- 1Medical College Bydgoszcz, Nicolaus Copernicus University in Torun, Torun, Poland
- 2Emergency Department, Regional Specialist Hospital, Dr. Wladyslaw Biegański, Grudziądz, Poland
- 3Wroclaw Medical University, Wroclaw, Poland
- 4Unit Interbank and Telemedicine, Regional Specialist Hospital, Dr. Wladyslaw Biegański, Grudziądz, Poland
This analysis is based on a review of 224 out of 323 cases of trauma deaths in Regional Specialist Hospital of Grudziądz during the period of 2003–2017. In this study, we have described and systematized the most common situations resulting in severe personal injury. We then evaluated whether the diagnostic procedures and treatments that were employed were correct. From the objective statistical parameters described, we evaluate the level of quality of emergency medicine and the effectiveness of the integrated medical rescue system. Ultimately, the most significant component is PTDR (preventable trauma death rate). Inspiration for our research came from direct observation of our daily experiences in the ED where we derived great satisfaction from treating patients successfully. More importantly, however, we suffered the severe disappointments of failure that always and inevitably raised the same question: Have we done everything humanely possible to save this patient? In the daily struggle of saving lives, the question always remains: What could we have done differently? Better? More effectively? To answer this question, we have to examine our emergency procedures and activities. Were they correct and effective? This documentation not only shows us a statistical picture of the injuries sustained by trauma victims, but also presents a dynamic reconstruction of events as well as the pathophysiology of dying. When we view all this material as a complete picture, we see that it provides the opportunity to assess the accuracy of judgment, especially during the critical moments of diagnosis and subsequent treatment of the casualties. Not only did we describe the anatomic results of injuries, including rankings to proper regions of the body, we also reconstructed the pathophysiology of dying such as airway obstruction—suffocation, bleeding—exsanguination, or severe complications such as acute respiratory distress syndrome, pulmonary emboli, thrombosis of intracranial vasculature, and fatal, irreversible organ damage. We checked operating procedures that had been done and those that should have been done to give the patient a chance for survival but were not due to wrong decisions. We have demonstrated that the element of time is critically important in diagnosing and implementing treatment of patients with major injuries; further, we have enumerated the potential complications, time errors, missed injury, and general mismanagement as professional risks for the emergency team: physicians, nurses, and paramedics. We have determined that almost half of all trauma deaths occur within the first 2 days following major injury, with most of those occurring within the first 6 h of hospitalization. The other deaths—“late deaths”—are the result of unsuccessful treatment or the development of complications in intensive care unit. In all hospital trauma deaths the leading causes are severity of brain injury (51%), exsanguination (31%), and asphyxiation (13%).
Introduction
A review of world literature concerning traumatology, injury prevention, and organization of treatment procedures of victims of serious accidents and fatalities due to trauma indicates that, at the beginning of the decade 2001–2010, ~40 to 50% of accident fatalities brought to hospitals with signs of life could have probably been saved.
The results of this research demonstrated the need for creating a safer prehospital admission protocol, improving preparation of patients at the scene of the accident, and improving transport of patients to a reorganized network of hospitals, as well as refining hospital protocols to improve treatment of patients with severe multiple injuries.
Numerous educational and organizational programs have been implemented to create trauma centers and hospital networks cooperating together, as well as attempting to create a registry of accidents and a quality control system for evaluating the three phases of prehospital treatment, transport to hospital, and in-hospital care, that is, implementation of clinical procedures in the emergency department (ED) and in other specialized clinical departments.
Preventable trauma death rate (PTDR) was used as a measure for quality control to compare the effectiveness of various trauma systems operating in different areas and at different times.
Probability of survival is expressed by the indicator PTDR, which is based on the Trauma Revised Injury Severity Score (TRISS) methodology. This is calculated on the basis of the Injury Severity Score (ISS), indicator that describes the anatomical effects of trauma. Revised Trauma Score (RTS) describes physiological dysfunction and takes into account the patient's age and type of injury. This, in turn, is modified by an adjustment coefficient—coefficients B0–B3—and meets criteria for the objective quality indicators (Boyd et al., 1987; Champion et al., 1990; Nast-Kolb et al., 2006). “Coefficients B0–B3 are derived from the Major Trauma Outcome Study, a registry of several thousand trauma patients used to generate predictable adult death rates.”
The purpose of this study is to analyze the dynamic changes that occur in PTDR and to describe irregularities that occur in diagnostic and therapeutic processes based on proprietary material collected by Dr. Władysław Biegaǹski in Grudziądz Regional Specialist Hospital during the years 2003 to 2017.
Inspiration for our research came from direct observation of our daily clinical workflow in the ED, where we experienced satisfaction from our successes, as well as the bitterness of our failures and losses. Every time we lost a patient, it raised the same question: Did we do everything possible to save the patient?
This article investigates the most common mechanisms that cause serious injuries and carries out a retrospective analysis of the accuracy of diagnostic and therapeutic procedures that were implemented with regard to omissions and errors that have been committed, the degree of severity of the injuries, and the probability of survival of the trauma patients evaluated with respect to the relevant scales of posttraumatic AIS/ISS, RTS, and TRISS.
The period of early death is the time interval in which emergency medicine must perform. Execution must be swift, decisive, and accurate, consistent with the latest achievements in science and in the art of medicine to reduce mortality, morbidity, and suffering and the degree of disability due to injury. The level of emergency medical care and the efficiency of the emergency medical system itself are best evidenced by quality indicators. Of critical importance is the rate of avoidable deaths (Boyd et al., 1987; Champion et al., 1990; Esposito et al., 1995; Kunihiro, 2005; Chiara et al., 2006; Saltzherr et al., 2011; Kim et al., 2012; Seong et al., 2015; Jung et al., 2019).
Materials and Methods
To answer this question, we have to analyze our emergency procedures and activities. Were they correct and effective? The most important information we have is what we have learned from the deaths of accident victims. This information not only shows us a statistical picture of the injuries sustained by trauma victims, but also provides a dynamic reconstruction of events, as well as the pathophysiology of dying. When all this material is viewed as a complete picture, it provides the opportunity to assess the accuracy of judgment, especially during the critical moments of diagnosis and treatment of the casualties. The study is based on a review of 224 of 323 cases of trauma deaths in Grudziądz Hospital during the years 2003 to 2017. The study includes only those patients for whom we have complete medical records, including autopsy examinations.
Not only the anatomic consequences of injuries have been described by assigning rankings to proper regions of the body, but also the pathophysiological changes they caused such as choking, bleeding, or severe complications such as acute respiratory distress syndrome (ARDS), thromboembolism, and fatal, irreversible organ damage.
Descriptions are provided of operating procedures that had been done, as well as those that definitely should have been done for patients in critical condition to increase their chances for survival. The study of autopsies provides a clear, kaleidoscopic image of major trauma patients and enables us to assess fairly the correctness of diagnostic and treatment processes.
The study defines the frequency of pneumothorax, hemopneumothorax, hematoma, and damage to the heart and major systemic vessels. It further emphasizes the importance of the reduction and stabilization of fractures of the pelvis in order to control retroperitoneal hemorrhage caused by these fractures.
In assessing the effectiveness of treatment of trauma patients, it is also important to take into consideration “the identified errors in the delivery of care,” which are included in the following factors:
1) Time factor—delay in implementing ATLS due to delay in reaching out to accident victims or prolonged lapse of time between the occurrence of an accident until implementation of highly specialized procedures in the ED.
2) Failure to comply with standards of ED parallelism in diagnosis and treatment.
3) Irregularities/errors involving unresolved or delayed diagnosis of life-threatening conditions: airway obstruction, traumatic internal bleeding, intracranial hematoma, pneumothorax, and pericardial tamponade.
4) Irregularities/errors involving incomplete diagnosis related to oversight of a seriously injured organ at different stages of diagnosis and treatment, as well as the associated delays in commencing surgery: for emergency laparotomy or thoracotomy: emergency time greater than 2 h; for emergency craniotomy: emergency time greater than 4 h.
5) Lack of quick and efficient diagnostic procedures as well as using improper methods to transport patients safely within the hospital who are either unconscious or unstable.
6) Lack of decisiveness and competence among the treatment team in not applying the principle of more “aggressive treatment” for patients in critical condition.
7) Lack of proper coordination between the members of the “trauma team” and the absence of a decision-making leader.
8) Lack of an “on-call operating room,” which is in constant readiness and designated exclusively for emergency procedures.
9) Lack or shortage of medical equipment and other necessary hospital services: laboratory diagnostics, imaging, blood bank.
The study employs the widely used TRISS methodology, based on RTS and Abbreviated Injury Scale/Injury Severity Score (AIS/ISS) to assess the probability of survival, Probability of survival of trauma patient (Ps), and PTDR, the rate of preventable trauma deaths.
TRISS formula removes subjective impact on the calculation of the rate of Ps and locates the deaths identified as definitely to avoid—DP ratio above 0.50 Ps; PP, possible to avoid between 0.25 and 0.5 Ps; and NP, unavoidable below 0.25 Ps. TRISS calculator simplifies complex mathematical calculations; DP, determination to avoid; PP, probably inevitable, unavoidable NP; PDR, definitions: preventable death rate is the proportion of the deaths judged to be preventable if optimal trauma care has been delivered.
Trauma deaths defined as preventable need to meet three criteria
1) The injuries produced by trauma and its sequelae must be survivable.
2) The care that has been delivered must be suboptimal when compared with standards.
3) The identified errors in the delivery of care have contributed directly or indirectly to the patient's outcome.
Traditionally, we use the following classification of deaths to avoid: DPD—definitely preventable death–definitely avoidable, if treatment of the injury is done by conventional methods in a facility with standard equipment. PPD—possible preventable death, death may be avoided if the injuries are severe but curable in the present state of medicine, provided that the patient goes immediately to a highly qualified treatment center having the highest standards of knowledge and art of medicine, where he/she receives appropriate treatment within a suitably short period of time. NP—non-preventable death, death is inevitable because of mortal injury, incurable in the present state of knowledge. This group includes each patient with a score of 6 on the AIS scale for even one of the six body regions; this injury is definitely fatal (Boyd et al., 1987; Champion et al., 1990; Bose and Tejwani, 2006; Chiara et al., 2006; Gao et al., 2006; Gruen et al., 2006; Shen et al., 2006; Stanescu et al., 2006; Seong et al., 2015).
We evaluated 71 variables including the mechanism of injury, the nature of the injuries, pathophysiological changes that they caused, and the time of the accident, as well as the time it takes for medical rescue operations and procedures of clinical emergency medicine to begin, errors in diagnostic and therapeutic procedures, survival, the leading causes of death, and early- and late-stage complications. The study used statistical analysis to examine the relationship of selected criteria among the patients who were observed.
The study uses statistical analysis to examine the dependence of PTDR on the observation time of patients as well as on other selected criteria.
The study of PTDR variability over time was calculated by specifying this parameter as a function of time. The PTDR (i) designates the PTDR calculated for the first (i) patients. This approach makes it possible to study the dynamics of PTDR changes over time. Comparison of PTDR in two predominant groups is accomplished by comparing PTDR changes within these groups. The statistical significance of PTDR decline (variance) is examined by testing the significance of the appropriate simple regression form: PTDR = A t + B, where A and B are coefficients determined on the basis of patient data; t is observation time (in practice, this count represents the sequential order of patients). In the groups of patients analyzed, it was shown that A < 0. This means that PTDR decreases as observation time increases.
Results
The results of this study emphasize the key moments in the decision-making process of diagnosis and treatment and make it apparent that the art of healing is subject to adverse events, which are a part of the professional risks for physicians, nurses, and paramedics.
We have shown that pneumothorax and intracranial hematoma are dynamic processes that can appear at any stage of posttraumatic injury.
Nearly half of all trauma deaths occurred within the first 2 days following major injury, with most of those occurring during the first hours of hospitalization. The other “late deaths” are the result of complications during treatment in intensive care unit (ICU).
The primary causes of late deaths are mostly multiorgan failure (MOF) and sepsis. Autopsy studies have shown that pneumonia, as a result of ventilator-associated ARDS, accounts for 34% of trauma deaths, and thromboembolism accounts for 6% of trauma deaths.
In the material presented, other significant causes of death were early bleeding (30%) and asphyxiation (12%). However, the leading cause of all deaths in hospital was the severity of central nervous system (CNS) damage (50%).
Every fifth trepanation/craniotomy was performed too late, when raised intracranial pressure was present. In every seventh fatal accident, a laparotomy of the victim was necessary but overlooked and not done, or was done too late, resulting in significant damage.
In light of the autopsy findings, our persistent and prolonged struggle for survival of patients in the final stage of the disease who due to changes in venous sinus thrombosis and autolysis of the brain along with irreversible organ damage in the course of the MOF had no chance of survival turned out to be ineffective and doomed to failure.
In 33% of trauma deaths that occurred while patients were in hospital, severe brain injury as a result of high-energy impact contributed to the patients' demise.
In 66 patients with CNS injuries (40%), we found no fracture of the skull despite serious injury to the brain.
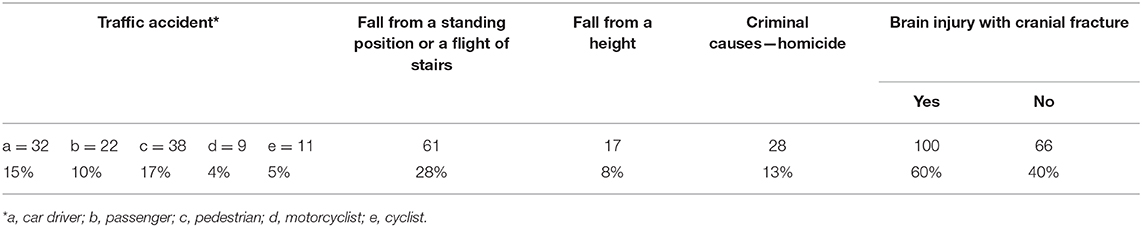
Pedestrians struck by cars were the largest group of fatalities. The fourth largest group was due to falls—from one-story or down a flight of stairs. Deaths due to criminal assault cover the eighth rank of victims. The most common combination of injuries was head, chest, legs, and pelvis injuries.
Quite often as many as 26% of deaths of injuries were attributable to hemopneumothorax or pleural hematoma with pulmonary contusion. Fourteen percent were for rupture of large systemic vessels and/or the heart. In every fifth patient, there was damage to abdominal organs. Pelvic fracture with retroperitoneal hematoma was found in one-sixth of the dead, but the stabilization of the fracture of the pelvis with associated retroperitoneal hemorrhage was performed sporadically. In one-fifth of the deceased, surgery was not performed or was not performed early enough.
Cranial trepanation or craniotomy was the most frequently performed surgery−108 treatments. This large number is a result of the enormous number of head traumas; CNS damage was found in 70% of fatalities. Respirotherapy subjects were 170 patients or 76%, and the majority of them died due to pulmonary complications: ARDS, pneumonitis, and pulmonary emboli. Intracranial hematoma was not recognized in 10 (4%) and pneumothorax in 13 (6.0%) patients.
In 4% of patients, autopsy revealed aspiration of gastric contents into the airways. In one-third of the deceased patients, rescue action and emergency procedures were delayed in excess of the golden hour; they relate to different stages in the chain of survival.
In 21% of mortalities, the source or intensity of bleeding site had been underestimated. Multiorgan failure and/or sepsis was the cause of every fourth trauma-related death. They were the primary cause of late death. Pleural drainage was as common a procedure as laparotomy (42 vs. 39 cases) and twice as frequently as fusion of the long bones. A thoracotomy was performed intermittently 4 cases (2%). However, it was indicated in 15% of cases if we include repair procedures that would have been done on an injured heart and major vessels. However, the patients were being delivered to the hospital in a moribund state, and the procedures were beyond the capabilities of a local hospital. In the majority of chest injury cases going to surgery, there was sufficient drainage of the pleural cavity.
Below we present results of our research in numbers and percentages (Table 1).
Early and late deaths: Early deaths <24 h: n = 70 (31%), >24 but <48 h: n = 20 (9%), late deaths >48 h: n = 134 (60%).
Anatomical areas of the body with known injury: head n = 185 (83%), thorax n = 102 (46%), abdomen n = 52 (23%), limbs and pelvis n = 67 (30%), others n = 12 (5%).
PTDR in period of 2003–2017: period of 2003–2006 PTDR = 30/54 (55%), period of 2007–2010 PTDR = 19/56 (34%), period of 2011–2015 PTDR = 25/84 (30%), period of 2016–2017 PTDR = 7/30 (23%).
Type of injuries: only one region injuries n = 105 (47%), multiregion injuries n = 119 (53%).
Anatomical Effects of Injuries
1. Fatal CNS damage, n = 75 (33%)
2. Ribs fracture without edema and/or pneumothorax, n = 30 (13%)
3. Multiple rib fracture with pneumothorax and hemothorax, n = 59 (26%)
4. Pulmonary contusion, n = 60 (27%)
5. Major systemic vessels and heart rupture 30 (14%)
6. Abdominal injuries 46, n = (21%) (damage is usually found according to cited order: liver, spleen, mesenterium of small intestine, and the small intestine)
7. Pelvic fracture with retroperitoneal hematoma, n = 38 (17%)
8. Long-bones fracture, n = 43 (29%)
9. Spinal fracture, n = 19 (8%).
Operative Strategies of Injured Patients
1. Craniotomy/trepanation of the skull, n = 108 (48%)
2. Drain of pleural cavity, n = 42 (19%)
3. Thoracotomy, n = 4 (2%)
4. Laparotomy with corrective surgery, n = 39 (17%)
5. Fusion of long bones, n = 16 (8%)
6. No surgical procedure, n = 49 (25%)
7. Respirotherapy, n = 170 (76%).
The Most Common Early Complications
1. Bleeding, n = 64 (29%)
2. Asphyxiation, n = 27 (12%)
3. Irreversible trauma shock, n = 64 (29%)
4. Subtentorial and tonsillar herniation, n = 76 (34%).
The Most Common Late Complications
1. Suffocation due to pneumothorax and tension pneumothorax during respirotherapy, n = 5 (2%)
2. ARDS + pneumonia ventilator, n = 76 (34%)
3. Intracranial thrombosis and brain self-destruction, n = 30 (13%)
4. Neuroinfection accompanying CNS injury, n = 10 (4%)
5. MOF + sepsis, n = 64 (31%).
6. Pulmonary embolism, n = 14 (6%).
Most Common and Most Serious Adverse Events
1. Unrecognized pneumothorax, n = 13 (6.0%)
2. Unrecognized source or intensity of bleeding as well as underestimated, n = 43 (19%)
3. Aspiration of gastric contents into the respiratory tract, n = 8 (4%)
4. Late craniotomy (trepanation of skull), n = 49 (22%)
5. Late laparotomy or needed laparotomy was not done, n = 27 (12%)
6. Delay in rescue operations—exceeding the golden hour, n = 73 (33%)
7. Unrecognized intracranial hematoma, n = 10 (4%)
8. Injury beyond the capabilities of the local hospital, n = 11(4%).
Leading Causes of Deaths
1. Severity of CNS injury, n = 115 (51%)
2. Bleeding, n = 62 (31%)
3. Asphyxiation, n = 28 (13%)
4. Diagnostic errors—a failure to recognize significant damage or incorrect assessment of the severity and extent of damage, failure to recognize the serious complications in the course of treatment, n = 46 (20%)
5. Late complications during treatment in the ICU, n = 103 (46%).
Monitoring the Efficiency of the State Emergency Medical System in Trauma Using PTDR
The PTDR analysis revealed a significant statistical decline in value during the period under consideration, indicating a substantial improvement in the merits of the State Emergency Medical System.
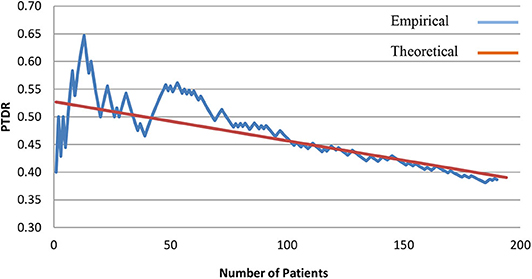
Figure 1 shows the dependence of PTDR on the patient number and observation time using a simple regression to describe this relationship. In the initial phase, PTDR shows significant fluctuations, but after some time, these fluctuations decrease. The simple regression equation is: PTDR = −0.00071 t + 0.527406. The relationship of the examined data is statistically significant at a significance level of p < 0.0001. The correlation coefficient is equal to r = −0.70.
A joint effort significantly improved the rate of preventable trauma deaths from 55% in 2003–2006, to 34% in 2007–2010, to 30% in 2011–2015, and 23% in 2016–2017.
The analysis of PTDR volatility demonstrated a statistically significant decline in its value during the specified time period, indicating a substantial improvement in the quality of the PRM (State Emergency Medical) system. Progress in reducing the rate of avoidable trauma deaths during the study period is particularly evident among men in the subgroup classified as early deaths within the larger group including diagnostic errors and bleeding. The foregoing relationships were presented in the form of statistical models.
PTDR Gender Dependence
The number of women (58) in the study is three times smaller than the number of men (166).
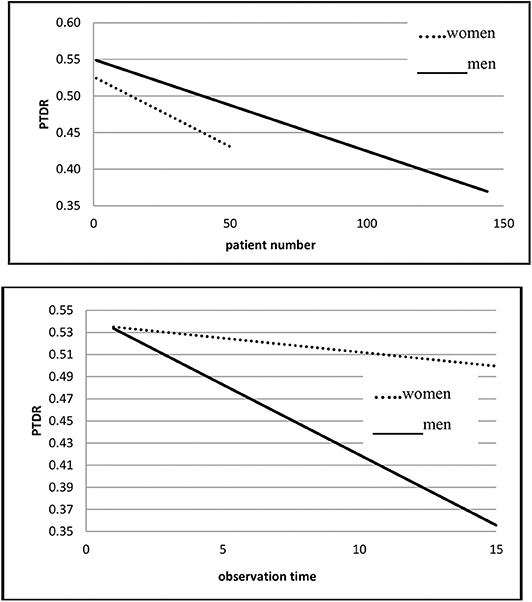
The decrease in PTDR is slightly higher for men than for women in the period studied. The simple regression as a model of decline for women is almost statistically insignificant (p = 0.045, r = −0.28), whereas for men, the linear model captures the nature of time dependence very well (p < 0.0001, r = −0.68). A decrease from 0.55 to 0.39 was noted in the study period.
Figure 2 presents simple regression charts for gender.
Comment
Men are, predominantly, the victims of traffic accidents and criminal activity—beatings. The decrease in PTDR is most evident in the group of people with multiple injuries associated with the above accidents. This group comprised mostly men.
PTDR Variability Dependent on the Occurrence of CNS Injuries
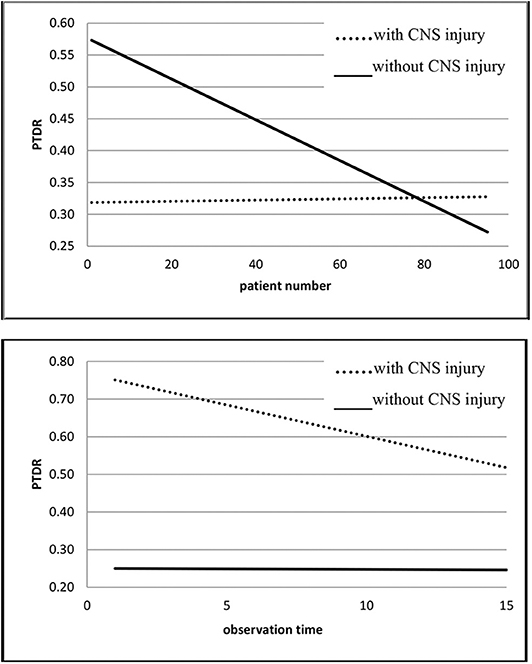
For CNS = 1, the regression line is statistically constant (p = 0.44, r = −0.08). For CNS = 0, the decrease in PTDR is significant (r = −0.78, p < 0.0001), from 0.57 to 0.24 (0.26 in the model). Figure 3 shows the PTDR waveform for CNS = 1 and CNS = 0.
Comment
For patients with CNS injuries, PTDR is statistically stable throughout the study period. The causes for lack of progress in reducing the rate are complex.
Early deaths are typically the result of delayed rescue operations: calling the ambulance too late, delay in performing diagnostic and therapeutic clinical procedures such as computed tomography scan of the head, intubation and respiratory therapy, and surgery—skull trepanation/craniotomy. Previously, there was intussusception and debarking, resulting in death. This applies especially to people who were brutally beaten, under the influence of alcohol and psychoactive substances, as well as to older people, most often living alone in single-level homes who experience falls from a low height—often downstairs—and sustain head injuries.
In contrast, late deaths among ICU patients with CNS injuries are due to severe septic complications, neuroinfections, venous sinus thrombosis, and brain necrosis.
For patients with CNS injury, PTDR rate remains constant throughout the study period. Once again, causes for lack of progress in lowering the rate are complex.
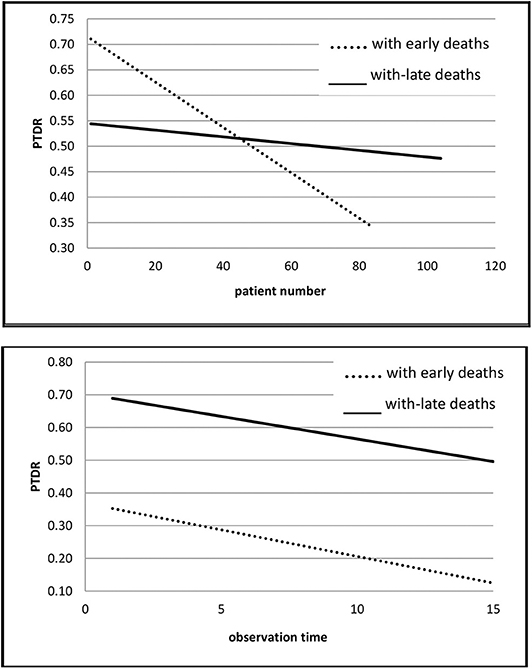
Early and Late Deaths
The decrease in PTDR for early deaths is significant (p < 0.0001, r = −0.88) and varies from 0.72 to 0.38 (0.35 in the model), whereas the decrease for late deaths is “minimally” significant (p = 0.025, r = −0.22). For late deaths, the decrease dropped from 0.54 to 0.4 (0.47 in the model).
Figure 4 illustrates the course of simple regression for early and late deaths.
Comment
The marginally significant decrease in the PTDR rate for late deaths in the ICU is related to numerous lethal complications that occur during ICU treatment that determine the patient's outcome. Patients who have received highly specialized medical assistance during emergency procedures in the early phase after an accident are more likely to survive than a patient treated in the ICU during the late phase in the presence of MOF.
This barely significant decrease in PTDR for late deaths in the ICU is due to numerous fatal complications. A patient is more likely to survive when receiving treatment during the early phase after an accident.
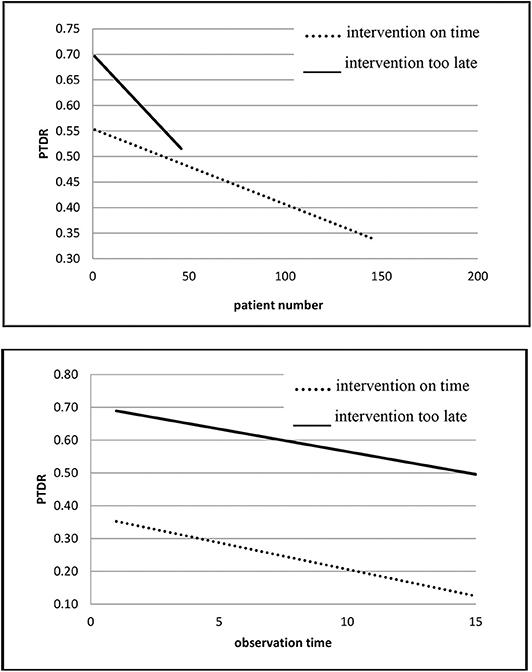
Late Intervention
For both groups, late intervention and no intervention, a significant decrease in PTDR is observed. In the group with delayed intervention, there is a decrease from 0.7 to 0.54 (0.52 in the model) and is significant (p < 0.0001, r = −0.59).
Figure 5 illustrates the course of the regression for instances of late intervention and interventions carried out without delay. In the group without late intervention, there is a decrease from 0.56 to 0.33 (0.34 in the model) and is also significant (p < 0.0001, r = −0.26).
Comment
The late intervention group managed to lower PTDR by improving the performance of the trauma patient treatment system. However, the fact that there is a delay in transport, emergency medical operations and emergency medicine clinical procedures still determine the high terminal value of the indicator.
A lower PTDR rate was achieved by improving the performance of the system treating trauma patients in the late intervention group. Notwithstanding delays in transport, emergency medical activities, and clinical procedures, emergency medicine still continues ultimately to determine the high value of the indicator.
For quality, late intervention has been able to lower PTDR by improving the performance of the trauma patient treatment system.
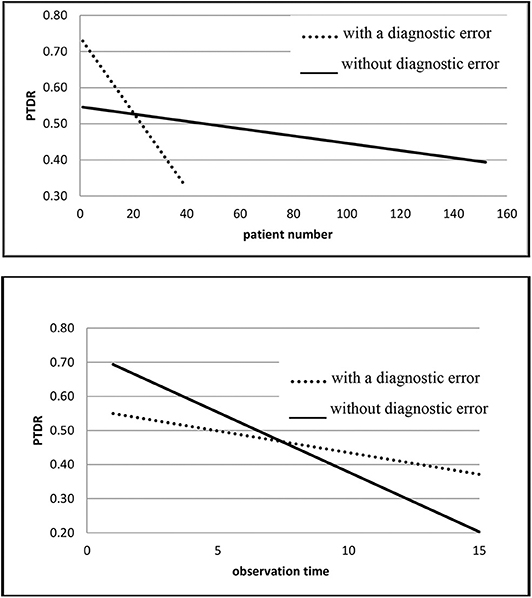
Diagnostic Errors
For both groups: with and without diagnostic errors, a significant decrease in PTDR was observed. In the group that had diagnostic errors, the decrease is significant (p < 0.0001, r = −0.78), from 0.76 to 0.33 (in the model 0.33), whereas in the group without diagnostic errors, a significant drop is also observed (p < 0.0001, r = −0.66), from 0.56 to 0.33 (0.39 on the model).
Figure 6 illustrates the relationship between instances where errors were found and those where they were not found.
Comment
Where the cause of high PTDR was due to diagnostic errors, measures were taken to eliminate them by introducing new standards and procedures to achieve better results—a lower PTDR—rather than for cases where death was determined by factors other than errors.
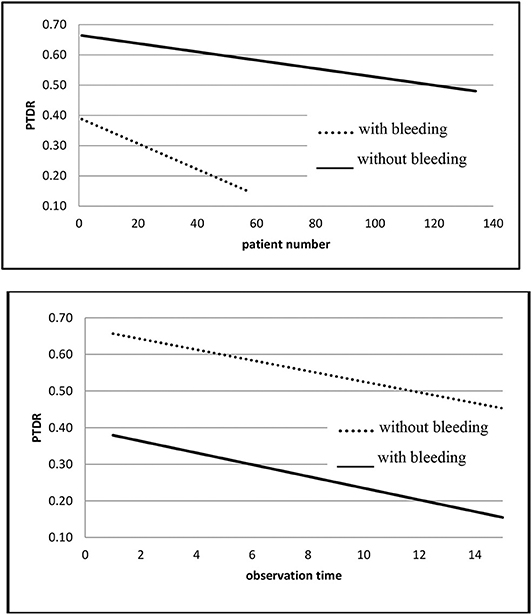
Bleeding
For both groups, bleeding and no bleeding, a significant decrease in PTDR is observed.
In the bleeding group, a significant decrease is observed (p < 0.0001, r = −0.62), from 0.4 to 0.2 (0.15 in the model), whereas in the non-bleeding group we have a significant decrease (r = −0.56, p < 0.0001), from 0.66 to 0.48 (0.48 in the model).
Figure 7 contains graphs of PTDR showing the relationship between bleeding and absence of bleeding.
Comment
Patients with bleeding showed a significant decrease in PTDR, down to 0.15, which clearly demonstrates the effectiveness of rescue efforts resulting from improvements in organizing the emergency medical and rescue system to save patients with bodily injuries and thereby providing still better opportunities for improving the effectiveness of emergency medicine. For the group of patients for whom the leading cause of death was not bleeding, the initial and final PTDR values still remain relatively high. This is due to the severity of organ damage, especially the CNS.
Late Complications
Comment
In the group of patients with late death due to complications during ICU treatment, a significant decrease in PTDR from 0.5 to 0.35 was obtained during the analyzed 15 years, which is evidence of increasingly more effective treatment of this group of extremely compromised patients.
Discussion
Where the system incorporating traumatology was implemented and trauma centers were established, PTDR was reduced from 30–50% to 10–20%, which resulted in a significant reduction in the number of fatalities and permanent disability (Iau et al., 1998; Kunihiro, 2005; Saltzherr et al., 2011; Sanddal et al., 2011; Kim et al., 2012; Park et al., 2017; Jung et al., 2019).
For hospitals annually treating only 50 to 100 patients with severe injuries (ISS > 15), PTDR still remains high in the 30 to 40% range. For hospitals treating more than 1,200 trauma patients a year, including at least 240 patients with severe injuries or more than 35 patients per surgeon per year, the rate is significantly reduced to 10 to 20% (Kunihiro, 2005).
Air transport of patients with severe injuries provides the opportunity to initiate advanced clinical procedures within 15 min, which considerably improves a patient's chances for survival. An assortment of “errors” that occur during the prehospital period that have an impact on PTDR are estimated to be ~30%; those committed in the ED are 50%, and those related to failures in clinical treatment and hospital structure/organization are ~40 to 50% (Kunihiro, 2005; Nast-Kolb et al., 2006; Pamerneckas et al., 2006; Salim et al., 2006; Sanddal et al., 2011; Park et al., 2017).
Mistakes that were made most frequently were related to delay in initiating BTLS and ATLS, prolonged transport of patients, unsafe transport of unconscious patients within the hospital, mistakes in providing for a patent airway for patients with chest injury, “careless” examination and assessment of patients, delay in ordering diagnostic imaging and laboratory tests due to overlooking significant injury, disregard for parallel diagnostics, and treatment of unstable patients and getting them to emergency surgery.
Diagnostic and treatment errors documented in the medical record play a significant role in describing the continuously high rate of avoidable trauma deaths—PTDR. They consist mainly of superficial patient assessment, underestimating the importance of gathering accurate information, underestimating the impact of serious injury, faulty interpretation of follow-up tests results, and incorrect preliminary diagnosis and delay in decisive treatment of the patient. Keep in mind the basic principle: “The more serious the injury, the more important it is to activate correct, decisive rescue procedures in the ED.”
The simpler the pathophysiology of death, the faster the death. Fatal injuries leading to immediate deaths are the result of organ damage, primarily the brain, massive hemorrhage from major system vessels and/or the heart, and suffocation.
Early deaths are caused by intracranial hematoma, bleeding from torn intercostal artery, ruptured parenchyma of abdominal organs, torn mesentery of the intestine, and retroperitoneal bleeding caused by an unstable pelvic fracture.
The leading cause of late death, occurring in ICU, involves complications of a complex pathogenesis appearing as the result of the spread of systemic inflammatory response syndrome (SIRS) and MOF.
The most common diagnostic errors belong to misdiagnosis: posttraumatic intracranial hematoma, pneumothorax, or internal bleeding, or underestimating its severity. It has been shown that pneumothorax and cerebral hemorrhage are dynamic processes that appear to go through different stages in the development of the disease process.
An important role in reducing PTDR is played by the algorithm for the initial management of polytrauma patients. After the initial traumatic examination and Whole Body Computed Tomography (WBCT), the polytrauma patient should be immediately transferred to the operating theater or the ICU.
“Timing and priorities of operative interventions in polytrauma patients depending on the physiological status” (Keel M.). Compromised vital functions—lifesaving primary surgery, highly unstable/in extremis—damage control surgery, stable vital functions—delayed primary surgery—day 1. Hyperinflammation (SIRS)—second looks only! Days 2–4. Window of opportunity—scheduled definitive surgery 5–10 day. Recovery—secondary reconstructive surgery after 3 weeks (Keel et al., 2006).
All the preceding work cited has become part of the total experience of other international health centers—European, American, and Asian—and the results obtained are comparable to the documentation of other practitioners writing on these topics. The results cited above demonstrate that we are an integral and important part of global emergency medicine (Helling et al., 2005; Keel et al., 2006; Sampson et al., 2006; Shen et al., 2006; Stanescu et al., 2006; Saltzherr et al., 2011; Sanddal et al., 2011; Kim et al., 2012; Seong et al., 2015; Park et al., 2017; Jung et al., 2019).
Conclusions
1. The introduction of the Act of the State Emergency Medical System and the system of treating trauma patients in Poland significantly influenced the reduction of avoidable traumatic deaths and thus increased survival in the group of patients who suffered severe trauma.
2. The decline in PTDR is modeled to varying degrees by specific variables, of which the most important are late intervention, diagnostic errors, bleeding, and severe CNS injury. Where the cause of high PTDR was due to diagnostic errors, measures were taken to eliminate them by introducing new standards and procedures to achieve better results—a lower PTDR—rather than for cases where death was determined by factors other than errors.
3. An important role in reducing PTDR is played by the algorithm for the initial management of polytrauma patients and timing. Patients who have received highly specialized medical assistance during emergency procedures in the early phase after an accident are more likely to survive than a patient treated in the ICU during the late phase in the presence of MOF.
4. Despite a significant improvement in the emergency medical system's operation, the number of errors made, expressed as an indicator of preventable traumatic deaths, is still high. In the years 2016–2017, PTDR amounted to 23%. The preceding obliges us to intensify our activities and look for more effective solutions, following the example of the world's leading trauma centers. There is an urgent need to build a trauma patient treatment system based on trauma centers and “network hospitals” cooperating with these centers.
Data Availability Statement
All datasets generated for this study are included in the article/supplementary material.
Author Contributions
AW collecting full medical records and developing a work concept. Determining the objectives of the work and developing the methodology for conducting it. Tracing world literature and writing a pioneering original work on PTDR and medical errors in the field of emergency medicine in Poland over a two-decade time perspective. JJ scientific consultant of the above work. RM collecting material in the form of medical documentation needed. TW statistical study of collected material. All authors contributed to the article and approved the submitted version.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Abbreviations
PTD, traumatic deaths to avoid; PTDR, the rate of posttraumatic deaths to avoid; AIS, ISS, RTS, commonly used in traumatology scales and indicators of the severity of injuries; TRISS calculation, scientific methodology for severe injuries, which allows calculation of Ps and PTDR using statistical methodology based on the collective, multicenter epidemiological studies of victims of serious accidents.
References
Bose, D., and Tejwani, N. C. (2006). Evolving trends in the care of polytrauma patients. Injury 37, 20–28. doi: 10.1016/j.injury.2005.06.054
Boyd, C. R., Mary, T. A., and Copes, W. S. (1987). Evaluating trauma care: the TRISS Method. J. Trauma 27, 370–378. doi: 10.1097/00005373-198704000-00005
Champion, H. R., Sacco, W. J., Lawnick, M. M., Keast, S. L., Bain, L. W., Flanagan, M. E., et al. (1990). The major trauma outcome study: establishing national norms for trauma care. J. Trauma 30, 1356–1365. doi: 10.1097/00005373-199011000-00008
Chiara, O., Cimbanassi, S., Pitidis, A., and Vesconi, S. (2006). Preventable trauma deaths: from panel review to population based-studies. World J. Emerg. Surg. 1:12. doi: 10.1186/1749-7922-1-12
Esposito, T. J., Sanddal, N. D., Hansen, J. D., and Reynolds, S. (1995). Analysis of preventable trauma deaths and inappropriate trauma care in a rural state. J. Trauma 39, 955–962. doi: 10.1097/00005373-199511000-00022
Gao, J. M., Gao, Y. H., and Zeng, J. B. (2006). Polytrauma with thoracic and/or abdominal injuries: Experience in 1540 cases. Chinese J. Traumatol. 9, 108–114.
Gruen, R. L., Jarkovich, G. J., and McIntyre, L. K. (2006). Patterns of errors contributing to trauma mortality: lessons learned from 2594 deaths. Ann. Surg. 244, 371–380. doi: 10.1097/01.sla.0000234655.83517.56
Helling, T. S., Nelson, P. W., and Moore, B. T. (2005). Is trauma centre care helpful for less severely injured patients? Injury 36, 1293–1297. doi: 10.1016/j.injury.2005.06.041
Iau, P., Ong Steven, C. L., and Chan, T. F. (1998). Preventable trauma deaths in Singapore. Aust. New Zealand J. Surg. 68, 820–824. doi: 10.1111/j.1445-2197.1998.tb04695.x
Jung, K., Kim, I., Park, S. K., Cho, H., Park, C. Y., Yun, J.-H., Kim, O. H., et al. (2019). Preventable trauma death rate after establishing a national trauma system in Korea. J. Korean Med. Sci. 34:e65. doi: 10.3346/jkms.2019.34.e65
Keel, M., Eid, K., Labler, L., Seifert, B., Trentz, O., and Ertel, W. (2006). Influence of injury pattern on incidence and severity of inflammatory post-traumatic complications in severely injured patients. Eur. J. Trauma 32, 387–395. doi: 10.1007/s00068-006-5140-3
Kim, H., Jung, K. Y., Kim, S. P., Kim, S. H., Noh, H., and Jang, H. Y. (2012). Changes in preventable death rates and traumatic care systems in Korea. J. Korean Soc. Emerg. Med. 23, 189–197.
Kunihiro, M. (2005). Trauma system in Japan: history, present status and future perspectives. J. Nippon Med. Sch. 72, 194–202. doi: 10.1272/jnms.72.194
Nast-Kolb, D., Ruchholtz, S., and Waydhas, C. (2006). Management of polytrauma. Chirurg 77, 871–873. doi: 10.1007/s00104-006-1231-2
Pamerneckas, A., Macas, A., and Blazgys, A. (2006). The treatment of multiple injuries: prehospital emergency aid. Medicina 42, 395–300.
Park, D. J., Park, C. Y., Cho, H. M., Lee, K. H., and Han, H. (2017). Current status and future prospects of trauma centers in Korea. J. Korean Med. Assoc. 60, 530–532. doi: 10.5124/jkma.2017.60.7.530
Salim, A., Sangthong, B., and Martin, M. (2006). Whole body imaging in blunt multisystem trauma patients without obvious signs of injury: results of prospective study. Arch. Surg. 141, 468–473. doi: 10.1001/archsurg.141.5.468
Saltzherr, T. P., Wendt, K. W., Nieboer, P., Nijsten, M. W., Valk, J. P., Luitse, J. S., et al. (2011). Preventability of trauma deaths in Dutch Level – 1 trauma centre. Injury 42, 870–873. doi: 10.1016/j.injury.2010.04.007
Sampson, M. A., Colquhoun, K. B., and Hennessy, N. L. (2006). Computed tomography whole body imaging in multi-trauma: 7 years experience. Clin. Radiol. 61, 365–369. doi: 10.1016/j.crad.2005.12.009
Sanddal, T. L., Esposito, T. J., Whitney, J. R., Hartford, D., Taillac, P. P., Mann, N. C., et al. (2011). Analysis of preventable trauma deaths and opportunities for trauma care improvement in Utah. J. Trauma 70, 970–977. doi: 10.1097/TA.0b013e3181fec9ba
Seong, C. K., Song, K. J., Shin, S. D., Lee, S. C., Park, J. O., and Holmes, J. F. (2015). Preventable deaths in patients with traumatic brain injury. Clin. Exp. Emerg. Med. 2, 51–58. doi: 10.15441/ceem.14.023
Shen, L. Y., Marcotte, K. N., and Helmer, S. D. (2006). Correlation of clinical findings and autopsy results after fatal injury from motor vehicular-related crashes. Am. Surg. 72, 282–287.
Keywords: PTDR, TRISS, traumatic deaths, patterns of errors contributing to trauma mortality, polytrauma, timing and priorites in polytrauma patients, probability of survival of trauma patient
Citation: Witkowski A, Jakubaszko J, Mańka R and Witkowski T (2020) Preventable Trauma Deaths Rate (PTDR)—Analysis of Variables That Shape Its Value With Patterns of Errors Contributing to Trauma Mortality. Fifteen Years of Experience Based on the Example of a Polish Specialist Regional Hospital. Front. Sustain. Cities 2:24. doi: 10.3389/frsc.2020.00024
Received: 23 February 2020; Accepted: 06 May 2020;
Published: 30 June 2020.
Edited by:
Dorota Lasota, Medical University of Warsaw, PolandReviewed by:
Ewa Raniszewska, Medical University of Gdansk, PolandBeata Rybojad, Medical University of Lublin, Poland
Copyright © 2020 Witkowski, Jakubaszko, Mańka and Witkowski. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Andrzej Witkowski, YW53aXRAd3AucGw=
 Andrzej Witkowski
Andrzej Witkowski Juliusz Jakubaszko3
Juliusz Jakubaszko3