- 1Department of Social Work, University of North Dakota, College of Nursing and Professional Disciplines, Grand Forks, ND, United States
- 2Department of Psychiatry, Ditmanson Medical Foundation, Chia-Yi Christian Hospital, Chiayi City, Taiwan
- 3Department of Psychiatry, Kaohsiung Medical University Hospital and School of Medicine, Graduate Institute of Medicine, Kaohsiung Medical University, Kaohsiung, Taiwan
The theoretical explanation of human problems is derived from the complex interplay of psychological, social, economic, political, and physical factors.
Aims: This study examined the roles of behavioral health (i.e., alcohol abuse and suicidality) and social environment (i.e., family support, school connectedness, and favorable neighborhood) and mental health [i.e., depression, anxiety, and attention deficit hyperactivity disorder (ADHD)] in predicting insomnia in adolescents in an ecological perspective.
Methods: Approximately 6445 high school students in Taiwan were administered an anonymous self-report survey. Hierarchical multiple regression was performed to examine how multidimensional social environment, behavioral health, and mental health factors were associated with insomnia in adolescents.
Results: The prevalence rate of insomnia in the sample was 30%. The results indicated that alcohol abuse (β = 0.04), suicidality (β = 0.06), depression (β = 0.29), anxiety (β = 0.14), and ADHD (β = 0.11) were positively associated with insomnia (p < 0.001), whereas family support (β = −0.06), school connectedness (β = −0.05), and favorable neighborhood (β = −0.10) were negatively associated with insomnia (p < 0.001). Sex did not predict insomnia, but age was positively associated with insomnia (β = 0.09, p < 0.001). Among all predictors of insomnia in the study, mental health factors, especially depression, play a major role on insomnia among adolescents, and is as much important as social environment factors.
Conclusion: This study demonstrated how both psychosocial variables (social environment and behavioral health) and psychological symptoms were associated with insomnia in adolescents when the demographic variables (sex and age) were controlled and provided valuable information and evidence for clinicians, social workers, and health professionals who provide support to adolescents with insomnia. Applying an ecological approach in practice can aid in understanding at individual, family, school, and community levels and in identifying the strengths and weaknesses of their interactions with each other.
Implications: This perspective enables practitioners in effectively treating problems and addressing the needs of the various levels, including the individual, family, school, and the broader community. Thus, prevention and intervention of insomnia in adolescents should focus on multidimensional risk and protective factors, including mental health, behavioral health, and social environment, in the context of an ecological system.
Introduction
Insomnia is a subjective complaint, defined as difficulty in falling asleep, trouble in staying asleep, or having poor sleep quality (Ohayon, 2002). In Taiwan, >25% (n = 36,743) of adults and 18.7% adolescents (aged 12–18 years) experienced insomnia (Kao et al., 2008; Huang et al., 2010). The most common insomnia type was the difficulty in initiating sleep, followed by early morning awakening and difficulty in maintaining sleep (Kao et al., 2008). In the United States, the age-adjusted prevalence of insomnia was 18.8% (Cunningham et al., 2015) and was 19.3% among young children and preadolescents (Calhoun et al., 2014).
Why study insomnia in adolescents? Insufficient and unsatisfactory sleep in adolescents is associated with adverse outcomes across various areas of youth development, including physical health (e.g., inflammation), cognitive and behavioral function, school performance, delinquency, substance use, depression, diminished quality of life, and even suicide ideation and self-harm behavior (Roberts et al., 2001; Sadeh et al., 2003; Curcio et al., 2006; Clinkinbeard et al., 2011; Mueller et al., 2011; Wong et al., 2011; Pasch et al., 2012; Park et al., 2016; Wang et al., 2017). Moreover, sleep is critical for all areas of adolescent development. However, sleep disruption and insufficient sleep are frequent among youth (Calhoun et al., 2014). Therefore, in addition to previous studies focusing on physical conditions such as chronic painful physical condition as a major contributive factor for insomnia (Ohayon, 2005), it is important for the present study to identify psychological, social, behavioral, and contextual barriers and aids to induce good sleep.
Considering the person-in-environment perspective, it is important to understand an individual and individual behavior in light of the environment contexts in which that person lives and acts. Thus, in addition to mental health [i.e., depression, anxiety, and attention deficit hyperactivity disorder (ADHD)], the current study also examined the roles of behavioral health (i.e., alcohol abuse and suicidality) and social environment (i.e., family support, school connectedness, and favorable neighborhood) simultaneously in predicting insomnia in adolescents. First, regarding behavioral health, alcohol abuse and suicidality are potential barriers to good sleep and risk factors for insomnia. Concerning alcohol abuse, studies have found that chronic alcoholic exposure can cause sleep disruptions, which is manifested by increasing sleep-onset latency and wakefulness (Thakkar et al., 2015). In addition, alcohol often interacts with sleep deprivation and sleep restriction to exacerbate daytime sleepiness and alcohol-induced performance impairments (Roehrs and Roth, 2001). Regarding suicidality, a meta-analysis concluded that sleep disturbance was significantly associated with an increased relative risk of suicidal ideation, suicide attempt, and suicide (Pigeon et al., 2012). Similarly, a longitudinal study identified variability in sleep timing and insomnia as warning signs of suicide ideation (Bernert et al., 2017). However, little research examined whether higher levels of suicidality was associated with higher levels of sleep problems.
Second, regarding psychosocial and contextual factors in the ecological system (Bronfenbrenner, 1979), family support, school connectedness, and favorable neighborhood are potential aids to good sleep and preventive factors of insomnia. Concerning family support, having strained family relationships was associated with more troubled sleep, whereas supportive family relationships are associated with less disturbed sleep, particularly in individuals who are in frequent contact with the family members (e.g., adolescents) (Ailshire and Burgard, 2012). Sleep troubles are most evident when family relationships are highly strained and provide inadequate emotional support. In the context of family stress, Tsai et al. (2018) reported that parental support was associated with longer sleep duration, less sleep variability, and less time spent awake during the night. It suggested that cohesive family relationships and support provide a sense of stability and security that is necessary for healthy sleep. Regarding the school-level predictors of insomnia, most of the research focuses on the effects of insomnia on school performance or the link between academic stress and insomnia (Yan et al., 2018). However, not much research has explored the relationship between school connectedness and insomnia among adolescents. In a sample of Chinese male adolescents, although sleep problems at the beginning of the school year predicted lower levels of school connectedness at the end of the school year, but school connectedness at the beginning of the school year did not predict sleep problems at the end of the school year (Bao et al., 2018). In a sample of Latino and Asian adolescents, a sense of school belongingness buffered the negative effect of overt discrimination on sleep (Huynh and Gillen-O’Neel, 2016), which suggested that school belongingness represents a positive support for adolescents that induce good sleep. Regarding community-level predictors of insomnia, adverse neighborhood and social environment (e.g., high disorder, low safety and social cohesion, violence, and noise) were associated with a higher prevalence of short sleep and insomnia (DeSantis et al., 2013; Simonelli et al., 2017). Moreover, the results of a global analysis of six countries (n = 39,590) indicated that perceived neighborhood safety is negatively associated with insomnia symptoms and poor sleep quality in the past 30 days (Hill et al., 2016). Therefore, favorable neighborhood is a potential preventive factor of insomnia.
Third, regarding mental health, depression, anxiety, and ADHD are potential barriers to good sleep and risk factors for insomnia. Concerning depression, the relationship between insomnia and depression was found to be reciprocal (Roberts and Duong, 2013; Lovato and Gradisar, 2014). Individuals with insomnia have a twofold risk of depression compared with those with no sleep difficulties (Baglioni et al., 2011). By contrast, adolescents with depression experienced significantly more wakefulness in bed, lighter sleep, and more subjective sleep disturbance (Lovato and Gradisar, 2014). Depressive symptoms in adolescents significantly predicted sleep problem development and persistence at a 4-year follow-up (Patten et al., 2000). Adolescents who reported depressive symptoms were 50% more likely to develop sleep problems than those who did not report any symptoms. Regarding anxiety, a systematic review has reported a one-way relationship where anxiety predicted excessive daytime sleepiness (Alvaro et al., 2013). Another study in youth found that anxiety preceded insomnia 73% of the time after adjustments for gender, race, and ethnicity (Johnson et al., 2006). Similarly, an epidemiological study in India revealed that anxiety was independently associated with insomnia after adjustments for other variables (Khan et al., 2018). Regarding ADHD, a study in the Netherlands showed that 43% of patients with ADHD reported significant insomnia (odds ratio = 2.66) and 41% reported short sleep duration (Wynchank et al., 2018). Another study in Ankara, Istanbul found that probability of insomnia was higher (2.7-fold) among those with probable ADHD, and both inattentiveness and hyperactivity dimensions of ADHD was related to insomnia severity (Evren et al., 2019). A clinical review paper indicated high rates of parental reports of sleep disturbances in children with ADHD (Cohen-Zion and Ancoli-Israel, 2004). Notably, children with ADHD have a fivefold increase in sleep problems than children without ADHD.
Therefore, this study expands on the previous research by simultaneously examining multidimensional psychosocial determinants, such as behavioral health (i.e., alcohol abuse and suicidality), social environment (i.e., family support, school connectedness, and favorable neighborhood), and mental health (i.e., depression, anxiety, and ADHD) to determine their association with insomnia in adolescents in the context of an ecological system. Concordant with previous research, we hypothesized that alcohol abuse, suicidality, depression, anxiety, and ADHD would be the risk factors for insomnia in adolescents, after control for sex and age. By contrast, family support, school connectedness, and conducive neighborhood would be the preventive factors associated with insomnia.
Materials and Methods
Participants
The participants in this study were enrolled from the 2009 Project for the Health of Children and Adolescents in Southern Taiwan, a research program studying the mental health status of children and adolescents living in four counties and three metropolitan areas in southern Taiwan (Yen et al., 2010a). In 2009, there were 254,130 students in 205 junior high schools and 202,883 students in 143 senior high/vocational schools in this area. On the basis of the definitions of urban and rural districts in the Taiwan-Fukien Demographic Fact Book (Ministry of the Interior, 2002), a stratified random sampling strategy was used to ensure that there was proportional representation of districts and schools. Two-stage random cluster sampling was used to select schools and classes for the study. Five junior high schools and five senior high or vocational schools were randomly selected from urban districts. Similarly, five junior high schools and four senior high or vocational schools were randomly selected from the rural districts. The classes were randomly selected from these schools. All students in the selected classes were invited to participate in the study, except the students with special needs. Subsequently, 6703 students from grades 7 to 12 participated in the study.
Procedure
This study was approved by the Institutional Review Board (IRB) of Kaohsiung Medical University before sampling and data collection. The research presents no more than minimal risk of harm to subjects and involves no procedures for which written consent is normally required outside of the research context. And, the data were recorded in a manner that individuals cannot be identified in the anonymous survey. The waiver of written parental consent form did not adversely affect the rights and welfare of the subjects and was approved by IRB. The passive parental consent was used. Prior to the administration of the survey, parents/guardians of all student participants received written notice letter that their child would be recruited to participate in the study and explaining the study purpose and procedure, emphasizing the voluntary and confidential nature of the study. Parents were given the opportunity to exclude their daughter/son from participation in the study and asked to respond within 3 days. Students took the letter home for their parents or guardians, who were given a choice to call the researchers, write in the school communications book, or ask their children to directly, all convey to their refusal for their children to join the study. In addition, the students were given the liberty to refuse participation in this study by returning blank questionnaires along with those from other students.
Measures
Based on the ecological system theory, we included three layers of social environment as predictors in the study: family support, school connectedness, and favorable neighborhood. We assessed the students’ experiences with insomnia, mental health (i.e., depression, anxiety, and ADHD), behavioral health (i.e., alcohol use and suicidality), and social environment (i.e., family support, school connectedness, and favorable neighborhood) by using the self-reported surveys. A pilot study (n = 76) was conducted to ensure adequate reliability of all research instruments by performing a 2-week test–retest reliability.
Insomnia
The 8-item Athens Insomnia Scale (AIS-8) was used to assess the severity of subjective insomnia over the preceding month (Soldatos et al., 2000). The items of the AIS-8 correspond to the taxonomies for the diagnosis of insomnia per the International Classification of Diseases, Tenth Edition. The first five items assess difficulty with sleep induction, awakening during the night, early morning awakening, total sleep time, and overall quality of sleep. The last three items assess the next-day consequences of any insomnia, including problems with a sense of well-being, functioning, and daytime sleepiness. The Taiwanese version of the AIS-8 scale has been validated in previous study (Chung et al., 2011; Sun et al., 2011). Each item of the AIS-8 was rated on a four-point rating scale from 0 to 3 with a higher score indicating severe insomnia. The mean score was calculated. The Cronbach’s alpha in the present study was 0.69, and the 2-week test–retest reliability was 0.72 (p < 0.001).
Depression
The 20-item Mandarin-Chinese version of the Center for Epidemiological Studies-Depression (CES-D) Scale was used to assess the frequency of depressive symptoms in the previous week (Radloff, 1977; Chien and Cheng, 1985). Each item of the CES-D was rated on a 4-point rating scale from 0 to 3. A higher score indicated severe depression. The mean score was calculated. The Cronbach’s alpha for the CES-D was 0.89, and the 2-week test–retest reliability was 0.78.
Anxiety
We used the Taiwanese Version of the Multidimensional Anxiety Scale for Children (MASC-T) to assess the participants’ self-reported anxiety symptoms (March, 1997; Yen et al., 2010b). The MASC-T consisted of 39 items answered on a 4-point Likert scale from 0 to 3. A higher score represented a severe level of anxiety. The mean score was calculated. The Cronbach’s alpha for the MASC-T in the present study was 0.89.
ADHD
An 18-item self-report ADHD scale was modified from the Vanderbilt ADHD Diagnostic Parent Rating Scale (Wolraich et al., 2003) and represented the 18 diagnostic symptoms of ADHD from the DSM-IV, Text Revision (American Psychiatric and Association, 2000). Items 1–9 measure inattention symptoms, and items 10–18 measure hyperactivity and impulsivity symptoms. Taiwanese version of ADHD scale has been validated in previous study (Gau et al., 2008). Participants rated their symptoms on a 4-point Likert scale from 0 to 3 with a higher score indicating symptom severity. The mean score was calculated. The Cronbach’s alpha was 0.88.
Alcohol Abuse
The 5-item alcohol abuse scale was adapted from the CRAFFT substance abuse screening test to assess problematic alcohol use in adolescents (Knight et al., 2002). We removed one item “CAR” to increase the reliability. The “yes” answer was scored as 1 and “no” as 0. A higher total score on the scale represented a severe level of alcohol abuse. The Cronbach’s alpha for the alcohol abuse scale was 0.65.
Suicidality
The 5-item questionnaire from the epidemiological version of the Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS-E; Puig-Antich and Chambers, 1978) was used to assess suicidal ideation and attempt in the preceding year. Questions were as follows: (1) “Has there ever been a period of 2 weeks or longer when you thought a lot about death, including thoughts of your death, somebody else’s death, or death in general?” (2) “Has there ever been a period of 2 weeks or longer when you had a desire to die?” (3) “Have you ever thought of attempting suicide?” (4) “Have you had a suicidal plan?” (5) “Have you ever attempted suicide?” Each question elicited a “yes” or “no” answer. In a previous study in Taiwan, the Cohen’s kappa coefficient of agreement (j) between participants’ self-reported suicide attempts and their parents’ reports was 0.54 (p < 0.001) (Tang et al., 2009). The Cronbach’s alpha in this study was 0.79.
Family Support
The 5-item Chinese version of the Family APGAR Index (Smilkstein, 1978; Chen et al., 1980) was applied to measure participants’ satisfaction with aspects of family support on a 4-point rating scale from 0 to 3. A higher score represented a higher level of family support. The mean score was calculated. The Cronbach’s alpha in the present study was 0.85.
School Connectedness
The level of connectedness to school was assessed based on five statements: “I enjoy my school life,” “I get along well with my teachers,” “I get along well with my schoolmates,” “I feel that I am popular,” and “I feel no interest to interact with friends or schoolmates (revise coded).” The participants scored the items on a 4-point Likert scale from 0 to 3, with a higher score indicating more agreement with the statements. To make the interpretation easier, we reverse-coded these items and calculated the sum score. After recoding, a higher score indicating a higher level of school connectedness. The mean score was calculated. The Cronbach’s alpha was 0.68.
Favorable Neighborhood
The 8-item favorable living environment scale was adapted from the Taiwanese Quality of Life Questionnaire for Adolescents (Fuh et al., 2005) to assess experiences in the preceding 2 weeks. A sample question was as follows: “Do you feel safe and protected in your home?” The participants reported their experiences on a 5-point rating scale from 0 to 4. A higher score indicated better quality of life over the preceding 2 weeks. The mean score was calculated. The Cronbach’s alpha in this study was 0.89.
Analysis Plan
Statistical analysis was performed using the SPSS Statistical Package for Windows, version 24. First, descriptive statistics were used to assess the distribution of adolescents’ insomnia, behavioral health (i.e., alcohol abuse and suicidality), social environment (i.e., family support, school connectedness, and favorable neighborhood), and mental health (i.e., depression, anxiety, and ADHD) based on the ecological system theory. Second, we conducted correlational analyses using the Pearson coefficient of correlation to illustrate interrelationships between each of the variables. Third, we performed hierarchical regression to examine the effects of behavioral health, social environment, and mental health on insomnia in adolescents, after control for age and sex.
Results
Descriptive Statistics and Correlations
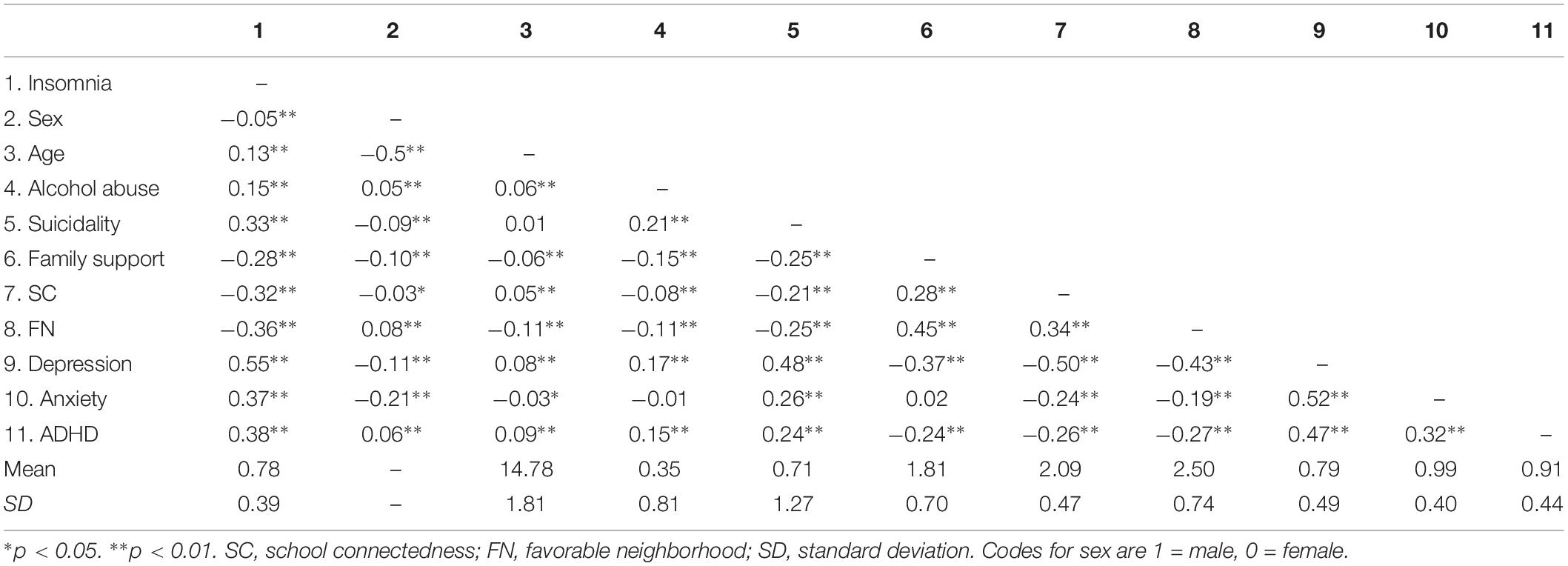
Overall, 6445 participants completed the research questionnaires without withdrawal, of which 52% were girls and 48% were boys. Table 1 presents the correlation coefficients of all study variables and the descriptive statistics of the means and standard deviations of the variables. The prevalence rate of insomnia in the sample was 30%, based on the optimal cut-offs for AIS-8 (Chung et al., 2011).
Effects of Psychosocial Determinants on Insomnia
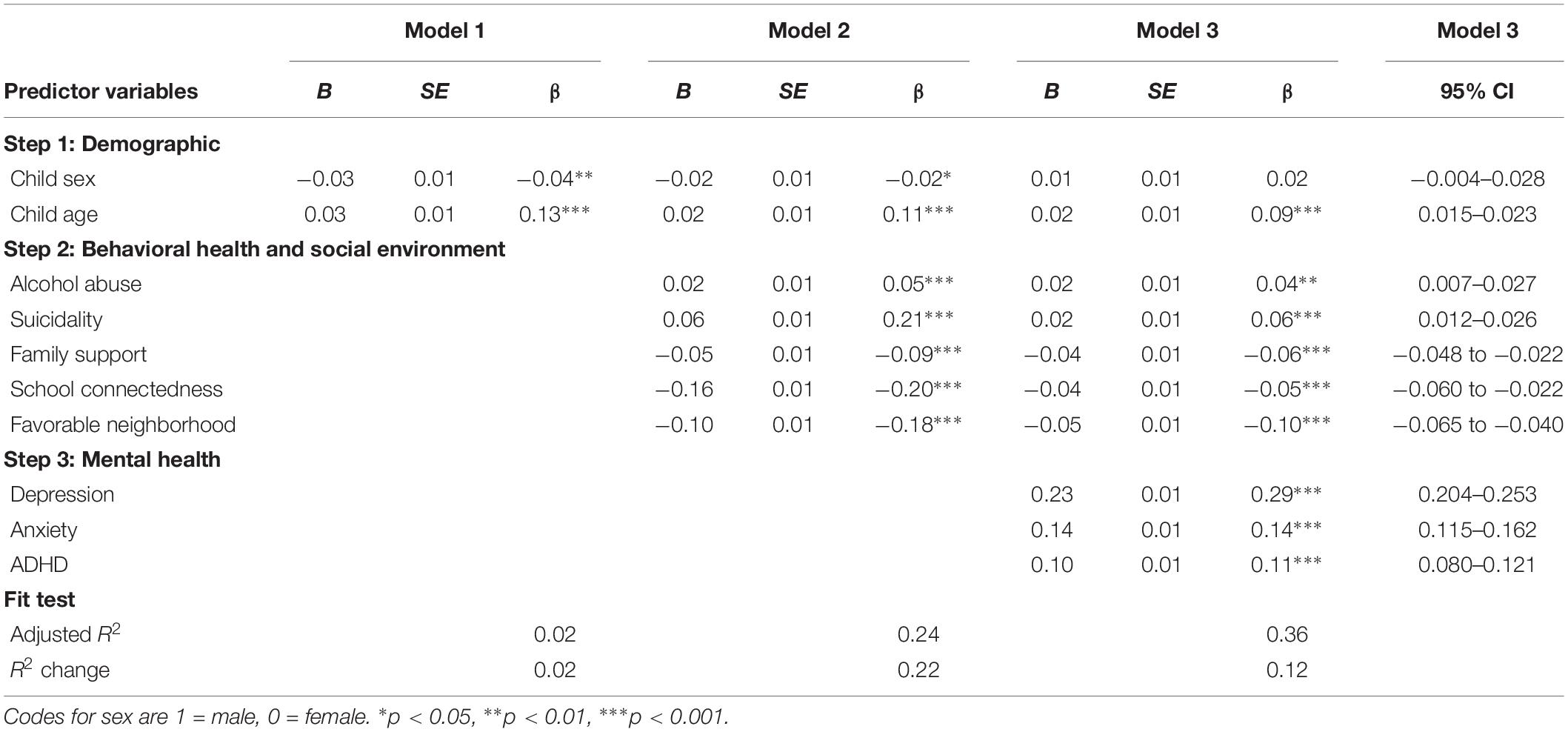
Prior to conducing a hierarchical multiple regression, the relevant assumptions of this statistical analysis were tested. Firstly, a sample size of 6445 was deemed adequate given 10 independent variables to be included in the analysis (Tabachnick et al., 2007). The assumption of singularity was also met as the independent variables were not a combination of other independent variables. An examination of correlations (Table 1) revealed that no independent variables were highly correlated, with the exception of depression and anxiety (r = 0.52). As the collinearity statistics (i.e., Tolerance and VIF) were all within accepted limits, the result indicated that multicollinearity was not a concern (Hair et al., 1998). The residual plots, the normal probability plot, and scatter plots indicated that the assumptions of normality, linearity, and homoscedasticity were all satisfied (Hair et al., 1998; Pallant, 2013; Supplementary Appendix 1). And, the value of Durbin–Watson test statistic was 2 that indicated the residuals were uncorrelated (Durbin and Watson, 1951). Hierarchical regression analyses were used to examine whether adolescents’ two behavioral health and three social environment factors, and three mental health factors were significant contributors to insomnia, after control for sex and age. Table 2 summarizes the results from the hierarchical regression. The demographic variables (sex and age) were entered into the regression model of insomnia in the first step (Model 1). Behavioral health and social environment variables (i.e., alcohol abuse, suicidality, family support, school connectedness, and favorable neighborhood) were entered into the regression model in the second step (Model 2). Mental health variables (i.e., depression, anxiety, and ADHD) were entered in the third and final step (Model 3).
The results showed that adolescents’ sex and age significantly contributed to the regression model, F(2,6388) = 61.18, p < 0.001 and accounted for 2% of the variance in insomnia. Introducing two behavioral health and three social environmental variables significantly explained an additional 22% of the variance in insomnia and this change in R2 was significant, F(5,6383) = 371.98, p < 0.001. Finally, the addition of three mental health variables to the regression model explained an additional 12% of the variance in insomnia and this change in R2 was also significant, F(3,6380) = 403.69, p < 0.001 (ΔR2 = 0.12, p < 0.001). Taken together, in the final model, these demographic, behavioral health variables, social environment variables, and mental health variables significantly explained 36% of the variance in insomnia. The sum of square was 345.71 and the sum of square error was 610.86. A Mallow’s Cp value (Cp = 11) that was close to the number of predictors plus the constant indicated that the model produced relatively precise and unbiased estimates. The regression coefficients indicated that alcohol abuse (β = 0.04), suicidality (β = 0.06), depression (β = 0.29), anxiety (β = 0.14), and ADHD (β = 0.11) were positively associated with insomnia (p < 0.001), whereas family support (β = −0.06), school connectedness (β = −0.05), and favorable neighborhood (β = −0.10) were negatively associated with insomnia (p < 0.001). Therefore, adolescents who reported higher levels of alcohol abuse, suicidality, depression, anxiety, and ADHD were more likely to have insomnia. In contrast, adolescents who perceived higher levels of family support, school connectedness, and favorable neighborhood were less likely to have insomnia. Sex did not predict insomnia. Age was positively associated with insomnia (β = 0.09, p < 0.001). Older adolescents reported more insomnia than younger adolescents. Among all predictors of insomnia in the study, mental health factors, especially depression, play a major role on insomnia among adolescents, and is as much important as social environment factors. When applying stepwise elimination approach, depression was the best predictor that accounted for the most of the variance in insomnia [ΔR2 = 0.30, p < 0.001; F(1,6389) = 2775.41, p < 0.001], followed by ADHD and favorable neighborhood, and school connectedness accounted for the least of the variance in insomnia.
Discussion
The present study extends the previous research regarding the impact of behavioral and mental health and social environment on insomnia in adolescents. This study addressed the increasing problems of insomnia in adolescents and added to the fund of knowledge by analyzing how multidimensional factors contribute to insomnia in adolescents at individual, family, school, and community levels in the ecological system. The results supported our hypotheses. First, we found empirical support that adolescent alcohol abuse and suicidality were positively associated with insomnia, after control for age, sex, and other factors. Second, we revealed that family support, school connectedness, and favorable neighborhood were negatively associated with adolescent insomnia, after control for demographics and other covariates. Third, we found that mental health problems such as depression, anxiety, and ADHD were positively associated with insomnia when controlling the demographics and other covariates. Both the behavioral health and social environment variables and the mental health variables explained the significant variance in the model.
Behavioral and Mental Health and Insomnia
Regarding behavioral health problems, the study confirmed the relationship between alcohol abuse and insomnia among adolescents in Taiwan – concordant with previous research on adult samples (Chaudhary et al., 2015). Adolescents with alcohol abuse issues are at a higher risk of a chronic predicament of insomnia. The correlation between alcohol abuse and insomnia was also found in a Polish study sample that indicated >60% of alcohol-dependent patients screened positive for insomnia (Zhabenko et al., 2012), and insomnia was also found to be prevalent in 75% of alcohol-dependent adults in a US sample (Chaudhary et al., 2015). On the other hand, sleep disturbances may place adolescents without alcohol abuse issues at a high risk of alcohol abuse (Hasler et al., 2014). Furthermore, concordant with a previous research of an extensive school-based survey and a longitudinal study in the United States (Roberts et al., 2001; Wong et al., 2011), this study on a Taiwanese sample confirmed that suicidality was associated with insomnia among the adolescents, after accounting for depression, anxiety, PTSD, and alcohol abuse. Regarding mental health problems, most studies found strong relationships with insomnia in adults or older adults (Cho et al., 2008). For example, a Swedish study of a general population sample found that depression at its baseline is related to subsequent symptoms of insomnia (Jansson-Fröjmark and Lindblom, 2008). In addition, a prospective study in the United Kingdom on an adult sample revealed that depression predicted the incidence of insomnia at 1-year follow-up (Morphy et al., 2007). This study conducted in Taiwan showed that depression, anxiety, and ADHD significantly affected insomnia in adolescents, after control for the effects of the social environment and behavioral health.
Social Environment and Insomnia
Considering that behavioral and mental health problems were the risk factors for insomnia, we examined the potential preventive factors in the three social environment levels that were related to low insomnia levels. This relationship has not been explored much previously. We hypothesized three preventive factors in the context of family, school, and community to represent the social environment in the ecological system. The results supported the hypotheses that higher family support, school connectedness, and a conducive neighborhood contributed to low risk of insomnia among adolescents. Based on the stress-buffering model, social support protected individuals from the negative psychological consequences of a wide range of stressful events that can help reduce insomnia (Cohen and Wills, 1985; Cohen et al., 2000). Family support and school connectedness are two essential types of social support for adolescents. Adolescents perceived a high level of social support when they felt that they were cared for, loved, held in high esteem, and were members of a network of mutual obligations. These perceptions enabled the adolescents to cope and adapt in life (Cobb, 1976), and consequently reduced sleep problems. Concordant with a previous US study on an adult sample (Ailshire and Burgard, 2012), we confirmed that perceived family support was associated with less insomnia in adolescents. The relationship between school connectedness and insomnia among the adolescents has not been researched much, but previous research suggested that school belongingness/connectedness may be a positive support for the adolescents (Huynh and Gillen-O’Neel, 2016). Our results support the hypothesis that adolescents who perceived higher school connectedness had fewer sleep problems, such as insomnia. Finally, our study on Taiwanese adolescents found that favorable neighborhood was associated with less insomnia, which was concordant with a previous research in the United States on adult samples that found higher prevalence of insomnia related to adverse neighborhood (Hill et al., 2009; DeSantis et al., 2013; Simonelli et al., 2017).
Strengths and Limitations
A strength of our study is the use of an ecological perspective to examine the roles of mental health and multidimensional psychosocial determinants, such as behavioral health (i.e., alcohol abuse and suicidality) and social environment (i.e., family support, school connectedness, and favorable neighborhood), in insomnia in adolescents. Holistic thinking can provide a paradigm to understand how various systems and their interactions can contribute to an individual’s problem and behavior. Another strength is the large size of the study sample. By contrast, a limitation of the study is its cross-sectional design that can only draw conclusions regarding the correlation between the study variables and not interpret the cause-and-effect. Moreover, some of the variables may have a reciprocal relationship with insomnia. For example, depression predicts insomnia, whereas insomnia also predicts depression. Future research may be warranted to examine the reciprocal relationships between the psychosocial variables and insomnia and identify patterns of a negative cycle.
Implications
The study provides valuable information and evidence for clinicians, social workers, and health professionals providing support to adolescents with insomnia. Applying an ecological approach in practice aids in understanding the issues at individual, family, school, and community levels and identify the strengths and weaknesses of the interactions between them. This perspective allows the practitioner to effectively treat problems and address the needs of the various levels, including the individual, family, school, and the broader community. The prevention and intervention of insomnia in the adolescents should focus on multidimensional risks and preventive factors, including mental health, behavioral health, and social environment in the context of an ecological system.
Data Availability
The raw data supporting the conclusions of this manuscript will be made available by the authors, without undue reservation, to any qualified researcher.
Ethics Statement
This study was approved by the IRB of Kaohsiung Medical University before sampling and data collection. Before conducting the study, we prepared a leaflet explaining the study purpose and procedure, emphasizing the voluntary and confidential nature of the study. Students took the leaflets home for their parents or guardians, who were given a choice to call the researchers, write in the school communications book, or ask their children to directly, all convey to their refusal for their children to join the study. In addition, the students were given the liberty to refuse participation in this study by returning blank questionnaires along with those from other students.
Author Contributions
Y-PH: conceptualization, methodology, software, validation, formal analysis, investigation, resources, data curation, writing – original draft preparation, review and editing, and visualization. W-HL and C-FY: conceptualization, validation, investigation, resources, data curation, review and editing, supervision, project administration, and funding acquisition.
Funding
This research was funded by the Ministry of Science and Technology, Taiwan (Grant Numbers: NSC98-2410-H-037-005-MY3 and 99-2314-B-037-028-MY2).
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fnins.2019.00848/full#supplementary-material
References
Ailshire, J. A., and Burgard, S. A. (2012). Family relationships and troubled sleep among US adults: examining the influences of contact frequency and relationship quality. J. Health Soc. Behav. 53, 248–262. doi: 10.1177/0022146512446642
Alvaro, P. K., Roberts, R. M., and Harris, J. K. (2013). A systematic review assessing bidirectionality between sleep disturbances, anxiety, and depression. Sleep 36, 1059–1068. doi: 10.5665/sleep.2810
American Psychiatric and Association (2000). Diagnostic and Statistical Manual of Mental Disorders, 4th Edn. Washington DC: American Psychiatric Association.
Baglioni, C., Battagliese, G., Feige, B., Spiegelhalder, K., Nissen, C., Voderholzer, U., et al. (2011). Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J. Affect. Disord. 135, 10–19. doi: 10.1016/j.jad.2011.01.011
Bao, Z., Chen, C., Zhang, W., Jiang, Y., Zhu, J., and Lai, X. (2018). School connectedness and chinese adolescents’ sleep problems: a cross-lagged panel analysis. J. Sch. Health 88, 315–321. doi: 10.1111/josh.12608
Bernert, R. A., Hom, M. A., Iwata, N. G., and Joiner, T. E. (2017). Objectively assessed sleep variability as an acute warning sign of suicidal ideation in a longitudinal evaluation of young adults at high suicide risk. J. Clin. Psychiatry 78, e678–e687. doi: 10.4088/JCP.16m11193
Bronfenbrenner, U. (1979). The Ecology Of Human Development. Cambridge, MA: Harvard university press.
Calhoun, S. L., Fernandez-Mendoza, J., Vgontzas, A. N., Liao, D., and Bixler, E. O. (2014). Prevalence of insomnia symptoms in a general population sample of young children and preadolescents: gender effects. Sleep Med. 15, 91–95. doi: 10.1016/j.sleep.2013.08.787
Chaudhary, N. S., Kampman, K. M., Kranzler, H. R., Grandner, M. A., Debbarma, S., and Chakravorty, S. (2015). Insomnia in alcohol dependent subjects is associated with greater psychosocial problem severity. Addict. Behav. 50, 165–172. doi: 10.1016/j.addbeh.2015.06.021
Chen, Y. C., Hsu, C. C., Hsu, S. H., and Lin, C. C. (1980). A preliminary study of family APGAR index. Gaoxiong Yi Xue Ke Xue Za Zhi 21, 210–217.
Chien, C. P., and Cheng, T. A. (1985). Depression in taiwan: epidemiological survey utilizing CES-D. Seishin Shinkeigaku Zasshi 87, 335–338.
Cho, H. J., Lavretsky, H., Olmstead, R., Levin, M. J., Oxman, M. N., and Irwin, M. R. (2008). Sleep disturbance and depression recurrence in community-dwelling older adults: a prospective study. Am. J. Psychiatry 165, 1543–1550. doi: 10.1176/appi.ajp.2008.07121882
Chung, K. F., Kan, K. K. K., and Yeung, W. F. (2011). Assessing insomnia in adolescents: comparison of insomnia severity index, athens insomnia scale and sleep quality index. Sleep Med. 12, 463–470. doi: 10.1016/j.sleep.2010.09.019
Clinkinbeard, S. S., Simi, P., Evans, M. K., and Anderson, A. L. (2011). Sleep and delinquency: does the amount of sleep matter? J. Youth Adolesc. 40, 916–930. doi: 10.1007/s10964-010-9594-6
Cobb, S. (1976). Social support as a moderator of life stress. Psychosomatic Med. 38, 300–314. doi: 10.1097/00006842-197609000-00003
Cohen, S., Gottlieb, B. H., and Underwood, L. G. (2000). “Social relationships and health,” in Social Support Measurement And Intervention: A Guide For Health And Social Scientists, eds S. Cohen, L. G. Underwood, and B. H. Gottlieb (New York, NY: Oxford University Press), 3–25.
Cohen, S., and Wills, T. A. (1985). Stress, social support, and the buffering hypothesis. Psychol. Bull. 98, 310–357. doi: 10.1037/0033-2909.98.2.310
Cohen-Zion, M., and Ancoli-Israel, S. (2004). Sleep in children with attention-deficit hyperactivity disorder (ADHD): a review of naturalistic and stimulant intervention studies. Sleep Med. Rev. 8, 379–402. doi: 10.1016/j.smrv.2004.06.002
Cunningham, T. J., Ford, E. S., Chapman, D. P., Liu, Y., and Croft, J. B. (2015). Independent and joint associations of race/ethnicity and educational attainment with sleep-related symptoms in a population-based US sample. Prev. Med. 77, 99–105. doi: 10.1016/j.ypmed.2015.05.008
Curcio, G., Ferrara, M., and De Gennaro, L. (2006). Sleep loss, learning capacity and academic performance. Sleep Med. Rev. 10, 323–337. doi: 10.1016/j.smrv.2005.11.001
DeSantis, A. S., Diez Roux, A. V., Moore, K., Baron, K. G., Mujahid, M. S., and Nieto, F. J. (2013). Associations of neighborhood characteristics with sleep timing and quality: the multi-ethnic study of atherosclerosis. Sleep 36, 1543–1551. doi: 10.5665/sleep.3054
Durbin, J., and Watson, G. S. (1951). Testing for serial correlation in least squares regression. II. Biometrika 38, 159–177.
Evren, B., Evren, C., Dalbudak, E., Topcu, M., and Kutlu, N. (2019). The impact of depression, anxiety, neuroticism, and severity of Internet addiction symptoms on the relationship between probable ADHD and severity of insomnia among young adults. Psychiatry Res. 271, 726–731. doi: 10.1016/j.psychres.2018.12.010
Fuh, J. L., Wang, S. J., Lu, S. R., and Juang, K. D. (2005). Assessing quality of life for adolescents in taiwan. Psychiatry Clin. Neurosci. 59, 11–18. doi: 10.1111/j.1323-1316.2005.01306.x
Gau, S. S. F., Shang, C. Y., Liu, S. K., Lin, C. H., Swanson, J. M., Liu, Y. C., et al. (2008). Psychometric properties of the chinese version of the swanson, nolan, and pelham, version IV scale–parent form. Int. J. Methods Psychiatr. Res. 17, 35–44. doi: 10.1002/mpr.237
Hair, J. F., Anderson, R. E., Tatham, R. L., and Black, W. C. (1998). Multivariate Data Analysis. Jersey City, NJ: Englewood Cliff.
Hasler, B. P., Martin, C. S., Wood, D. S., Rosario, B., and Clark, D. B. (2014). A longitudinal study of insomnia and other sleep complaints in adolescents with and without alcohol use disorders. Alcoholism 38, 2225–2233. doi: 10.1111/acer.12474
Hill, T. D., Burdette, A. M., and Hale, L. (2009). Neighborhood disorder, sleep quality, and psychological distress: testing a model of structural amplification. Health Place 15, 1006–1013. doi: 10.1016/j.healthplace.2009.04.001
Hill, T. D., Trinh, H. N., Wen, M., and Hale, L. (2016). Perceived neighborhood safety and sleep quality: a global analysis of six countries. Sleep Med. 18, 56–60. doi: 10.1016/j.sleep.2014.12.003
Huang, Y. S., Wang, C. H., and Guilleminault, C. (2010). An epidemiologic study of sleep problems among adolescents in north taiwan. Sleep Med. 11, 1035–1042. doi: 10.1016/j.sleep.2010.04.009
Huynh, V. W., and Gillen-O’Neel, C. (2016). Discrimination and sleep: the protective role of school belonging. Youth Soc. 48, 649–672. doi: 10.1177/0044118x13506720
Jansson-Fröjmark, M., and Lindblom, K. (2008). A bidirectional relationship between anxiety and depression, and insomnia? a prospective study in the general population. J. Psychos. Res. 64, 443–449. doi: 10.1016/j.jpsychores.2007.10.016
Johnson, E. O., Roth, T., and Breslau, N. (2006). The association of insomnia with anxiety disorders and depression: exploration of the direction of risk. J. Psychiatr. Res. 40, 700–708. doi: 10.1016/j.jpsychires.2006.07.008
Kao, C. C., Huang, C. J., Wang, M. Y., and Tsai, P. S. (2008). Insomnia: prevalence and its impact on excessive daytime sleepiness and psychological well-being in the adult taiwanese population. Q. Life Res. 17, 1073–1080. doi: 10.1007/s11136-008-9383-9
Khan, I. W., Juyal, R., Shikha, D., and Gupta, R. (2018). Generalized anxiety disorder but not depression is associated with insomnia: a population based study. Sleep Science 11, 166–173. doi: 10.5935/1984-0063.20180031
Knight, J. R., Sherritt, L., Shrier, L. A., Harris, S. K., and Chang, G. (2002). Validity of the CRAFFT substance abuse screening test among adolescent clinic patients. Arch. Pediatr. Adolesc. Med. 156, 607–614.
Lovato, N., and Gradisar, M. (2014). A meta-analysis and model of the relationship between sleep and depression in adolescents: recommendations for future research and clinical practice. Sleep Med. Rev. 18, 521–529. doi: 10.1016/j.smrv.2014.03.006
March, J. S. (1997). Multidimensional Anxiety Scale For Children. North Tonawanda, NY: Multi-Health Systems Inc.
Ministry of the Interior (2002). 2001 Taiwan-Fukien Demographic Fact Book: Republic of China. Taiwan: Executive Yuan, Taipei.
Morphy, H., Dunn, K. M., Lewis, M., Boardman, H. F., and Croft, P. R. (2007). Epidemiology of insomnia: a longitudinal study in a UK population. Sleep 30, 274–280.
Mueller, C. E., Bridges, S. K., and Goddard, M. S. (2011). Sleep and parent-family connectedness: links, relationships and implications for adolescent depression. J. Fam. Stud. 17, 9–23. doi: 10.5172/jfs.2011.17.1.9
Ohayon, M. M. (2002). Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med. Rev. 6, 97–111. doi: 10.1053/smrv.2002.0186
Ohayon, M. M. (2005). Relationship between chronic painful physical condition and insomnia. J. Psychiatr. Res. 39, 151–159. doi: 10.1016/j.jpsychires.2004.07.001
Park, H., Tsai, K. M., Dahl, R. E., Irwin, M. R., McCreath, H., Seeman, T. E., et al. (2016). Sleep and inflammation during adolescence. Psychos. Med. 78, 677–685. doi: 10.1097/PSY.0000000000000340
Pasch, K. E., Latimer, L. A., Cance, J. D., Moe, S. G., and Lytle, L. A. (2012). Longitudinal bi-directional relationships between sleep and youth substance use. J. Youth Adolesc. 41, 1184–1196. doi: 10.1007/s10964-012-9784-5
Patten, C. A., Choi, W. S., Gillin, J. C., and Pierce, J. P. (2000). Depressive symptoms and cigarette smoking predict development and persistence of sleep problems in US adolescents. Pediatrics 106, e23–e23. doi: 10.1542/peds.106.2.e23
Pigeon, W. R., Pinquart, M., and Conner, K. (2012). Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J. Clin. Psychiatry 73, e1160–e1167. doi: 10.4088/JCP.11r07586
Puig-Antich, J., and Chambers, W. (1978). The Schedule For Affective Disorders And Schizophrenia For School Age Children (Kiddie-SADS). New York, NY: New York State Psychiatric Institute.
Radloff, L. S. (1977). The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Measure. 1, 385–401. doi: 10.1177/014662167700100306
Roberts, R. E., and Duong, H. T. (2013). Depression and insomnia among adolescents: a prospective perspective. J. Affect. Disord. 148, 66–71. doi: 10.1016/j.jad.2012.11.049
Roberts, R. E., Roberts, C. R., and Chen, I. G. (2001). Functioning of adolescents with symptoms of disturbed sleep. J. Youth Adolesc. 30, 1–18. doi: 10.1023/a%3A1005230820074
Roehrs, T., and Roth, T. (2001). Sleep, sleepiness, and alcohol use. Alcohol. Res. Health 25, 101–101.
Sadeh, A., Gruber, R., and Raviv, A. (2003). The effects of sleep restriction and extension on school-age children: what a difference an hour makes. Child Dev. 74, 444–455. doi: 10.1111/1467-8624.7402008
Simonelli, G., Dudley, K. A., Weng, J., Gallo, L. C., Perreira, K., Shah, N. A., et al. (2017). Neighborhood factors as predictors of poor sleep in the sueno ancillary study of the hispanic community health study/study of latinos. Sleep 40, 1–8. doi: 10.1093/sleep/zsw025
Smilkstein, G. (1978). The family APGAR: a proposal for a family function test and its use by physicians. J. Fam. Practice 6, 1231–1239.
Soldatos, C. R., Dikeos, D. G., and Paparrigopoulos, T. J. (2000). Athens insomnia scale: validation of an instrument based on ICD-10 criteria. J. Psychos. Res. 48, 555–560. doi: 10.1016/s0022-3999(00)00095-7
Sun, J. L., Chiou, J. F., and Lin, C. C. (2011). Validation of the taiwanese version of the athens insomnia scale and assessment of insomnia in taiwanese cancer patients. J. Pain Symptom Manag. 41, 904–914. doi: 10.1016/j.jpainsymman.2010.07.021
Tabachnick, B. G., Fidell, L. S., and Ullman, J. B. (2007). Using Multivariate Statistics. Boston, MA: Pearson.
Tang, T. C., Ko, C. H., Yen, J. Y., Lin, H. C., Liu, S. C., Huang, C. F., et al. (2009). Suicide and its association with individual, family, peer and school factors in a population of 10,233 adolescents in southern Taiwan. Suicide Life Threaten. Behav. 39, 91–102. doi: 10.1521/suli.2009.39.1.91
Thakkar, M. M., Sharma, R., and Sahota, P. (2015). Alcohol disrupts sleep homeostasis. Alcoholism 49, 299–310. doi: 10.1016/j.alcohol.2014.07.019
Tsai, K. M., Dahl, R. E., Irwin, M. R., Bower, J. E., McCreath, H., Seeman, T. E., et al. (2018). The roles of parental support and family stress in adolescent sleep. Child Dev. 89, 1577–1588. doi: 10.1111/cdev.12917
Wang, C. C., Liu, T. L., Hsiao, R. C., Wu, Y. Y., Hu, H. F., and Yen, C. F. (2017). The relationships of insomnia and short and long nocturnal sleep durations with quality of life and the moderating effects of sex and age in taiwanese adolescents. Neuropsychiatry 7, 217–223.
Wolraich, M. L., Lambert, W., Doffing, M. A., Bickman, L., Simmons, T., and Worley, K. (2003). Psychometric properties of the vanderbilt ADHD diagnostic parent rating scale in a referred population. J. Pediatr. Psychol. 28, 559–568. doi: 10.1093/jpepsy/jsg046
Wong, M. M., Brower, K. J., and Zucker, R. A. (2011). Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J. Psychiatr. Res. 45, 505–511. doi: 10.1016/j.jpsychires.2010.09.005
Wynchank, D., ten Have, M., Bijlenga, D., Penninx, B. W., Beekman, A. T., Lamers, F., et al. (2018). The association between insomnia and sleep duration in adults with attention-deficit hyperactivity disorder: results from a general population study. J. Clin. Sleep Med. 14, 349–357. doi: 10.5664/jcsm.6976
Yan, Y. W., Lin, R. M., Su, Y. K., and Liu, M. Y. (2018). The relationship between adolescent academic stress and sleep quality: a multiple mediation model. Soc. Behav. Pers. 46, 63–77. doi: 10.2224/sbp.6530
Yen, C. F., Ko, C. H., Wu, Y. Y., Yen, J. Y., Hsu, F. C., and Yang, P. (2010a). Normative data on anxiety symptoms on the multidimensional anxiety scale for children in taiwanese children and adolescents: differences in sex, age, and residence and comparison with an american sample. Child Psychiatry Hum. Dev. 41, 614–623. doi: 10.1007/s10578-010-0191-4
Yen, C. F., Yang, P., Wu, Y. Y., Hsu, F. C., and Cheng, C. P. (2010b). Factor structure, reliability and validity of the taiwanese version of the multidimensional anxiety scale for children. Child Psychiatry Hum. Dev. 41, 342–352. doi: 10.1007/s10578-010-0172-7
Keywords: insomnia, suicidality, alcohol abuse, family support, school connectedness, favorable neighborhood, mental health, adolescent
Citation: Hsieh Y-P, Lu W-H and Yen C-F (2019) Psychosocial Determinants of Insomnia in Adolescents: Roles of Mental Health, Behavioral Health, and Social Environment. Front. Neurosci. 13:848. doi: 10.3389/fnins.2019.00848
Received: 25 April 2019; Accepted: 30 July 2019;
Published: 09 August 2019.
Edited by:
Amir H. Pakpour, Qazvin University of Medical Sciences, IranReviewed by:
Zainab Alimoradi, Qazvin University of Medical Sciences, IranMaryam Ganji, Tehran University of Medical Sciences, Iran
Copyright © 2019 Hsieh, Lu and Yen. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Wei-Hsin Lu, d2lpc2VlbkBnbWFpbC5jb20=; Cheng-Fang Yen, Y2hmYXllQGNjLmttdS5lZHUudHc=; cDAzMTMyMDA2QGdtYWlsLmNvbQ==
 Yi-Ping Hsieh
Yi-Ping Hsieh Wei-Hsin Lu2*
Wei-Hsin Lu2* Cheng-Fang Yen
Cheng-Fang Yen