- 1Department of Occupational and Recreational Therapies, University of Utah, Salt Lake City, UT, United States
- 2Department of Health Behavior, Texas A&M University, College Station, TX, United States
- 3Center for Community Health and Aging, Texas A&M University, College Station, TX, United States
- 4Department of Recreation Sciences, East Carolina University, Greenville, NC, United States
- 5Department of Recreation and Leisure Studies, California State University Long Beach, Long Beach, CA, United States
- 6Department of Environmental and Occupational Health, Texas A&M University, College Station, TX, United States
Background: With the global rise in dementia prevalence, there is a growing interest in accessible, engaging, and preventive interventions for cognitive decline in older adults. Immersive virtual reality (VR) technologies have shown promise for delivering cognitively stimulating activities, yet limited research has examined the feasibility and acceptability of puzzle-based VR interventions among older adults.
Objective: This study aimed to evaluate the feasibility, usability, and acceptability of an immersive puzzle-based virtual reality (IPVR) intervention using VR Cubism among older adults, including those with mild cognitive impairment (MCI).
Methods: A single-arm feasibility study was conducted with 14 community-dwelling older adults (mean age = 72.3 years, SD = 5.3; 85.7% female) recruited from senior centers in Texas. Participants completed eight sessions of the IPVR program over 4 weeks. Cognitive screening was conducted using the Montreal Cognitive Assessment (MoCA), with a cutoff score of ≤18 used for exclusion. Usability, acceptability, and technology acceptance were evaluated using the System Usability Scale (SUS), Technology Acceptance and Attitudes Scale (TAAS), and Senior Technology Acceptance Model (STAM), respectively.
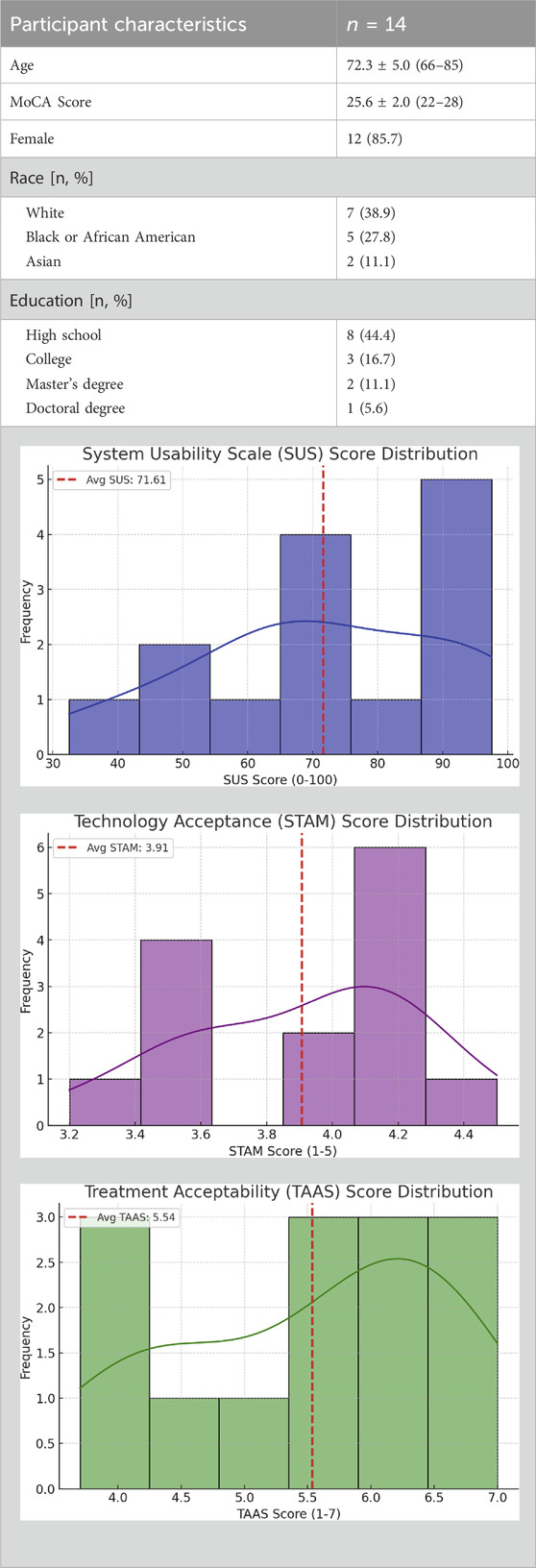
Results: Participants had MoCA scores ranging from 22 to 28 (M = 25.5, SD = 1.9); 50% scored in the normal cognitive range and 50% in the MCI range. The mean SUS score was 71.61 (SD = 15.8), indicating good usability. TAAS scores averaged 5.54/7, reflecting strong acceptability. The mean STAM score was 3.91/5, suggesting moderate to high technology acceptance, although some hesitancy and anxiety were reported. Participants expressed strong interest in using VR for future leisure activities and reported high enjoyment levels during the intervention.
Conclusion: Findings demonstrate that an immersive puzzle-based VR activity is feasible, usable, and acceptable for community-dwelling older adults, including those with MCI. This study supports the integration of engaging, technology-based interventions to promote cognitive health in aging populations. Practically, VR puzzle programs could be implemented in community centers, senior services, and clinical rehabilitation settings as accessible, enjoyable tools to encourage cognitive stimulation. These results highlight the potential of VR not only as a preventive wellness activity but also as a scalable adjunct to traditional cognitive health programs, warranting further evaluation in larger controlled trials.
Introduction
Dementia prevention has become a significant public health priority as the number of people diagnosed with dementia continues to rise and is expected to triple by 2030 (Rajan et al., 2021). People experiencing cognitive impairment face significant challenges with executive functioning, participation in daily activities, and pursuing an independent, active lifestyle (Ong et al., 2022). These challenges often lead to reduced quality of life, increased social isolation and loneliness, and a greater burden on caregivers (Schröder, 2024).
A host of genetic, lifestyle, and environmental factors that increase the risk of dementia onset and progression have been identified (Alzheimer, 2025). In response, public health researchers have developed and implemented programs that have been shown to delay dementia symptomology by improving the cognitive functioning of older adults (Lampit et al., 2015; La, 2010; Lee et al., 2024). One of the most effective activity-based programs is participation in cognitively stimulating activities such as puzzles, games, and reading books or magazines (Lampit et al., 2015; La, 2010; Lee et al., 2024) These previous studies provided evidence of the effects of cognitively stimulating activities on improving both positive and negative affect and the cognitive functioning of older adults. Among cognitively stimulating activities, puzzles can serve as an effective activity in facilitating improved cognitive and emotional benefits for older adults (Cegolon and Jenkins, 2022; Lin et al., 2023). Substantial empirical evidence has been provided that puzzles enhance a variety of domains of cognitive function including memory, mental rotation, perceptual reasoning, visual-spatial ability, and executive functioning (Cheng et al., 2024; Fissler et al., 2018; Givon Schaham et al., 2022). Neurologically, research findings have suggested that cognitive activities provide stronger protective effects for brain health than physical or social activities and lead to improved cognitive performance (Su et al., 2022).
Most recently, virtual reality (VR) technologies have emerged as an innovative and immersive platform for delivering cognitive training interventions. VR technology use can increase the motivation, engagement, and accessibility experienced by older adults with early-stage cognitive decline (Liao et al., 2019; Park et al., 2020; Parsons, 2015) emphasized the capacity of VR technologies to support cognitive interventions by integrating multisensory engagement and dynamic feedback, while Liu et al. (2022) highlighted their potential for positive effects when used in stroke rehabilitation and cognitive recovery. Various forms of VR-based interventions enhanced user motivation, adherence, and learning outcomes due to their game-like, interactive nature (Araiza-Alba et al., 2021; Wu et al., 2020).
A small number of studies have focused on the ability of puzzle-based VR games to produce health benefits for users (Liu et al., 2022; Taçgın, 2024; Choi et al., 2025; Wu and Chang, 2020). Taçgın (2024) demonstrated that puzzle-based VR environments evoke greater curiosity and persistence compared to non-immersive puzzle activities and suggested that immersive VR activity participation has the potential to increase user engagement and satisfaction. According to Wu and Chang (2020) VR puzzle game use has been found to improve the behavioral symptoms of people living with dementia. Similarly, Liu et al. (2022) observed improvements in the executive functioning of post-stroke patients following VR puzzle intervention participation. Choi et al. (2025) further noted that the emotionally safe environment of VR fosters resilience and reduces fear of failure.
While a small number of studies have provided evidence of the efficacy of a puzzle-based VR program on health benefits, there is currently, a limited research focused on the feasibility, acceptability, and usability of an immersive puzzle-based VR (IPVR) program by community-dwelling older adults. Most current evidence stems from clinical settings or controlled environments, which leaves a critically important gap in our understanding of how these tools function in real-world scenarios. By recruiting from senior centers and including participants with both normal cognition and mild cognitive impairment, this study uniquely extends the evidence base to a diverse, community-based sample.
Therefore, the purpose of this study is to address this gap by investigating the feasibility, acceptability, and usability of an IPVR program by community-dwelling older adults. The findings of our study provide practical insights into the design of future technology-based cognitive interventions for aging populations. Specifically, our investigation of the feasibility, acceptability, and usability of an IPVR program can lead to the design and assessment of an innovative intervention for future clinical trials.
Methodology
Study design and participants
We employed a single-arm design to assess the feasibility, usability, and acceptability of an IPVR program by community-dwelling older adults recruited through senior centers located in Texas. Eligibility criteria included: (a) aged 60 or older, (b) no prior experience with virtual reality, and (c) no diagnosis of dementia. Exclusion criteria included: (a) a history of dementia or major depressive disorder, and (b) severe sensory impairments related to vision or hearing.
Data collection and measurement
The research team contacted directors of senior centers in Texas via email and held informational meetings to explain the purpose of the study and, with their approval, posted recruitment flyers on center bulletin boards. Interested individuals were screened for eligibility and, upon qualification, received a demonstration of the VR equipment and the IPVR program.
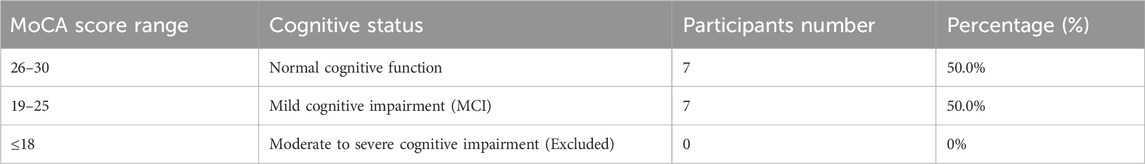
Following the screening and demonstration, participants provided written informed consent. Each participant completed eight sessions of the IPVR program, with each session lasting approximately 20–30 min. The Montreal Cognitive Assessment (MoCA) was used to assess the cognitive ability of the participants on the first day of the study. The cut-off MoCA score that we used to exclude participants was any score ≤18 (evidence of moderate to severe cognitive impairment).
Upon completion of the intervention, participants completed post-assessment measures, including the System Usability Scale (SUS) (Peres et al., 2013), the Technology Acceptance and Attitudes Scale (TAAS) (Van Der Laan et al., 1997), and the Senior Technology Acceptance Model (STAM) (Chen and Chan, 2014) questionnaire. SUS is a 10-item questionnaire that assesses users’ perception of the usability of a system. Scores range from 0 to 100, with scores above 68 generally considered above average in usability. TAAS includes subscales such as perceived usefulness, ease of use, and intention to use. Higher scores indicate positive attitudes and greater acceptance of technology. STAM reflects perceived usefulness, ease of use, and anxiety. Higher scores indicate greater acceptance using technology. In addition to the standardized measures, we asked supplementary questions regarding their interest in using VR for future activities. Ethical approval for this study was granted by the Institutional Review Board of the sponsoring institution.
Intervention description
Immersive puzzle-based virtual reality program
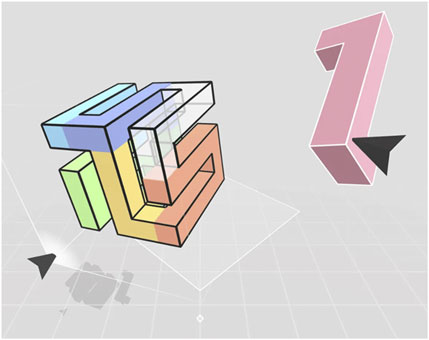
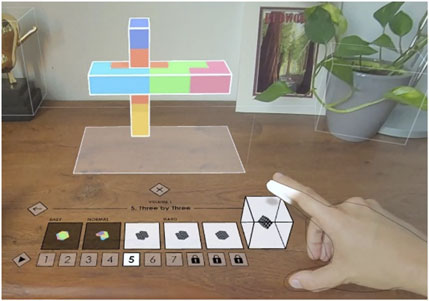
We used a commercially available application, VR Cubism, an immersive three-dimensional puzzle-based VR program that engages users in visuospatial reasoning and problem-solving tasks. Using a head-mounted display and two-handed controllers (Meta Quest 2), participants manipulate, rotate, and assemble geometric pieces to complete complex shapes (see Figure 1). The puzzle progressively increased in difficulty, starting from flat forms and advancing to more complex abstract shapes (e.g., pyramid, intersection, 3 by 3). The hand-tracking features allowed participants to use their hand directly to pick up and manipulate floating pieces (see Figure 2) Each session lasted approximately 20–30 min in a quiet room under the supervision of trained research staff. The program was delivered over eight sessions and tailored to older adults with no prior VR experience. Research staff provided guidance and technical support as needed, ensuring a safe and accessible experience.
Results
Study participants
A total of 14 community-dwelling older adults (mean age = 72.3 years, SD = 5.3; 85.7% female) participated in the feasibility study of the IPVR intervention using VR Cubism (see Table 1). Table 1 presents the demographic characteristics of the participants. The sample included a racially diverse group of participants: 38.9% identified as White (n = 7), 27.8% as Black or African American (n = 5), and 11.1% as Asian (n = 2). Educational backgrounds varied, with the majority having completed high school (22.2%, n = 4) or 12th grade (22.2%, n = 4), followed by college degrees (16.7%, n = 3), master’s degrees (11.1%, n = 2), with one participant reporting a doctoral degree (5.6%). Table 1 presents the full demographic characteristics of the participants. MoCA scores ranged from 22 to 28 (M = 25.5, SD = 1.9) (See Table 2). Based on the cutoffs, 50% of participants (n = 7) scored within the normal cognitive range (≥26), while the remaining 50% (n = 7) scored within the range indicative of mild cognitive impairment (Wu et al., 2020; Taçgın, 2024; Choi et al., 2025; Wu and Chang, 2020; Peres et al., 2013; Van Der Laan et al., 1997; Chen and Chan, 2014).
Usability
The usability of the IPVR system was evaluated using the SUS. The mean SUS score across participants was 71.61 (SD = 15.8), indicating an overall good usability rating that was above the commonly accepted threshold of 68. Approximately 79% (n = 11) of participants rated the system above this benchmark, suggesting that the VR Cubism puzzle application was generally perceived as easy to learn and use. Individual item analysis revealed high scores on statements such as “I found the system easy to use” (M = 4.00, SD = 1.04) and lower scores for items such as “I needed technical support to use this system” (M = 2.79, SD = 0.97) that highlighted minor usability concerns reported by a small subset of participants.
Acceptability
Acceptability was measured using the TAAS. The average TAAS score was 5.54 out of 7, which indicates a favorable perception of the relevance, clarity, and appropriateness of the VR puzzle activity. Most participants expressed agreement or strong agreement with statements evaluating the usefulness of and enjoyment experienced during the activity, supporting the acceptability of this intervention by study participants.
Technology acceptance
Participant general attitudes toward IPVR and technology were captured using the STAM scale. The mean overall STAM score was 3.91 out of 5, indicating a moderate to high level of technology acceptance. Participants reported feeling relatively confident using VR for leisure activities (M = 3.86, SD = 0.36), and a moderate willingness to use similar programs regularly in the future (M = 3.57, SD = 0.51). Some hesitancy was noted in responses related to making uncorrectable mistakes and general apprehension about technology, with a mean score of 2.57 (SD = 1.16) on those items.
Additional findings
We also captured self-reported quality of life indicators. Enjoyment of the activity was positively rated (M = 3.86, SD = 0.36), and most participants reported that the system was easy for them to use for leisure purposes (M = 3.29, SD = 0.91).
Discussion
In this pilot study, we assessed the feasibility, applicability, and usability of an IPVR activity for older adult participants including those with mild cognitive impairment. Our findings indicate that our older adult participants without moderate or severe dementia symptoms reported acceptable usability, acceptability, and technology acceptance scores. Despite the inherent complexity of puzzle activities, older adult participants reported that the IPVR program was easy to engage with and operate, which provides evidence that IPVR program use can be instrumental in promoting a sense of enjoyment for older adult users. Our findings provide evidence that IPVR program use has the potential to provide health benefits to older adult participants in a large-scale clinical trial.
Prior studies have provided evidence that traditional puzzle activities are associated with emotional regulation, stress reduction, and physical engagement. (Lin et al., 2023; Bacsu et al., 2019; Lazar and Nguyen, 2017). For example, Lin et al. (2023) reported that older adults frequently engage with puzzles not only to maintain mental acuity, but also to achieve a sense of emotional satisfaction and relaxation. Consistent with these findings, our findings suggest that puzzle activities that are facilitated through a VR platform can generate similar enjoyment and active engagement outcomes. Notably, puzzle activity participation fosters goal-directed behavior and intrinsic motivation that are important aspects in maintaining autonomy and psychological wellbeing in later life (Cegolon and Jenkins, 2022; Chen et al., 2022). Our findings support the potential of IPVR use to provide mental health benefits and improved overall wellbeing.
Our findings are consistent with prior studies demonstrating the puzzle-based or cognitive stimulating VR activities can promote engagement and enjoyment in older adults (Liu et al., 2022; Wu and Chang, 2020). Similar to Wu and Chang (2020), who reported improvement in behavioral symptoms in individuals with dementia using VR puzzle games, our participants reported significant enjoyment and willingness to continue. Likewise, Liu et al. (2022), underscoring the potential benefits in executive functioning among post-stroke patients. In addition, recent research conducted by GomezRomero-Borquez et al. (2024) compared three different puzzle-based VR games (e.g., Cubism, Puzzling Places, and Tetris) and found that each produced different outcomes across cognitive domains. These findings highlight the importance of selecting and tailoring VR game content to meet the specific cognitive needs of participants. Our study provides evidence that IPVR program use is feasible and acceptable to older adult users; however, future research is needed to identify which specific cognitive and health domains are most influenced by the intervention.
Despite the positive reception of the program by participants, participant STAM scores revealed some VR use hesitancy (7.14%). This result is aligned with previous findings that reported that older adult participants experienced technology anxiety and low levels of technology-related self-efficacy (Spears and Zheng, 2020). Alvseike and Brønnick (2012) reported that the cognitive deficits and low levels of perceived self-efficacy reported by older adults were significantly associated with the technology use barriers experienced by this user population. In our study, four participants (28.6%) expressed concerns about making mistakes or navigating the unfamiliar VR environment, highlighting that high usability and acceptance can coexist with underlying anxiety. Beyond psychological factors, practical barriers such as the high cost of VR hardware and limited accessibility for individuals with fewer technological resources also warrant consideration. Addressing these challenges will be essential to ensure equitable implementation and long-term adherence in both community and clinical settings. These findings underscore the need for a data-driven, strategic approach to reduce technology-related anxiety and build user confidence.
The findings of this study have several practical implications. In community settings such as senior centers, libraries, or adult day programs, immersive puzzle-based VR could be offered as a group or individual leisure activity that promotes both engagement and cognitive stimulation. In clinical environments, VR puzzle interventions may serve as a complementary tool in cognitive rehabilitation programs for older adults with MCI, providing a motivating alternative to traditional paper-based or computerized tasks. At the individual level, commercially available VR systems could be adapted for home use, enabling older adults to independently engage in cognitively stimulating activities as part of their daily routines. For successful integration, it will be important to provide structured orientation, ongoing technical support, and strategies to minimize barriers such as cost, accessibility, and technology-related anxiety.
Limitations and future directions
Some study limitations must be addressed. First, although our single-arm study focused on feasibility, acceptability, and usability of the IPVR program, we did not report any preliminary health outcomes associated with participation. In addition, the absence of a control group limits the ability to draw conclusions about the efficacy of the intervention. Future research should assess potential mental and cognitive health outcomes using a randomized controlled trial design. While this study was framed within the context of cognitive health, no pre/post cognitive outcome measures were included. Future trials should incorporate validated cognitive assessments to evaluate potential cognitive benefits. Also, all outcome measures were based on self-report, which may be subject to social desirability bias. Future studies should integrate objective measures such as task performance, physiological data, or behavioral observations. Secondly, the small sample size limits the generalizability of findings. As this was an initial feasibility pilot, the intent was to gather preliminary data to inform the design of larger randomized controlled trials. Future studies with larger, more representative samples are needed to strengthen external validity. Also, given the small sample size, subgroup comparison between participants with normal cognition and those with MCI was not conducted. It would be beneficial if future researchers investigated the relationship between the effects of IPVR program use on health benefits at different participant cognitive levels. Lastly, the majority of participants were female (85.7%). This imbalance reflects demographic trends in aging research, where women are often overrepresented. Also, all participants were recruited from senior center, which may represent a relatively active and socially engaged. As such, the findings may not fully generalize to older adults with lower activity levels. Nonetheless, future research should include recruitment strategies that actively engage male participants to enhance representativeness. In addition, as demographic factors such as age, sex, educational background, and residential setting can affect technology acceptance, feasibility, and the usability of the program, these variables should be studied in depth in the future.
Conclusion
In this study, we examined the acceptance, usability, and acceptability of the IPVR technology program by older adults with primarily normal cognition, with a minority classified as having MCI. Our findings provide much needed insights into the practical considerations involved in the design and development of large-scale efficacy trials and provide empirical evidence that the IPVR program used in this study was practical, engaging, and usable by an aging population in real-world environments.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by texas a&m university institutional review board. The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study.
Author contributions
YK: Writing – original draft, Visualization, Formal Analysis, Conceptualization, Writing – review and editing. JuK: Writing – original draft, Supervision, Writing – review and editing, Methodology, Conceptualization, Project administration. JaK: Methodology, Formal Analysis, Writing – review and editing, Validation. CL: Validation, Formal Analysis, Methodology, Writing – review and editing, Conceptualization, Resources. MO: Writing – review and editing.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
The author(s) declared that they were an editorial board member of Frontiers, at the time of submission. This had no impact on the peer review process and the final decision.
Generative AI statement
The author(s) declare that Generative AI was used in the creation of this manuscript. The use of artificial intelligence (AI) in the preparation of this manuscript was limited solely to proofreading and language refinement. No AI tools were used for data analysis, content generation, interpretation of results, or drawing scientific conclusions.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Alvseike, H., and Brønnick, K. (2012). Feasibility of the iPad as a hub for smart house technology in the elderly; effects of cognition, self-efficacy, and technology experience. J. Multidiscip. Healthc. 5, 299–306. doi:10.2147/JMDH.S35344
Alzheimer, A. (2025). Alzheimer’s disease facts and figures. Available online at: https://www.alz.org/getmedia/ef8f48f9-ad36-48ea-87f9-b74034635c1e/alzheimers-facts-and-figures.pdf.
Araiza-Alba, P., Keane, T., Matthews, B., Simpson, K., Strugnell, G., Chen, W. S., et al. (2021). The potential of 360-degree virtual reality videos to teach water-safety skills to children. Comput. Educ. 163, 104096. doi:10.1016/j.compedu.2020.104096
Bacsu, J., McIntosh, T., Viger, M., Johnson, S., Jeffery, B., and Novik, N. (2019). Supporting older adults’ engagement in health-care programs and policies: findings from a rural cognitive health study. Home Health Care Serv. Q. 38 (3), 209–223. doi:10.1080/01621424.2019.1614505
Cegolon, A., and Jenkins, A. (2022). Older adults, cognitively stimulating activities and change in cognitive function. Int. J. Lifelong Educ. 41 (4–5), 405–419. doi:10.1080/02601370.2022.2082574
Chen, K., and Chan, A. H. S. (2014). Gerontechnology acceptance by elderly Hong Kong Chinese: a senior technology acceptance model (STAM). Ergonomics 57 (5), 635–652. doi:10.1080/00140139.2014.895855
Chen, P. J., Hsu, H. F., Chen, K. M., and Belcastro, F. (2022). Effects of tabletop games on cognition in older adults: a systematic review and meta-analysis. Games Health J. 11 (4), 225–235. doi:10.1089/g4h.2021.0132
Cheng, Q., Wang, H., Cui, M., Wang, Q., and Li, L. (2024). Efficacy of wooden toy training in alleviating cognitive decline in elderly individuals with cognitive impairment: a cluster randomized controlled study. PLoS One 19 (10), e0309685. doi:10.1371/journal.pone.0309685
Choi, M., Cui, D., Volonte, M., Koilias, A., Kao, D., and Mousas, C. (2025). Toward understanding the effects of intelligence of a virtual character during an immersive jigsaw puzzle Co-Solving task. ACM Trans. Appl. Percept. 22 (2), 1–28. doi:10.1145/3700822
Fissler, P., Küster, O. C., Laptinskaya, D., Loy, L. S., Von Arnim, C. A. F., and Kolassa, I. T. (2018). Jigsaw puzzling taps multiple cognitive abilities and is a potential protective factor for cognitive aging. Front. Aging Neurosci. 10, 299. doi:10.3389/fnagi.2018.00299
Givon Schaham, N., Buckman, Z., and Rand, D. (2022). The effect of daily practice of puzzle-game apps on cognition in two groups of older adults: a pre-post experimental study. Int. J. Environ. Res. Public Health 19 (23), 15454. doi:10.3390/ijerph192315454
GomezRomero-Borquez, J., Del-Valle-Soto, C., Del-Puerto-Flores, J. A., Castillo-Soria, F. R., and Maciel-Barboza, F. M. (2024). Implications for serious game design: quantification of cognitive stimulation in virtual reality puzzle games through MSC and SpEn EEG analysis. Electron. (Basel) 13 (11), 2017. doi:10.3390/electronics13112017
La, R. A. (2010). Healthy brain aging: role of cognitive reserve, cognitive stimulation, and cognitive exercises. Clin. Geriatr. Med. 26 (1), 99–111. doi:10.1016/j.cger.2009.11.003
Lampit, A., Hallock, H., Suo, C., Naismith, S. L., and Valenzuela, M. (2015). Cognitive training-induced short-term functional and long-term structural plastic change is related to gains in global cognition in healthy older adults: a pilot study. Front. Aging Neurosci. 7, 14. doi:10.3389/fnagi.2015.00014
Lazar, A., and Nguyen, D. H. (2017). “Successful leisure in independent living communities: understanding older adults’ motivations to engage in leisure activities,” in Proceedings of the 2017 CHI conference on human factors in computing systems, 7042–7056.
Lee, J., Kim, J., and Valdivia, D. S. (2024). A longitudinal analysis of the relationship between different levels of cognitively stimulating leisure activity and cognitive function among older adults with MCI. J. Cognitive Enhanc. 8 (3), 257–270. doi:10.1007/s41465-024-00293-2
Liao, Y. Y., Hsuan Chen, I., Lin, Y. J., Chen, Y., and Hsu, W. C. (2019). Effects of virtual reality-based physical and cognitive training on executive function and dual-task gait performance in older adults with mild cognitive impairment: a randomized control trial. Front. Aging Neurosci. 11, 162. doi:10.3389/fnagi.2019.00162
Lin, M. L., Lopez, J. D., Silva, A., Ali, K., Brookshaw, V. Y., Martinez, M. G., et al. (2023). Cognitive and socio-emotional benefits of puzzle working in older adults. Act. Adapt Aging. 47 (3), 348–363. doi:10.1080/01924788.2022.2120761
Liu, Z., He, Z., Yuan, J., Lin, H., Fu, C., Zhang, Y., et al. (2022). Application of immersive virtual-reality-based puzzle games in elderly patients with post-stroke cognitive impairment: a pilot study. Brain Sci. 13 (1), 79. doi:10.3390/brainsci13010079
Ong, M., Pek, K., Tan, C. N., Chew, J., Lim, J. P., Yew, S., et al. (2022). Social frailty and executive function: association with geriatric syndromes, life space and quality of life in healthy community-dwelling older adults. J. Frailty Aging 11 (2), 206–213. doi:10.14283/jfa.2021.43
Park, J. S., Jung, Y. J., and Lee, G. (2020). Virtual reality-based cognitive–motor rehabilitation in older adults with mild cognitive impairment: a randomized controlled study on motivation and cognitive function. Healthcare 8, 335. doi:10.3390/healthcare8030335
Parsons, T. D. (2015). Virtual reality for enhanced ecological validity and experimental control in the clinical, affective and social neurosciences. Front. Hum. Neurosci. 9, 660. doi:10.3389/fnhum.2015.00660
Peres, S. C., Pham, T., and Phillips, R. (2013). “Validation of the system usability scale (SUS) SUS in the wild,” in Proceedings of the human factors and ergonomics society annual meeting (Los Angeles, CA: Sage Publications Sage CA), 192–196.
Rajan, K. B., Weuve, J., Barnes, L. L., McAninch, E. A., Wilson, R. S., and Evans, D. A. (2021). Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020–2060). Alzheimer’s and Dementia 17 (12), 1966–1975. doi:10.1002/alz.12362
Schröder, J. (2024). The burden and quality of life of dementia caregivers: exploring the roles of care recipients’ social cognition. Mem. Exec. Funct.
Spears, J., and Zheng, R. (2020). Older adults’ self-efficacy in computer use and the factors that impact their self-efficacy: a path analysis. Educ. Gerontol. 46 (12), 757–767. doi:10.1080/03601277.2020.1815976
Su, S., Shi, L., Zheng, Y., Sun, Y., Huang, X., Zhang, A., et al. (2022). Leisure activities and the risk of dementia: a systematic review and meta-analysis. Neurology 99 (15), e1651–e1663. doi:10.1212/wnl.0000000000200929
Taçgın, Z. (2024). Unlocking the Puzzle: Investigating Problem-Solving Patterns in 2D and 3D Virtual Reality Environments Through Mixed Methods Analysis.Int. J. Hum. Comput. Interact., 1–15. doi:10.1080/10447318.2024.2369368
Van Der Laan, J. D., Heino, A., and De Waard, D. (1997). A simple procedure for the assessment of acceptance of advanced transport telematics. Transp. Res. Part C Emerg. Technol. 5 (1), 1–10. doi:10.1016/s0968-090x(96)00025-3
Wu, Y., and Chang, W. (2020). Research on the treatment of the elderly with Alzheimer disease in virtual reality puzzle games. Front. Soc. Sci. Technol. 3, 5–8. doi:10.25236/FSST.2021.030702
Keywords: virtual reality, dementia, puzzle, older adult, feasibility and acceptability
Citation: Kim Y, Kim J, Kim J, Lee C and Ory MG (2025) Feasibility and acceptability of an immersive puzzle-based virtual reality activity for community-dwelling older adults. Front. Virtual Real. 6:1655981. doi: 10.3389/frvir.2025.1655981
Received: 29 June 2025; Accepted: 13 October 2025;
Published: 12 November 2025.
Edited by:
Jorge Peña, University of California, Davis, United StatesReviewed by:
Samet Aktaş, Batman University, TürkiyeGrace Madonna Singh, Swami Rama Himalayan University, India
Copyright © 2025 Kim, Kim, Kim, Lee and Ory. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Junhyoung Kim, a2ltOUB0YW11LmVkdQ==
 Yongseop Kim
Yongseop Kim Junhyoung Kim
Junhyoung Kim Jaehyun Kim4
Jaehyun Kim4 Marcia G. Ory
Marcia G. Ory