- 1Department of ORL–Head and Neck Surgery and Audiology, Odense University Hospital, Odense, Denmark
- 2Department of Endocrinology and Metabolism, Odense University Hospital, Odense, Denmark
Background: Patients with goiter referred for thyroidectomy report swallowing difficulties. This might be associated with esophageal compression and deviation as this is present in a significant number of patients. Studies on how goiter and subsequently its treatment affect the esophagus are sparse and point in various directions. Our aim was to investigate, through a systematic review, the impact of goiter and thyroidectomy on esophageal anatomy, esophageal physiology, and subjective swallowing dysfunction.
Methods: The search period covered 1 January 1975 to 1 July 2018, using the scientific databases PubMed and EMBASE. Inclusion criteria were adult patients with goiter who were either observed or underwent thyroidectomy. Search terms were variations of the terms for goiter, esophagus, swallowing, and dysphagia. From an initial 3,040 titles, 55 full text evaluations led to the final inclusion of 27 papers. Seventeen papers investigated, prospectively, the impact of thyroidectomy on the esophagus, while five observational and five retrospective studies were also included.
Results: Esophageal anatomy impairment: Esophageal deviation occurred in 14% and esophageal compression in 8–27% of goiter patients. The prevalence increased with goiter size and with the extent of substernal extension. The smallest cross-sectional area of the esophagus increased by median 34% after thyroidectomy. Esophageal physiology changes: Goiter patients had increased esophageal transit time, positively correlated with goiter size, but unrelated to esophageal motility disturbances. Decrease in the upper esophageal sphincter pressure occurred early after surgery, and normalized within 6 months. Swallowing related patient-reported outcomes: Evaluated by validated questionnaires, swallowing symptoms worsened in the early period after thyroidectomy, but improved after 6 months, as compared to baseline.
Conclusions: Thyroidectomy relieved patients with goiter from dysphagia, within 6 months of surgery probably via increase in the cross-sectional area of the esophagus. Attention to the impact by goiter on the esophagus is needed, and balanced and individualized information about the potential benefits and risks of thyroid surgery is crucial in the management of patients with goiter.
Introduction
Nodularity of the thyroid gland–caused by delicate interactions between genetic and environmental factors such as low iodine intake and cigarette smoking-is common and, depending on definition and type of imaging, affect 20–76% of the population (1–4). The vicinity of the thyroid to vital structures in the neck and upper mediastinum, i.e., the trachea, esophagus, nerves, and blood vessels, combined with a tendency to gradually increase in size, leads to a variety of potential clinical manifestations of the goiter. These include compromised respiration and dysphagia, as well as globus and choking sensation, as some of the most prevalent symptoms (5–9). The positive correlation between goiter size and tracheal compression, and the relief following thyroidectomy is well accepted (10). However, studies on how goiter and subsequently its treatment affect the esophagus are sparse and point in various directions.
Patients with goiter referred for thyroidectomy report swallowing difficulties (11–15) and these may be associated with esophageal compression and deviation, which are abnormalities found to be present in a significant number of patients (8, 16). Thyroidectomy seems to improve both swallowing difficulties (12, 17, 18) and quality of life (19–21) in patients with goiter. The latter improves already 3 months after surgery (19), whereas at least 6 months need to pass before improvements in swallowing symptoms can be expected (11, 22). Comparison of the obviously inhomogeneous studies of the esophagus is almost impossible, which makes it difficult to offer patients with goiter evidence-based information on the surgical effect regarding esophageal compression, dysphagia, and globus sensation.
The aim of the present study was, through a systematic review, to investigate the impact of goiter and thyroidectomy on esophageal anatomy and physiology, and swallowing related patient reported outcomes.
Methods
Study Design, Search Terms, and Extraction of Data
We identified all available English language publications regarding the relationship between goiter and the esophagus, covering the period from 1 January 1975 to 1 July 2018. The search terms used in the scientific databases PubMed and EMBASE were variations of the terms for goiter, esophagus, swallowing, and dysphagia, with MESH terms being Goiter, Esophagus, Deglutition, and Deglutition disorders.
Initially, we screened publication titles and then selected abstracts of relevance. Each identified paper was screened in accordance with the inclusion criteria being: data obtained in humans; age ≥18 years; individuals should undergo thyroidectomy or be offered observation alone; any study should include a minimum of 15 patients. The reference list of each paper was screened for missed publications. The data extracted included number of patients, gender, study design, blinding, inclusion, and exclusion criteria, summary of results, and the presence of major confounders as well as limitations and biases. Biases were assessed for the individual studies using the “Cochrane Risk of Bias tool” (23).
Results
Study Selection and Characteristics
From PubMed and EMBASE 3,040 relevant titles were included, supplemented by 20 articles obtained from the reference lists of included papers (Figure 1). We excluded 3,005 papers after review of titles and abstracts, leaving 55 for full text evaluation. Twenty-eight full text papers failed to meet the inclusion criteria, resulting in 27 papers for the final analyses.
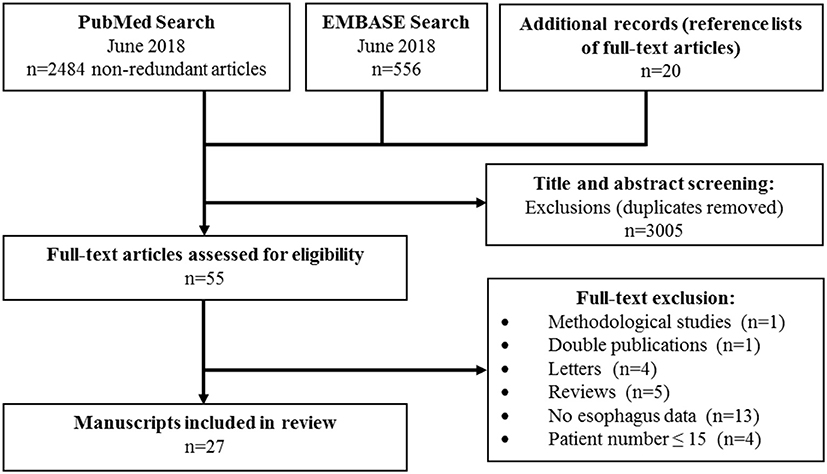
Figure 1. Flow diagram of manuscript selection of final inclusion and final inclusion of full-text manuscripts.
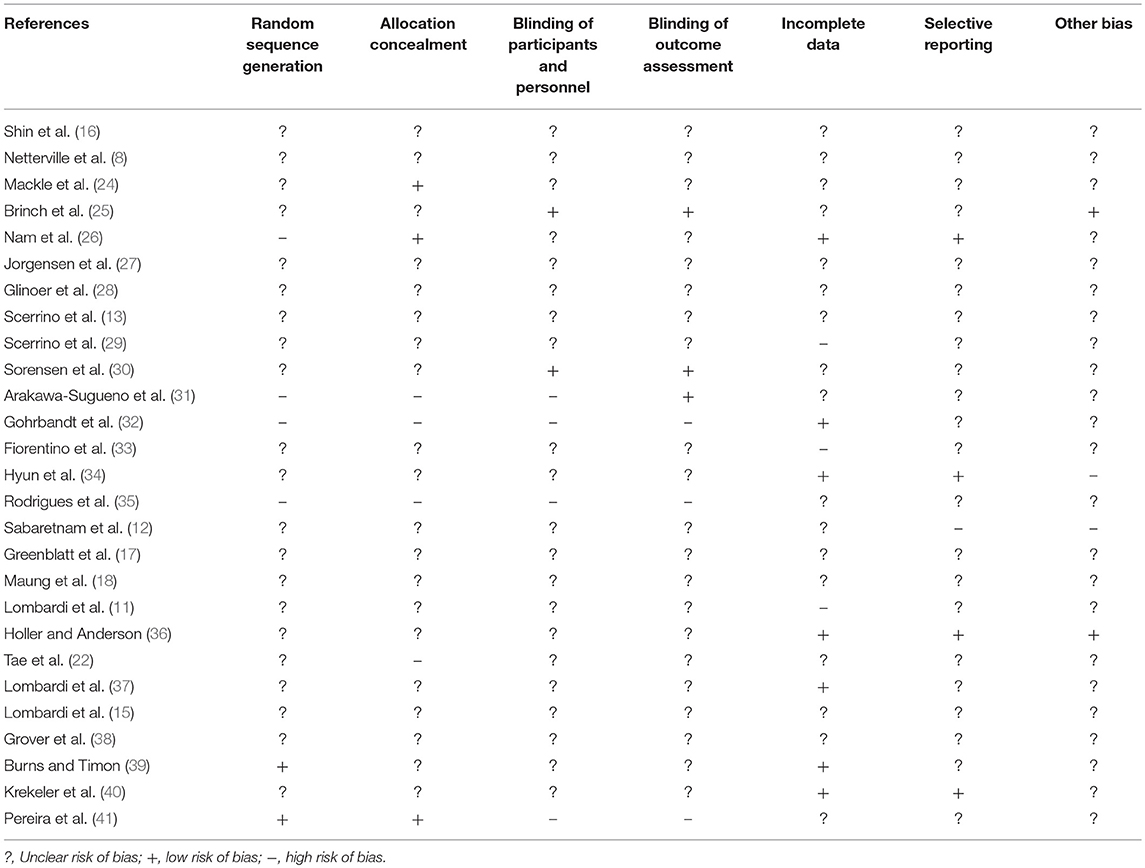
Applying the “Cochrane Risk of Bias tool” across studies (23), we found a considerable risk of bias as many studies failed to describe inclusion procedures, include control groups, randomize for treatment, or blind observers or participants (Table 1). As a consequence, we made no attempt to perform a meta-analysis. Most of the included studies (Tables 2, 3) were small, with 60 or fewer individuals in 14 of the 27 studies. Only one study applied randomization (15) and three studies used some blinding of participants, personnel or the evaluated outcomes (25, 30, 31). There were five observational studies, 17 studies investigating the impact of thyroidectomy, and five retrospective studies with two studies investigating thyroidectomy (Tables 2, 3). As evident from the heterogenous studies, the level of evidense range from low to moderate (Table 4).
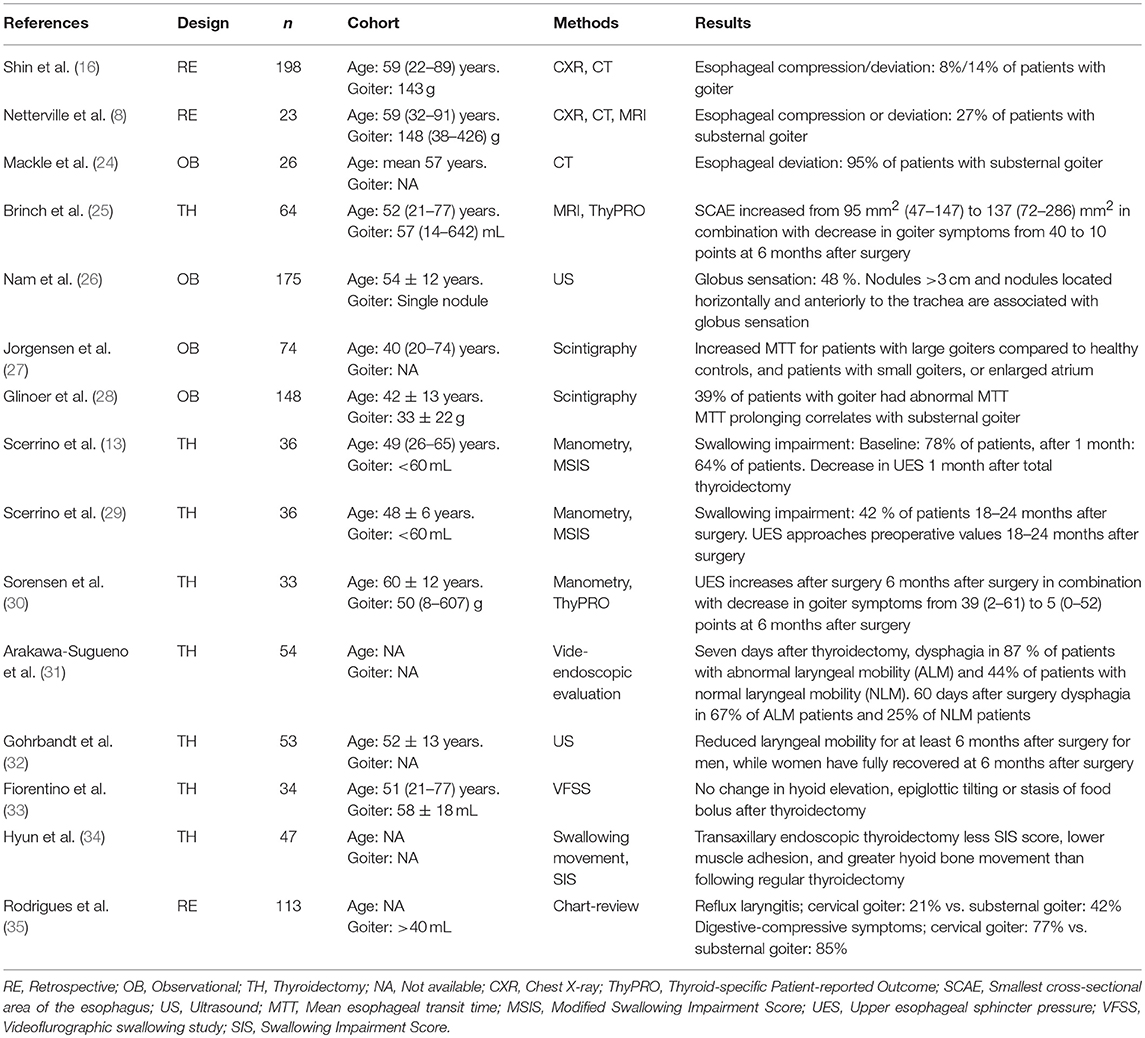
Table 2. Studies investigating the effect of goiter on the esophagus anatomy abnormalities and the esophageal physiology changes.
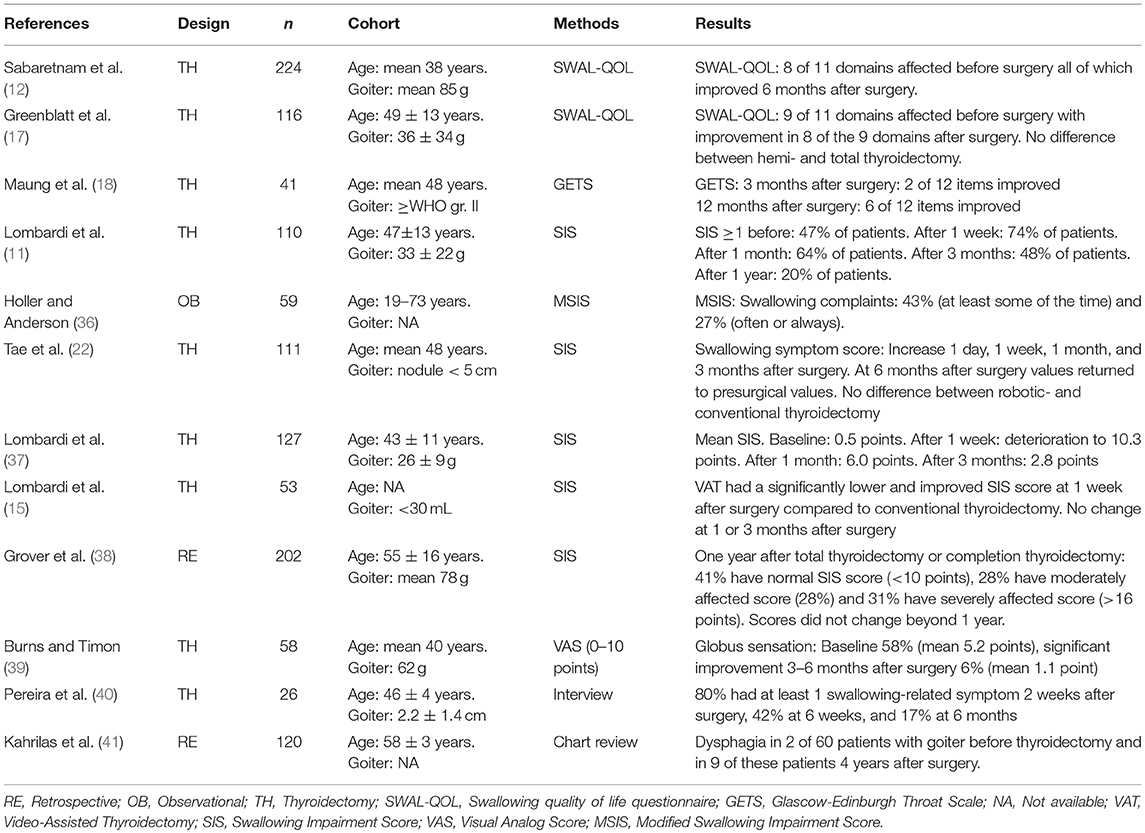
Table 3. Studies investigating the effect of goiter on the swallowing-related patient reported outcomes.
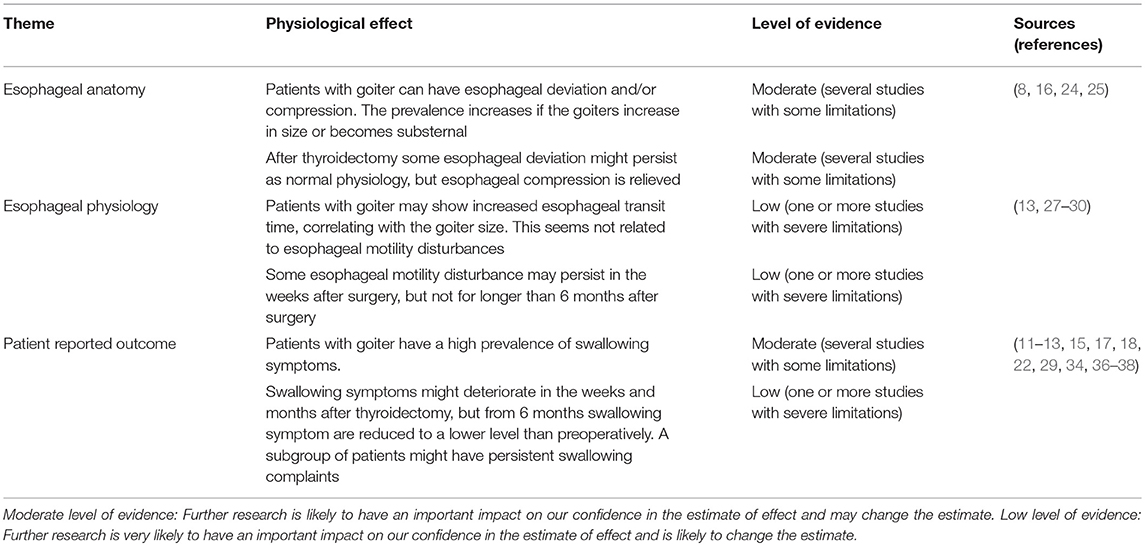
Table 4. Recommendations based on strength of evidence (50).
Esophageal Anatomy Abnormalities
Affection of the esophagus was a common finding among patients with goiter (Table 2). Four studies evaluated, by chest X-ray, CT, or MRI, the prevalence of esophageal compression and/or deviation in patients undergoing thyroidectomy (8, 16, 24, 25). A study of 198 patients found esophageal deviation in 14% of individuals, and esophageal compression in even fewer (8%) (16). A higher prevalence of esophageal compression was found in another study of only 23 patients, with six patients (26%) having esophageal compression (8). A third study found 24 of 26 patients (95%) with substernal goiter to have esophageal midline deviation (24). All the above studies had shortcomings, such as unclear definitions of either esophageal deviation and/or compression.
A more recent study (25), with well-defined definitions of both esophageal deviation and compression, evaluated 65 well-characterized goiter patients undergoing neck MRI before and 6 months after thyroidectomy. In that study, the median esophageal deviation decreased significantly from 4 mm (range: 0–23 mm) to 3 mm (range: 0–10 mm). More importantly, the median smallest cross-sectional area of the esophagus (SCAE) increased from 95 mm2 (range: 47–147 mm2) at baseline to 137 mm2 (range: 72–286 mm2) after surgery, corresponding to a median increase of 34% (range, −17 to 253%) in SCAE (25). The anterior-posterior depth of the esophagus did not change significantly following surgery, while the median-lateral width of the esophagus achieved a small but significant increase from a median of 15 mm (range: 10–21 mm) to 17 mm (range: 12–24) after surgery (Table 2). The esophagus had a small midline deviation, and this persisted after surgery. More importantly, there was an increase in the cross-sectional area of the esophagus following surgery, and a change from a more round to a more ellipsoid shape. The preoperative volumes of the thyroid and the SCAEs were significantly inversely correlated, with reduction in SCAE of 0.35 mm2 for every 10% increase in goiter volume. In addition, the SCAE increased by 1% for every 10% increase in the weight of the removed thyroid tissue (25). This implies that patients with the initially largest goiters also experienced the most pronounced improvements in SCAE, following thyroid surgery.
In relation to the impact of individual nodules on esophageal anatomy, one study found globus sensation to be present in 48% of patients. Nodules >3 cm in diameter, and/or located anteriorly and horizontally to the trachea were more often present in patients with globus sensation than in patients with smaller nodules or nodules located laterally to the trachea (26).
Esophageal Physiology Changes
The swallowing function had been investigated by various objective methods (Table 2). Using scintigraphic methods for assessment, an increase in the esophageal transit time by 2–7 s were demonstrated in patients with a large goiter (>7 cm long or >3 cm in depth, evaluated by ultrasound), as compared to smaller goiters (27). Another study, also using nuclear medicine techniques, found 39% of goiter patients to have increased esophageal transit time (28).
A study of 36 patients identified a decrease in the upper esophageal sphincter (UES) pressure, using water manometry, in the early period after total thyroidectomy (13). However, these findings were normalized 18–24 months after surgery in a subsequent study of the same patient cohort (29). Another study of 33 patients, found normal esophageal motility, both before and 6 month after surgery (30). Only the UES basal pressure increased significantly from 71 to 88 mmHg 6 month after surgery, the latter value being within the normal limits (30). In our study, using the Chicago classification version 3.0 for assessing motility disturbances (42), only one of the 33 patients with a benign goiter (3%) had a minor peristaltic disorder preoperatively, defined as >50% weak or failed coordinated esophageal muscle contractions during 10 swallowing events (30). Two patients (6%) fulfilled these criteria 6 months after surgery. Importantly, as patient characteristics as well as the manometric examination techniques (i.e., water manometry and high resolution esophageal manometry), differed between the studies, a direct, comparison across studies is not meaningful. Nevertheless, it seems that decrease in the UES pressure potentially may be present in the early period after surgery as the goiter is removed. This issue is of no greater concern beyond 6 months after surgery.
A few studies have investigated the hyoid bone movement, epiglottic tilting, and laryngeal mobility in goiter patients (31–35). A study of 54 patients demonstrated a preoperative association between abnormal laryngeal mobility and the prevalence of dysphagia in patients with goiter (31). In the immediate weeks after surgery the laryngeal mobility was reduced, with recovery at 6 months postoperatively (32). Another study found the hyoid bone movement to be unchanged after surgery in an investigation of 34 patients (33). In a study with 54 patients divided into two groups using neither randomization nor blinding, trans-axillary thyroidectomy was associated with a lower degree of neck muscle adhesion and a greater hyoid bone movement, as compared with conventional thyroidectomy (34). The prevalence of reflux laryngitis was also found lower in patients with cervical compared to substernal goiter, at 21 vs. 42%, respectively (35).
Swallowing Related Patient-Reported Outcomes
Three studies, using validated swallowing specific questionnaires, have investigated the patients' perception of swallowing before and after thyroidectomy (Table 3) (12, 17, 18). By using the “swallowing related quality of life questionnaire,” eight (12) and nine (17) of 11 swallowing related domains were affected in studies of 116 and 224 patients with goiter, respectively, all of whom were referred for thyroidectomy. Using the validated Glasgow-Edinburgh throat scale, only two of 12 items improved at 3 months after surgery, while six items had improved after 12 months (18).
Nine studies, the largest including more than 100 patients, used the non-validated swallowing impairment score or modified versions hereof (11, 13, 15, 22, 29, 34, 36–38). Prior to thyroidectomy, the prevalence of dysphagia varied between 48 and 78% (11, 13, 36). At 1 week, 1 month, and 3 months after thyroidectomy, three studies found increased prevalence (i.e., worsening) of swallowing symptoms compared to the preoperative level (11, 22, 37), while a single study of 53 patients found a decreased level of dysphagia (15). However, at 6 months or later after surgery, patients had fewer symptoms than at baseline (11, 22, 29), although a subgroup had persistent swallowing complaints (38). Studies using other examination techniques, such as qualitative analyses, supported these findings (39–41). The impact on swallowing symptoms seemed uninfluenced by the surgical technique or whether hemi- or total thyroidectomy was performed (15, 17, 18, 22).
Two recent studies, carried out by our group on the same patient cohort, assessed the impact of thyroidectomy and esophageal dysfunction by use of the well-validated disease-specific ThyPRO questionnaire (25, 30). Goiter patients had a significantly affected mean Goiter Symptom score of 40 points at baseline (maximum of 100 points equals severe symptoms), which improved significantly to a mean of 10 points postoperatively (25) (minimum of 0 points equals no symptoms) (Table 2). All 11 items of the Goiter Symptom scale improved 6 months after surgery. The items related to swallowing difficulties, such as “discomfort swallowing,” underwent a significant score reduction from a mean of 1.8 points (maximum of 4 points) to 0.3 points, postoperatively. Similarly, the mean score for “difficulty swallowing” decreased significantly from 1.2 to 0.2 points after surgery, while “Globus sensation” decreased from 2.3 to 0.7 points.
Discussion
Studies using objective measures of the effect of goiter on the esophagus are limited. Nevertheless, the existing literature suggests that presence of goiter is associated with both esophageal deviation and compression, and that this is relieved by surgery (8, 16, 24, 25). In addition, goiter patients may show a prolonged passage and some impact on the esophageal peristaltic movement and/or sphincter pressure, as determined by either nuclear medicine techniques or various forms of esophageal manometry (13, 27, 28, 30). Importantly, surgery does not cause deterioration in the above mentioned parameters.
Objective analyses of the esophagus support the high prevalence of preoperative swallowing difficulties as reported by 48–78% of the patients (11, 13, 36). Evaluated by patient reported outcomes, reports on swallowing symptoms during the first 3 months after surgery have shown conflicting results (11, 13, 15, 22, 37). In fact, some studies have shown deterioration until 6 months after surgery (11, 22, 37). More consistently, all studies demonstrate significant improvement of the swallowing symptoms beyond 6 months after surgery (11, 12, 17, 22, 38), although a subgroup of patients have persistent complaints more than 1 year after surgery (38). More generally, the Goiter Symptom Score, extracted from the ThyPRO instrument, improved after surgery, with significantly reduced globus sensation and swallowing difficulties (25, 30). However, symptom assessment obtained by questionnaires cannot be performed with blinding of the patients, which may have influenced the outcome in all studies of this kind.
Further studies are needed to examine the relation between goiter and the esophagus, and the effect of treatment. In particular, it is of interest to compare surgical and non-surgical techniques–such as radioiodine therapy (43) and ultrasound-guided thermal procedures in the form of e.g., laser or radiofrequency ablation (44). These non-surgical ablation techniques are less prone to side-effects such as voice changes and postoperative hypothyroidism (45–48), while the potential effects on the esophagus remain unknown. Awaiting such studies, and comparison with the long-established surgical approaches, leaves a gap in our ability to provide individual-tailored therapy for goiter patients.
Study Limitations
Although inclusion of solely English language publications theoretically might have caused bias, this does not seem to be the case (49). Women constitute the majority of patients, de facto and in the cited literature. This means that some of the conclusions may not be as valid for male as for female goiter patients. The majority of the identified studies contained a limited number of patients, and many of the intervention studies are hampered by loss to follow-up in 20% of patients (15, 17, 33), or higher (11, 37, 38), especially in studies of esophagus motility due to patient discomfort associated with these procedures (9).
Comparing studies of mixed patient populations regarding age, setting of recruitment, diagnosis i.e., thyroid malignancy, hyper- and hypothyroidism, and benign nodular goiter, complicates interpretation of the results. The fact that patients were included from highly selected populations and from both primary, secondary and tertiary centers, as well as from surgical and medical departments constitute additional limitations. Needless to say, it is unknown to which degree these influence our conclusions and generalizability of the manuscript.
Implications for the Future
Future studies should compare 131I therapy and ultrasound-guided thermal ablation techniques with various surgical techniques for goiter ablation, as for the effect on the esophagus. Such studies should be performed using validated swallowing and quality-of-life-related questionnaires, with measurements of the esophageal anatomy and function as the potential primary endpoints. Follow-up should be a minimum of 6 months, since improvement of swallowing dysfunction at an earlier time point cannot be expected, at least not after surgical goiter ablation.
Conclusions
Patients with goiter benefit substantially from thyroidectomy, with profound improvements in dysphagia and increase in the cross-sectional area of the esophagus. However, in most patients the improvements do not occur before 6 months after thyroidectomy. In fact, deterioration in dysphagia may be seen in the early period after surgery. Studies evaluating the long-term status of these parameters, and comparing surgical and non-surgical goiter treatment techniques, are warranted.
Author Contributions
All authors (JS, CG, SB, and LH) contributed in the conception of design, interpretation, revising the manuscript critically, and approval of the final manuscript. JS contributed with acquisition and analysis of data, and drafting the work.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Carle A, Krejbjerg A, Laurberg P. Epidemiology of nodular goitre. Influence of iodine intake. Best Pract Res Clin Endocrinol Metab. (2014) 28:465–79. doi: 10.1016/j.beem.2014.01.001
2. Gharib H, Papini E, Paschke R, Duick DS, Valcavi R, Hegedüs L, et al. American Association of Clinical Endocrinologists, Americal College of Endocrinology, and Associazione Medici Endocrinologi medical guidelines for clinical practice for the diagnosis and management of thyroid nodules−2016 update. Endocr Pract. (2016) 22:622–39. doi: 10.4158/EP161208.GL
3. Brix TH, Kyvik KO, Hegedüs L. Major role of genes in the etiology of simple goiter in females: a population-based twin study. J Clin Endocrinol Metab. (1999) 84:3071–5. doi: 10.1210/jcem.84.9.5958
4. Hegedüs L, Bonnema SJ, Bennedbaek FN. Management of simple nodular goiter: current status and future perspectives. Endocr Rev. (2003) 24:102–32. doi: 10.1210/er.2002-0016
5. Abdul-Sater L, Henry M, Majdan A, Mijovic T, Franklin JH, Brandt MG, et al. What are thyroidectomy patients really concerned about? Otolaryngol Head Neck Surg. (2011) 144:685–90. doi: 10.1177/0194599811399556
6. Stang MT, Armstrong MJ, Ogilvie JB, Yip L, McCoy KL, Faber CN, et al. Positional dyspnea and tracheal compression as indications for goiter resection. Arch Surg. (2012) 147:621–6. doi: 10.1001/archsurg.2012.96
7. Watt T, Hegedüs L, Rasmussen AK, Groenvold M, Bonnema SJ, Bjorner JB, et al. Which domains of thyroid-related quality of life are most relevant? Patients and clinicians provide complementary perspectives. Thyroid (2007) 17:647–54. doi: 10.1089/thy.2007.0069
8. Netterville JL, Coleman SC, Smith JC, Smith MM, Day TA, Burkey BB. Management of substernal goiter. Laryngoscope (1998) 108:1611–7. doi: 10.1097/00005537-199811000-00005
9. Sorensen JR. The impact of surgery on quality of life, esophageal motility, and tracheal anatomy and airflow in patients with benign nodular goiter. Dan Med J. (2018) 65:B5472.
10. Sorensen JR, Lauridsen JK, Døssing H, Nguyen N, Hegedüs L, Bonnema SJ, et al. Thyroidectomy improves tracheal anatomy and airflow in patients with nodular goiter: a prospective cohort study. Eur Thyroid J. (2017) 6:307–14. doi: 10.1159/000480348
11. Lombardi CP, Raffaelli M, De Crea C, D'Alatri L, Maccora D, Marchese MR, et al. Long-term outcome of functional post-thyroidectomy voice and swallowing symptoms. Surgery (2009) 146:1174–81. doi: 10.1016/j.surg.2009.09.010
12. Sabaretnam M, Mishra A, Chand G, Agarwal G, Agarwal A, Verma AK, et al. Assessment of swallowing function impairment in patients with benign goiters and impact of thyroidectomy: a case control study. World J Surg. (2012) 36:1293–9. doi: 10.1007/s00268-012-1562-8
13. Scerrino G, Inviati A, Di Giovanni S, Paladino NC, Di Paola V, Lo Re G, et al. Esophageal motility changes after thyroidectomy; possible associations with postoperative voice and swallowing disorders: preliminary results. Otolaryngol Head Neck Surg. (2013) 148:926–32. doi: 10.1177/0194599813482299
14. Sorensen JR, Hegedüs L, Kruse-Andersen S, Godballe C, Bonnema SJ. The impact of goitre and its treatment on the trachea, airflow, oesophagus and swallowing function. A systematic review. Best Pract Res Clin Endocrinol Metab. (2014) 28:481–94. doi: 10.1016/j.beem.2014.03.002
15. Lombardi CP, Raffaelli M, D'Alatri L, De Crea C, Marchese MR, Maccora D, et al. Video-assisted thyroidectomy significantly reduces the risk of early postthyroidectomy voice and swallowing symptoms. World J Surg. (2008) 32:693–700. doi: 10.1007/s00268-007-9443-2
16. Shin JJ, Grillo HC, Mathisen D, Katlic MR, Zurakowski D, Kamani D, et al. The surgical management of goiter: part I. Preoperative evaluation. Laryngoscope (2011) 121:60–7. doi: 10.1002/lary.21084
17. Greenblatt DY, Sippel R, Leverson G, Frydman J, Schaefer S, Chen H. Thyroid resection improves perception of swallowing function in patients with thyroid disease. World J Surg. (2009) 33:255–60. doi: 10.1007/s00268-008-9837-9
18. Maung KH, Hayworth D, Nix PA, Atkin SL, England RJ. Thyroidectomy does not cause globus pattern symptoms. J Laryngol Otol. (2005) 119:973–5. doi: 10.1258/002221505775010760
19. Sorensen JR, Watt T, Cramon P, Dossing H, Hegedüs L, Bonnema SJ, et al. Quality of life after thyroidectomy in patients with nontoxic nodular goiter: a prospective cohort study. Head Neck (2017) 39:2232–40. doi: 10.1002/hed.24886
20. Cramon P, Bonnema SJ, Bjorner JB, Ekholm O, Feldt-Rasmussen U, Frendl DM, et al. Quality of life in patients with benign nontoxic goiter: impact of disease and treatment response, and comparison with the general population. Thyroid (2015) 25:284–91. doi: 10.1089/thy.2014.0433
21. Bukvic BR, Zivaljevic VR, Sipetic SB, Diklic AD, Tausanovic KM, Paunovic IR. Improvement of quality of life in patients with benign goiter after surgical treatment. Langenbecks Arch Surg. (2014) 399:755–64. doi: 10.1007/s00423-014-1221-7
22. Tae K, Kim KY, Yun BR, Ji YB, Park CW, Kim DS, et al. Functional voice and swallowing outcomes after robotic thyroidectomy by a gasless unilateral axillo-breast approach: comparison with open thyroidectomy. Surg Endosc. (2012) 26:1871–7. doi: 10.1007/s00464-011-2116-0
23. Higgins JPT, Green S. Cochrane Handbook for Systematic Revieews of Interventions. Version 5.1.0. (2011). Available online at: http://handbook.cochrane.org
24. Mackle T, Meaney J, Timon C. Tracheoesophageal compression associated with substernal goitre. Correlation of symptoms with cross-sectional imaging findings. J Laryngol Otol. (2007) 121:358–61. doi: 10.1017/s0022215106004142
25. Brinch A, Døssing H, Nguyen N, Bonnema S, Hegedüs L, Godballe C, et al. The impact of esophageal compression on goiter symptoms before and after thyroid surgery. Eur Thyroid J. (2018) 6:307–14. doi: 10.1159/000493542
26. Nam IC, Choi H, Kim ES, Mo EY, Park YH, Sun DI. Characteristics of thyroid nodules causing globus symptoms. Eur Arch Otorhinolaryngol. (2015) 272:1181–8. doi: 10.1007/s00405-015-3525-9
27. Jorgensen F, Hesse B, Gronbaek P, Fogh J, Haunso S. Abnormal oesophageal function in patients with non-toxic goiter or enlarged left atrium, demonstrated by radionuclide transit measurements. Scand J Gastroenterol. (1989) 24:1186–92. doi: 10.3109/00365528909090785
28. Glinoer D, Verelst J, Ham HR. Abnormalities of esophageal transit in patients with sporadic nontoxic goitre. Eur J Nucl Med. (1987) 13:239–43. doi: 10.1007/BF00252600
29. Scerrino G, Inviati A, Di Giovanni S, Paladino NC, Di Giovanni S, Paladino NC, et al. Long-term esophageal motility changes after thyroidectomy: associations with aerodigestive disorders. G Chir. (2017) 37:193–9. doi: 10.11138/gchir/2016.37.5.193
30. Sorensen JR, Markoew S, Dossing H, Hegedüs L, Bonnema SJ, Godballe C. Changes in swallowing symptoms and esophageal motility after thyroid surgery: a prospective cohort study. World J Surg. (2017). 42:998–1004. doi: 10.1007/s00268-017-4247-5
31. Arakawa-Sugueno L, Ferraz AR, Morandi J, Capobianco DM, Cernea CR, Sampaio MA, et al. Videoendoscopic evaluation of swallowing after thyroidectomy: 7 and 60 days. Dysphagia (2015) 30:496–505. doi: 10.1007/s00455-015-9628-z
32. Gohrbandt AE, Aschoff A, Gohrbandt B, Keilmann A, Lang H, Musholt TJ. Changes of laryngeal mobility and symptoms following thyroid surgery: 6-month follow-up. World J Surg. (2016) 40:636–43. doi: 10.1007/s00268-015-3323-y
33. Fiorentino E, Cipolla C, Graceffa G, Cusimano A, Cupido F, Lo Re G, et al. Local neck symptoms before and after thyroidectomy: a possible correlation with reflux laryngopharyngitis. Eur Arch Otorhinolaryngol. (2011) 268:715–20. doi: 10.1007/s00405-010-1394-9
34. Hyun K, Byon W, Park HJ, Park Y, Park C, Yun JS. Comparison of swallowing disorder following gasless transaxillary endoscopic thyroidectomy versus conventional open thyroidectomy. Surg Endosc. (2014) 28:1914–20. doi: 10.1007/s00464-013-3413-6
35. Rodrigues MG, Araujo VJFF, Matos LL, Hojaij FC, Simoes CA, Araujo VJFN, et al. Substernal goiter and laryngopharyngeal reflux. Arch Endocrinol Metab. (2017) 61:348–53. doi: 10.1590/2359-3997000000266
36. Holler T, Anderson J. Prevalence of voice & swallowing complaints in pre-operative thyroidectomy patients: a prospective cohort study. J Otolaryngol Head Neck Surg. (2014) 43:28. doi: 10.1186/PREACCEPT-8455644671045748
37. Lombardi CP, Raffaelli M, D'Alatri L, Marchese MR, Rigante M, Paludetti G, et al. Voice and swallowing changes after thyroidectomy in patients without inferior laryngeal nerve injuries. Surgery (2006) 140:1026–32; discussion 32–4. doi: 10.1016/j.surg.2006.08.008
38. Grover G, Sadler GP, Mihai R. Morbidity after thyroid surgery: patient perspective. Laryngoscope (2013) 123:2319–23. doi: 10.1002/lary.23850
39. Burns P, Timon C. Thyroid pathology and the globus symptom: are they related? A two year prospective trial. J Laryngol Otol. (2007) 121:242–5. doi: 10.1017/S0022215106002465
40. Krekeler BN, Wendt E, Macdonald C, Orne J, Francis DO, Sippel R, et al. Patient-reported dysphagia after thyroidectomy: a qualitative study. JAMA Otolaryngol Head Neck Surg. (2018) 144:342–8. doi: 10.1001/jamaoto.2017.3378
41. Pereira JA, Girvent M, Sancho JJ, Parada C, Sitges-Serra A. Prevalence of long-term upper aerodigestive symptoms after uncomplicated bilateral thyroidectomy. Surgery (2003) 133:318–22. doi: 10.1067/msy.2003.58
42. Kahrilas PJ, Bredenoord AJ, Fox M, Gyawali CP, Roman S, Smout AJ, et al. The Chicago classification of esophageal motility disorders, v3.0. Neurogastroenterol Motil. (2015) 27:160–74. doi: 10.1111/nmo.12477
43. Bonnema SJ, Hegedüs L. Radioiodine therapy in benign thyroid diseases: effects, side effects, and factors affecting therapeutic outcome. Endocr Rev. (2012) 33:920–80. doi: 10.1210/er.2012-1030
44. Ha EJ, Baek JH, Kim KW, Pyo J, Lee JH, Baek SH, et al. Comparative efficacy of radiofrequency and laser ablation for the treatment of benign thyroid nodules: systematic review including traditional pooling and bayesian network meta-analysis. J Clin Endocrinol Metab. (2015) 100:1903–11. doi: 10.1210/jc.2014-4077
45. Chung SR, Suh CH, Baek JH, Park HS, Choi YJ, Lee JH. Safety of radiofrequency ablation of benign thyroid nodules and recurrent thyroid cancers: a systematic review and meta-analysis. Int J Hyperthermia (2017) 33:920–30. doi: 10.1080/02656736.2017.1337936
46. Gharib H, Hegedüs L, Pacella CM, Baek JH, Papini E. Clinical review: nonsurgical, image-guided, minimally invasive therapy for thyroid nodules. J Clin Endocrinol Metab. (2013) 98:3949–57. doi: 10.1210/jc.2013-1806
47. Dossing H, Bennedbaek FN, Hegedüs L. Interstitial laser photocoagulation (ILP) of benign cystic thyroid nodules–a prospective randomized trial. J Clin Endocrinol Metab. (2013) 98:E1213–7. doi: 10.1210/jc.2013-1503
49. Moher D, Pham B, Lawson ML, Klassen TP. The inclusion of reports of randomised trials published in languages other than english in systematic reviews. Health Technol Assess. (2003) 7:1–90. doi: 10.3310/hta7410
Keywords: goiter, thyroidectomy, esophagus, swallowing, thyroid dysfunction, patient-reported outcomes, systematic review
Citation: Sorensen JR, Bonnema SJ, Godballe C and Hegedüs L (2018) The Impact of Goiter and Thyroid Surgery on Goiter Related Esophageal Dysfunction. A Systematic Review. Front. Endocrinol. 9:679. doi: 10.3389/fendo.2018.00679
Received: 24 September 2018; Accepted: 29 October 2018;
Published: 20 November 2018.
Edited by:
Giampaolo Papi, Azienda Unità Sanitaria Locale di Modena, ItalyReviewed by:
Michele Minuto, Università degli Studi di Genova, ItalyRocco Bruno, Independent Researcher, Matera, Italy
Copyright © 2018 Sorensen, Bonnema, Godballe and Hegedüs. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jesper Roed Sorensen, amVzcGVyLnJvZWQuc29yZW5zZW5AcnN5ZC5kaw==
 Jesper Roed Sorensen
Jesper Roed Sorensen Steen Joop Bonnema2
Steen Joop Bonnema2 Christian Godballe
Christian Godballe