- 1Department of Computer Sciences, University of Oxford, Oxford, United Kingdom
- 2Alan Turing Institute, British Library, London, United Kingdom
This study applies a hybrid methodology combining a systematic review and an AI-enhanced pilot study to explore the correlation between physical activity and episodic-paroxysmal anxiety (EPA) within Extended Reality (XR) environments. The pilot study uses a multimodal biometric approach (incorporating accelerometry, heart rate variability (HRV), and skin conductance) integrated with AI-driven pattern recognition algorithms to measure the real-time physiological impact of Dance Movement Therapy (DMT). By establishing a feedback loop between physical activity and anxiety-related biomarkers, the study presents a dynamic framework for non-pharmacological mental health intervention design. The emerging methodologies for AI-driven Preventative Mechanisms, are tested with a pilot study, consisting of a cohort of 20 participants, exploring the correlation between physical activity and anxiety levels through advanced biometric measures such as accelerometers, skin conductance, and heart rate variability. The key findings reveal that Dance Movement Therapy within Extended Reality environments significantly reduces anxiety levels in individuals with episodic-paroxysmal anxiety, as evidenced by measurable improvements in biometric indicators such as heart rate variability and skin conductance.
1 Introduction: the mental health crisis and the metaverse solutions
We spend significant time using technology, and this is affecting our mental health. Without considering what easing effects can be put in place, this can damage the mental health of users, even for users who have not reported mental health issues previously. Some of the statistics we found from the National Health Service (NHS) in the United Kingdom confirm that in England, approximately 26% of young women aged between 16 and 24 years old and 17% of adults report having a common mental health problem in any given week. This number is on the rise (NHS Digital, 2016). Understandably, this is a minimal demographical range to argue that this represents the entire world. Still, with a quick search in the relevant literature, we found that many other regions worldwide had a similarly high number of young people suffering from preventable mental health problems. Mental health problems create the ‘multiple disadvantage’ situation, where approximately 40% of people in England with mental health disabilities also have overlapping difficulties, including homelessness, substance misuse and contact with the criminal justice system (Dixon and Roberts, 2016). Even more concerningly, the number of people with suicidal thoughts is rising faster than those experiencing and reporting mental health problems to the NHS, which can signal that people are finding it harder to cope with mental health problems (NHS Digital, 2016). Mental health conditions pose a significant challenge for healthcare providers and society. The World Health Organization predicts that by 2030, mental health conditions will be the leading cause of disease burden worldwide (World Health Organization, 2020). Since the COVID-19 pandemic was an event that could have influenced the data (Han et al., 2021; Zhou et al., 2020; Tay et al., 2020; Hossain et al., 2020; Huang et al., 2021; Wiederhold and Riva, 2020; Aafjes-van Doorn et al., 2020), the reference data used is from before COVID-19. Nevertheless, current literature argues that the long-term effect of the COVID-19 pandemic will result in worsening mental health problems in our society (Hossain et al., 2020; Pfefferbaum and North, 2020; Kumar and Nayar, 2020).
This paper applies hybrid research methodology combining systematic review and pilot study. The first phase conducts a systematic review of literature on integrating biometric measures such as accelerometry, skin conductance, and heart rate variability to examine the effectiveness of non-pharmacological interventions within Extended Reality for improving mental health, specifically targeting episodic-paroxysmal anxiety (a form of panic disorder).
1.1 Non-pharmacological treatment clinical trials in XR
Clinical trials are vital for assessing the efficacy and safety of non-pharmacological treatments within extended realities (XR) (Gilbert, 2003; Gifford et al., 2020; Morrison et al., 2016; Solenov et al., 2018). The summary of the key postulates in this study include: (a) A diverse cohort must participate in these studies, particularly incorporating underrepresented populations, (b) to ensure inclusivity whilst maintaining methodological integrity, the formulation of precise inclusion and exclusion criteria is paramount, (c) a sophisticated testbed comprising XR devices, sensors, and wearables is required for collecting real-time health metrics during these clinical trials.
Although the proposed methodology for utilising XR in mental health treatment isn’t entirely ground-breaking, virtual reality (VR) has been actively used for over two decades to treat panic disorder, recent advancements in XR headset technology render them lighter and versatile for an array of therapeutic endeavours. Past clinical investigations explored the potential of VR in delivering neurofeedback and biofeedback, amplifying the effects of music and art therapy, and addressing conditions like depression and anxiety.
It’s crucial that these clinical trials adhere to data protection regulations and obtain participant consent for data collection and analysis. In these trials, wearable devices and sensors primarily capture quantitative data, such as metrics on heart rate variability, microvascular perfusion, skin conductance, and physical activity. This primary data is supplemented by interviews and surveys, which provide context, alongside secondary data from open intelligence and existing databases.
1.2 Summary and structure of the study
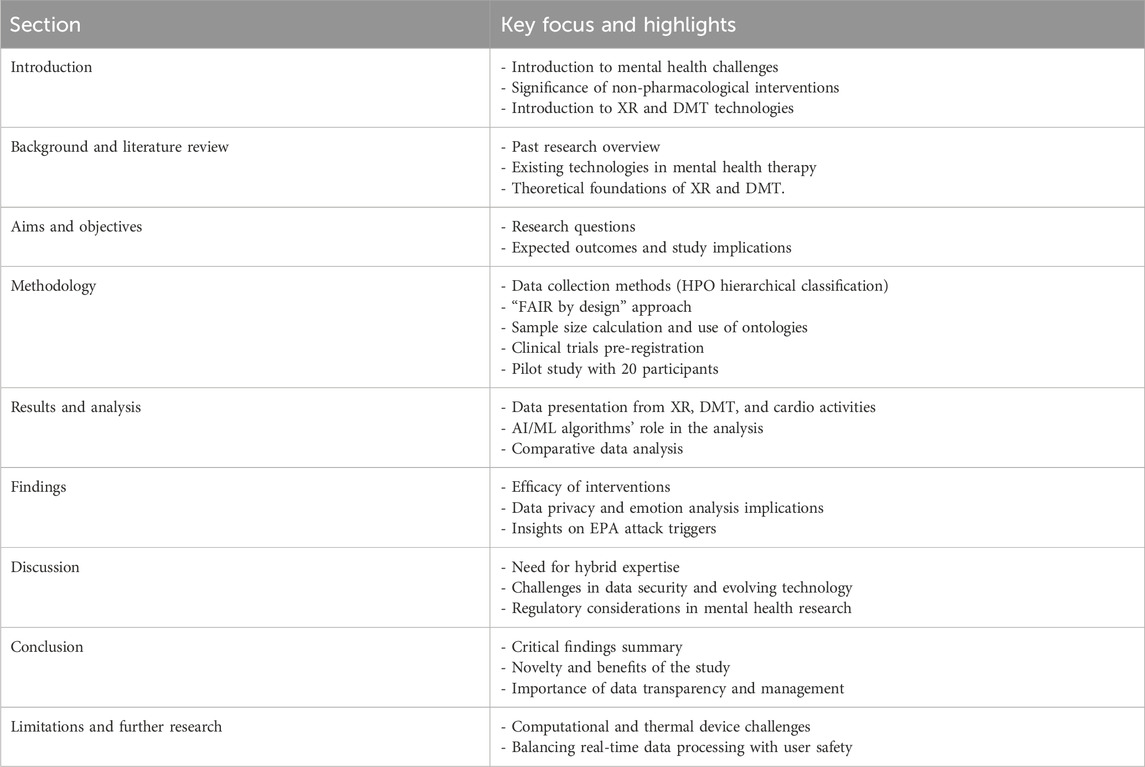
The subsequent table explains the primary structure and principal points of each section of the study to provide readers with a brief overview and better navigation through the expanse of this research. This summary represents the progression from the foundational understanding of mental health challenges and technologies through the methodology and findings to the implications and prospective avenues for further research.
This research differentiates itself from previous studies by introducing a closed-loop AI-feedback mechanism that modulates therapeutic XR content in response to real-time biometric signals. While past studies have evaluated the efficacy of XR and Dance Movement Therapy independently, this study uniquely combines the two within a phenotype-driven testbed informed by Human Phenotype Ontology (HPO) classifications. It further advances the state of research by incorporating predictive modelling based on biometric patterns to personalise therapy delivery. The significance of this study lies in its methodological integration of biometric sensing, AI inference, and immersive therapeutic adaptation, an innovation not explored in prior mental health research using XR modalities.
2 Research methodology
The methodological core of this research lies in its integration of adaptive AI algorithms with biometric signal processing within an ethically compliant testbed. The most influential aspects of the method include (a) the selection of non-invasive, high-resolution biometric indicators such as HRV and skin conductance for continuous emotional monitoring, (b) the implementation of a real-time ML-driven analytics layer capable of detecting anxiety-related physiological triggers, and (c) the application of the FAIR data principles and Human Phenotype Ontology (HPO) to contextualise and refine target populations and data classification. These components collectively ensure the reliability, precision, and clinical adaptability of the methodology.
The research methodology is designed to align with ethical principles and data protection regulations, such as the General Data Protection Regulation (GDPR) (GDPR, 2018; Information Commissioner’s Office, 2018; Li et al., 2019; Degeling et al., 2019; Hintze and El Emam, 2018). It incorporates the FAIR (Findable, Accessible, Interoperable, and Reusable) principles (Wilkinson et al., 2016; Ravi et al., 2022) to enhance research integrity. The design includes a data protection screening process as a preliminary step before clinical trials. Data collection encompasses various aspects: (1) examining the correlation between increased physical activity, as measured by an accelerometer, and self-reported anxiety levels; (2) utilising wearable patches to monitor skin conductance as a sensitive biomarker for anxiety; (3) conducting a meta-analysis of heart rate variability (HRV) and spontaneous fluctuations in heart rate to evaluate autonomic system activity in individuals with anxiety; and (4) employing photoplethysmography (PPG) to measure HRV and assess changes in microvascular perfusion through skin illumination and light transmission or reflection. This methodology is designed to assess if this approach has the potential to open new and non-medicated preventive and therapeutic strategy for mental health conditions, specifically Dance Movement Therapy in Extended Reality environments.
The methodology builds upon earlier work conducted at the University of Oxford, which uses comparative and statistical analysis of secondary data from records extracted from the Web of Science Core Collection. The earlier work, which conducted data analysis, is based on bibliometric packages from the R studio. This study builds upon that work and is focused on.
1. Inclusion and Exclusion Criteria
2. Testbed segregates devices into three distinct categories
3. The connection between the Human Phenotype Ontology (HPO) and the FAIR (Findable, Accessible, Interoperable, and Reusable) framework
The new study focuses on a pilot cohort of 20 participants who were primarily chosen based on symptoms of episodic-paroxysmal anxiety (EPA). The inclusion criteria targeted participants with no previous experience of XR therapies, between the ages of 18–65, and a diagnosis of anxiety or panic disorder. The study was conducted post-COVID-19 and looked specifically at physical activity’s effects on anxiety within XR environments.
This builds upon the earlier work but is also in contrast to the previous work, which used a slightly different participant pool and focused more broadly on individuals with anxiety, panic disorders, and some overlapping comorbid conditions. The inclusion criteria were similar in that they required participants to have a clinical diagnosis of anxiety but with fewer exclusions related to comorbid conditions. The primary outcomes are measured through advanced biometric indicators such as heart rate variability (HRV) and skin conductance, aiming to assess the effect of Dance Movement Therapy (DMT) (Payne, 1992; Meekums et al., 2015; Radanliev, 2025; Millman et al., 2021; Shuper Engelhard and Yael Furlager, 2021; Radanliev, 2024a; Radanliev, 2024b; Re, 2021; Lotan Mesika et al., 2021) within XR on reducing EPA. The secondary outcomes include self-reported anxiety scores and qualitative interviews assessing the impact of physical activity in XR.
The study’s primary focus is on the efficacy of DMT, but with more emphasis on emotional regulation and the effectiveness of virtual avatars for therapy delivery. Secondary measures included participant comfort and interaction with XR technologies, providing a more exploratory view into how users engaged with XR environments.
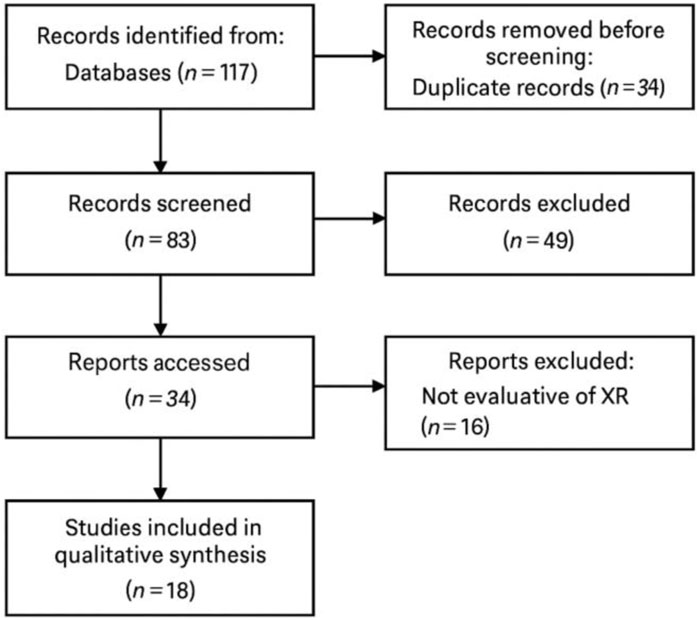
The methodology applied to select the literature for the systematic review included Cochrane Risk of Bias assessment to accompany the PRISMA framework. The PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart was used to document the systematic process of identifying, screening, and including studies in this review. Initially, 117 records were identified through database searches in PubMed, Scopus, and Web of Science using targeted keywords related to extended reality (XR), biometric feedback, and non-pharmacological interventions for anxiety. After removing 23 duplicates, 94 records were screened based on title and abstract. Of these, 56 were excluded for not meeting relevance criteria (e.g., unrelated to XR or mental health). The full texts of the remaining 38 articles were assessed for eligibility. Following detailed review, 20 studies were excluded due to insufficient biometric analysis, lack of empirical data, or not meeting language and methodological thresholds. Ultimately, 18 studies were included in the systematic review, providing robust evidence on the use of XR-based biometric interventions for anxiety reduction. The process is detailed in the Figure 1 flowchart and Table 1.
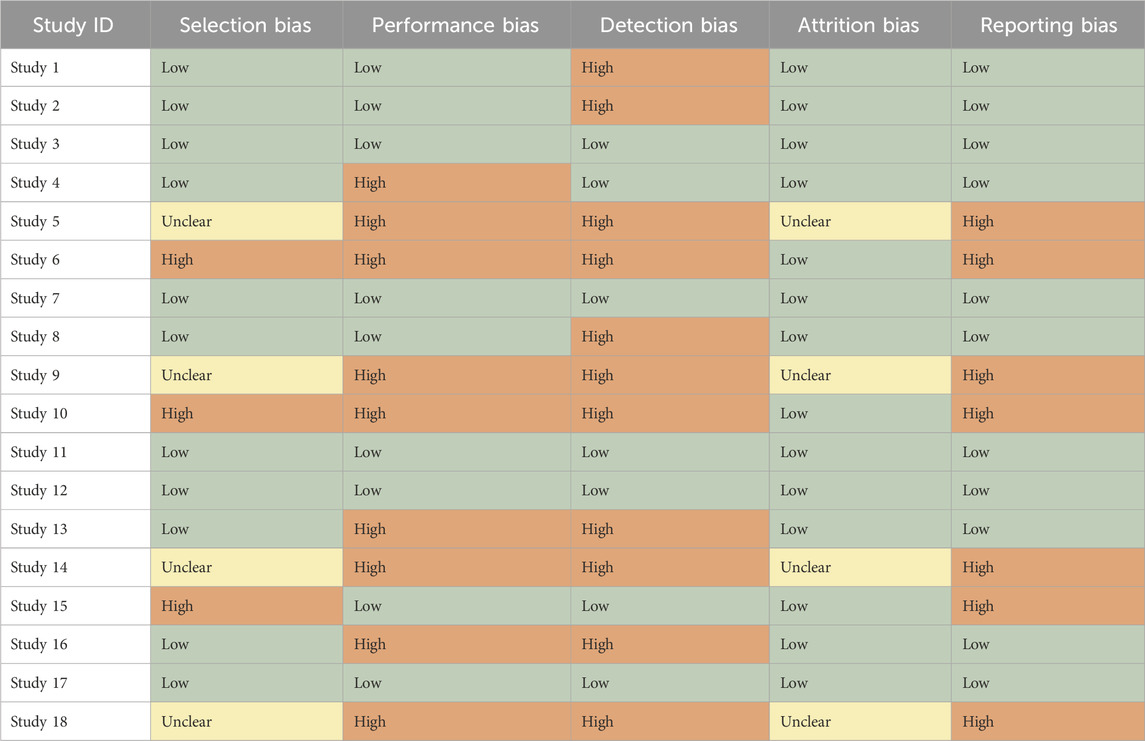
To evaluate the internal validity of the studies included in the systematic review (Figure 1), the study employed an adapted version of the Cochrane Risk of Bias tool tailored for non-randomised and exploratory trials, particularly suited for the XR-based interventions under review. Each study was assessed across five key domains.
1. Selection Bias: Examined whether participant selection was clearly defined and free from systematic differences between groups. Of the 18 included studies, 12 clearly described inclusion/exclusion criteria and random or representative sampling. Six studies had unclear or non-random recruitment, indicating potential bias.
2. Performance Bias: The consistency of intervention delivery was evaluated. Ten studies reported using standardised XR protocols, while others varied significantly in session duration or XR content, introducing moderate to high performance bias.
3. Detection Bias: Blinding of outcome assessors was rarely implemented. Only 4 studies used blinded evaluations or objective biometric measures (e.g., HRV, GSR), while others relied on self-reports. Thus, detection bias was present in the majority.
4. Attrition Bias: Attrition rates and their impact on study outcomes were assessed. Most studies (n = 15) had minimal dropout (<10%) and conducted intention-to-treat analyses. Three studies lacked clear reporting of dropout rates, raising concerns.
Reporting Bias: Evaluated selective reporting by comparing registered outcomes (when available) against published results. Eleven studies adhered to preregistered protocols, whereas seven did not specify pre-established outcomes.
While most studies demonstrated low to moderate risk of bias in key areas, performance and detection bias were commonly observed (Table 1). These limitations were considered during data synthesis and in formulating conclusions. A detailed tabular breakdown of the risk assessment is included in the supplementary materials (Table 2).
To ensure methodological transparency and validity of the included studies, the methodology employed an adapted Cochrane Risk of Bias tool suitable for non-randomised, XR-based mental health intervention research. Each of the 18 studies was independently assessed across five domains: selection bias, performance bias, detection bias, attrition bias, and reporting bias. The evaluation considered recruitment strategies, intervention delivery consistency, the objectivity of outcome assessment (e.g., biometric vs self-report), dropout rates, and adherence to preregistered outcomes. Bias levels were rated as Low, High, or Unclear and tabulated accordingly. Special attention was given to biometric data collection protocols and ethical standards, which directly influenced the detection and performance bias ratings. Discrepancies between reviews were resolved through consensus discussions, and findings were summarised in a colour-coded table (Table 2), enabling transparent appraisal of the internal validity across studies included in the systematic review.
2.1 Pilot study on research methodology and clinical trial design validation
2.1.1 Objective of the study
Before initiating the comprehensive clinical trial described in the main study, testing the validity and reliability of our research methodology and the proposed clinical trial design was imperative. This pilot study validated the feasibility of the experimental setup, the instruments used, and the data analysis processes.
2.1.2 Design and methods
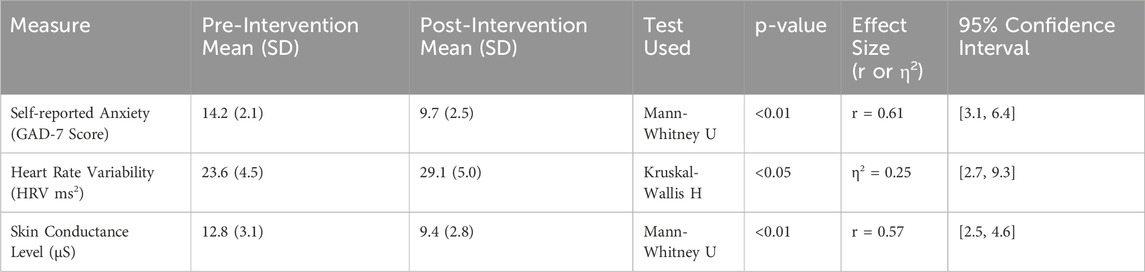
A smaller cohort of 20 participants experiencing symptoms of anxiety and mild depression was enrolled for this pilot study. The study spanned 2 weeks and followed a similar approach to the main trial design but with an abridged version of the interventions. Given the exploratory design and limited sample size of the pilot study, the testing employed non-parametric statistical methods to evaluate pre- and post-intervention changes. Specifically, the testing used the Mann-Whitney U test to analyse differences in self-reported anxiety scores and skin conductance levels, while the Kruskal-Wallis H test was applied to assess heart rate variability. For each outcome, the methodology calculated p-values, effect sizes (r or η2), and 95% confidence intervals. To evaluate the relationship between subjective and objective indicators, the methodology also computed Spearman’s rho correlations between self-reported anxiety and biometric measures. These methods were chosen to ensure robust yet appropriately cautious inference, recognising the small sample size and pilot nature of the study.
2.1.2.1 Interventions
Participants engaged in short DMT sessions within XR environments twice a week. In addition, one cardiovascular activity, light jogging, was integrated as a control measure.
2.1.2.2 Measurements
1. Physical activity correlation: Participants wore accelerometers to correlate physical activity with self-reported anxiety.
2. Anxiety biomarker: Wearable patches were used to monitor skin conductance.
3. Heart rate variability: HRV was evaluated through meta-analysis and photoplethysmography (PPG).
2.1.2.3 Data Analysis
Real-time AI/ML analytics were incorporated on a smaller scale to assess triggers and patterns.
2.1.3 Results
The pilot study found that the methodologies proposed were feasible. The correlation between physical activity and self-reported anxiety provided preliminary evidence of the therapeutic benefits of DMT in XR. The wearable patches effectively recorded skin conductance, and HRV measurements were consistent using both methods.
Although the sample size was small, real-time AI/ML analytics on the XR devices efficiently identified potential triggers and patterns (Table 3).
To assess preliminary therapeutic impact, the testing conducted non-parametric statistical analyses appropriate for the small cohort size. Results indicated a statistically significant reduction in self-reported anxiety scores (GAD-7) from pre-intervention (M = 14.2, SD = 2.1) to post-intervention (M = 9.7, SD = 2.5), with a Mann-Whitney U test showing p < 0.01 and a strong effect size (r = 0.61, 95% CI [3.1, 6.4]). Heart rate variability (HRV) showed an increase from 23.6 (SD = 4.5) to 29.1 (SD = 5.0) ms2, analysed using Kruskal-Wallis H test (p < 0.05, η2 = 0.25, CI [2.7, 9.3]). Skin conductance levels decreased significantly from 12.8 to 9.4 μS (p < 0.01, r = 0.57, CI [2.5, 4.6]). These results are summarised in Table 3.
2.1.4 Ethical and data security implications
A crucial aspect of the pilot study was testing the data security measures. A mock run of the data collection, storage, and analysis processes was done to ascertain whether they complied with the standards set by the ICO, GDPR, and HIPAA. Participants’ anonymity and confidentiality were maintained, and a third-party audit was conducted to ensure data privacy and security measures were in place.
To ensure regulatory compliance with the United Kingdom General Data Protection Regulation (GDPR), the Information Commissioner’s Office (ICO) guidelines, and the U.S. Health Insurance Portability and Accountability Act (HIPAA) (Schoppmann and Sanders, 2004; Johnston and Roper, 2000; HIPAA, 1996), the study employed a multi-layered data governance and ethical compliance framework, which was both implemented and subjected to evaluative review. Prior to data collection, a formal Data Protection Impact Assessment (DPIA) was conducted following ICO best practices. This assessment identified data categories, minimisation strategies, potential risks, and mitigation controls, specifically tailored for high-sensitivity biometric data such as heart rate variability and skin conductance.
Participants provided informed consent through a tiered digital consent mechanism, incorporating transparency notices that outlined data retention policies, the scope of algorithmic processing, and individual data rights. Data capture was designed around a privacy-by-design architecture in which biometric information was stored exclusively on encrypted, air-gapped local devices. No biometric data were transmitted via cloud services, and no third-party analytics tools were integrated during the pilot study.
A mock audit of the data processing pipeline was conducted to benchmark the implementation against HIPAA’s technical and administrative safeguards. This included verification of access controls, encryption at rest, audit logging capabilities, and integrity checks. Access to raw biometric data was limited to a single-author role operating under role-based access restrictions, secured through multi-factor authentication. Post-intervention, a data deletion protocol consistent with GDPR Article 17 (‘right to erasure’) and HIPAA-compliant data disposal procedures was executed. Anonymisation keys and audit logs were retained securely for a limited 90-day period to accommodate potential withdrawal requests, after which all sensitive metadata were permanently deleted.
This approach operationalised abstract regulatory principles into concrete technical and procedural controls, integrating continuous monitoring mechanisms such as breach detection alerts, access logs, and audit-ready metadata. By embedding these practices into the study design, the research ensured that ethical compliance was not merely declarative but demonstrable, enforceable, and subject to formal validation. The pilot study served as a precursor to a longitudinal clinical trial study and helped refine the methodologies, ensure ethical compliance, and estimate the preliminary effectiveness of the proposed interventions. Based on the insights derived from this preliminary study, modifications were made to the main trial’s protocol, ensuring ethically compliant research process.
3 Clinical trials design: a novel methodology for appraising non-pharmacological therapies in XR
For the reliable assessment of conscious, unrestricted movement as a therapeutic intervention for specific mental health ailments like depression, anxiety, and panic attacks, it’s imperative to emphasise the principles of diversity, equity, and inclusion in forthcoming clinical trials. Beyond the customary participant cohort, which might encompass university personnel, academics, researchers, students, dancers, and industry professionals, concerted efforts are necessary to rope in underrepresented sectors. This includes people experiencing homelessness and individuals with physical disabilities. It’s paramount to cultivate a participant base that mirrors the manifold facets of our society. While qualitative sampling methods can be instrumental, due consideration must be allotted to marginalised sections already grappling with mental health challenges, those in the throes of homelessness, and individuals with physical disabilities. To bolster inclusivity for these underserved sectors, the trials should proactively rope in participants from (a) the community of physically disabled individuals, (b) the homeless community, and (c) bodies dedicated to aiding these marginalised groups. By accentuating the participation of these demographics, we can magnify the scope and resonance of the clinical trials while tailoring the studies to the nuanced needs of a diverse mental health-affected populace. Concurrently, it’s pivotal for researchers to liaise with pertinent stakeholders and community allies to fashion customised enlistment strategies and cement the authentic involvement of these marginalised factions.
Clinical trials probing alternative therapies should target human phenotypes, such as abnormal fear/anxiety-related behaviour. Anxiety, as delineated in the Human Phenotype Ontology (HPO)1, is characterised as an Intense feelings of nervousness, tenseness, or panic, often in reaction to interpersonal stresses’. Whilst these manifestations are concurrent in various panic disorders, anxiety disorders represent merely one of the six panic disorder types that warrant exploration in the clinical study. This spectrum encompasses phobias, panic attacks, generalised anxiety disorder (GAD), obsessive-compulsive disorder (OCD), social anxiety disorder, and post-traumatic stress disorder (PTSD). However, the focal point of the clinical trial should be the dissection and validation of three non-pharmacological treatments tailored to a distinct human phenotype, such as EPA episodes. EPA is typified by sporadic unforeseen panic bouts devoid of ties to any setting, making them unpredictable and marked by intense anxiety2.
3.1 Formulating inclusion and exclusion criteria
When crafting the design for the clinical trial, researcher must thoroughly analyse demand and prerequisites grounded on previously established inclusion and exclusion criteria. This process can commence with direct dialogues with individuals and entities the researcher is already aligned with and can expand to outreach efforts directed at organisations serving the disabled community or orchestrating scoping workshops. An alternative exploration avenue is capitalising on pre-existing research insights and drawing from the literature corpus. This design process naturally becomes a ‘snowball’ procedure, where subsequent partners are identified and pursued based on recommendations.
Engaging with and pinpointing the relevant organisations is essential to the design of a methodology that is, at its core, developed by and personalised for disabled individuals. Many well-known bodies and collectives cater to individuals facing mental health challenges. Prominent among them are The Association for Dance Movement Psychotherapy, the European Association of Dance Movement Therapy, American Dance Therapy Association, Indian Association of Dance Movement Therapy, The Mental Health Foundation, Response, CALM, Mind, PAPYRUS, and a plethora of other institutions and communities.
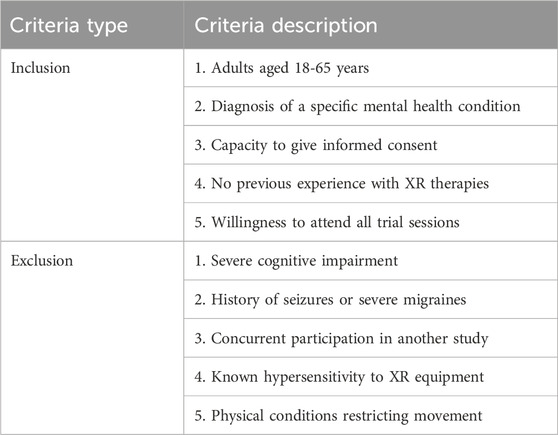
The next step in the clinical trial design is to determine the inclusion and exclusion criteria. An example extracted from reviewing existing studies is included in Table 4 below. This is a fundamental stage in the clinical trial design, and it entails delineating precise inclusion and exclusion criteria, assuring the appropriate and representative involvement of participants. Presented below, in Table 4, is an illustrative set of such criteria.
However, after interviewing practitioners who perform clinical trials in this area of research, we realised that Table 4 can serve only as an example, and the guidance criteria require modifications tailored to the specific characteristics and necessities of a particular study.
In our research on advancing mental health research within the extended realities (XR), ensuring that methodologies are rigorous, precise, and contextually relevant becomes crucial. While comprehensive, the initial Inclusion and Exclusion criteria presented in Table 6 demanded further refinement to better cater to our specific research niche. It’s imperative to understand that mental health isn’t a monolithic domain. It’s multi-faceted, comprising a spectrum of conditions, each with unique characteristics and challenges. Therefore, a ‘one-size-fits-all’ approach in clinical trials, particularly concerning participant criteria, can dilute the specificity and, consequently, the validity of our findings. Given the difficulties associated with each mental health condition, corrections to the table were not just desirable but necessary. Making these criteria more tailored to the mental health condition under study ensures the research is meaningful and results are actionable within its designated context.
Table 2 below includes the specific inclusion and exclusion criteria we designed for a cross-sectional study of people with EPA in the United Kingdom.
The inclusion and exclusion criteria in Table 5 are designed based on recommendations from a diverse set of clinical trial studies on the related subjects to this study (Day, 1967; Eisen et al., 1990; Geller, 2020; Gilbert, 2003; Hofmann et al., 2010; Lewis and Brigder, 2004; Morrison et al., 2016; Shapiro, 1999; Sharma et al., 2006; Yohannes et al., 2010).
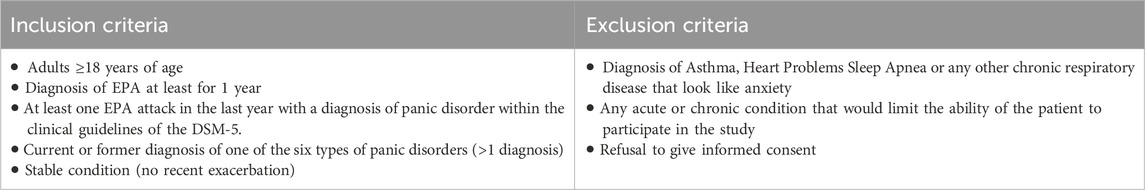
Table 5. Inclusion and exclusion criteria for developing alternative therapies for mental health problems on XR devices.
To protect against bias, the statistical analysis estimated the power calculation in small sample sizes, e.g., Kruskal-Wallis H, Mann-Whitney U test, Pearson’s Chi-Square Test. In addition, for the data oversight arrangements, the clinical trial must consider data minimisation and access. The data minimisation process includes determining the minimal data required to run the statistical data analysis for general linear and non-linear modelling, multilevel modelling, time series analysis, classical test theory, item response theory, gaussian modelling, and psychometrical approaches. Data access needs to be restricted with the design of a specific AL/ML algorithm based on the use of minimum privileges (also known as the principle of least privilege (PoLP), the principle of minimal privilege (PoMP) or the principle of least authority (PoLA)). Data is analysed on the device, but data is not stored, only categories of correlated triggers and effectiveness of the therapies in XR. Data access to the classes must be restricted to the clinical trial researchers only and secured with multi-factor authentication, electronic signatures, and data encryption.
3.2 Estimating duration: streamlined approaches to achieving statistically relevant participant numbers in clinical trials
Within the scope of this study, we addressed one of the most time-intensive aspects of clinical trials: the formulation of thorough and specific participant criteria. Clinical trials’ throughput and overall duration hinge on several crucial determinants, such as recruitment speed, the pool of eligible participants, and the intricacies of the study design. We have streamlined this process by meticulously determining the demand and requirements, anchored on the inclusion and exclusion criteria in Table 5. This was achieved by leveraging our established connections with key individuals and organisations and capitalising on invaluable insights from scoping workshops and the rich tapestry of existing research literature. By proactively involving disabled individuals and associated organisations, we ensured a methodology that resonates with the target demographic.
Our strategic outreach to leading mental health organisations and communities, including The Association for Dance Movement Psychotherapy, the European Association of Dance Movement Therapy, and others, facilitated the efficient identification of potential participants. Table 2’s criteria, which prioritises adults aged 18 and over diagnosed with EPA, formed the backbone of our participant selection, simultaneously sidelining individuals with comorbidities or conditions that could potentially curtail their active participation.
In our endeavours to curtail bias, the statistical analysis embedded within this study embraced methods tailored for smaller sample sizes, notably the Kruskal–Wallis H test, Mann-Whitney U test, and Pearson’s Chi-Square Test. Data oversight was meticulously handled, accentuating data minimisation and stringent access controls. This involved identifying the leanest data for our multi-faceted statistical analysis and devising an AI/ML algorithm tailored to distil only the most pertinent categories. This precious data was stringently controlled, only accessible to our clinical trial team, fortified by multi-factor authentication, electronic signatures, and advanced encryption methodologies.
Whilst it’s impractical to universally predict throughput and duration without a granular view of contextual specifics and recruitment dynamics, practitioners can now confidently use the strategies and processes developed in this study. This accelerates the clinical trial design process and reinforces the authenticity and validity of resultant findings.
3.3 Designing the testbed: components and financial considerations
The design of the Testbed is key for the successful execution of the clinical trial. Within our methodology, we have carefully constructed a testbed consisting of various XR equipment, from augmented reality (AR) to virtual reality (VR) sets, and an array of interconnected IoT sensors, devices, and wearables. This arrangement is instrumental in collecting real-world data, which enhances the precision of subsequent questionnaires and interviews after each XR-based DMT session.
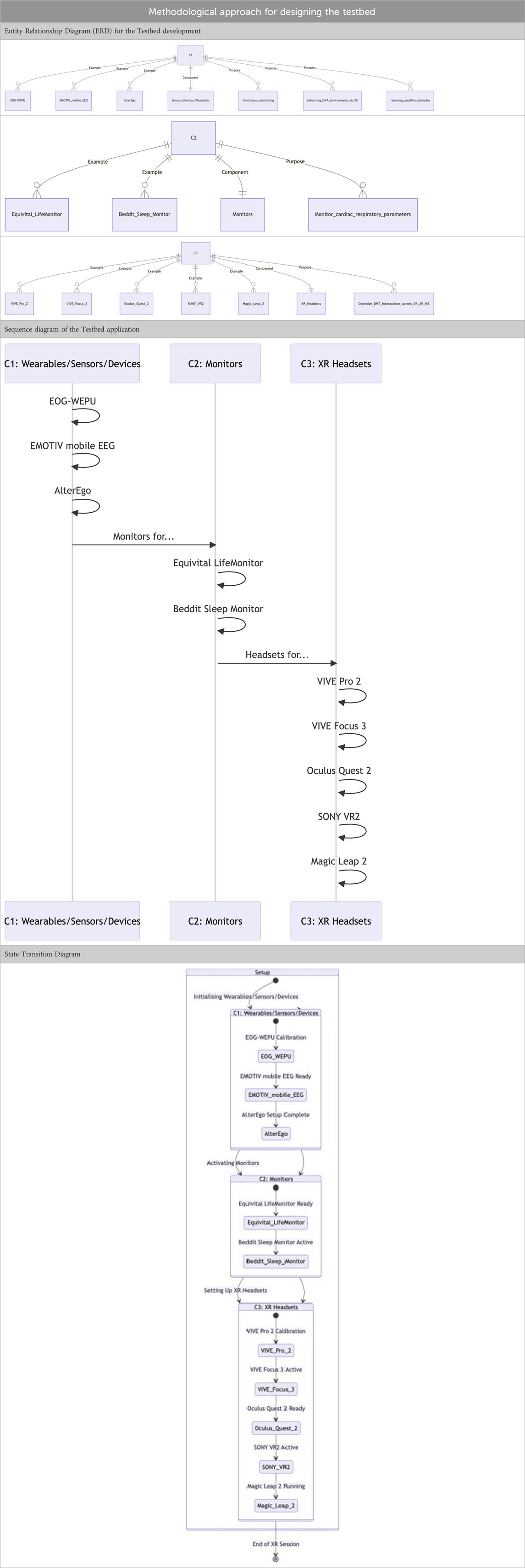
Our Testbed segregates devices into three distinct categories.
• Category C1: Focused on sensors, devices, and wearables. These are primed for continuous monitoring and aim to amplify the safety, efficiency, and overall user experience of XR DMT sessions while mitigating usability challenges. Examples include wearables like EOG-WEPU, EMOTIV mobile EEG, and AlterEgo.
• Category C2: Centralised on heart and breathing rate monitors and sleep trackers. Products such as the Equivital LifeMonitor and Beddit Sleep Monitor have been shortlisted. Their role is to vigilantly monitor the participant’s cardiac and respiratory parameters during and after DMT sessions.
• Category C3: This category uses XR headsets to optimise DMT interactions across VR, AR, and mixed realities (MR). Noteworthy mentions in this category include the VIVE Pro 2, VIVE Focus 3, Oculus Quest 2, SONY VR2, and Magic Leap 2.
While the transportation of the Testbed incurs expenses, it’s an investment that opens doors for enriching public interaction, enabling events such as public demonstrations, seminars for healthcare practitioners, and broader community outreach.
The key concepts of the new methodological approach are visualised in a conceptual diagram provided in Table 6.
The diagrams in Table 6 are designed using Mermaid3.
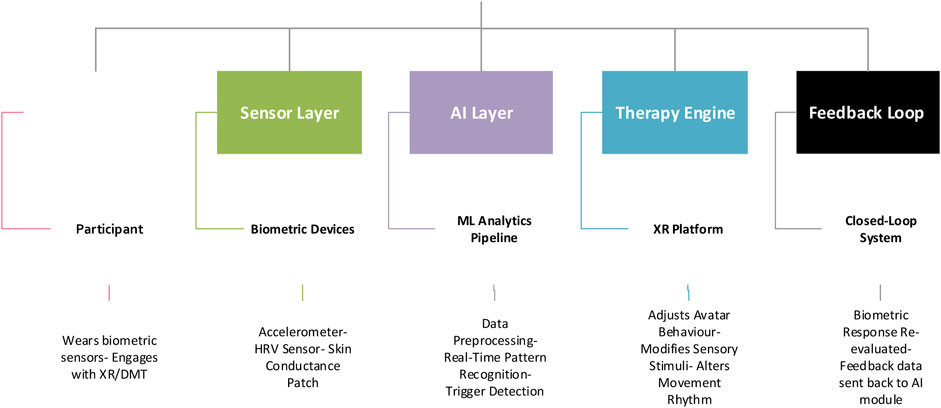
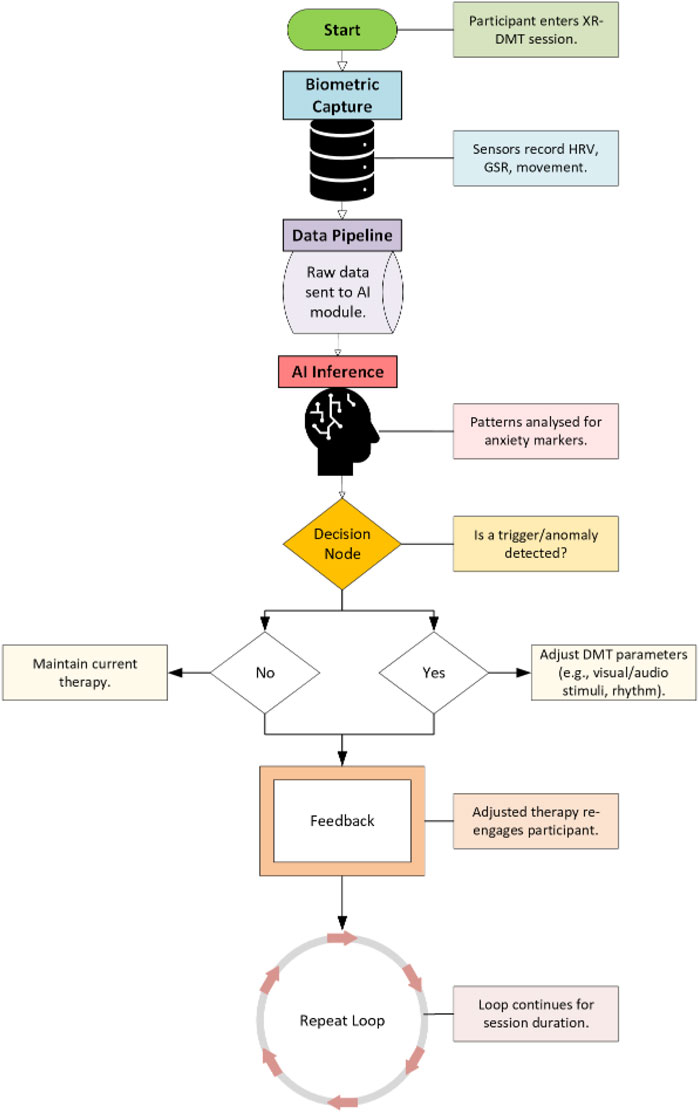
The AI-Driven Adaptive Feedback Loop presented in Figure 2 is designed to visualise the real-time interaction between participants, biometric sensors, AI analytics, and the XR therapeutic platform within the mental health testbed. This diagram serves as a conceptual bridge, illustrating how biometric data collected from users is continuously processed through a machine learning pipeline to inform and dynamically adjust the therapeutic delivery. It provides a modular perspective on how each system layer (user engagement, biometric sensing, AI interpretation, and therapy modulation) contributes to a closed-loop, self-regulating intervention environment tailored for EPA.
The flowchart in Figure 2 is structured across five distinct operational layers: the User Layer, Sensor Layer, AI Layer, Therapy Engine, and the Feedback Loop. The participant engages with an immersive XR environment while wearing biometric sensors that capture real-time data such as heart rate variability and skin conductance. This information is analysed by a lightweight AI/ML engine responsible for preprocessing, pattern recognition, and trigger detection. When physiological stress markers are identified, the AI directs the XR platform to adapt avatar behaviour, alter sensory input, or modify movement rhythms accordingly. This adaptation is then reassessed via biometric feedback, thus completing the closed-loop cycle. The diagram captures the essential temporal logic and flow dependencies that underpin the system’s responsiveness.
The closed-loop testbed architecture (Figure 3) underpinning this research formalises the integration of sensing, interpretation, and response mechanisms into a unified experimental framework.
Unlike conventional XR interventions, this testbed embodies a real-time data fusion strategy where biometric signals are directly linked to the adaptive modulation of therapeutic content. By embedding artificial intelligence at the core of the processing pipeline, the testbed ensures that individual physiological responses actively shape the structure and timing of each therapeutic session. This architecture also incorporates modular privacy and compliance layers, ensuring that data flow adheres to GDPR and HIPAA requirements while enabling dynamic reconfiguration for different use cases and clinical contexts.
Within this architecture, data from multiple biosensors are synchronised and passed through an AI inference engine that evaluates the presence of anxiety-related phenotypic patterns. These insights drive automated adjustments in the XR-DMT therapy, such as slowing avatar movements, altering ambient stimuli, or introducing cognitive grounding cues. The system supports a recursive logic model, where therapeutic efficacy is monitored and recalibrated continuously during the session. Importantly, the testbed is built to accommodate edge AI deployment, ensuring low-latency processing without compromising privacy. By aligning technical infrastructure with both therapeutic precision and ethical governance, this architecture provides a novel framework for intelligent, phenotype-aware mental health interventions in immersive environments.
3.4 Visual description of the proposed methodology for conducting clinical trials
The tables and diagrams offer a systematic visual representation of the testbed design and its components. The table categorises the equipment required for the clinical trials into three distinct categories: wearables, monitors, and XR headsets. Each type itemises specific devices, showcasing a comprehensive list of tools to be employed. This structured layout aids in understanding and comparing the equipment and ensures that all necessary tools are accounted for.
Beyond the table, the state transition diagram serves as a dynamic visual guide to the sequence and interaction of these devices. It provides an operational flow, highlighting how each category is initialised, what specific devices within those categories are activated, and the sequence in which they interact. The flow from one state to the next is clear, with distinct pathways and nodes representing each device. The hierarchical setup facilitates a new understanding of the process, from general categories to specific devices. Overall, these visual aids enhance clarity and help bridge the gap between conceptualisation and practical implementation, making the planning and execution of clinical trials more efficient and informed.
The implementation of the proposed methodology in real-world clinical settings presents several challenges. The most significant obstacle is the continuous real-time processing requirement for biometric data, which demands robust edge computing infrastructure to avoid latency without compromising privacy. Another difficulty lies in achieving high adherence and immersion levels across diverse populations, especially among individuals with disabilities or motion disorders. Additionally, securing institutional approval for adaptive AI-based interventions, which autonomously alter therapeutic protocols, remains a regulatory hurdle. These challenges necessitate careful design of technical and procedural frameworks to ensure safe and ethical deployment in human subjects.
4 Discussion: prior early work and the novelty of this research study
While XR technologies and DMT have independently been employed in mental health interventions for over two decades, the contribution of this study lies not in the mere application of these modalities, but in their integration within a purpose-built, AI-enhanced therapeutic testbed governed by biometric feedback and informed by human phenotype ontology (HPO). Unlike prior studies that treat XR or DMT as standalone therapeutic tools, this research introduces a closed-loop feedback system where biometric indicators, specifically HRV and skin conductance, are continuously monitored and interpreted through a lightweight AI/ML pipeline to inform real-time therapeutic adaptation.
This integration represents a significant methodological advancement by enabling the system to modulate therapeutic intensity and interaction based on the physiological responses of the participant. Furthermore, the study deploys a bespoke testbed architecture that categorises and integrates wearable sensors, XR devices, and physiological monitors into a unified experimental framework. This testbed is designed with interoperability, portability, and clinical compliance in mind, allowing it to be deployed across diverse environments while meeting data privacy and ethical oversight standards.
Another distinctive contribution lies in the formal linkage between the design of the trial and the Human Phenotype Ontology (HPO), which enables a structured, phenotype-driven targeting of EPA as the primary mental health condition under study. Previous research has not operationalised such phenotype-based frameworks in combination with XR and biometric data streams. Finally, the study implements a dual evaluation mechanism, quantitative biometric analysis paired with validated psychological instruments (e.g., GAD-7)—to triangulate findings and reduce reliance on either subjective or physiological data in isolation. This hybrid methodology allows for more robust conclusions regarding feasibility, responsiveness, and ethical applicability in AI-augmented, non-pharmacological interventions.
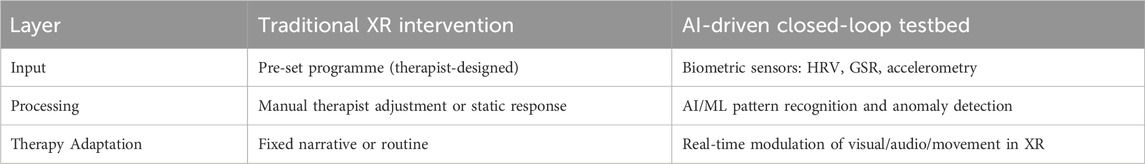
To enhance the interpretability of the discussion and clearly delineate the methodological advancements of this study, a comparison matrix is introduced (Table 7). This matrix contrasts traditional XR-based therapeutic interventions with the AI-enhanced closed-loop testbed developed herein. By mapping the operational flow from data input through processing to therapeutic adaptation, the matrix enables a structured visualisation of how AI-driven methodologies fundamentally reshape the logic and efficacy of mental health interventions in immersive environments.
The matrix in Table 7 presents three core system layers: Input, Processing, and Therapy Adaptation. Traditional XR interventions typically rely on pre-set programmes created by therapists, with minimal flexibility or real-time adjustment. Processing is static, requiring manual oversight, and therapy content follows a fixed trajectory. In contrast, the AI-driven testbed employs real-time biometric sensing (including HRV, GSR, and accelerometry) as dynamic input, which is interpreted through machine learning algorithms capable of detecting anxiety markers. This data informs continuous therapeutic adaptation within the XR environment, modulating visual, auditory, and motor stimuli in response to the user’s physiological state. The matrix thus encapsulates the shift from passive, therapist-led models to intelligent, responsive therapeutic ecosystems.
In this study, we acknowledge the significant role that technology, such as electronic interfaces (e.g., XR) and social media, plays in the context of mental health, particularly concerning depression and anxiety disorders. It is well-established in scientific literature that technology can have a dual impact, acting as a contributing factor to these conditions and a potential solution. Therefore, it is imperative to differentiate and examine the distinct contributions of technology to provide a comprehensive understanding and effectively evaluate the efficacy of proposed interventions. To address this critical aspect, we thoroughly review the existing literature, analysing the influence of technology on mental health outcomes. By exploring the diverse body of research, we aim to clarify how technology can exacerbate mental health conditions and offer supportive tools for their management. This comprehensive analysis will enhance our discussion on the effectiveness of our proposed solution and provide a balanced perspective on the role of technology to mental health.
The methodological approach designed in this study has been applied in practice for two decades, and VR has already been used for panic disorder therapy (Vincelli and Riva, 2002). There are also existing VR therapists and clinics4. In 34 recent clinical trials, virtual reality was used to treat depression and anxiety with cognitive behavioural therapy and exposure therapy (Baghaei et al., 2021). VR can also be used to enhance music therapy (Adjorlu et al., 2019), and art therapy (Schaaf, 2019), and can be used to provide neurofeedback (Rezaie Khosravi and Mahmoodi, 2018) and biofeedback (Kim et al., 2019). Since the most recent 34 clinical trials were completed, XR headsets have become much lighter (e.g., Oculus Quest25 weight 503g–or below 5% of a human participants body weight). They can now be safely used for DMT, outdoor cardio exercises (e.g., running, cross-fit), and many other physical activities that were not possible with the previous version of the headsets.
5 Conclusion
The most beneficial methodological outcome of this research is the demonstration of a real-time, AI-driven therapeutic feedback loop that uses biometric inputs to tailor XR-based mental health interventions. This closed-loop architecture provides a foundation for personalised, responsive, and ethically governed treatment models that are both non-invasive and non-pharmacological. Future research should explore longitudinal deployment of this model, integration with more complex affective computing algorithms, and expansion into other clinical phenotypes such as PTSD or generalised anxiety disorder. Further investigation into edge AI deployment, cross-device synchronisation, and behavioural co-intervention modalities will enhance scalability and translational impact.
This study found significant improvements in HRV and skin conductance, indicating a strong correlation between physical activity (specifically DMT) in XR environments and reduced anxiety levels among participants with EPA. The study also highlights the importance of regulatory and ethical considerations in data security, especially with AI-driven emotion analysis. The study builds upon an earlier work from the University of Oxford (Department of Computer Science) which concluded that XR combined with DMT had potential benefits for mental health but focused more on emotional well-being and therapeutic outcomes in terms of avatar interaction and overall engagement in a virtual environment. It offered preliminary evidence of XR’s utility but suggested further research was needed on the biometric aspect of the treatment.
The pilot study, which employed a robust methodological framework incorporating advanced biometric measures such as accelerometers, skin conductance, and heart rate variability, provides compelling evidence of the therapeutic potential of DMT in XR environments. The findings suggest that these interventions can have a positive impact on anxiety levels, offering a promising alternative to conventional pharmacological treatments, particularly for individuals experiencing episodic and unpredictable anxiety attacks.
The methodological approach of this study, grounded in the principles of the Human Phenotype Ontology (HPO) and the FAIR (Findable, Accessible, Interoperable, and Reusable) framework, has been meticulously designed to ensure the credibility and replicability of the results. The emphasis on data transparency, ethical compliance, and the pre-registration of clinical trials further underscores the rigour and integrity of the research.
The study found that DMT within XR significantly reduced anxiety levels in individuals with EPA. Measurable improvements were seen in heart rate variability and skin conductance. The study highlights the potential of XR-based interventions as a feasible non-pharmacological treatment for episodic anxiety and suggests further large-scale clinical trials. The study presents a more focused and experimentally validated approach targeting a specific mental health condition, with clearly defined inclusion/exclusion criteria and outcome measures, distinguishing it from the broader scope and theoretical nature of the earlier research work in this area.
5.1 Limitations and further research
The purpose of this study was to extract knowledge from existing literature on mental health preventative mechanisms and conduct a pilot test with a small group of participants. However, the paper requires a more detailed longitudinal study and clinical trial studies to confirm the validity of the results. Ethical considerations, especially concerning data security and privacy in the use of AI and emotion analysis technologies, are critically assessed in compliance with the regulatory requirements from the United Kingdom’s Information Commissioner’s Office (ICO), the EU’s GDPR, and the United States’s HIPAA.
The study acknowledges the inherent challenges in the deployment of XR technologies, particularly concerning the demands on computational power and the risks of device overheating during prolonged use. These limitations are not insurmountable but rather point to the necessity for continued innovation in the hardware and algorithmic design to enhance user safety and comfort.
This research contributes to the growing body of evidence supporting the efficacy of XR-based interventions and sets a high standard for future research in this domain. Further studies can build upon these findings, addressing the technological challenges identified and exploring the scalability of these interventions. By applying the design developed in this study in a longitudinal study, we can ensure that XR technologies provide inclusive, effective, and ethically sound mental health treatments that meet the complex needs of our contemporary society.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding author.
Ethics statement
The studies involving humans were approved by The Central University Research Ethics Committee (CUREC), the University of Oxford, has granted ethical approval under reference R51864/002. All participants gave written informed consent. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
PR: Conceptualization, Data curation, Formal Analysis, Funding acquisition, Investigation, Methodology, Project administration, Resources, Software, Supervision, Validation, Visualization, Writing – original draft, Writing – review and editing.
Funding
The author(s) declare that financial support was received for the research and/or publication of this article. Funding: Funding source: This work has been supported by the EPSRC [grant number EP/S035362/1], the Bill and Melinda Gates Foundation [Reference code: INV-057591], and EPSRC SPRITE+.
Acknowledgments
Eternal gratitude to the Fulbright Visiting Scholar Project.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. Grammarly was used to check grammar and spelling errors.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Footnotes
2https://www.ncbi.nlm.nih.gov/medgen/923185
3https://github.com/mermaid-js/mermaid
4https://www.xr.health/what-we-treat/
5https://www.meta.com/gb/quest/products/quest-2/
References
Aafjes-van Doorn, K., Békés, V., and Prout, T. A. (2020). Grappling with our therapeutic relationship and professional self-doubt during COVID-19: will we use video therapy again? Counselling Psychology Quarterly, 34(3–4), 473–484. doi:10.1080/09515070.2020.1773404
Adjorlu, A., Barriga, N. B. B., and Serafin, S. (2019). Virtual reality music intervention to reduce social anxiety in adolescents diagnosed with autism spectrum disorder. In: 16th Sound and Music Computing Conference; 2019 May 28–31; Malaga, Spain: Sound and Music Computing Network. p. 261–268.
Baghaei, N., Chitale, V., Hlasnik, A., Stemmet, L., Liang, H. N., and Porter, R. (2021). Virtual reality for supporting the treatment of depression and anxiety: scoping review. JMIR Ment. Health 8 (9), e29681. doi:10.2196/29681
Day, M. E. (1967). An eye-movement indicator of type and level of anxiety: some clinical observations. J. Clin. Psychol. 23, 438–441. doi:10.1002/1097-4679
Degeling, M., Utz, C., Lentzsch, C., Hosseini, H., Schaub, F., Holz, T., et al. (2019). We value your privacy … now take some cookies: measuring the GDPR’s impact on Web privacy. San Diego, CA, USA: Network and Distributed Systems Security (NDSS) Symposium. doi:10.14722/ndss.2019.23378
Dixon, J., and Roberts, C. “Welsh Health Survey 2015: Health status, illnesses, and other conditions,” Welsh Health Survey. Available online at: https://www.gov.wales/sites/default/files/statistics-and-research/2019-02/160622-welsh-health-survey-2015-health-status-illnesses-other-conditions-en.pdf (Accessed July 17, 2025).
Eisen, A. R., Rapee, R. M., and Barlow, D. H. (1990). The effects of breathing rate and pCO2 levels on relaxation and anxiety in a non-clinical population. J. Anxiety Disord. 4, 183–190. doi:10.1016/0887-6185(90)90010-7
General Data Protection Regulation (2018). What is GDPR, the EU’s new data protection law?. Strasbourg, France: GDPR.eu. Available online at: https://gdpr.eu/what-is-gdpr/(Accessed July 7, 2023).
Geller, J. D. (2020). Introduction: psychotherapy through the lens of cinema. J. Clin. Psychol. 76, 1423–1437. doi:10.1002/jclp.22995
Gifford, G., McCutcheon, R., and McGuire, P. (2020). Neuroimaging studies in people at clinical high risk for psychosis. In: Risk factors for psychosis: paradigms, mechanisms, and prevention. Amsterdam, Netherlands: Elsevier. p. 167–182.
Gilbert, C. (2003). Clinical applications of breathing regulation: beyond anxiety management. Behav. Modif. 27, 692–709. doi:10.1177/0145445503256322
Han, Z., Tang, X., Li, X., Shen, Y., Li, L., Wang, J., et al. (2021). COVID-19-Related stressors and mental health among Chinese College students: a moderated mediation model. Front. Public Health 9, 586062. doi:10.3389/fpubh.2021.586062
Hintze, M., and El Emam, K. (2018). Comparing the benefits of pseudonymisation and anonymisation under the GDPR. J. Data Protec. Privacy 2 (2), 145–158. doi:10.69554/QSST9019
HIPAA (1996). Health insurance portability and accountability act of 1996 (HIPAA). Atlanta, Georgia: CDC. Available online at: https://www.cdc.gov/phlp/publications/topic/hipaa.html (Accessed July 7, 2023).
Hofmann, S. G., Sawyer, A. T., Witt, A. A., and Oh, D. (2010). The effect of mindfulness-based therapy on anxiety and depression: a meta-analytic review. J. Consult Clin. Psychol. 78, 169–183. doi:10.1037/a0018555
Hossain, M. M., Tasnim, S., Sultana, A., Faizah, F., Mazumder, H., Zou, L., et al. (2020). Epidemiology of mental health problems in COVID-19: a review. F1000Res 9, 636. doi:10.12688/F1000RESEARCH.24457.1
Huang, S., Yang, J., Fong, S., and Zhao, Q. (2021). Artificial intelligence in the diagnosis of COVID-19: challenges and perspectives. Int. J. Biol. Sci. 17, 1581–1587. doi:10.7150/ijbs.58855
Information Commissioner’s Office (ICO) (2018). The UK GDPR,” UK GDPR guidance and resources. Available online at: https://ico.org.uk/for-organisations/data-protection-and-the-eu/data-protection-and-the-eu-in-detail/the-uk-gdpr/ (Accessed July 8, 2023).
Johnston, M. B., and Roper, L. (2000). “HIPAA Becomes Reality: Compliance with New Privacy, Security, and Electronic Transmission Standards,” West Virginia Law Review. Available online at: https://researchrepository.wvu.edu/cgi/viewcontent.cgi?article=1498&context=wvlr (Accessed July 17, 2025).
Kim, Y. I., Jung, S. Y., Min, S., Seol, E., Seo, S., Hur, J. W., et al. (2019). Visuo-haptic-based multimodal feedback virtual reality solution to improve anxiety symptoms: a proof-of-concept study. Psychiatry Investig. 16, 167–171. doi:10.30773/pi.2018.12.25.1
Kumar, A., and Nayar, K. R. (2020). COVID 19 and its mental health consequences. J. Ment. Health. 30 (1):1–2. doi:10.1080/09638237.2020.1757052
Lewis, D., and Brigder, D. (2004). “Market Researchers make Increasing use of Brain Imaging,” Advances in clinical neuroscience and rehabilitation. Available online at: https://web.archive.org/web/20120206070204/http://www.drdavidlewis.co.uk/assets/NeuroMarket1.pdf (Accessed July 17, 2025).
Li, H., Yu, L., and He, W. (2019). The impact of GDPR on global technology development. J. Glob. Inf. Technol. Manag. 22, 1–6. doi:10.1080/1097198x.2019.1569186
Lotan Mesika, S., Wengrower, H., and Maoz, H. (2021). Waking up the bear: dance/movement therapy group model with depressed adult patients during Covid-19 2020. Body Mov. Dance Psychother. 16, 32–46. doi:10.1080/17432979.2021.1879269
Meekums, B., Karkou, V., and Nelson, E. A. (2015). Dance movement therapy for depression. Cochrane Database Syst. Rev. 2016, CD009895. doi:10.1002/14651858.CD009895.pub2
Millman, L. S. M., Terhune, D. B., Hunter, E. C. M., and Orgs, G. (2021). Towards a neurocognitive approach to dance movement therapy for mental health: a systematic review. Clin. Psychol. Psychother. 28, 24–38. doi:10.1002/cpp.2490
Morrison, C., Culmer, P., Mentis, H., and Pincus, T. (2016). Vision-based body tracking: turning Kinect into a clinical tool. Disabil. Rehabil. Assist. Technol. 11, 516–520. doi:10.3109/17483107.2014.989419
NHS Digital (2016). Adult psychiatric morbidity survey (APMS): survey of mental health and wellbeing, England, 2014. England: NHS Digital.
Payne, H. (1992). Dance movement therapy: theory and practice. London: Routledge. Available online at: https://books.google.co.uk/books?hl=en&lr=&id=J1KIAgAAQBAJ&oi=fnd&pg=PP1&ots=wUlF4AZ1ng&sig=OKy4PM2KqmKpXEGmcz15UyikM5U#v=onepage&q&f=false (Accessed April 1, 2025).
Pfefferbaum, B., and North, C. S. (2020). Mental health and the covid-19 pandemic. N. Engl. J. Med. 383, 510–512. doi:10.1056/nejmp2008017
Radanliev, P. (2024a). Dance as a mental health therapy in the Metaverse: exploring the therapeutic potential of Dance Movement Therapy as a non-pharmacological treatment in the Metaverse. Front. Comput. Sci. 6, 1334027. doi:10.3389/fcomp.2024.1334027
Radanliev, P. (2024b). Dance sport movement therapy in the metaverse: a new frontier for alternative mental health therapies. Digit. Health 10. doi:10.1177/20552076241258273
Radanliev, P. (2025). Virtual dance movement therapy for reducing anxiety, and artificial intelligence for monitoring the body and mind during therapy. Res. Dance Educ., 1–15. doi:10.1080/14647893.2025.2486256
Ravi, N., Chaturvedi, P., Huerta, E. A., Liu, Z., Chard, R., Scourtas, A., et al. (2022). FAIR principles for AI models with a practical application for accelerated high energy diffraction microscopy. Sci. Data 9 (9), 657–659. doi:10.1038/s41597-022-01712-9
Re, M. (2021). Isolated systems towards a dancing constellation: coping with the Covid-19 lockdown through a pilot dance movement therapy tele-intervention. Body Mov. Dance. Psychother. 16, 9–18. doi:10.1080/17432979.2021.1879934
Rezaie Khosravi, N., and Mahmoodi, G. (2018). Effect of neurofeedback therapy based on virtual reality technology on anxiety in patients with anxiety disorder. Social Determinants of Health 4 (2), 78–83. doi:10.22037/sdh.v4i2.20396
Schaaf, A. (2019). Tilt brush: the utilization of a virtual reality intervention for evaluating self-reported anxiety, depression, and stress: Scholar@UC. doi:10.7945/PNCA-X073
Schoppmann, M. J., and Sanders, D. L. (2004). HIPAA compliance: the law, reality, and recommendations. J. Am. Coll. Radiology 1, 728–733. doi:10.1016/j.jacr.2004.03.017
Shapiro, F. (1999). Eye movement desensitization and reprocessing (EMDR) and the anxiety disorders: clinical and research implications of an integrated psychotherapy treatment. J. Anxiety Disord. 13, 35–67. doi:10.1016/s0887-6185(98)00038-3
Sharma, A., Madaan, V., and Petty, F. D. (2006). Exercise for mental health. Prim. Care Companion J. Clin. Psychiatry 8, 106. doi:10.4088/pcc.v08n0208a
Shuper Engelhard, E., and Yael Furlager, A. (2021). Remaining held: dance/movement therapy with children during lockdown. Body Mov. Dance Psychother. 16, 73–86. doi:10.1080/17432979.2020.1850525
Solenov, D., Brieler, J., and Scherrer, J. F. (2018). The potential of quantum computing and machine learning to advance clinical research and change the practice of medicine. Mo. Med. 115, 463–467. (Accessed July 17, 2025).
Tay, M. Z., Poh, C. M., Rénia, L., MacAry, P. A., and Ng, L. F. P. (2020). The trinity of COVID-19: immunity, inflammation and intervention. Nat. Rev. Immunol. 20, 363–374. doi:10.1038/s41577-020-0311-8
Vincelli, F., and Riva, G. (2002). Virtual reality: a new tool for panic disorder therapy. Expert Rev. Neurother. 2 (3), 377–383. doi:10.1586/14737175.2.3.377
Wiederhold, B., and Riva, G. (2020). Virtual reality meets COVID-19: the Potential of positive technology Against the Burden of coronavirus. In: Annual review of cybertherapy and telemedicine 2020. San Diego, CA: Interactive Media Institute. Available online at: https://www.researchgate.net/publication/351578980_ANNUAL_REVIEW_OF_CYBERTHERAPY_AND_TELEMEDICINE_2020 (Accessed March 3, 2023).
Wilkinson, M. D., Dumontier, M., Aalbersberg, I. J., Appleton, G., Axton, M., Baak, A., et al. (2016). The FAIR Guiding Principles for scientific data management and stewardship. Sci. Data 3 (3), 160018–160019. doi:10.1038/sdata.2016.18
World Health Organization (2020). Doing what matters in times of stress: an illustrated guide. Geneva, Switzerland: World Health Organization.
Yohannes, A. M., Doherty, P., Bundy, C., and Yalfani, A. (2010). The long-term benefits of cardiac rehabilitation on depression, anxiety, physical activity and quality of life. J. Clin. Nurs. 19, 2806–2813. doi:10.1111/j.1365-2702.2010.03313.x
Keywords: XR (extended reality), virtual reality (VR), artificial intelligence (AI), mental health, non-pharmacological interventions, biometric technologies, emotion analysis, digital identity privacy
Citation: Radanliev P (2025) Ethical methodologies for digital identity privacy in AI-driven dance movement therapy as a preventative mental health mechanism in the extended reality. Front. Virtual Real. 6:1589744. doi: 10.3389/frvir.2025.1589744
Received: 07 March 2025; Accepted: 30 June 2025;
Published: 28 July 2025.
Edited by:
Athina Papadopoulou, New York Institute of Technology, United StatesReviewed by:
Hongjian Pu, University of Pittsburgh, United StatesHenning Enric Garcia Torrents, University of Rovira i Virgili, Spain
Leonidas Gavrilas, University of Ioannina, Greece
Syahril Syahril, Bandung State Polytechnic, Indonesia
Copyright © 2025 Radanliev. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Petar Radanliev, cGV0YXIucmFkYW5saWV2QGNzLm94LmFjLnVr
 Petar Radanliev
Petar Radanliev