- 1Faculty of Health Sciences, University of Bielefeld, Bielefeld, Germany
- 2Department of Business and Economics, Chair of Statistics and Econometrics, Johannes Gutenberg University Mainz, Mainz, Germany
- 3Department of Global Health, Institute of Public Health and Nursing Research, University of Bremen, Bremen, Germany
- 4Heidelberg Institute of Global Health, Heidelberg University Hospital, Heidelberg, Germany
- 5Division of Primary Care and Population Health, Department of Medicine, Stanford University, Stanford, CA, United States
Climate change poses a serious threat to human health and is a key driver of both health system stress and disaster-related health impacts. As climate-related crises become more frequent and intense, the likelihood of climate-induced disasters increases, bringing a wide range of health consequences, including climate-sensitive diseases (CSDs) and exacerbating health inequities. Strengthening disaster preparedness in health facilities is essential for managing increased service demands, ensuring continuity of care, and minimizing the impact of disasters on communities. However, there is limited evidence on how well health facilities are prepared to manage climate-related disasters and deliver CSD diagnosis and treatment services, particularly in low-and middle-income countries (LMICs) such as Nepal. This study aims to address that gap by linking data from the 2021 Nepal health facility Service Provision Assessment survey with local-level climate-related disaster data from the Nepal Disaster Risk Portal (2018–2020). We explore climate related disaster preparedness and the availability of CSD-related services across different types of health facilities, assessing overall emergency preparedness and the availability of six CSD services based on their past exposure to disasters. Furthermore, we compare differences in preparedness and CSD service availability between facilities with high and low levels of disaster exposure. The study provides an overview of how well various types of health facilities are prepared to respond to climate-related disasters and CSDs, while also highlighting disparities in preparedness and service availability across facility types. Although the findings indicate some degree of adaptation of some type of health facilities to climate-related disaster exposure, it calls for comprehensive assessments that integrate all components of a climate-resilient health system as defined by the WHO, to support evidence-based planning and strengthen Nepal’s progress toward a climate-resilient health system.
1 Introduction
Climate change is a global health priority, impacting public health through both direct and indirect effects. Factors such as rising temperatures, rising sea levels, ocean acidification, and more extreme weather events contribute to increased health vulnerabilities (Keim, 2008; Birkmann and von Teichman, 2010). With the increasing frequency of extreme weather and climate-related crises, the risk of climate-related disasters grows, leading to a wide range of health consequences (International O, 2025). These include immediate effects such as injuries and fatalities, as well as natural and human system-mediated impacts such as air pollution, exposure to climate sensitive diseases (CSD) including vector-borne diseases, mental stress and undernutrition (Guihenneuc et al., 2023).
Healthcare systems play a critical role in managing and recovering from disasters impacts. Health facilities (HFs) should remain operational during disasters, with sufficient capacity to manage surges in patient volume. They are required to respond to evolving threats and operational challenges, and to coordinate effectively with broader emergency management systems (Arboleda et al., 2009). As such, effective disaster preparedness in HFs is essential to ensuring service continuity, managing increasing demand, and minimizing disaster effects on communities (Arboleda et al., 2009).
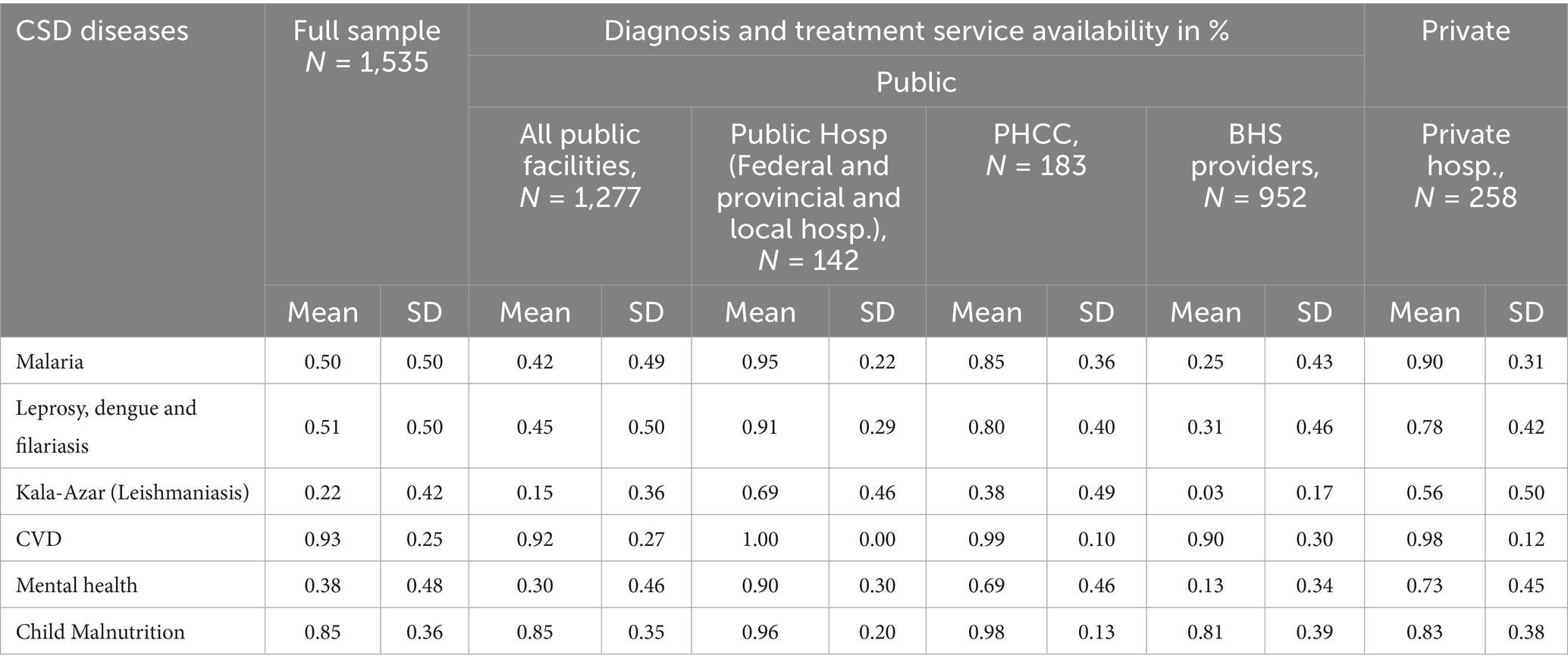
The World Health organization (WHO) promotes a climate-resilient health systems framework, which comprises ten key components: (1) leadership, (2) a climate-smart workforce, (3) risk assessments, (4) early warning systems, (5) research, (6) sustainable infrastructure, (7) environmental health management, (8) climate-informed programs, (9) emergency preparedness, and (10) financing. Among these, emergency preparedness and management are critical elements for ensuring that the health systems can anticipate, respond to, and recover from climate-related shocks (WHO, 2015). These components align with WHO’s six health system building blocks: workforce, information systems, medical technologies, financing, governance, and service delivery (Figure 1).
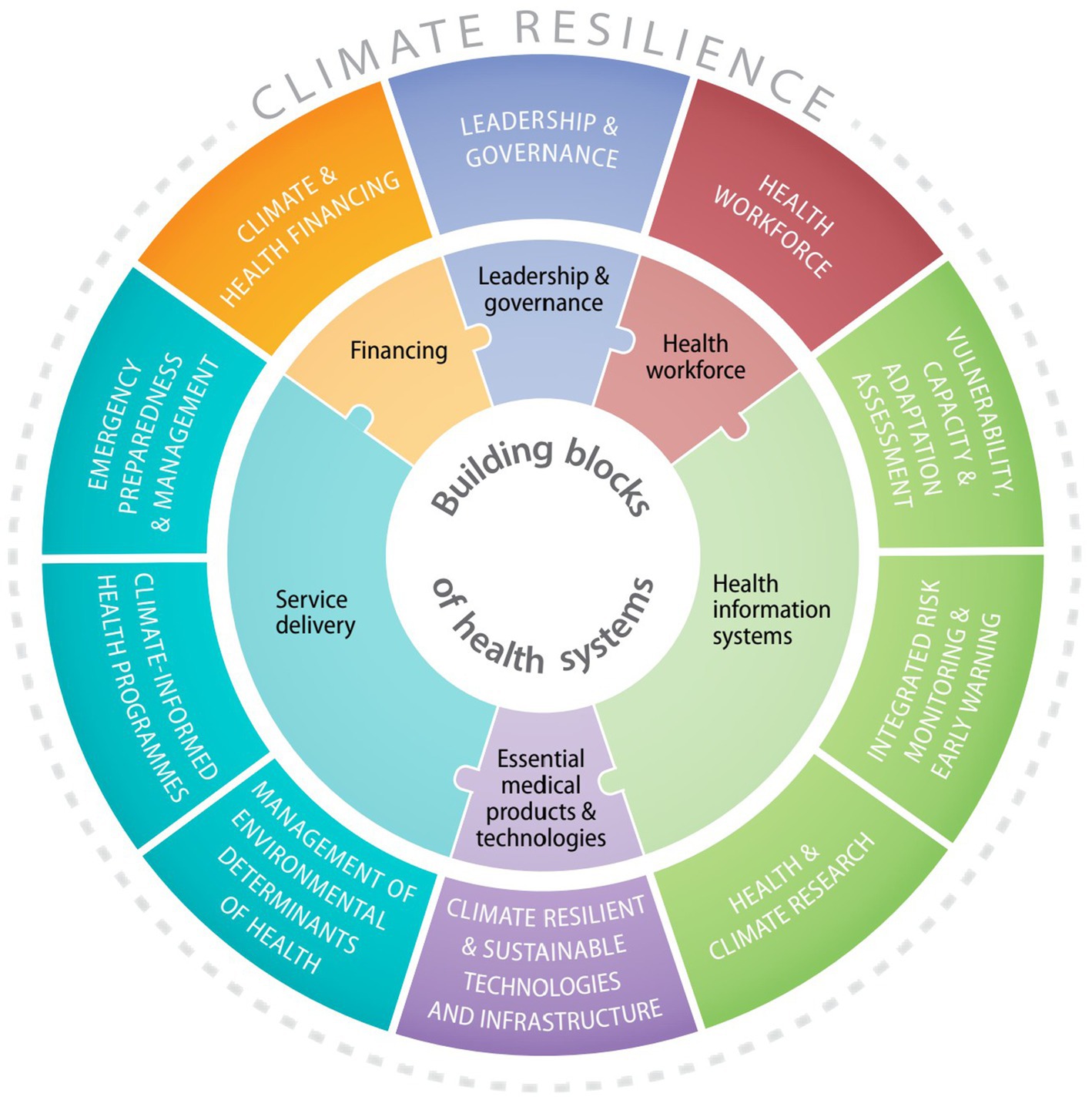
Figure 1. Ten components comprising the WHO Operational framework for climate-resilient health systems and the main connections to the building blocks of health systems (WHO, 2015).
Furthermore, the WHO provides guidelines for assessing the Hospital Safety Index (HSI) for hospitals focusing on several key domains such as hazard exposure, structural and non-structural safety, health system capacity, and hospital vulnerabilities (WHO, 2015). Similarly, the Health Emergency and Disaster Risk Management (Health EDRM) framework also presents a comprehensive, risk-based approach to strengthen health systems’ preparedness, response, and resilience to disasters (WHO, 2019). Despite the availability of these frameworks, there is no standard definition in the literature for assessing disaster preparedness. A systematic review reveals a lack of consensus regarding the definition and implementation of disaster preparedness in hospitals (Verheul and Dückers, 2020).
Emergency preparedness and disaster preparedness are terms often used interchangeably in literature. The WHO and the United Nations Office for Disaster Risk Reduction (UNDRR) define these concepts in similar terms, but with notable differences in scope. The WHO describes emergency preparedness as the knowledge and capacities to effectively anticipate, respond to, and recover from the impacts of likely, imminent, or current hazardous events or conditions, which may or may not escalate into disasters (WHO, 2017). In contrast, the UNDRR defines disaster preparedness more specifically as the knowledge and capacities developed by various stakeholders to anticipate, respond to, and recover from the impacts of likely, imminent, or current disasters. This includes activities such as contingency planning, stockpiling essential equipment and supplies, establishing coordination and evacuation protocols, disseminating public information, and conducting related training and drills (UNDRR, 2017). Response is one of the key elements within the broader framework of emergencies and/or disaster preparedness. In this paper, even if the terms ‘disaster preparedness’ and ‘emergency preparedness’ are sometimes used interchangeably, our focus is specifically on climate-related disasters.
Although disaster preparedness and response efforts for climate resilience increasingly recognize the critical role of the health sector, a limited understanding of how this recognition is translated into practice remains. Insights from the literature highlight key components of overall HF preparedness, such as the development of disaster plans, adequate staffing, effective coordination, and training (Verheul and Dückers, 2020; WHO, 2017). However, most existing studies to date addressing this issue have primarily focused on the infrastructural capacity for understanding resilience of HFs. In contrast, comparatively less attention has been given to their preparedness for managing climate-related disaster events and providing diagnostic and treatment services for CSDs, which commonly emerge in the aftermath of such events (Heidaranlu et al., 2015). Moreover, the majority of disaster preparedness research originates from high-income countries (HICs) and is largely centered on tertiary level hospitals. A scoping review mapping the academic evidence base for disaster planning and management in the health sector within Low-and Middle-Income Countries (LMICs) reveals a significant lack of research on disaster preparedness in these regions. While in HICs, the focus is primarily on emergency preparedness, efforts in LMICs are more often directed toward disaster response (Lee et al., 2014). Despite the growing number of studies on the health impacts of disasters and mounting evidence indicating that LMICs are more vulnerable to climate related disasters, the evidence supporting how to best ensure preparedness of HFs for addressing the health effects of disasters in these settings remains understudied (Schwerdtle et al., 2024).
1.1 Key terms and concepts used in the study
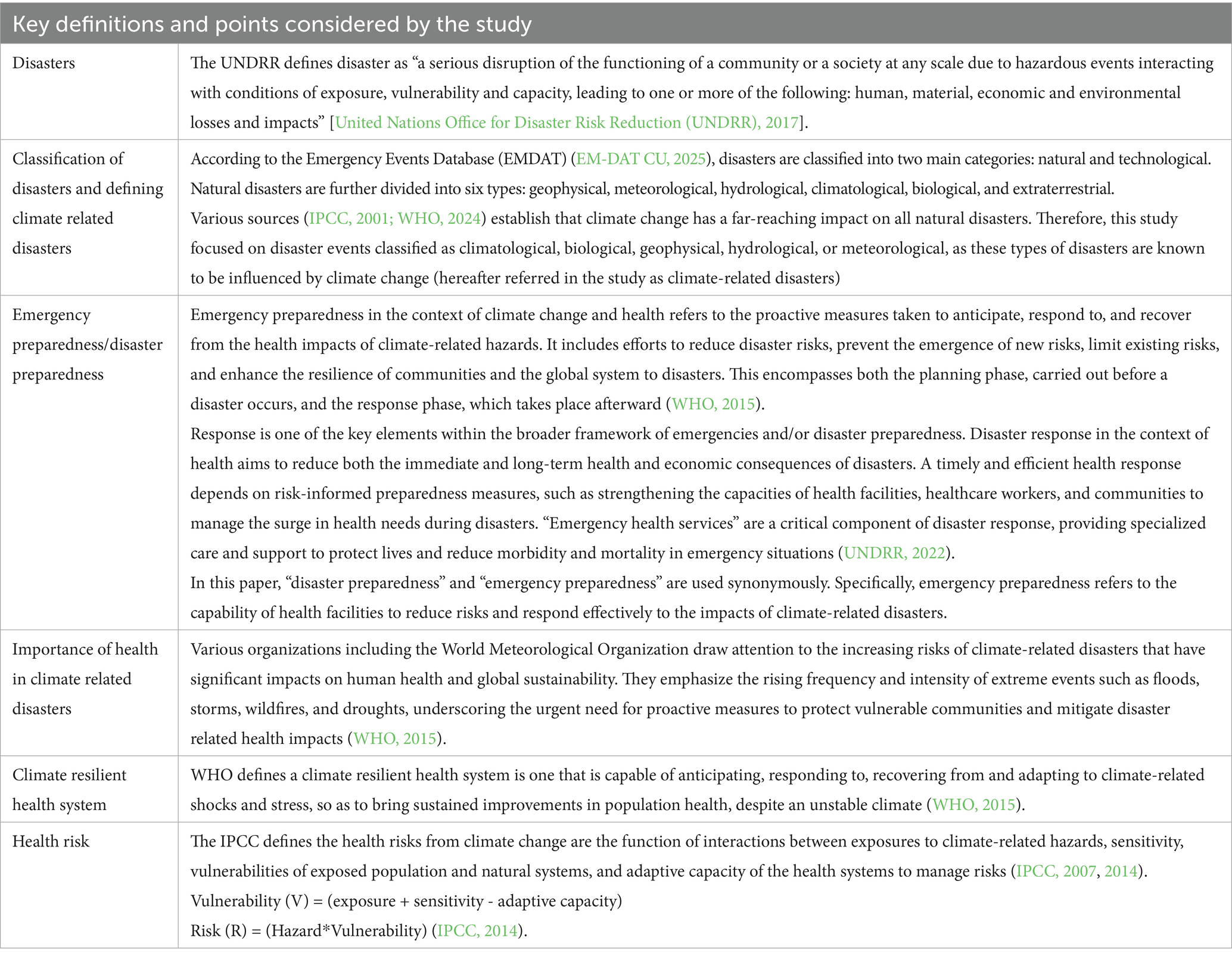
Table 1 summarizes the key definitions and concepts that guide this study, highlighting disaster classifications and the central role of health systems and preparedness in reducing climate-related risks and impacts.
1.2 Climate change and disaster preparedness in Nepal
Nepal, a federal democratic republic in South Asia, is a landlocked country with a population of more than 29 million. Divided into three ecological regions-mountains, hills, and the Terai, the country’s terrain varies greatly, ranging from towering mountains like Mount Everest (8,848 m), to low-lying plains in the south where elevations drop below 100 meters (Bank WBGaAD, 2021). Nepal ranks fourth on the Global Climate Risk Index, highlighting its vulnerability to climate-related hazards (MoFE, 2021).
Since transitioning to a federal governance system in 2017, the country has operated through three administrative levels: one federal government, seven provincial governments and 753 local governments (which include metropolitan cities, sub-metropolitan cities, urban municipalities, and rural municipalities) (MoFE, 2021). Each year, the country experiences frequent disaster events that result in significant loss of life (MoHA G, 2022a). Many of these fatalities are caused by climate-related disasters such as thunderstorms, forest fires, and floods (MoHA G, 2022b). With ongoing climate change, both the frequency and severity of these climate related disaster events are projected to increase (Tome et al., 2022). The country’s diverse geography further heightens its susceptibility to extreme climatic events. For example, the Terai region, in particular, faces increased flood risks during the monsoon season when intense rainfall coincides with snow and glacier melt from higher elevations (MoHA G, 2024).
The Nepal National Adaptation Program of Action (NAPA) identifies public health as one of the sectors most vulnerable to climate change (MoFE, 2021). Growing evidence indicates that climate variability is increasingly affecting health outcomes, with vulnerabilities differing across regions and diseases. For instance, seven districts in the Terai and two in the Far West Mountains are classified as highly vulnerable, while areas in the Central Terai, Mid-Western Hills, and Western Hills are considered moderately vulnerable. In contrast, parts of the Western and Central Hills exhibit relatively low vulnerability (MoH G, 2015).
The country also reports varying levels of CSD-specific vulnerabilities. Between 2005 and 2020, malaria cases in Nepal exhibited a gradual decline, with the majority of districts reporting fewer than 1,500 cases annually; however, several districts recorded over 3,000 cases during the period from 2005 to 2012. Japanese encephalitis incidence remained relatively stable below 1,000 cases per year, with a significant increase observed in 2017. Dengue cases increased markedly in 2020. Although undernutrition cases fluctuated overall, certain districts experienced a rise in prevalence. Additionally, new cases of kala-azar were reported in the hilly regions. Reported cases of mental illness escalated sharply, reaching a peak following the 2015 earthquakes (MoHP G, 2022). These health challenges are influenced by factors such as geography, population dynamics, settlement patterns, occupational exposure, and socio-cultural conditions (MoHA G, 2024). Effectively addressing these issues may require tailored, context specific interventions to build resilience.
1.3 Disaster preparedness governance structures in Nepal
The Government of Nepal (GoN) is a signatory to the Sendai Framework for Disaster Risk Reduction (SFDRR) (MoHA G, 2022c), and the Constitution of Nepal prioritizes disaster risk management (DRM) for all levels of government (MoFGA G, 2023). Key government policies such as the MoHA (2018b), the GoN (2017, amended 2018), and the National Disaster Risk Reduction National Strategic Plan of Action (DRRNSPA) (2018–2030), outline the need for enhanced disaster preparedness measures to strengthen disaster governance and response in the country. These documents emphasize priorities such as hazard modeling, emergency medical care enhancement, and integrated climate change adaptation with sustainable development (MoHA G, 2022c). For example, the DRRNSPA sets 32 targets, 18 priority actions, and over 270 activities to strengthen disaster response and risk management in Nepal (MoHA, 2018a). In alignment with SFDRR priorities, Nepal has also undertaken significant efforts in understanding disaster including: understanding disaster risk, strengthening disaster risk governance to manage disaster risk, investing in disaster risk reduction for resilience, and enhancing disaster preparedness for effective response and to “Build Back Better” in recovery, rehabilitation, and reconstruction (MoHA G, 2022b).
Nepal’s disaster management framework is multi-tiered, reflecting its federal governance structure (Figure 2). At the federal level, the National Council for Disaster Risk Reduction and Management (NCDRRM) is responsible for policy formulation, while the Ministry of Home Affairs (MoHA) leads disaster response. The National Disaster Risk Reduction and Management Authority (NDDRMA) (NDRRMA G, 2022), established in 2019 under the leadership of MoHA, implements disaster-related policies and coordinates efforts across all levels of government. It also manages the Nepal Disaster Risk Reduction (NDRR) portal, which records all disasters occurring across the country (MoHA G, 2019). This disaster database records 18 disaster events, most of them are climate related (MoHA G, 2024). Additionally, the Cluster Coordination Mechanism under the MoHA includes representatives from all relevant line ministries, facilitating coordinated disaster response. This includes the Ministry of Health and Population (MoHP) and the Ministry of Forests and Environment (MoFE) (MoFE, 2021), the latter serving as the focal agency for climate change-related issues in Nepal.
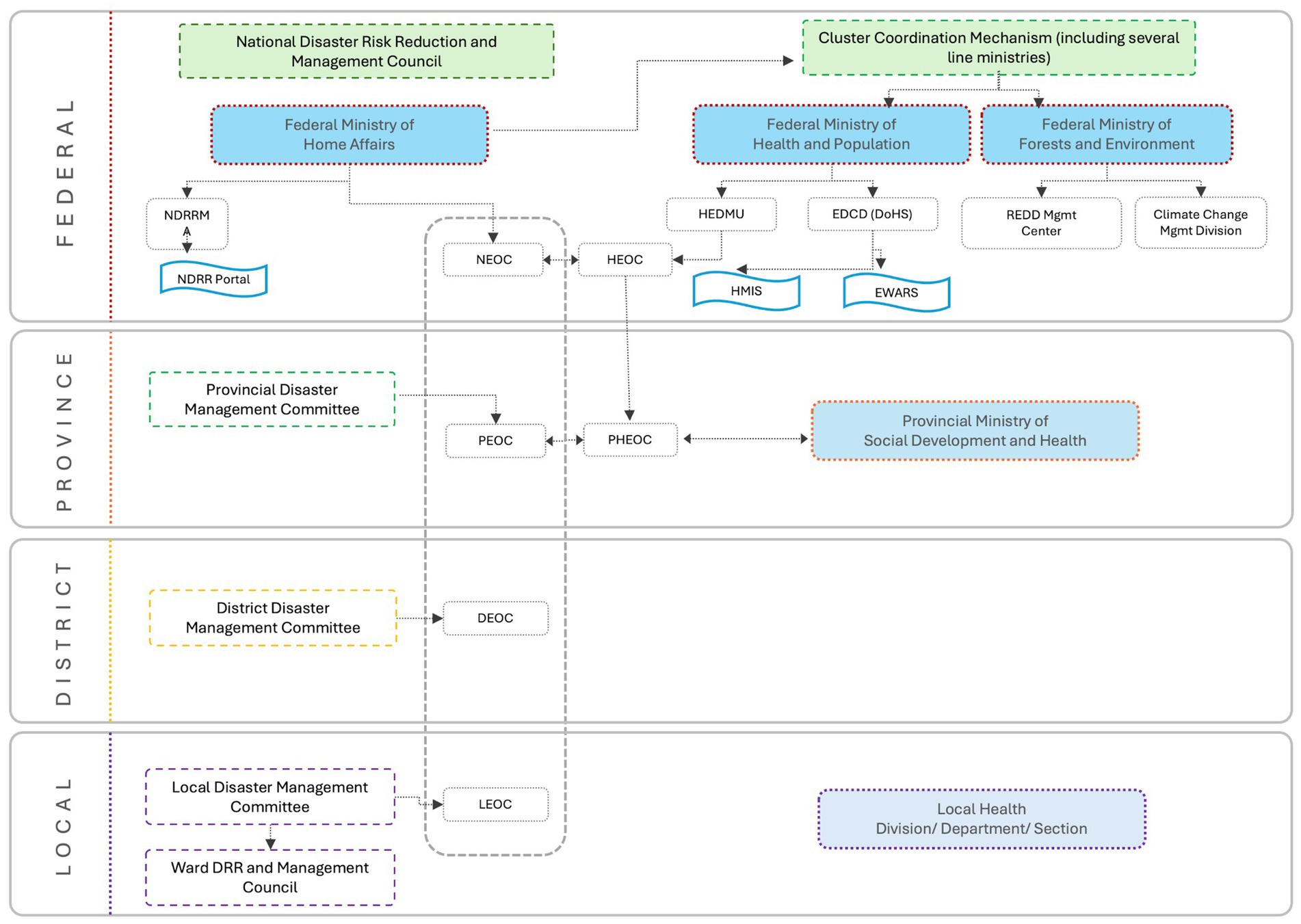
Figure 2. Key institutional arrangement of Nepal to manage disasters and climate related health impacts [adapted from Nepal, Pashupati NRK, Sharma, Bishnu Prasad Pangali (2018).
At the provincial level, Provincial Disaster Management Committees (PDMCs) develop disaster plans and coordinate activities between national and local authorities. At the local level, Local Disaster Management Committees (LDMCs) and Ward Level Disaster Management Committees (WDMCs) focus on community-based preparedness and response (MoFGA G, 2023).
The MoHP is integral to disaster risk management (DRM) and climate change-related health concerns. Several policy documents outline the MoHP’s responsibilities, including the National Climate Change Policy 2019; National Health Policy 2019; the Nepal Health Sector Strategic Plan (2023–2030); and the Health National Adaptation Plan (H-NAP) 2016–2020 (Dhimal et al., 2017). Within the MoHP, the Health Emergency and Disaster Management Unit (HEDMU) oversees disaster preparedness, response, and recovery, while the Health Emergency Operation Center (HEOC) serves as the central command for emergency health response. At the sub-national level, provincial HEOCs have been established in all seven provinces to act as command centers for provincial governments during all emergencies and disasters and to coordinate with relevant health and non-health sector partners, to enhance preparedness and response readiness (WHO Ma, 2021).
Additionally, the Epidemiology and Disease Control Division (EDCD) of the MoHP monitors disease outbreaks, epidemics, and a few CSDs. As part of these efforts, an Early Warning and Reporting System (EWARS) a hospital-based sentinel surveillance system has been established in 134 hospitals across Nepal. EWARS is designed to strengthen the flow of information on outbreak-prone and vector-borne diseases and support timely responses by Rapid Response Teams (RRTs) at federal, provincial, and local levels. It complements the MoHP’s Health Management Information System (HMIS) by providing weekly, timely reports on six priority diseases/syndromes along with other epidemic-prone conditions. However, effective reporting and coordination on climate change related issues among various divisions within the MoHP and other government sectors remains a persistent challenge (Khanal and Boeckmann, 2025).
Owing to the increasing frequency of disasters in the country (MoFE G, 2021), the MoHP has prioritized strengthening the resilience of health institutions, focusing on enhancing the capacity of hospitals and staff to respond effectively to disasters and public health emergencies. With support from the WHO, HEOC has helped hospitals to develop Hospital Disaster Preparedness Response Plans (HDPRPs) and to train personnel on various aspects of disaster preparedness such as implementing the Hospital Incident Command System (ICS) and managing surge capacity (Phuyal et al., 2023; Adhikari et al., 2024).
The MoHP in collaboration with the Demographic and Health Survey (DHS) Program, conducted two rounds of the Service Provision Assessment (SPA) in 2015 and 2021. Alongside evaluating other health programs, these surveys included some indicators related to disaster preparedness, response capacity, and the availability of services for CSDs in selected HFs in Nepal (Ministry of Health and Population, Nepal; New ERA, Nepal; and ICF Nepal, 2022).
With the increasing threats posed by climate change, the GoN is committed to strengthening disaster preparedness and response, including efforts to address potential health impacts. However, despite these initiatives, there is still a limited understanding of how prepared HFs are to manage the health impacts of climate change, including those associated with climate-related disaster events and the provision of CSD-related services. Furthermore, existing data from different government bodies have remained largely disconnected, preventing a comprehensive understanding of the intersection between climate related disaster frequency and the preparedness of HFs to respond to these climate related disaster events.
Drawing on data from the SPA survey 2021 and the Nepal Disaster Risk Reduction (NDRR) portal of MoHA, this study aimed to explore the preparedness of HFs for climate related disaster management and their service availability of CSDs across different levels of HFs in Nepal, particularly in relation to the frequency of climate related disaster events from 2018 to 2020. Specific objectives of the study included:
1. To understand disaster preparedness and CSD service availability across different types of HFs.
2. Based on climate-related disaster events exposure between 2018 and 2020:
a. comparing disaster preparedness and CSD service availability across facilities.
b. assessing the availability of all six disaster preparedness indicators in HFs.
c. exploring service availability for all six CSDs across different facility types.
2 Materials and methods
2.1 Survey data from the Service Provider Assessment (SPA) 2021
This study used data from the 2021 SPA survey, which assessed healthcare service availability, facility readiness, service quality, and client satisfaction in HFs across Nepal. The primary aim of the survey was to evaluate the availability and quality of essential health services, including maternal and newborn care, child health, family planning, NCDs, mental health, and selected infectious diseases. It also examined HF preparedness to deliver these services, identified gaps in resources and processes, and assessed adherence to quality standards. The survey was structured to yield nationally representative data across various types of HFs and aimed to produce representative findings for all seven provinces in Nepal. Detailed sampling information is available in the SPA 2022 report (Ministry of Health and Population, Nepal; New ERA, Nepal; and ICF Nepal, 2022).
Using a stratified sampling approach, the SPA survey collected data from 1,633 HFs, including their GPS location coordinates. While the data only reports on the district location of the HFs, we merged in local level information based on an ESRI shapefile (vector data storage format for geographic information systems) including administrative boundaries at the local level and the GPS locations. This step was important to link HF information to disaster event data at the local level (instead of the less precise district-level information). To this end, we linked the point layer of the HFs from the SPA survey with the polygon layer of the ESRI shape file. For each SPA point, we calculated the polygon in which it was located and extracted the corresponding local level name (Nepal OD, 2018). Subsequently, we merged in climate-related disaster exposure at the local level (see 2.2).
2.1.1 Selection of health facility/health outcome indicators
Altogether, six key indicators related to emergency and disaster preparedness, four indicators on basic emergency services and service availability for six CSDs were included in the analysis.
Given that this study relied on secondary data from the 2021 SPA survey, the analysis was constrained to the indicators available within the dataset. All disaster preparedness indicators documented under the disaster management section of the SPA assessment were selected. This comprised of six components (a) drill-down exercises, reported and (b) observed (c) outbreak management plans, (d) mass casualty plans, and the presence of (e) functional Incident Command System (ICS) and (f) Rapid Response Team (RRT).
Several of these indicators also align with the domains of HSI (WHO, 2015) and the WHO’s Health Emergency and Disaster Risk Management framework (Health EDRM) (WHO, 2019).
For basic emergency services, only those explicitly and directly related to disaster preparedness were selected. These included the availability of (a) general emergency management and referral, (b) minor surgical services, (c) acute pain management and referral, and (d) isolation rooms.
The selection of CSDs was based on Nepal’s Health Vulnerability and Risk Assessment for Climate Change, conducted by the MoHP which identified 12 CSDs. This includes seven vector-borne diseases (malaria, kala-azar, Japanese encephalitis, scrub typhus, dengue, zika, and chikungunya), two food-and water-borne diseases (cholera and acute gastroenteritis), one respiratory disease (severe acute respiratory infections), and two other conditions (undernutrition and mental illness) (MoHP G, 2022). Only five of these diseases (malaria, leprosy/dengue/filariasis, kala-azar (leishmaniasis), mental health and child malnutrition) were covered in the 2021 SPA (Ministry of Health and Population, Nepal; New ERA, Nepal; and ICF Nepal, 2022), and were selected for analysis. In addition, CVD was included due to its increasing recognition as a CSD, linking environmental stressors to adverse cardiovascular outcomes (Watts et al., 2021; Kazi et al., 2024), and its inclusion as an indicator in the SPA assessment.
We excluded standalone HIV Testing and Counselling (HTC) centers from the SPA 2021 dataset because they do not offer any additional CSD-related services.
2.2 Climate related disaster events data
Climate-related disaster event data was sourced from the NDRR (Nepal Disaster Risk Reduction Portal [Internet], n.d.) Portal of the MoHA, a public domain dataset available from the GoN. We selected data on disasters occurring between 2018 and 2020 at the local levels where the 2021 SPA survey was conducted.
As Nepal began its transition to a federal system in 2015, no complete local-level data was available for earlier time periods. Since the transition lasted until 2017, we considered data from 2018 onwards to capture more accurate representation of the new federal system, in which provincial and local governments took on more clearly defined roles within the federal framework. Despite this, climate related disaster events in many cases were still reported according to the old administrative structures (district wise). Moreover, since some VDCs were restructured at the ward level, certain entries required manual adjustments. To address this, we compared the originally reported locations of these events (from the NDRR portal) with the updated list of administrative units from various government sources and reclassified them according to the new local levels. This alignment enabled effective integration of the disaster events data with the SPA 2021 data. The dataset covered the total number of disaster events, categorized by type and location.
2.2.1 Selection of disaster events data
To capture and classify the disaster events in Nepal, we followed the International Disaster Database classification for disasters (EMDAT) (EM-DAT CU, 2025) which is also adopted by the NDRR guideline (GoN, 2017). The study focused on natural disasters classified as climatological, biological, geophysical, hydrological, or meteorological, as these types of disasters are known to be influenced by climate change (referred to as climate-related disasters as explained in Table 1) (EM-DAT CU, 2025).
Furthermore, only climate related disaster events with complete data for all 3 years (2018–2020) were included in the analysis. As a result, six types of disaster events were selected: floods, landslides, thunderbolts, heavy rainfall, windstorm and high-altitude events.
2.3 Analysis
The goal of this study was to document HF preparedness for climate-related disaster events in Nepal and to explore whether past exposure to such events is associated with more emergency preparedness and service availability for CSDs. Three types of outcome variables were analyzed:
a. Emergency preparedness indicators.
b. Basic emergency service availability indicators.
c. CSD diagnosis and treatment service availability.
Additionally, we calculated the percentage of HFs that had all six emergency preparedness indicators and all six CSD services available, categorized by facility type, using a threshold of exposure to more than five disaster events.
Climate-related disaster event exposure was defined based on the number of events on local level where the HF was located. HFs were classified as high exposure if they experienced more than five events between 2018 and 2020; and as low exposure if they experienced up to five events. The exposure threshold of five or more events was determined based on the distribution of these disaster events at local level during that period. Approximately 48% of HFs reported experiencing up to five events, whereas only about 25% had experienced more than ten events. Nevertheless, we conducted an additional analysis for emergency preparedness indicators using a threshold of more than ten events to understand whether similar effect patterns occurred when looking at the higher cutoff.
Following descriptive analyses to document service availability by past disaster risk exposure, we performed mean comparisons to assess differences between HFs with lower and higher climate incident exposure in the years preceding the survey. Since the outcome variables were categorical, we employed the χ2-test to identify differences in mean values between groups. The significance level was set at p < 0.05. Stata 18 was used for all statistical analyses and QGIS for linking climate and health facility data (based on geocoded location information of the HFs).
2.4 Ethical considerations
This study was based on an analysis of existing public domain survey data that are freely available online. The original SPA survey was approved by the Nepal Health Research Council (NHRC) and the Institutional Review Board of ICF International in the USA (Ministry of Health and Population, Nepal; New ERA, Nepal; and ICF Nepal, 2022). Additionally, the authors obtained approval from the DHS program to use the secondary data from the survey.
3 Results
3.1 Disaster incidents and distribution of HFs
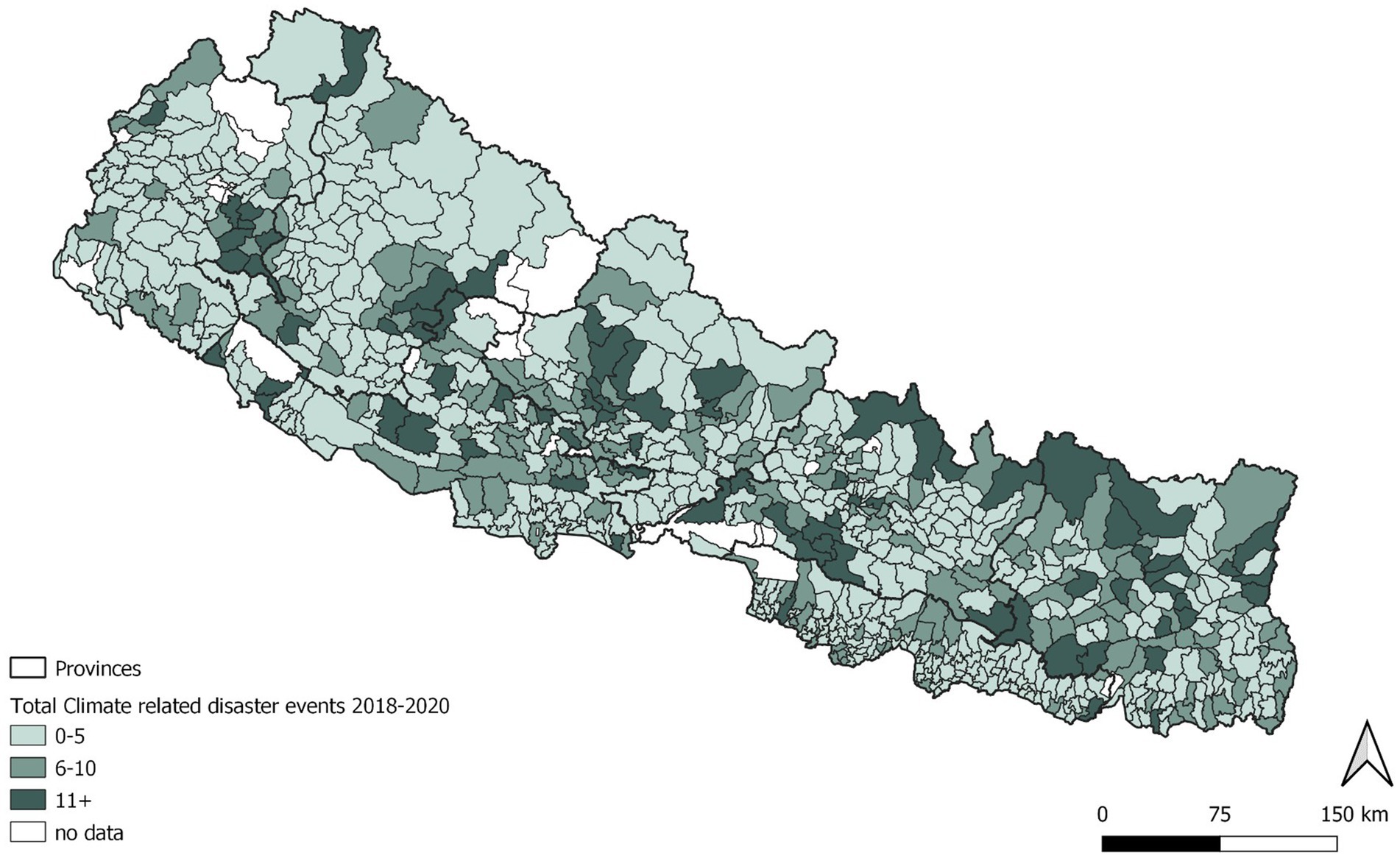
Between 2018 and 2020 a total of 12,226 disaster events were recorded on the portal. Only six of the climate-related disasters had complete data across all 3 years and were included in our analysis.
Overall, the data show a general upward trend in disaster occurrences, with some year-to-year variation. In total, 3,188 climate-related disasters from these six events were reported at the local levels where the HFs were located. The occurrence of these disaster events over time is illustrated in Figure 3.
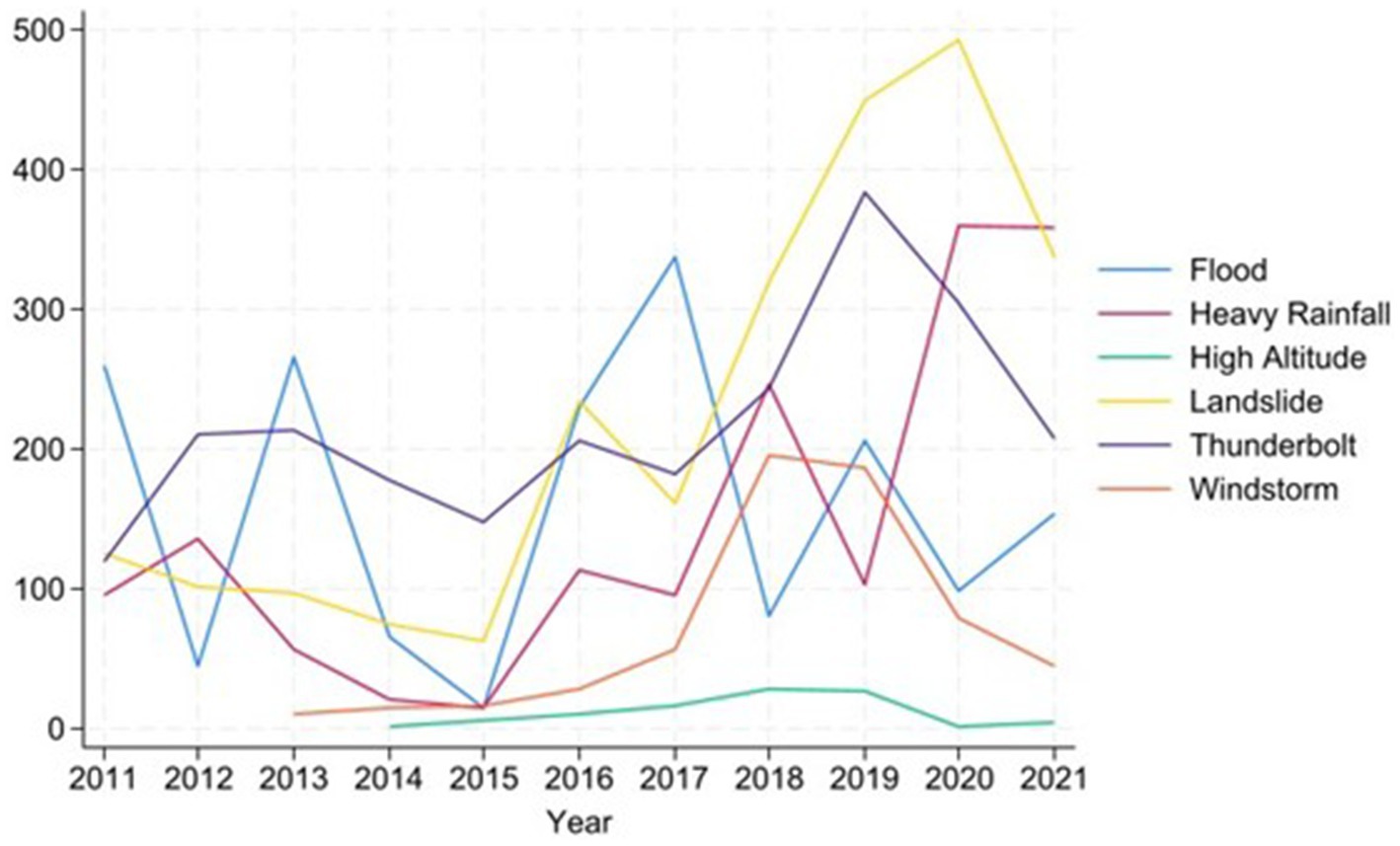
Figure 3. Occurrence of the six climate-related disaster events over time at local levels with health facilities (the number of disasters is displayed in absolute values).
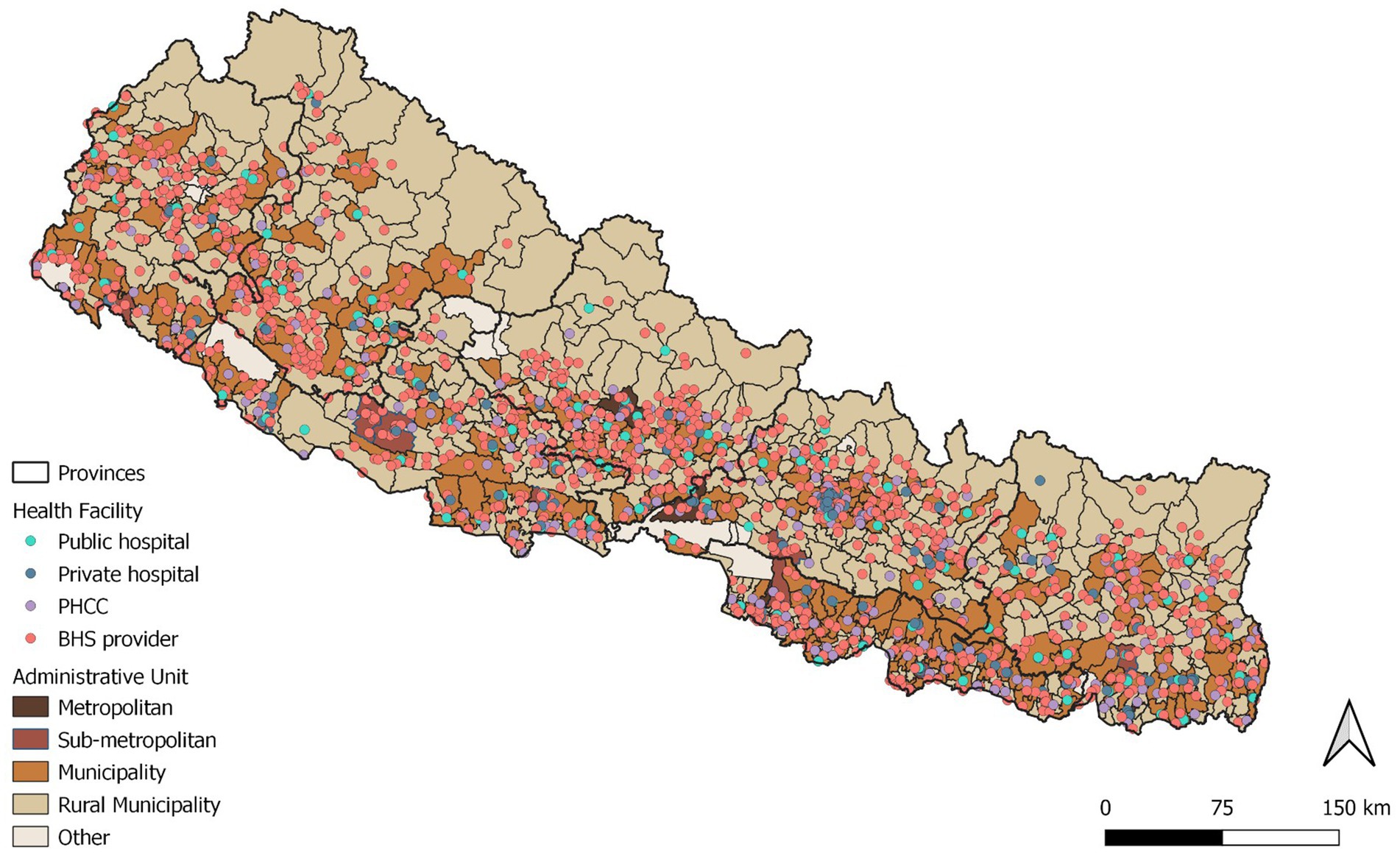
The 2021 SPA included HFs from 70 local levels in its sampling frame. After removing the HTCs from the sample, our analysis included a total of 1,535 HFs, 83% in the public sector. Of those, 6% were federal hospitals, 3% local hospitals, 12% Primary Health Care Centres (PHCCs) and 62% Basic Healthcare Service (BHS) providers (including HP, UHCC). 17% of the HFs were private. All private facilities included in the samples were hospitals. The geographic distribution of different types of HFs included in the SPA 2021 survey along with the frequency of disaster events are shown in Figures 4, 5 respectively.
Between 2018 and 2020, HFs experienced an average of eight climate-related disaster events, each with the number ranging from zero to as many as 51. During this period, 97.27% of facilities were affected by at least one of the six disaster types-landslides being the most frequently reported, with an average of three incidents per facility, followed by thunderbolts, floods, rainfall, windstorms, and high-altitude events (Annex 2). In terms of frequency of events experienced by the HFs, 25.3% of facilities reported more than 10 events, 24.45% experienced 6–10 events, 47.4% encountered 1–5 events, and only 2.7% reported none between 2018 and 2020. Data on at least one of our disaster events of interest were missing for 4% of HFs in 2020 (SD 0.21), 5% in 2019 (SD.22), and 7% in 2018 (SD.25), indicating a slight improvement in data reporting over the three-year period.
3.2 Health facilities preparedness
3.2.1 Key emergency preparedness indicators
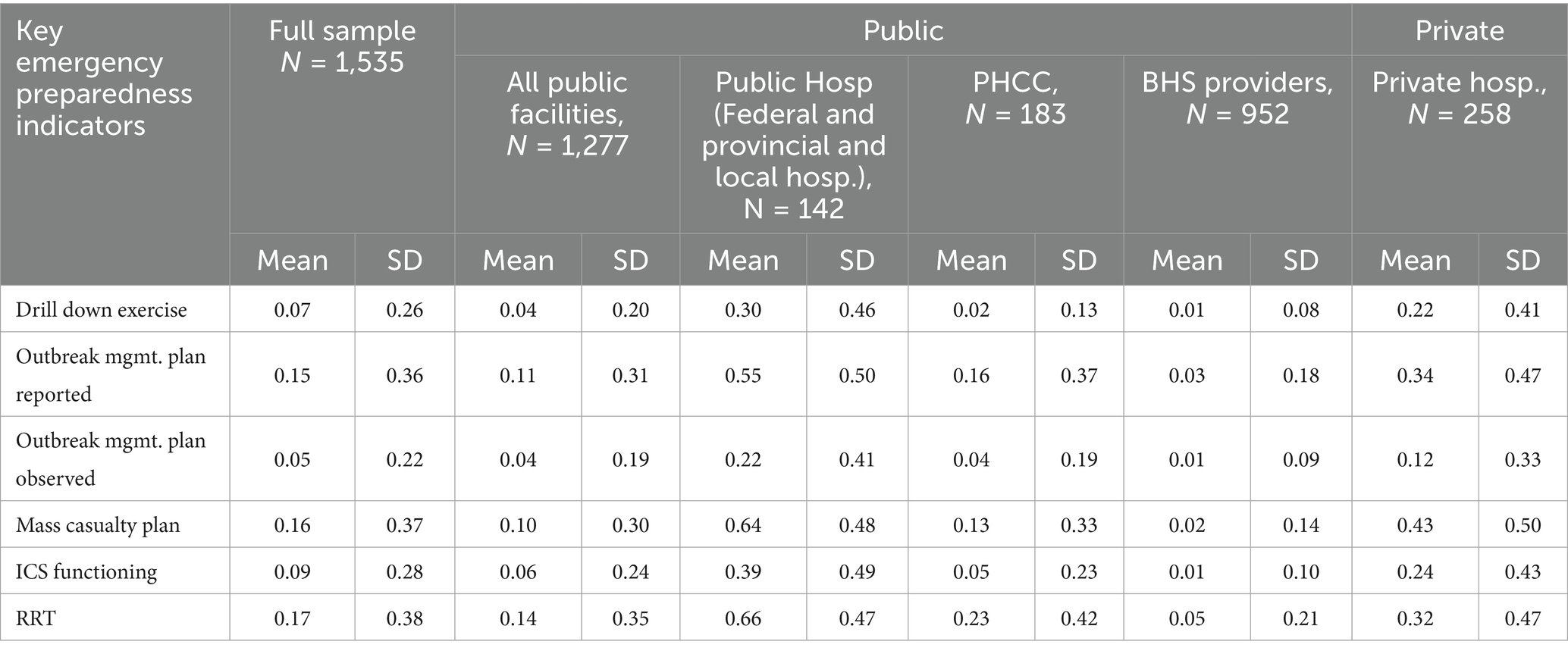
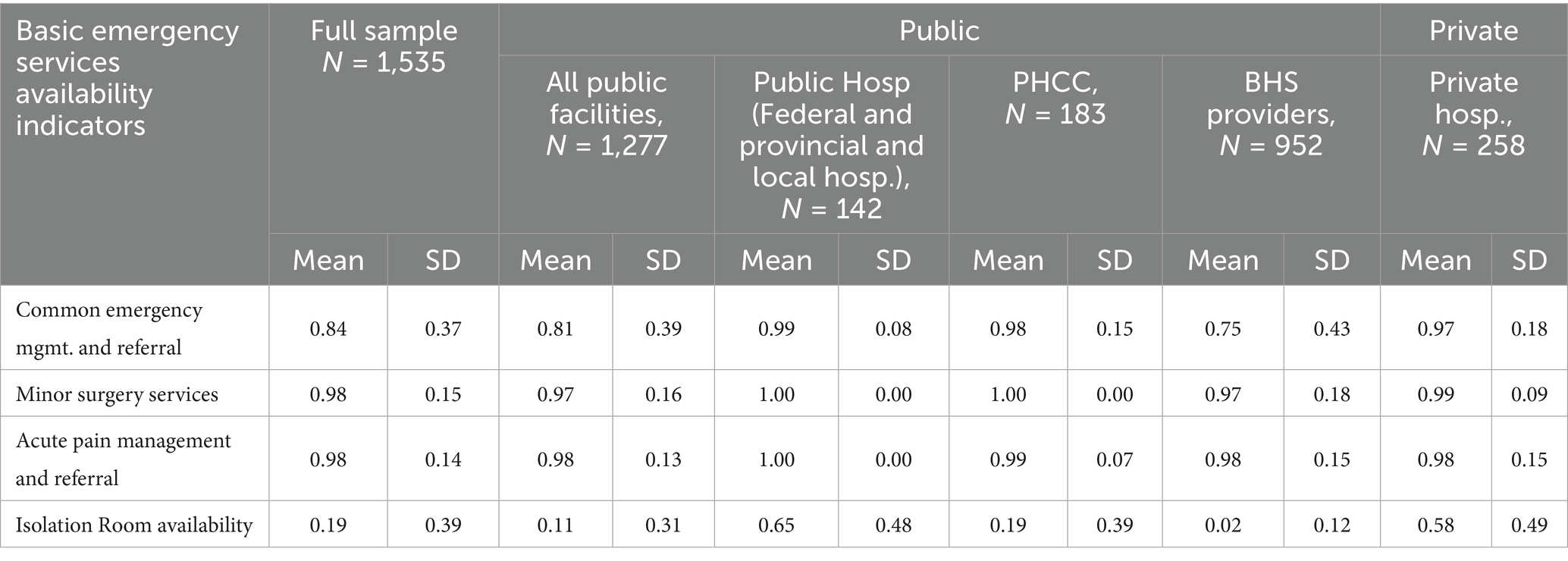
Table 2 presents the general status of six key emergency preparedness indicators across HFs.
Overall, disaster preparedness among HFs in Nepal remains limited. Only 7% of HFs reported conducting a drill-down exercise as part of disaster preparedness training. Among all public HFs, regardless of type, only 4% had conducted drill down exercise, while 22% of the private HFs reported doing so. However, when comparing all public hospitals to private ones, 30% of public hospitals had conducted drill-down exercise, surpassing the 22% reported by private hospitals. Federal and provincial hospitals had an even higher percentage at 38%, while local hospitals reported only 11%. Only 2% of PHCCs and 1% of BHS providers had conducted drill down exercises.
15% of all HFs reported having an outbreak management plan, but it was observed in only 5% of HFs. The public-private divide among hospitals showed 55% of all public hospitals reported having a plan, with 22% observed, while only 34% of private hospitals reported having a plan, with 12% observed. The percentage of outbreak management plans reported and observed was higher in federal and provincial hospitals (66 and 27%) compared to local hospitals (31 and 11%). Likewise, the percentage of the outbreak management plan observed in PHCCs, and BHS providers were 4 and 1%, respectively.
The mass casualty plan was reported in 16% of all HFs; present in 10% of all public and 43% of private facilities. Among public hospitals, 64% reported having the plan, including 66% of the federal and provincial hospitals and 31% of local level hospitals. Additionally, 13% of PHCCs and 2% of other BHS providers reported having the mass casualty plan in place.
Overall, only 9% of all HFs had a functioning Incident Command System (ICS) in place. This was reported in 6% of all public HFs and 24% of private facilities (hospitals). However, the percentage was higher in public hospitals (39%), with federal and provincial public hospitals reporting 49%, compared to 18% in local public hospitals. ICS functioning was relatively low in PHCCs at 5% and lowest among BHS providers at 1%.
Similarly, a Rapid Response Team (RRT) was available in 17% of all HFs, with 14% of public facilities and 32% of private facilities (hospitals) reporting their presence. Among public hospitals, 66% had RRT, with 75% in federal and provincial public hospitals and 47% in local public hospitals. Additionally, 23% of PHCCs and 5% of other BHS providers had it in place.
3.2.2 Basic emergency services availability indicators
Table 3 summarizes the selected basic emergency service availability across different types of HFs. Most selected emergency services were available in nearly all facilities; however, public hospitals generally demonstrated a higher availability across most indicators compared to private hospitals. The overall availability of isolation rooms was the lowest among the selected services (19%), with limited availability among the public hospitals (11%). Nevertheless, public hospitals still reported a comparatively higher proportion of isolation room availability than private hospitals.
3.2.3 Diagnosis and treatment service availability for the six CSDs
The availability of services for the selected CSDs varied across different facility types and diseases (Table 4). Service availability for CVD and child malnutrition were broadly available in both private and public facilities, as well as across different types of public facilities. While public hospitals showed better service availability for the CSDs, their availability in PHCCs was limited, especially in providing services for kala-azar and mental health. Public hospitals also consistently demonstrated a higher service availability than the private ones for all six CSDs.
3.3 Key emergency preparedness and services availability by exposure to disaster events in the preceding years
Comparing key disaster preparedness indicators between HFs that experienced more than five disaster events and those experiencing up to five events from 2018 to 2020 revealed no significant differences for most indicators. However, notable differences were observed in two indicators. The outbreak management plan (reported) was present in 18.09% of facilities with exposure to more than five events, compared to 13.88% in those up to five events. Similarly, the availability of a mass casualty plan was higher in the more exposed group (20.52%) than in the less exposed group (14.63%).
Likewise, mean comparisons for two key basic emergency services-minor surgical services and the availability of isolation rooms for infectious diseases, revealed significantly higher availability in HFs exposed to more than five disaster events, compared to those exposed to up to five events. Mean comparisons of CSD service availability between the two categories also yielded similar results, with no statistically significant differences observed as shown in Table 5.
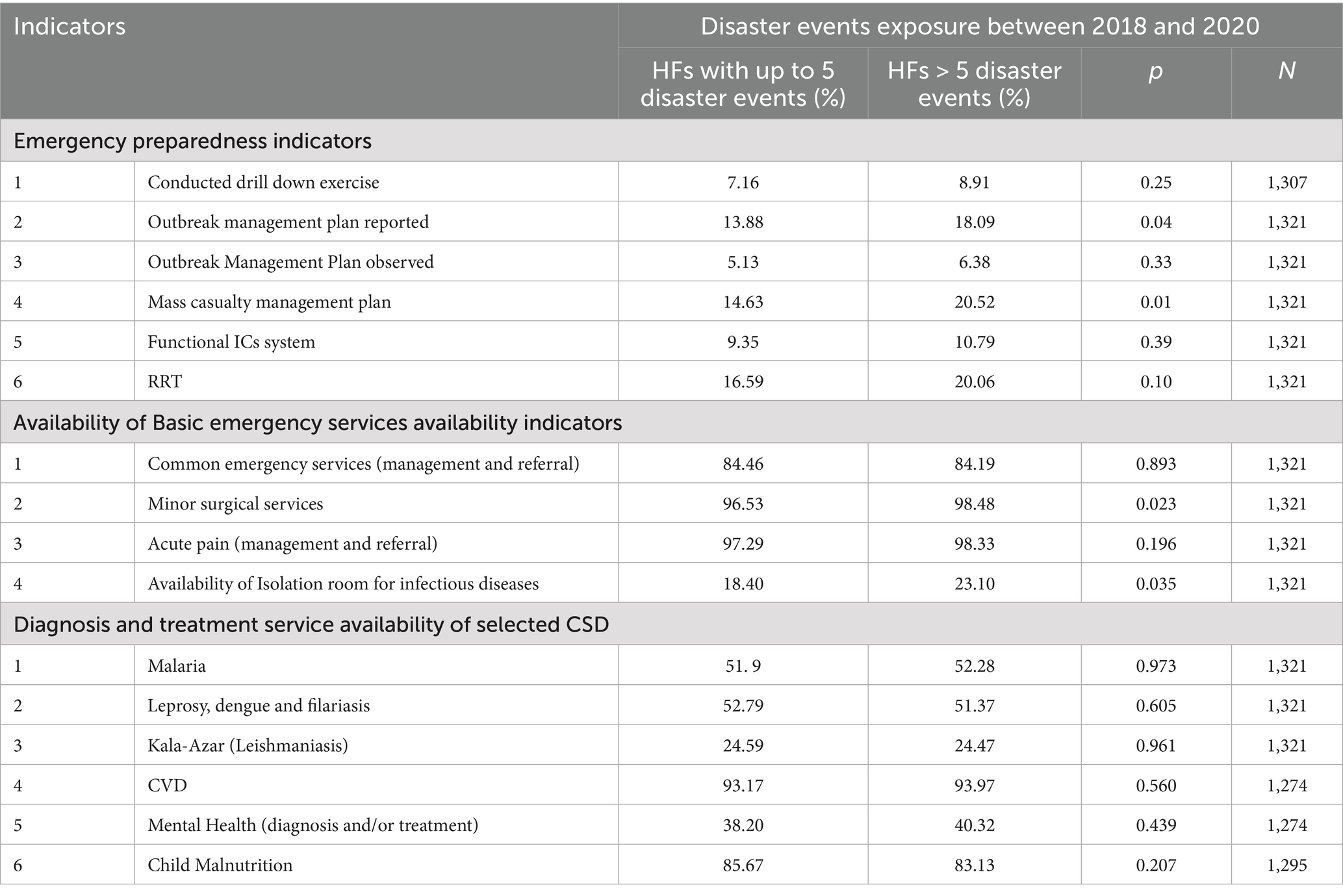
Table 5. Key emergency preparedness and services availability by exposure to disaster events in the preceding years.
When comparing the average preparedness of HFs based on their exposure to more than ten vs. a maximum of 10 disaster events, HFs that experienced more than ten disaster events showed significantly stronger emergency and preparedness indicators compared to those with 10 or fewer events. Notable differences included a 5.02% higher rate of conducting drill-down exercises, a 10.19% greater availability of outbreak management plan reported, a 3.89% increase in outbreak management plan observed, a 11.26% higher availability of mass casualty plans, a 4.91% greater presence of functional Incident Command System (ICS), and an 8.65% higher availability of Rapid Response Team (RRT) (Table 6). These results were robust to excluding local levels with over 50 disaster event exposures as outliers (Annex 3).
Table 6. Mean Comparisons of emergency preparedness indicators with exposure to more than 10 vs. less than 10 disaster events at the local level.
3.4 Comparative summary of key emergency preparedness and services availability by exposure, disaggregated by facility types
The overall preparedness levels seemed to align with the tier of the HFs, with higher-tier facilities exhibiting better preparedness indicators than lower-tier ones in both groups. The public-private comparison showed that public hospitals consistently demonstrated greater preparedness than private hospitals, outperforming them on emergency preparedness indicators across both high and low-exposure cases. In contrast, the availability of CSD services showed little variation between the two groups, regardless of disaster events exposure. However, public hospitals reported higher availability for all CSD services, except for malaria, which was slightly more available in private hospitals (Table 7).
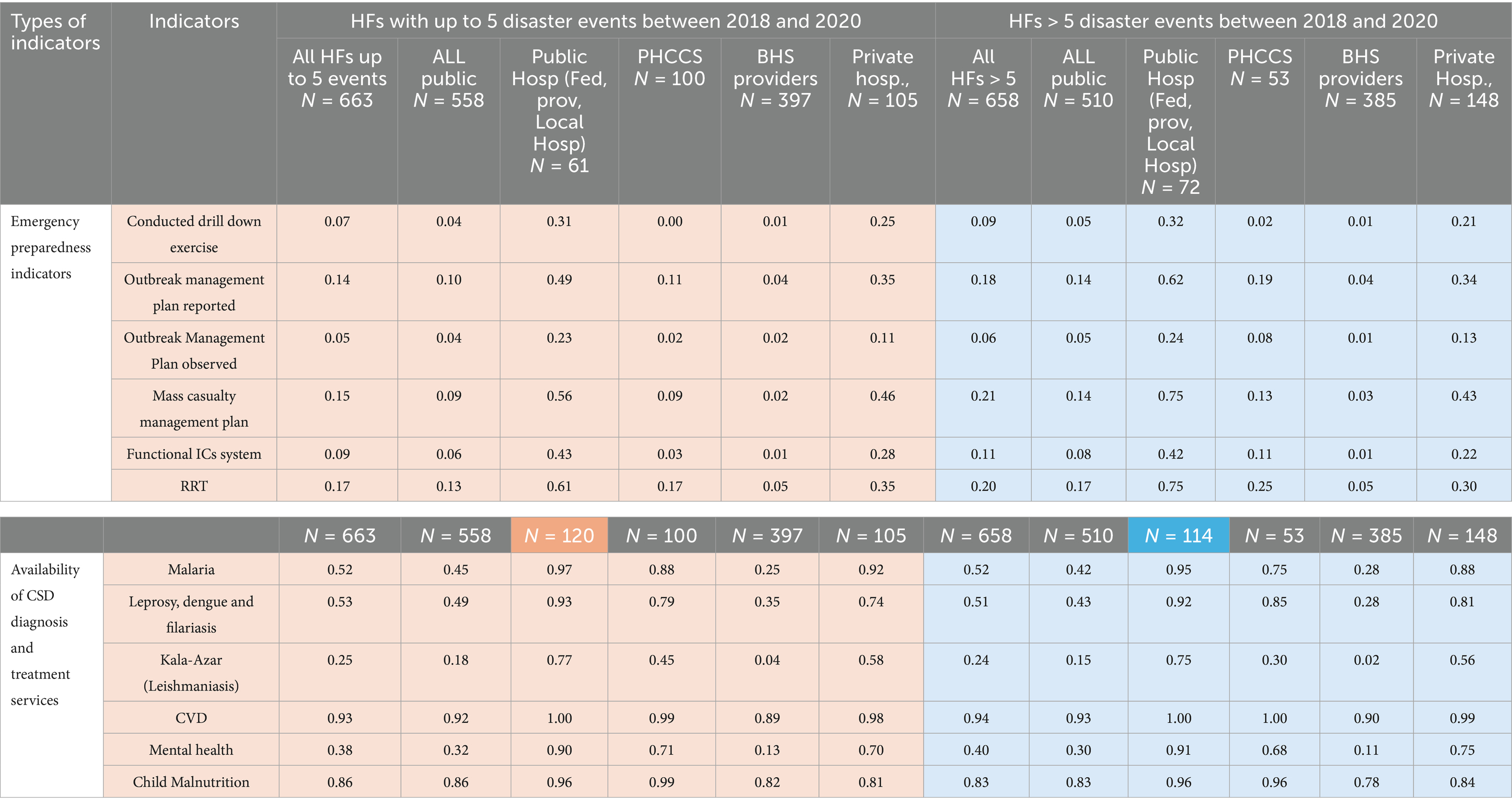
Table 7. Comparative summary of the emergency readiness indicators for HFs exposed to more than 5 disaster events versus those exposed to fewer than 5 events, broken down by facility types.
3.5 Availability of all six-emergency preparedness and CSD services indicators by disaster exposure
Overall, the presence of all six emergency preparedness measures was generally low across all HFs. As shown in Table 7 below, when comparing the aggregate availability of all six disaster preparedness indicators, HFs with low exposure (≤5 events) tended to demonstrate stronger emergency preparedness than those with high exposure (>5 events). Specifically, only 1.69% of HFs with high-exposure reported having all six emergency preparedness indicators, whereas 2.26% of HFs with low-exposure areas met this criterion.
When examining a core set of three key indicators, namely drill-down exercises, Incident Command System (ICS) and Rapid Response Team (RRT), facilities with low exposure appeared to perform slightly better overall (4.83%), reporting the presence of all three indicators.
Regarding the diagnosis and treatment services for CSDs, almost a similar percentage of all HFs with high exposure (15.84%) and low exposure (14.79%) reported offering services for all the six CSDs.
A comparison of private hospitals across low and high exposures also revealed a stronger preparedness in low-exposure areas for both the full set of six emergency preparedness and the core set of three. However, the availability of CSD services was nearly identical between the two exposure groups. These findings suggest that only a small proportion of private HFs in high-disaster areas are adequately equipped to respond comprehensively to future climate-related disaster events (Table 8).
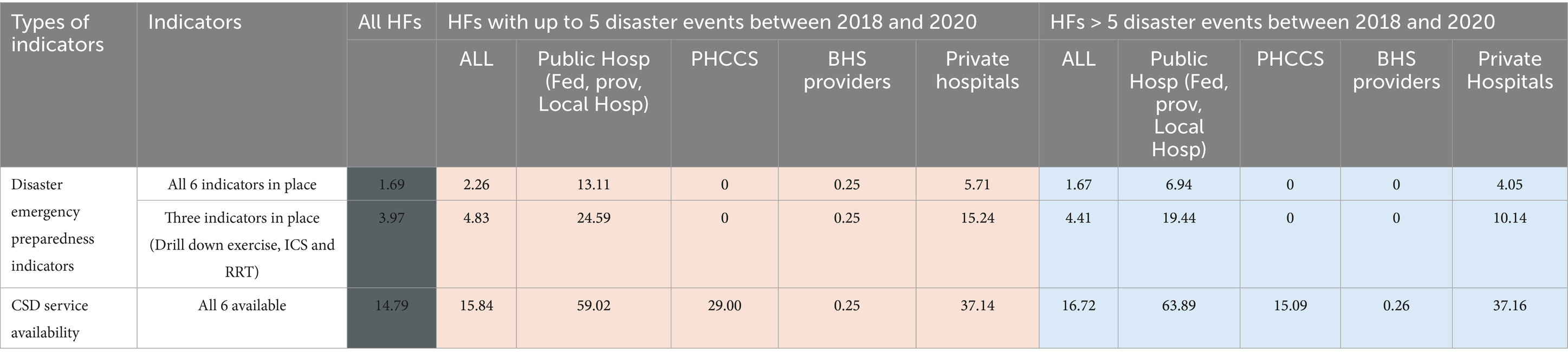
Table 8. Overall emergency preparedness and service availability of CSD across different types of HFs.
4 Discussion
4.1 Evidence gaps in HF preparedness for climate-related disasters in Nepal
Focused studies specifically assessing the preparedness of HFs for climate-related disaster events remain scarce. To address this critical gap, the present study leveraged existing data to explore HF preparedness. Although research on climate change-related disasters, and disasters in general, has increased over time in Nepal (Tome et al., 2022), relatively few studies have explored the preparedness of the health system to such climate related disaster events.
Our study offers valuable insights into some of the existing strengths and weaknesses within Nepal’s health system and highlights key areas requiring urgent attention to enhance resilience against future climate-related disasters. However, it is by no means a comprehensive assessment. Building climate resilient HFs and systems require addressing both the immediate and long-term effects of disasters, strengthening preparedness for future events, and incorporating all components outlined in health system resilience frameworks (WHO, 2015) alongside the domains of established disaster preparedness frameworks (WHO, 2015; WHO, 2019).
Although this study relied on limited number of indicators for understanding disaster preparedness and managing the demand for increased CSD services during disasters, it is the first to systematically analyze existing data on the occurrence of various climate-related disasters and assess the HF’s preparedness to manage such events and provide services for CSDs. Importantly, it also represents the first instance in which publicly available datasets from two different government entities have been combined to understand both disaster frequency and health facility preparedness, highlighting a significant gap in research at this intersection in Nepal.
Our analysis of data from the NDRR portal found consistent reporting for only six types of climate-related disasters: floods, landslides, thunderbolts, rainfall, windstorms, and high-altitude events. Among these, landslides were the most frequently reported, followed by thunderbolts and floods. These findings align with earlier national studies that identify landslides and floods as among the deadliest disasters in Nepal (Chapagain et al., 2022). Other notable but less systematically reported climate-related disaster types such as thunderstorms, cold waves, heatwaves, hailstorms, frost, snowstorms, and avalanches, could not be examined due to data limitations, highlighting significant gaps and weaknesses in disaster reporting systems in Nepal and other LMICs (Osuteye et al., 2017).
A systematic review of post 2020 literature on climate change and vulnerability in Nepal identified 37 studies that assessed vulnerability of health systems to disaster events. This study found that while emergency preparedness and early warning systems for disease and vector surveillance exist, climate change has not been sufficiently integrated into long term disaster planning efforts. Moreover, none of the reviewed studies assessed the preparedness of HFs, either in general or specifically for climate related disasters (Tome et al., 2022). Other studies that have been conducted in this area are also mostly a response to the 2015 earthquake and have largely focused on hospitals and infrastructure-related aspects with respect to disaster preparedness (Adhikari et al., 2024; Watts et al., 2021). While these findings highlight important progress, they also point to a key area for future research, particularly in strengthening climate-resilient health systems.
Globally, EM-DAT records disaster events at the country level based on human and economic losses meeting at least one of the following criteria: (i) 10 or more fatalities; (ii) 100 or more people affected; (iii) declaration of a state of emergency; or (iv) a call for international assistance (EM-DAT CU, 2025). In Nepal, the NDRR portal captures some of this information, such as the number of fatalities and affected individuals. However, persistent challenges in data quality and availability limit the ability to fully assess the severity of events, pointing to an important gap in both disaster data and research (Nepal Disaster Risk Reduction Portal [Internet], n.d.). This data limitation is documented in Annex 4.
4.2 Uneven disaster preparedness across HF levels and exposures
Regardless of exposure levels, both disaster preparedness and the availability of services for CSDs remain uneven across HFs, with PHCCs and BHS providers particularly lacking in critical preparedness and service availability. This observation is consistent with both global and national literature, pointing to a concentration of strategic planning and resources at higher levels of the healthcare system, leaving lower-level facilities, often serving the most vulnerable populations, significantly underprepared (Sharma, 2015; Lamberti-Castronuovo et al., 2022; Gao et al., 2018; Hashikawa and Gold, 2018). Since climate-related disasters are often localized and their impacts and vulnerabilities are highly context-specific requiring tailored local solutions, additional initiatives at the local level are necessary to drive the progress further.
In this context, an evaluation of disaster preparedness in climate-vulnerable regions of Bangladesh highlights the urgent need for systematic improvements in both emergency preparedness and healthcare service delivery to address the impacts of climate change (Bangladesh PI, 2024). Several other studies have also underscored the importance of assessing vulnerabilities and strengthening the preparedness for disasters as well as service delivery for CSD at primary-level HFs to enhance post-disaster response efforts (Walsh et al., 2015; Lestari et al., 2022; Masbi et al., 2024). However, such an approach seems to be underutilized in Nepal. In a resource-limited setting like Nepal, implementing a universal preparedness program is not feasible, making targeted and specific interventions the most practical solution (Robinson, 2009; Gaire et al., 2015). Therefore, strengthening the link between disaster preparedness, climate change, and health is key to building resilience and reducing disaster risks. This involves using existing policies, systems, and expertise across sectors, and leveraging data tools and information networks to improve preparedness, efficiency, and coordination to promote joint action (Banwell et al., 2018; Moulton et al., 2017).
Comparing HFs with low exposure to those with high exposure did not consistently reveal a clear pattern of increased preparedness among those with higher exposure levels. Notably, HFs demonstrated significant improvements in disaster preparedness indicators only when the exposure was more than ten events. This suggests that preparedness efforts in the country are often influenced by past disaster experiences, indicating a tendency for a more reactive approach. Although some studies suggest that HFs naturally improve their preparedness with repeated exposure to disasters, other research shows that this is not always the case (Bian et al., 2022). To ensure effective and sustainable disaster risk management from a systems perspective, HFs must adopt proactive measures to be better equipped to handle both anticipated and unforeseen disasters (Tabish and Syed, 2015). This concern has also been highlighted in a review of Nepal’s DRR policies and institutional frameworks, which reveals that the country remains more focused on response and relief, with relatively less emphasis on long-term preparedness (Nepal, Pashupati NRK, Sharma, Bishnu Prasad Pangali, 2018).
Due to the lack of established core indicators specifically tailored to assess preparedness for climate-related disaster events, this study evaluated the presence of key preparedness measures identified in the SPA survey as essential for effective disaster response. Several guidelines and studies have independently emphasized the importance of having drill-down exercises, ICS and RRT in place to effectively respond to emergencies (WHO, 2019; Gebbie et al., 2006; WHO, 2011). These three components were considered as core set of disaster preparedness indicators in our analysis, and we also assessed their presence collectively. However, the availability of this core set was generally low across most HFs, with no significant difference observed between those with lower or higher exposure levels. These inconsistencies where some facilities are relatively well-prepared while others remain critically underprepared despite higher climate related disaster exposure highlights the need for a more systematic, needs-based approach to take the disaster efforts forward within Nepal’s health system. Similar findings were observed in Nepal following the 2015 earthquake, where studies revealed substantial gaps in the health system’s capacity to respond to disasters (Sharma, 2015).
4.3 Federalism and disaster resilience: strengthening local capacities
Federalism presents a unique opportunity to adopt a more needs-based approach to disaster preparedness. Research from both the health sector and beyond suggests that decentralization and federalism promotes more needs-based and context-specific planning by enabling strategies tailored to the unique vulnerabilities of communities and local levels (Shair-Rosenfield, 2024; Devkar et al., 2019). With political, financial, and administrative autonomy, local governments are often well-positioned to advance disaster resilience (Manyena Bernard, 2006). However, for local governments to fully leverage this potential, more efforts are needed to raise awareness about the importance of climate related disaster preparedness and to build capacity in this area at the local level (Khanal and Boeckmann, 2025).
While prioritizing the readiness of tertiary and secondary HFs is understandable due to their relatively stronger capacities, it is equally vital to focus on strengthening preparedness at local level. When only higher-level HFs are prepared with weak lower-level HFs, it places excessive pressure on tertiary hospitals, often exceeding their capacity to manage increased demand during disaster events (Masbi et al., 2024). Therefore, a balanced and integrated approach, combining both top-down and bottom-up strategies, is crucial. Evidence shows that successful decentralization depends on effective coordination across all levels of government, enhanced local financial capacity, institutional strengthening, and a more prominent role for private providers (Manyena Bernard, 2006; Robinson, 2009).
4.4 Private sector engagement: a critical component of disaster preparedness
Our study also indicates the need to strengthen disaster preparedness and CSD service delivery across all HFs, both public and private alike. The particularly poor disaster preparedness indicators observed in private hospitals are concerning, especially given the increasing reliance on the private sector over time, its varying role across countries and services, and its crucial contribution to healthcare delivery in Nepal (Karkee and Kadariya, 2013). Although we found no prior study specifically comparing disaster preparedness and CSD service availability between public and private facilities in Nepal, existing evidence from other health programs in the country suggests that the private sector generally demonstrates better overall service preparedness (Thapa et al., 2024; Farah et al., 2023). Therefore, our finding that private hospitals were less prepared for climate related disasters or had low CSD services was contrary to our expectations.
Despite longstanding challenges with private sector regulation and partnership within the MoHP across all the health programs, their contribution in health service delivery has been recognized to add value and alleviate some of the financial and health systems constraints faced by the government in delivering quality services (Auzzir et al., 2014). Wallace et al., in their review of the private sector’s role across four countries, including Nepal, emphasize how private sector participation during emergencies can relieve some of the pressure on public HFs and support government efforts (Wallace et al., 2022). In line with international evidence, our study further reinforces the need to encourage private sector involvement in disaster preparedness (Mashari, 2022).
4.5 Data gaps and challenges in disaster preparedness planning
Our study showed significant gaps related to data, both in terms of availability as well as utilization of existing information for disaster preparedness and planning. Various sectors, including the MoHP, have conducted vulnerability risk assessments (VRAs) to better understand the impacts of climate change, and to identify areas and populations most at risk, particularly concerning CSDs (MoHP G, 2022). Although our study did not assess the availability of CSD services based on reported and treated cases from MoHP’s EWARS and HMIS data, the generally low availability of these services raises concern about whether the findings from VRA assessments are effectively utilized for service strengthening.
Furthermore, our analysis, which considers the frequency of climate-related disaster events, points that HFs in areas with more frequent events continue to be inadequately prepared and vulnerable to future disasters and CSD outbreaks. This highlights a critical gap. Despite several initiatives by the MoHP and other ministries, current disaster preparedness efforts in healthcare facilities lack a data-driven and need-based approach.
Addressing this gap requires not only better utilization of available data but also stronger underlying data systems (Aung and Whittaker, 2013). In Nepal, the absence of well-functioning disaster data systems remains a significant barrier, particularly when attempting to integrate disaster and health facility data. Our own challenges in accessing and analyzing disaster data illustrate these difficulties. However, these challenges are not unique to our study. A comprehensive assessment of Nepal’s disaster and risk information systems similarly identified the lack of clear and standardized guidelines for recording disaster data, including the documentation of human impacts such as fatalities, injuries, and displacement. Such information is essential for assessing the severity of disaster events and aligning with global benchmarks like EM-DAT (Oxford Policy Management, and Policy and Institutions Facility, 2020; Development WCfH, n.d.).
Given the persistent data gaps in Nepal’s disaster preparedness evaluations, there is a need to integrate more disaster-specific indicators into existing national surveys. This need is particularly pressing as no further rounds of DHS/SPA surveys are currently planned. In Nepal’s new federal governance structure, leveraging disaster-related data at the local level could facilitate the application of EM-DAT classification criteria in future research, thereby promoting better alignment with global standards and enabling more meaningful comparisons. This represents a critical area for further studies.
Poor data availability however is just one of several barriers. Gaps in implementing existing policies and plans also pose major challenges. Although Nepal has formulated climate-resilience plans across government levels, their execution remains limited (Dhimal et al., 2017; Rijal et al., 2020). Similar to other LMICs, Nepal faces challenges such as resource constraints and weak integration of climate and health policies (Khanal and Boeckmann, 2025; Ansah et al., 2024). Few studies including ours (Khanal and Boeckmann, 2025) and Landry et al. (2016), point to poor coordination and unclear institutional roles as key obstacles. Addressing these governance issues requires stronger intersectoral collaboration and clearer responsibilities to effectively integrate climate resilience into health and disaster planning.
4.6 Study limitations
The study has several limitations. Overall, the findings of this study should not be interpreted as causal; rather, we document patterns of associations intended to inform and inspire future research. However, data availability constrained us to work with the number of disasters as exposure, and therefore the findings cannot be directly discussed against the framework such as those established by EM-DAT benchmarks. Nevertheless, as this is the first study to link climate-related disasters to HF preparedness in Nepal, we believe that this descriptive work is an important step toward further research in this area.
Regarding available data, one key limitation is the lack of robust historical data on disasters, climate-related disasters and emergency preparedness. As aforementioned, following Nepal’s transition to a federal system in 2015, complete local-level data from earlier years were not available. Consequently, we included data from 2018 onward to ensure a more accurate reflection of the federal structure, as provincial and local governments had by then, assumed more clearly defined roles within the new governance framework. A detailed development of disaster events over the years, as reported in the NDRR portal is shown in Annex 4. Additionally, the scope of the analysis was constrained by the quality of data on disaster events and the availability of CSD services. Since the disaster events included in the study were based on the data available in the NDRR portal, several frequently occurring climate-related disaster events (identified in other studies), were excluded due to inadequate or incomplete reporting. For many events, data was missing for certain years due to reporting gaps. We assume that the restructuring of physical infrastructure and reporting mechanisms under the new federal system may also have further contributed to these data gaps and underreporting.
Secondly, in the absence of focused study on HFs preparedness for disaster events, we used secondary data drawn from the only available national survey assessing health facility readiness (SPA survey). The SPA survey was primarily designed to evaluate service readiness for key health areas, particularly maternal and child health and infectious diseases. However, it includes only a small set of indicators related to disaster preparedness, emergency response, and CSDs. While data from a comprehensive, nationwide HF assessment of overall disaster preparedness would have provided a deeper understanding, the analysis was constrained by the scope of available data in the survey. Furthermore, only two rounds of the SPA survey have been conducted to date, and in both instances, the CSD and emergency preparedness indicators show inconsistencies between the two surveys, highlighting the need for more research in this area.
Thirdly, we recognize that preparedness and response to climate-related disasters depend on several broader factors, including the overall readiness of HFs, which were not covered in this study. While an analysis of geographic variation in preparedness and CSD service availability could have yielded valuable insights, we deliberately chose to limit the study’s scope to ensure a more focused and manageable analysis.
Fourthly, it is important to note that all private HFs included in the SPA survey were hospitals. While private clinics and other types of private facilities also play a significant role in health service delivery in Nepal, their exclusion from the sample limits the overall comprehensiveness and representativeness of the findings. Nonetheless, in addition to offering a comparative analysis on overall public and private HFs, our study specifically examines differences between public and private hospitals.
Finally, we acknowledge that the vulnerability of health facilities to climate-related disasters is shaped not only by their exposure to such climate hazards but also by other critical factors, including the sensitivity and vulnerability of the populations they serve, the condition of surrounding natural systems, and the adaptive capacity of the health system to manage associated risks (Table 1). Our study did not delve into these broader dimensions of vulnerability, nor did it quantify the severity of climate-related events in terms of damage or loss of life. Instead, the analysis focused solely on the frequency of reported climate-related disaster events experienced by the HFs.
5 Conclusion
HFs serve on the frontlines of response efforts during climate-related disasters, making their preparedness essential. Despite the increasing frequency of climate related disasters in recent years, limited research has explored the preparedness of HFs in LMICs. This study assessed the disaster preparedness of HFs in Nepal, specifically in relation to climate-related disaster events that occurred between 2018 and 2020. It provides insights into the levels of preparedness and the availability of CSDs services across different facility types.
The findings reveal substantial inconsistencies in both disaster preparedness and the provision of CSD related services across HFs in Nepal. While some patterns indicated a degree of adaptation to climate-related disaster exposure, overall preparedness was found to be inadequate across all facility types. The study underscores the need to better align climate related disaster preparedness and availability of CSD services, particularly by focusing efforts at the local level and fostering greater engagement from the private sector.
Additionally, the study also emphasizes the importance of improving documentation and systematic reporting of climate-related disasters to enable more detailed analyses and support evidence-based planning. Although not exhaustive, the study lays the groundwork for raising awareness among policymakers about the need to enhance HF preparedness as part of efforts to build a climate-resilient health system. In light of these findings and the complexity of disaster risk preparedness and response, a more comprehensive assessment of overall health system preparedness is recommended, incorporating all components of a climate-resilient health system as outlined by the WHO.
Data availability statement
The data analyzed in this study is subject to the following licenses/restrictions: Disaster data is publicly available through the government website (http://drrportal.gov.np/). Formal authorization was obtained from the DHS Program for the use of the SPA 2021 datasets. Requests to access these datasets should be directed to https://www.dhsprogram.com/data/dataset_admin/login_main.cfm.
Ethics statement
This study used secondary data from the 2021 SPA Survey and the Nepal Disaster Risk Reduction (NDRR) Portal. The NDRR data are publicly available, and permission to use the SPA dataset was obtained from the DHS Program. As no primary data were collected, no interactions with participants occurred, and the data contained no identifiable information, ethical approval was not required. The study was conducted in accordance with Frontiers ethical guidelines.
Author contributions
SK: Writing – original draft, Methodology, Conceptualization, Data curation, Writing – review & editing, Project administration. TS: Visualization, Data curation, Validation, Writing – review & editing. MB: Supervision, Writing – review & editing. FP: Formal analysis, Data curation, Methodology, Validation, Writing – review & editing, Conceptualization.
Funding
The author(s) declare that no financial support was received for the research and/or publication of this article.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Generative AI statement
The authors declare that no Gen AI was used in the creation of this manuscript.
Any alternative text (alt text) provided alongside figures in this article has been generated by Frontiers with the support of artificial intelligence and reasonable efforts have been made to ensure accuracy, including review by the authors wherever possible. If you identify any issues, please contact us.
Publisher’s note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fclim.2025.1625829/full#supplementary-material
References
Adhikari, H. P., Singh, K., Devkota, N., and Bartaula, M. (2024). Hospital’s disaster preparedness and management in tertiary level hospitals of Kathmandu Valley. Afr J Biomed 27, 570–575. doi: 10.53555/AJBR.v27i1S.1526
Ansah, E. W., Amoadu, M., Obeng, P., and Sarfo, J. O. (2024). Health systems response to climate change adaptation: a scoping review of global evidence. BMC Public Health 24:2015. doi: 10.1186/s12889-024-19459-w
Arboleda, C. A. A., Dulcy, M., Richard, J.-P. P., and Lubitz, R. (2009). Vulnerability assessment of health care facilities during disaster events. J. Infrastruct. Syst. 15, 149–161. doi: 10.1061/(ASCE)1076-0342(2009)15:3(149)
Aung, E., and Whittaker, M. (2013). Preparing routine health information systems for immediate health responses to disasters. Health Policy Plan. 28, 495–507. doi: 10.1093/heapol/czs081
Auzzir, Z. A., Haigh, R. P., and Amaratunga, D. (2014). Public-private partnerships (PPP) in disaster management in developing countries: a conceptual framework. Procedia Econ. Finance 18, 807–814. doi: 10.1016/S2212-5671(14)01006-5
Bangladesh PI. Health Facility Assessment Disaster Preparedness and Service Readiness Assessment of the Health Facilities in the Climate Vulnerable North-Eastern Areas in Bangladesh Dhaka, Bangladesh. Dhaka, Bangladesh: Pathfinder International and Publisher (2024)
Bank WBGaAD. Climate Risk Country Profile Nepal. Washington, DC: World Bank Group and publication. (2021).
Banwell, N., Rutherford, S., Mackey, B., and Chu, C. (2018). Towards improved linkage of disaster risk reduction and climate change adaptation in health: a review. Int. J. Environ Res. Public Health. 15.
Bian, Q., Liang, Y., and Ma, B. (2022). Once bitten, twice shy? Does the public adopt more disaster preparedness practices after experiencing more disasters? Int J Disaster Risk Reduct 77:3057. doi: 10.1016/j.ijdrr.2022.103057
Birkmann, J., and von Teichman, K. (2010). Integrating disaster risk reduction and climate change adaptation: key challenges—scales, knowledge, and norms. Sustain. Sci. 5, 171–184. doi: 10.1007/s11625-010-0108-y
Chapagain, D., Bharati, L., and Borgemeister, C. (2022). Declining vulnerability but rising impacts: the trends of climatic disasters in Nepal. Regional Environmental Change. 22.
Development WCfH. (n.d.). Scoping Review and Case Studies of Health Data Management Before, During and After Emergencies and Disasters. Available online at: https://wkc.who.int/resources/projects/item/scoping-review-and-case-studies-of-health-data-management-before-during-and-after-emergencies-and-disasters?utm (Accessed January 25, 2025).
Devkar, G., Thillai Rajan, A., Narayanan, S., and Elayaraja, M. S. (2019). Provision of basic services in slums: a review of the evidence on top-down and bottom-up approaches. Dev. Policy Rev. 37, 331–347. doi: 10.1111/dpr.12355
Dhimal, M., Dhimal, M. L., Pote-Shrestha, R. R., Groneberg, D. A., and Kuch, U. (2017). Health-sector responses to address the impacts of climate change in Nepal. WHO South-East Asia Journal of Public Health. 6, 9–14. doi: 10.4103/2224-3151.213795
EM-DAT CU. (2025). Brussels, Belgium. Disaster Classification System, Historical and Current Classification System of Disasters. Available online at: https://doc.emdat.be/docs/data-structure-and-content/disaster-classification-system/#fnref:5 (Accessed November 10, 2024).
Farah, B., Pavlova, M., and Groot, W. (2023). Hospital disaster preparedness in sub-Saharan Africa: a systematic review of English literature. BMC Emerg. Med. 23:71. doi: 10.1186/s12873-023-00843-5
Gaire, S., Castro Delgado, R., and Arcos Gonzalez, P. (2015). Disaster risk profile and existing legal framework of Nepal: floods and landslides. Risk Manag Healthc Policy. 8, 139–49.
Gao, L., Wu, Q., Li, Y., Ding, D., Hao, Y., Cui, Y., et al. (2018). How prepared are hospitals’ emergency management capacity? factors influencing efficiency of disaster rescue. Disaster Med. Public Health Prep. 12, 176–83.
Gebbie, K. M., Valas, J., Merrill, J., and Morse, S. (2006). Role of exercises and drills in the evaluation of public health in emergency response. Prehosp. Disaster Med. 21, 173–182. doi: 10.1017/S1049023X00003642
GoN. (2017). “Disaster risk reduction and management act,” in Nepal Law Commission GoN, editor. Kathmandu, Nepal.
Guihenneuc, J., Ayraud-Thevenot, S., Roschnik, S., Dupuis, A., and Migeot, V. (2023). Climate change and health care facilities: a risk analysis framework through a mapping review. Environ. Res. 216:114709. doi: 10.1016/j.envres.2022.114709
Hashikawa, M., and Gold, K. J. (2018). Disaster preparedness in primary care: ready or not? Disaster Med Public Health Prep. 12, 644–8.
Heidaranlu, E., Ebadi, A., Khankeh, H. R., and Ardalan, A. (2015). Hospital disaster preparedness tools: a systematic review. PLoS Curr. :7. doi: 10.1371/currents.dis.7a1ab3c89e4b433292851e349533fd77
International O. 5 natural disasters that beg for climate action. (2025). Available online at: https://www.oxfam.org/en/5-natural-disasters-beg-climate-action. (Accessed January 25, 2025).
IPCC (2007). Climate Change 2007: Synthesis Report. Contribution of Working Groups I, II and III to the Fourth Assessment Report of the Intergovernmental Panel on Climate Change. Geneva: IPCC. Available online at: https://www.ipcc.ch/report/ar4/syr/
IPCC (2014). Climate Change 2014: Synthesis Report. Contribution of Working Groups I, II and III to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Geneva, Switzerland: IPCC.
IPCC. (2001). Third Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge: Cambridge University Press.
Karkee, R., and Kadariya, J. (2013). Choice of health-care facility after introduction of free essential health services in Nepal. WHO South East Asia J Public Health. 2, 96–100. doi: 10.4103/2224-3151.122941
Kazi, D. S., Katznelson, E., Liu, C. L., Al-Roub, N. M., Chaudhary, R. S., Young, D. E., et al. (2024). Climate change and cardiovascular health: a systematic review. JAMA Cardiol. 9, 748–757. doi: 10.1001/jamacardio.2024.1321
Keim, M. E. (2008). Building human resilience: the role of public health preparedness and response as an adaptation to climate change. Am. J. Prev. Med. 35, 508–516. doi: 10.1016/j.amepre.2008.08.022
Khanal, S. B. S., and Boeckmann, M. (2025). Exploring barriers and facilitators to integrating health equity into health and climate change policies in Nepal – a qualitative study among federal level stakeholders. BMC Health Serv. Res. 25:687. doi: 10.1186/s12913-025-12862-y
Lamberti-Castronuovo, A., Valente, M., Barone-Adesi, F., Hubloue, I., and Ragazzoni, L. (2022). Primary health care disaster preparedness: A review of the literature and the proposal of a new framework. IJDRR. 81.
Landry, M. D., Leung, K., Retis, C., Salvador, E. C., and Sr, R. (2016). The 2015 Nepal earthquake(s): lessons learned from the disability and rehabilitation sector’s preparation for, and response to, natural disasters. Phys. Ther. 96, 1714–1723. doi: 10.2522/ptj.20150677
Lee, A. C., Booth, A., Challen, K., Gardois, P., and Goodacre, S. (2014). Disaster management in low-and middle-income countries: scoping review of the evidence base. Emerg. Med. J. 31, e78–e83. doi: 10.1136/emermed-2013-203298
Lestari, F., Paramitasari, D., Kadir, A., Firdausi, N. A., Fatmah,, Yani Hamid, A., et al. (2022). The application of hospital safety index for analyzing primary healthcare center (PHC) disaster and emergency preparedness. Sustainability 14.
Manyena Bernard, S. (2006). Rural local authorities and disaster resilience in Zimbabwe. Disaster Prev Manag 15, 810–820. doi: 10.1108/09653560610712757
Masbi, M., Tavakoli, N., and Dowlati, M. (2024). Challenges of providing of special care services in hospitals during emergencies and disasters: a scoping review. BMC Emerg. Med. 24:238. doi: 10.1186/s12873-024-01160-1
Mashari, H. A. (2022). Enhancing Private Health Sector Preparedness in Oman: An Evaluation of Effective Public-Private Partnerships in Healthcare Disaster Management. Poole, England: Bournemouth University.
Ministry of Health and Population, Nepal; New ERA, Nepal; and ICF Nepal. (2022). Report Ministry of Health and Population, Kathmandu, Nepal, 2022 Kathmandu; New ERA, Nepal; and ICF, Rockville, Maryland, USA.
MoFE G. (2021). Vulnerability and risk assessment and identifying adaptation options: summary for policymakers. Kathmandu, Nepal: Ministry of Forests and Environment (MoFE).
MoFGA G (2023). DISASTER RISK MANAGEMENT LOCALIZATION MANUAL: an operational training manual for DRM capacity building of local governments ministry of federal affairs and general administration. Nepal: Ministry of Federal Affairs & General Administration GoN.
MoHA G (2019). Nepal Disaster Risk Reduction and Management Act, 2074 And Disaster Risk Reduction and Management Rules, 2076. Kathmandu, Nepal: Minsitry of Home Affairs GoN.
MoHA G. (2022a). Risk to Resilience: Disaster Risk Reduction and Management in Nepal. Kathmandu, Nepal: Government of Nepal.
MoHA G. (2022b). Crisis to resilience: transforming through disaster risk reduction and management. Kathmandu, Nepal: Government of Nepal.
MoHA G (2022c). Mid-term review of the implementation of the Sendai framework for disaster risk reduction (2015—2030), Nepal National Voluntary Report. Kathmandu, Nepal: Ministry of Home Affairs, Government of Nepal.
MoHA G (2024). Disaster report: focus on reconstruction and resilience. Singhadurbar, Kathamndu, Nepal: MoHA G.
MoHA, G. (2018b). Disaster Risk Reduction National Policy, 2075. Kathmandu, Nepal. Retrieved from http://drrportal.gov.np/uploads/document/1476.pdf
MoHA, G. (2018a). Disaster risk reduction National Strategic Plan of action 2018–2030. Kathmandu, Nepal: Ministry of Home Affairs GoN.
MoH G. (2015). Health National Adaptation Plan (H-NAP), Climate Change Health Adaptation Strategies and Action Plans of Nepal (2016–2020). Kathmandu, Nepal: Ministry of Health and Population (MoHP).
MoHP G (2022). Vulnerability and adaptation assessment of climate sensitive diseases and health risks in Nepal. Kathmandu, Nepal: Ministry of Health and Population GoN.
Moulton, A. D., and Schramm, P. J. (2017). Climate change and public health surveillance: toward a comprehensive strategy. J. Public Health Manag. Pract. 23, 618–26.
NDRRMA G (2022). Emergency preparedness and response assessment 2022-2030: using the ready 2 respond methodology. Kathmandu, Nepal: National Disaster Risk Reduction and Maagement Authority GoN.
Nepal Disaster Risk Reduction Portal [Internet]. (n.d.) Government of Nepal. Available online at: http://www.drrportal.gov.np/ (Accessed January 30, 2024).
Nepal OD. Administrative boundaries geographic data of 753 municipalities in Nepal Nepal: CKAN API, CKAN Association. (2018). Available online at: https://opendatanepal.com/dataset/nepal-municipalities-wise-geographic-data-shp-geojson-topojson-kml (Accessed December 20, 2024).
Nepal, Pashupati NRK, Sharma, Bishnu Prasad Pangali (2018). Policies and institutions for disaster risk management in Nepal: a review. Geogr. J. Nepal. 11, 1–24. doi: 10.3126/gjn.v11i0.19546
Osuteye, E., Johnson, C., and Brown, D. (2017). The data gap: An analysis of data availability on disaster losses in sub-Saharan African cities. IJDRR 26, 24–33.
Oxford Policy Management, and Policy and Institutions Facility. (2020). Strengthening the Government of Nepal’s Portal for Data on Disaster and Disaster Risks. Oxford Policy Management. Available at: https://www.opml.co.uk/sites/default/files/migrated_bolt_files/strengthening-the-bipad-portal-for-data-on-disaster.pdf.
Phuyal, N., Bajracharya, S., Adhikari, A., Katwal, S., and Shrestha, A. (2023). Development and update of hospital disaster preparedness and response plan of 25 hub hospitals of Nepal – process documentation. J Gen Pract Emerg Med Nepal 10, 53–59. doi: 10.59284/jgpeman229
Rijal, S., Adhikari, S., and Shrestha, A. (2020). Guiding documents for disaster risk reduction and Management in Health Care System of Nepal. JNMA J. Nepal Med. Assoc. 58, 831–833. doi: 10.31729/jnma.5041
Robinson, M. (2009). Does decentralisation improve equity and efficiency in public service delivery provision? IDS Bull. 40, 22–35. doi: 10.1111/j.1759-5436.2009.00004.x
Schwerdtle, N., Ngo, T. A., Hasch, F., Phan, T. V., Quitmann, C., and Montenegro-Quiñonez, C. A. (2024). Climate change resilient health facilities: a scoping review of case studies in low and middle-income countries. Environ. Res. Lett. 19:21. doi: 10.1088/1748-9326/ad472b
Shair-Rosenfield, S. (2024). Decentralisation, intergovernmental coordination, and response to extreme events in Southeast Asia. Reg. Stud. 59:9716. doi: 10.1080/00343404.2024.2319716
Sharma, D. C. (2015). Nepal earthquake exposes gaps in disaster preparedness. Lancet 385, 1819–1820. doi: 10.1016/S0140-6736(15)60913-8
Tabish, S. A., and Syed, N. (2015). Disaster preparedness: current trends and future directions. Int J Sci Res 4, 227–252. Available online at: https://immediatecaretraining.co.uk/Plugin/Papers/assets/pdf/ICT-Disaster-Preparedness-Current-Trends.pdf
Thapa, R., Acharya, K., Bhattarai, N., and Bam, K. (2024). Readiness of the health system to provide non-communicable disease services in Nepal: a comparison between the 2015 and 2021 comprehensive health facility surveys. BMC Health Serv Res 24:1237. doi: 10.1186/s12913-024-11606-8
Tome, J., Richmond, H. L., Rahman, M., Karmacharya, D., and Schwind, J. S. (2022). Climate change and health vulnerability in Nepal: a systematic review of the literature since 2010. Glob. Public Health 17, 1406–1419. doi: 10.1080/17441692.2021.1924824
UNDRR. (2022). Health Emergency and Disaster Risk Management: An emerging framework for achieving synergies among the Sendai Framework, the 2030 Agenda for Sustainable Development, the New Urban Agenda and the Paris Agreement. Geneva, Switzerland: United Nations Office for Disaster Risk Reduction.
UNDRR. The Sendai Framework Terminology on Disaster Risk Reduction. “Preparedness” (2017). Available online at: https://www.undrr.org/terminology/preparedness (Accessed October 20, 2024).
United Nations Office for Disaster Risk Reduction (UNDRR). The Sendai Framework Terminology on Disaster Risk Reduction. (2017). Available online at: https://www.undrr.org/terminology/disaster.
Verheul, M. L. M. I., and Dückers, M. L. A. (2020). Defining and operationalizing disaster preparedness in hospitals: a systematic literature review. Prehosp. Disaster Med. 35, 61–68. doi: 10.1017/S1049023X19005181
Wallace, L. J., Agyepong, I., Baral, S., Barua, D., Das, M., Huque, R., et al. (2022). The role of the private sector in the COVID-19 pandemic: experiences from four health systems. Front. Public Health 10:878225. doi: 10.3389/fpubh.2022.878225
Walsh, L., Craddock, H., Gulley, K., Strauss-Riggs, K., and Schor, K. W. (2015). Building health care system capacity to respond to disasters: successes and challenges of disaster preparedness health care coalitions. Prehosp Disaster Med. 30, 112–22.
Watts, N., Amann, M., Arnell, N., Ayeb-Karlsson, S., Beagley, J., Belesova, K., et al. (2021). The 2020 report of the lancet countdown on health and climate change: responding to converging crises. Lancet 397, 129–170. doi: 10.1016/S0140-6736(20)32290-X
WHO (2011). Hospital emergency response checklist, An all-hazards tool for hospital administrators and emergency managers. Geneva: World Health Organization Regional Office for Europe.
WHO (2017). A strategic framework for emergency preparedness. Geneva: World Health Organization. Available at: https://www.who.int/publications/i/item/a-strategic-framework-for-emergency-preparedness.
Keywords: disaster preparedness, climate sensitive diseases, climate resilient health systems, climate change, climate change and health, LMICs, Nepal
Citation: Khanal S, Schubert T, Boeckmann M and Pradella F (2025) Assessing health facility preparedness in Nepal for addressing climate-related disasters and climate-sensitive diseases. Front. Clim. 7:1625829. doi: 10.3389/fclim.2025.1625829
Edited by:
Adugna Woyessa, Ethiopian Public Health Institute, EthiopiaReviewed by:
Connie Cai Ru Gan, Griffith University, AustraliaNathan Myers, Indiana State University, United States
Copyright © 2025 Khanal, Schubert, Boeckmann and Pradella. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Melanie Boeckmann, bWVsYW5pZS5ib2Vja21hbm5AdW5pLWJyZW1lbi5kZQ==; Sudeepa Khanal, c3VkZWVwYS5raGFuYWxAdW5pLWJpZWxlZmVsZC5kZQ==
 Sudeepa Khanal
Sudeepa Khanal Tabea Schubert
Tabea Schubert Melanie Boeckmann
Melanie Boeckmann Fabienne Pradella
Fabienne Pradella