- 1Department of Oral and Maxillofacial Surgery, Peking University School and Hospital of Stomatology, National Center of Stomatology, National Clinical Research Center for Oral Diseases, National Engineering Research Center of Oral Biomaterials and Digital Medical Devices, Beijing Key Laboratory of Digital Stomatology, Research Center of Engineering and Technology for Computerized Dentistry, Ministry of Health, NMPA Key Laboratory for Dental Materials, Beijing, China
- 2MOE Key Laboratory of Dynamics and Control of Flight Vehicle, School of Aerospace Engineering, Beijing Institute of Technology, Beijing, China
Objective: This study presents an innovative articular fossa prosthesis generated by the envelope surface of condyle movement, and compares its mandible movements, muscle activities, and joint reaction forces with two temporomandibular joint (TMJ) prostheses using multibody musculoskeletal simulation.
Methods: A healthy 23-year-old female was recruited for this study. Cone-beam computed tomographic (CBCT) was performed to reconstruct the mandibular bone geometry. A customized TMJ fossa prosthesis was designed based on the subject-specific envelope surface of condyle movement (ESCM). Mandibular kinematics and jaw-closing muscle electromyography (EMG) were simultaneously recorded during maximum jaw opening-closing movements. To validate our prosthesis design, a mandibular musculoskeletal model was established using flexible multibody dynamics and the obtained kinematics and EMG data. The Biomet fossa prosthesis and the ellipsoidal fossa prosthesis designed by imitating the lower limb prostheses were used for comparison. Simulations were performed to analyze the effects of different fossa prostheses on jaw opening-closing motions, mandibular muscle activation, and contact forces.
Results: The maximum opening displacement for the envelope-based fossa prosthesis was greater than those for Biomet and ellipsoidal prostheses (36 mm, 35 mm, and 33 mm, respectively). The mandibular musculoskeletal model with ellipsoidal prosthesis led to dislocation near maximal jaw opening. Compared to Biomet, the envelope-based fossa reduced the digastric and lateral pterygoid activation at maximal jaw opening. It also reduced the maximal resistance to condylar sliding on the intact side by 63.2 N.
Conclusion: A customized TMJ fossa prosthesis was successfully developed using the ESCM concept. Our study of musculoskeletal multibody modeling has highlighted its advantages and potential. The artificial fossa design successfully achieved a wider condylar range of motion. It also reduced the activation of jaw opening muscles on the affected side and resistance on the intact side. This study showed that an ESCM-based approach may be useful for optimizing TMJ fossa prostheses design.
1 Introduction
The temporomandibular joint (TMJ) is the only movable joint of the human oral and maxillofacial region, and is actively involved in several daily activities (Zheng et al., 2019). TMJ disorders, such as tumors and ankylosis, can affect its integrity and cause joint dysfunction (Mercuri, 2000). Total joint replacement is an effective method for TMJ reconstruction and functional restoration (Sidebottom, 2008).
Currently, there are two commercially-available TMJ replacement systems approved by the Food and Drug Administration, Biomet Microfixation (Jacksonville, FL, USA) (Imola and Liddell, 2016) and TMJ Concepts (Ventura, CA, USA) (Wolford et al., 1994). Both these systems consist of condylar and fossa components (Kiehn et al., 1974). The TMJ Concepts prostheses are constructed using patient-specific cone-beam computed tomography (CBCT) data (Wolford et al., 2003). Meanwhile, Biomet has three stock components with different lengths and styles (Imola and Liddell, 2016). The Biomet artificial fossa is a flat and ellipsoidal surface, and the TMJ fossa and mandibular ramus may need to be trimmed in order to fit with it.
Existing TMJ prostheses were designed solely based on medical imaging, and cannot completely restore the physiological condylar kinematics (Zou et al., 2020). The natural condyle has sliding and rotational movements (van Loon et al., 1999). Although TMJ replacement significantly improves mandibular movement, the condylar kinematics for the prosthesis are different compared to the natural TMJ (Westermark, 2010; Gruber et al., 2015; Gonzalez-Perez et al., 2016). In particular, condylar sliding may be completely lost after TMJ replacement (Sonnenburg and Sonnenburg, 1985; Merlini and Palla, 1988; Mercuri et al., 1995). This may be because the geometry of the TMJ prosthesis restricts the condylar range of motion (ROM) (van Loon et al., 1999). In vitro experiments performed by Celebi et al.(2011) demonstrated that the artificial condyle is more deeply enclosed within the articular fossa compared to the natural condyle. This makes achieving the normal condylar ROM nearly impossible.
A function-based prosthesis may be designed by imitating the artificial joints of the lower limb. For example, the instantaneous center of rotation of the knee joint was considered when designing artificial knee implants (Walker, 2001). It has been observed that the physiological knee kinematics cannot be achieved by restoring its anatomical morphology alone (Wang et al., 2021). Similarly, TMJ fossa prostheses may also be custom-made based on the three-dimensional (3D) condylar movement. According to the finite element analysis using a canine model, this may result in a reasonable strain distribution (Xu et al., 2017). Reconstruction of the functional condylar surface, i.e., the envelope surface of condylar movement (ESCM), in normal adults was proposed by Huang et al. (2021). The use of the ESCM concept for designing TMJ fossa prostheses can allow physiologically accurate kinematics (Chen et al., 2022a; Chen et al., 2022b).
The ESCM surface concept has not yet been applied for the real-world design of human TMJ fossa prostheses. An important reason is the lack of systematic comparison of the effect of different TMJ prostheses on mandibular biomechanics. Radiographic, ultrasonic, magnetic, and optoelectronic tracking methods have previously been used for in vivo quantification of the mandibular kinematics (Woodford et al., 2020). Based on these measured kinematics data, multibody dynamics modeling provided an in silico method to investigate the hidden biomechanics of the mandibular musculoskeletal system. This has proven to be effective and reliable in quantifying the functional outcomes after mandibular surgery and reconstruction (Hannam et al., 2010; Hannam, 2011). Previous studies have also validated the feasibility of simulating maximal jaw opening-closing movements based on flexible multibody dynamics (Broser et al., 2021; Guo et al., 2022).
This study is the first to propose a TMJ fossa prosthesis design based on the ESCM concept. Functional outcomes of this fossa design, including mandibular movements, muscle activity, and joint reaction forces, were predicted based on musculoskeletal multibody simulations, and compared with those of the Biomet and ellipsoidal fossa prostheses. We hypothesized that the customized envelope-based fossa prosthesis would improve the functional outcomes, including condylar ROM and jaw opening muscle activations.
2 Materials and methods
2.1 Subject
This study was approved by the Institutional Review Board of Peking University School and Hospital of Stomatology, Beijing, China (Pkussirb-201947091). A 23-year-old female volunteer with no symptoms and signs of TMJ disorder or a history of TMJ disorder or orthodontic treatment was selected. Written informed consent to publish the findings was obtained.
2.2 CBCT
Skull base and mandibular CBCT scans (NewTom VG, NewTom, Imola, Italy; Voxel size: 0.3 mm, Field of view: 16 cm × 16 cm) were performed in the intercuspal position. The segmentation and 3D reconstructions were performed in stereolithographic format using CBCT data in the Proplan CMF software (version 3.0, Materialise, Leuven, Belgium).
2.3 Mandibular movements and electromyography (EMG)
The subject was instructed to perform two warm-up cycles and one test cycle of maximal opening-closing movements, beginning and ending in the maximum intercuspal position (Baqaien et al., 2007; Koeppel et al., 2015). The WINJAW ultrasound system (Zebris Medical GmbH, Isny, Germany) was used to record the mandibular motion. Mandibular position relative to the upper dentition was recorded using the Trios intraoral scanner (3Shape, Copenhagen, Denmark).
The WINJAW EMG device (Zebris Medical GmbH, Isny, Germany) was used to simultaneously record bilateral stomatognathic muscle activities during each cycle of mandibular movements. The electrodes were positioned on the anterior temporalis and masseter muscle bellies bilaterally. The subject was instructed to perform maximum voluntary contractions (MVCs) thrice to obtain the maximal muscle force-generating capacity for each muscle (Ferrario et al., 2004; Owashi et al., 2017). Raw EMG signals were rectified and low-pass filtered (Lloyd and Besier, 2003; Guo et al., 2020), and the data were normalized using the MVC values (Quental et al., 2012). The obtained dimensionless signal was used as input to analyze muscular activation based on the first-order activation dynamics equation (Thelen, 2003; Guo et al., 2022).
2.4 TMJ fossa protheses and ellipsoidal condyle design
The TMJ fossa prothesis, based on the ESCM concept, was designed as follows. The maxilla, mandible and mandibular border movement trajectories were registered. Then according to the trajectories, the mandibular border movement was simulated, and the positions of the functional surfaces of the condyle at each moment were saved in the same 3D coordinated system. The condylar functional surface was defined as the coverage of the transverse ridge 6 mm forward. Condylar functional surface data was merged to construct the ESCM, as reported previously (Huang et al., 2021). The procedure used to obtain the ESCM is shown in Figure 1. Subsequently, the geometry of envelope surface was smoothened and refined using the Geomagic Studio software (version 2012, 3D Systems, Rock Hill, SC, USA). The envelope surface was uniformly thickened by 1 mm, and the customized fossa prosthesis was obtained (Figures 2A, B).

FIGURE 1. Procedure of obtaining the ESCM. The coronal section (A) and sagittal section (B) of positions of the condylar functional surfaces at each moment. The coronal section (C) and sagittal section (D) of ESCM generated by merging the condylar functional surface data.
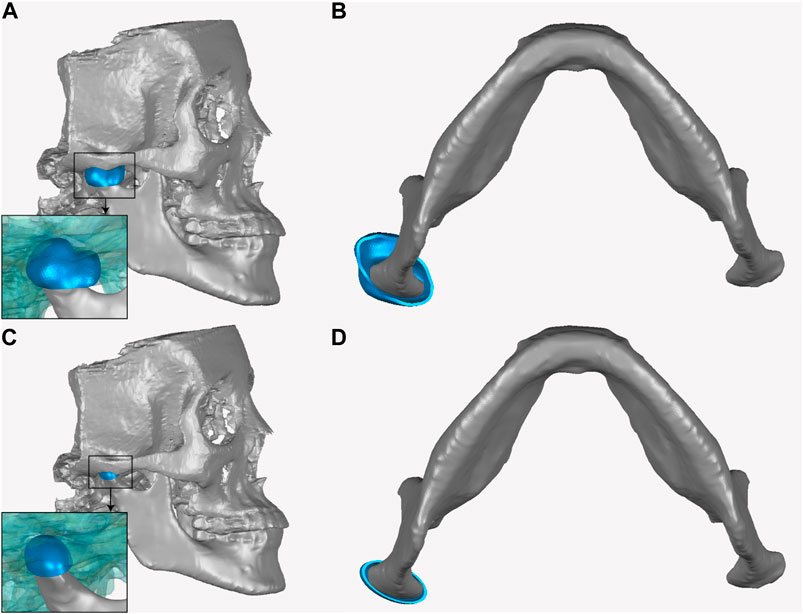
FIGURE 2. The sagittal section (A) and cross section (B) of envelope-based fossa prosthesis. The sagittal section (C) and cross section (D) of the ellipsoidal fossa prosthesis.
The Biomet fossa used in this study was obtained by increasing the overall size of the stock fossa prosthesis by 25% to fit the shape of the subject’s natural fossa. An ellipsoidal fossa prosthesis was obtained by setting a hemi-ellipsoid to fit the subject’s natural condyle (Figures 2C, D). The ellipsoidal fossa prosthesis was designed by imitating the lower limb joint implants and ignoring the condylar translation. The ellipsoidal fossa prosthesis was used to demonstrate the importance of condylar movements in TMJ prosthesis designing. Previous studies (Oberg et al., 1971; Zhao et al., 2019) have reported that the mandibular condyles of most adults are nearly ellipsoidal. The major (mediolateral) axis of the condyle is twice as long as the minor (anteroposterior) axis. Similarly, the mediolateral to anteroposterior diameter ratio of the ellipsoidal fossa prosthesis was 2:1.
The condylar ROMs for different fossa prostheses are shown in Figure 3. A least-squares fit of the subject-specific CBCT was used to determine the condylar radius, assuming the condylar surface to be frictionless (Yao et al., 2011; Modenese and Kohout, 2020; Guo et al., 2022). The condyle on the intact side was kept in the natural shape.
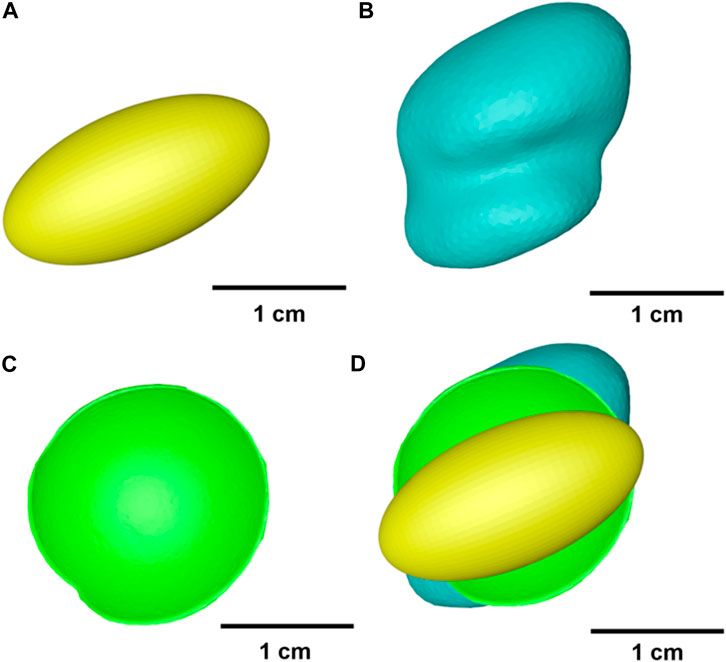
FIGURE 3. Geometry of different fossa prostheses. (A) Ellipsoidal fossa prosthesis. (B) Envelope-based fossa prothesis. (C) Biomet fossa prosthesis. (D) Comparison of the range of condylar motion.
2.5 Mandibular multibody musculoskeletal model
Mandibular subject-specific musculoskeletal modeling and simulation were based on a study by Guo et al. (2022). The subject-specific mandibular and skull geometry was obtained from the reconstructed CBCT data (Koolstra and van Eijden, 2005). The mandibular model was driven by 24 muscle bundles (de Zee et al., 2007), which were discretized by a flexible muscle element with a typical Hill-type model. Muscle insertion contours within the generic model were mapped onto the subject-specific bone morphology using the non-rigid iterative closest point algorithm.
The surface geometry of each fossa prosthesis type was extracted, and their vertices were set as contact detection points. Condylar contact geometry on the affected side was simplified as an ellipsoid, and the TMJ contact was modeled as a group of contact points to the rotating body. The normal contact force for the TMJ was calculated using a frictionless contact force model for soft materials (Flores and Ambrósio, 2010), with a friction coefficient of 0.001 (Xu et al., 2017).
Numerical simulations were performed using the inverse-forward dynamic coupling approach (Guo et al., 2022). The 3D mandibular movements were selected as the kinematic inputs to constrain the mandibular bone kinematics. Hyoid location in the intercuspal and maximal opening positions were measured using CBCT, and its movement trajectories were simplified through linear interpolation (Silva and Ambrósio, 2003; Guo et al., 2022). The musculotendon length for each muscle was calculated using the inverse dynamics approach. Motion constraints were removed during forward dynamics estimations. Mandibular muscle forces were estimated via feedback control using their lengths as the target value. A proportional derivative controller was used to calculate the activations for each muscle bundle. The schematic overview of establishing the subject-specific mandible musculoskeletal model is shown in Figure 4.
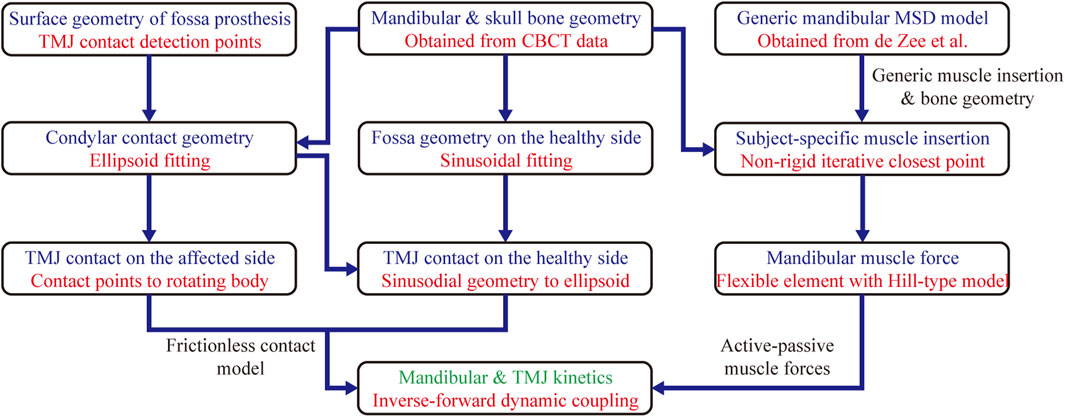
FIGURE 4. The schematic overview of establishing the subject-specific mandible musculoskeletal model. MSD, Multibody System Dynamics.
3 Results
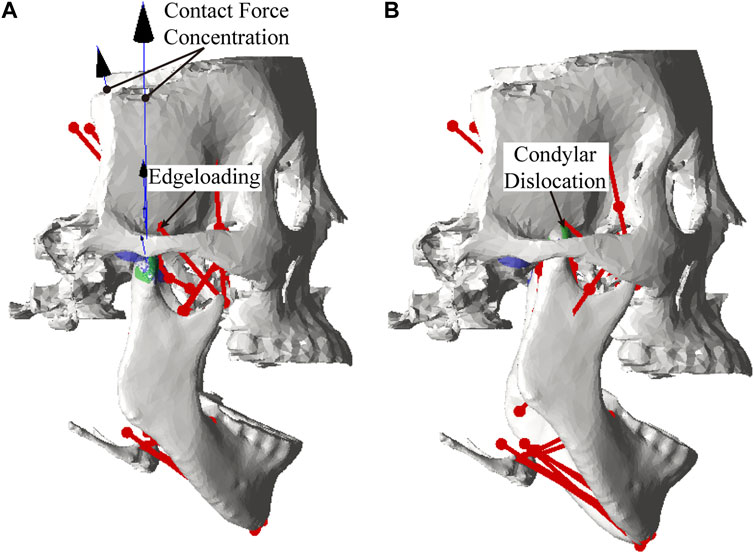
Lower incisor movements for different artificial fossa types are shown in Figure 5. The maximum jaw opening magnitudes for the envelope-based, Biomet, and ellipsoidal fossae were 36 mm, 35 mm, and 33 mm, respectively. With an ellipsoidal fossa prosthesis implanted, the condyle of the affected side performed joint dislocation (Figure 6). Condylar ROMs on the affected side were nearly identical for the envelope-based and Biomet prostheses.
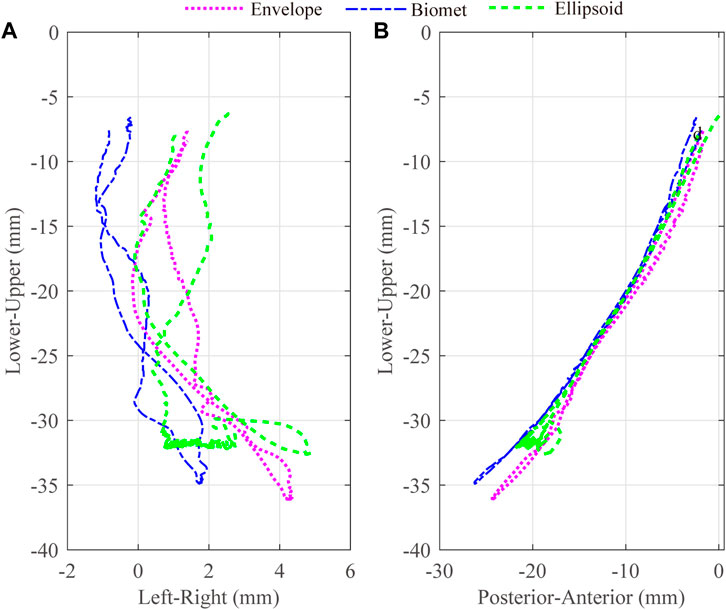
FIGURE 5. 3D trajectories for the lower incisors with different artificial fossae. The axes were separated as two different panes, Left-Right (A) and Posterior-Anterior (B).
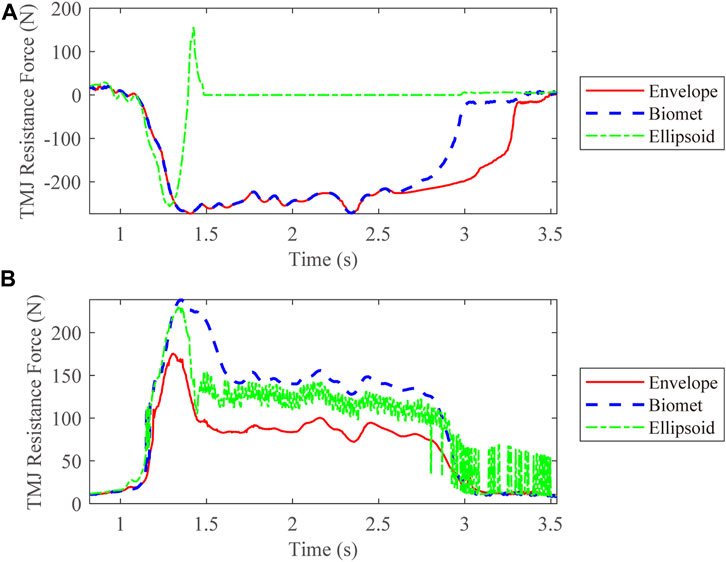
We also compared the kinetic data during jaw-opening motions. The activation of the digastric and lateral pterygoid muscles during maximal jaw opening was reduced with envelope-based fossa prosthesis compared to Biomet (Figure 7). Bilateral contact forces for the envelope-based and Biomet fossae were similar during and at maximal jaw opening. However, the TMJ with the envelope-based fossa allowed greater normal contact forces than Biomet (Figure 8). When the condyle traveled through the apex, the resistance for forward condylar translation with the envelope-based fossa decreased by 62.4 N (Figure 9). Moreover, the condylar contact force was unevenly distributed for different prostheses, and the maximal contact force for the envelope-based fossa at maximal jaw opening was greater than that for Biomet (Figure 10).
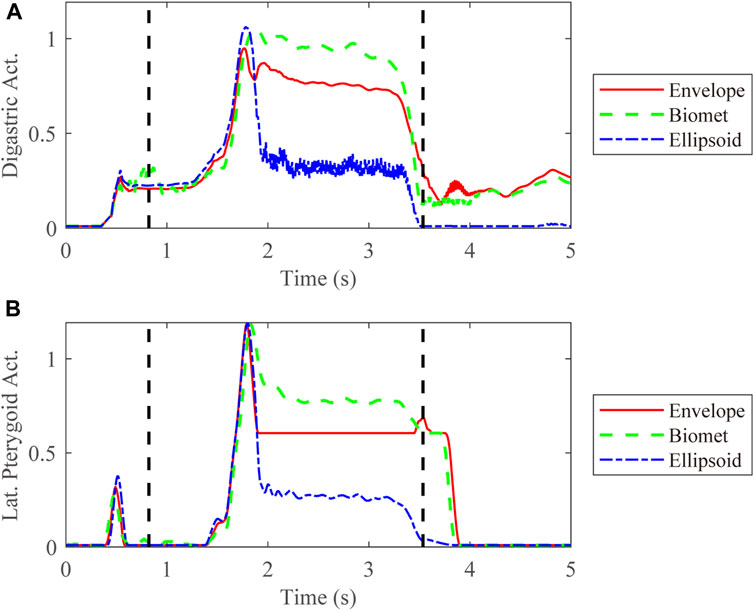
FIGURE 7. Activation of the digastric (A) and lateral pterygoid (B) muscles on the affected side. The vertical dotted line demonstrates the time range for jaw opening-closing movements. Act. = Activation. Lat. = lateral.
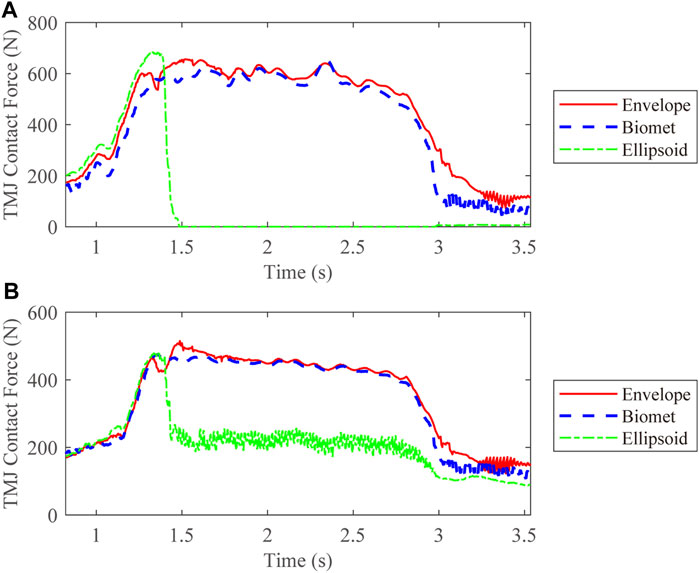
FIGURE 8. TMJ contact forces for different types of articular fossa types. (A) Intact side; (B) Affected side.

FIGURE 10. Distribution of TMJ contact forces with the condyles moving to edges of different fossa prostheses.
4 Discussion
Total joint replacement is commonly used to treat severe degenerative conditions of the TMJ, particularly when conservative treatment has been ineffective. A major goal of TMJ reconstruction is the restoration of normal function. However, current TMJ prostheses that conform to the anatomical shape of TMJ cannot completely restore the physiological condylar kinematics; the geometry of the prostheses reduces the condylar ROM (van Loon et al., 1999; Zheng et al., 2019; Zou et al., 2019). The present study combined the TMJ fossa prosthesis with a functional condylar surface, which was different from the commercially-available TMJ prostheses, allowing physiologically accurate kinematics (Chen et al., 2022b).
The present study was the first to apply the ESCM concept to TMJ fossa prostheses, and a subject-specific mandibular musculoskeletal model was used to simulate mandibular movements, muscle activation, and resistance forces with different prostheses. As a subject-specific model for the human mandibular musculoskeletal system, it had been validated for predicting mandibular trajectories during jaw opening-closing movements in two previous studies, one with seven healthy subjects (Guo et al., 2022), and the other with the patients suffering from oral and maxillofacial tumors (Guo et al., 2023). Calculation precision of the musculoskeletal model would be verified in the further study with patients of TMJ replacement surgery. The kinematic results were compared among the envelope-based, stock Biomet, and ellipsoidal fossa prostheses. The maximum jaw opening magnitude for the stock Biomet fossa prosthesis was 35 mm, which was similar to the long-term outcomes for Biomet following TMJ replacement reported in previous studies (Gonzalez-Perez et al., 2016; Kanatsios et al., 2018). Compared to the Biomet, the envelope-based artificial fossa reduced jaw-opening muscle activation on the affected side and resistance on the intact side. It also increased the maximum jaw opening magnitude while maintaining the condylar ROM and bilateral contact forces. These results suggested that in terms of restoring the natural ROM of TMJ, the ESCM-based TMJ fossa prosthesis did show advantages and potential.
We developed the ellipsoidal fossa prosthesis based on the lower limb joint implants, such as the artificial hip joint (Hernigou et al., 2017). For the ellipsoidal fossa prosthesis design, we only considered condylar rotation and ignored its forward translation. We found that the ellipsoidal fossa limited the postoperative ROM of the TMJ. This indicates the importance of considering all condylar movements while designing prostheses, and reflects the rationale for envelope-based fossa prosthesis.
As showed in the results, there were advantages of the ESCM-based fossa prosthesis. It could not only improve the maximal jaw opening magnitude and condylar ROM, but also increased the efficiency of the jaw-opening process, as shown by the significant decrease in lateral pterygoid activation at maximum jaw opening. These indicated that the ESCM-based artificial fossa successfully replicated the functional anatomy of the mandibular musculoskeletal system. The physiological movement of TMJ could be affected by many factors, such as the posterior slope of articular eminence, the shape and deformation of articular disc, and traction of muscles (Mack, 1989). The articular eminence could provide a stable fulcrum for anterior condyle rotation (Van Eijden et al., 1997), while significant volume of the articular fossa and eminence bone has to be sacrificed for commercial condylar prostheses (Bai et al., 2015). In a study of 165 TMJs reconstructed using the Biomet stock prosthesis, Zhao et al. (2018) found that some patients required significant bone trimming or grafting to adjust the condyle-ramus angle and fossa for stable prosthesis implantation. As a result, the complete structure of articular eminence was damaged. On the other hand, the ESCM-based fossa prosthesis generated by the condylar functional surface data would provide physiological support and guidance for the condylar movement (Chen et al., 2022b; Chen et al., 2023). It may play a combined role of articular eminence, articular disc, capsule, ligament and so on, which could also provide the stable fulcrum for anterior condyle rotation as same as articular eminence. That increased the moment arms of the jaw-opening muscles (Spencer, 1998) and so could explain the significant decrease in digastric activation at the maximal jaw opening. Moreover, the guidance of ESCM-based fossa prosthesis for the condyle to slide forward could explain the significant decrease in lateral pterygoid activation at maximum jaw opening.
This study also had some limitations. First, the data used were obtained from a single subject. Studies with larger sample sizes will be required in the future. In addition, the subject of this study had no history of TMJ diseases, while total TMJ replacement is a biomechanical treatment option for patients with end-stage TMJ diseases (Sidebottom, 2008). For the patients whose articular fossa is damaged by the tumor and the condyle is intact and the condylar movement is normal, their envelope surfaces of condylar movement can still be obtained by the method used in this study. Moreover, in the case where the unilateral condyle is damaged but the patient could still perform normal mandibular movements, the mirroring of the intact side could be applied using the same method. This method could not be applied to those patients who were unable to perform normal mandibular movements, such as, patients with TMJ ankylosis. A method for predicting the shape of ESCM based on the facial morphology had been proposed in the previous study (Chen et al., 2023). Although further research was needed, it may be helpful in future ESCM data collection of patients with TMJ diseases whose normal mandibular movements could not be performed. Second, the complex TMJ morphology and loading patterns were simplified for our musculoskeletal models. TMJ cartilage and articular disk of the intact side were not modelled, which may have influenced the contact mechanics of the intact side. Besides, given that the mandibular kinematics would change for different other positions, more mastication loading conditions other than the maximum intercuspal position should be considered in the further study. Third, the condylar geometry on the affected side was simplified as an ellipsoid. An articular fossa prosthesis should be matched with a suitable condylar prosthesis based on the patient-specific functional anatomy. ESCM-based fossa prostheses still require some improvements. For example, the peak contact force for the envelop-based fossa was greater than that for Biomet at maximum jaw opening. This may have been because of the uneven distribution of contact forces, resulting from the bistable shape of the envelope-based fossa prosthesis, which could be influenced by the articular eminence morphology (Huang et al., 2021; Chen et al., 2022b). Compared with the envelope-based artificial fossa, the surface geometry of the Biomet fossa was flatter, making the contact force distribution more even. The uneven geometry of the envelope-based fossa prosthesis reduced the contact area with the condyle, resulting in an increased contact force. This would increase the potential for component wear, material failure, and TMJ dislocation (Kent et al., 1986; Giannakopoulos et al., 2012). Moreover, an anterior stop of the ESCM-based fossa prosthesis may be needed to avoid TMJ luxation, which will be considered in the further study. Despite these limitations, the study offers a novel perspective for TMJ fossa prostheses design. The customized envelope-based fossa prosthesis described in this study may allow the optimization of TMJ fossa prosthesis design.
5 Conclusion
A customized TMJ fossa prosthesis was successfully developed using the ESCM concept. Our study of musculoskeletal multibody modeling has highlighted its advantages and potential. The artificial fossa design successfully achieved a wider condylar ROM. It also reduced the activation of jaw opening muscles on the affected side and resistance on the intact side. This study showed that an ESCM-based approach may be useful for optimizing TMJ fossa prostheses design.
Data availability statement
The raw data supporting the conclusion of this article will be made available by the authors, without undue reservation.
Ethics statement
The studies involving humans were approved by the Institutional Review Board of Peking University School and Hospital of Stomatology, Beijing, China (Pkussirb-201947091). The studies were conducted in accordance with the local legislation and institutional requirements. The participants provided their written informed consent to participate in this study. Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author contributions
J-LW: Conceptualization, Data curation, Investigation, Methodology, Validation, Writing–original draft. JW: Conceptualization, Data curation, Investigation, Methodology, Validation, Writing–original draft. K-NC: Data curation, Visualization, Writing–original draft. J-QG: Funding acquisition, Resources, Software, Supervision, Writing–review and editing. X-LX: Funding acquisition, Resources, Software, Supervision, Writing–review and editing. C-BG: Conceptualization, Writing–review and editing.
Funding
The author(s) declare financial support was received for the research, authorship, and/or publication of this article. This work was supported by grants from the National Natural Science Foundations of China (grant number 12102035, 12132009), Beijing Municipal Science and Technology Commission (grant number Z201100005520055), Clinical Research Foundation of Peking University School and Hospital of Stomatology (grant number PKUSS-2023CRF205); and the Peking University Medicine Fund for World’s Leading Discipline or Discipline Cluster Development (grant number BMU2022XKQ003).
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
References
Bai, G., Yang, C., He, D., Zhang, X., and Abdelrehem, A. (2015). Application of fossa bone graft to stabilize stock total joint prosthesis in temporomandibular joint surgery. J. Craniomaxillofac. Surg. 43, 1392–1397. doi:10.1016/j.jcms.2015.06.048
Baqaien, M. A., Al-Salti, F. M., and Muessig, D. (2007). Changes in condylar path inclination during maximum protrusion between the ages of 6 and 12 years. J. Oral Rehabil. 34, 27–33. doi:10.1111/j.1365-2842.2006.01690.x
Broser, P. J., Marquetand, J., Middelmann, T., Sometti, D., and Braun, C. (2021). Investigation of the temporal and spatial dynamics of muscular action potentials through optically pumped magnetometers. J. Electromyogr. Kinesiol. 59, 102571. doi:10.1016/j.jelekin.2021.102571
Celebi, N., Rohner, E. C., Gateno, J., Noble, P. C., Ismaily, S. K., Teichgraeber, J. F., et al. (2011). Development of a mandibular motion simulator for total joint replacement. J. Oral Maxillofac. Surg. 69, 66–79. doi:10.1016/j.joms.2010.05.085
Chen, K. N., Jiang, J. Q., Wang, J. L., Sun, Y. C., Guo, C. B., and Xu, X. L. (2022a). Preliminary measurement and analysis of the condylar movement envelope surface parameters in healthy adults. Chin. J. Stomatol. 57, 1015–1021. doi:10.3760/cma.j.cn112144-20220630-00355
Chen, K. N., Wang, J., Chen, J. P., Wang, J. L., Sun, Y. C., Xu, X. L., et al. (2022b). Comparative study of temporomandibular articular fossa bone surface and the envelope surface of the condyle movement. Chin. J. Dent. Res. 25, 179–187. doi:10.3290/j.cjdr.b3317993
Chen, K., Zhang, Z., Jiang, J., Wang, J., Wang, J., Sun, Y., et al. (2023). Prediction of condylar movement envelope surface based on facial morphology. Heliyon 9, e17769. doi:10.1016/j.heliyon.2023.e17769
De Zee, M., Dalstra, M., Cattaneo, P. M., Rasmussen, J., Svensson, P., and Melsen, B. (2007). Validation of a musculo-skeletal model of the mandible and its application to mandibular distraction osteogenesis. J. Biomech. 40, 1192–1201. doi:10.1016/j.jbiomech.2006.06.024
Ferrario, V. F., Sforza, C., Zanotti, G., and Tartaglia, G. M. (2004). Maximal bite forces in healthy young adults as predicted by surface electromyography. J. Dent. 32, 451–457. doi:10.1016/j.jdent.2004.02.009
Flores, P., and Ambrósio, J. (2010). On the contact detection for contact-impact analysis in multibody systems. Multibody Syst. Dyn. 24, 103–122. doi:10.1007/s11044-010-9209-8
Giannakopoulos, H. E., Sinn, D. P., and Quinn, P. D. (2012). Biomet microfixation temporomandibular joint replacement system: a 3-year follow-up study of patients treated during 1995 to 2005. J. Oral Maxillofac. Surg. 70, 787–794. doi:10.1016/j.joms.2011.09.031
Gonzalez-Perez, L. M., Gonzalez-Perez-Somarriba, B., Centeno, G., Vallellano, C., and Montes-Carmona, J. F. (2016). Evaluation of total alloplastic temporo-mandibular joint replacement with two different types of prostheses: a three-year prospective study. Med. Oral Patol. Oral Cir. Bucal. 21, e766–e775. doi:10.4317/medoral.21189
Gruber, E. A., Mccullough, J., and Sidebottom, A. J. (2015). Medium-term outcomes and complications after total replacement of the temporomandibular joint. Prospective outcome analysis after 3 and 5 years. Br. J. Oral Maxillofac. Surg. 53, 412–415. doi:10.1016/j.bjoms.2014.12.010
Guo, J., Chen, J., Wang, J., Ren, G., Tian, Q., and Guo, C. (2022). EMG-assisted forward dynamics simulation of subject-specific mandible musculoskeletal system. J. Biomech. 139, 111143. doi:10.1016/j.jbiomech.2022.111143
Guo, J., Huang, H., Yu, Y., Liang, Z., Ambrósio, J., Zhao, Z., et al. (2020). Modeling muscle wrapping and mass flow using a mass-variable multibody formulation. Multibody Syst. Dyn. 49, 315–336. doi:10.1007/s11044-020-09733-1
Guo, J., Wang, J., Chen, J., Ren, G., Tian, Q., and Guo, C. (2023). Multibody dynamics modeling of human mandibular musculoskeletal system and its applications in surgical planning. Multibody Syst. Dyn. 57, 299–325. doi:10.1007/s11044-023-09876-x
Hannam, A. G. (2011). Current computational modelling trends in craniomandibular biomechanics and their clinical implications. J. Oral Rehabil. 38, 217–234. doi:10.1111/j.1365-2842.2010.02149.x
Hannam, A. G., Stavness, I. K., Lloyd, J. E., Fels, S. S., Miller, A. J., and Curtis, D. A. (2010). A comparison of simulated jaw dynamics in models of segmental mandibular resection versus resection with alloplastic reconstruction. J. Prosthet. Dent. 104, 191–198. doi:10.1016/S0022-3913(10)60120-5
Hernigou, P., Dubory, A., Potage, D., Roubineau, F., and Flouzat, L. C. H. (2017). Dual-mobility arthroplasty failure: a rationale review of causes and technical considerations for revision. Int. Orthop. 41, 481–490. doi:10.1007/s00264-016-3328-7
Huang, C., Xu, X., Li, L., Sun, Y., and Guo, C. (2021). Study on the reconstruction of a four-dimensional movement model and the envelope surface of the condyle in normal adults. Br. J. Oral Maxillofac. Surg. 60, 884–889. doi:10.1016/j.bjoms.2021.08.006
Imola, M. J., and Liddell, A. (2016). Temporomandibular joint reconstruction. Curr. Opin. Otolaryngol. Head. Neck Surg. 24, 336–342. doi:10.1097/MOO.0000000000000282
Kanatsios, S., Breik, O., and Dimitroulis, G. (2018). Biomet stock temporomandibular joint prosthesis: long-term outcomes of the use of titanium condyles secured with four or five condylar fixation screws. J. Craniomaxillofac. Surg. 46, 1697–1702. doi:10.1016/j.jcms.2018.07.002
Kent, J. N., Block, M. S., Homsy, C. A., Prewitt, J. M. R., and Reid, R. (1986). Experience with a polymer glenoid fossa prosthesis for partial or total temporomandibular joint reconstruction. J. Oral Maxillofac. Surg. 44, 520–533. doi:10.1016/s0278-2391(86)80092-1
Kiehn, C. L., Desprez, J. D., and Converse, C. F. (1974). A new procedure for total temporomandibular joint replacement. Plast. Reconstr. Surg. 53, 221–226. doi:10.1097/00006534-197402000-00022
Koeppel, T., Sapin-De, B. E., and Bonnet, A. S. (2015). Three dimensional functional analysis of the human mandibular movements. Comput. Methods Biomech. Biomed. Engin. 18, 1964–1965. doi:10.1080/10255842.2015.1069569
Koolstra, J. H., and Van Eijden, T. M. (2005). Combined finite-element and rigid-body analysis of human jaw joint dynamics. J. Biomech. 38, 2431–2439. doi:10.1016/j.jbiomech.2004.10.014
Lloyd, D. G., and Besier, T. F. (2003). An EMG-driven musculoskeletal model to estimate muscle forces and knee joint moments in vivo. J. Biomech. 36, 765–776. doi:10.1016/s0021-9290(03)00010-1
Mack, P. J. (1989). A computer analysis of condylar movement as determined by cuspal guidances. J. Prosthet. Dent. 61, 628–633. doi:10.1016/0022-3913(89)90290-4
Mercuri, L. G. (2000). The use of alloplastic prostheses for temporomandibular joint reconstruction. J. Oral Maxillofac. Surg. 58, 70–75. doi:10.1016/s0278-2391(00)80020-8
Mercuri, L. G., Wolford, L. M., Sanders, B., White, R. D., Hurder, A., and Henderson, W. (1995). Custom CAD/CAM total temporomandibular joint reconstruction system: preliminary multicenter report. J. Oral Maxillofac. Surg. 53, 106–115. doi:10.1016/0278-2391(95)90381-x
Merlini, L., and Palla, S. (1988). The relationship between condylar rotation and anterior translation in healthy and clicking temporomandibular joints. Schweiz. monatsschr. Zahnmed. 98, 1191–1199.
Modenese, L., and Kohout, J. (2020). Automated generation of three-dimensional complex muscle geometries for use in personalised musculoskeletal models. Ann. Biomed. Eng. 48, 1793–1804. doi:10.1007/s10439-020-02490-4
Oberg, T., Carlsson, G. E., and Fajers, C. M. (1971). The temporomandibular joint. A morphologic study on a human autopsy material. Acta Odontol. Scand. 29, 349–384. doi:10.3109/00016357109026526
Owashi, V. K. P., Sapin-De, B. E., and Bonnet, A. S. (2017). Electromyography of the masticatory muscles during biting. Comput. Methods Biomech. Biomed. Engin. 20, 155–156. doi:10.1080/10255842.2017.1382908
Quental, C., Folgado, J., Ambrósio, J., and Monteiro, J. (2012). A multibody biomechanical model of the upper limb including the shoulder girdle. Multibody Syst. Dyn. 28, 83–108. doi:10.1007/s11044-011-9297-0
Sidebottom, A. J. (2008). Guidelines for the replacement of temporomandibular joints in the United Kingdom. Br. J. Oral Maxillofac. Surg. 46, 146–147. doi:10.1016/j.bjoms.2006.12.001
Silva, M. T. D., and Ambrósio, J. (2003). Solution of redundant muscle forces in human locomotion with multibody dynamics and optimization tools. Mech. Based Des. Struct. Mach. 31, 381–411. doi:10.1081/SME-120022856
Sonnenburg, I., and Sonnenburg, M. (1985). Total condylar prosthesis for alloplastic jaw articulation replacement. J. Maxillofac. Surg. 13, 131–135. doi:10.1016/s0301-0503(85)80033-3
Spencer, M. A. (1998). Force production in the primate masticatory system: electromyographic tests of biomechanical hypotheses. J. Hum. Evol. 34, 25–54. doi:10.1006/jhev.1997.0180
Thelen, D. G. (2003). Adjustment of muscle mechanics model parameters to simulate dynamic contractions in older adults. J. Biomech. Eng. 125, 70–77. doi:10.1115/1.1531112
Van Eijden, T. M., Korfage, J. A., and Brugman, P. (1997). Architecture of the human jaw-closing and jaw-opening muscles. Anat. Rec. 248, 464–474. doi:10.1002/(sici)1097-0185(199707)248:3<464::aid-ar20>3.0.co;2-m
Van Loon, J. P., Falkenström, C. H., De Bont, L. G., Verkerke, G. J., and Stegenga, B. (1999). The theoretical optimal center of rotation for a temporomandibular joint prosthesis: a three-dimensional kinematic study. J. Dent. Res. 78, 43–48. doi:10.1177/00220345990780010501
Walker, P. S. (2001). A new concept in guided motion total knee arthroplasty. J. Arthroplasty. 16, 157–163. doi:10.1054/arth.2001.28723
Wang, Z. W., Wen, L., Luan, Y. C., Ma, D. S., Dong, X., Cheng, C. K., et al. (2021). Restoration of joint inclination in total knee arthroplasty offers little improvement in joint kinematics in neutrally aligned extremities. Front. Bioeng. Biotechnol. 9, 673275. doi:10.3389/fbioe.2021.673275
Westermark, A. (2010). Total reconstruction of the temporomandibular joint. Up to 8 years of follow-up of patients treated with Biomet(®) total joint prostheses. Int. J. Oral Maxillofac. Surg. 39, 951–955. doi:10.1016/j.ijom.2010.05.010
Wolford, L. M., Cottrell, D. A., and Henry, C. H. (1994). Temporomandibular joint reconstruction of the complex patient with the Techmedica custom-made total joint prosthesis. J. Oral Maxillofac. Surg. 52, 2–10. doi:10.1016/0278-2391(94)90003-5
Wolford, L. M., Pitta, M. C., Reiche-Fischel, O., and Franco, P. F. (2003). TMJ Concepts/Techmedica custom-made TMJ total joint prosthesis: 5-year follow-up study. Int. J. Oral Maxillofac. Surg. 32, 268–274. doi:10.1054/ijom.2002.0350
Woodford, S. C., Robinson, D. L., Mehl, A., Lee, P. V. S., and Ackland, D. C. (2020). Measurement of normal and pathological mandibular and temporomandibular joint kinematics: a systematic review. J. Biomech. 111, 109994. doi:10.1016/j.jbiomech.2020.109994
Xu, X., Luo, D., Guo, C., and Rong, Q. (2017). A custom-made temporomandibular joint prosthesis for fabrication by selective laser melting: finite element analysis. Med. Eng. Phys. 46, 1–11. doi:10.1016/j.medengphy.2017.04.012
Yao, X., Fan, S., An, G., and Wang, Z. (2011). The measurements and analysis of temporomandibular joint bony structures. J. Pract. Stomatol. 06, 801–804. doi:10.3969/j.issn.1001-3733.2011.06.016
Zhao, J., Zou, L., He, D., and Ellis, E. R. (2018). Comparison of bone adaptation after modification in biomet standard alloplastic temporomandibular joint prostheses. J. Craniomaxillofac. Surg. 46, 1707–1711. doi:10.1016/j.jcms.2018.07.024
Zhao, Q., Sun, N., Zhang, F., Song, D., Lu, Z., Sun, N., et al. (2019). Measurement of temporomandibular joint and surrounding accessory structures. J. Shandong Univ. Health Sci. 01, 87–91. doi:10.6040/j.issn.1671-7554.0.2018.766
Zheng, J., Chen, X., Jiang, W., Zhang, S., Chen, M., and Yang, C. (2019). An innovative total temporomandibular joint prosthesis with customized design and 3D printing additive fabrication: a prospective clinical study. J. Transl. Med. 17, 4. doi:10.1186/s12967-018-1759-1
Zou, L., Zhao, J., and He, D. (2019). Preliminary clinical study of Chinese standard alloplastic temporomandibular joint prosthesis. J. Craniomaxillofac. Surg. 47, 602–606. doi:10.1016/j.jcms.2019.01.045
Keywords: articular fossa prosthesis, envelope surface, musculoskeletal simulation, flexible multibody dynamics, temporomandibular joint, mandibular movement
Citation: Wang J-L, Wang J, Chen K-N, Guo J-Q, Xu X-L and Guo C-B (2023) Designing customized temporomandibular fossa prosthesis based on envelope surface of condyle movement: validation via in silico musculoskeletal simulation. Front. Bioeng. Biotechnol. 11:1273263. doi: 10.3389/fbioe.2023.1273263
Received: 05 August 2023; Accepted: 16 October 2023;
Published: 31 October 2023.
Edited by:
Zhenxian Chen, Chang’an University, ChinaReviewed by:
Giovanni Badiali, University of Bologna, ItalyKaushik Mukherjee, Indian Institute of Technology Delhi, India
Copyright © 2023 Wang, Wang, Chen, Guo, Xu and Guo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jian-Qiao Guo, Z3VvamlhbnFpYW9AYml0LmVkdS5jbg==; Xiang-Liang Xu, a3F4eGxAMTI2LmNvbQ==
†These authors have contributed equally to this work
 Jun-Lin Wang
Jun-Lin Wang Jing Wang1†
Jing Wang1† Jian-Qiao Guo
Jian-Qiao Guo Xiang-Liang Xu
Xiang-Liang Xu Chuan-Bin Guo
Chuan-Bin Guo