- 1Wladyslaw Bieganski Collegium Medicum, Jan Długosz University in Częstochowa, Częstochowa, Poland
- 2Faculty of Medicine, Academy of Silesia in Katowice, Katowice, Poland
- 3MedCu Technologies Ltd., Herzliya, Israel
- 4The Skin Research Institute, The Dead-Sea and Arava Science Center, Masada, Israel
- 5Department of General Surgery, Surgical Outpatient Clinic of Healthcare Centre of Jan Paweł II District Hospital in Włoszczowa, Włoszczowa, Poland
Introduction: Local treatment of venous leg ulcers is often a prolonged and painful process. The latest recommendations from the European Wound Management Association emphasize a holistic approach to patient care, integrating pharmacological and non-pharmacological methods.
Objective: The aim of the study was to assess the impact of virtual reality (used during wound cleansing procedure) on the quality of life of patients with venous leg ulcers.
Methods: The randomized controlled trial included 60 patients with venous leg ulcers, who were randomly divided into two groups. The experimental group was exposed to virtual reality during wound cleansing, while the control group did not. Patients’ quality of life was analyzed with the WHOQOL-BREF questionnaire.
Results: At a follow-up assessment conducted 7 days post-treatment, patients in the experimental group reported significantly higher ratings of overall quality of life—across multiple domains—as well as individual perceptions of health, compared to those in the control group.
Conclusion: Virtual reality can serve as a supportive therapy in the treatment of venous leg ulcers, acting as a non-pharmacological tool to reduce pain, improve quality of life, and positively influence patients’ attitudes toward treatment.
1 Introduction
The problem of hard-to-heal wounds is a global issue. The presence of wounds, particularly hard-to-heal ones, significantly affects patients’ quality of life. As society ages and faces growing health challenges such as cardiovascular diseases, diabetes, obesity, infections, and antibiotic resistance, it is predicted that hard-to-heal wounds will become a major clinical, social, and economic challenge. Wound treatment requires a holistic approach, as well as the involvement of multidisciplinary clinical teams (Harding, 2022).
The exact prevalence of hard-to-heal wounds in many European countries remains unclear due to the complexity of disease classification systems (such as the International Statistical Classification of Diseases and Related Health Problems–ICD-10) and inadequate epidemiological surveillance. Without national wound registries, epidemiological and treatment cost estimates are often extrapolated from data from industrialized countries with comprehensive statistics (Lazarus et al., 1994).
Venous leg ulcers occur most often in elderly individuals with chronic venous insufficiency. Due to the lack of a systematized registration process, it is not possible to provide exact data related to its epidemiology (Probst et al., 2023). In Poland, there are also no precise statistics regarding the status of hard-to-heal wounds. In the largest epidemiological study conducted in Poland so far, which included 40,095 patients of family doctors, active venous ulcers were detected in 0.55% of respondents, while the presence of active or healed ulcers was found in 1.52% of individuals. Therefore, it is necessary to conduct continuous research and establish a common methodological strategy to determine the exact scale of the problem (Jawień et al., 2011).
Patients with hard-to-heal wounds often suffer from persistent pain, stress, depression, and anxiety about an uncertain future, which can lead to social exclusion. Due to pain, limited mobility, and the need for ongoing medical care, they struggle to participate in public and family life. Many are forced to leave their jobs and social activities, leading to isolation and a decreased quality of life. Additionally, access to specialized wound care clinics and hospitals can be challenging for many patients (Kapp and Santamaria, 2017; Finlayson et al., 2017).
When planning care for a patient with a hard-to-heal wound, it is always necessary to consider not only physical limitations but also economic status, education, access to medical facilities, living conditions, and support from loved ones (Vogt et al., 2020). The economic situation can directly impact treatment and rehabilitation, as poor socio-economic conditions affect both access to healthcare services and the ability to use them (Borges et al., 2018).
According to the World Health Organization (WHO), quality of life is defined as the “individual perception by a person of their life position in the cultural context and value system in which they live, and in relation to tasks, expectations, and standards determined by environmental conditions” (WHOQOL Group, 1995). This definition presents a holistic approach, including health, social, and economic aspects. In the treatment process of venous leg ulcers, attention is often focused solely on the wound itself, whereas for many patients, whose wounds have a poor prognosis, improving quality of life becomes more important (Olsson and Friman, 2020). Quality of life questionnaires provide essential information about the domains of life that deteriorate and allow for the overall monitoring of a patient’s quality of life, helping to implement necessary interventions to improve it (Savadkoohi et al., 2023).
Quality of life questionnaires have been used for a long time among patients with hard-to-heal wounds (Eckert et al., 2023). There are many general and specific tools for assessing quality of life in patients with non-healing wounds, differing in length and complexity, which is why various studies aim to develop a standardized quality-of-life tool for patients with hard-to-heal wounds (Krupová and Pokorná, 2020). In one of these studies, an assessment of quality of life was conducted in patients included in the Comprehensive Chronic Wound Treatment Program during their first and last visit to the clinic (after 4 weeks). Implementation goal of this program is not only the treatment of hard-to-heal wounds but also prevention and education for patients and their families. The study utilized WHOQOL-BREF and Wound QoL as tools for collecting data on quality of life. After 4 weeks, higher mean values of quality of life assessment were found in all domains (Pytlak et al., 2023). The development and implementation of wound treatment strategies, which focus on improving health-related quality of life and effectively reducing costs for this patient group, is a challenge for modern healthcare systems worldwide (Olsson et al., 2019).
Successful wound treatment depends on multiple factors, including dressings, compression therapy, proper nutrition education, smoking cessation, physiotherapy, and pain management. It is proven, that stress, sleep disorders, poor nutrition, and depression also directly impact the inflammatory response, thereby hindering wound healing (Moffatt et al., 2009). However, pain management remains one of the most overlooked aspects of wound care. Many patients experience severe pain, especially during dressing changes, and while nonsteroidal anti-inflammatory drugs (NSAIDs) are often the first choice, escalating pain frequently leads to the use of narcotics (Szkiler et al., 2024).
Pharmacological treatment should follow the World Health Organization (WHO) analgesic ladder. NSAIDs have a ceiling effect beyond which they cause adverse effects without additional pain relief. Furthermore, prolonged use of NSAIDs, corticosteroids, anticoagulants, aspirin, or other blood thinners can delay wound healing (Szkiler et al., 2024). Indeed, many patients report that the painkillers they receive are insufficient, and the wound dressing change procedure is stressful, negatively affecting their daily functioning (Herberger et al., 2011).
Differences in pain perception between women and men have been observed in numerous studies in recent years, with women showing increased pain sensitivity. Many biopsychosocial mechanisms contribute to differences in pain perception between genders, including sex hormones, genetic factors, and coping strategies for pain (Bartley and Filingim, 2013). A multicentre study found that women with hard-to-heal wounds have a lower quality of life compared to men (Reinboldt-Jockenhöfer et al., 2021).
The longer the pain lasts, the higher the probability of structural changes in the brain, particularly atrophy of grey matter. The consequences of these changes may include: difficulties in establishing social interactions, sleep problems, and an increased risk of depression. People prone to catastrophizing experience greater difficulties in rehabilitation, avoid movement, which can lead to deep vein thrombosis or pneumonia. There is also a high probability that such patients will want to take higher doses of painkillers. Additionally, stress causes excessive cortisol secretion, and its increased level may limit glucose absorption by muscles. Untreated pain contributes to an increase in cortisol levels, which, in turn, begins to destroy muscles, leading to muscle mass loss and delaying the wound healing process (Lalkhen, 2021).
All in all, pain significantly worsens patients’ quality of life. Recognizing this, the European Wound Management Association released a document, Holistic Management of Wound-Related Pain, advocating for the integration of non-pharmacological methods alongside standard pharmacotherapy (Holloway et al., 2024). One such approach is virtual reality, which serves as a distraction tool by engaging both vision and hearing. This immersive technology creates the illusion of being in a relaxing and familiar virtual environment, reducing stress and pain during medical procedures such as wound cleaning and dressing changes (Spyrka et al., 2024).
Virtual reality, as a non-pharmacological method of pain relief, has already been used in the treatment of burns (Smith et al., 2022), in the rehabilitation of burn patients (Lan et al., 2023), and as an educational and training tool in medicine (Izard et al., 2018). It has been observed that virtual reality helps improve both physical and mental functioning (Riches et al., 2023). This is particularly important in modern times, with the occurrence of various pandemics, such as COVID-19, bringing significant changes to most aspects of life, and patients themselves being more exposed to stress, low mood, and negative effects related to physical and mental health (Siani and Marley, 2021).
Using an appropriate application and introducing the patient into a state of relaxation can not only alleviate pain symptoms but also create a positive attitude toward treatment. For many years, scientists have been studying the relationship between positive thinking, quality of life, disease prevention, and treatment. Numerous studies indicate a beneficial impact of a positive attitude on health, and patients with such an attitude are less vulnerable to stress and illness (Ismail, 2023).
However, in the available literature there is no study showing the impact of virtual reality on the quality of life of patients with venous leg ulcers. Therefore, this study is original, and the results can be subject to international discussion. Virtual reality may become an essential element in the treatment process of venous leg ulcers, positively influencing all domains of life. VR has also the potential to be used during dressing changes, as emphasized by EWMA (European Wound Management Association) in recent document concerning palliative wound care.
2 Materials and methods
2.1 Research group
The randomized controlled trial included 60 patients with venous leg ulcers, randomly assigned to an experimental or control group. Patients in the experimental group used virtual reality goggles during mechanical wound cleaning, while those in the control group underwent the procedure without virtual reality (VR).
The study was conducted at three different medical centres: Surgical Outpatient Clinic of Krapkowice Health Centre, Surgical Outpatient Clinic and Healthcare Centre of Jan Paweł II District Hospital in Włoszczowa, Wound Treatment Clinic of Specialist Hospital of priest B. Markiewicz Subcarpathian oncology Centre in Brzozowo.
The data were collected between July and October 2023.
2.2 Inclusion and exclusion criteria
Inclusion Criteria:
• A wound that has been treated unsuccessfully for more than 3 months
• A wound with an area of up to 20 cm2
• A wound in the proliferative phase of healing
• Signed informed consent to participate in the study
Exclusion Criteria:
• Patients with claustrophobia
• Patients with epilepsy or schizophrenia
• Patients who had undergone cataract surgery or other eye procedures
• Patients with a history of stroke currently undergoing neurological treatment
• Patients with wounds on other stage of healing than proliferative
• Patients who did not provide informed consent
• Patients with complete hearing loss
2.3 Research tools
2.3.1 Virtual reality
The study used Oculus Meta Quest 2, a stand-alone virtual reality headset that does not require a computer connection. The Guided Meditation VR application, available on the Meta Quest platform, allowed patients to immerse themselves in a chosen virtual setting, such as a beach or mountains (Figure 1).
The headset includes a communication module along with the built-in SNAPDRAGON XR2 processor, internal memory, battery, speakers, microphone, and two motion-tracking controllers. It is equipped with an adjustable head strap, as well as customizable interpupillary distance (IPD) and image sharpness settings. The Quest 2 headset is particularly well-suited for individuals whose pupillary distance ranges from 56 to 70 mm, which is typical for 95% of the adult population. Each display offers a resolution of 1832 × 1,920 pixels, yielding a combined total resolution of 3,664 × 1,920 pixels.
Virtual reality equipment isolates the user from the real world. Patients wore VR goggles and noise-cancelling headphones, which blocked hospital sounds and replaced them with immersive sound effects and relaxing music. The displayed visuals responded to head movements, enhancing the sensation of being in a different environment and increasing the distracting effect during the procedure.
2.3.2 Life quality questionnaire
Patients completed on study inclusion the WHOQOL-BREF questionnaire, which evaluates quality of life across four domains:
1. Physical health (daily activities, energy, pain, mobility) – D1
2. Psychological health (self-esteem, emotions, memory, concentration) – D2
3. Social relationships (personal relationships, social support, sexual activity) – D3
4. Environment (financial resources, healthcare access, safety, recreation, transport) – D4
The WHOQOL-BREF questionnaire was developed based on the WHOQOL-100 questionnaire, which was created in the early 1990s at the request of the WHO as a universal research tool for assessing quality of life. It consists of 26 questions. Additionally, the WHOQOL-BREF includes items analyzed separately: the individual overall perception of quality of life (WHO 1) and the individual overall perception of health (WHO 2).
Patients repeated the WHOQOL-BREF questionnaire in a follow-up visit after 7 days. Additionally, the following data were analyzed: sex, age, education, marital status, source of income, place of residence, socio-economic conditions, duration of ulcer and wound area.
2.4 Research procedure–wound debridement
All patients underwent Doppler ultrasound to assess lower limb blood flow and exclude ulcers of non-venous origin.
Patients were also carefully analyzed for inclusion and exclusion criteria. In particular, it was ensured that the wounds were at the same stage of healing in both groups and that there was no difference between groups in terms of the wound initial condition. Moreover, Clinical, Etiological, Anatomical, Pathophysiological classification (CEAP scale) of ulcers was performed in all patients included in the study.
During dressing changes, patients lay on an examination couch in a semi-upright or semi-seated position in a room maintained at 23°C with 40% humidity. In experimental group, they were given basic instructions on using the VR headset, and the lens spacing was adjusted for optimal clarity. Patients were then fitted with the headset and given 5 minutes to acclimate before the dressing change began. Patients in control group underwent dressing change procedure without VR headset application.
In both groups the wound was cleaned using an antiseptic solution containing 0.1% polyhexanide and poloxamer 188, followed by mechanical debridement with a sterile Volkmann spoon. After debridement a copper wound dressing (MedCu Technologies Ltd.) was applied for 7 days.
2.5 Statistical analysis
The statistical analysis was carried out using the Statistica 13.3 TIBCO software from StatSoft, while the database and graphical presentation of results were prepared in Microsoft Excel. Both parametric and non-parametric tests were used for variable analysis. The choice of parametric test was conditioned by meeting its basic assumptions, i.e., the conformity of the distributions of the examined variables with the normal distribution, which was verified using the Shapiro-Wilk test. To assess differences in the average level of a numerical variable in two populations, the Student’s t-test for independent variables was used (Table 1), or alternatively, the Mann-Whitney U test if parametric assumptions were not met (Tables 3–5). A statistical significance level of p < 0.05 was adopted.
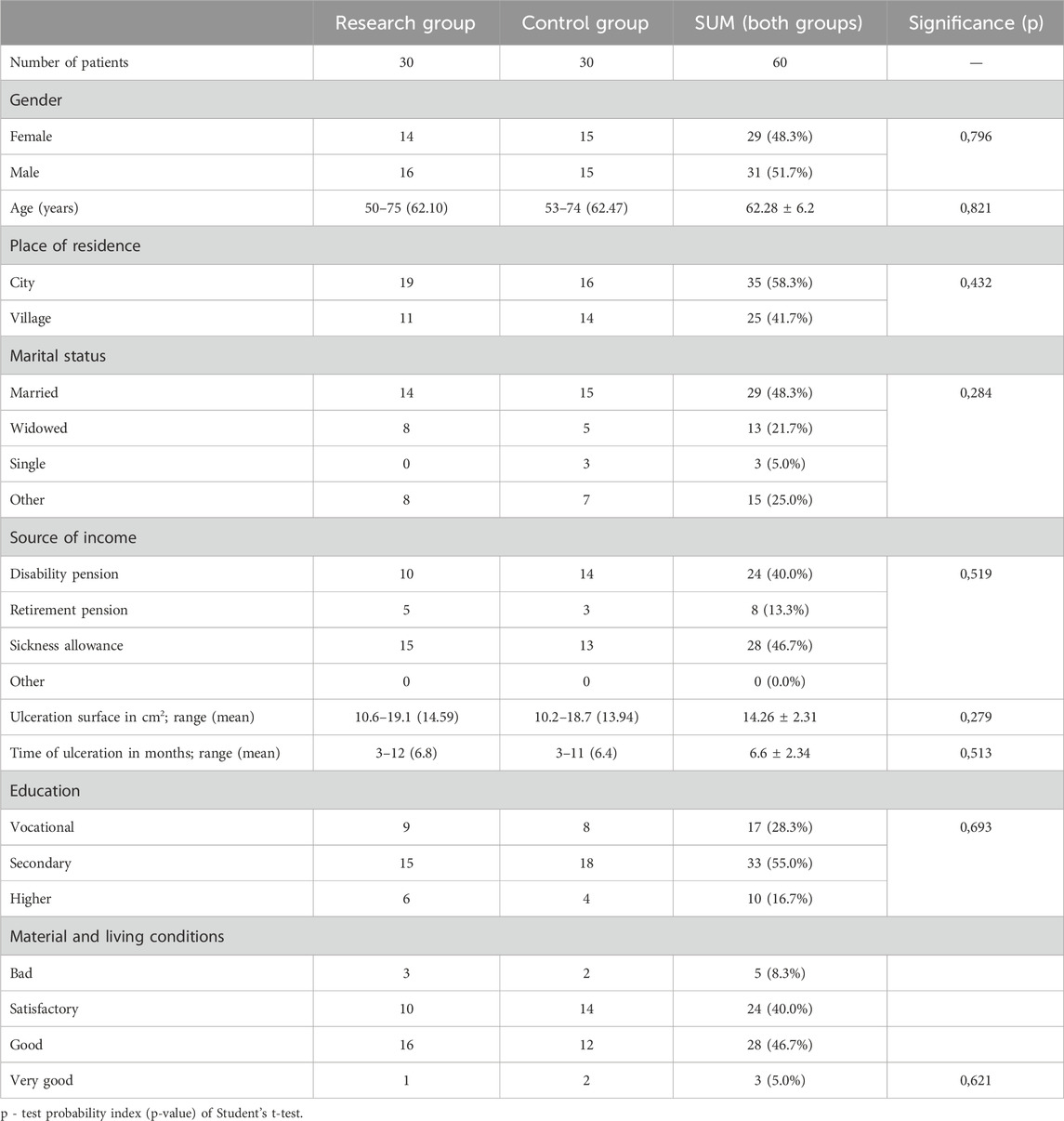
Table 1. Characteristics of the research groups–the most important anthropometric and clinical features.
3 Results
No statistically significant differences were found between the groups in terms of age, gender, marital status, source of income, education, place of residence, source of income, ulcer surface area, and ulcer duration among the respondents from the two groups (Table 1).
According to CEAP scale, most patients suffered from superficial vein system active ulcers and venous reflux (Table 2).
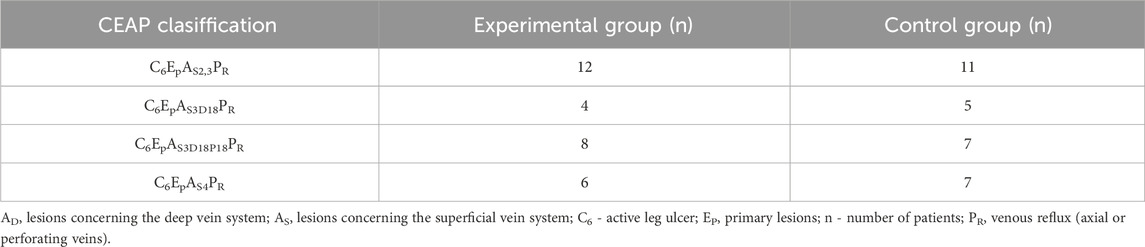
Table 2. Classification of patients according to the clinical, etiological, anatomical, pathophysiological (CEAP) scale.
The changes of values (measurement II–measurement I) obtained in the assessment of quality of life in the periods before and 7 days after wound cleansing were recorded (Table 3).
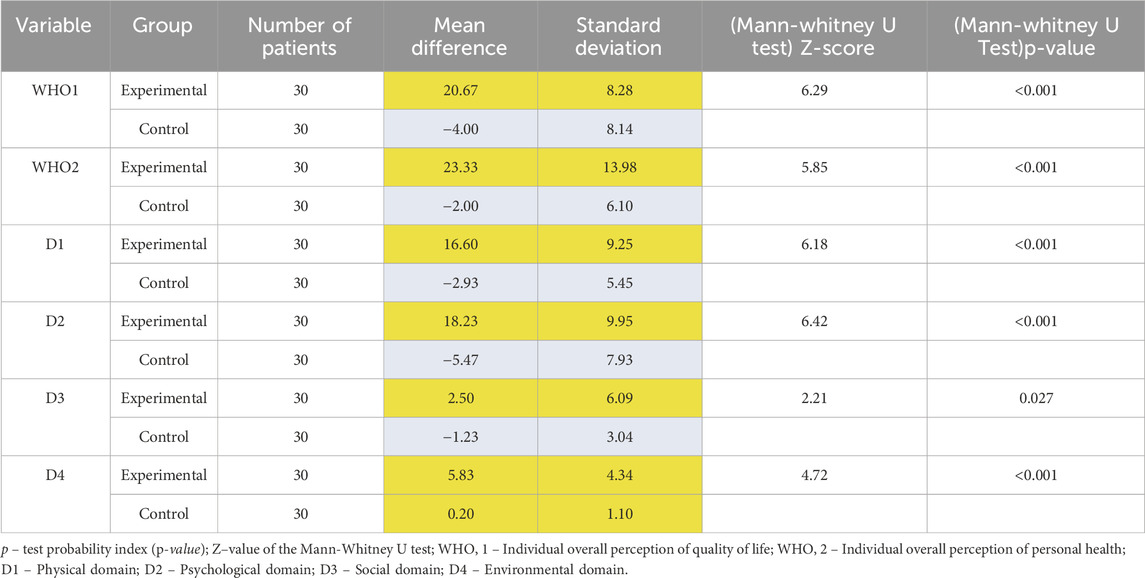
Table 3. Analysis of the difference in quality of life between two measurements (measurement II–measurement I).
Positive results (measurement II > measurement I) indicated an improvement in the quality of life of patients in the period after wound cleansing. Negative results (measurement II < measurement I) indicated a deterioration in their quality of life after wound cleansing. These results were marked respectively in yellow (positive) and blue (negative).
In the experimental group (using VR), a significant improvement was obtained in each of the domains. It could be due to the fact, that VR technology created a sense of safety and relaxation, improving patient comfort during wound care. The least significant improvement was noted in domain D3 (social relationships), but it is still clinically significant.
In contrast, in the control group, improvement was noted only in the environmental domain (D4). In other domains, negative values were obtained, indicating a deterioration in patients’ quality of life. However, the absolute values of these negative changes in the control group are much smaller than the values of positive changes in the experimental group, so this deterioration may not have been clinically significant.
In the pre-wound cleansing measurement, younger individuals (under 60 years old) had a significantly higher quality of life compared to older individuals (60 years and above) in somatic domain - D1 (p = 0.045) and environmental domain - D4 (p = 0.048) (Table 3). In Measurement II, significant differences were observed only in the environmental domain (D4) (p = 0.045).
Overall analysis of the data suggest that quality of life remained higher in younger individuals, but the differences are not always statistically significant (Table 4).
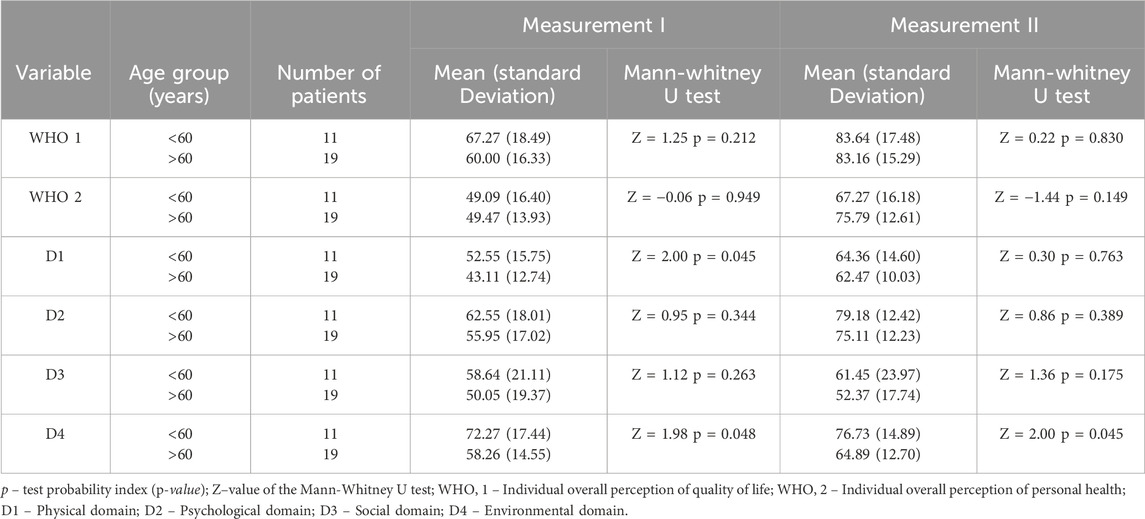
Table 4. Analysis of quality of life in the experimental group between two measurements (measurement II–measurement I) – depending on age.
The quality of life of patients in the pre-wound cleansing measurement was significantly differentiated based on the duration of their illness (p < 0.05). Patients who had been ill for a shorter period (up to 6 months) always reported a higher quality of life compared to those who had been ill for more than 6 months.
In the post-wound cleansing measurement, significant differences between the two groups (patients with disease duration up to 6 months vs over 6 months) were observed in psychological domain (D2), social domain (D3) and environmental domain (D4) (p < 0.05) (Table 5).
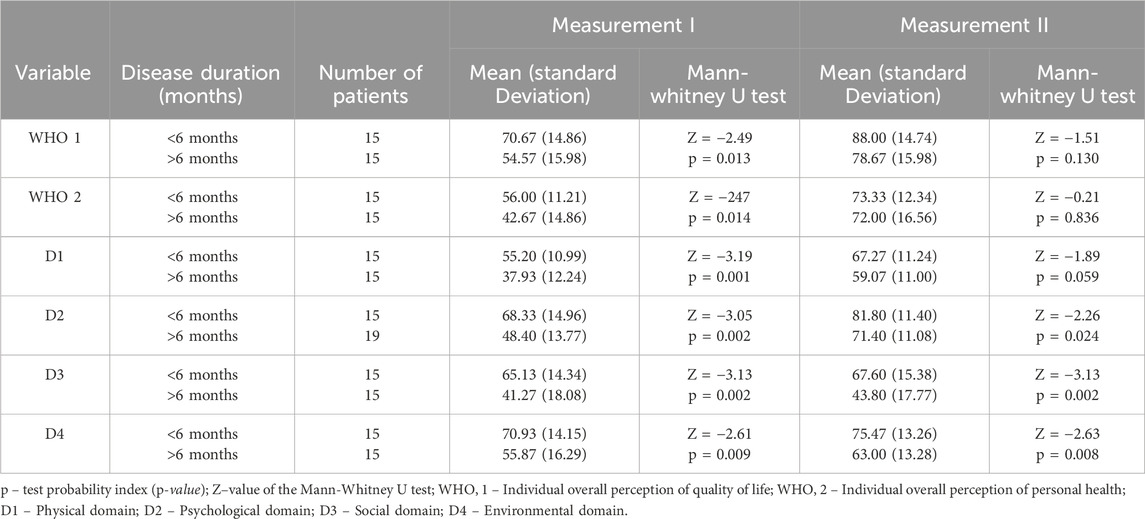
Table 5. Analysis of quality of life in the experimental group between two measurements (measurement II–measurement I) – depending disease duration.
However (independently of statistical significance) patients who had been ill for a shorter period (up to 6 months) had a higher quality of life compared to those who had been ill for more than 6 months (Table 5).
4 Discussion
In the treatment of hard-to-heal wounds, several factors may affect patient adherence to medical recommendations. Quality of life questionnaires can assist in identifying potential barriers to effective treatment.
According to the research conducted by Domingues et al. (2016) and Vieira and Araújo (2018), which used two different tools to assess quality of life in patients with hard-to-heal wounds, most respondents had a low education level and a low family income. Both low education levels and low family income can contribute to longer treatment times and impact patients’ quality of life. For most families, income is focused on meeting basic needs such as food, clothing, and education, while additional treatment costs can affect their living conditions. Additionally, patients with low education levels may have difficulty understanding how to follow self-care guidelines (Oliveira et al., 2013). Our findings revealed that the majority of participants had completed secondary education - 55%. However, 28.3% had vocational education, which may have impacted their level of comprehension regarding clinical guidelines and instructions.
Hard-to-heal wounds affect all spheres of life, particularly the professional activity of patients, whose absence from work becomes so significant that they are forced to transition to early disability pension or retirement (Szewczyk et al., 2015). Research undertaken by Szewczyk et al. demonstrated that, 52% of patients received a disability pension, 85.7% of respondents had to temporarily give up work, and venous leg ulcers were the main reason for early retirement (Szewczyk et al., 2007). Chase’s study, using the SF-36 questionnaire, showed, in turn, that venous leg ulcers cause longer absences from professional activity (Chase et al., 2000). Our experiment confirmed that the primary source of income for most patients was a disability pension or sickness allowance (Table 1). This financial limitation may hinder the treatment process, especially if patients are required to purchase specialized dressings more frequently. In our study, we applied in all 60 patients a non-adherent copper wound dressing that could be maintained on the wound for up to 7 days at any stage of the healing process (Melamed and Borkow, 2023; Borkow and Melamed, 2025).
Age, gender, marital status, and duration of illness are also factors analyzed to determine correlations between them and the quality of life of patients. The aging society is at risk of developing hard-to-heal wounds, as there is a negative relationship between the wound healing process and age (Wicke et al., 2009). In a study conducted in primary healthcare in Singapore among patients with hard-to-heal wounds, the average age of patients was 61.2 years (Zhu et al., 2022), while in other studies, such as in Germany it was 65.3 years (Blome et al., 2014), and in Brazil it was 61.0 years (Vogt et al., 2020). Throughout our study, we identified, the average patient’s age was 62.28 years, which is a similar value to studies conducted by other researchers. A negative impact of age on the domain of vitality and mental health was observed in a study conducted in Brazil, where the SF-36 quality of life questionnaire was used (Dantas et al., 2022). The present study observed that younger individuals, under the age of 60, had a significantly higher quality of life–particularly in the somatic and environmental domains–compared to older individuals aged 60 and above (Table 4).
Many patients with venous leg ulcers experience discomfort due to the existing wound, and this feeling is further intensified by exudate and wound odor. This often leads to withdrawal and limitation of social contacts. Ironically, although social contacts become rarer, patients become increasingly dependent on their families for care (Hareendran et al., 2005). According to empirical findings, individuals who are separated or divorced have been shown to experience a diminished quality of life, especially regarding physical and emotional functioning (Dantas et al., 2022). Family support turns out to be essential in the wound healing process and significantly impacts patients’ quality of life (Lamotte et al., 2022). In our study, the majority of patients were married (Table 1), which could have translated into support and assistance with wound care and adherence to recommendations, such as the use of compression therapy, which is a necessary element in the treatment of venous leg ulcers.
The duration of illness also plays an important role in the quality of life of patients with hard-to-heal wounds. An investigation performed by Zhu et al. showed a worsening in the range of motion among patients who had been ill for more than 6 months (Zhu et al., 2022). Other studies have also noted a decline in quality of life among patients who had been ill for more than 6 months (Hopman et al., 2014; De Oliveira et al., 2019). Similarly, our findings revealed that patients with a shorter illness duration (up to 6 month) reported a higher quality of life compared to those who had been ill for more than 6 months. Thus, our experiment confirmed significant differences between the two groups in the psychological, social, and environmental domains (Table 5).
Virtual reality (VR) enables users to immerse themselves in virtual simulations of natural environments, thereby facilitating the experience of the benefits associated with exposure to nature without the necessity of physically visiting these locales. This technology engenders a sense of presence that promotes profound relaxation and concentrated attention, which are essential elements of mindfulness practice (Riva, 2005). Indeed, our study using the Guided Meditation VR application shows that virtual reality is helpful in improving quality of life, and its effectiveness is supported by research from other scientists. In particular, the use of nature elements has a beneficial impact on mental health.
In research conducted by Ma et al. (2025), preliminary evidence has been presented regarding the efficacy of brief virtual reality-based mindfulness interventions in mitigating symptoms of depression and anxiety among university students. A total of forty-nine university students participated in this quasi-experimental research, which involved assessments at three distinct time points (pre-intervention, post-intervention and follow-up). The results demonstrated that the intervention produced an immediate and statistically significant reduction in anxiety and depression symptoms, alongside improvements in mindfulness, olfactory perception, chemosensory functioning, and sensory imagery. Importantly, the observed decrease in symptoms of depression and anxiety was sustained for 1 week following the intervention (Ma et al., 2025). Our experiment confirmed that exposure to virtual reality during wound cleansing had a positive impact, as observed during the follow-up visit. In the experimental group (using VR), a significant improvement was obtained in each of the domains (Table 3).
The integration of mindfulness practices with exposure to natural environments has been demonstrated to produce substantial enhancements in mental health, particularly in mitigating symptoms associated with anxiety, depression, and cognitive fatigue (Hanley et al., 2017). Natural settings have historically been acknowledged as potent facilitators of mindfulness practices, chiefly due to their capacity to promote cognitive restoration and enhance emotional wellbeing. Consequently, specific natural scenes, including oceans, flowers, rivers, and forests, are frequently incorporated to support mindfulness practice (Ma et al., 2023). The WHOQOL-BREF scale used in our study includes a question regarding the experience of negative feelings such as depression, despair and anxiety (D2 – Psychological health), which significantly impact the healing process and cooperation with the patient. Our experiment confirmed that the use of nature-based applications has potential in distracting patients during painful procedures such as wound debridement.
Other numerous studies have also substantiated the efficacy of virtual reality (VR)-based interventions in enhancing mental health outcomes, particularly concerning anxiety and depression. For example, Failla et al. (2022) identified that VR-enhanced mindfulness interventions were linked to significant reductions in symptoms of anxiety and depression. In a similar vein, Navarro-Haro et al. (2017) demonstrated that VR-facilitated mindfulness could augment mindfulness engagement by immersing participants in tranquil, nature-based virtual environments. These studies underscore the potential of VR to not only replicate natural surroundings but also to intensify the advantages of mindfulness by providing users with a fully immersive and distraction-free experience that fosters emotional regulation and cognitive restoration.
To sum up, a holistic approach to patients with venous leg ulcers may be the key to effective treatment based on good cooperation between patient and medical staff. In the present study, the collected data allowed for the identification of obstacles in the treatment process and the determination of the role of virtual reality in improving quality of life across specific domains. So far, no similar study has been conducted. Distraction through virtual scenes such as forests or beaches during dressing changes may prove to be crucial for patients with hard-to-heal wounds.
4.1 Conclusion
The present study confirmed that the use of virtual reality in patients with venous leg ulcers can have a significant positive impact on all life domains of these patients. We also proved that factors such as age, education, and disease duration play some role in the success of venous leg ulcers’ treatment.
Moreover, the results suggest that virtual reality can also influence the patient’s attitude toward treatment, thereby impacting their engagement, adherence to recommendations, and even shortening the wound healing time. Patients who experienced distraction during treatment may stop associating primary healthcare or hospitals with painful procedures and instead see them as places where they can take a virtual journey each time, steadily working toward wound healing.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by Research Ethics Committee of the Jan Długosz University in Częstochowa. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
KS: Writing – review and editing, Writing – original draft, Formal Analysis, Conceptualization, Methodology, Data curation, Investigation. ER: Writing – review and editing, Supervision, Writing – original draft. AS: Supervision, Writing – review and editing, Formal Analysis. JB: Writing – review and editing, Data curation. GB: Writing – review and editing, Formal Analysis. MK: Investigation, Formal Analysis, Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Acknowledgments
The authors thank Joanna Nowicka MSc for the help and consultation in statistical analysis of the results.
Conflict of interest
Author GB was employed by MedCu Technologies Ltd.
The remaining authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Bartley, E., and Filingim, R. (2013). Sex differences in pain: a brief review of clinical and experimental findings. Br. J. Anaesth. 111 (1), 52–58. doi:10.1093/bja/aet127
Blome, C., Baade, K., Sebastian Debus, E., Price, P., and Augustin, M. (2014). The “wound-QoL”: a short questionnaire measuring quality of life in patients with chronic wounds based on three established disease-specific instruments. Wound Repair Regen. 222 (4), 504–514. doi:10.1111/wrr.12193
Borges, E., Nascimento Filho, H., and Pires Júnior, J. (2018). Prevalência de lesões crônicas de município da zona da mata mineira (brasil). Rev. Min. Enferm. 22, e-1143. doi:10.5935/1415-2762.20180074
Borkow, G., Melamed, E., and Shorr, A. F. (2025). At the intersection of critical care and infectious diseases: the year in review. Biomedicines 12, 562–581. doi:10.3390/biomedicines12030562
Chase, S., Whittemore, R., Crosby, N., Freney, D., Howes, P., and Phillips, T. J. (2000). Living with chronic venous leg ulcers: a descriptive study of knowledge and functional health status. J. Comm. Health Nurs. 17, 1–13. doi:10.1207/S15327655JCHN1701_01
Dantas, J., Silva, A., Augusto, F., Agra, G., Oliveira, J., Ferreira, L., et al. (2022). Health-related quality of life in people with chronic wounds and associated factors. Texto Contexto Enferm. 31, 1–14. doi:10.1590/1980-265x-tce-2022-0010en
De Oliveira, A., De Macêdo, R., Bezerra, S., Andrade, E., Dos Santos, A., and Nogueira, L. (2019). Quality of life of people with chronic wounds. Acta Paul. Enferm. 32 (2), 194–201. doi:10.1590/1982-0194201900027
Domingues, E., Alexandre, N., and Silva, J. (2016). Cultural adaptation and validation of the freiburg life quality assessment - wound module to Brazilian Portuguese. Rev. Latino-Am. Enferm. 24, 2684–2688. doi:10.1590/1518-8345.0289.2684
Eckert, K. A., Fife, C. E., and Carter, M. J. (2023). The Impact of underlying conditions on quality-of-life measurement among patients with chronic wounds, as measured by utility values: a review with an additional study. Adv. Wound Care 12 (12), 680–695. doi:10.1089/wound.2023.0098
Failla, C., Marino, F., Bernardelli, L., Gaggioli, A., Doria, G., Chilà, P., et al. (2022). Mediating mindfulness-based interventions with virtual reality in non-clinical populations: the state-of-the-art. Healthcare 10 (7), 1220. doi:10.3390/healthcare10071220
Finlayson, K., Miaskowski, Ch., Alexander, K., Liu, W. H., Aouizera, t B., Parker, Ch., et al. (2017). Distinct wound healing and quality-of-life outcomes in subgroups of patients with venous leg ulcers with different symptom cluster experiences. J. Pain Symptom Manag. 53 (5), 871–879. doi:10.1016/j.jpainsymman.2016.12.336
Hanley, A. W., Derringer, S. A., and Hanley, R. T. (2017). Dispositional mindfulness may be associated with deeper connections with nature. Ecopsychology 9 (4), 225–231. doi:10.1089/eco.2017.0018
Harding, K. (2022). Chronic wounds: a clinical problem requiring ownership and coordination. Br. J. Dermatology 187, 133–134. doi:10.1111/bjd.21650
Hareendran, A., Bradbury, A., Budd, J., Geroulakos, G., Hobbs, R., Kenkre, J., et al. (2005). Measuring the impact of venous leg ulcers on quality of life. J. Wound Care 14 (2), 53–57. doi:10.12968/jowc.2005.14.2.26732
Herberger, K., Rustenbach, S., Haartje, O., Franzke, N., Schafer, I., Radtke, M., et al. (2011). Quality of life and satisfaction of patients with leg ulcers--results of a community-based study. Vasa 40 (2), 131–138. doi:10.1024/0301-1526/a000083
Holloway, S., Ahmajärvi, K., Frescos, N., Jenkins, S., Oropallo, A., Slezáková, S., et al. (2024). Holistic management of wound-related pain. J. Wound Manag. 25 (1 Suppl. 1), S1–S84. doi:10.35279/jowm2024.25.01.sup01
Hopman, W., Vandenkerkhof, E., Carley, M., Kuhnke, J., and Harrison, M. (2014). Factors associated with health-related quality of life in chronic leg ulceration. Qual. Life Res. 23 (6), 1833–1840. doi:10.1007/s11136-014-0626-7
Ismail, J. (2023). Mind over matter: the impact of positive thinking on health outcomes. J. Community Health Provis. 3 (1), 27–33. doi:10.55885/jchp.v3i1.212
Izard, S., Juanes, J., Penalvo, F., Estella, J., Ledesma, M., and Ruisoto, P. (2018). Virtual reality as an educational and training tool for medicine. J. Med. Syst. 1 (42), 3–50. doi:10.1007/s10916-018-0900-2
Jawień, A., Szewczyk, M. T., Kaszuba, A., Gaciong, Z., Krasiński, Z., Wroński, J., et al. (2011). Guidelines for the management of chronic venous leg ulceration. Recommendations of a multidisciplinary expert group. Leczenie Ran 8 (3), 59–80.
Kapp, S., and Santamaria, N. (2017). The financial and quality-of-life cost to patients living with a chronic wound in the community. Int. Wound J. 14 (6), 1108–1119. doi:10.1111/iwj.12767
Krupová, L., and Pokorná, A. (2020). Quality of life in patients with non-healing wounds, with particular focus on assesment tools - a literature review. Cent. Eur. J. Nurs. Midw 11 (2), 94–103. doi:10.15452/CEJNM.2020.11.0010
Lalkhen, A. G. (2021). Pain: the science of the feeling brain. London, United Kingdom: Atlantic Books.
Lamotte, S., Rappl, A., Freiberger, E., Sieber, C., and Gehr, J. (2022). Functional status and quality of life of geriatric patients with wounds in acute hospitals: a comparison between patients with acute and chronic wounds: a cross-sectional study. Gerontol. Geriatr. 55 (1), 32–37. doi:10.1007/s00391-021-01975-8
Lan, X., Tan, Z., Zhou, T., Huang, Z., Huang, Z., Wrang, Ch., et al. (2023). Use of virtual reality in burn rehabilitation: a systematic review and meta-analysis. Arch. Phys. Med. Rehabil. 104 (3), 502–513. doi:10.1016/j.apmr.2022.08.005
Lazarus, G. S., Cooper, D. M., Knighton, D. R., Margolis, D. J., Percoraro, R. E., Rodeheaver, G., et al. (1994). Definitions and guidelines for assessment of wounds and evaluation of healing. Wound Repair Regen. 2, 165–170. doi:10.1046/j.1524-475x.1994.20305.x
Ma, J., Li, H., Liang, C., Li, S., Liu, Z., and Qu, C. (2025). A brief virtual reality-based mindfulness intervention can improve olfactory perception while reducing depression and anxiety symptoms in university students. Humanit Soc. Sci. Commun. 12, 294. doi:10.1057/s41599-025-04584-7
Ma, J., Zhao, D., Xu, N., and Yang, J. (2023). The effectiveness of immersive virtual reality (VR) based mindfulness training on improvement mental-health in adults: a narrative systematic review. Explore 19 (3), 310–318. doi:10.1016/j.explore.2022.08.001
Melamed, E., and Borkow, G. (2023). Continuum of care in hard-to-heal wounds by copper dressings: a case series. J. Wound Care 32 (12), 788–796. doi:10.12968/jowc.2023.32.12.788
Moffatt, C., Vowden, K., Price, P., and Vowden, P. (2009). “Psychological factors and delayed healing. European wound management association (EWMA),” in Position document. Hard-to-heal wounds: a holistic approach. Available online at: https://woundsinternational.com/best-practice-statements/hard-heal-wounds-holistic-approach-ewma-position-document/(Accessed March 15, 2025).
Navarro-Haro, M. V., López-del-Hoyo, Y., Campos, D., Linehan, M. M., Hoffman, H. G., García-Palacios, A., et al. (2017). Meditation experts try virtual reality mindfulness: a pilot study evaluation of the feasibility and acceptability of virtual reality to facilitate mindfulness practice in people attending a mindfulness conference. PLoS ONE 12 (11), e0187777. doi:10.1371/journal.pone.0187777
Oliveira, B., Castro, J., and Granjeiro, J. (2013). Epidemiologic and clinical overview of patients with chronic wounds treated at an outpatient clinic. Rev. Enferm. UERJ 21 (1), 612–617. doi:10.1590/2177-9465-EAN-2020-0139
Olsson, M., and Friman, A. (2020). Quality of life of patients with hard-to-heal leg ulcers: a review of nursing documentation. Br. J. Community Nurs. 1 (25), 13–19. doi:10.12968/bjcn.2020.25.Sup12.S12
Olsson, M., Järbrink, K., Divakar, U., Bajpai, R., Upton, Z., Schmidtchen, A., et al. (2019). The humanistic and economic burden of chronic wounds: a systematic review. Wound Repair Regen. 27 (1), 114–125. doi:10.1111/wrr.12683
Probst, S., Saini, C., Gschwind, G., Stefanelli, A., Bobbink, P., Pugliese, M., et al. (2023). Prevalence and incidence of venous leg ulcers—a systematic review and meta-analysis. Int. Wound J. 20 (9), 3906–3921. doi:10.1111/iwj.14272
Pytlak, K., Szymańska, P., Skórka, M., and Bazaliński, D. (2023). Quality of life of patients covered by the complex treatment of chronic wounds. Surg. Vasc. Nurs. 17 (1), 38–45.
Reinboldt-Jockenhöfer, F., Babadagi, Z., Dieter, H., Risse, A., Rammos, Ch., Cyrek, A., et al. (2021). Association of wound genesis on varying aspects of health-related quality of life in patients with different types of chronic wounds: results of a cross-sectional multicentre study. Int. Wound J. 18 (4), 432–439. doi:10.1111/iwj.13543
Riches, S., Jeyarajaguru, P., Taylor, L., Fialho, C., Littles, J., Ahmed, L., et al. (2023). Virtual reality relaxation for people with mental health conditions: a systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 58 (7), 989–1007. doi:10.1007/s00127-022-02417-5
Riva, G. (2005). Virtual reality in psychotherapy: review. Cyberpsychol Behav. 8 (3), 220–230. doi:10.1089/cpb.2005.8.220
Savadkoohi, H., Barasteh, S., Ebadi, A., Ashrafizadeh, H., Amirdehi, M. A., Safdari, A., et al. (2023). Psychometric properties of Persian version of wound-QOL questionnaire among older adults suffering from chronic wounds. Front. Psychol. 26, 1041754. doi:10.3389/fpsyg.2022.1041754
Siani, A., and Marley, S. (2021). Impact of the recreational use of virtual reality on physical and mental wellbeing during the Covid-19 lockdown. Health Technol. 11 (2), 425–435. doi:10.1007/s12553-021-00528-8
Smith, K., Wang, Y., and Colloca, L. (2022). Impact of virtual reality technology on pain and anxiety in pediatric burn patients: a systematic review and meta-analysis. Front. Virtual Real 2:751735 2, 751735. doi:10.3389/frvir.2021.751735
Spyrka, K., Rojczyk, E., Brela, J., Sieroń, A., and Kucharzewski, M. (2024). Virtual reality as a promising method of pain relief in patients with venous leg ulcers. Int. Wound J. 21 (10), e70082. doi:10.1111/iwj.70082
Szewczyk, M., Mościcka, P., Jawień, A., Cwajda-Białasik, J., Czierzniakowska, K., Ślusarz, R., et al. (2015). Quality of life in patients with leg ulcers or skin lesions – a pilot study. Adv. Dermatology Allergology XXXII (6), 465–469. doi:10.5114/pdia.2014.40983
Szewczyk, M., Rogala, J., Cwajda-Białasik, J., Czierzniakowska, K., and Jawień, A. (2007). Psychological and social problems of patients with chronic venous disease. Adv. Dermatology Allergology 24, 207–210.
Szkiler, E., Kucharzewski, M., Krasowski, G., Bartoszewicz, B., Banasiewicz, T., Chrapusta, A., et al. (2024). Algorithms and guidelines for therapeutic management in non-healing wounds. Update 2024. Forum Leczenia Ran 5 (1), 1–34. doi:10.15374/FLR2024005
Vieira, C., and Araújo, T. (2018). Prevalence and factors associated with chronic wounds in older adults in primary care. Rev. Esc. Enferm. Usp. 52, 03415–03418. doi:10.1590/S1980-220X2017051303415
Vogt, T., Koller, F., Dias Santos, P., Lenhani, B., Guimaraes, P., and Kalinke, L. (2020). Quality of life assessment in chronic wound patients using the Wound-QoL and FLQA-Wk instruments. Invest Educ. Enferm. 38 (3), e11. doi:10.17533/udea.iee.v38n3e11
WHOQOL Group (1995). The World Health Organisation quality of life assessment (WHOQOL): position paper from the world health organisation. Soc. Sci. Med. 41, 1403–1409. doi:10.1016/0277-9536(95)00112-k
Wicke, C., Bachinger, A., Coerper, S., Beckert, S., Witte, M., and Königsrainer, A. (2009). Aging influences wound healing in patients with chronic lower extremity wounds treated in a specialized wound care center. Wound Repair Regen. 17, 25–33. doi:10.1111/j.1524-475X.2008.00438.x
Keywords: quality of life, leg ulcer, pain, virtual reality, non-pharmacological methods
Citation: Spyrka K, Rojczyk E, Sieroń A, Brela J, Borkow G and Kucharzewski M (2025) Positive impact of virtual reality during wound debridement on quality of life in patients with venous leg ulcers. Front. Virtual Real. 6:1617665. doi: 10.3389/frvir.2025.1617665
Received: 24 April 2025; Accepted: 26 June 2025;
Published: 08 July 2025.
Edited by:
Marcos Brioschi, University of São Paulo, BrazilReviewed by:
Wafaa Amer, Prince Sattam Bin Abdulaziz University, Saudi ArabiaÖmer Taşçı, Mus Alparslan University, Türkiye
Copyright © 2025 Spyrka, Rojczyk, Sieroń, Brela, Borkow and Kucharzewski. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Ewa Rojczyk, ZXdhcm9qY3p5a0BnbWFpbC5jb20=
 Kinga Spyrka
Kinga Spyrka Ewa Rojczyk
Ewa Rojczyk Aleksander Sieroń2
Aleksander Sieroń2