Hatada, Y., and Narumi, T. (2024). “Social simon effect in virtual reality: investigating the impact of Co-actor avatar’s visual representation,” in ACM international conference proceeding series (Australia, Melbourne: Association for Computing Machinery), 157–167.
Liang, H., Liu, S., Wang, Y., Pan, J., Zhang, Y., and Dong, X. (2023). Multi-user upper limb rehabilitation training system integrating social interaction. Comput. Graph. (Pergamon). 111, 103–110. doi:10.1016/j.cag.2023.01.008
Lobo, M. A., Moeyaert, M., Cunha, A. B., and Babik, I. (2017). Single-case design, analysis, and quality assessment for intervention research. J. Neurologic Phys. Ther. 41 (3), 187–197. doi:10.1097/npt.0000000000000187
Marks, A., Oliveira Barbosa, S., Napoli, D., and D’Andrea, S. E. (2025). Anodal tDCS and virtual reality gait rehabilitation in individuals with chronic stroke: a case series report. Front. Stroke 4, 1489031. doi:10.3389/fstro.2025.1489031
Mekbib, D. B., Han, J., Zhang, L., Fang, S., Jiang, H., Zhu, J., et al. (2020). Virtual reality therapy for upper limb rehabilitation in patients with stroke: a meta-analysis of randomized clinical trials. Brain Inj. 34, 456–465. doi:10.1080/02699052.2020.1725126
Meseguer-Henarejos, A. B., Sánchez-Meca, J., López-Pina, J. A., and Carles-Hernández, R. (2018). Inter- and intra-rater reliability of the Modified Ashworth Scale: a systematic review and meta-analysis. Eur. J. Phys. Rehabil. Med. 54 (4), 576–590. doi:10.23736/s1973-9087.17.04796-7
Mnif, M., Chikh, S., and Jarraya, M. (2022). Effect of social context on cognitive and motor behavior: a systematic review. J. Mot. Behav. 54 (5), 631–647. doi:10.1080/00222895.2022.2060928
Mohd, I. N., and Abu Bakar, A. Y. (2014). Developing sampling frame for case study: challenges and conditions. World J. Educ. 4 (3). doi:10.5430/wje.v4n3p29
Movella. Mtw Awinda (2025). Available online at: https://www.movella.com/products/wearables/xsens-mtw-awinda.
Muller, D., and Butera, F. (2007). The focusing effect of self-evaluation threat in coaction and social comparison. J. Pers. Soc. Psychol. 93 (2), 194–211. doi:10.1037/0022-3514.93.2.194
Najm, A., Michael-Grigoriou, D., Kyrlitsias, C., Christofi, M., Hadjipanayi, C., and Sokratous, D. (2020). “A virtual reality adaptive exergame for the enhancement of physical rehabilitation using social facilitation,” in ICAT-EGVE (Florida, Orlando: posters and demos), 1–2.
Neibling, B. A., Jackson, S. M., Hayward, K. S., and Barker, R. N. (2021). Perseverance with technology-facilitated home-based upper limb practice after stroke: a systematic mixed studies review. J. NeuroEngineering Rehabilitation 18, 43. doi:10.1186/s12984-021-00819-1
Nichols, T. (2014). “Social loafing: a review of the literature,”. Article in Journal of Management Policy and Practice. Available online at: https://www.researchgate.net/publication/285636458 (Accessed May 27, 2025).
Novak, D., Nagle, A., Keller, U., and Riener, R. (2014). Increasing motivation in robot-aided arm rehabilitation with competitive and cooperative gameplay. J. Neuroeng Rehabil. 11 (1), 64–15. doi:10.1186/1743-0003-11-64
Oh, C. S., Bailenson, J. N., and Welch, G. F. (2018). A systematic review of social presence: definition, antecedents, and implications. Front. Robot. AI 5, 114. doi:10.3389/frobt.2018.00114
Puderbaugh, M., and Emmady, P. D. (2023). “Neuroplasticity,” in StatPearls (Florida, Treasure Island: StatPearls Publishing).
Rojo, A., Santos-Paz, J. Á., Sánchez-Picot, Á., Raya, R., and Garcia-Carmona, R. (2022). FarmDay: a gamified virtual reality neurorehabilitation application for upper limb based on activities of daily living. Appl. Sci. 12 (14), 7068. doi:10.3390/app12147068
Rong, J., Ding, L., Xiong, L., Zhang, W., Wang, W., Deng, M., et al. (2021). Mirror visual feedback prior to robot-assisted training facilitates rehabilitation after stroke: a randomized controlled study. Front. Neurol. 12, 683703. doi:10.3389/fneur.2021.683703
Schmitt, B. H., Gilovich, T., Goore, N., and Joseph, L. (1986). Mere presence and social facilitation: one more time. J. Experi. Soc. Psychol. 22 (3), 242–248. doi:10.1016/0022-1031(86)90027-2
Sebanz, N., and Knoblich, G. (2009). Prediction in joint action: what, when, and where. Top. Cogn. Sci. 1 (2), 353–367. doi:10.1111/j.1756-8765.2009.01024.x
Shernoff, D., Hamari, J., and Rowe, E. (2014). “Measuring flow in educational games and gamified learning environments,” in EdMedia+ Innovate Learning. Association for the Advancement of Computing in Education (AACE), 2276–2281. doi:10.1037/t46666-000
Slater, M., Sadagic, A., Usoh, M., and Schroeder, R. (2000). Small-group behavior in a virtual and real environment: a comparative study. Presence, 9 (1), 37–51. doi:10.1162/105474600566600
Slijper, A., Svensson, K. E., Engström, H., and Sunnerhagen, K. S. (2014). Computer game-based upper extremity training in the home environment in stroke persons: a single subject design. J. Neuroeng. Rehabil. 11, 35. doi:10.1186/1743-0003-11-35
Solmi, F., Onghena, P., Salmaso, L., and Bulté, I. (2014). A permutation solution to test for treatment effects in alternation design single-case experiments. Commun. Stat. Simul. Comput. 43 (5), 1094–1111. doi:10.1080/03610918.2012.725295
StataCorp LLC (1994). Stata: Statistical Software for Data Science. Available online at: https://www.stata.com/ (Accessed May 27, 2025).
Steed, A., Pan, Y., Watson, Z., and Slater, M. (2018). “We Wait”-The impact of character responsiveness and self embodiment on presence and interest in an immersive news experience. Front. Robot. AI 5, 112. doi:10.3389/frobt.2018.00112
Sterna, R., Szczugieł, J., Pilarczyk, J., Siry, A., and Kuniecki, M. (2024). Like a human: the social facilitation/inhibition effect in presence of a virtual observer depends on arousal. Virtual Real 28 (1), 55. doi:10.1007/s10055-024-00972-7
Stone, K. D., Dijkerman, H. C., Bekrater-Bodmann, R., and Keizer, A. (2019). Mental rotation of feet in individuals with body integrity identity disorder, lower-limb amputees, and normally-limbed controls. PLoS One 14 (8), e0221105. doi:10.1371/journal.pone.0221105
Strauss, B. (2002). Social facilitation in motor tasks: a review of research and theory. Psychol. Sport Exerc. 3. 237–256. doi:10.1016/s1469-0292(01)00019-x
Strojny, P. M., Dużmańska-Misiarczyk, N., Lipp, N., and Strojny, A. (2020). Moderators of social facilitation effect in virtual reality: co-presence and realism of virtual agents. Front. Psychol. 11, 11. doi:10.3389/fpsyg.2020.01252
Syed, U. E., and Kamal, A. (2021). Video game-based and conventional therapies in patients of neurological deficits: an experimental study. Disabil. Rehabil. Assist. Technol. 16 (3), 332–339. doi:10.1080/17483107.2019.1679266
Thielbar, K., Spencer, N., Tsoupikova, D., Ghassemi, M., and Kamper, D. (2020). Utilizing multi-user virtual reality to bring clinical therapy into stroke survivors’ homes. J. Hand Ther. 33 (2), 246–253. doi:10.1016/j.jht.2020.01.006
Triandafilou, K. M., Tsoupikova, D., Barry, A. J., Thielbar, K. N., Stoykov, N., and Kamper, D. G. (2018). Development of a 3D, networked multi-user virtual reality environment for home therapy after stroke. J. Neuroeng Rehabil. 15, 88–13. doi:10.1186/s12984-018-0429-0
World Health Organization (2016). World health statistics 2016 [OP]: monitoring health for the sustainable development goals (SDGs). Geneva, Switzerland: World Health Organization.
Warraich, Z., and Kleim, J. A. (2010). Neural plasticity: the biological substrate for neurorehabilitation. PM R. 2 (12 Suppl.), S208–S219. doi:10.1016/j.pmrj.2010.10.016
Keywords: virtual reality, rehabilitation, stroke, social facilitation, co-presence, virtual agents
Citation: Hadjipanayi C, Sokratous D, Kyrlitsias C, Banakou D and Michael-Grigoriou D (2025) Social facilitation within immersive virtual reality enhances perseverance in stroke rehabilitation training. Front. Virtual Real. 6:1581240. doi: 10.3389/frvir.2025.1581240
Received: 25 February 2025; Accepted: 13 May 2025;
Published: 13 June 2025.
Edited by:
Albert Rizzo, University of Southern California, United StatesReviewed by:
Christine Seaver, University of Central Florida, United StatesSamson Peter Mvandal, Muhimbili National Hospital, Tanzania
Copyright © 2025 Hadjipanayi, Sokratous, Kyrlitsias, Banakou and Michael-Grigoriou. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Despina Michael-Grigoriou, ZGVzcGluYS5ncmlnb3Jpb3VAY3V0LmFjLmN5
†ORCID: Christos Hadjipanayi, orcid.org/0000-0001-7444-5406; Dimitris Sokratous, orcid.org/0000-0002-7595-4349; Christos Kyrlitsias, orcid.org/0000-0003-0810-1685; Domna Banakou, orcid.org/0000-0002-0974-6971; Despina Michael-Grigoriou, orcid.org/0000-0003-0824-7684
 Christos Hadjipanayi
Christos Hadjipanayi Dimitris Sokratous
Dimitris Sokratous Christos Kyrlitsias
Christos Kyrlitsias Domna Banakou
Domna Banakou Despina Michael-Grigoriou
Despina Michael-Grigoriou