- 1Institute of Biomedical Ethics and History of Medicine, University of Zürich, Zürich, Switzerland
- 2Department of Psychiatry and Behavioral Sciences, Stanford University School of Medicine, Stanford, CA, United States
Background: Metaverse-based mental health services may be poised to increase access and augment treatment; doing so ethically requires anticipating risks and actively shaping how this emerging setting might support care. With limited means to directly evaluate the Metaverse’s potential role in the provision of appropriate mental health care, there is value in conceptual expert input.
Methods: The aim of the present Delphi study was to gather global academic experts to explore where opinions converged and diverged regarding three foundational topics: 1) A working definition of the Metaverse; 2) A conception of appropriate care in the Metaverse that identifies key potential challenges; and 3) Conditions that may help align mental health offerings in the Metaverse with tenets of appropriate care. The study was carried out in an e-Delphi format–asynchronously online–in three rounds with statements divided according to the study aims. Panelists rated agreement with statements, suggested modifications, provided commentary on their position, suggested additional statements, and reviewed panelist-generated statements.
Results: The 14 panelists, identified through literature review, represented top universities and pioneering research labs in the field. Of the 27 original statements, all reached consensus by Round Three. 27 new statements were generated based on panel suggestion, of which 20 reached consensus. Panelists produced a working definition of the Metaverse, exhibited clarity regarding the possible suitability of the Metaverse as a setting for appropriate mental healthcare, identified challenges to providing such care, and identified interventions that may meaningfully address Metaverse-specific care concerns.
Conclusion: Additional research building on the identified issues and solutions is needed to responsibly shape the form and content of both future mental health offerings and the Metaverse itself. Next steps should involve service users to voice their perspective; clinicians to shape best clinical practice; industry to consider standards; and policymakers to build upon the suggested regulatory measures.
Introduction
Context
Mental health services within the Metaverse are expected to flourish, but relatively little has been published in academic journals to support an understanding of the Metaverse’s potential role in the provision of appropriate mental health care. With mental disorders a leading cause of illness and disability worldwide, and treatment failing to reach or benefit many of those suffering, virtual services may play an important role in delivering effective treatment (Us et al., 2022). There is early evidence to suggest that Metaverse-based technologies may increase access, including for those who are homebound, remote, disabled, isolated, or fearing stigma (Us et al., 2022; Ali et al., 2023; Lush et al., 2020). Metaverse-based innovations may also enhance current treatment modalities, potentially advancing interventions generally and improving care for certain conditions in particular, such as attention deficit disorder, body dysmorphia, specific phobias, post-traumatic stress disorder, and chronic pain (Us et al., 2022; Glanz et al., 2003; Ioannou et al., 2020).
The Metaverse has unique potential to shape mental health services. Intimate knowledge of the user that tracks vital parameters such as heart rate, respiratory rate, or blood pressure along with gaze, facial expressions, and voice pitch could be used to predict emotional states, which, combined with artificial intelligence, holograms, immersive worlds, and/or avatars, could be directed towards therapeutic aims (Gloeckler and Biller-Andorno, 2023).
Critical concerns have been raised, though, regarding the provision of care in this setting, particularly over privacy and data use; coercion and mental integrity; transparency and informed consent; and the risk of bias (Gloeckler and Biller-Andorno, 2023).
In its nascent state, the “Metaverse” is not precisely defined; what it will become remains open. In this phase of envisioning, it is worth considering what care in the Metaverse might consist of and how it may or may not meet the tenets of appropriate care. Appropriate care is understood as care that is evidence-based, draws on clinical expertise, is patient-centered, uses resource wisely, and is equitable (Robertson-Preidler et al., 2017). Providing appropriate care is an aim of well-functioning health systems. There is not strong evidence available to directly evaluate the Metaverse’s role in offering appropriate services nor to reliably indicate the position of experts on the topic. For example, a broad Pubmed search of “Metaverse” AND “Mental health” from January 2024 yielded only 48 results with varying relevance. The concerns raised about care in this setting should be examined in a systematic way to help inform the establishment of sound practices and ethical services, shaping not only mental health offerings in the Metaverse but also the Metaverse itself.
Delphi technique
Delphi studies tend to be employed in health fields when “available knowledge is incomplete or subject to uncertainty and other methods that provide higher levels of evidence cannot be used. The aim is to collect expert-based judgments and often to use them to identify consensus” (Niederberger and Spranger, 2020). In this case, a Delphi method was selected given the relatively little academic literature available on the topic of mental healthcare in the Metaverse. With limited means to identify and evaluate challenges and solutions in practice, there is value in having experts provide conceptual insight into the question of appropriate care in this setting. The study was reviewed in accordance with the ethical review process of the University of Zürich and approved under the checklist for ethical evaluation of empirical studies that do not need mandatory authorization (CEBES): No. 2027-7_CEBES. The present study falls outside the scope of the Swiss Human Research Act.
Study aim
The primary aim of the present study was to gather a panel of global, academic experts well-suited to reflect on the potential of the Metaverse as a setting for the provision of appropriate care in order to explore where opinions converged and diverged regarding three foundational topics: 1) A working definition of the Metaverse; 2) A conception of appropriate care in the Metaverse that identifies key potential challenges to delivering such care; and 3) Conditions that may help align health offerings in the Metaverse with tenets of appropriate care. At present, the Metaverse remains largely an idea; the reflections invite projections about the future as the Metaverse comes into existence. Item one, a working definition of the Metaverse, was necessary to ground discussion of items two and three. Ultimately, the goal of this present study was to provide foundational material for further inquiry, with experts identifying concerns and interventions deserving of further, formal attention. The intention was to spur academic and policy efforts to determine how the Metaverse may best support the provision of high-quality and accessible mental health care.
Methods
Panelists
Potential panelists were identified via a review of the literature: those who had written at least one academic article in English on the topic of the Metaverse and mental health were screened for possible inclusion. Those who were then invited to participate held academic positions in relevant fields, such as psychology or communication sciences, or otherwise demonstrated relevant expertise through their position in industry or clinical practice. Those who were excluded tended to have made minor contributions to the identified article, not yet earned graduate degrees, and/or were in fields less closely related to the topic without additional publications or affiliations to indicate topic-relevant knowledge of both the Metaverse and mental health. In the letter of invitation, experts were asked to suggest additional colleagues with relevant expertise; other potential panelists were identified through such snowball sampling. These additional suggested participants did not necessarily have one academic publication on the topic of the Metaverse and mental health but were screened using the other criteria. All panelists who met inclusion criteria were sent an invitation email describing the purpose of the study and its methodology. The research team had a priori determined a preferred target panelists size of 10–40 experts (Nasa et al., 2021); given the relatively small pool of candidates, the research team did not predetermine a plan for further screening in the event that more than 40 expressed interest. Panelists who joined the study did not know each other’s identities until the end of the last round, and all responses were kept fully anonymous. Panelists were not compensated for their time nor otherwise incentivized to participate in the study.
Instrument
The survey instrument was developed following a scoping review of the relevant literature, which focused on existing, available definitions of the Metaverse; applications of the Metaverse in the delivery of mental health services; ethical and practical concerns related to using the Metaverse for such services; and suggestions to mitigate harm. The scoping review findings were then translated into statements; key articles from the scoping review that informed the statements can be found in the article [redacted for anonymity]. To meet the study aims, the survey was divided across three sections: Definition of the Metaverse, The role of the Metaverse in the provision of appropriate mental healthcare, and Conditions for appropriate mental healthcare in the Metaverse. The research team set a target number of statements between 20 and 30 to limit participant fatigue. Early versions of the instrument with more than 30 statements were piloted with three reviewers: one with expertise in Delphi studies, one with an academic background similar to the panelists’, and one with relevant experience in industry. Reviewers were asked to evaluate whether each statement consisted of one point, the wording was clear, and the content highly salient. Reviewers shared their evaluation of statements and suggested improvements. Based on pilot feedback, the lead instrument-writer refined the statement, sometimes soliciting additional feedback from reviewers to do so. Twenty-seven statements were thus established for Round 1.
Delphi procedure
In addition to a preliminary description of the study’s overall protocol sent during recruitment, detailed instructions regarding the structure of each round were shared with panelists at the beginning of that round. Panelists participated independently by completing an online questionnaire. Questionnaires were distributed and responses anonymized and stored using the software Tivian. Electronic informed consent was obtained from each panelist at the start of each round. Panelists gave explicit consent for their names and affiliations to be shared in a publication of study findings. Panelists were given 1.5 weeks to complete each round, and the time between rounds was approximately 3 weeks; panelists received, by email, all anonymized results from the previous round 1 week before the next was circulated. Three days before a round was set to close, panelists who had not yet submitted responses were sent a reminder email. At the end of the three rounds, panelists received an email with the name and institutional affiliation of all panel members. No in-person meetings were held. See Figure 1, depicting the process of Delphi rounds from start to finish.
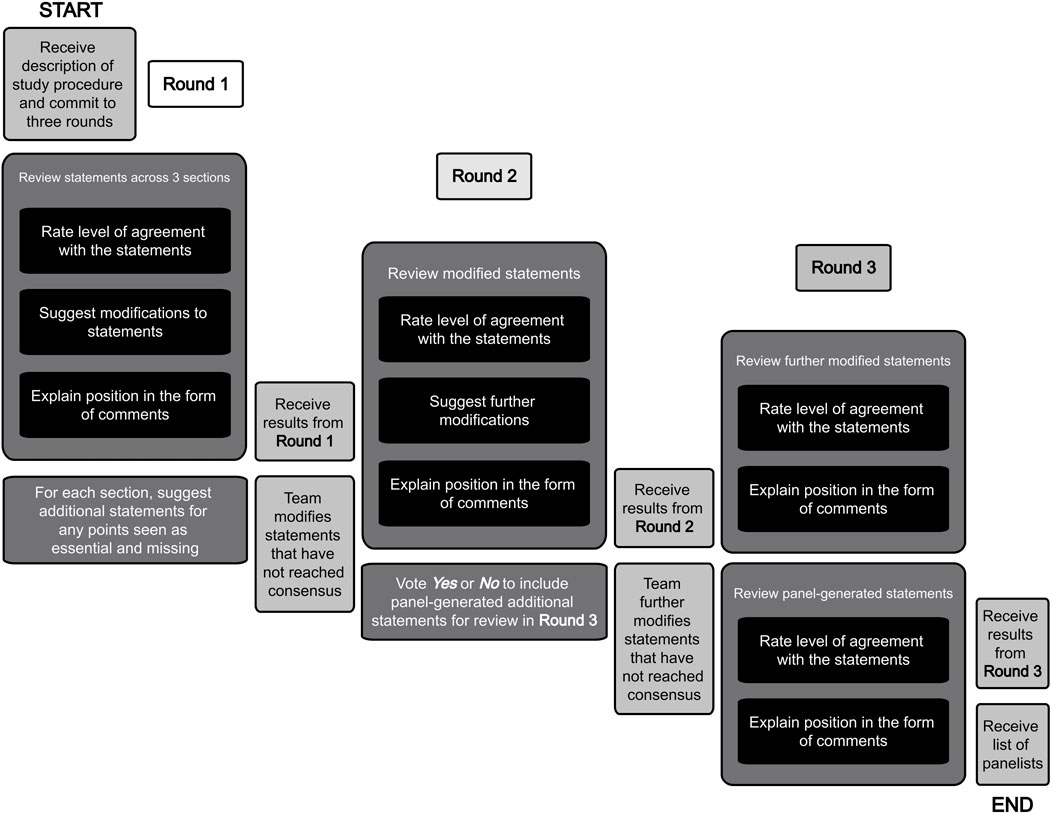
Figure 1. Study design. Legend body: This figure outlines and describes the study design and process of panelists’ review.
An a priori decision was made to carry out the study in three rounds to allow panelists the ability to suggest additional statements that could then be considered by the other panelists. At the end of Round 1, participants were invited to provide additional statements that they felt were essential and missing. Additional statements that were suggested by panelists in Round 1 were voted on for inclusion in Round 2: any statement generated in Round 1 that simple majority agreed in Round 2 should be included was then presented in Round 3 for experts to consider. Respondents reviewed all included statements according to a four-point Likert-rating scale (Strongly Disagree, Disagree, Agree, Strongly Agree) with a fifth point available for those who neither agreed nor disagreed (Other - comment on next page). This scale was selected to avoid the ambiguity of a Likert midpoint that might force respondents to indicate either neutrality or uncertainty.
In each round, respondents were asked to reflect on each statement and provide comments to support or explain their rated response. After the first two rounds, they were also invited to suggest any modifications that they felt would improve the accuracy or validity of a given statement. Statements that did not reach consensus were modified according to the position of the majority as indicated in the open-ended responses and included in subsequent rounds for further review. Any statement, whether original, modified, or newly suggested, that reached widespread agreement, with 75% or more of the panel agreeing or strongly agreeing, was deemed to have reached consensus and excluded from further review. Any statement that reached widespread disagreement, with 75% or more of the panel disagreeing or strongly disagreeing, would similarly have been removed.
Likert rating scales were analyzed according to frequency distribution. Open-ended responses were coded for main themes. One member of the research team was primarily responsible for translating open-ended responses into statement modifications and two other researchers, one with expertise in Delphi design and one with expertise on the topic, reviewed these modifications for consistency with panelist views. The modified statements were then refined. Each programmed round was piloted by a researcher naïve to its design for clarity and accuracy. At the end of Round 1, 2, and 3, panelists were invited to provide feedback to the research team that would not be shared with the other panelists.
Results
Panelists
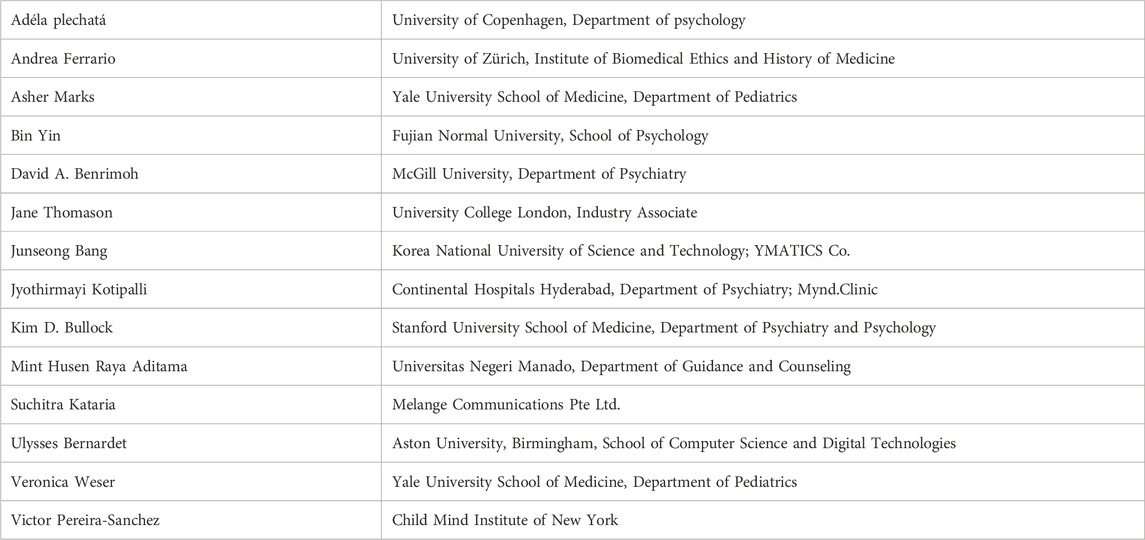
Panelists were recruited from July-September 2023. 66 were invited in total, 41% of whom (n = 27) were women. 16 committed to join the study, and 14 ultimately participated in the first round. Of those 14, all participated fully in all three rounds; there was a 100% completion rate. The first round was circulated September 2023 and the final round concluded December 2023. See Table 1 for the list of participants and their primary affiliations. Experts participated in their professional capacities and not representing the institutions with which they are affiliated. The expert panel consisted of three women, one person who identified as non-binary, one person who preferred not to disclose, and nine men. Panelists were from Australia, Canada, China, Czech Republic, India, Indonesia, Italy, Republic of Korea, Spain, Switzerland, and the United States. Nine of the panelists were clinicians in mental health and at least 5 were closely associated with relevant research labs, including Stanford’s Neurobehavioral Clinic and Virtual Reality and Immersive Technologies laboratory (leading the lab); Electronics and Telecommunications Research Institute of Korea; The McGill Lab for Computational Psychiatry and Translation (leading the lab); Yale’s play4REAL XR Lab; and The Cybernetic Human Lab at Aston University (leading the lab).
Responses
Overview
Of the 27 original statements, all reached consensus by Round 3, with five undergoing modifications. 27 new statements were generated based on suggestions from the panelists, 24 of those were voted on for inclusion in Round 3, and 20 ultimately reached consensus. In total, 47 statements reached consensus.
Section I: definition of the metaverse
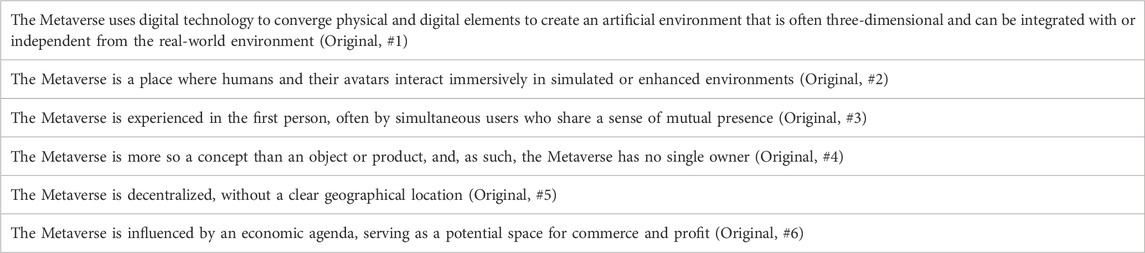
Six statements defining the Metaverse reached consensus; see Table 2.
Statements #2, #3, #4, and #5 reached consensus in the first round. Comments regarding these statements offered additional refinement: respondents defined avatars as a digital representation of the user (n = 3); flagged that experiences in the Metaverse are not always first-person (n = 2); and noted that certain platforms or services that comprise the Metaverse are owned (n = 4). For the two statements that did not initially reach consensus, respondents highlighted that the Metaverse is not necessarily three-dimensional (n = 2) and that the term physiological is ambiguous (n = 3). Respondents pushed back on the idea of economic factors being strongly defining of the Metaverse; they emphasized that economy was one shaping force amongst many (n = 5). The two remaining statements reached consensus in Round 2 once modified. Four additional statements were suggested by the panelists, of which one was voted for inclusion in Round 3 but did not ultimately reach consensus. See Figure 2 to review the evolution of statements in Section I across the three rounds and for the rates of agreement with each statement.
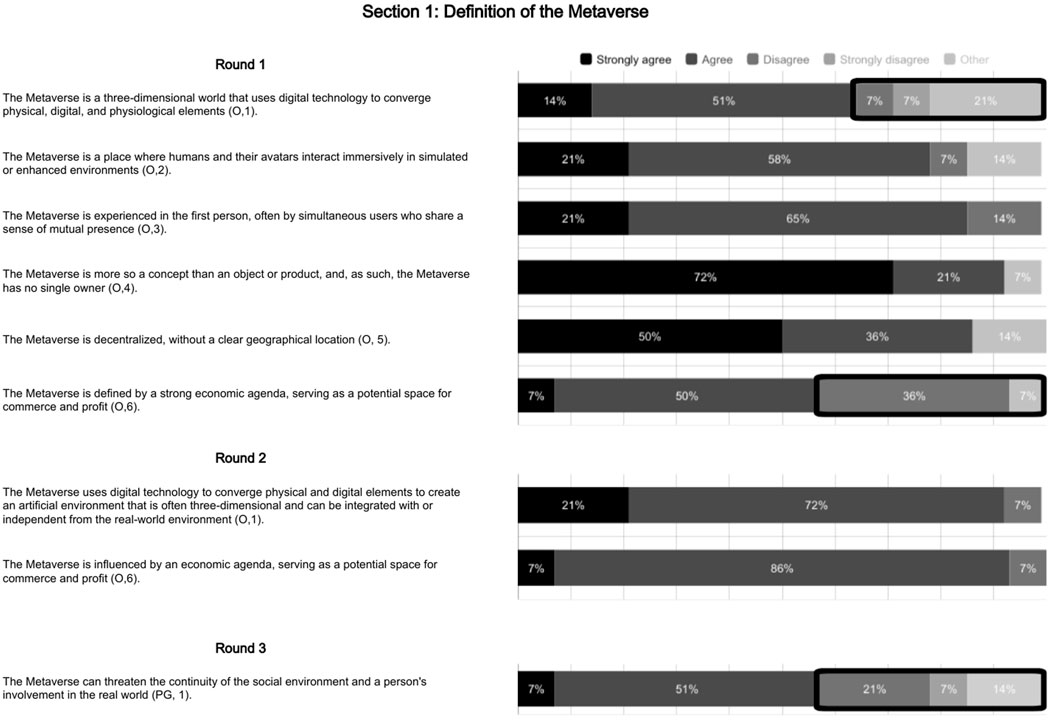
Figure 2. Definitions of the metaverse. Legend body: This figure visualizes panelists’ levels of consensus on statements on definitions of the Metaverse across each of the three rounds. Instances of stronger agreement are visualized in black; agreement in dark grey; disagreement in medium grey; strong disagreement in light grey; and “other” in the lightest grey. Lack of consensus is framed by a bold, round-cornered black rectangle.
Section II: the role of the metaverse in the provision of appropriate mental healthcare
Twenty-five statements regarding appropriate care in the Metaverse reached consensus. See Table 3.
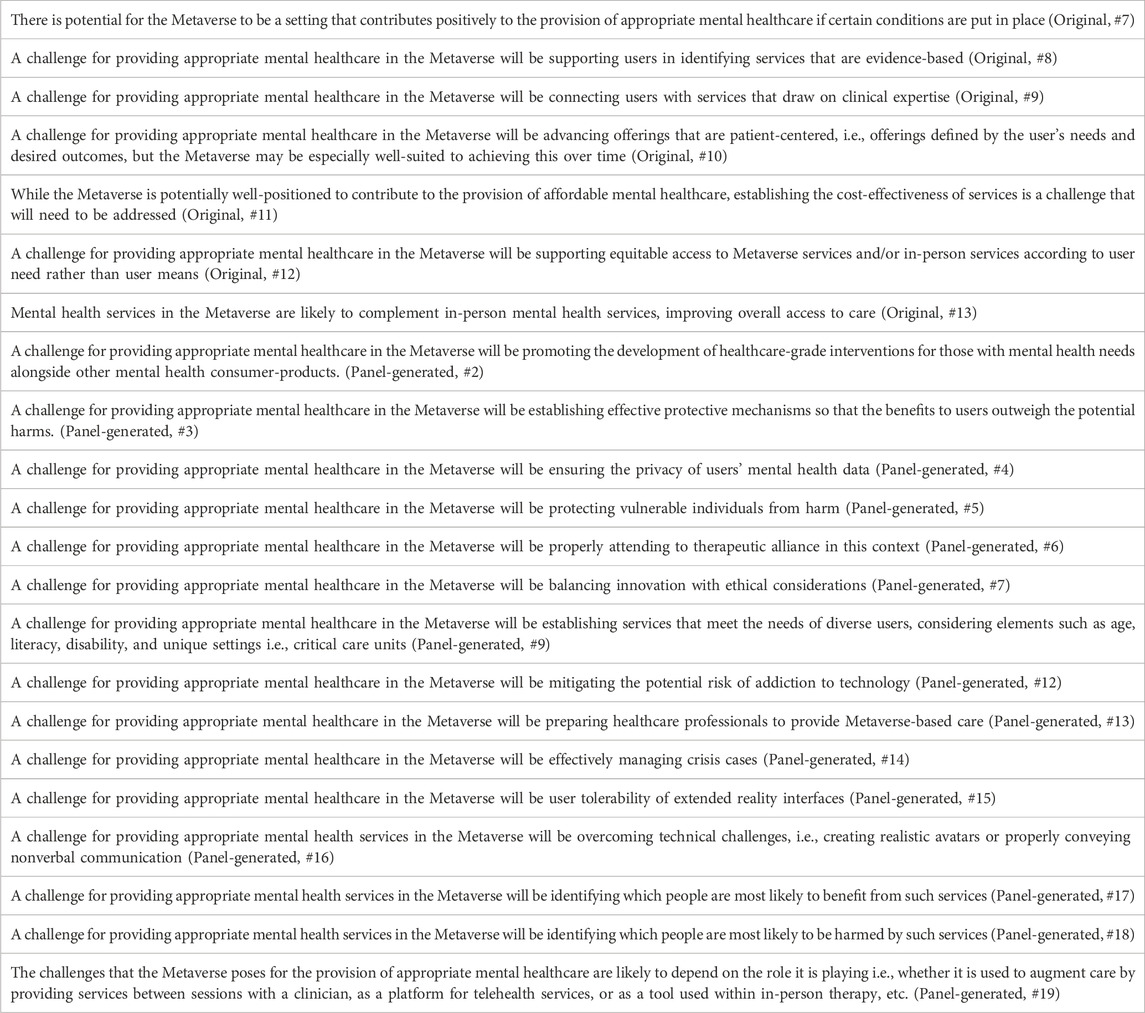
Table 3. Final statements on the role of the metaverse in the provision of appropriate mental health care.
Respondents expressed general optimism about the role of the Metaverse in the provision of appropriate mental health services, with 100% agreeing or strongly agreeing in Round 1 that “There is potential for the Metaverse to be a setting that contributes positively to the provision of appropriate mental health care if certain conditions are put in place.” Respondents emphasized the value of empirical and experimental work done prior to implementation to potentially mitigate areas where they did identify challenges (n = 5). Some comments emphasized that the originally framed challenges, which were associated with the five main tenets of appropriate care, were applicable to health care generally as opposed to issues unique to the Metaverse (n = 5). Panelists suggested 18 additional potential challenges for appropriate care, many of which were identified as Metaverse-specific challenges, such as, “A challenge for providing appropriate mental health care in the Metaverse will be mitigating the potential risk of addiction to technology.” 15 of those suggested statements reached consensus. Three comments rated challenges relative to one another or to healthcare in general. For example, “I don't believe this will be as challenging as the other challenges listed” or “This is a challenge that is true of all mental health care services and not unique to the Metaverse. It may be slightly less challenging within the Metaverse.”
For the statements that did not initially reach consensus, open-ended responses suggested that respondents tended to see opportunity, i.e., that the Metaverse might eventually be well-suited to providing personalized services (n = 4) and potentially able to overcome cost barriers to provide cost-effective services (n = 3). Respondents had the strongest opposition to the idea that the Metaverse may pose the risk of competitively replacing valuable in-person services, with 64% disagreeing or strongly disagreeing. Respondents emphasized that Metaverse services were likely to be complementary to presently available services (n = 5), citing the role the Metaverse may play in increasing access (n = 4) and emphasizing the high, unmet present need for mental health services (n = 4). See Figure 3 to review the evolution of statements in Section II across the three rounds and for the rates of agreement with each statement.
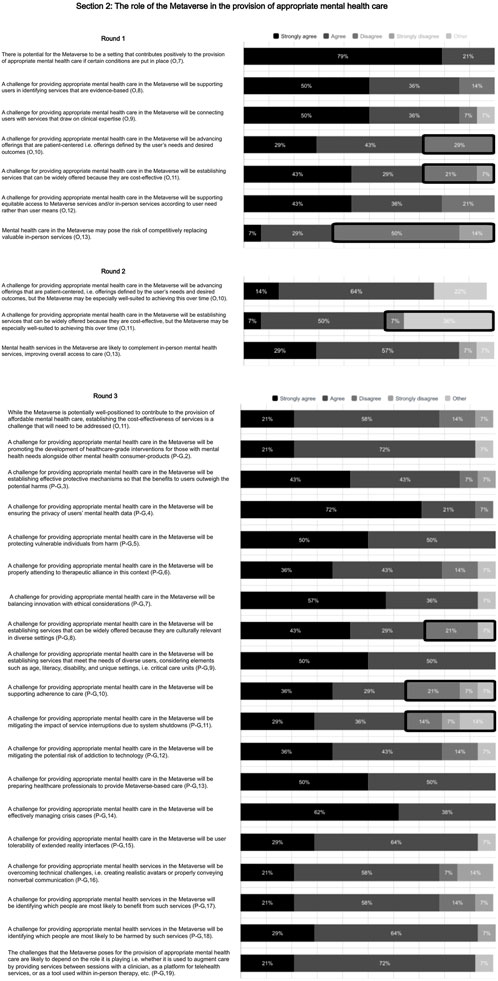
Figure 3. The Metaverse’s role in appropriate care. Legend body: This figure visualizes panelists’ levels of consensus on statements on the role of the Metaverse in the provision of appropriate mental healthcare across each of the three rounds. Instances of stronger agreement are visualized in black; agreement in dark grey; disagreement in medium grey; strong disagreement in light grey; and “other” in the lightest grey. Lack of consensus is framed by a bold, round-cornered black rectangle.
Section III: conditions for appropriate mental healthcare in the metaverse
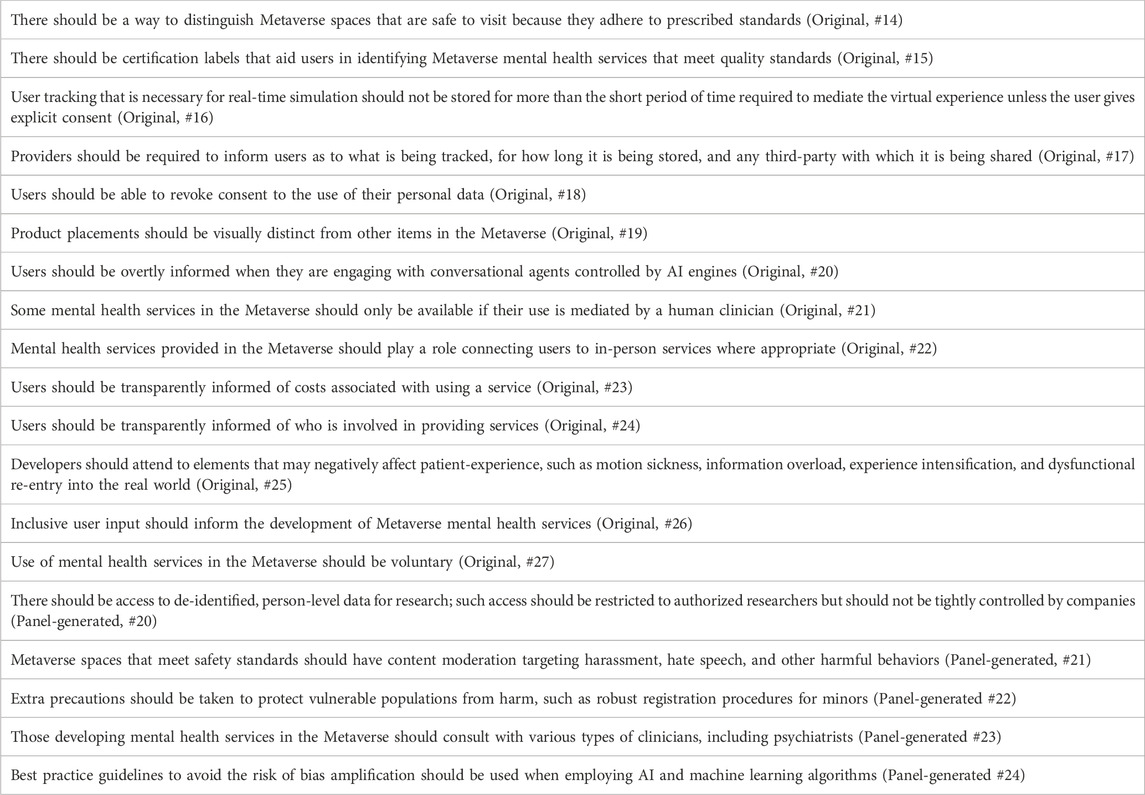
All original statements presenting conditions that might support appropriate care reached consensus in the first round with high rates of agreement. Five additional conditions were suggested by panelists, voted on for inclusion, and reached consensus in Round 3. See Table 4.
Open-ended responses in this section often related to feasibility (n = 9). For example, two noted that it is sometimes necessary to store data for long periods of time, i.e., for the use of deep learning models; two noted that cost transparency depends on the type of healthcare system in which the service is situated; and one remarked that some therapeutic techniques require the obscured identity of AI-controlled agents as such. Relatedly, respondents expressed concerns: three were worried about the harmful effects of content moderation and two raised concerns about governing bodies themselves being corrupt or profit driven. One highlighted that guidelines are insufficient to mitigate risks associated with bias. Some respondents offered suggestions for refinement (n = 3). For example, one panelist suggested that, in addition to being transparently informed of who is providing a service, users should also be informed of the functions, limitations, and risks of that service. See Figure 4 to review the evolution of statements in Section III across the three rounds and for the rates of agreement with each statement.
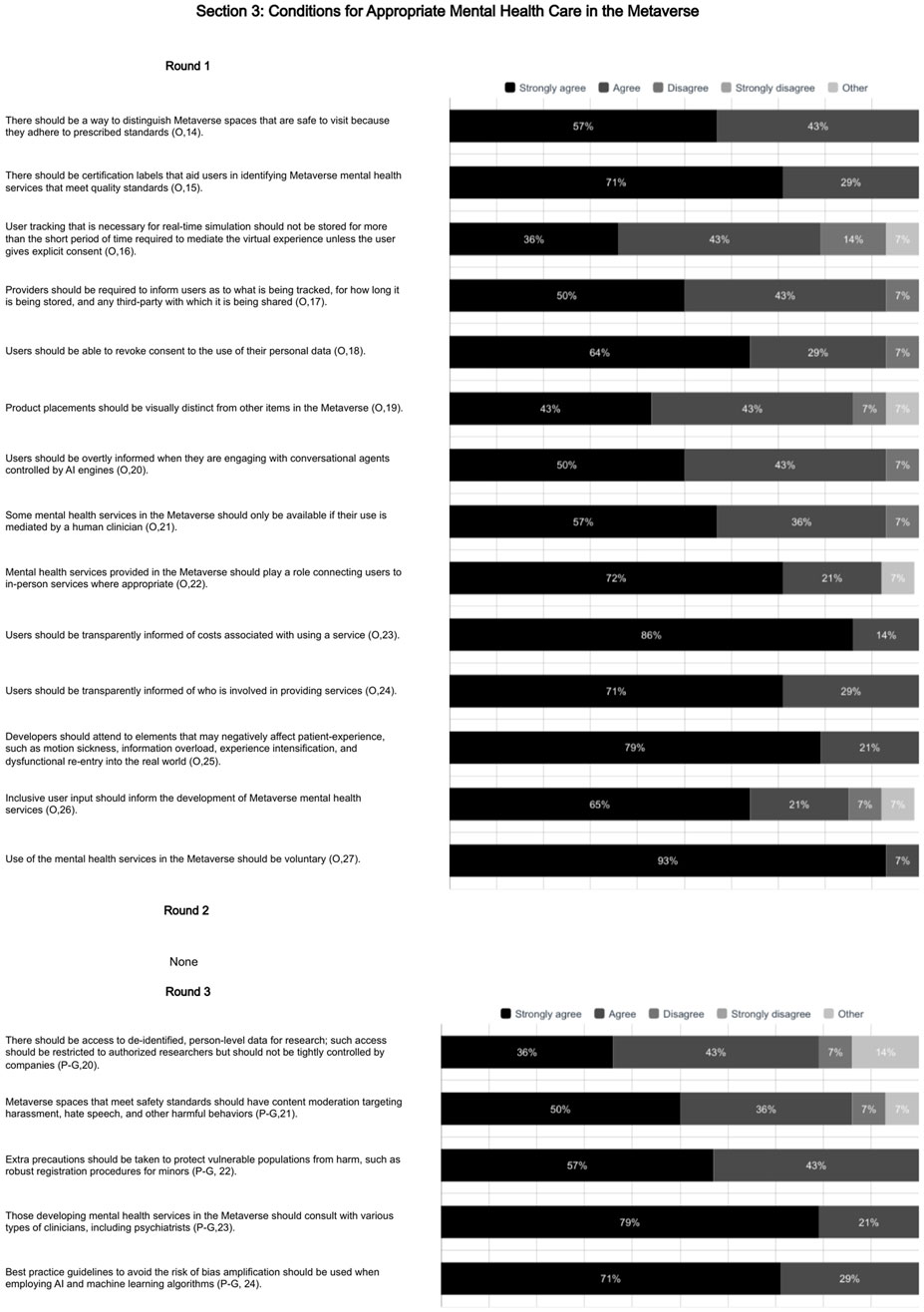
Figure 4. Appropriate care in the Metaverse. Legend body: This figure visualizes panelists’ levels of consensus on statements on conditions for appropriate mental healthcare in the Metaverse across each of the three rounds. Instances of stronger agreement are visualized in black; agreement in dark grey; disagreement in medium grey; strong disagreement in light grey; and “other” in the lightest grey. Lack of consensus is framed by a bold, round-cornered black rectangle.
Statements as a whole
The feedback to researchers tended to be positive, with eight comments across the three rounds offering general support for the value of the study. Three respondents noted that, when taken as a whole, there were redundancies in the final set of statements. Two mentioned the concern that statements were sometimes too general to be useful. Ten of the statements that reached consensus still had one or more comment flagging ambiguity. Three wanted clarification around the term “healthcare-grade interventions” (Panel-generated, #2) and two were unsure about the meaning of “visually distinct” advertisements (Original, #19). Each of the following statements had one comment questioning meaning: “integrated with the real-world” (Original, #1); “short period of time” (Original, #16); “inclusive user input” (Original, #26); voluntary use of Metaverse services (Original, #27); “therapeutic alliance” (Panel-generated, #6); “user-tolerability” (Panel-generated, #15); whether non-verbal communication referred to the therapist or client (Panel-generated, #16); and research access to deidentified, person-level data (Panel-generated, #20).
Discussion
Study aims
The study offered insights across the three main study aims.
1. The results indicate that the definition of the Metaverse as understood by experts is still emerging. When it came to describing the Metaverse, suggestions for refinement–even for statements with which participants agreed–and the lack of consensus around panel-generated statements suggested that panelists held distinct conceptions of the Metaverse. There was, though, ground for a common conversation. The debate generated in this section underscores the importance of establishing a common understanding of how the term “the Metaverse” is being used by discussants in order to anchor meaningful exchange. The agreed upon definitions primarily hold value for helping to align future discussion of the Metaverse around a shared conception.
2. The panelists had general optimism regarding the potential role the Metaverse could play in the provision of care, while acknowledging challenges that will need to be addressed. The panel indicated a strong sense of clarity on the possible suitability of the Metaverse as a setting for appropriate care and as a complement to existing services. Through their suggestions, panelists illustrated the need to reflect on Metaverse-specific challenges, highlighting that the setting introduces unique concerns. Their suggested statements regarding appropriate care in the Metaverse emphasize the need to think beyond familiar lines in an envisioning process that anticipates how this setting might transform practices.
3. Panelists recognized many possible interventions that could support the provision of appropriate care. Their consensus indicated potential interventions that might meaningfully address Metaverse-specific concerns and contribute to the possibility of providing appropriate care in this setting. Comments on these conditions, though, suggest the need for further reflection if the options are to be explored in practice. Panelists noted that the potential interventions themselves raise ethical concerns and questions of feasibility, for example, around the implication of content moderation or practicality of data-use transparency.
These findings tend to align with what is known regarding the Metaverse’s role in the provision of appropriate mental healthcare. For example, expert consensus supported existing literature that presents accessibility, equity, and cost of specialized technologies as notable potential challenges (Us et al., 2022; Gloeckler and Biller-Andorno, 2023; Benrimoh et al., 2022; Ford et al., 2023; Chen and Zhang, 2022). The panel’s view on conditions that might support appropriate care delivered in the Metaverse also tend to align with best practices and recommendations that appear in the literature regarding data privacy, transparency, user autonomy, and economic drivers (Us et al., 2022; Ali et al., 2023; Ioannou et al., 2020; Benrimoh et al., 2022; Ford et al., 2023; Chen and Zhang, 2022; Cerasa et al., 2022; Navas-Medrano et al., 2023). Given that both the body of panelists and the set of statements were identified through relevant, existing literature, this concordance is expected. The study findings, though, translated the literature into statements that are discrete, explicit, and concrete. Doing so generates a link between what is present in the literature and action steps for implementation.
Though, as expected with newly emerging concepts, ambiguities remain, and these are reflected in the panelists’ final statements. Some of the ambiguities ca be addressed by more straightforward efforts to refine definitions and add specificity. For example, panelists noted the lack of clarity around terms like: “healthcare-grade interventions” (Panel-generated, #2) and “visually distinct” advertisements (Original, #19). In these cases, “healthcare-grade interventions” could be better defined as those interventions that have undergone a standard review process and been approved by regulatory bodies that oversee the practice of medicine. “Visually distinct” could refer to a visual code that sets apart anything sponsored or promoted such that it can be readily recognized as an advertisement.
Other statements, though, require more than just refined specificity; they instead call for further consideration and development. For example, the concept of content moderation requires thoughtful exploration. Participants agreed that “Metaverse spaces that meet safety standards should have content moderation targeting harassment, hate speech, and other harmful behaviors” (Panel-generated, #21). What this might look like in practice and how to execute it is unclear. Pons et al. speaks to the potential benefits of a ‘mental health Metaverse,’ which would be defined by accessible and moderated group therapeutic modalities. Potential content moderation in a group therapeutic context might be clinically-informed censorship of speech or actions that could reduce therapeutic benefit; such platforms would be defined as settings for clinical benefit rather than settings for free expression. Developing this concept well and moving towards implementation requires significant further research with an eye to weighing risks and benefits.
Future research
Five important areas emerge for future work.
1. Gather input from mental health clinicians on how the Metaverse can best enhance mental health services: Panelists highlighted the importance of clinician involvement in developing Metaverse mental health offerings. Using the framing of the Metaverse generated by this present study as context, engage those able to speak to excellence in care in their respective fields. Draw on clinician guidance to inform appropriate Metaverse-based mental health offerings based on the needs, as recognized by clinicians, of various patient populations.
2. Directly involve patients to inform an understanding of how Metaverse-based mental health services might best meet the needs of future service users: Panelists highlighted the importance of involving service users in the development and design of Metaverse mental health offerings. Patient reactions to the challenges and conditions identified by the study should be elicited and taken into account; their expectations, concerns, and hopes regarding offerings in the Metaverse should be formally explored. Doing so is a key step in making sure that these findings are evaluated and further developed by those likely to be directly affected.
3. Encourage policymakers to reflect on the role of the Metaverse in healthcare at a systems level: Panelists raised questions about the implementation of interventions suggested. Navigating emerging digital technology is an important and complex task for policymaking; building the required expertise and the ability to respond in a timely fashion to a quickly moving field is an urgent task. Drawing on the issues and strategies identified in this present study, engage policy experts in efforts to understand what kinds of interventions are implementable and may have value when it comes to protecting the quality and equity of health services in the Metaverse.
4. Engage those in industry as they set technical standards: Given the key role industry leaders are likely to play in developing the devices and platforms that compose the Metaverse, efforts should be made to foster collaboration. Large companies have significant power as they set technical standards amongst themselves, and this is an important stage for researchers and clinicians to become involved. Next steps should seek opportunities for exchange amongst industry leaders, researchers, clinicians, and service users in the interest of high-quality, appropriate care that adheres to relevant ethical and legal standards.
5. Alter the structure of subsequent Delphi studies to increase utility and meaningfulness of results: In the current design, panelists did not have the ability to refine or prioritize the final set of statements. Opening the final set of statements to refinement, ranking, or prioritization could add value and clarity without heavy structural or methodological changes.
Limitations
A key limitation of the present study was its focused scope; the aim was to capture the view of academic experts in the field. From within that pool, the study only screened articles in English to identify potential experts. The study largely excluded those without an academic presence and did not explicitly look for panelists representing diverse field, such as clinicians and developers or those in industry and policy. The study did, ultimately, include the perspectives of both clinicians and those in industry, but not with the aim of doing so representatively. Including the perspective of potential service users, while key for the development of appropriate mental health offerings in the Metaverse, was also beyond the scope of the study. Finally, because the panel was predominantly male and more heavily weighted towards North America and Europe, there may have been limited perspectives represented despite concerted efforts to recruit a heterogenous panel.
When considering the significance of the final set of statements from this study, it is worth noting the constraints of the methodology. Panelist comments generated a set of statements as long as the original set of statements, and the predetermined methodology did not leave room to modify the panel-generated statements. There was also no opportunity to rank the value of challenges or interventions relative to one another nor refine the set as a whole to avoid redundancy. Comments from panelists suggested that these may have been valuable additional steps to improve the utility of the final set of statements.
Conclusion
The study offers a framing of the Metaverse that can align discussion around a common conception while identifying concerns, opportunities, and interventions deserving of further exploration. This is a critical moment to significantly influence the form of health offerings in the Metaverse and increase the likelihood that Metaverse-based services support efforts to provide appropriate care. The challenges here identified may be valuable for developers, policymakers, and clinicians to recognize where attention is needed to mitigate potential harms. The set of protective conditions here identified contribute to early efforts to determine possible strategies that might increase the safety, equity, efficacy, and efficiency of services. Much regarding healthcare in the Metaverse remains to be envisioned; there is an opportunity to shape the form and content of not only the mental health offerings being developed but also the Metaverse itself. To ensure that the findings from this present study offer a valuable contribution, the insights generated should give rise to further, timely investigation.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by The University of Zürich according to the checklist for ethical evaluation of empirical studies that do not need mandatory authorization (CEBES): No. 2027-7_CEBES. The present study falls outside the scope of the Swiss Human Research Act. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
SG: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Visualization, Writing – original draft, Writing – review and editing. TF: Investigation, Visualization, Writing – review and editing. NB-A: Conceptualization, Funding acquisition, Methodology, Supervision, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. This work was supported by The Commonwealth Fund under Grant 22-23085d.
Acknowledgments
Tania Manríquez Roa for her guidance on conceptualizing, designing, and conducting a Delphi study.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Ali, S., Abdullah, M., Armand, T. P. T., Athar, A., Hussain, A., Ali, M., et al. (2023). Metaverse in healthcare integrated with explainable AI and blockchain: enabling immersiveness, ensuring trust, and providing patient data security. Sensors (Basel) 23, 565. doi:10.3390/s23020565
Benrimoh, D., Chheda, F. D., and Margolese, H. C. (2022). The best predictor of the Future—The metaverse, mental health, and lessons learned from current technologies. JMIR Ment. Health 9, e40410. doi:10.2196/40410
Cerasa, A., Gaggioli, A., Marino, F., Riva, G., and Pioggia, G. (2022). The promise of the metaverse in mental health: the new era of MEDverse. Heliyon 8, e11762. doi:10.1016/j.heliyon.2022.e11762
Chen, D., and Zhang, R. (2022). Exploring research trends of emerging technologies in health metaverse: a bibliometric analysis. SSRN J. doi:10.2139/ssrn.3998068
Ford, T. J., Buchanan, D. M., Azeez, A., Benrimoh, D. A., Kaloiani, I., Bandeira, I. D., et al. (2023). Taking modern psychiatry into the metaverse: integrating augmented, virtual, and mixed reality technologies into psychiatric care. Front. Digit. Health 5, 1146806. doi:10.3389/fdgth.2023.1146806
Glanz, K., Rizzo, A., and Graap, K. (2003). Virtual reality for psychotherapy: current reality and future possibilities. Psychotherapy Theory, Res. Pract. Train. 40 (Skip), 55–67. doi:10.1037/0033-3204.40.1-2.55
Gloeckler, S., and Biller-Andorno, N. (2023). Mental health services in the metaverse: potential and concerns. Swiss Med. Wkly. 153, 40089. doi:10.57187/smw.2023.40089
Ioannou, A., Papastavrou, E., Avraamides, M. N., and Charalambous, A. (2020). Virtual reality and symptoms management of anxiety, depression, fatigue, and pain: a systematic review. SAGE Open Nurs. 6, 2377960820936163. doi:10.1177/2377960820936163
Lush, V., Buckingham, C., Edwards, S., and Bernardet, U. (2020). Towards accessible mental healthcare through augmented reality and self-assessment tools. Int. J. Onl. Eng. 16, 33–42. doi:10.3991/ijoe.v16i04.12095
Nasa, P., Jain, R., and Juneja, D. (2021). Delphi methodology in healthcare research: how to decide its appropriateness. World J. Methodol. 11, 116–129. doi:10.5662/wjm.v11.i4.116
Navas-Medrano, S., Soler-Dominguez, J. L., and Pons, P. (2023). Mixed reality for a collective and adaptive mental health metaverse. Front. Psychiatry 14, 1272783. doi:10.3389/fpsyt.2023.1272783
Niederberger, M., and Spranger, J. (2020). Delphi technique in health sciences: a map. Front. Public Health 8, 457. doi:10.3389/fpubh.2020.00457
Robertson-Preidler, J., Biller-Andorno, N., and Johnson, T. J. (2017). What is appropriate care? An integrative review of emerging themes in the literature. BMC Health Serv. Res. 17, 452. doi:10.1186/s12913-017-2357-2
Keywords: metaverse, mental health, mental health services, appropriate care, ethics, delphi study, policy
Citation: Gloeckler S, Ford TJ and Biller-Andorno N (2025) Delphi study on the metaverse as an appropriate setting for mental health care: conceptualization, opportunities, challenges, and conditions. Front. Virtual Real. 6:1587316. doi: 10.3389/frvir.2025.1587316
Received: 04 March 2025; Accepted: 06 October 2025;
Published: 21 October 2025.
Edited by:
Matthias Quent, Magdeburg Stendal University of Applied Sciences, GermanyReviewed by:
Triton Ong, Doxy.me Inc., United StatesTawseef Ahmad, Bharat Institute of Engineering and Technology (BIET), India
Copyright © 2025 Gloeckler, Ford and Biller-Andorno. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Nikola Biller-Andorno, YmlsbGVyLWFuZG9ybm9AaWJtZS51emguY2g=
 Sophie Gloeckler
Sophie Gloeckler T. J. Ford
T. J. Ford Nikola Biller-Andorno
Nikola Biller-Andorno