- 1Department of Applied Science and Technology, North Carolina Agricultural and Technical State University, Greensboro, NC, United States
- 2Department of Applied Engineering Technology, North Carolina Agricultural and Technical State University, Greensboro, NC, United States
Augmented reality, also known as AR, supplements reality by allowing the user to experience computer-generated graphics as though they appear in the real world. This literature review’s goal is to present a collection of data on AR-based exercise and rehabilitation applications. This literature review also aims to identify gaps within the existing research. The method of PRISMA was applied to systematic reviews for relevant articles published between 2017 and 2025. The databases include Academic Search Ultimate, British Library Serials, MEDLINE, and ProQuest Central. The results from the literature found that AR for rehabilitation could help patients physically and mentally and improve their motivation and engagement. Different types of AR tools were used to help with the rehabilitation of patients with health issues such as knee injuries or stroke. Questionnaires and medical tests were the common methods to gather data from the patients. AR rehabilitation technology may be able to bring a new form of human-computer interaction for patients.
1 Introduction
Augmented Reality (AR) is one of the interactive immersive technologies that have been studied and used in diverse fields, such as science (like chemistry), tourism and hospitality, gaming, digital media, healthcare, and education (Fombona-Pascual et al., 2022; Koulouris et al., 2022; Lin and Yang, 2024; Mirza et al., 2025; Nekar et al., 2022; Wei, 2019; Wu et al., 2025). AR has differences in the level of immersion and the way of interaction from other immersive technologies, such as Virtual Reality (VR) and Mixed Reality (MR). Virtual Reality refers to completely immersive technology that requires a device such as a headset to produce a virtual environment (Nekar et al., 2022). In contrast, Mixed Reality refers to immersing a person in a world that combines real and virtual world components (De Cecco et al., 2023). However, Augmented Reality refers to an interactive platform that has virtual objects superimposed into the real environment (Nekar et al., 2022). Specifically, AR supplements reality by allowing the user to experience computer-generated graphics as though they appear in the real world (Žilak et al., 2022).
Certain characteristics and features further define augmented reality. For instance, AR technology overlays the real world with simulated digital graphics using cameras or displays (Borresen et al., 2019; FDA, 2025). AR devices project the graphics onto specific locations and depths. These graphics can be three-dimensional (3D) objects (Fakolade et al., 2024; Fombona-Pascual et al., 2022). The types of displays and cameras used for AR can include a heads-up display (HUD), a smartphone, AR glasses, and a head-mounted display (Borresen et al., 2019; FDA, 2025; Fombona-Pascual et al., 2022; Koroleva et al., 2021). The digital graphics can typically be interacted with and manipulated by the person using the AR device Fakolade et al., 2024; FDA, 2025). For some individuals, using an AR device can lead to neck pain and discomfort when using a headset (Balloufaud et al., 2025; FDA, 2025).
Augmented reality has several applications when it comes to exercise and rehabilitation, including occupational or physical therapy. Occupational therapy (OT) refers to helping patients of all ages perform tasks that are significant to them (Perkins et al., 2024; Sievert, 2024). These tasks are usually referred to as “activities of daily living” (ADL) (Coninck et al., 2024). ADL can include tasks such as performing leisure activities, social participation, bathing, eating, work tasks, and dressing (Perkins et al., 2024; Sievert, 2024). During traditional OT, Patients may participate in cognitive rehabilitation, skill-based exercises, and sensory integration therapy (Sievert, 2024). Patients may also learn to use environmental modifications and adaptive equipment. Physical therapy (PT) refers to helping patients improve their strength, mobility, and physical function (Cavalcanti et al., 2019; Sievert, 2024). During traditional PT, patients may perform activities such as balance training, aquatic therapy, sensory integration, and therapeutic exercises to help restore and promote mobility and independence (Cavalcanti et al., 2019; Sievert, 2024). PT also helps with relieving pain and addressing a person’s impairment (Sievert, 2024; Xu et al., 2024). Physical therapy can assist patients in increasing their ability to perform “activities of daily living’ (ADLs); however, it does not primarily address specific ADLs, which is a focus area of OT (Sievert, 2024).
Regarding the studies of AR use in occupational and physical therapy, AR has been studied to see if it can significantly improve physical performance, upper limb performance balance, and muscle strength (Koulouris et al., 2022; Lee et al., 2018; Lee et al., 2017; Li et al., 2021; Yu et al., 2023). For example, by using AR-based Otago exercise, self-exercise, and yoga on 30 participants for 12 weeks during 60-min sessions, Lee et al. (2017) indicated that AR can be used to significantly help prevent falls in elderly people by assisting them with physical factors involving falls, muscle strength, and balance. The use of AR in physical therapy and therapeutics has been an important topic of discussion and research in the healthcare area (Borresen et al., 2019; Lee et al., 2018; Yu et al., 2023). In addition, augmented reality can be used along with conventional occupational therapy, which could lead to better improvements for post-stroke patients in their cognitive function and upper limb motor function than just using conventional occupational therapy alone (Li et al., 2021). These demonstrated an interest in AR technology among researchers concerning exercise, rehabilitation, and physical/occupational therapy.
There are also additional advantages to using AR-based rehabilitation/therapy rather than traditional methods. Traditional forms of rehabilitation/therapy can be repetitive and boring, which leads to patients’ abandonment of rehabilitation tasks (Li et al., 2021). Therapy has a better effect on those who participate more frequently, so if patients are losing interest and are not performing the task as instructed, then the healing process may be delayed (Li et al., 2021). Traditional forms of rehabilitation/therapy may also be inconvenient for some people (Li et al., 2021). Thus, AR has been proposed as a potential tool to address these challenges. For example, AR’s feedback, visual, and movement-tracking features can help patients (like stroke patients) be able to perform self-guided tasks at home and could increase enthusiasm through AR game play (Li et al., 2021; Vaida et al., 2024). AR’s user interface features can provide different game modes and can target more complex motions to provide an AR-based rehabilitation/therapy that is a fun and motivating experience by allowing users to participate in interactive AR games (Vaida et al., 2024). AR games that require patients, like those who face challenges with joint or leg movement, to move a certain body part to hit a superimposed visual/graphical target can help them stay motivated to continue therapy (Vaida et al., 2024). AR applications might include “Football,” where players’ movements are tracked, allowing them to simulate hitting a virtual ball, or “Color,” requiring patients to hit colored visually tracked targets with their foot (Vaida et al., 2024). Overall, these games can help keep patients engaged and motivated to continue therapy.
Furthermore, AR’s user interface features can provide customization and adaptability options to select treatment that matches the individual medical problems, and AR’s real-time feedback feature and visual position tracking can provide visual position guidance for the user (Cunha et al., 2023; De Cecco et al., 2023; Vaida et al., 2024). For example, these features of AR could help with “activities of daily living,” such as setting up a table, while providing feedback for the user (De Cecco et al., 2023). A therapist could have a patient set up a table by having them match the visually superimposed objects with the real objects on the table. The AR devices would help measure the angle and placement/position of objects to help identify a patient’s capabilities and progress (De Cecco et al., 2023). AR’s motion/movement tracking feature with a real-time feedback feature can also help track a person’s motions, which can help provide feedback so the patient can correct their movement (Vaida et al., 2024). Therefore, there are certain benefits to using AR technology versus traditional rehabilitation methods.
Moreover, augmented reality may be able to improve the recovery experience of those who have physical disabilities/mobility issues by offering additional, appealing ways to perform exercises. A majority of those with disabilities are optimistic and open to innovative technologies (Žilak et al., 2022). As a result, there is potential for augmented reality to bring new forms of human-computer interactions (Žilak et al., 2022). Researchers have explored using augmented reality to aid those with mobility issues due to old age, injury, and other health conditions (Lee et al., 2018; Lee et al., 2017). AR uses a platform where users/patients can interact with virtual objects that are superimposed in the real world, which allows users to perform a task to improve their health (Nekar et al., 2022). As mentioned before, different AR devices are implemented depending on someone’s circumstances. For example, somebody may need different equipment or recovery time depending on if they are suffering from knee issues, muscle strength issues, stroke, or balance issues (Kang et al., 2022; Lee et al., 2017; Lee et al., 2018; Yu et al., 2023). Several devices can be utilized to help people with rehabilitation and recovery exercises, such as Active 3D-glasses, AR mobile games, and AR headsets (Borresen et al., 2019; Li et al., 2021; Vaida et al., 2024). However, researchers do not focus on studying the same demographics or potential physical benefits of AR technology for physical exercise, physical/occupational therapy, and rehabilitation.
Finally, physical improvements are not the only aspect of AR technology that researchers are studying. Researchers also discuss the topic and study the effects that using AR technology has on a person’s experience (Cavalcanti et al., 2019; Koulouris et al., 2022; Lee et al., 2017; Yu et al., 2023). For instance, AR can help improve motivation for those using AR technology for rehabilitation and physical/occupational therapy (Cavalcanti et al., 2019; Koulouris et al., 2022). According to Koulouris et al. (2022), AR can also help promote physical activity. Moreover, according to Vaida et al. (2024) and Yu et al. (2023), AR can help people with engagement. Therefore, there is also a collective interest among researchers in how AR technology affects the motivation and engagement of people using AR during physical activity, such as exercising, physical therapy, and rehabilitation. This literature review aims to provide an overview of the current research data on AR technology applications in recovery exercise, physical therapy, and rehabilitation, and the impact of the use of AR on patients’ experience. The research questions in this study include:
• Research Question 1: What types of participants have been included in the AR studies related to rehabilitation and recovery?
• Research Question 2: What research methods have been applied in the AR studies related to rehabilitation?
• Research Question 3: What are the effects of using AR on the outcomes and experiences in rehabilitation and recovery exercise?
2 Methods
2.1 Initial search settings
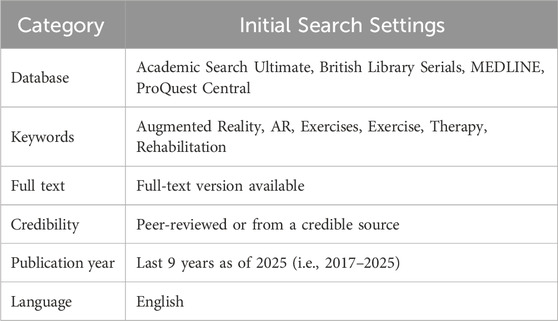
In constructing this literature review, several databases were used to find written work to analyze, including Academic Search Ultimate, British Library Serials, MEDLINE, and ProQuest Central. Each database provided written works that aided in the development of this literature review. Certain key elements were used to help narrow down the search results. For instance, search inputs such as Boolean/phrases were utilized. In addition, limiters such as (1) the written work needing a full-text version, (2) being peer-reviewed/credible, and (3) having a publication date within the last 9 years were used to narrow down the search even further. Based on the results of the search, several articles were chosen to review and determine if they would be appropriate for this paper. The reasons for choosing these factors are discussed next.
The first factor was Boolean/phrases. Written works were first filtered by Boolean/phrases that were searched in the databases. The keywords that were searched were a combination of words such as “augmented,” “reality,” “AR,” “exercise,” “therapy,” and “rehabilitation.” These words were chosen to help ensure that the literature review stayed on topic. Some of these words appeared within the keyword section of a written work, while some of these words appeared throughout the text. The second factor used in narrowing down the search required that potential written works have a full-text version. This was to ensure that the written work could be reviewed in its entirety so that all the information could be obtained. Without a full-text version of the written work, information may be unclear and therefore, could not provide the context needed for this literature review. This can be seen in the table below (see Table 1).
The time of publication was the third factor in selecting a written work for review. To make sure that the literature review was up-to-date, only written work within the last 9 years as of writing this paper (year 2025) was used. Relevance is important, especially when it comes to technological information. Outdated information could harm the impact of this literature review. This time frame will help keep the information relevant. The final factor used to select the writings for this literature review was whether the written work itself was peer-reviewed or from a credible source. Either the source of the written work had to be peer-reviewed, or it had to be from a credible source to be considered for the literature review. This criterion was chosen to make sure that the works selected were of high quality. The quality of the work is important to ensure that the literature review contains accurate information. This can be seen in the table below (see Table 1).
2.2 Inclusion criteria
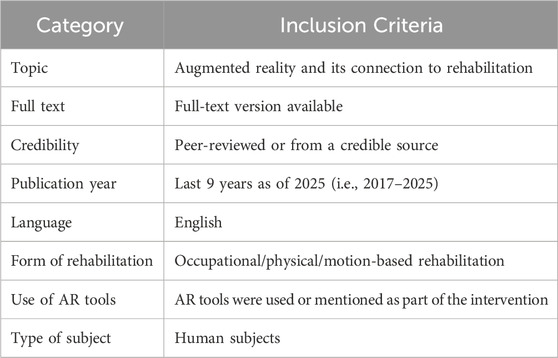
The databases provided many written works that could be used for this literature review based on the initial search settings. Each article was briefly inspected, and the ones initially selected for potential use in this paper were based on eight categories and their criteria. The first category was the topic. For an article to be chosen for use in the literature review, the criteria were that the articles had to be about augmented reality and its connection to rehabilitation. The second category was “full text.” The criteria required that articles have a full-text version. The third category concerns the article’s credibility. Thus, the written work criteria required that sources be peer-reviewed or credible, ensuring the use of high-quality work for this paper. The fourth category was publication year. As noted previously, to ensure that the written works chosen for this literature review were up to date, the criterion was that written works were selected within the last 9 years to keep information relevant. The fifth category was the paper’s written language. The criteria were that articles needed to be in English since the primary researcher’s native language was English. This would make comprehending the paper easier. Additional criteria were also used to help focus the literature review. This can be seen in the table below (see Table 2).
The sixth category was the rehabilitation method used. The criteria were that the articles selected mentioned some form of physical, occupational, or motion-based rehabilitation. The seventh category was the use of AR tools. The criteria were that articles had to use an AR tool or be mentioned as part of the intervention in the experiments. The eighth category was the type of subject. The criteria were that articles had to utilize human subjects. These criteria help give the literature review a better focus. As a result of using these eight categories and criteria, written works were chosen to be potentially used in this literature review that matched a certain topic and provided some of the most relevant information. This can be seen in the table below (see Table 2).
2.3 Exclusion criteria
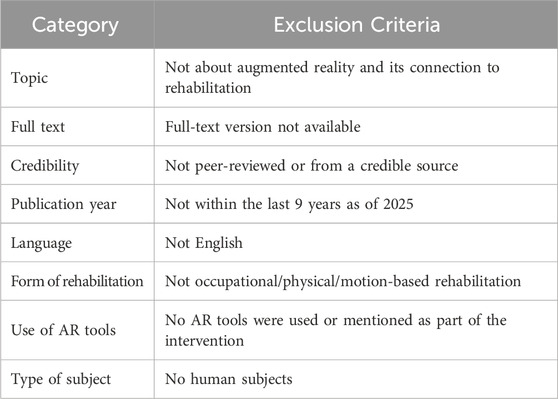
When determining which articles to potentially use in this literature review, articles were excluded if they did not meet the inclusion criteria. The following were the exclusion criteria. First, augmented reality and its connection to rehabilitation were not mentioned in the article. Second, the full-text version of the article was not available. Third, the article was not peer-reviewed or from a credible source. Fourth, the article was not published from 2017 to 2025. Fifth, the article was not in English. Sixth, physical occupational, or motion-based forms of rehabilitation were not implemented. Seventh, AR tools were not utilized or mentioned as part of the intervention. Eighth, human subjects were not used during the intervention. The exclusion criteria can be seen in the table below (see Table 3).
2.4 Systematic search
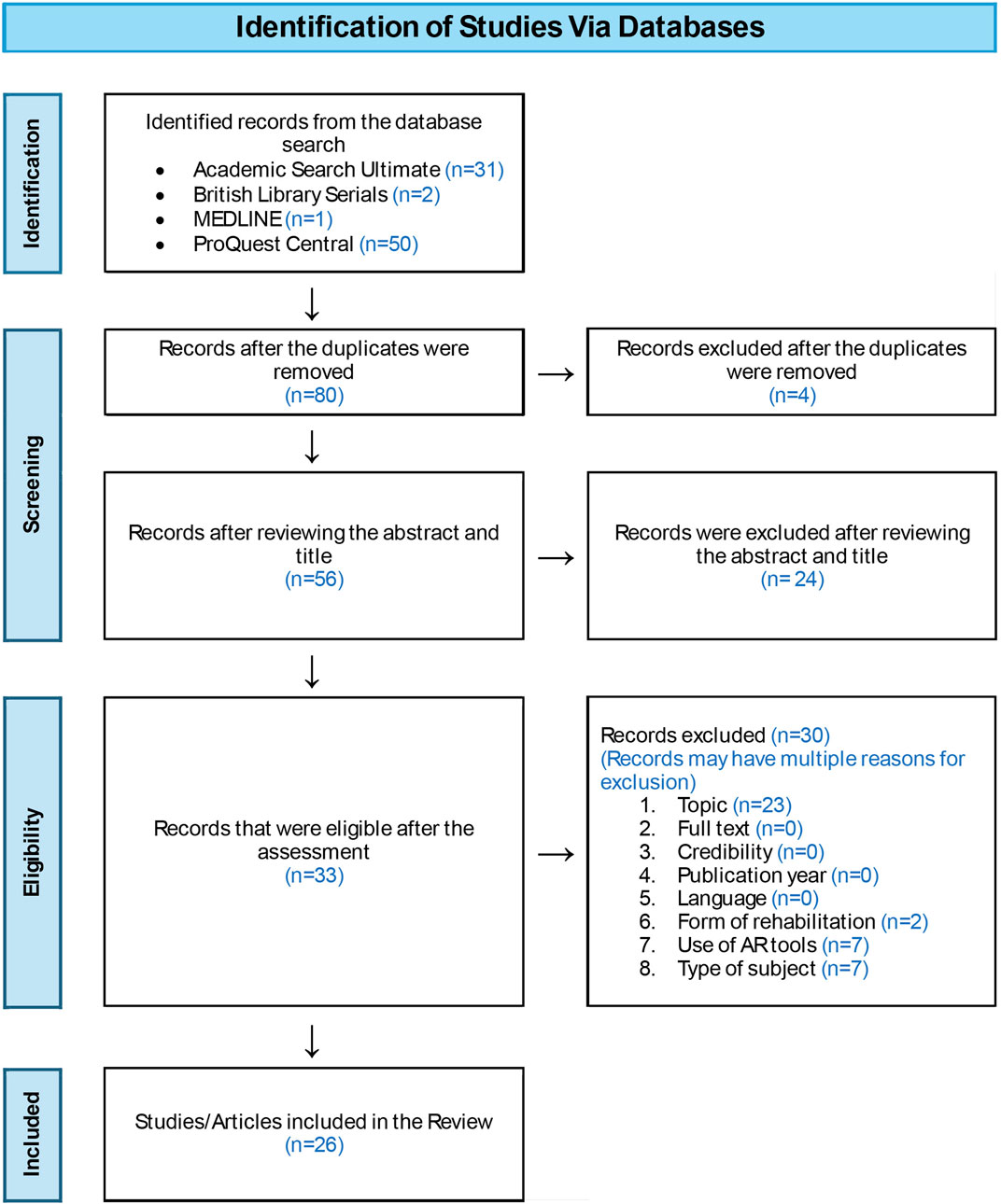
A systematic search was important to conduct when writing this literature review on AR for rehabilitation. It helped to narrow down the results within the database and find articles to use in this literature review. It also helped in finding some higher-quality written works. In this case, a method of PRISMA (Page et al., 2021) was used for this literature review to help provide a clear data-searching systematic process. The PRISMA is displayed in the figure below (see Figure 1).
3 Results
While reviewing the written works chosen for this literature review, a structure was set up for organizing the information gathered from the studies. This structure also aided in the comparison of the written works. Each study was broken down into the aspects of demographics, methodology, and findings.
3.1 Gender, health conditions, and age
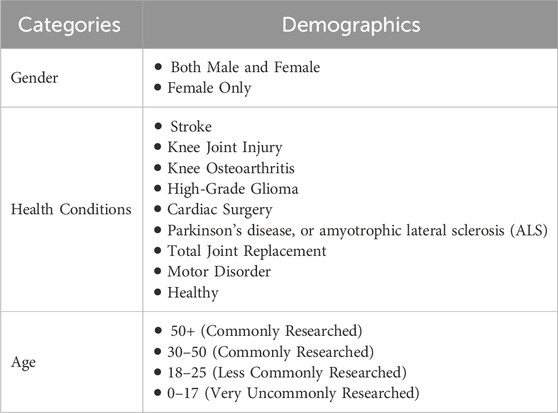
Knowing the demographic of the study is important for identifying who the focus was on. This information can be used to understand Research Question 1 (i.e., What types of participants have been included in the AR studies related to rehabilitation and recovery?). The topics for the demographics chosen for this literature review were age, health conditions, and gender of participants. One study reported the age range for the participants to be 20–60 years old (Koulouris et al., 2022). One reported the age range for the study to be 68.39 ± 4.24 to 69.54 ± 3.12 years old (Yu et al., 2023). There were three males and 21 females utilized (Yu et al., 2023). Lee et al. (2017) reported the age range for their study to be 72.60 ± 2.67 years, with only females being used. It was also reported that the age range for a different study was 18–43 (average age of 21.95; SD = 4.72), and only 29 males and 16 females were used (Cavalcanti et al., 2019). Health-wise, a combination of healthy adults and adults who experienced a health condition was utilized (Borresen et al., 2019; Cavalcanti et al., 2019; Lee et al., 2018; Lee et al., 2017; Yu et al., 2023).
Furthermore, the demographic for one study included a total of 46 male participants and 10 female participants, with an average age of 30–35 years old (Ji et al., 2024). The demographic for another study was Elderly patients who may have had a stroke, Parkinson’s disease, or amyotrophic lateral sclerosis (ALS) (Vaida et al., 2024). Xu et al. (2024) reported that their demographic was 60 participants with knee osteoarthritis (OA) aged 40–85 years old. One demographic was 10 healthy participants who ranged between the ages of 23–55 years old (Rizzi et al., 2023). 60 people who were in the cardiac surgery intensive care unit at a hospital in Mashhad were used in another study (Moghaddam et al., 2023). One study used patients who had Total Knee Arthroplasty and were 50 years or older (Shim et al., 2023). Another study used participants who would be having an isolated meniscus repair (Wang et al., 2023).
Moreover, the demographic for one study was 15 patients, including 10 male patients who were between 20 and 70 years old with knee osteoarthritis of Kellgren-Lawrence grades I to III (Baptiste et al., 2023). 19 patients with balance disorders were reported during one experiment (Tsakanikas et al., 2022). 27 people who had developmental disability were reported during a different experiment (Kang et al., 2022). The demographic for one study was a total of 24 patients with autism spectrum disorder between the ages of 6–18 (Nekar et al., 2022). Guinet et al. (2022) reported their demographic to be 14 children between the ages of 10–18 with cerebral palsy, with a seven-week minimum between the surgery and the intervention utilized (Guinet et al., 2022). Timmermans et al. (2021) reported utilizing 40 people who had a stroke less than or equal to 3 months prior (Timmermans et al., 2021).
In addition, a demographic of 42 older adults with total joint replacement (TJR) was used for a different study (Fakolade et al., 2024). Pieczyńska et al. (2023) reported using 27 people who had high-grade glioma (HGG) and who were to undergo radiotherapy after tumor resection (Pieczyńska et al., 2023). Yang et al. (2022) used 39 Chronic stroke participants in their study (Yang et al., 2022). Li (2022) utilized 40 patients who had undergone knee joint injury surgery (Li, 2022). Healthy users, patients, and clinical experts (occupational therapists) were the demographic for one of the experiments, too (De Cecco et al., 2023). Stroke patients were the demographic in another study as well (Koroleva et al., 2021). 30 post-stroke participants were also used (Li et al., 2021).
Therefore, it was noted that few studies focused primarily on young adults or children, but more focused primarily on older adults or the elderly. In addition, when gender was mentioned, the groups were not usually close to being even. Sometimes, healthcare professionals were also included in the study, and not just the patient. This was likely to get the healthcare professionals’ view on AR technology as well. Both healthy individuals and those needing rehabilitation due to a health condition were also included. Moreover, many of the studies focused on people who had knee injuries, stroke, or a motor disorder. This shows there are differences in the demographics chosen for the studies. Examples of the demographics are summarized in the table below (see Table 4).
3.2 Adopted devices, instruments, and application ways
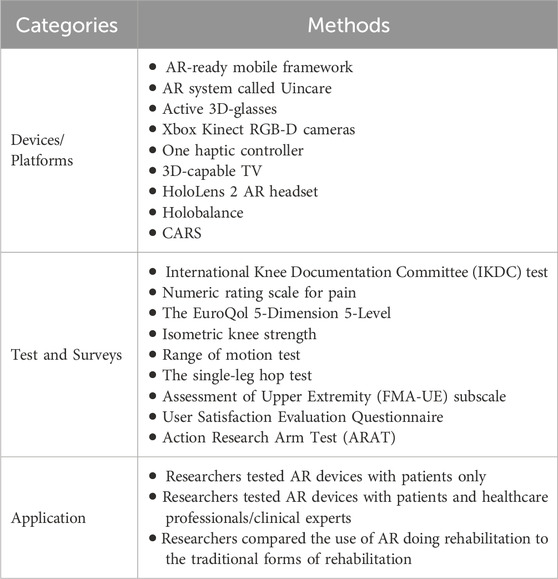
Several aspects of the research methodology can affect the study. This includes the devices and materials used, the purpose of the study/the testing focus, the way the study is conducted, and the method by which data is gathered. This information can be used to explain Research Question 2 (i.e., What research methods have been applied in the AR studies related to rehabilitation?). For example, to determine the benefits of AR technology and/or whether it helped in the improvement of physical health, different types of devices were used to test a person physically. A study conducted by Koulouris et al. (2022) used a prototype that consisted of an AR-ready mobile framework that included an application for IoT wearables (tracks user biosignals and activity). It also included a cloud platform with a web application endpoint (which allows healthcare professionals to be able to analyze results and configure games remotely) (Koulouris et al., 2022).
Another study referred to using an AR system called Uincare (Lee et al., 2018). Unicare is composed of a task-specific game-based system (Lee et al., 2018). One experiment involved the use of an AR rehabilitation tool called ARkanoidAR (Cavalcanti et al., 2019). It uses a Kinect sensor to track human body movement (Cavalcanti et al., 2019). There was another study that involved the use of an AR telerehabilitation System with Haptics (ARTESH), Active 3D-glasses, Xbox Kinect RGB-D cameras, one haptic controller, and a 3D-capable TV (Borresen et al., 2019). A different study used AR rehabilitation that utilized specially designed software for motor rehabilitation, along with biofeedback training and motion sensors (Koroleva et al., 2021). Another study consisted of using two groups, which included one that received conventional rehabilitation and the other group that received digital healthcare rehabilitation (Shim et al., 2023). The intervention lasted for 12 weeks (Shim et al., 2023). The digital healthcare rehabilitation consisted of an AR-based digital healthcare system (UINCARE Home +). This included a computer, a 3D-depth camera (Xbox One Kinect), and a display such as a monitor or TV (Shim et al., 2023). Despite studies using different devices, they were still able to achieve a similar objective of determining whether the device affected a person physically.
To understand the performance of training and exercises, the function of different parts of the body, such as legs, hands, and knees, was evaluated. This occurred by implementing AR to aid in physical exercise, physical/occupational therapy, and rehabilitation. One of the studies focused on heart rate, a participant’s aim, the severity of trembling hands, and the number of steps (Koulouris et al., 2022). A different study focused on knee flexion, knee extension, range of motion, and muscle strength (pre- and post-surgery) (Yu et al., 2023). Strengthening, balance training, knee flexion, and ankle dorsiflexion strength were the focus of one experiment (Lee et al., 2017). Testing the balance of stroke patients was also conducted (Lee et al., 2018). In addition, testing motor rehabilitation and the ability to perform certain physical tasks correctly was conducted during another experiment (Cavalcanti et al., 2019). A physical examination of patients with upper extremity complaints was conducted, too (Borresen et al., 2019). It was noticed that balance and strengthening training, as well as knee flexion, were tested among multiple studies.
Furthermore, during a study, 30 people were randomly assigned to an AR group, a yoga group, and a self-exercise group. AR balance training, strengthening, and yoga were practiced three times a week for 12 weeks during 60-min sessions (Lee et al., 2017). Other studies use different methods of gathering data. For example, Ji et al. (2024) mentioned using one group of patients to use the AR-based telecommunication system to help them with their rehabilitation, while another group used a brochure-based rehabilitation program with the self-log to help with their rehabilitation (Ji et al., 2024). The tests used to evaluate improvement were the International Knee Documentation Committee (IKDC) test for the primary outcome and the secondary outcomes test using a numeric rating scale for pain, the EuroQol 5-Dimension 5-Level measurement system, isometric knee strength test, range of motion test, and the single-leg hop test (Ji et al., 2024). In another study, a combination of serious gaming and augmented reality (AR) with the LegUp parallel robot was used (Vaida et al., 2024). This was to help bedridden patients go through rehabilitation of the hip, knee, and ankle while using the parallel robot called LegUp, with the HoloLens 2 AR headset (Vaida et al., 2024).
In another study, a single-blind randomized controlled trial was used in which 30 people were assigned to the treatment group and the other thirty were assigned to the control group (Xu et al., 2024). For the treatment group, they used a combination of augmented reality and computer vision technology to help patients with sports rehabilitation training (Xu et al., 2024). The exercises were conducted using a phone that had a camera, which increases its widespread use (Xu et al., 2024). The test used to evaluate the patient was the Western Ontario and McMaster University Osteoarthritis Index (WOMAC) (Xu et al., 2024). In one study, AR devices were designed to help patients with passive mobilization (in theory) during hospitalization (Rizzi et al., 2023). This is important because some patients do not receive this treatment due to the limited availability of hospital workers, so this technology could allow them to perform the exercises on their own (Rizzi et al., 2023). 10 healthy participants, who use the AR device, ranked their experience based on expertise, workload, design, satisfaction, usability, and instruction (Rizzi et al., 2023). In addition, another study used augmented reality to evaluate 60 people in a treatment group who were in the cardiac surgery intensive care unit (Moghaddam et al., 2023). These participants were to perform physical exercises to help with physical cardiac rehabilitation (Moghaddam et al., 2023). In a different study, one group of participants was assigned to use the digital rehabilitation program, which involved using augmented reality and computer vision technology (Wang et al., 2023). The control group received in-clinic physical therapy sessions weekly (Wang et al., 2023).
Moreover, one study used dual test exercise-based augmented reality to help those with flexibility, endurance, muscle strength, and balance ability (Kang et al., 2022). This intervention lasted 8 weeks (Kang et al., 2022). During a different experiment, one of the groups used AR-based cognitive motor games while the other group received conventional cognitive training (Nekar et al., 2022). The group that received the AR-based game was the treatment group, while the one that did not was the control group (Nekar et al., 2022). Each group participated in a four-week program with training sessions lasting 30 min twice a week (Nekar et al., 2022). Guinet et al. (2022) reported about one group of participants who received an augmented reality rehabilitation of cerebral palsy AVG program, while the control group received rehabilitation training on a treadmill (Guinet et al., 2022). This was a randomized controlled clinical trial (Guinet et al., 2022). A walking test, a muscle power sprint test, and satisfactory tests were conducted (Guinet et al., 2022).
Furthermore, during one experiment, six focus groups and 11 semi-structured interviews were conducted to get a better understanding of users’ feelings on how to design a 3D augmented reality-based rehabilitation system (Fakolade et al., 2024). In an article by Pieczyńska et al. (2023), participants were split into the experimental group and the control group. The experimental group received an augmented reality-based rehabilitation exercise to help with physical fitness, while the control group received the usual care (Pieczyńska et al., 2023). Tests such as the 6-min walk test and grip tests were conducted to evaluate performance (Pieczyńska et al., 2023). Augmented reality rehabilitation systems were also integrated into patient care during COVID-19 (Yang et al., 2022). Li (2022) mentioned that during their experiment, one group was assigned to use AR-based rehabilitation methods while the other group used traditional rehabilitation methods (Li, 2022). Each group was tested on functional recovery, swelling, structural recovery, pain value, the ability to return to work, x-rays, and weight-bearing (Li, 2022).
In a study by De Cecco et al. (2023), patients and the clinical expert were both given AR devices to use so that the clinical expert could interact with the patient during the AR rehabilitation process, regarding OT. The goal was to see the effects on both the patient and the clinical expert when using the AR rehabilitation system together (De Cecco et al., 2023). One study used a randomized controlled trial to get a better understanding of how an augmented reality cell phone game called CARS helps stroke survivors with rehabilitation training, including OT (Li et al., 2021). The treatment group received 30 min of rehabilitation using augmented reality and 30 min using conventional occupational therapy (Li et al., 2021). The control group that participated received 1 h of occupational therapy (Li et al., 2021). Different methods of evaluating the patient’s performance and feelings were used, such as a Fugl-Meyer Assessment of Upper Extremity (FMA-UE) subscale, a User Satisfaction Evaluation Questionnaire, and an Action Research Arm Test (ARAT) (Li et al., 2021).
Moreover, an augmented reality device was used to display targeted footprints on the floor to help compare the difference between normal and reduced stride length in patients (Baptiste et al., 2023). Holobalance, which is a rehabilitation program that includes augmented reality, was assigned to patients to help with balance disorders, so that researchers could test the accuracy of the device (Tsakanikas et al., 2022). In another study, one of the groups received an augmented reality-based program for walking, while the other group participated in the FALLS program using physical content (Timmermans et al., 2021). This was to help patients with their walking after a stroke, as well as evaluate how the different approaches affect patients’ rehabilitation process (Timmermans et al., 2021).
Overall, this indicates that there are different methods of understanding the effects of AR regarding rehabilitation. Some studies focused strictly on testing and evaluating the effects of the AR software itself, while other studies compared the use of AR technology to traditional means of rehabilitation. Many studies offer questionnaires as well as different medical evaluation tests to get a better understanding of the user and their performance. There were also different parts of the body and functions that the researchers focused on. Some researchers focused more on the legs, knees, and/or hands, while others focused on walking abilities or balance. This shows there are both similarities and differences between how researchers went about studying AR technology regarding rehabilitation. Examples of the methods are summarized in the table below (see Table 5).
3.3 The effects of using AR on the patients’ experience during rehabilitation
There are similarities and differences between the results in each of the studies. This information can be used to answer Research Question 3 (i.e., What are the effects of using AR on the outcomes and experiences in rehabilitation and recovery exercise?). As a part of the discussion, some of the studies mentioned that there was an improvement in people’s emotional state while using AR technology (Cavalcanti et al., 2019; Koulouris et al., 2022; Lee et al., 2017; Yu et al., 2023). Koulouris et al. (2022) specifically mentioned how AR can promote physical activity. Regarding motivation, most of them indicated an improvement in motivation while using AR technology for rehabilitation and physical/occupational therapy (Cavalcanti et al., 2019; Koulouris et al., 2022; Lee et al., 2018; Lee et al., 2017; Yu et al., 2023). It was also mentioned that AR may help patients with engagement during their rehabilitation (Vaida et al., 2024; Yu et al., 2023). This showed that this is a common topic of discussion.
Regarding physical improvement, most of them indicated an improvement in physical capabilities using AR technology, with some studies indicating that AR technology showed better improvement than traditional exercise, rehabilitation, and physical/occupational therapy (Cavalcanti et al., 2019; Koulouris et al., 2022; Lee et al., 2018; Lee et al., 2017; Li, 2022; Yu et al., 2023). However, in some studies, there was no significant difference in the rehabilitation improvement between the group that used AR and the group that did not (Ji et al., 2024; Timmermans et al., 2021). For example, there was no significant difference between the scores of the participants who used the AR-based program and those who used a FALLS program (non-AR application/traditional means of rehabilitation) (Timmermans et al., 2021). Reaction time and executive function were also significantly improved for those who used the AR-based game than for those in the control group (Nekar et al., 2022). Augmented reality-based rehabilitation was also able to help patients with functional outcomes (Shim et al., 2023). It was noted that it may even be an alternative to conventional forms of rehabilitation (Shim et al., 2023).
In addition, the results of one study indicated that those who received the AR intervention showed better cardiovascular management self-efficacy during patient time in the intensive care unit, from the time of discharge (Moghaddam et al., 2023). Moreover, it was reported that using shorter stride lengths with AR technology did help patients with knee problems (Baptiste et al., 2023). The results of another study indicated that Holobalance, along with machine learning, was able to increase accuracy in scoring patients’ rehabilitation exercises (Tsakanikas et al., 2022). There was a statistically significant improvement in flexibility, muscle endurance, balance ability, and muscle strength for those who participated in using AR devices to help with passive mobilization (Kang et al., 2022). Lee et al. (2018) also mention how AR can improve balance for users with a stroke. In addition, there was overall satisfaction while using AR for passive mobilization exercises (Rizzi et al., 2023). Some results indicate that AR applications could also help with motor recovery (Koroleva et al., 2021).
Furthermore, there are several benefits to using AR for occupational therapy. Results indicated that using augmented reality along with conventional occupational therapy, delivered by an occupational therapist, led to better improvements for post-stroke patients in their upper limb motor function than just using conventional occupational therapy alone (Li et al., 2021). AR also provides a low-cost and user-friendly system that can be used at home for an occupational therapist’s patient (Li et al., 2021). Moreover, AR can help occupational therapists evaluate patients’ performances regarding ADL (Activities of Daily Living), like setting up a table (De Cecco et al., 2023). This is accomplished by having the occupational therapist and patient use a “shared AR” environment in which the occupational therapist can contextualize and have natural interaction with real-time data based on the patient’s performance (De Cecco et al., 2023).
AR can also help with pain during rehabilitation through digital healthcare (Shim et al., 2023). The results of another study indicated that those with HGG could use augmented reality-based exercises to help prevent muscle strength and attention loss during radiation therapy (Pieczyńska et al., 2023). A different experiment indicated that AR was effective, helped fulfill training goals for patients, and reduced the need for human professionals (Yang et al., 2022). However, it was also found that when a clinical expert uses AR alongside the patient, this helps the clinical expert be more involved with the patient’s recovery (De Cecco et al., 2023). In addition, the remote clinician was neutral when asked if remote or in-person evaluation would lead to similar results (Borresen et al., 2019).
Regarding the usability and design of AR devices, an article by Borresen et al. (2019) mentioned that AR systems were easy to learn and utilize. Furthermore, the results of a different study indicated that patients are looking for options such as a cost-effective device that includes virtual avatars and voice activation as features of the augmented reality system (Fakolade et al., 2024). Other people did not prefer avatars or vocal control (Fakolade et al., 2024). Some preferred remote control (Fakolade et al., 2024). However, some articles were not able to provide information on users’ preferences or the effects of using AR on the Patients’ Experience during Rehabilitation at the time of the experiment (Guinet et al., 2022; Wang et al., 2023; Xu et al., 2024).
Overall, this indicates that different studies were able to find different results regarding the relationship between AR and rehabilitation. Some studies focused on how AR affected a person physically, while others focused on how it affected the patient both physically and mentally. These results elaborated on how to improve AR technology and how participants felt about it in general. Some of the results were based on healthy participants, while others were based on participants who had a health condition. Other studies even obtained results from healthcare professionals to get their opinions on AR technology for rehabilitation. These studies had different ways of approaching the topic of AR and rehabilitation. Therefore, there were a variety of results that discussed different aspects of the topic. This information is summarized in the table below (see Table 6).
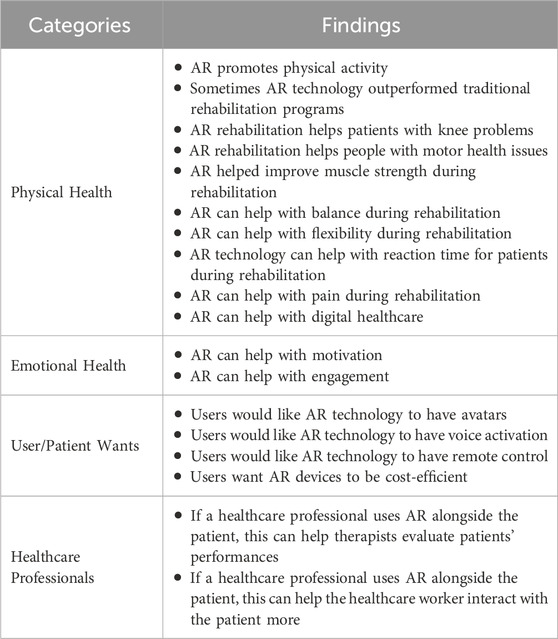
Table 6. Findings about the effects of using AR on the outcomes and experiences during rehabilitation.
4 Discussion and conclusion
Augmented Reality is known for supplementing reality using computer-generated graphics and allowing the user to experience them as though they appear in the real world (Žilak et al., 2022). There are a lot of benefits to using AR technology for physical health procedures. Written works chosen for this literature review were based on their relevance to the topic of AR technology for physical health, time of publication, and whether the database or source was peer-reviewed and/or credible. The studies showed different AR technologies, demographics, methodologies, testing focuses, and ways of collecting research. The research indicated that several people have done studies on the topic of how AR technology can affect a person’s physical health situation and rehabilitation progress. Some researchers have also conducted experiments on how AR technology can increase people’s motivation and affect their opinion on AR when participating in rehabilitation and physical health procedures. Therefore, AR technology has the potential to bring new forms of human-computer interactions (Žilak et al., 2022).
Moreover, the study also found that AR applications can help people with their motor recovery (Koroleva et al., 2021). These findings align with an article that indicated that AR telerehabilitation can help patients with motor rehabilitation (Kolsanov et al., 2020; Naqvi et al., 2024). In addition, augmented reality can improve mobility for post-stroke patients (Li et al., 2021). These findings align with an article by Gorman et al. (2022), which indicated that stroke patients were cautious yet open to the idea of using augmented reality for stroke rehabilitation during a focus group. Moreover, during the focus group, the themes that were discussed were that everything was computerized lately, and that possibilities were endless (Gorman et al., 2022). Lee et al. (2018) also expressed that AR can improve balance for users with a stroke. These findings align with an article that indicated that AR technology can help improve people’s balance levels during rehabilitation (Guo et al., 2024). Also, if AR set-ups are used alongside the patient, this can help medical professionals get more involved with the patient’s recovery (De Cecco et al., 2023). These findings align with an article by Cunha et al. (2023) that indicated that when a clinical expert uses AR alongside the patient, this helps the clinical expert be more involved with the patient’s recovery. AR can also help with a patient’s pain during rehabilitation through the use of digital healthcare (Shim et al., 2023). These findings align with an article by Guo et al. (2024) that indicated AR can help with pain during rehabilitation through digital healthcare.
Still, there are several gaps in the research that could be addressed in the future, such as studies that clearly specify that the experiments are about occupational therapy/occupational therapists. Although several papers mention OT in the report, they do not specify that the study is mainly about OT. As of now, there is a greater focus on PT, or the studies will address OT elements without specifically naming OT as one of the main focuses. There is also a lack of focus on those 25 years old and younger, and what people are looking for in an AR recovery application. Specifically, several of the written works found for this literature review focused on people 30 years and older. As a result, there is not a lot of data focused on people between 0 and 25 years old. It was also noted that a lot of the research focused on healthy people or those who experience injury, but the studies do not specify whether the participant was born with a certain health condition. In addition, it was also discovered that most of the research discussed motivation and emotions, but it is not the focus. Also, there is little information on what people are looking for in an AR recovery app, and whether their ideas/suggestions for the app will affect their motivation. Thus, it would be suggested that future AR research could consider including younger individuals, such as those aged 25 and under or who were born with or developed neuromuscular disabilities, and investigate the impact of using AR in rehabilitation or recovery exercise on their experiences (e.g., improvement, motivation, enjoyment, and engagement). Additionally, exploring and understanding what features or functions the patients are looking for when engaging with AR-based tools could help design more effective and personalized rehabilitation tools.
Data availability statement
The original contributions presented in the study are included in the article/supplementary material, further inquiries can be directed to the corresponding authors.
Author contributions
DM: Investigation, Writing – original draft, Conceptualization, Visualization, Data curation, Methodology, Formal Analysis. Y-TK: Conceptualization, Writing – review and editing, Supervision, Resources, Validation, Methodology.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The author(s) declare that no Generative AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Balloufaud, M., Boujut, A., Romain, M., Guinaldo, A., Fourcade, L., Hamonet-Torny, J., et al. (2025). Augmented reality exergames for upcoming cognitive-motor rehabilitation: user-centered design approach and user experience of healthy children. JMIR Rehabilitation Assistive Technol. 12, e69205. doi:10.2196/69205
Baptiste, U., Pereira, L. C., Jolles, B. M., and Favre, J. (2023). Walking with shorter stride length could improve knee kinetics of patients with medial knee osteoarthritis. J. Biomechanics 147, 111449. doi:10.1016/j.jbiomech.2023.111449
Borresen, A., Wolfe, C., Lin, C.-K., Tian, Y., Raghuraman, S., Nahrstedt, K., et al. (2019). Usability of an immersive augmented reality based Telerehabilitation system with haptics (artesh) for synchronous remote musculoskeletal examination. Int. J. Telerehabilitation 11, 23–32. doi:10.5195/ijt.2019.6275
Cavalcanti, V. C., Ferreira, M. I. D. S., Teichrieb, V., Barioni, R. R., Correia, W. F. M., and Da Gama, A. E. F. (2019). Usability and effects of text, image and audio feedback on exercise correction during augmented reality based motor rehabilitation. Comput. and Graph. 85, 100–110. doi:10.1016/j.cag.2019.10.001
Coninck, L. D., Declercq, A., Bouckaert, L., Döpp, C., Graff, M. J. L., and Aertgeerts, B. (2024). Promoting meaningful activities by occupational therapy in elderly care in Belgium: the ProMOTE intervention. BMC Geriatr. 24, 1–15. doi:10.1186/s12877-024-04797-6
Cunha, B., Ferreira, R., and Sousa, A. S. P. (2023). Home-based rehabilitation of the shoulder using auxiliary systems and artificial intelligence: an overview. Sensors 23 (16), 7100. doi:10.3390/s23167100
De Cecco, M., Luchetti, A., Butaslac III, I., Pilla, F., Guandalini, G. M. A., Bonavita, J., et al. (2023). Sharing augmented reality between a patient and a clinician for assessment and rehabilitation in daily living activities. Information 14 (4), 204. doi:10.3390/info14040204
Fakolade, A., Salvia, A. C., Phadke, S., and Kunz, M. (2024). An interactive vision-based 3D augmented reality system for in-home physical rehabilitation: a qualitative inquiry to inform system development. Health expectations Int. J. public participation health care health policy 27 (5), e70020. doi:10.1111/hex.70020
FDA (2025). Augmented reality and virtual reality in medical devices. Washington, DC: U.S. Food and Drug Administration. Available online at: https://www.fda.gov/medical-devices/digital-health-center-excellence/augmented-reality-and-virtual-reality-medical-devices#what-is.
Fombona-Pascual, A., Fombona, J., and Vicente, R. (2022). Augmented reality, a review of a way to represent and manipulate 3D chemical structures. J. Chem. Inf. Model. 62 (8), 1863–1872. doi:10.1021/acs.jcim.1c01255
Gorman, C., Gustafsson, L., and Gomura, C. (2022). The perspectives of stroke survivors and health professionals on the use of augmented reality for inpatient stroke rehabilitation: an anticipatory exploration. Brain Impair. 23 (2), 206–215. doi:10.1017/brimp.2021.11
Guinet, A., Bams, M., Payan-Terral, S., Khouri, N., Otmane, S., Bouyer, G., et al. (2022). Effect of an augmented reality active video game for gait training in children with cerebral palsy following single-event multilevel surgery: protocol for a randomised controlled trial. BMJ Open 12 (10), e061580. doi:10.1136/bmjopen-2022-061580
Guo, L., Li, S., Xie, S., Bian, L., and Shaharudin, S. (2024). The impact of digital healthcare systems on pain and body function in patients with knee joint pain: a systematic review and meta-analysis. Sci. Rep. 14 (1), 3310–3318. doi:10.1038/s41598-024-53853-z
Ji, Y. L., Yu, H. J., Kim, S. H., Lee, J. I., Jae-Young, L., Wang, J. H., et al. (2024). Effectiveness of in-home, augmented reality–based telerehabilitation after anterior cruciate ligament reconstruction: a randomized controlled trial. Orthop. J. Sports Med. 12 (10), 23259671241271729. doi:10.1177/23259671241271729
Kang, H. Y., Lee, D. Y., Hong, J. H., Kim, J. S., Kim, S. G., Seo, Y. G., et al. (2022). Effects of augmented reality-based dual-task program on physical ability by cognitive stage with developmental disabilities. Healthc. Basel, Switz. 10 (10), 2067. doi:10.3390/healthcare10102067
Kolsanov, A., Chaplygin, S., Rovnov, S., and Ivaschenko, A. (2020). Augmented reality application for hand motor skills rehabilitation. Int. J. Adv. Comput. Sci. Appl. 11 (4). doi:10.14569/IJACSA.2020.0110408
Koroleva, E. S., Kazakov, S. D., Tolmachev, I. V., Loonen, A. J. M., Ivanova, S. A., and Alifirova, V. M. (2021). Clinical evaluation of different treatment strategies for motor recovery in poststroke rehabilitation during the first 90 days. J. Clin. Med. 10 (16), 3718. doi:10.3390/jcm10163718
Koulouris, D., Menychtas, A., and Maglogiannis, I. (2022). An IoT-enabled platform for the assessment of physical and mental activities utilizing augmented reality exergaming. Sensors 22 (9), 3181. doi:10.3390/s22093181
Lee, J., Yoo, H.-N., and Lee, B.-H. (2017). Effects of augmented reality-based Otago exercise on balance, gait, and physical factors in elderly women to prevent falls: a randomized controlled trial. J. Phys. Ther. Sci. 29 (9), 1586–1589. doi:10.1589/jpts.29.1586
Lee, H. S., Chang, W. H., Lee, J. Y., and Hwang, J. H. (2018). Therapeutic potential of the home-based exercise program with the augmented reality system on balance in stroke patients: a preliminary report. Ann. Phys. Rehabilitation Med. 61, e36. doi:10.1016/j.rehab.2018.05.079
Li, L. (2022). Effect of remote control augmented reality multimedia technology for postoperative rehabilitation of knee joint injury. Comput. and Math. Methods Med. 9320063. doi:10.1155/2022/9320063
Li, C., Song, X., Chen, S., Wang, C., He, J., Zhang, Y., et al. (2021). Long-term effectiveness and adoption of a cellphone augmented reality system on patients with stroke: randomized controlled trial. JMIR serious games 9 (4), e30184. doi:10.2196/30184
Lin, M., and Yang, K. (2024). Breakthroughs and applications of augmented reality (AR) technology in the digital media field. Appl. Math. Nonlinear Sci. 9 (1), 20241530. doi:10.2478/amns-2024-1530
Mirza, T., Dutta, R., Tuli, N., and Mantri, A. (2025). Leveraging augmented reality in education involving new pedagogies with emerging societal relevance. Discov. Sustain. 6 (1), 77–15. doi:10.1007/s43621-025-00877-8
Moghaddam, N. G., Namazinia, M., Hajiabadi, F., and Mazlum, S. R. (2023). The efficacy of phase I cardiac rehabilitation training based on augmented reality on the self-efficacy of patients undergoing coronary artery bypass graft surgery: a randomized clinical trial. BMC Sports Sci. Med. and Rehabilitation 15, 1–9. doi:10.1186/s13102-023-00770-9
Naqvi, W. M., Naqvi, I. W., Mishra, G. V., and Vardhan, V. D. (2024). The future of telerehabilitation: embracing virtual reality and augmented reality innovations. Pan Afr. Med. J. 47, 157–4. doi:10.11604/pamj.2024.47.157.42956
Nekar, D. M., Dong-Yeop, L., Ji-Heon, H., Jin-Seop, K., Seong-Gil, K., Seo, Y.-G., et al. (2022). Effects of augmented reality game-based cognitive–motor training on restricted and repetitive behaviors and executive function in patients with autism spectrum disorder. Healthcare 10 (10), 1981. doi:10.3390/healthcare10101981
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., et al. (2021). The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Biomed. Cent. 10, 89. doi:10.1186/s13643-021-01626-4
Perkins, N. A., McCormack, G., and Dunlea, A. (2024). Designing and implementing an integrated occupational therapy foundations course: occupational science and occupational therapy perspectives. Int. J. Interdiscip. Educ. Stud. 19 (1), 163–174. doi:10.18848/2327-011X/CGP/v19i01/163-174
Pieczyńska, A., Zasadzka, E., Pilarska, A., Procyk, D., Adamska, K., and Hojan, K. (2023). Rehabilitation exercises supported by monitor-augmented reality for patients with high-grade glioma undergoing radiotherapy: results of a randomized clinical trial. J. Clin. Med. 12 (21), 6838. doi:10.3390/jcm12216838
Rizzi, J., Andrea, D. ’A., Proto, A., Piva, G., Lamberti, N., Bonfè, M., et al. (2023). A framework integrating augmented reality and wearable sensors for the autonomous execution of rehabilitation exercises. Electronics 12 (24), 4958. doi:10.3390/electronics12244958
Shim, G. Y., Kim, E. H., Lee, S. J., Chang, C. B., Lee, Y. S., Lee, J. I., et al. (2023). Postoperative rehabilitation using a digital healthcare system in patients with total knee arthroplasty: a randomized controlled trial. Archives Orthop. and Trauma Surg. 143 (10), 6361–6370. doi:10.1007/s00402-023-04894-y
Sievert, D. (2024). Occupational therapy vs physical therapy. Los Angeles, CA: UCLA Medical School. Available online at: https://medschool.ucla.edu/news-article/occupational-therapy-vs-physical-therapy.
Timmermans, C., Roerdink, M., Meskers, C. G. M., Beek, P. J., and Janssen, T. W. J. (2021). Walking-adaptability therapy after stroke: results of a randomized controlled trial. Trials 22 (1), 923. doi:10.1186/s13063-021-05742-3
Tsakanikas, V., Gatsios, D., Pardalis, A., Tsiouris, K. M., Georga, E., Doris-Eva, B., et al. (2022). Automated assessment of balance rehabilitation exercises with a data-driven scoring model: algorithm development and validation study. JMIR Rehabilitation Assistive Technol. 9 (3), e37229. doi:10.2196/37229
Vaida, C., Rus, G., Tucan, P., Machado, J., Pisla, A., Zima, I., et al. (2024). Enhancing robotic-assisted lower limb rehabilitation using augmented reality and serious gaming. Appl. Sci. 14 (24), 12029. doi:10.3390/app142412029
Wang, L., Chen, X., Deng, Q., You, M., Xu, Y., Liu, D., et al. (2023). Effectiveness of a digital rehabilitation program based on computer vision and augmented reality for isolated meniscus injury: protocol for a prospective randomized controlled trial. J. Orthop. Surg. Res. 18, 936–937. doi:10.1186/s13018-023-04367-3
Wei, W. (2019). Research progress on virtual reality (VR) and augmented reality (AR) in tourism and hospitality: a critical review of publications from 2000 to 2018. J. Hosp. Tour. Technol. 10 (4), 539–570. doi:10.1108/JHTT-04-2018-0030
Wu, J., Zhang, D., Lee, S., and Xian, J. (2025). Game on! Digital gaming and augmented reality/virtual reality in language learning. Int. J. Comput. - Assisted Lang. Learn. Teach. 15 (1), 1–15. doi:10.4018/IJCALLT.367601
Xu, Y., Chen, X., Wang, L., You, M., Deng, Q., Liu, D., et al. (2024). Efficacy of a computer vision-based system for exercise management in patients with knee osteoarthritis: a study protocol for a randomised controlled pilot trial. BMJ Open 14 (11), e077455. doi:10.1136/bmjopen-2023-077455
Yang, Z.-Q., Du, D., Wei, X.-Y., and Tong, R. K.-Y. (2022). Augmented reality for stroke rehabilitation during COVID-19. J. NeuroEngineering and Rehabilitation (JNER) 19 (1), 136–15. doi:10.1186/s12984-022-01100-9
Yu, J.-H., Nekar, D. M., Kang, H.-Y., Lee, J.-W., and Oh, S.-Y. (2023). Comparison of physical activity training using augmented reality and conventional therapy on physical performance following a total knee replacement: a randomized controlled trial. Appl. Sci. 13 (2), 894. doi:10.3390/app13020894
Keywords: augmented reality, rehabilitation, AR, physical therapy, occupational therapy
Citation: Modlin D and Kuo Y-T (2025) The effects of using augmented reality in rehabilitation and recovery exercise on patients’ outcomes and experiences: a systematic review. Front. Virtual Real. 6:1641316. doi: 10.3389/frvir.2025.1641316
Received: 04 June 2025; Accepted: 10 September 2025;
Published: 14 October 2025.
Edited by:
Cristina Dumitrescu, Binghamton University, United StatesReviewed by:
Emmanuel Egbunu, University of Ilorin, NigeriaJoaquin Dillen, Instituto Politecnico do Cavado e do Ave Laboratorio de Inteligencia Artificial Aplicada, Portugal
Copyright © 2025 Modlin and Kuo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Deiadra Modlin, ZGVtb2RsaW5AYWdnaWVzLm5jYXQuZWR1; Yu-Tung Kuo, eWt1b0BuY2F0LmVkdQ==
 Deiadra Modlin
Deiadra Modlin Yu-Tung Kuo
Yu-Tung Kuo