- 1Department of Cardiovascular Medicine, The Second Xiangya Hospital, Central South University, Changsha, China
- 2Department of Pathology, The Second Xiangya Hospital, Central South Univerisity, Changsha, China
Natural killer/T-cell (NK/T-cell) lymphoma is a rare-type non-Hodgkin lymphoma derived from NK cells or cytotoxic T cells. Here, we present a case of a 40-year-old woman who experienced quick-developed global heart failure and then was diagnosed with NK/T-cell lymphoma through lymphoid biopsy. Neither transthoracic echocardiography nor any radiological images detected a mass in her heart or pericardium. Elevated plasma troponin level and diffused patchy areas of gadolinium late enhancement on cardiac magnetic resonance were compatible with myocarditis. Considering the persistently elevated cytokine level, systemic inflammation symptoms, acute respiratory distress syndrome, and cardiac dysfunction, a cytokine storm secondary to NK/T-cell lymphoma was considered. Due to the refractory malignant arrhythmia, the patient died soon after being admitted to our hospital.
Introduction
Natural killer (NK)/T-cell lymphoma (NKTL) is a rare and aggressive type of non-Hodgkin lymphoma derived from NK cells or cytotoxic T cells (1). NKTL mostly occurs in the nasal area and upper aerodigestive tract; although extranodal lymphoma was reported in about 30% of non-Hodgkin lymphoma (NHL) (2), cardiac NHL is rarely reported in clinical settings (3, 4).
Compared with diffuse large B-cell lymphomas and T-cell lymphomas, NKTL has a higher tendency to invade heart. Moreover, the presence of cardiac involvement is associated with poor prognosis in patients with lymphoma (5).
Cytokine storm is an umbrella term encompassing several disorders of immune dysregulation characterized by constitutional symptoms, systemic inflammation, and multiple dysfunctions that can lead to multiorgan failure (6). There are multiple clinical causes of cytokine storms, including iatrogenic, pathogen-induced, and monogenic and autoimmune disorders. Of note, hemophagocytic lymphohistiocytosis caused by Epstein–Barr virus (EBV) infection in patients with genetic susceptibility can trigger a cytokine storm (6).
Here, we report a case of an EBV-positive NKTL patient who presented progressive heart failure as an initial manifestation without evidence of cardiac lymphoma infiltration, and a lymphoma-induced cytokine storm was considered the cause of cardiac injury and rapidly deteriorating heart failure.
Case Presentation
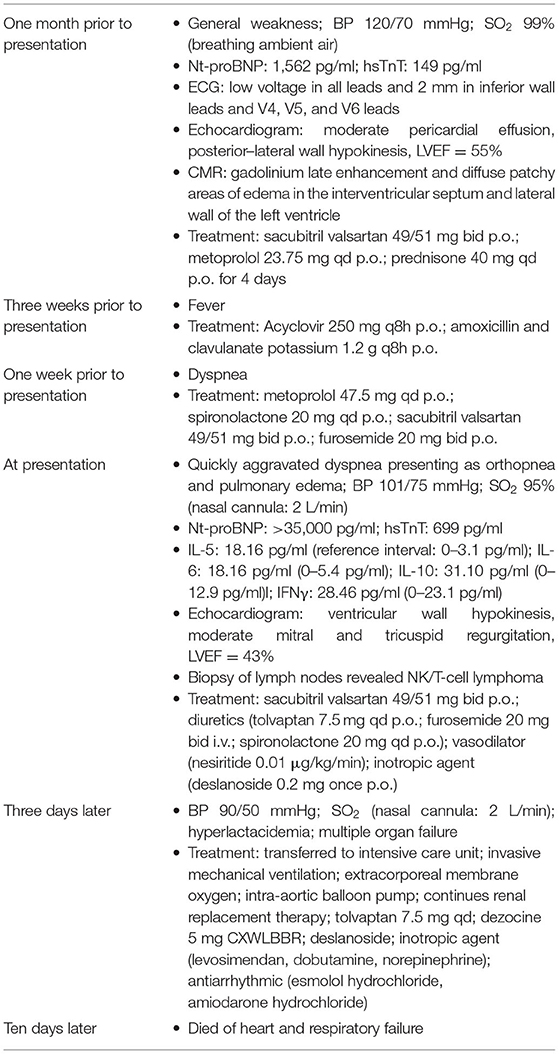
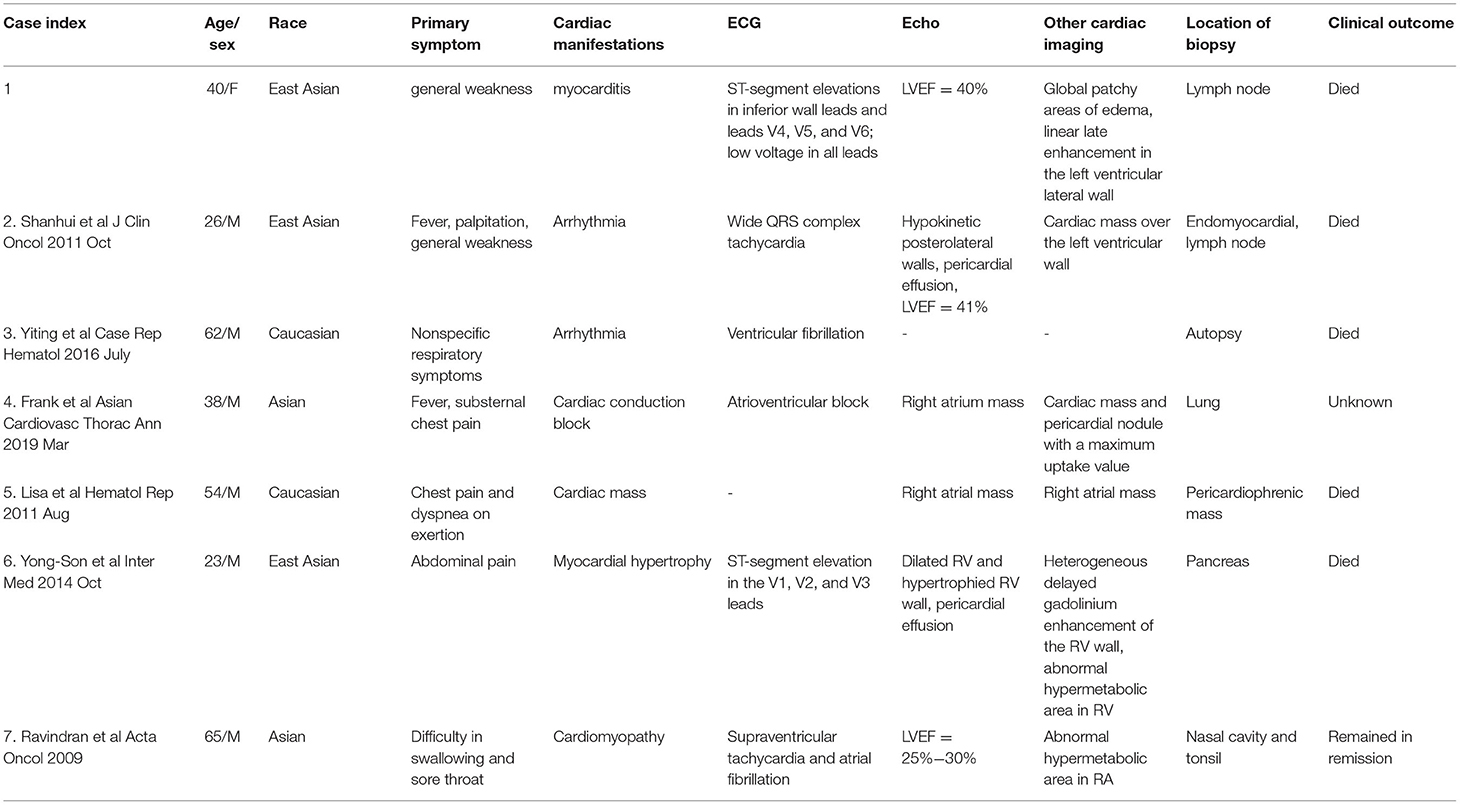
A 40-year-old woman was admitted to our hospital because of fever and orthopnea. A month before her admission, she felt general weakness and was hospitalized. At that time, a laboratory test found increased N-terminal pro-brain natriuretic peptide (Nt-proBNP: 1,562 pg/ml), high-sensitivity troponin (hsTnT: 149 pg/ml), and DNA load of EBV (1,890 copies/ml). The 12-lead electrocardiography demonstrated low voltage in all leads and ST-segment elevation of 2 mm in inferior wall leads and leads of V4, V5, and V6 (Figure 1). A transthoracic echocardiogram showed a moderate pericardial effusion, posterior–lateral wall hypokinesis, and normal left ventricular contractility (LVEF = 55%). As acute coronary disease was considered, coronary angiography was performed and revealed normal coronary arteries with no atheromatous finding. Cardiac magnetic resonance (CMR) showed global gadolinium late enhancement and diffuse patchy areas of edema in the interventricular septum and lateral wall of the left ventricle (Figure 1). Myocarditis was presumptively diagnosed. The patient was prescribed with prednisone at 40 mg qd, but her condition did not improve and even deteriorated. When she was transferred to our hospital, she had severe heart failure (NYHA IV) and could not lay down more than a few minutes; otherwise, she would be out of breath. On admission, she was found to have a fever, several enlarged cervical lymph nodes measuring 0.5 cm, and enlargement of the liver and spleen. Lab tests revealed that NT-proBNP was more than 35,000 pg/ml and that hsTnT was 699 pg/ml. The patient had elevated IL-5 (18.16 pg/ml), IL-6 (18.16 pg/ml), IL-10 (31.10 pg/ml), and IFNγ (28.46 pg/ml). An echocardiogram showed ventricular wall hypokinesis and moderate mitral and tricuspid regurgitation, LVEF = 43% (additional files). Biopsy of the enlarged cervical lymph nodes was performed, and the histopathology showed atypical T cells with prominent hyperplasia and necrosis and lymph nodes lacking lymphoid follicles with structure destruction. A immunohistochemical study showed that these malignant cells were positive for CD4, CD3ε, CD163, and CD56 (Figure 2). EBV in situ hybridization was also positive (Figure 2). These features were compatible with the diagnosis of NKTL. Positron emission tomography-computed tomography (PET-CT) was not performed as the patient could not lie down.
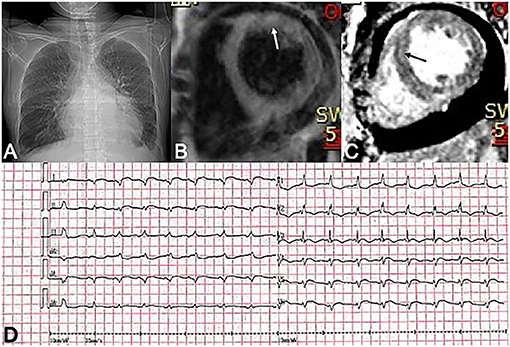
Figure 1. (A) A chest X-ray shows pleural effusion and enlarged heart shadow. (B,C) Diffuse patchy areas of edema (white arrow) and heterogeneous delay enhancement (black arrow) in the left ventricle on CMR images. (D) ECG demonstrates low voltage in all leads and ST-segment elevations of 2 mm in inferior wall leads and leads of V4, V5, and V6.
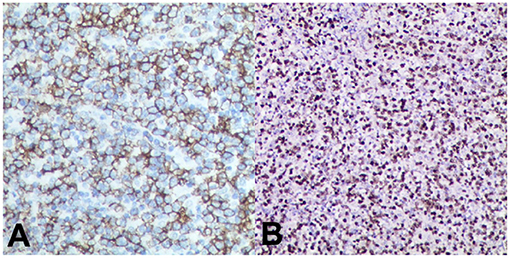
Figure 2. Immunochemistry of lymph nodes derived from the neck area. (A) Atypical cells are positive for CD56. (B) Cells are also positive for EBV with in situ hybridization.
The patient was refractory to pharmaceutical treatment for heart failure, and her condition deteriorated rapidly (7). She was transferred to the intensive care unit for circulatory and respiratory support and expired 8 days later because of cardiopulmonary failure (Table 1).
Discussion
We reported a case of NKTL who presented with a quickly aggravated heart failure, elevated troponin, and diffuse patchy edema, and late gadolinium enhancement of the left ventricle on CMR, which suggested the diagnosis of myocarditis (8). Myocardial injury in lymphoma is uncommon. Previously, infiltration of lymphoma cells into the myocardium was considered as the cause of myocardial dysfunction. Compared with B-cell lymphoma and T-cell lymphoma, NKTL was reported to have a higher incidence of cardiac infiltration (5). In these reported cases of NKTL with cardiac involvement, evidence of lymphoma infiltration, which may manifest as a cardiac mass, abnormal thickening of myocardium, and pericardial effusion, was found by echocardiogram examination, CT/PET-CT, or cardiac MRI (Table 2) (9–14). These patients exhibited variable cardiac presentation, and all had a poor prognosis.
However, different from previous reports, there was no clinically detectable evidence of cardiac lymphoma infiltration on echocardiography and on CMR in our reported case. Elevated cTnT and diffuse patchy myocardial LGE were compatible with myocarditis (8). A cytokine storm secondary to NKTL was considered the possible mechanism leading to myocardial injury, malignant arrhythmia, and respiratory failure, which was different from previous reports.
Cytokine storms and cytokine releasing syndrome are life-threatening systemic inflammatory syndromes involving elevated levels of circulating cytokines and immune-cell hyperactivation that can be triggered by various reasons (6). For instance, the Coronavirus Disease 2019 (COVID-19) is characterized as a severe immune response caused by SARS-CoV-2 (the severe acute respiratory syndrome coronavirus 2) infection. Other causes for cytokine storms include autoinflammatory disorders, hemophagocytic lymphohistiocytosis, cancers, and monogenic disorders (6). Hematological malignancy, especially involving peripheral T cells or the NK-cell lineage, is the most common and has the worst prognosis for cytokine storm syndrome (15–17).
NK cells play a pivotal role in modulating the initial response of antigen-presenting cells and attenuate the subsequent activation of antigen-specific T cells, especially cytotoxic T lymphocytes (CTLs) (1). NK-cell dysfunction had been reported to cause the inability to terminate the inflammatory response of CTL and macrophage, ultimately leading to persistent releasing of pro-inflammatory cytokines and cytokine storms. Patients might exhibit acute systemic inflammatory symptoms and multiorgan dysfunction (18–20). Systemically elevated cytokines are known to be cardiotoxic and have the potential to result in profound myocardial injury and arrhythmia, as observed in patients with COVID-19.
Conclusion
Our case and summarized previously reported cases in this manuscript suggest that (1) the cardiovascular injury is a significant contributor to the poor prognosis in patients with NKTL. (2) The cardiac injury in NKTL can manifest with a variety of clinical presentations such as cardiac lymphoma, ventricular arrhythmia, and cytokine-mediated myocarditis. (3) CMR and/or PET-CT are more sensitive than echocardiography in detecting cardiac injury in NKTL.
Data Availability Statement
The original contributions presented in the study are included in the article/Supplementary Material, further inquiries can be directed to the corresponding author/s.
Ethics Statement
Written informed consent was obtained from the individual(s) for the publication of any potentially identifiable images or data included in this article.
Author Contributions
DP identified the case. ZZ and SW conducted the literature search and prepared the first draft of the manuscript. QL contributed to the pathological part of the study. All authors contributed to the articles and approved the submitted version.
Funding
This work was supported by the National Natural Science Foundation of China [No. 81870336 and 81670426 to DP].
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fcvm.2021.685736/full#supplementary-material
References
1. Tse E, Kwong YL. The diagnosis and management of NK/T-cell lymphomas. J Hematol Oncol. (2017) 10:85. doi: 10.1186/s13045-017-0452-9
2. Muller AM, Ihorst G, Mertelsmann R, Engelhardt M. Epidemiology of non-Hodgkin's lymphoma (NHL): trends, geographic distribution, and etiology. Ann Hematol. (2005) 84:1–12. doi: 10.1007/s00277-004-0939-7
3. McDonnell PJ, Mann RB, Bulkley BH. Involvement of the heart by malignant lymphoma: a clinicopathologic study. Cancer. (1982) 49:944–51. doi: 10.1002/1097-0142(19820301)49:5<944::aid-cncr2820490519>3.0.co;2-c
4. Gordon MJ, Danilova O, Spurgeon S, Danilov AV. Cardiac non-Hodgkin's lymphoma: clinical characteristics and trends in survival. Eur J Haematol. (2016) 97:445–52. doi: 10.1111/ejh.12751
5. Chinen K, Izumo T. Cardiac involvement by malignant lymphoma: a clinicopathologic study of 25 autopsy cases based on the WHO classification. Ann Hematol. (2005) 84:498–505. doi: 10.1007/s00277-005-1009-5
6. Fajgenbaum DC, June CH. Cytokine Storm. N Eng J Med. (2020) 383:2255–73. doi: 10.1056/NEJMra2026131
7. Bozkurt B, Coats AJS, Tsutsui H, Abdelhamid M, Adamopoulos S, Albert N, et al. Universal definition and classification of heart failure: A report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure Endorsed by Canadian Heart Failure Society, Heart Failure Association of India, the Cardiac Society of Australia and New Zealand, and the Chinese Heart Failure Association. Eur J Heart Fail. (2021) 23:352–80. doi: 10.1002/ejhf.2115
8. Ammirati E, Frigerio M, Adler ED, Basso C, Birnie DH, Brambatti M, et al. Management of acute myocarditis and chronic inflammatory cardiomyopathy an expert consensus document. Circ Heart Fail. (2020) 13:e007405. doi: 10.1161/CIRCHEARTFAILURE.120.007405
9. Kanesvaran R Tao M Huat IT Weng DT Eng DN Thye LS. Malignant arrhythmia: a case report of nasal NK/T-cell lymphoma with cardiac involvement. Acta Oncol. (2009) 48:637–9. doi: 10.1080/02841860902740923
10. Huang SH, Hsieh SC, Ko BS, Liu YB. Cardiac involvement of natural killer/T-cell lymphoma presenting with electrical storm after cardioverter-defibrillator implantation. J Clin Oncol. (2011) 29:e833–6. doi: 10.1200/JCO.2011.36.7276
11. Lepeak LM, Yang DT, Chang JE. Extranodal NK/T-cell lymphoma presenting with primary cardiac involvement. Hematol Rep. (2011) 3:e9. doi: 10.4081/hr.2011.e9
12. Baek YS, Shin SH, Yi HG, Kim DH, Woo SI, Park KS, et al. Cardiac involvement in CD56 negative primary pancreatic extranodal NK/T-cell lymphoma, nasal type, presenting with ventricular tachycardia during the early stages of chemotherapy. Intern Med. (2014) 53:2333–6. doi: 10.2169/internalmedicine.53.2764
13. Li Y, Damjanov I. Extranodal NK/T Cell Lymphoma Causing Cardiorespiratory Failure. Case Rep Hematol. (2016) 2016:2394809. doi: 10.1155/2016/2394809
14. Farfán-Leal F, Esteban A, Hinojar R, García-Cosío M, Contreras F. Primary cardiac natural killer/T-cell lymphoma, a very rare form of lymphoma. Asian Cardiovasc Thorac Ann. (2019) 27:210–2. doi: 10.1177/0218492318798230
15. Ramos-Casals M, Brito-Zerón P, López-Guillermo A, Khamashta MA, Bosch X. Adult haemophagocytic syndrome. Lancet. (2014) 383:1503–16. doi: 10.1016/S0140-6736(13)61048-X
16. Lehmberg K, Nichols KE, Henter JI, Girschikofsky M, Greenwood T, Jordan M, et al. Consensus recommendations for the diagnosis and management of hemophagocytic lymphohistiocytosis associated with malignancies. Haematologica. (2015) 100:997–1004. doi: 10.3324/haematol.2015.123562
17. Ren Q, Chan KW, Huang H, Wang Z, Fang X, Guo C, et al. Platelet-derived alpha-granules are associated with inflammation in patients with NK/T-cell lymphoma-associated hemophagocytic syndrome. Cytokine. (2020) 126:154878. doi: 10.1016/j.cyto.2019.154878
18. Filipovich AH. Hemophagocytic lymphohistiocytosis (HLH) and related disorders. Hematoly Am Soc Hematol Educ Program. (2009) 2009:127–31. doi: 10.1182/asheducation-2009.1.127
19. Chandrakasan S, Filipovich AH. Hemophagocytic lymphohistiocytosis: advances in pathophysiology, diagnosis, and treatment. J Pediatr. (2013) 163:1253–59. doi: 10.1016/j.jpeds.2013.06.053
Keywords: NK/T-cell lymphoma, heart failure, cytokine strom, inflammation, myocarditis
Citation: Zhang Z, Wang S, Liang Q and Peng D (2021) Progressive Heart Failure and Death as the Initial Manifestation of NK/T-Cell Lymphoma: A Case Report and Literature Review. Front. Cardiovasc. Med. 8:685736. doi: 10.3389/fcvm.2021.685736
Received: 25 March 2021; Accepted: 19 May 2021;
Published: 24 June 2021.
Edited by:
Cezar Angi Iliescu, University of Texas MD Anderson Cancer Center, United StatesReviewed by:
Alessandra Cuomo, Federico II University Hospital, ItalyChiara Lestuzzi, Santa Maria degli Angeli Hospital Pordenone, Italy
Copyright © 2021 Zhang, Wang, Liang and Peng. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Daoquan Peng, cGVuZ2RxQGNzdS5lZHUuY24=
†These authors have contributed equally to this work
 Ziyu Zhang
Ziyu Zhang Shuai Wang1†
Shuai Wang1†