- 1Department of Cardiovascular Surgery, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Fuwai Hospital, Beijing, China
- 2Department of Ultrasound, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Fuwai Hospital, Beijing, China
- 3Department of Intensive Care Unit, National Center for Cardiovascular Diseases, Chinese Academy of Medical Sciences and Peking Union Medical College, Fuwai Hospital, Beijing, China
Background: Pulmonary arterial hypertension (PH) is a common complication in patients with obstructive hypertrophic cardiomyopathy (OHCM). The risk factor of PH in patients with OHCM has not been fully elucidated, and even atrial fibrillation (AF) was considered a risk factor of PH. Thus, our study aimed to investigate risk factors of PH and the relationship between PH and AF in patients with OHCM.
Methods: We retrospectively enrolled 483 consecutive patients diagnosed with OHCM at Fuwai Hospital (Beijing, China) from January 2015 to December 2017. Clinical and echocardiographic parameters were compared between patients with and without PH.
Results: Eighty-two (17.0%) patients were diagnosed with PH in this study. Compared to patients without PH, those with PH were significantly older, had a lower body mass index (BMI), were more likely to be female and more symptomatic [New York Heart Association Class 3 or 4 symptoms], and had a higher AF prevalence. A multivariate analysis indicated that AF was an independent risk factor of PH (odds ratio [OR] 2.31, 95% confidence interval [CI] 1.03–5.20, p = 0.042). Moreover, PH was independently associated with a higher AF incidence after adjusting for age and left atrial diameter (OR 2.24, 95% CI 1.07–4.72, p = 0.034).
Conclusion: AF was independently associated with PH in patients with OHCM. Further, PH was significantly associated with an increased risk of AF, which suggested that AF could aggravate PH and that PH may promote AF processes, forming a vicious circle.
Introduction
Pulmonary arterial hypertension (PH), characterized by a progressive increase in pulmonary vascular resistance, leading to right ventricular dysfunction, is a common complication in patients with hypertrophic cardiomyopathy (HCM) (1, 2). Patients with HCM and PH usually have worse outcomes, a higher incidence of atrial fibrillation (AF), and even more embolic events than patients with only HCM (3, 4). Several mechanisms, such as elevated left-side diastolic pressures, secondary to diastolic dysfunction, left ventricular outflow tract (LVOT) obstruction with mitral regurgitation, and systolic dysfunction in a minority of cases, may contribute to PH in patients with HCM (5, 6). However, risk factors of PH in patients with HCM have not been fully elucidated. PH and AF share many risk factors, and even some studies indicated that AF is a risk factor of PH in patients with HCM (5, 7, 8). Whereas, whether PH is a risk factor of AF in patients with HCM is still unknown. Therefore, this study aimed to investigate the risk factors of PH and the relationship between PH and AF in patients with obstructive HCM (OHCM).
Materials and Methods
Population
A total of 483 consecutive patients diagnosed with OHCM at Ward 7 of cardiovascular surgery of the Fuwai Hospital (Beijing, China) from January 2015 to December 2017 were enrolled in this study. All patients enrolled in this study were admitted to our hospital for surgical treatment, and no outpatients were included because their complete medical records cannot be obtained. We retrospectively analyzed patient echocardiographic data and divided patients into patients with PH (N = 82) and patients without PH (N = 401) groups based on the pulmonary artery systolic pressure (PASP) at initial evaluation. Clinical and echocardiographic parameters were compared between the two groups.
AF diagnosis was based on medical records and in-hospital 12-lead echocardiography, and OHCM diagnosis was based on the 2020 American Heart Association/American College of Cardiology and the 2014 European Society of cardiology guidelines, which mainly included unexplained septal hypertrophy with a thickness >15 mm or a septal cardium with a thickness >13 mm with a family history of HCM as OHCM indicators (9, 10). A LOVT gradient ≥50 mmHg at rest or during provocation was an indicator for LVOT obstruction. PH was defined as patients having a PASP >35 mmHg (11).
All study patients signed informed consent forms before enrollment, and this study was also approved by the Ethics Committee of the Fuwai hospital. All study procedures were conducted in accordance with the ethical principles stated in the Declaration of Helsinki.
Echocardiography
Transthoracic echocardiographic studies were performed using a commercially available ultrasound system (E9 ultrasound system, GE Healthcare, Horten, Norway). Complete M-mode, two-dimensional, and Doppler studies were performed on patients in the left lateral decubitus or supine position, using standard parasternal, apical, and subcostal approaches. Diameters of cardiac chambers were presented as the maximum value of the anteroposterior diameter in cardiac cycles. Maximum left ventricular (LV) wall thickness was the greatest dimension measured at any site within the LV chamber at end diastole. The LVOT gradient was scanned with a continuous-wave Doppler ultrasound to measure the maximal outflow velocity and was estimated using the simplified Bernoulli equation. PASP was estimated from the tricuspid regurgitant jet velocity using the modified Bernoulli equation and adding to right atrial pressure (RAP) when patients' tricuspid regurgitation jet can be detected. Moreover, we measured mean pulmonary arterial pressure (PAP) through peak pulmonary regurgitation (PR) velocity among those who failed to measure PASP through the tricuspid regurgitation jet. Furthermore, mean PAP was calculated using the following formula: mean PAP = 4(peak PR velocity)2 + RAP. Patients with a mean PAP >25 mmHg were also considered to have PH. When a patient was suspected of having PH, we would detect PR end-velocity to estimated pulmonary aterial diastolic pressure (PADP) and then use an equation of mean PAP = 2/3rd of PADP + 1/3rd of PASP to calculate PASP. In this study, 79 patients diagnosed with PH through TR jet velocity and 3 patients through peak PR velocity. The RAP (5, 10, and 15 mmHg) was estimated in the subcostal view based on the inferior vena cava size and collapsibility during inspiration at rest (12, 13). More details can be found in our previous publication (14).
Statistical Analysis
Results are presented as mean ± standard deviations or as number (percentage), as appropriate. Independent variables were compared using Student's t-test, and continuous variables were compared using the Mann-Whitney U test continuous variables; the χ2 test or Fisher's exact test was used to compare nominal variables, as appropriate. A least absolute shrinkage and selection operator (LASSO) logistic regression analysis was performed to select variables associated with AF to be included in a multivariate logistic regression model (Figure 1). All p-values were two-tailed, and a p-value < 0.05 was considered statistically significant. SPSS version 26.0 (IBM), R version 3.6.0, and GraphPad Prism version 8.0 (GraphPad Software Inc., La Jolla, CA, USA) were used for calculation and illustration, respectively.

Figure 1. Feature selection using the least absolute shrinkage and selection operator binary logistic regression model. (A) Binomial deviance was plotted against the log (lambda) sequence. (B) A coefficient profile plot was produced against the log (λ) sequence. In this study, predictors were selected according to the minimum criteria. Four nonzero coefficients (age, left atrial diameter, Pulmonary arterial hypertension and rest left ventricular outflow gradient) were selected to construct a Atrial fibrillation risk predictive model.
Results
Baseline Patient Characteristics
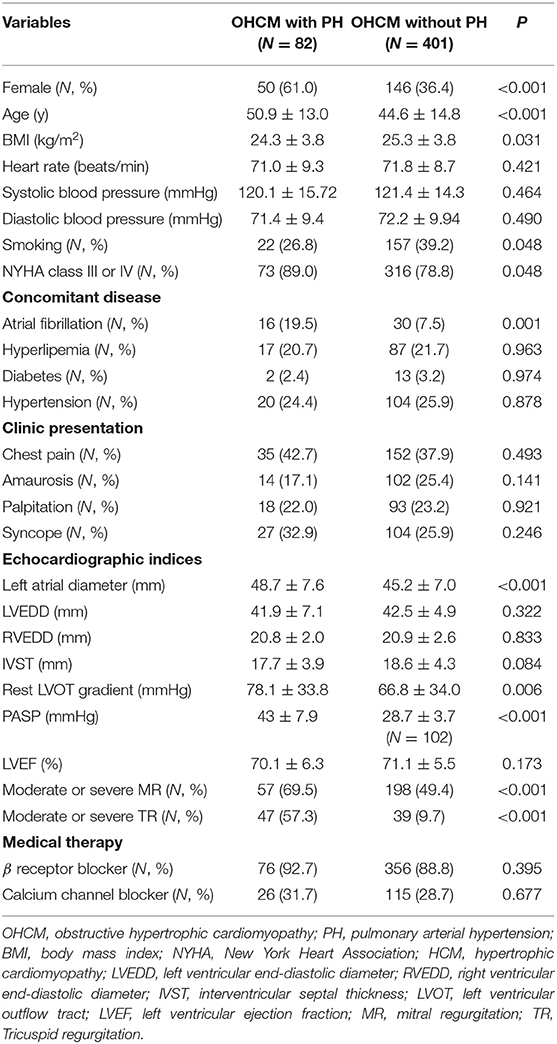
A total of 82 (17.0%) patients were diagnosed with PH at initial echocardiographic evaluation. The clinical characteristics of patients with and without PH are presented in Table 1. Compared to patients without PH, those with PH were significantly older (50.9 ± 13.0 vs. 44.6 ± 14.8, p < 0.001), had a lower body mass index (BMI) (24.3 ± 3.8 vs. 25.3 ± 3.8, p = 0.031), were more likely to be female [50 (61.0%) vs. 146 (36.4%), p < 0.001] and more symptomatic [New York Heart Association Class 3 or 4 symptoms] [73 (89.0%) vs. 316 (78.8%), p = 0.048], and had a higher AF prevalence [16 (19.5 %) vs. 30 (7.5%), p = 0.001]. Moreover, values of echocardiographic parameters such as left atrial diameter, LVOT gradient, and the proportion of moderate or severe mitral and tricuspid regurgitations were significantly higher in patients with PH than those without PH.
PASP and Clinical Parameters
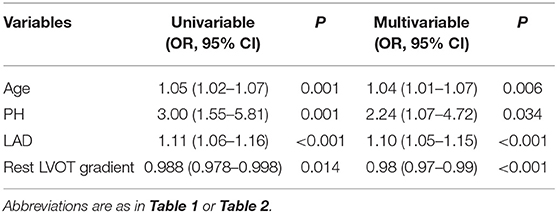
Relationships between age, left atrial diameter, right ventricular diameter, LVOT gradient and PASP are presented in Figure 2. In this study, PASP reportedly increased when left atrial diameter (Spearman rho = 0.30, p = 0.006) and pulmonary aterial diameter (Spearman rho = 0.22, p = 0.048) increased. However, we did not find a direct association between PASP and the rest LVOT gradient (Spearman rho = 0.15, p = 0.179) and age (Spearman rho = 0.06, p = 0.589). When we divided patients with PH into two groups based on PASP (PASP ≤ 50 mmHg, group I; and >50 mmHg, group II), AF prevalence was higher in patients with PH than in patients without PH; however, AF prevalence was the same in group I and group II (Figure 3).
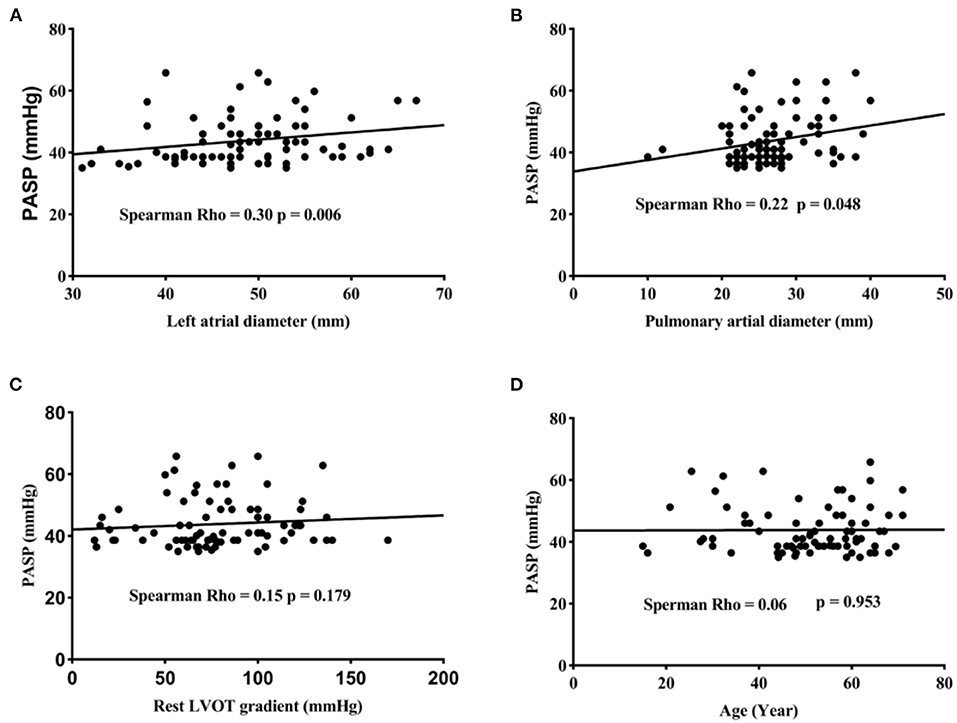
Figure 2. PASP increased with left atrial diameter (A) and Pulmonary arterial diameter (B). No relationship was found between PASP and the rest left ventricular outflow tract gradient (C). Pulmonary artery systolic pressure (PASP) is not correlated with age (D).
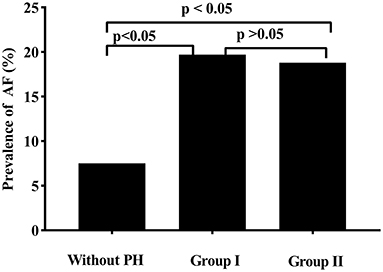
Figure 3. Compared to patients without pulmonary arterial hypertension (PH), patients with PH had a significantly atrial fibrillation (AF) higher incidence. No diffidence in AF prevalence was found between patients with a pulmonary artery systolic pressure (PASP) <50 mmHg (Group I) and patients with a PASP ≥ 50 mmHg (Group II).
Analysis of Risk Factors
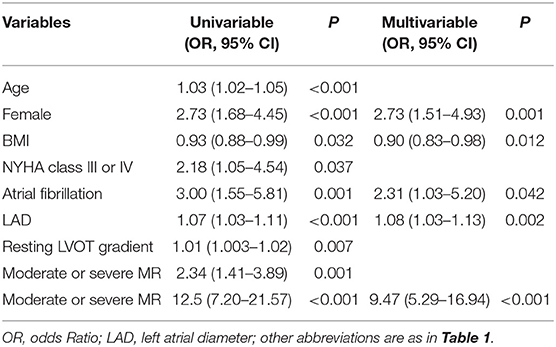
Risk factors associated with PH and AF selected from the LASSO logistic regression analysis are present in Tables 2, 3. In the multivariate analysis, in addition to female sex, BMI, left atrial diameter, and moderate or severe mitral and moderate or severe tricuspid regurgitation, AF was found to be an independent risk factor of PH (odds ratio [OR] 2.31, 95% confidence interval [CI] 1.03–5.20, p = 0.042). Furthermore, the multivariate analysis revealed that, in addition to age, left atrial diameter, and rest LVOT gradient, PH (OR 2.24, 95% CI 1.07–4.72, p = 0.034) was an independent risk factor of AF (Univariate analysis of the differences between patients with and without AF was presented in Supplementary Table 1).
Discussion
The main findings of this study are that, first, PH prevalence in this study population is ~17.0%. Second, in addition to female sex, BMI, left atrial diameter, moderate or severe mitral and tricuspid regurgitation, AF was found to be an independent risk factor of PH. Third, PH was independently associated with a higher incidence of AF, even though there was no relationship between PASP and AF prevalence.
PH Prevalence in HCM Patients
Studies concerning PH prevalence in patients with HCM were limited. PH prevalence in this single-center cohort study was 17.0%, and PH frequency was similar to that noted in Musumeci's study, which had a PH incidence of 11.4% at initial evaluation (3). In a highly selected population of patients with OHCM undergoing septal reduction therapy, PH prevalence was 53% (15). In another large HCM population, the incidence of PH was 38.2%, which included 37.5% of patients with OHCM (4). This remarkable difference in PH prevalence between studies may be caused by different PH thresholds or different PH measurement methods in the literature. Moreover, selection bias, ethnic differences, and geographical differences may also significantly contribute to this difference.
Risk Factors of PH Patients
There were several factors that may contribute to the development of PH in patients with HCM. Consistent with previous studies, our findings confirmed that PH has a strong female predominance, which suggested that sex-related differences in the production and metabolism of hormones may affect the pulmonary vasculature (4, 11, 15, 16). Further, it is previously known that left-side heart disease increases left atrial pressure, which passively reaches the pulmonary vasculature and consequently leads to vascular resistance (6). This can explain our findings that left atrial diameter and mitral regurgitation were associated with a PH higher incidence. Moreover, increased left atrial pressure led to atrial stretch and remolding, resulting in an increase in repolarization dispersion; this may allow ectopic triggers to maintain AF (7). Moreover, atrial dysfunction caused by AF usually elevates left atrial pressure, which leads to the development of post-capillary pulmonary hypertension and, subsequently, aggravated PH (5, 8). Moreover, higher BMI was found to be independently associated with a lower incidence of PH in our present study. Several studies have demonstrated a negative correlation between BMI and pulmonary arterial pressure previously, and even excess BMI was found to be a mortality protective factor in patients with PH (17–19). The obesity paradox was common in patients with cardiovascular disease, even though the mechanisms of this paradox have not been fully elucidated yet. A potential mechanism of the obesity paradox in patients with PH was that an excessive expression of sympathetic nervous activity differentially regulated the pulmonary vascular tone, thereby limiting unfavorable effects of severe PH (20). Surprisingly, although patients with PH were older than those without PH, we did not find any association between age and PH after adjusting for other variables. Furthermore, no relation was found between age and PASP in our study population. Many investigators believed that age-related ventricular dysfunction may contribute to a higher PH incidence in HCM patients (15). However, morphological features and genetic variants of HCM differed among different age groups; this had a great impact on ventricular function in patients with HCM (21, 22). Based on existing studies, the relationship between age and PH in patients with HCM remains unsolved. Further studies are needed to focus on PH mechanisms in patients with OHCM.
Impact of PH on AF
Previous studies reported a higher incidence of supraventricular arrhythmia, AF, and stroke events in patients with PH than those without PH (3, 23, 24). However, the impact of PH on AF has not been fully illustrated. In this study, we confirmed that PH was independently associated with an increased AF risk. The potential mechanism between PH and AF may be as follows. First, PH elevates right atrial pressure, leading to right atrium dilation and stretching; this results in electrical remolding, which increases propensity for AF (25). Some changes, such as the prolongation of sinus restoration time, atrial conduction slowing with a significant decrease in conduction velocity, and an increase in activation times at a global and regional level, were observed in the right atrium of patients with PH (26). An animal experiment demonstrated that PH promoted right ventricular hypertrophy due to pressure overload, resulting in a right pressure increase (27). As a result of right atrium mechanical loading, tissue fibrosis and electrical abnormalities, including altered conduction and repolarization properties, were observed (27). Moreover, an increased expression of genes related to hypertrophy, inflammation, apoptosis, and fibrosis were observed in the PH group compared to controls (27). These genes and abnormalities result in a proarrhythmic substrate that increases AF vulnerability. Thus, further studies in the future need to be conducted with an emphasis on the mechanism between right-side heart dysfunction and AF.
Clinical Implication
Pulmonary hypertension is a common complication in patients with HCM and is usually associated with worse survival. A large population study reported a 40% risk of death at 10 years after the initial evaluation of OHCM in patients with PH who were treated medically; this rate is two-fold higher than in OHCM patients without PH (4). Moreover, higher incidences of AF and strokes were observed in patients with PH than in those without PH (3). Conversely, the risk of death at 10 years postoperatively in OHCM patients with PH was similar to those without PH, meaning that relieving the outflow gradient abolished unfavorable outcomes associated with PH in patients with OHCM (4). Another study confirmed that surgical myectomy treatments could reduce right ventricular systolic pressure in HCM patients with PH, especially in patients with moderate or severe PH (15). Besides, PH continued to decline during follow-up among those patients (15). Relieving the outflow gradient in patients with OHCM could decrease PH via improving left ventricular function and reducing left atrial loading. Therefore, we expect that early and timely diagnosis and appropriate treatments will reduce PH in OHCM patients and will eventually improve patient symptoms and long-term prognosis.
Limitation
Our study was a single-center, retrospective, observational study with some inherent limitations. Due to the relatively small sample size of patients diagnosed with PH, our study findings should be prudently extrapolated to other centers, and further studies with a larger population are needed to confirm our results. Moreover, because of the retrospective nature of data collection, some factors, such as right atrial diameter, main pulmonary arterial diameter, level of right atrial fibrosis, and the electric remolding of the right atrium could not be evaluated in this study. This limited our ability to illustrate the role of PH in AF development directly. Moreover, PH assessment was based on echocardiography, not right heart catheterization, which is the gold standard for evaluating pulmonary pressure.
In conclusion, in addition to female sex, BMI, left atrial diameter, moderate or severe mitral and tricuspid regurgitation, AF was found to be independently associated with PH in patients with OHCM. Further, PH was independently associated with an increased risk of AF, which suggested that AF could aggravate PH and that PH may promote AF processes, forming a vicious circle.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author.
Ethics Statement
The studies involving human participants were reviewed and approved by Ethics Committee of Fuwai Hospital. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
CN and SYW contributed to the design of the study. CN, CZ, and MX contributed to the data collection and analysis, while all authors contributed to data interpretation. CN drafted the manuscript and ZL, QY, YM, and RW contributed significantly to the preparation. All authors critically revised the manuscript and gave final approval and agreed to be accountable for all aspects of the work, to ensure its integrity and accuracy.
Funding
This work was supported by Capital's Funds for Heath Major Project of Beijing Municipal Commission of Health (Grant Number: 2020-2-4036).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
The authors' deepest gratitude goes to the Information Center of Fuwai Hospital for providing us data collection of this study.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.666431/full#supplementary-material
References
1. Thenappan T, Ormiston ML, Ryan JJ, Archer SL. Pulmonary arterial hypertension: pathogenesis and clinical management. BMJ. (2018) 360. doi: 10.1136/bmj.j5492
2. Spirito P, Ferrazzi P. Pulmonary hypertension in hypertrophic cardiomyopathy: a forgotten marker in the identification of candidates to surgicalmyectomy? Eur Heart J Cardiovasc Imaging. (2016) 17:611–2. doi: 10.1093/ehjci/jew055
3. Kanbayashi K, Minami Y, Haruki S, Maeda R, Itani R, Ashihara K, et al. Association of elevated pulmonary artery systolic pressure with stroke and systemic embolic events in patients with hypertrophic cardiomyopathy. Int J Cardiol. (2017) 240:320–3. doi: 10.1016/j.ijcard.2017.05.019
4. Ong KC, Geske JB, Hebl VB, Nishimura RA, Schaff H V, Ackerman MJ, et al. Pulmonary hypertension is associated with worse survival in hypertrophic cardiomyopathy. Eur Heart J Cardiovasc Imaging. (2016) 17:604–10. doi: 10.1093/ehjci/jew024
5. Mitra A, Ghosh RK, Bandyopadhyay D, Ghosh GC, Kalra A, Lavie CJ. Significance of pulmonary hypertension in hypertrophic cardiomyopathy. Curr Probl Cardiol. (2020) 45:100398. doi: 10.1016/j.cpcardiol.2018.10.002
6. Vachiéry J-L, Tedford RJ, Rosenkranz S, Palazzini M, Lang I, Guazzi M, et al. Pulmonary hypertension due to left heart disease. Eur Respir J. (2019) 53:1801897. doi: 10.1183/13993003.01897-2018
7. Garg L, Gupta M, Sabzwari SRA, Agrawal S, Agarwal M, Nazir T, et al. Atrial fibrillation in hypertrophic cardiomyopathy: prevalence, clinical impact, and management. Heart Fail Rev. (2019) 24:189–97. doi: 10.1007/s10741-018-9752-6
8. Wu X, Cui H, Xiao MH, Lu J, Zhu CS, Wang SY, et al. Prevalence of pulmonary hypertension in patients with hypertrophic obstructive cardiomyopathy: a case-control study. Zhonghua Xin Xue Guan Bing Za Zhi. (2016) 44:1010–4.
9. Ommen SR, Mital S, Burke MA, Day SM, Deswal A, Elliott P, et al. AHA/ACC Guideline for the Diagnosis and Treatment of Patients With Hypertrophic Cardiomyopathy. Circulation. (2020) 42:25. doi: 10.1161/CIR.0000000000000937
10. Zamorano JL, Anastasakis A, Borger MA, Borggrefe M, Cecchi F, Charron P, et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the task force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. (2014) 35:2733–79. doi: 10.1093/eurheartj/ehu284
11. Musumeci MB, Mastromarino V, Casenghi M, Tini G, Francia P, Maruotti A, et al. Pulmonary hypertension and clinical correlates in hypertrophic cardiomyopathy. Int J Cardiol. (2017) 248:326–32. doi: 10.1016/j.ijcard.2017.07.010
12. Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, et al. Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American society of echocardiography. Endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography. J Am Soc Echocardiogr. (2010) 23:685–713. doi: 10.1016/j.echo.2010.05.010
13. Parasuraman S, Walker S, Loudon BL, Gollop ND, Wilson AM, Lowery C, et al. Assessment of pulmonary artery pressure by echocardiography-A comprehensive review. IJC Hear Vasc. (2016) 12:45–51. doi: 10.1016/j.ijcha.2016.05.011
14. Wang S, Cui H, Song C, Zhu C, Wu R, Meng L, et al. Obstructive sleep apnea is associated with nonsustained ventricular tachycardia in patients with hypertrophic obstructive cardiomyopathy. Hear Rhythm. (2019) 16:694–701. doi: 10.1016/j.hrthm.2018.12.017
15. Geske JB, Konecny T, Ommen SR, Nishimura RA, Sorajja P, Schaff H V, et al. Surgical myectomy improves pulmonary hypertension in obstructive hypertrophic cardiomyopathy. Eur Heart J. (2014) 35:2032–9. doi: 10.1093/eurheartj/eht537
16. Hester J, Ventetuolo C, Lahm T. Sex, gender, and sex hormones in pulmonary hypertension and right ventricular failure. Compr Physiol. (2019) 10:125–70. doi: 10.1002/cphy.c190011
17. Mazimba S, Holland E, Nagarajan V, Mihalek AD, Kennedy JLW, Bilchick KC. Obesity paradox in group 1 pulmonary hypertension: analysis of the NIH-Pulmonary Hypertension registry. Int J Obes (Lond). (2017) 41:1164–8. doi: 10.1038/ijo.2017.45
18. Zafrir B, Adir Y, Shehadeh W, Shteinberg M, Salman N, Amir O. The association between obesity, mortality and filling pressures in pulmonary hypertension patients; the “obesity paradox”. Respir Med. (2013) 107:139–46. doi: 10.1016/j.rmed.2012.10.019
19. Hu E-C, He J-G, Liu Z-H, Ni X-H, Zheng Y-G, Gu Q, et al. Survival advantages of excess body mass index in patients with idiopathic pulmonary arterial hypertension. Acta Cardiol. (2014) 69:673–8. doi: 10.1080/AC.69.6.1000010
20. Diong C, Jones PP, Tsuchimochi H, Gray EA, Hughes G, Inagaki T, et al. Sympathetic hyper-excitation in obesity and pulmonary hypertension: physiological relevance to the “obesity paradox”. Int J Obes (Lond). (2016) 40:938–46. doi: 10.1038/ijo.2016.33
21. Neubauer S, Kolm P, Ho CY, Kwong RY, Desai MY, Dolman SF, et al. Distinct Subgroups in Hypertrophic Cardiomyopathy in the NHLBI HCM Registry. J Am Coll Cardiol. (2019) 74:2333–45.
22. Binder J, Ommen SR, Gersh BJ, Van Driest SL, Tajik AJ, Nishimura RA, et al. Echocardiography-guided genetic testing in hypertrophic cardiomyopathy: septal morphological features predict the presence of myofilament mutations. Mayo Clin Proc. (2006) 81:459–67. doi: 10.4065/81.4.459
23. Shah TG, Sutaria JM, Vyas M V. The association between pulmonary hypertension and stroke: a systematic review and meta-analysis. Int J Cardiol. (2019) 295:21–4. doi: 10.1016/j.ijcard.2019.07.085
24. Cannillo M, Grosso Marra W, Gili S, D'Ascenzo F, Morello M, Mercante L, et al. Supraventricular arrhythmias in patients with pulmonary arterial hypertension. Am J Cardiol. (2015) 116:1883–9. doi: 10.1016/j.amjcard.2015.09.039
25. Waligóra M, Tyrka A, Miszalski-Jamka T, Urbańczyk-Zawadzka M, Podolec P, Kopeć G. Right atrium enlargement predicts clinically significant supraventricular arrhythmia in patients with pulmonary arterial hypertension. Heart Lung. (2018) 47:237–42. doi: 10.1016/j.hrtlng.2018.01.004
26. Medi C, Kalman JM, Ling L-H, Teh AW, Lee G, Lee G, et al. Atrial electrical and structural remodeling associated with longstanding pulmonary hypertension and right ventricular hypertrophy in humans. J Cardiovasc Electrophysiol. (2012) 23:614–20. doi: 10.1111/j.1540-8167.2011.02255.x
Keywords: pulmonary arterial hypertension, obstructive hypertrophic cardiomyopathy, atrial fibrillation, risk facors, left ventricular outflow tract
Citation: Nie C, Zhu C, Xiao M, Lu Z, Yang Q, Meng Y, Wu R and Wang S (2021) Risk Factors of Pulmonary Arterial Hypertension and Its Relationship With Atrial Fibrillation in Patients With Obstructive Hypertrophic Cardiomyopathy. Front. Cardiovasc. Med. 8:666431. doi: 10.3389/fcvm.2021.666431
Received: 10 February 2021; Accepted: 15 June 2021;
Published: 07 July 2021.
Edited by:
Jianzeng Dong, Capital Medical University, ChinaReviewed by:
Ribo Tang, Capital Medical University, ChinaLaura Muiño Mosquera, Ghent University Hospital, Belgium
Copyright © 2021 Nie, Zhu, Xiao, Lu, Yang, Meng, Wu and Wang. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Shuiyun Wang, d3N5bWRAc2luYS5jb20=
†These authors have contributed equally to this work and share first authorship
 Changrong Nie
Changrong Nie Changsheng Zhu1†
Changsheng Zhu1†